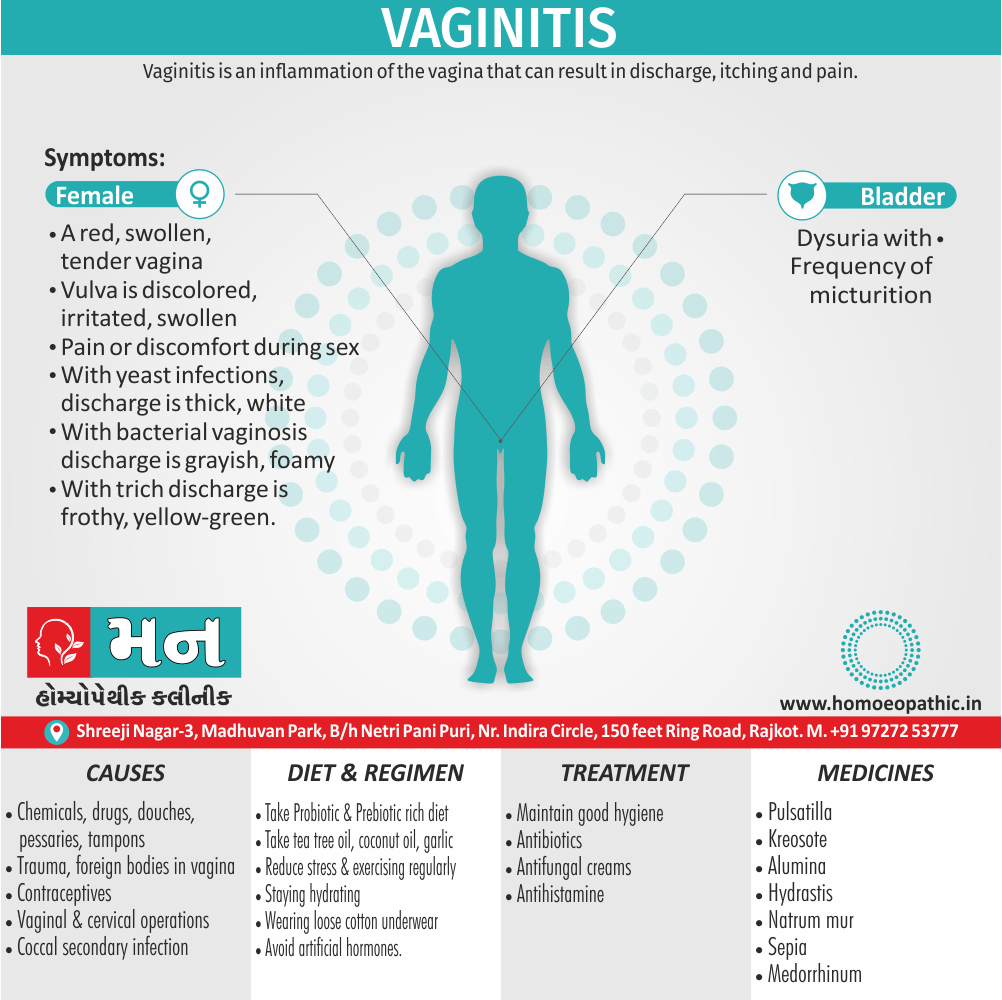
Overview of Vaginitis
Inflammatory conditions of the vulva and vagina. The cause is usually a change in the balance of vaginal bacteria or an infection.
Due to lack of estrogen, the vaginal defense is lost and the infection occurs easily, once introduced inside the vagina.[1]
Reduced estrogen levels after menopause and some skin disorders also can cause vaginitis.
Causes of Vaginitis
- Chemicals, drugs, douches, pessaries, tampons, trauma, foreign bodies such as rubber ring pessaries, contraceptives and even vaginal and cervical operations are all causative.
- Alteration in the pH towards alkalinity always favors nonspecific infection; hence, its common incidence is in the puerperium.
- The association of coccal secondary infection with trichomoniasis is important, since the isolation of the secondary organism may mask the presence of the Trichomonas, which is really responsible for the discharge.[5]
Risk factor of Vaginitis:
- Hormonal changes, such as those associated with pregnancy, birth control pills or menopause
- Sexual activity
- Having a sexually transmitted infection
- Medications, such as antibiotics and steroids
- Use of spermicides for birth control
- Uncontrolled diabetes
- Use of hygiene products such as bubble bath, vaginal spray or vaginal deodorant
- Douching
- Wearing damp or tight-fitting clothing
- Using an intrauterine device (IUD) for birth control. [2]
Classification of Vaginitis
The most common types of vaginitis are i.e.:
- Candida or “yeast” infections.
- Bacterial vaginosis.
- Trichomoniasis vaginitis.
- Either Chlamydia or Gonorrhoea.
- Viral vaginitis (herpes).
- Non-infectious vaginitis.
- Atrophic vaginitis.
Candida or “yeast” infections i.e.:
- Causative Organism Moniliasis is caused by Candida albicans, a gram-positive yeast-like fungus.
- Candida normally lives in your vagina, as well as in the mouth and digestive tract of all people, regardless of gender. An infection occurs when the normally occurring candida increases and cause bothersome symptoms.
- Discharge of Candida infection is white cottage cheese–like discharge.
- Candida infections should alert the health care provider to the patient’s use of antibiotic or immunosuppressive agents, or the presence of diabetes or human immunodeficiency virus (HIV).[3]
Bacterial vaginosis i.e.:
- Bacterial vaginosis (in other words, BV) is actually the most common vaginal infection in women of reproductive age.
- Bacterial vaginosis is caused by a combination of several bacteria that typically live in your vagina. These bacteria seem to overgrow in much the same way candida does when the vaginal pH balance is upset.
- Bacterial vaginosis is not asexually transmitted infection (STI), but it’s seen more often in sexually active people.
- Risk factors for bacterial vaginosis include: – New or multiple sexual partners, Douching, Cigarette smoking.
Trichomoniasis vaginitis i.e.:
- Vaginal trichomoniasis is the most common and important cause of vaginitis in the childbearing period.
- It is caused by Trichomonas vaginalis, a pear-shaped unicellular flagellate protozoon.
- The organism is predominantly transmitted by sexual contact, the male harbors the infection in the urethra and prostate.
- The transmission may also be possible by the toilet articles from one woman to the other or through examining gloves.
- The incubation period is 3–28 days.[1]
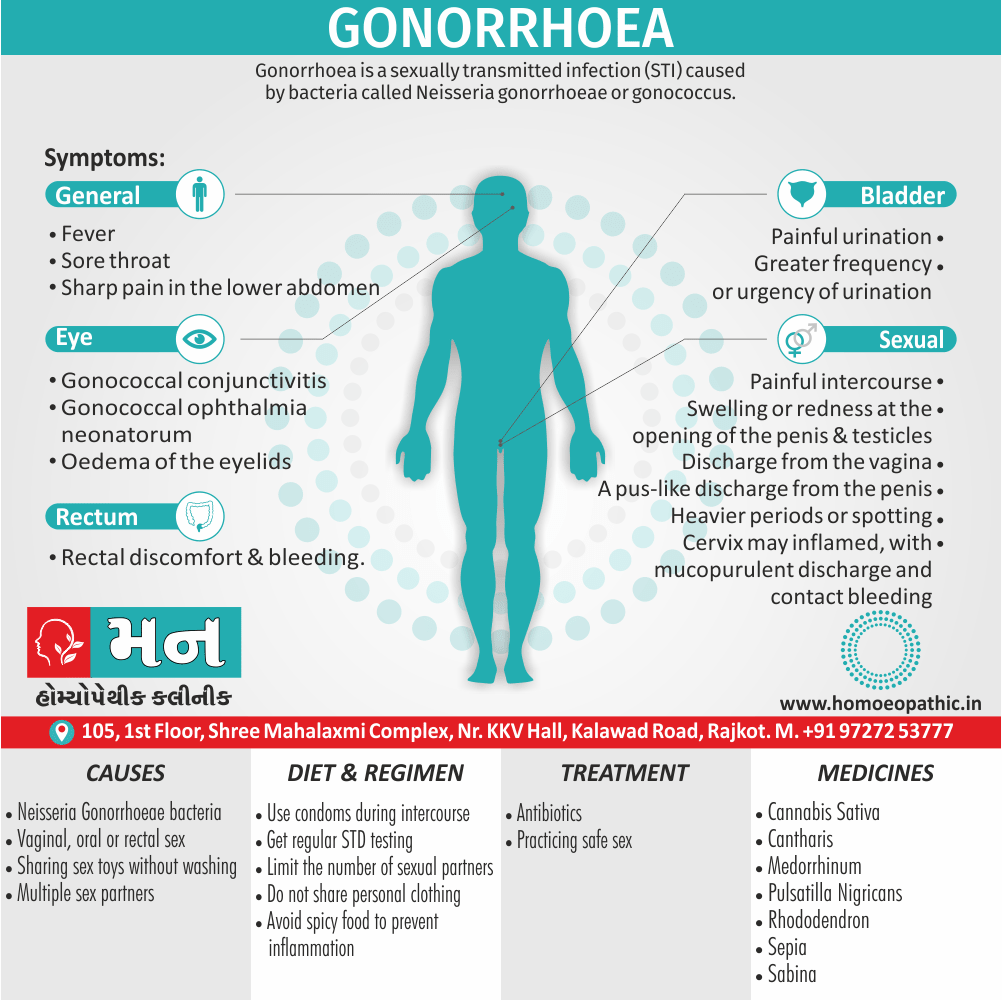
Chlamydia or Gonorrhoea i.e.:
- Chlamydia is the most common sexually transmitted infection (in other words, STI).
- Chlamydial vaginitis is most common in young adults aged 15 to 24 who have multiple sexual partners.
- Routine chlamydia screening is recommended by the Centers for Disease Control and Prevention (CDC) annually for sexually active women aged 24 and younger, and also at any age if you have multiple sexual partners, or are at risk.
- Gonorrhea, another bacterial STI, can also cause vaginitis symptoms. It often occurs with chlamydia.
- Sex partners should be tracked and treated appropriately to avoid re-infection.[4]
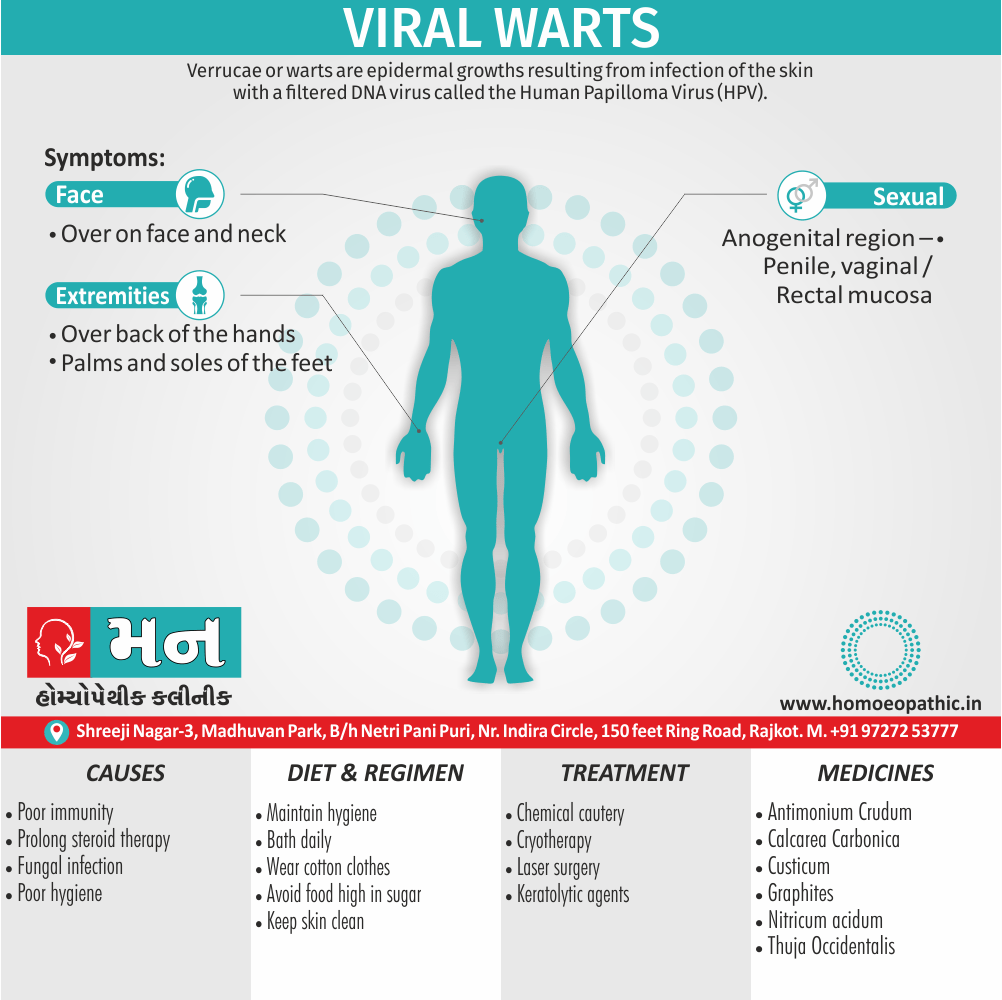
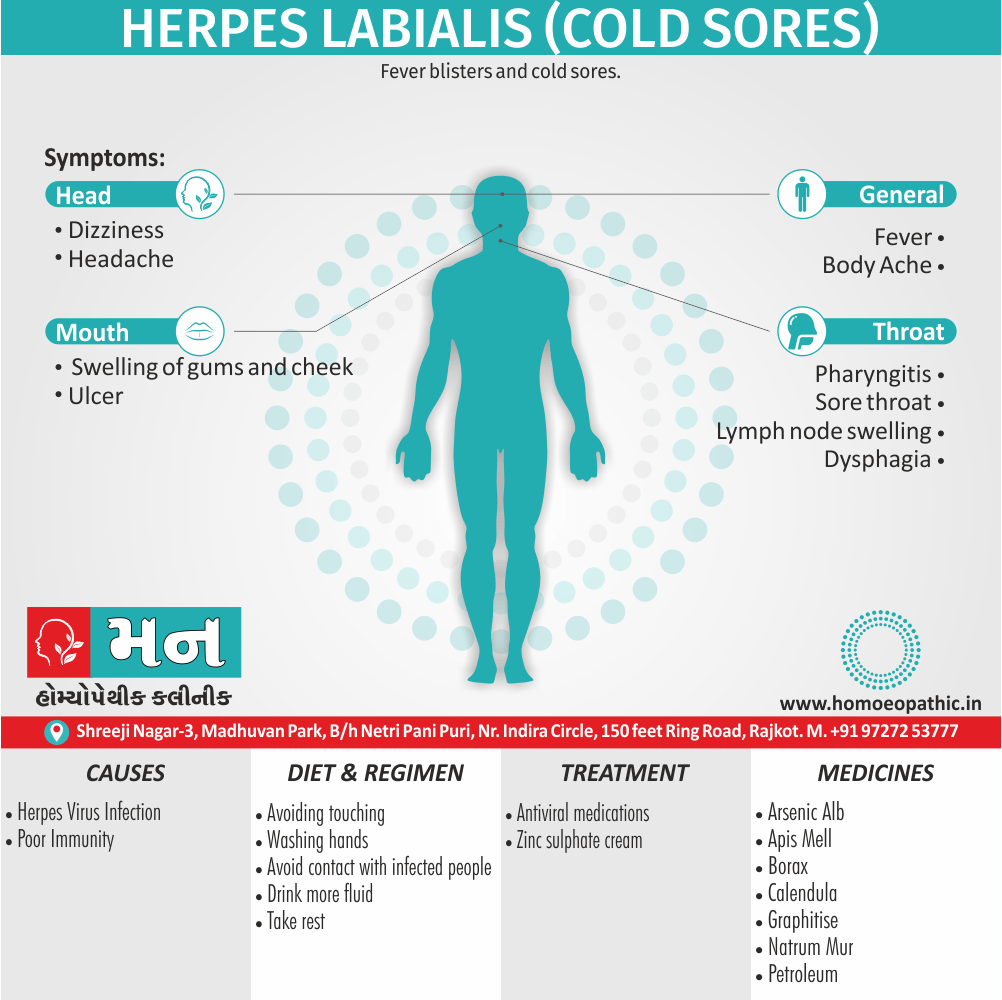
Viral vaginitis (herpes) i.e.:
Sexually transmitted viruses are a common cause of vaginitis that lead to inflammation of your genitals. The most common type of viral vaginitis is herpes simplex virus (HSV).
- Herpes simplex virus (HSV)- Herpes simplex virus is often just called a herpes infection. These infections are spread by sexual contact and often lead to painful sores. Herpes outbreaks are often associated with stress or emotional distress. You can also get herpes that affects your mouth-pharynx through oral sex.
- Low risk human papillomavirus (HPV) can lead to the development of condyloma, referred to as genital warts, and can be transmitted through vaginal, anal or oral sex.
Non-infectious vaginitis i.e.:
- Allergic reaction that causes vaginal irritation without having an infection.
- The most common cause is an allergic reaction or irritation from vaginal sprays, douches or spermicidal products.
- However, the skin around your vagina can also be sensitive to perfumed soaps, feminine products and wipes, lotions, sexual lubricants, detergents and fabric softeners.
Atrophic vaginitis i.e.:
- Vaginitis in postmenopausal women is called atrophic vaginitis. Additionally, The term is preferable to old age vaginitis.
- There is atrophy of the vulvovaginal structures due to estrogen deficiency. The vaginal defense is lost. Vaginal mucosa is thin and is more susceptible to infection and trauma. There may be desquamation of the vaginal epithelium which may lead to formation of adhesions also bands between the walls.
- Either Yellowish or blood-stained vaginal discharge.[1]
Sign & Symptoms of Vaginitis
- A red, swollen, tender vagina with irritation and burning.
- Dysuria with frequency of micturition [5]
- Our vagina and/or vulva is discolored, irritated, swollen, or uncomfortable.
- Pain or discomfort during sex.
- Vaginal discharge that isn’t normal for you:
- With yeast infections, discharge is usually thick, white, and odorless. You may also have a white coating in and around your vagina.
- With bacterial vaginosis, you may have vaginal discharge that’s grayish, foamy, and smells fishy.
- With trich, discharge is often frothy, yellow-green, smells bad, and may have spots of blood in it. [6]
Diagnosis of Vaginitis
- Review your medical history- This includes your history of vaginal or sexually transmitted infections.
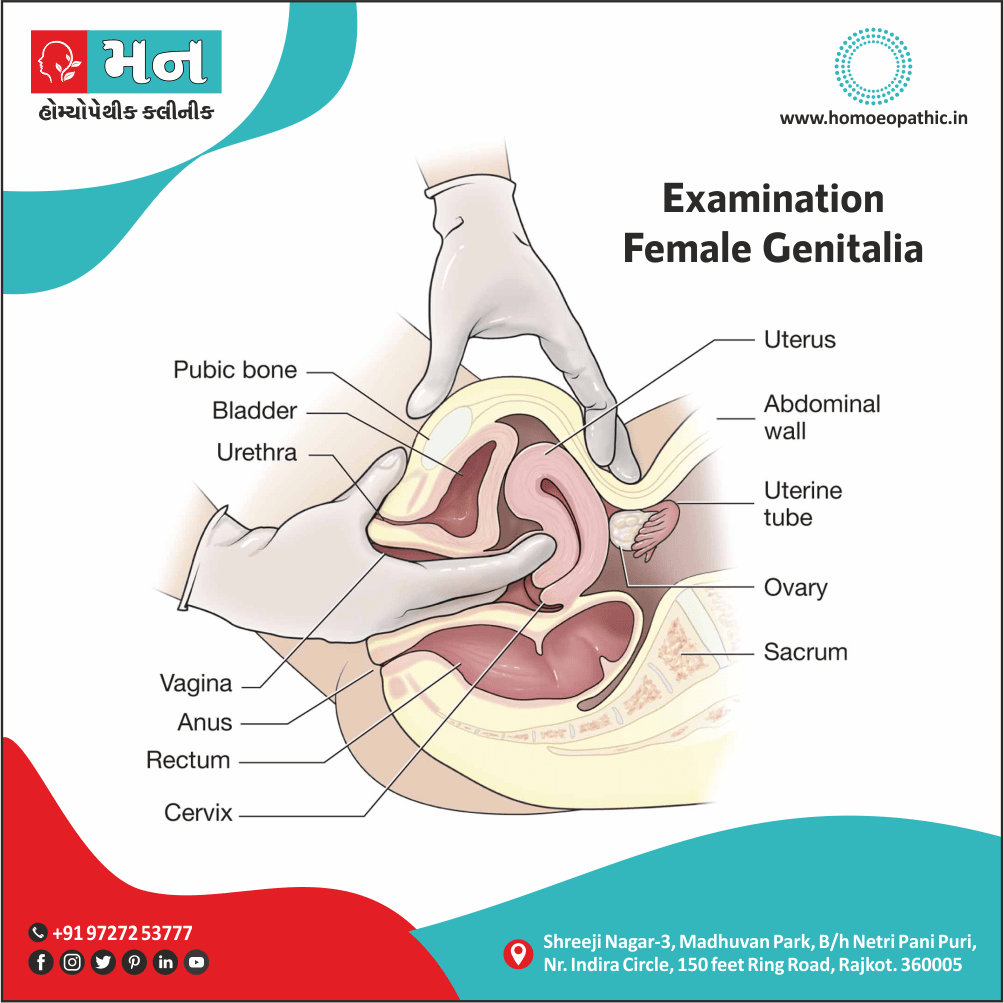
- Perform a pelvic exam- During the pelvic exam, your health care provider might use an instrument (speculum) to look inside your vagina for inflammation and discharge.
- Collect a sample for lab testing- Your health care provider might collect a sample of cervical or vaginal discharge for lab testing to confirm what kind of vaginitis you have.
- Perform pH testing- Your health care provider might test your vaginal pH by applying a pH test stick or pH paper to the wall of your vagina. An elevated pH can indicate either bacterial vaginosis or trichomoniasis. However, pH testing alone is not a reliable diagnostic test.[2]
Differential Diagnosis of Vaginitis
- Bacterial vaginosis
- Vulvovaginal candidiasis
- Trichomoniasis
- Desquamative inflammatory vaginitis
- Atrophic vaginitis
- Allergies
- Chemical irritation
- Cervicitis
- Foreign bodies. [7]
Treatment of Vaginitis
- The cause of the infection determines the appropriate treatment. It may include oral or topical antibiotics and/or antifungal creams, antibacterial creams, or similar medications.
- A cream containing cortisone may also use to relieve some of the irritation. If an allergic reaction involve, an antihistamine may also prescribe. For women who have irritation and inflammation caused by low levels of estrogen (postmenopausal), a topical estrogen cream might prescribe.
The following are typical treatments for trichomoniasis, bacterial vaginosis, and yeast infections i.e.:
- Trichomoniasis: Oral treatment with either metronidazole or tinidazole.
- "Sexual partner(s) should be treated simultaneously.
- Patients should advise to avoid sexual intercourse for at least 1 week and until they and their partner(s) have completed treatment and follow-up."
- Bacterial vaginosis: The most commonly used antibiotics are metronidazole, available in both pill and gel form, and clindamycin available in both pill and cream form.
- Yeast infections: Local azole, in the form of ovula and cream. All agents appear to be equally effective.
- These anti-fungal medications, which are available in over-the-counter form, are generally used to treat yeast infections.
- Treatment may last anywhere between one, three, or seven days.
- Trichomoniasis- Your health care provider may prescribe metronidazole (Flagyl) or tinidazole (Tindamax) tablets.
- Genitourinary syndrome of menopause (vaginal atrophy)- Estrogen — in the form of vaginal creams, tablets or rings — can treat this condition. This treatment is available by prescription from your health care provider, after other risk factors and possible complications reviewed.
- Noninfectious vaginitis- To treat this type of vaginitis, you need to pinpoint the source of the irritation and avoid it. Possible sources include new soap, laundry detergent, sanitary napkins or tampons.[2]
Prevention of Vaginitis
- Good hygiene might prevent some types of vaginitis from recurring and relieve some symptoms:
- Avoid baths, hot tubs and whirlpool spas.
- Avoid irritants – These include scented tampons, pads, douches and scented soaps. Rinse soap from your outer genital area after a shower and dry the area well to prevent irritation. Don’t use harsh soaps, such as those with deodorant or antibacterial action, or bubble bath.
- Wipe from front to back after using the toilet. Doing so avoids spreading fecal bacteria to your vagina.
- Avoid douching – Your vagina doesn’t require cleansing other than regular showering. Repetitive douching disrupts the good organisms that live in the vagina and can increase your risk of vaginal infection. Douching won’t clear up a vaginal infection.
- Practice safer sex – Using a condom and limiting the number of sex partners can help.
- Wear cotton underwear – Also wear pantyhose with a cotton crotch. Consider not wearing underwear to bed. Yeast thrives in moist environments.[2]
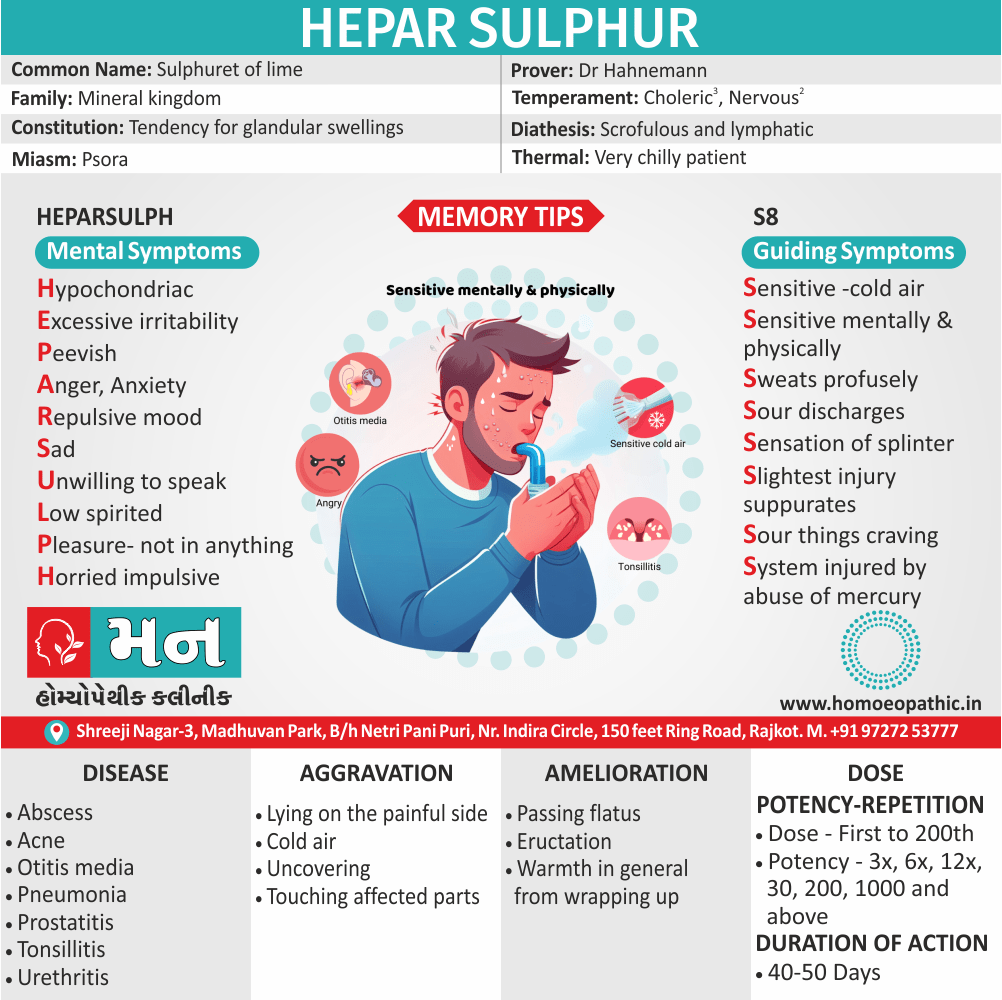
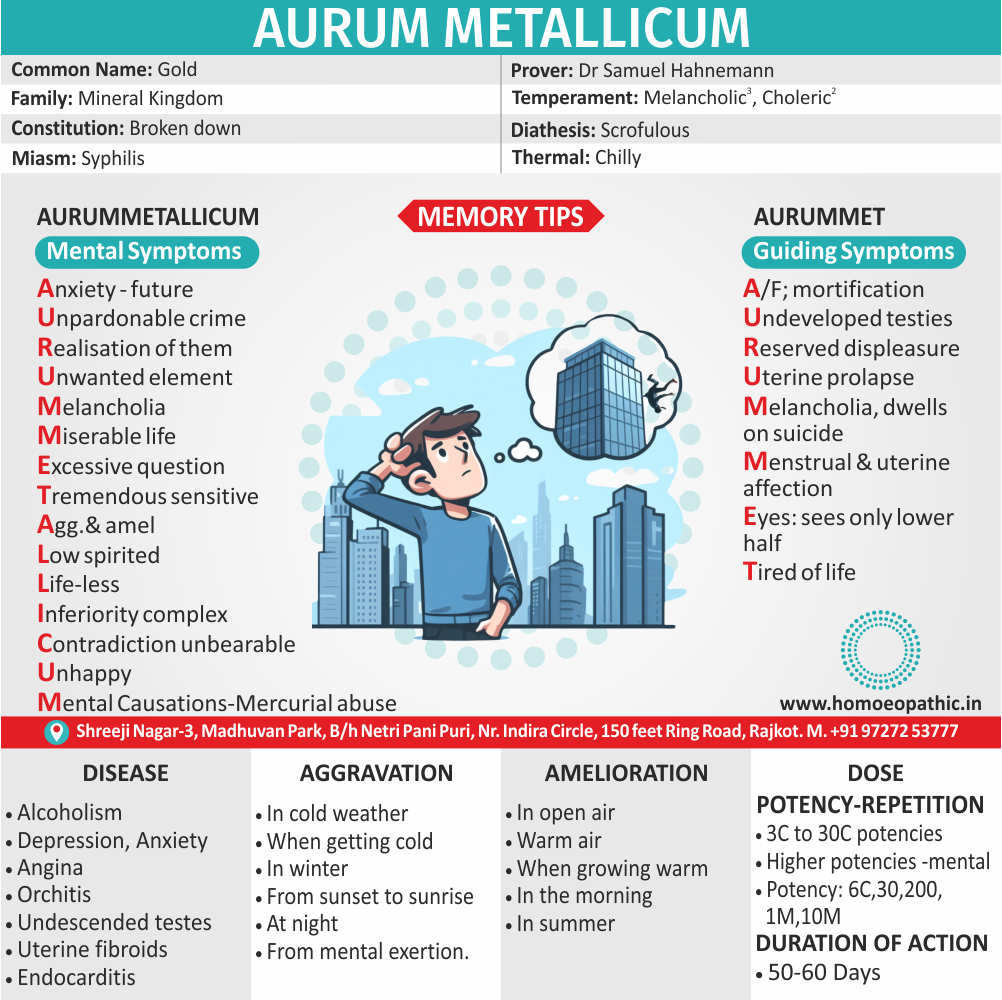
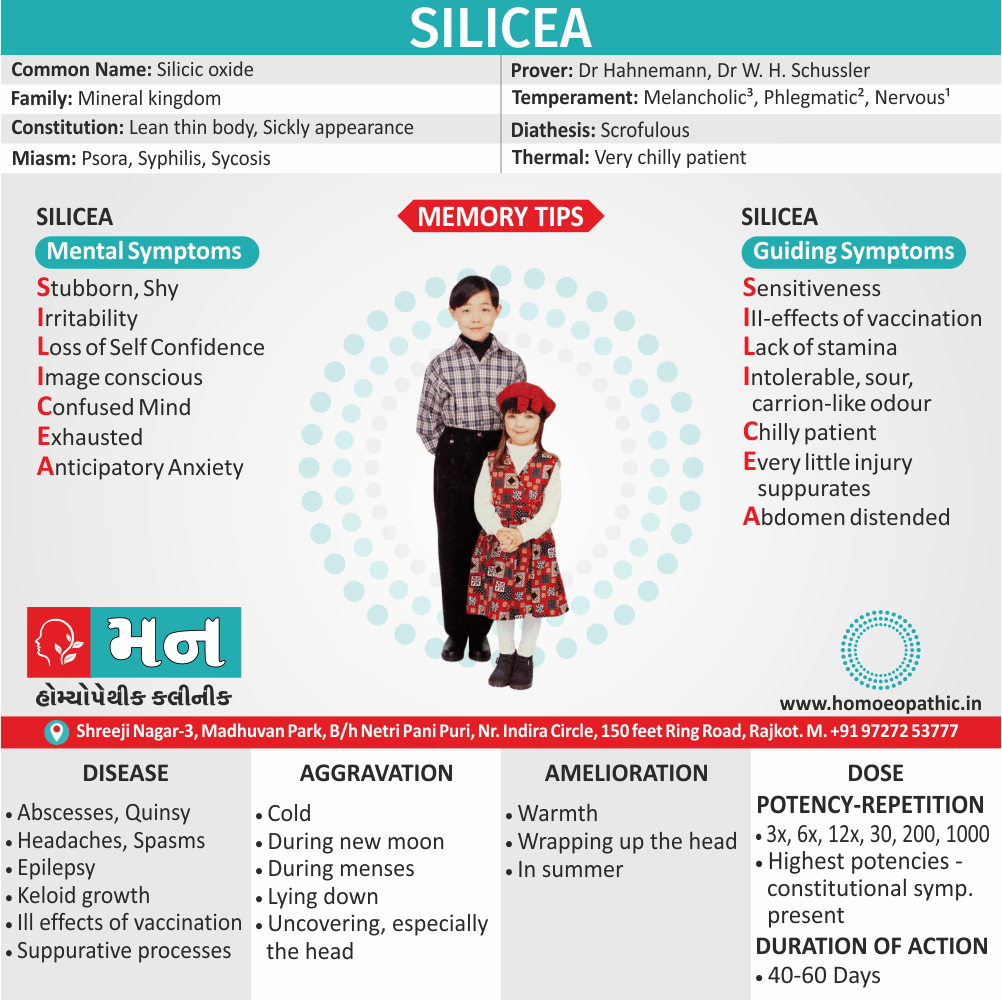
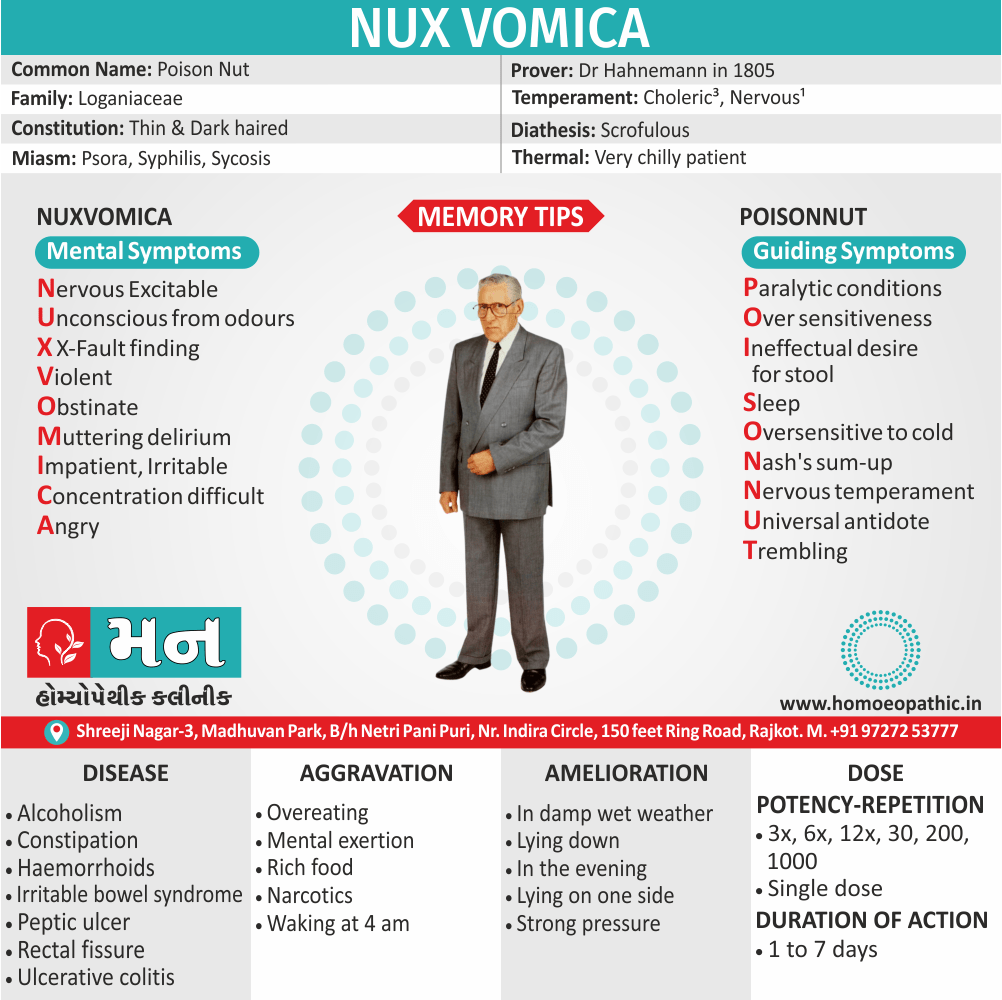
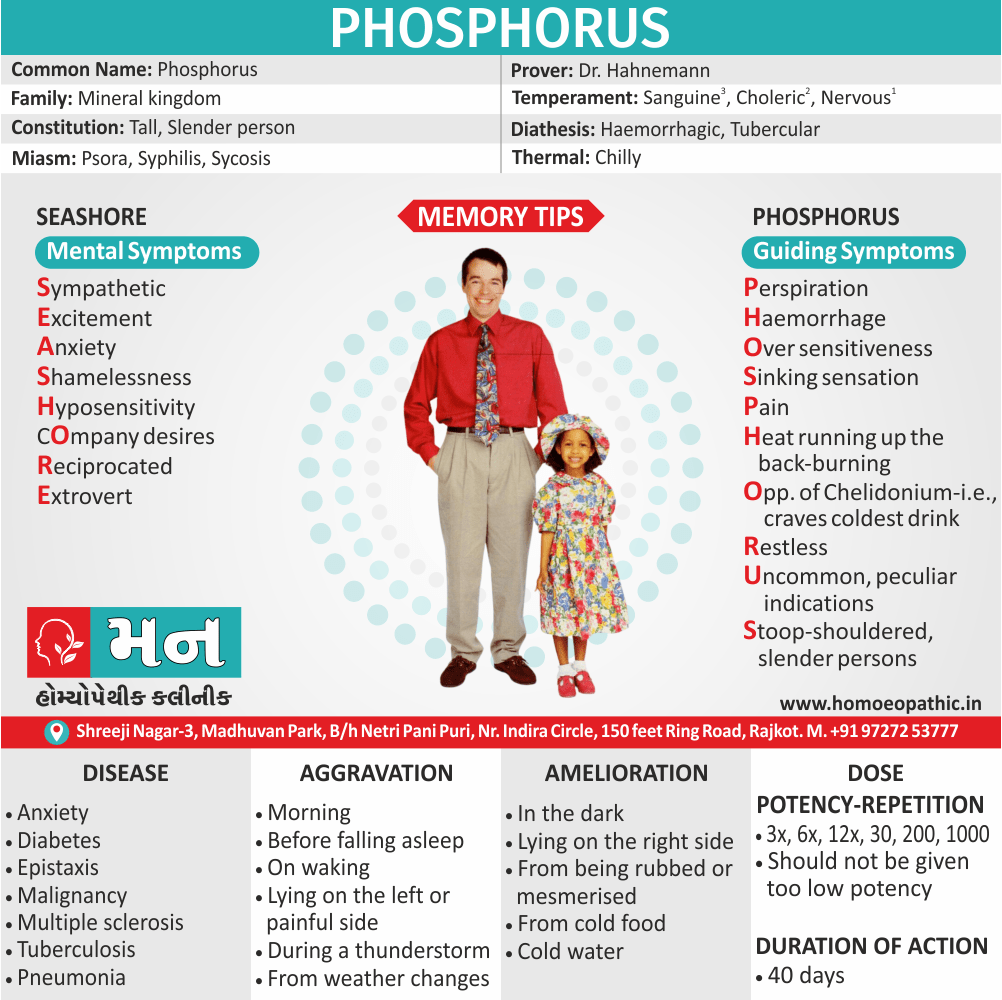
Homeopathic Treatment of Vaginitis
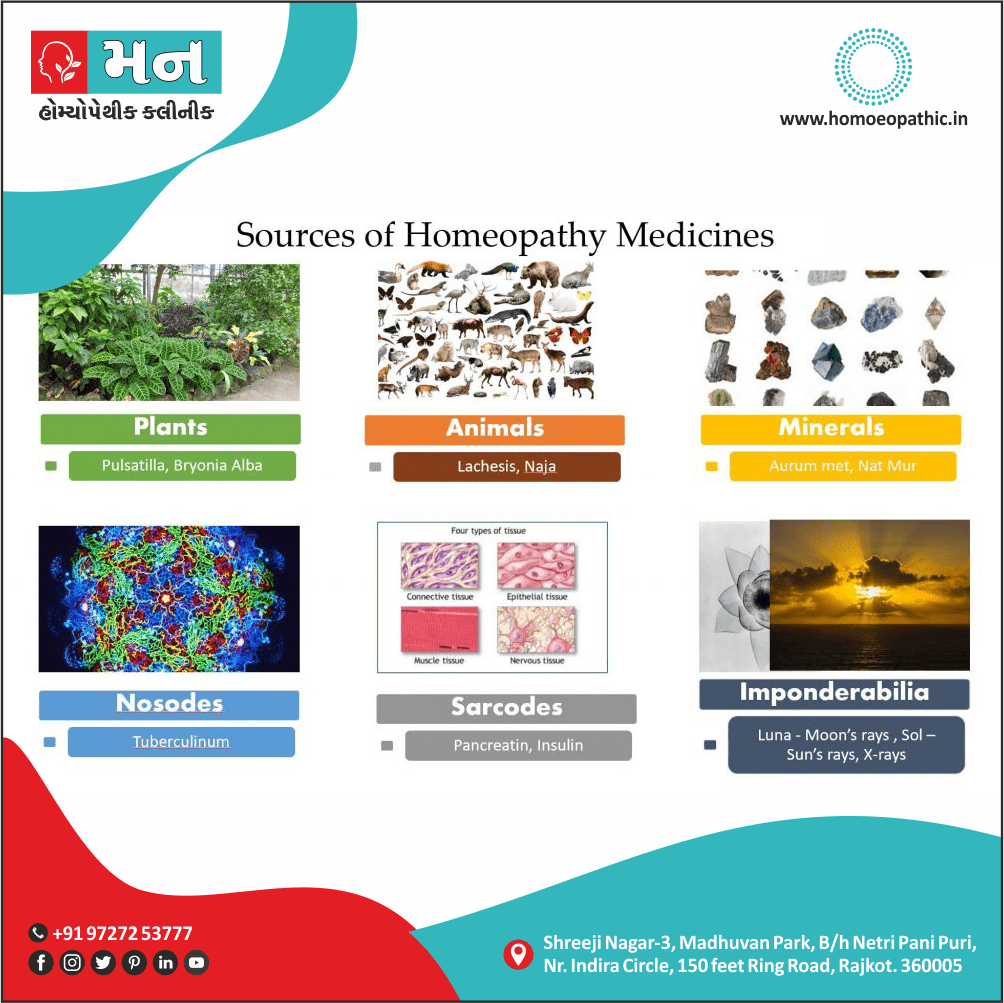
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
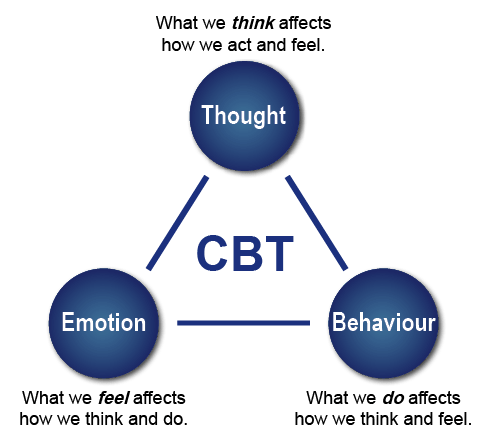
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
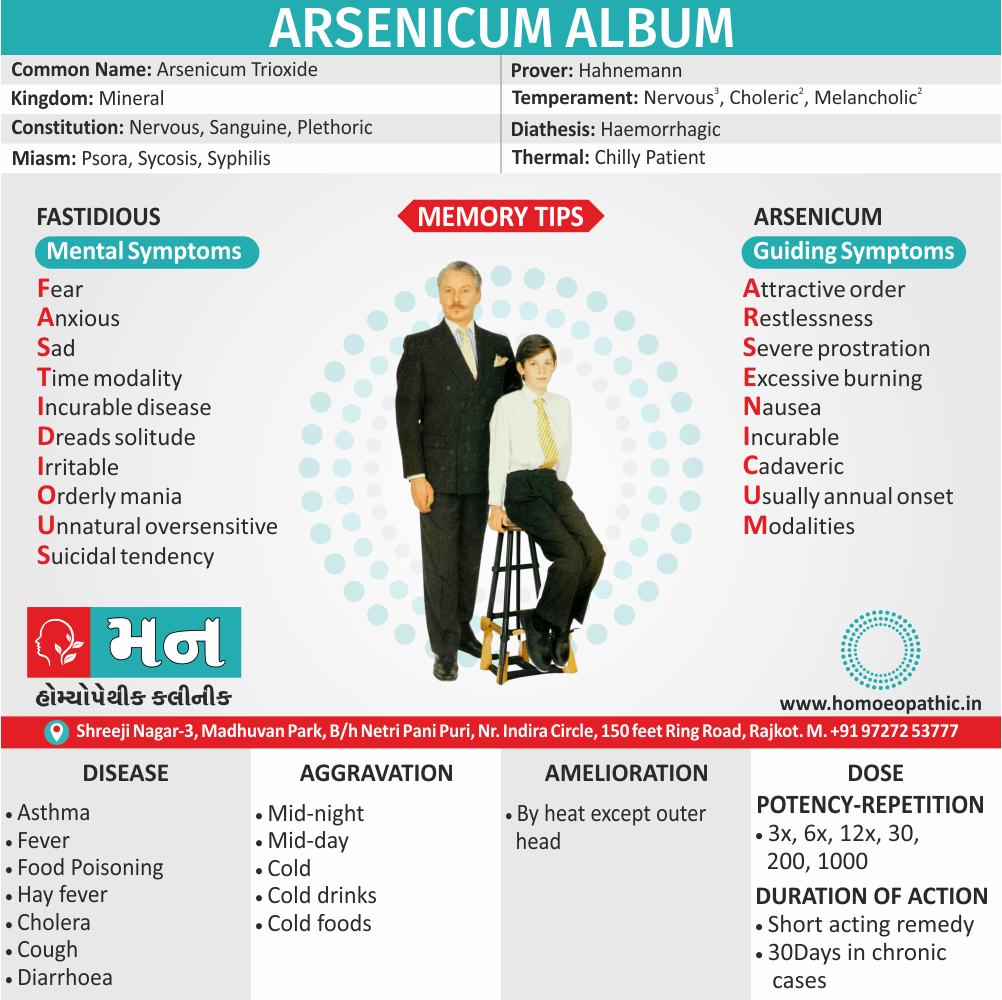
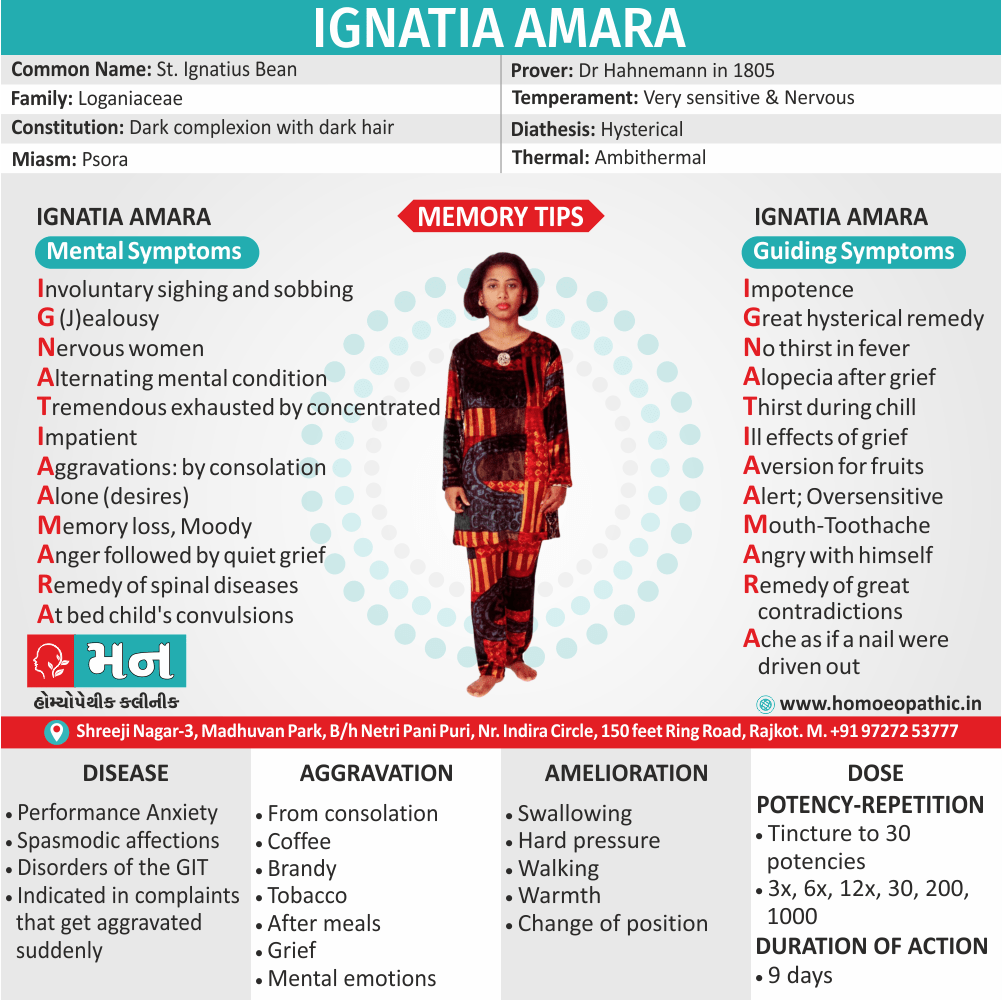
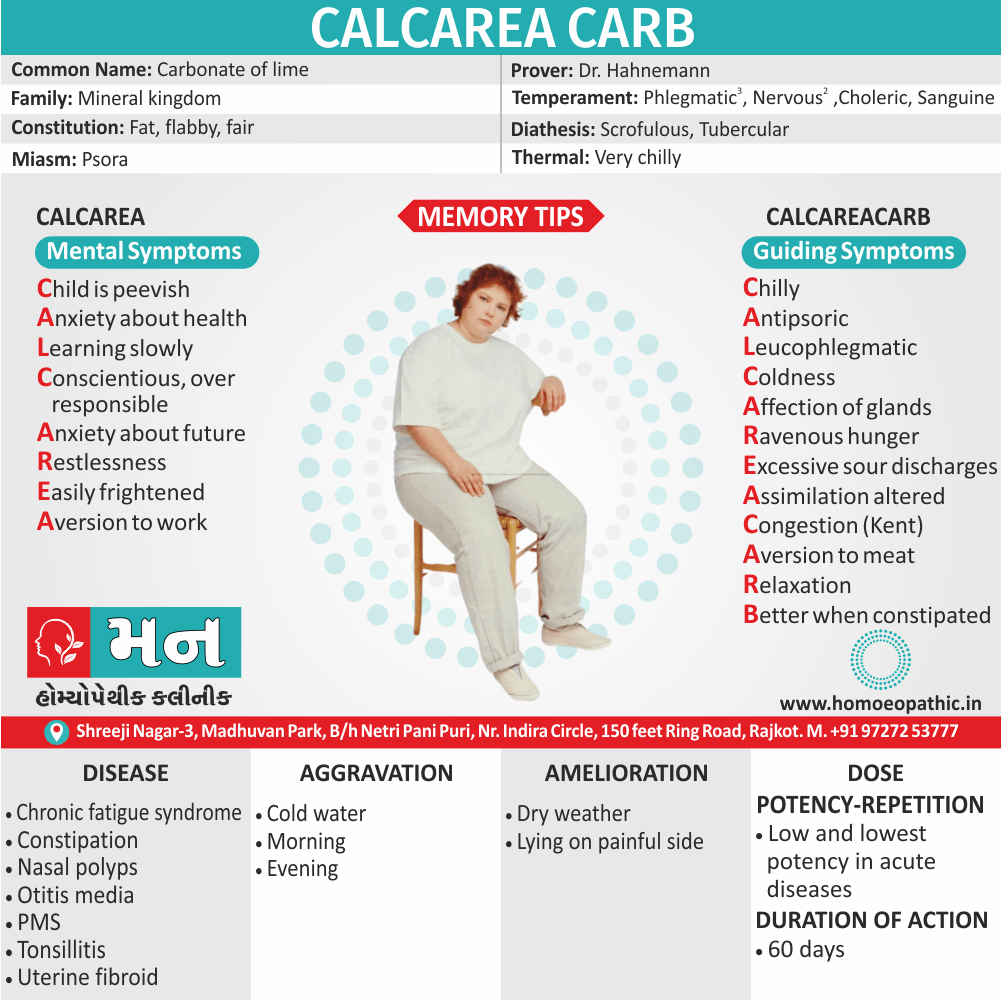
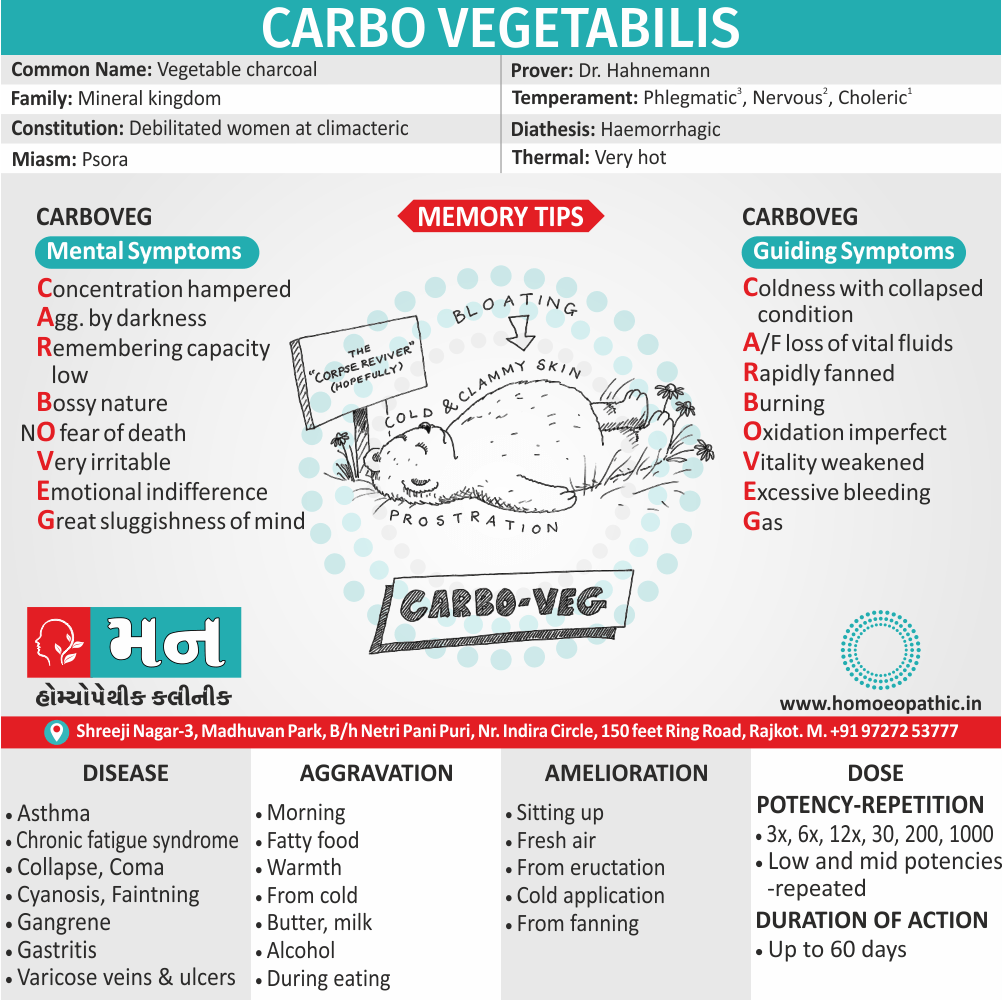
Homeopathic Medicines for Vaginitis:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
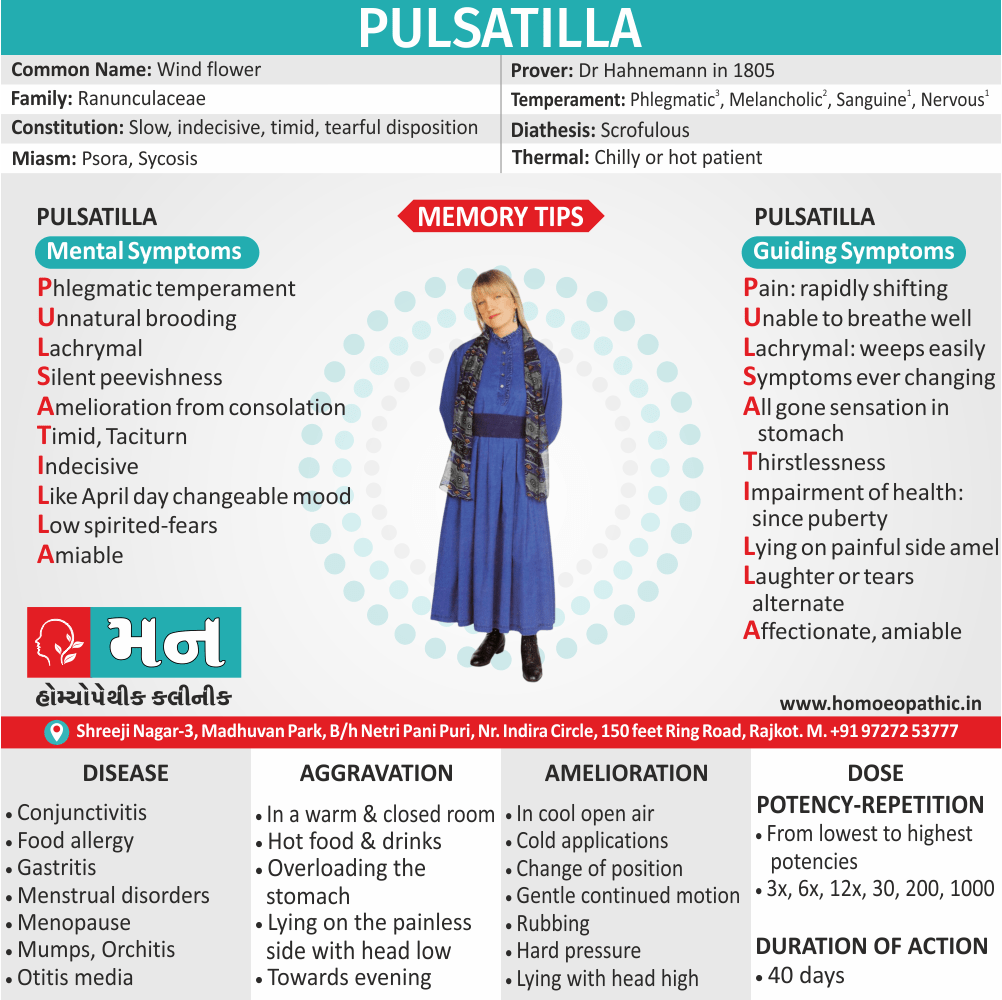
Pulsatilla – For vaginitis with Thick Vaginal Discharge
- Pulsatilla is a natural homeopathic medicine derived from a plant named Pulsatilla Nigricans or Wind-flower of the natural order Ranunculaceae.
- Pulsatilla is helpful for vaginitis when vaginal discharges are thick like cream.
- They are white (like milk) and get worse on lying down.
- There may be a burning felt in the vagina along with a backache.
Kreosote – For Itching in Vagina
- Kreosote is a natural medicine especially for itching in the vagina in cases of vaginitis.
- The itching is quite intense also violent.
- There may be soreness also burning in the vagina after scratching.
- Furthermore, The genitals are swollen too.
- The vaginal discharge may be either white or yellow and smells putrid.[4]
- Besides this, Standing and walking worsens the discharge.
- Weakness may appear with the discharges.
- Lastly, There is a frequent urge to urinate.
Alumina – For Vaginitis Vaginal Discharges Causing Burning in Vagina
- Alumina offers a natural cure for burning in the vagina due to vaginitis.
- The discharges are worse during the daytime and may be transparent or light yellow.
- They are also highly acrid, corrosive, excoriating.
- Cold washing tends to relieve the symptoms.
- In some cases, stitching and throbbing pain in the vagina is also felt.
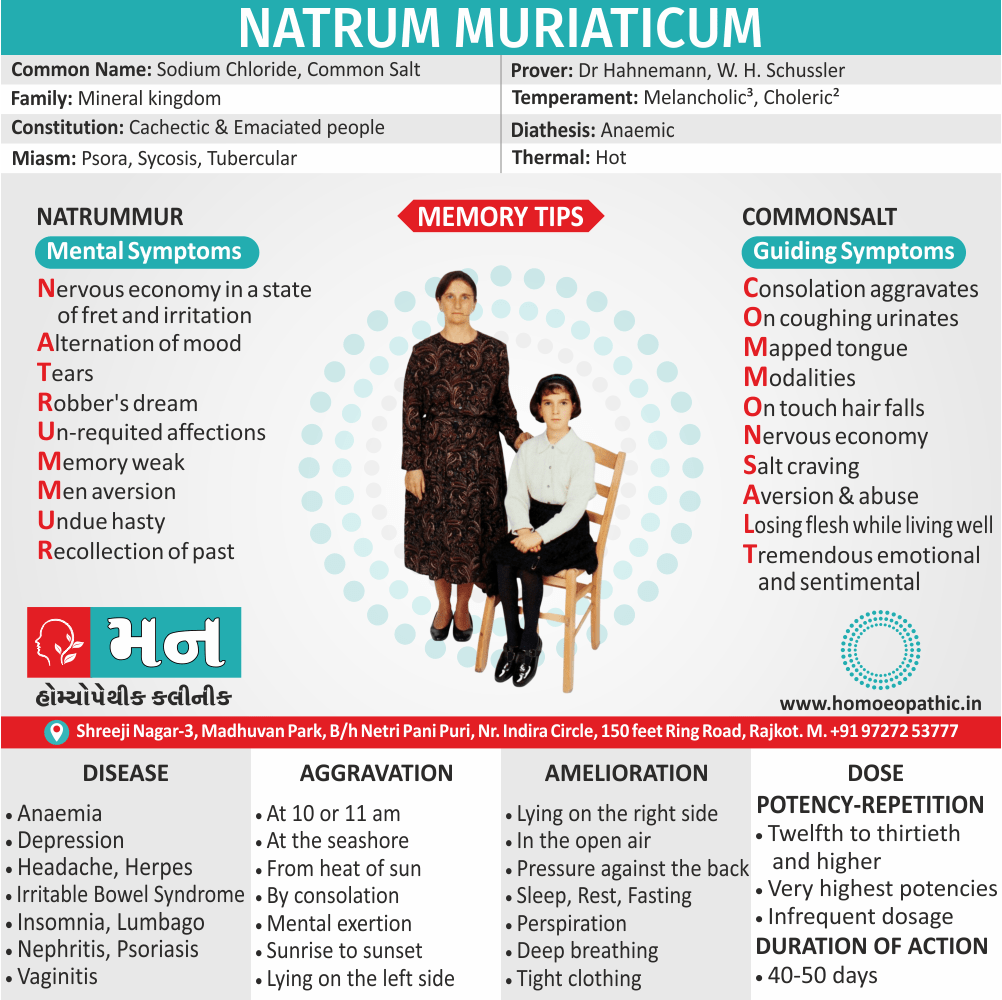
Natrum Mur – For Vaginitis with White Vaginal Discharge
- Natrum Mur is an effective natural medicine for vaginitis cases with white vaginal discharges.
- The discharges are thick and profuse and tend to get worse at night.
- They also tend to acrid and are attended with itching and a smarting pain in genitals.
- General weakness may also be present.
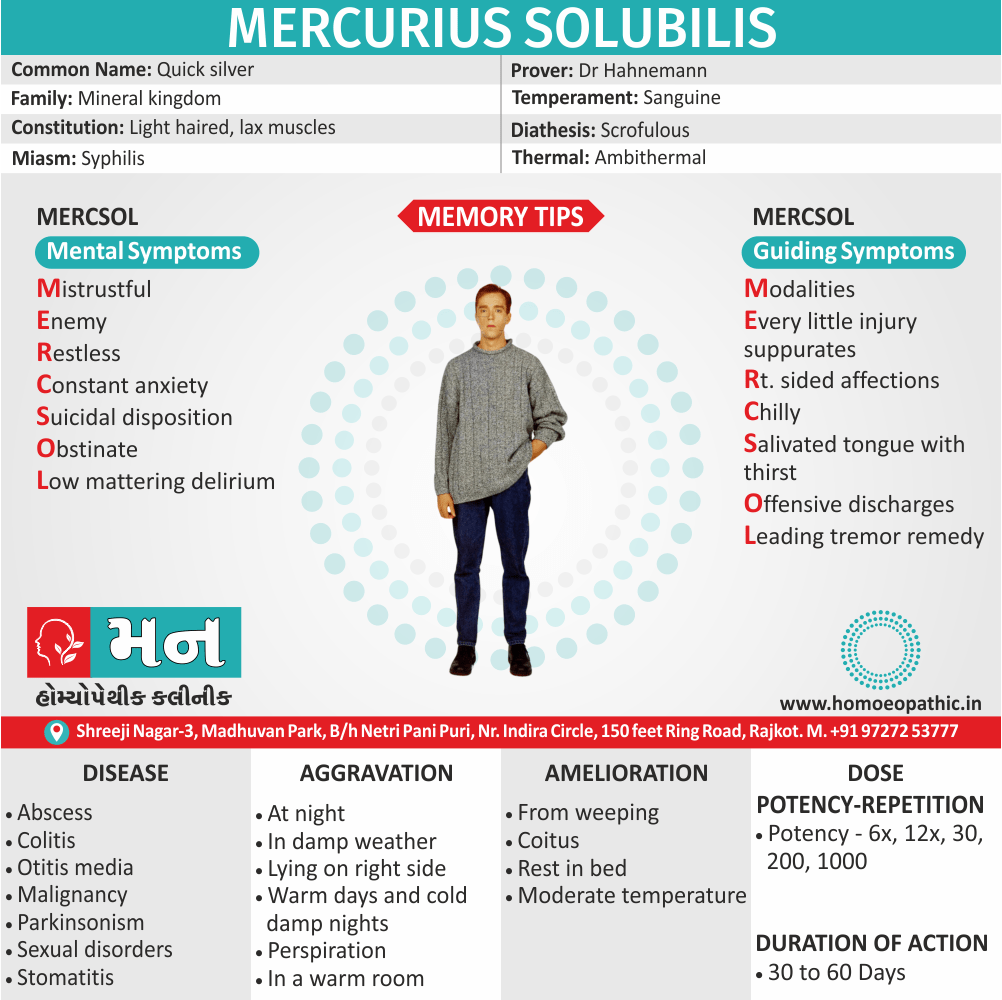
Merc Sol – For Greenish Vaginal Discharge in Vaginitis
- Merc Sol a homeopathic medicine used to treat vaginitis with greenish vaginal discharges.
- A night aggravation of the discharges may present.
- The discharges may blood-stained, corrosive and itchy, leading to scratching.
- Scratching often followed by burning.
- A smarting and biting sensation in genitals is also present.
- The genitals may also swollen.
- Pain, itching, and burning during urination in the genitals upon contact with urine is also present.
Hydrastis – For Yellow Vaginal Discharges in Vaginitis
- Homeopathic medicine Hydrastis prepare from the fresh root of a plant Hydrastis Canadensis.
- Use of Hydrastis consider in cases of vaginitis with a yellow discharge from the vagina.
- The discharges are profuse, thick, tenacious, and highly viscid.
- The discharges may stringy and ropy in some cases.
- Occasionally, they may offensive.
- Itching in the vagina appears from discharges.
Sepia – For Vaginitis with Painful Coition
- Sepia is a natural remedy for vaginitis with very painful coition.
- In cases where Sepia works effectively, the vaginal discharges are clear, watery or yellowish-greenish.
- They may also be blood-stained.
- They get worse after urinating.
- The discharges are excoriating with severe vaginal itching and burning pain.
- It may also have a fetid odor.
- Along with the above features, there is an increased frequency of urination.
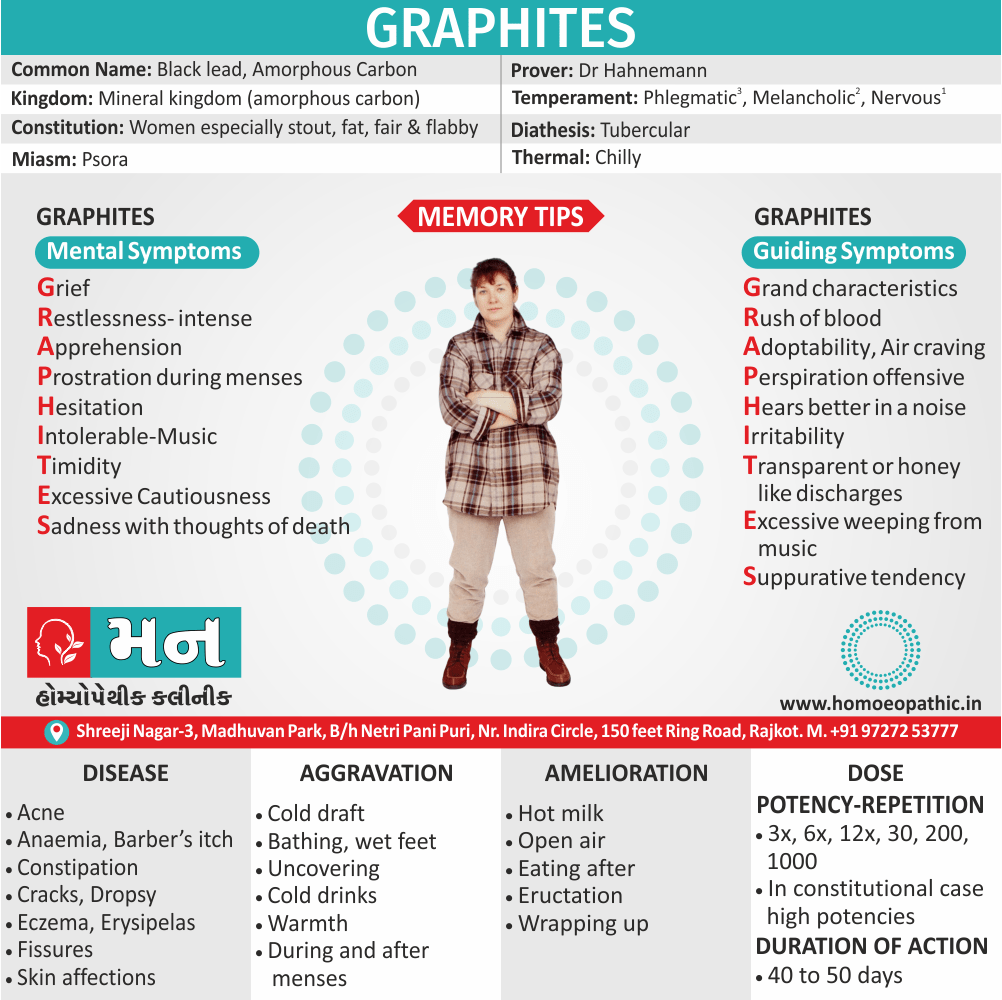
Graphites – To Manage Profuse, Gushing Vaginal Discharges in Vaginitis
- Homeopathic medicine Graphites is very beneficial for managing profuse, gushing vaginal discharges in vaginitis.
- The discharge is mainly white or yellowish-white.
- It flows through the day and night.
- The discharges are acrid and excoriate the skin.
- They also cause a biting pain in the vagina.
- The back feels weak due to these copious discharges.
Nitric Acid – For Vaginitis with Foul Vaginal Discharge
- Nitric Acid is a natural medicine for vaginitis with vaginal discharges that are offensive.
- In cases needing Nitric Acid, the color of vaginal discharge varies.
- It may be green, brown, flesh-colored or clear like water.
- The discharge is acrid and causes burning in the vulva and vagina.
- Stitching pain in the vagina may also be felt.
Natrum Phos – For Sour-Smelling Vaginal Discharges in Vaginitis
- Natrum Phos is an effective medicine for sour-smelling vaginal discharges in cases of vaginitis.
- The discharges from the vagina may be creamy or watery, and often honey-colored.
- They are often acidic.
Medorrhinum – For Vaginal Discharge with Fish-like Odours
- Medorrhinum is a natural remedy for vaginitis where the vaginal discharges have a peculiar fishy odor.
- The discharges are acrid, excoriating with excessive itching.
- Washing with lukewarm water relieves the itching.
- The discharges are also very thick.
- An attending gonorrhea infection may be present in cases needing Medorrhinum.
Diet & Regimen of Vaginitis
- Probiotic and Prebiotic compounds may also help stabilize vaginal pH by promoting the growth of healthy bacterial populations.
- Foods rich in Probiotics also Prebiotics include:
- Probiotics are: e.g. Soybeans, Bananas, Yogurt, Kimchi and sauerkraut.
- Prebiotics are: e.g. Onions, asparagus and Jerusalem artichoke, garlic, whole wheat products, oats.
- Benefits of natural remedies with antifungal, anti-inflammatory, or antioxidant properties for candida infection, including tea tree oil, coconut oil, and garlic.
- Reducing sweat around the vagina
- Exercising regularly
- Maintaining a healthy weight
- Staying hydrating
- Reducing stress
- Wearing loose-fitting cotton underwear
- Avoid either processed or heavily refined foods
- Avoid either foods or drinks with artificial hormones.[8]
References use for Article Vaginitis
1] DC Dutta’s Textbook of Gynecology: Including Contraception (6th edition)
2] https://www.mayoclinic.org › vaginitis
3] Clinical_Gynecology.pdf
4] https://my.clevelandclinic.org/health/diseases/9131-vaginitis
5] Gynacology VG Padubidri.pdf
6] https://www.plannedparenthood.org/learn/health-and-wellness/vaginitis
7] https://www.ncbi.nlm.nih.gov/books
8] https://www.medicalnewstoday.com/articles/327507#improving-vaginal-health
Frequently Asked Questions
What is Vaginitis?
Vaginitis is an inflammation of the vagina that can result in discharge, itching and pain.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Vaginitis?
- Pulsatilla
- Kreosote
- Alumina
- Natrum Mur
- Merc Sol
- Hydrastis
- Sepia
What causes Vaginitis?
- Chemicals
- Drugs
- Douches
- Pessaries
- Tampons
- Trauma
- Foreign bodies
- Alteration in the pH
What are the symptoms of Vaginitis?
- A red, swollen, tender vagina with irritation and burning.
- Dysuria with frequency of micturition
- Vagina and/or vulva is discolored, irritated, swollen, or uncomfortable.
- Pain or discomfort during sex.
Give the types of Vaginitis?
- Candida or “yeast” infections.
- Bacterial vaginosis.
- Trichomoniasis vaginitis.
- Chlamydia or Gonorrhoea.
- Viral vaginitis (herpes).
- Non-infectious vaginitis.
- Atrophic vaginitis.
Definition:
Vaginitis is an inflammation of the vagina that can result in discharge, itching and pain.[2]
Overview
Epidemiology
Causes
Risk Factors
Pathogenesis
Pathophysiology
Types
Clinical Features
Sign & Symptoms
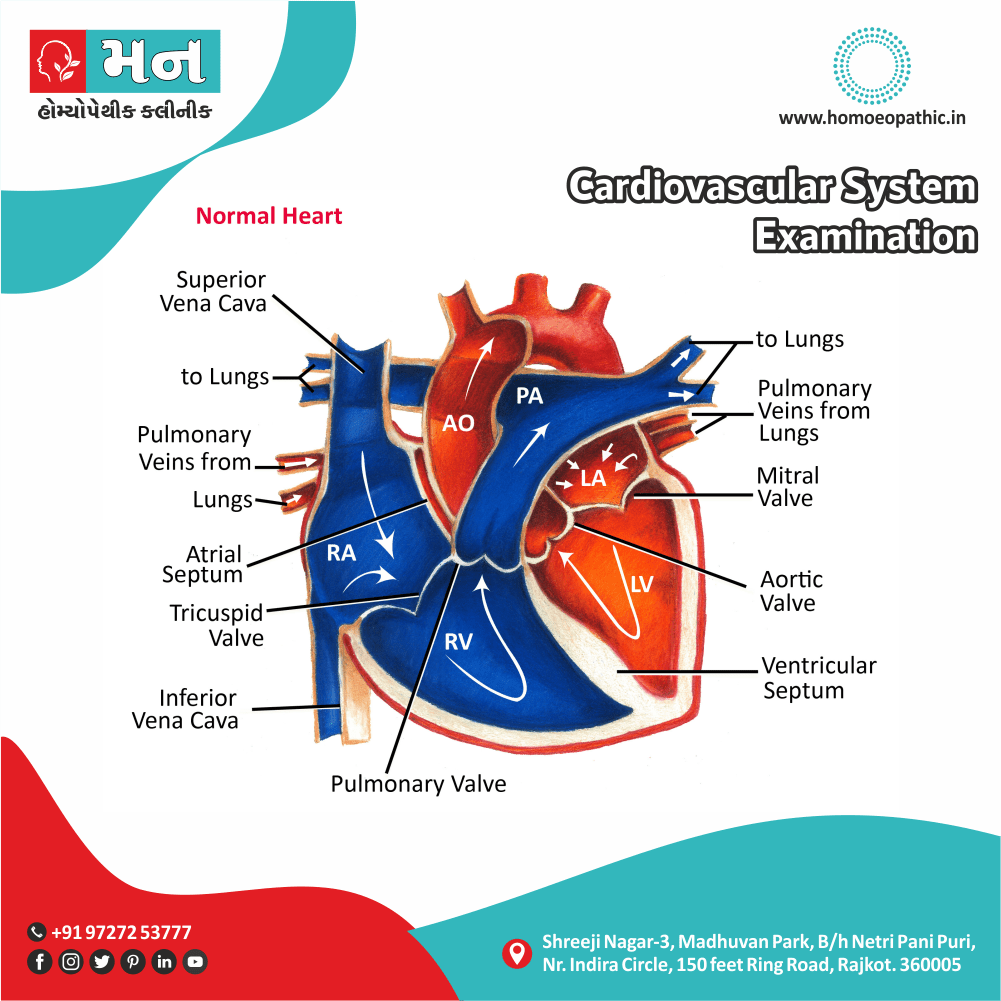
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Dont’s
Terminology
References
FAQ
Also Search As
Overview
Overview of Vaginitis
Inflammatory conditions of the vulva and vagina. The cause is usually a change in the balance of vaginal bacteria or an infection.
Due to lack of estrogen, the vaginal defense is lost and the infection occurs easily, once introduced inside the vagina.[1]
Reduced estrogen levels after menopause and some skin disorders also can cause vaginitis.
Epidemiology
Indian epidemiology then other
Causes
Causes of Vaginitis
- Chemicals, drugs, douches, pessaries, tampons, trauma, foreign bodies such as rubber ring pessaries, contraceptives and even vaginal and cervical operations are all causative.
- Alteration in the pH towards alkalinity always favors nonspecific infection; hence, its common incidence is in the puerperium.
- The association of coccal secondary infection with trichomoniasis is important, since the isolation of the secondary organism may mask the presence of the Trichomonas, which is really responsible for the discharge.[5]
Risk Factors
Risk factor of Vaginitis:
- Hormonal changes, such as those associated with pregnancy, birth control pills or menopause
- Sexual activity
- Having a sexually transmitted infection
- Medications, such as antibiotics and steroids
- Use of spermicides for birth control
- Uncontrolled diabetes
- Use of hygiene products such as bubble bath, vaginal spray or vaginal deodorant
- Douching
- Wearing damp or tight-fitting clothing
- Using an intrauterine device (IUD) for birth control. [2]
Pathogenesis
Pathogenesis refers to the development of a disease. It’s the story of how a disease gets started and progresses.
This is the entire journey of a disease, encompassing the cause but going beyond it.
Pathophysiology
Pathophysiology, on the other hand, focuses on the functional changes that occur in the body due to the disease. It explains how the disease disrupts normal physiological processes and how this disruption leads to the signs and symptoms we see.
Imagine a car accident. Pathogenesis would be like understanding how the accident happened – what caused it, the sequence of events (e.g., one car ran a red light, then hit another car). Pathophysiology would be like understanding the damage caused by the accident – the bent fenders, deployed airbags, and any injuries to the passengers.
In simpler terms, pathogenesis is about the "why" of a disease, while pathophysiology is about the "how" of the disease’s effects.
Types
Classification of Vaginitis
The most common types of vaginitis are i.e.:
- Candida or “yeast” infections.
- Bacterial vaginosis.
- Trichomoniasis vaginitis.
- Either Chlamydia or Gonorrhoea.
- Viral vaginitis (herpes).
- Non-infectious vaginitis.
- Atrophic vaginitis.
Candida or “yeast” infections i.e.:
- Causative Organism Moniliasis is caused by Candida albicans, a gram-positive yeast-like fungus.
- Candida normally lives in your vagina, as well as in the mouth and digestive tract of all people, regardless of gender. An infection occurs when the normally occurring candida increases and cause bothersome symptoms.
- Discharge of Candida infection is white cottage cheese–like discharge.
- Candida infections should alert the health care provider to the patient’s use of antibiotic or immunosuppressive agents, or the presence of diabetes or human immunodeficiency virus (HIV).[3]
Bacterial vaginosis i.e.:
- Bacterial vaginosis (in other words, BV) is actually the most common vaginal infection in women of reproductive age.
- Bacterial vaginosis is caused by a combination of several bacteria that typically live in your vagina. These bacteria seem to overgrow in much the same way candida does when the vaginal pH balance is upset.
- Bacterial vaginosis is not asexually transmitted infection (STI), but it’s seen more often in sexually active people.
- Risk factors for bacterial vaginosis include: – New or multiple sexual partners, Douching, Cigarette smoking.
Trichomoniasis vaginitis i.e.:
- Vaginal trichomoniasis is the most common and important cause of vaginitis in the childbearing period.
- It is caused by Trichomonas vaginalis, a pear-shaped unicellular flagellate protozoon.
- The organism is predominantly transmitted by sexual contact, the male harbors the infection in the urethra and prostate.
- The transmission may also be possible by the toilet articles from one woman to the other or through examining gloves.
- The incubation period is 3–28 days.[1]
Chlamydia or Gonorrhoea i.e.:
- Chlamydia is the most common sexually transmitted infection (in other words, STI).
- Chlamydial vaginitis is most common in young adults aged 15 to 24 who have multiple sexual partners.
- Routine chlamydia screening is recommended by the Centers for Disease Control and Prevention (CDC) annually for sexually active women aged 24 and younger, and also at any age if you have multiple sexual partners, or are at risk.
- Gonorrhea, another bacterial STI, can also cause vaginitis symptoms. It often occurs with chlamydia.
- Sex partners should be tracked and treated appropriately to avoid re-infection.[4]
Viral vaginitis (herpes) i.e.:
Sexually transmitted viruses are a common cause of vaginitis that lead to inflammation of your genitals. The most common type of viral vaginitis is herpes simplex virus (HSV).
- Herpes simplex virus (HSV)- Herpes simplex virus is often just called a herpes infection. These infections are spread by sexual contact and often lead to painful sores. Herpes outbreaks are often associated with stress or emotional distress. You can also get herpes that affects your mouth-pharynx through oral sex.
- Low risk human papillomavirus (HPV) can lead to the development of condyloma, referred to as genital warts, and can be transmitted through vaginal, anal or oral sex.
Non-infectious vaginitis i.e.:
- Allergic reaction that causes vaginal irritation without having an infection.
- The most common cause is an allergic reaction or irritation from vaginal sprays, douches or spermicidal products.
- However, the skin around your vagina can also be sensitive to perfumed soaps, feminine products and wipes, lotions, sexual lubricants, detergents and fabric softeners.
Atrophic vaginitis i.e.:
- Vaginitis in postmenopausal women is called atrophic vaginitis. Additionally, The term is preferable to old age vaginitis.
- There is atrophy of the vulvovaginal structures due to estrogen deficiency. The vaginal defense is lost. Vaginal mucosa is thin and is more susceptible to infection and trauma. There may be desquamation of the vaginal epithelium which may lead to formation of adhesions also bands between the walls.
- Either Yellowish or blood-stained vaginal discharge.[1]
Clinical Features
Tab Content
Sign & Symptoms
Sign & Symptoms of Vaginitis
- A red, swollen, tender vagina with irritation and burning.
- Dysuria with frequency of micturition [5]
- Our vagina and/or vulva is discolored, irritated, swollen, or uncomfortable.
- Pain or discomfort during sex.
- Vaginal discharge that isn’t normal for you:
- With yeast infections, discharge is usually thick, white, and odorless. You may also have a white coating in and around your vagina.
- With bacterial vaginosis, you may have vaginal discharge that’s grayish, foamy, and smells fishy.
- With trich, discharge is often frothy, yellow-green, smells bad, and may have spots of blood in it. [6]
Clinical Examination
Tab Content
Diagnosis
Diagnosis of Vaginitis
- Review your medical history- This includes your history of vaginal or sexually transmitted infections.
- Perform a pelvic exam- During the pelvic exam, your health care provider might use an instrument (speculum) to look inside your vagina for inflammation and discharge.
- Collect a sample for lab testing- Your health care provider might collect a sample of cervical or vaginal discharge for lab testing to confirm what kind of vaginitis you have.
- Perform pH testing- Your health care provider might test your vaginal pH by applying a pH test stick or pH paper to the wall of your vagina. An elevated pH can indicate either bacterial vaginosis or trichomoniasis. However, pH testing alone is not a reliable diagnostic test.[2]
Differential Diagnosis
Differential Diagnosis of Vaginitis
- Bacterial vaginosis
- Vulvovaginal candidiasis
- Trichomoniasis
- Desquamative inflammatory vaginitis
- Atrophic vaginitis
- Allergies
- Chemical irritation
- Cervicitis
- Foreign bodies. [7]
Complications
Complications are what happen after you have a disease. They are the negative consequences of the disease process.
Investigations
Tab Content
Treatment
Treatment of Vaginitis
- The cause of the infection determines the appropriate treatment. It may include oral or topical antibiotics and/or antifungal creams, antibacterial creams, or similar medications.
- A cream containing cortisone may also use to relieve some of the irritation. If an allergic reaction involve, an antihistamine may also prescribe. For women who have irritation and inflammation caused by low levels of estrogen (postmenopausal), a topical estrogen cream might prescribe.
The following are typical treatments for trichomoniasis, bacterial vaginosis, and yeast infections i.e.:
- Trichomoniasis: Oral treatment with either metronidazole or tinidazole.
- "Sexual partner(s) should be treated simultaneously.
- Patients should advise to avoid sexual intercourse for at least 1 week and until they and their partner(s) have completed treatment and follow-up."
- Bacterial vaginosis: The most commonly used antibiotics are metronidazole, available in both pill and gel form, and clindamycin available in both pill and cream form.
- Yeast infections: Local azole, in the form of ovula and cream. All agents appear to be equally effective.
- These anti-fungal medications, which are available in over-the-counter form, are generally used to treat yeast infections.
- Treatment may last anywhere between one, three, or seven days.
- Trichomoniasis- Your health care provider may prescribe metronidazole (Flagyl) or tinidazole (Tindamax) tablets.
- Genitourinary syndrome of menopause (vaginal atrophy)- Estrogen — in the form of vaginal creams, tablets or rings — can treat this condition. This treatment is available by prescription from your health care provider, after other risk factors and possible complications reviewed.
- Noninfectious vaginitis- To treat this type of vaginitis, you need to pinpoint the source of the irritation and avoid it. Possible sources include new soap, laundry detergent, sanitary napkins or tampons.[2]
Prevention
Prevention of Vaginitis
- Good hygiene might prevent some types of vaginitis from recurring and relieve some symptoms:
- Avoid baths, hot tubs and whirlpool spas.
- Avoid irritants – These include scented tampons, pads, douches and scented soaps. Rinse soap from your outer genital area after a shower and dry the area well to prevent irritation. Don’t use harsh soaps, such as those with deodorant or antibacterial action, or bubble bath.
- Wipe from front to back after using the toilet. Doing so avoids spreading fecal bacteria to your vagina.
- Avoid douching – Your vagina doesn’t require cleansing other than regular showering. Repetitive douching disrupts the good organisms that live in the vagina and can increase your risk of vaginal infection. Douching won’t clear up a vaginal infection.
- Practice safer sex – Using a condom and limiting the number of sex partners can help.
- Wear cotton underwear – Also wear pantyhose with a cotton crotch. Consider not wearing underwear to bed. Yeast thrives in moist environments.[2]
Homeopathic Treatment
Homeopathic Treatment of Vaginitis
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Vaginitis:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
Pulsatilla – For vaginitis with Thick Vaginal Discharge
- Pulsatilla is a natural homeopathic medicine derived from a plant named Pulsatilla Nigricans or Wind-flower of the natural order Ranunculaceae.
- Pulsatilla is helpful for vaginitis when vaginal discharges are thick like cream.
- They are white (like milk) and get worse on lying down.
- There may be a burning felt in the vagina along with a backache.
Kreosote – For Itching in Vagina
- Kreosote is a natural medicine especially for itching in the vagina in cases of vaginitis.
- The itching is quite intense also violent.
- There may be soreness also burning in the vagina after scratching.
- Furthermore, The genitals are swollen too.
- The vaginal discharge may be either white or yellow and smells putrid.[4]
- Besides this, Standing and walking worsens the discharge.
- Weakness may appear with the discharges.
- Lastly, There is a frequent urge to urinate.
Alumina – For Vaginitis Vaginal Discharges Causing Burning in Vagina
- Alumina offers a natural cure for burning in the vagina due to vaginitis.
- The discharges are worse during the daytime and may be transparent or light yellow.
- They are also highly acrid, corrosive, excoriating.
- Cold washing tends to relieve the symptoms.
- In some cases, stitching and throbbing pain in the vagina is also felt.
Natrum Mur – For Vaginitis with White Vaginal Discharge
- Natrum Mur is an effective natural medicine for vaginitis cases with white vaginal discharges.
- The discharges are thick and profuse and tend to get worse at night.
- They also tend to acrid and are attended with itching and a smarting pain in genitals.
- General weakness may also be present.
Merc Sol – For Greenish Vaginal Discharge in Vaginitis
- Merc Sol a homeopathic medicine used to treat vaginitis with greenish vaginal discharges.
- A night aggravation of the discharges may present.
- The discharges may blood-stained, corrosive and itchy, leading to scratching.
- Scratching often followed by burning.
- A smarting and biting sensation in genitals is also present.
- The genitals may also swollen.
- Pain, itching, and burning during urination in the genitals upon contact with urine is also present.
Hydrastis – For Yellow Vaginal Discharges in Vaginitis
- Homeopathic medicine Hydrastis prepare from the fresh root of a plant Hydrastis Canadensis.
- Use of Hydrastis consider in cases of vaginitis with a yellow discharge from the vagina.
- The discharges are profuse, thick, tenacious, and highly viscid.
- The discharges may stringy and ropy in some cases.
- Occasionally, they may offensive.
- Itching in the vagina appears from discharges.
Sepia – For Vaginitis with Painful Coition
- Sepia is a natural remedy for vaginitis with very painful coition.
- In cases where Sepia works effectively, the vaginal discharges are clear, watery or yellowish-greenish.
- They may also be blood-stained.
- They get worse after urinating.
- The discharges are excoriating with severe vaginal itching and burning pain.
- It may also have a fetid odor.
- Along with the above features, there is an increased frequency of urination.
Graphites – To Manage Profuse, Gushing Vaginal Discharges in Vaginitis
- Homeopathic medicine Graphites is very beneficial for managing profuse, gushing vaginal discharges in vaginitis.
- The discharge is mainly white or yellowish-white.
- It flows through the day and night.
- The discharges are acrid and excoriate the skin.
- They also cause a biting pain in the vagina.
- The back feels weak due to these copious discharges.
Nitric Acid – For Vaginitis with Foul Vaginal Discharge
- Nitric Acid is a natural medicine for vaginitis with vaginal discharges that are offensive.
- In cases needing Nitric Acid, the color of vaginal discharge varies.
- It may be green, brown, flesh-colored or clear like water.
- The discharge is acrid and causes burning in the vulva and vagina.
- Stitching pain in the vagina may also be felt.
Natrum Phos – For Sour-Smelling Vaginal Discharges in Vaginitis
- Natrum Phos is an effective medicine for sour-smelling vaginal discharges in cases of vaginitis.
- The discharges from the vagina may be creamy or watery, and often honey-colored.
- They are often acidic.
Medorrhinum – For Vaginal Discharge with Fish-like Odours
- Medorrhinum is a natural remedy for vaginitis where the vaginal discharges have a peculiar fishy odor.
- The discharges are acrid, excoriating with excessive itching.
- Washing with lukewarm water relieves the itching.
- The discharges are also very thick.
- An attending gonorrhea infection may be present in cases needing Medorrhinum.
Diet & Regimen
Diet & Regimen of Vaginitis
- Probiotic and Prebiotic compounds may also help stabilize vaginal pH by promoting the growth of healthy bacterial populations.
- Foods rich in Probiotics also Prebiotics include:
- Probiotics are: e.g. Soybeans, Bananas, Yogurt, Kimchi and sauerkraut.
- Prebiotics are: e.g. Onions, asparagus and Jerusalem artichoke, garlic, whole wheat products, oats.
- Benefits of natural remedies with antifungal, anti-inflammatory, or antioxidant properties for candida infection, including tea tree oil, coconut oil, and garlic.
- Reducing sweat around the vagina
- Exercising regularly
- Maintaining a healthy weight
- Staying hydrating
- Reducing stress
- Wearing loose-fitting cotton underwear
- Avoid either processed or heavily refined foods
- Avoid either foods or drinks with artificial hormones.[8]
Do’s and Dont’s
Tab Content
Terminology
Tab Content
References
References use for Article Vaginitis
1] DC Dutta’s Textbook of Gynecology: Including Contraception (6th edition)
2] https://www.mayoclinic.org › vaginitis
3] Clinical_Gynecology.pdf
4] https://my.clevelandclinic.org/health/diseases/9131-vaginitis
5] Gynacology VG Padubidri.pdf
6] https://www.plannedparenthood.org/learn/health-and-wellness/vaginitis
7] https://www.ncbi.nlm.nih.gov/books
8] https://www.medicalnewstoday.com/articles/327507#improving-vaginal-health
FAQ
Frequently Asked Questions
What is Vaginitis?
Vaginitis is an inflammation of the vagina that can result in discharge, itching and pain.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Vaginitis?
- Pulsatilla
- Kreosote
- Alumina
- Natrum Mur
- Merc Sol
- Hydrastis
- Sepia
What causes Vaginitis?
- Chemicals
- Drugs
- Douches
- Pessaries
- Tampons
- Trauma
- Foreign bodies
- Alteration in the pH
What are the symptoms of Vaginitis?
- A red, swollen, tender vagina with irritation and burning.
- Dysuria with frequency of micturition
- Vagina and/or vulva is discolored, irritated, swollen, or uncomfortable.
- Pain or discomfort during sex.
Give the types of Vaginitis?
- Candida or “yeast” infections.
- Bacterial vaginosis.
- Trichomoniasis vaginitis.
- Chlamydia or Gonorrhoea.
- Viral vaginitis (herpes).
- Non-infectious vaginitis.
- Atrophic vaginitis.
Also Search As
Frequently Asked Questions (FAQ)
XYZ
XXX
XYZ
XXX
XYZ
XXX
How can I find reputable homeopathy clinics or homeopathic doctors in my area?
You can found Homeopathic Clinic For XXXX by searching for
Specific city Examples are
You can also search for near you Examples are