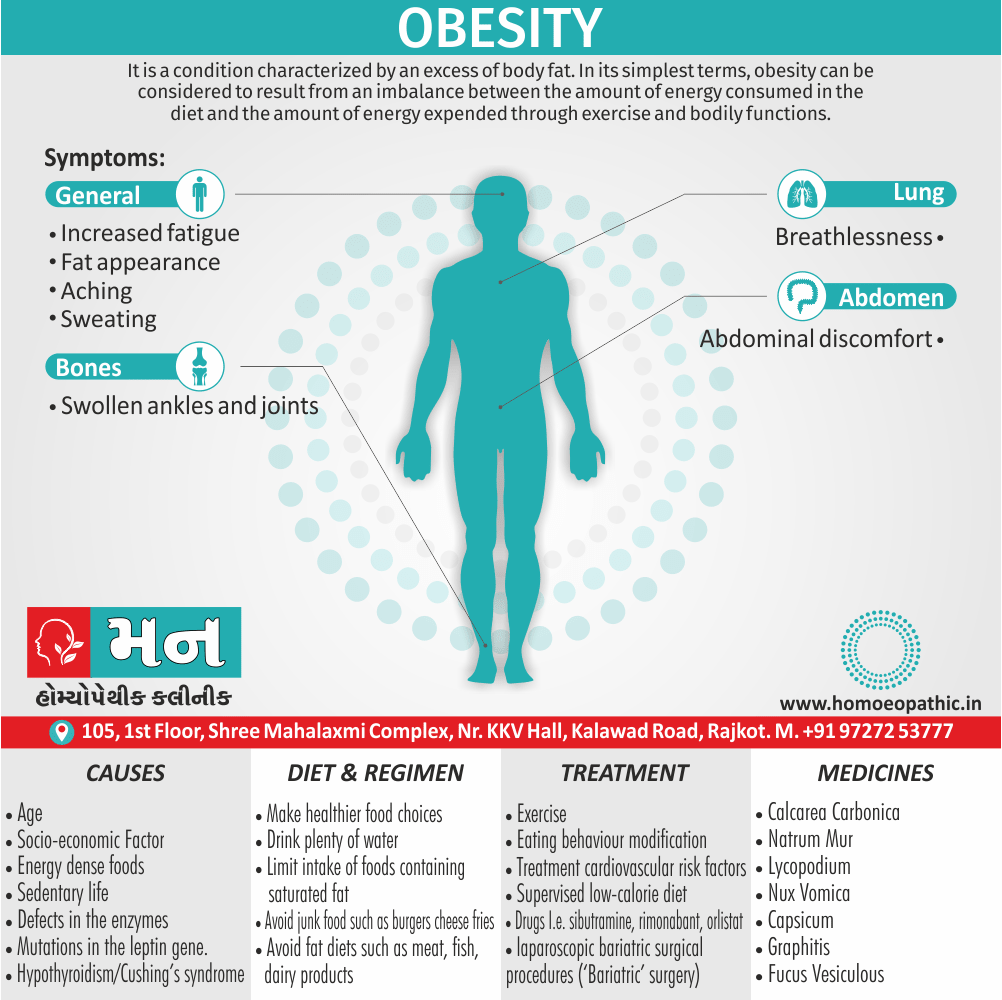
Obesity
Definition
It is a condition characterised by an excess of body fat. Additionally, In its simplest terms, obesity can be considered to result from an imbalance between the amount of energy consumed in the diet and the amount of energy expended through exercise also bodily functions.
In brief, Obesity is widely regarded as a pandemic, with potentially disastrous consequences for human health.
Demography
In developing countries, average national rates of heavier person are low, but these figures may disguise high rates of heavier person in urban communities; for example, nearly one quarter of women in urban India are higher weight body. In detail, There is increasing public awareness of the health implications of obesity. Many patients will seek medical help for their obesity, on other hand others will present with one of the complications of obesity.
In countries like the USA also the UK, fat deposition is affecting almost the entire population. Additionally, The weight distribution of almost the whole population is shifting upwards – the slim are becoming less slim while the fat is getting fatter. Specifically, In the UK, this translates into a 1-kilogram increase in weight per adult per year (on average over the adult population).
- Availability of cheap also heavily marketed energy rich foods
- Increase in labour saving devices (e.g. lifts and remote controls)
- Increase in passive transport (for example, cars as opposed to walking, cycling, or walking to public transport hubs).
Body Fat Distribution
Increased intra abdominal fat causes ‘central’ (for example; ‘abdominal’, ‘visceral’, ‘android’ or ‘apple shaped’) obesity, which contrasts with subcutaneous fat accumulation causing ‘generalised’ (either ‘gynoid’ or ‘pear-shaped’) obesity; the former is more common in men and is more closely associated with type 2 diabetes, the metabolic syndrome also cardiovascular disease .
Besides this; The key difference between these depots of fat may lie in their vascular anatomy, with intra abdominal fat draining into the portal vein and thence directly to the liver.
Causes
A continuous small daily positive energy balance of only 0.2–0.8 MJ (50–200 kcal; < 10% of intake) would lead to weight gain of 2–20 kg over a period of 4–10 years.
Age i.e.:
Basically; heavier person usually become higher weight body adults. In detail, Weight tends to increase throughout adult life, as BMR and physical activity decrease.
Socio-economic Factor i.e.:
Generally, India it is estimated that 5% of the population receives 40% of the available food energy, leading to obesity in the urban population in parallel with persisting undernutrition in some rural communities
Energy dense foods i.e.:
For example; drinks with highly refined sugar content and salty snacks.
Sedentary life i.e.:
In brief, Decrease in physical activity levels in recent years correlated positively with the number of hours spent watching television. inversely with levels of physical activity (e.g. stair climbing).
Genetic role i.e.:
Twin also adoption studies confirm a genetic influence on obesity.
A few rare single gene disorders i.e.:
This disorders have been identified that lead to severe childhood obesity i.e. melanocortin4 receptor (in other words; MC4R)
Defects in the enzymes processing proopiomelanocortin (POMC, the precursor for adrenocorticotrophic hormone (in other words; ACTH)) in the hypothalamus.
mutations in the leptin gene.
Additional genetic conditions i.e.:
like Prader– Willi also Lawrence–Moon–Biedl syndromes.
underlying disorder i.e.:
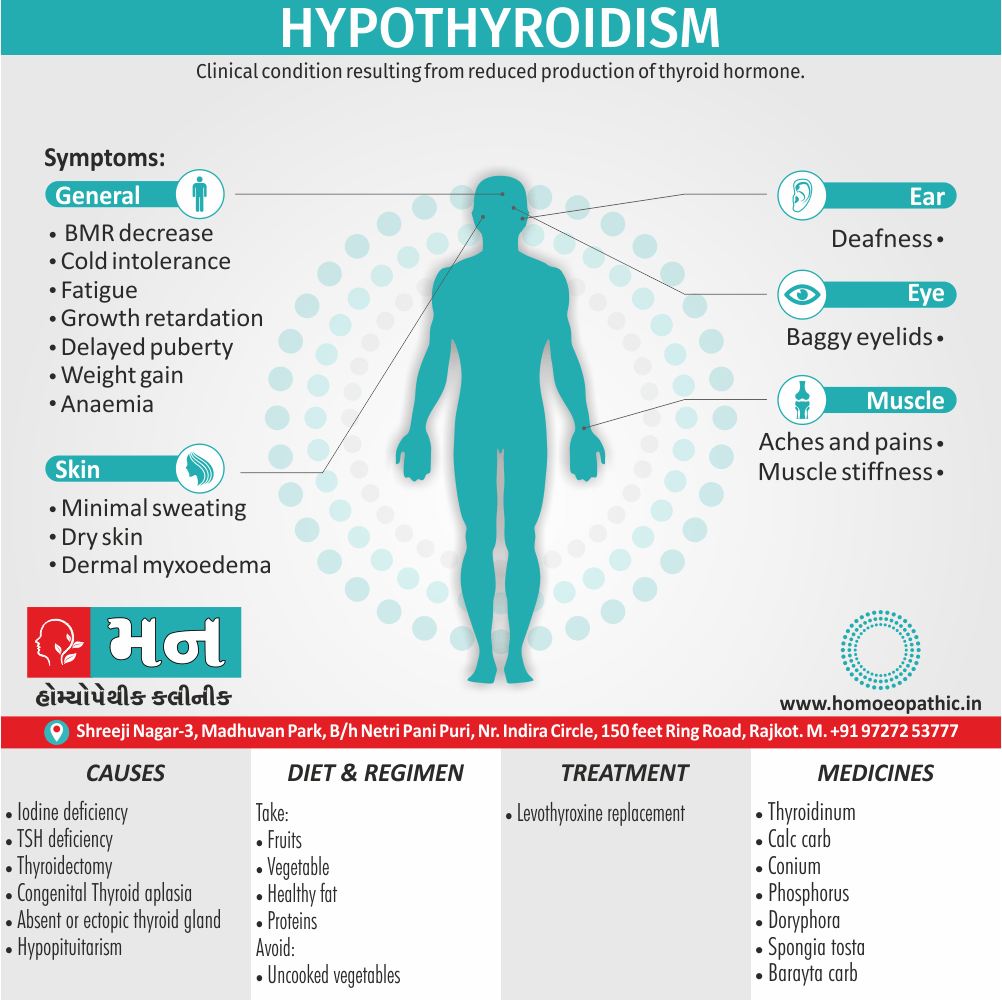
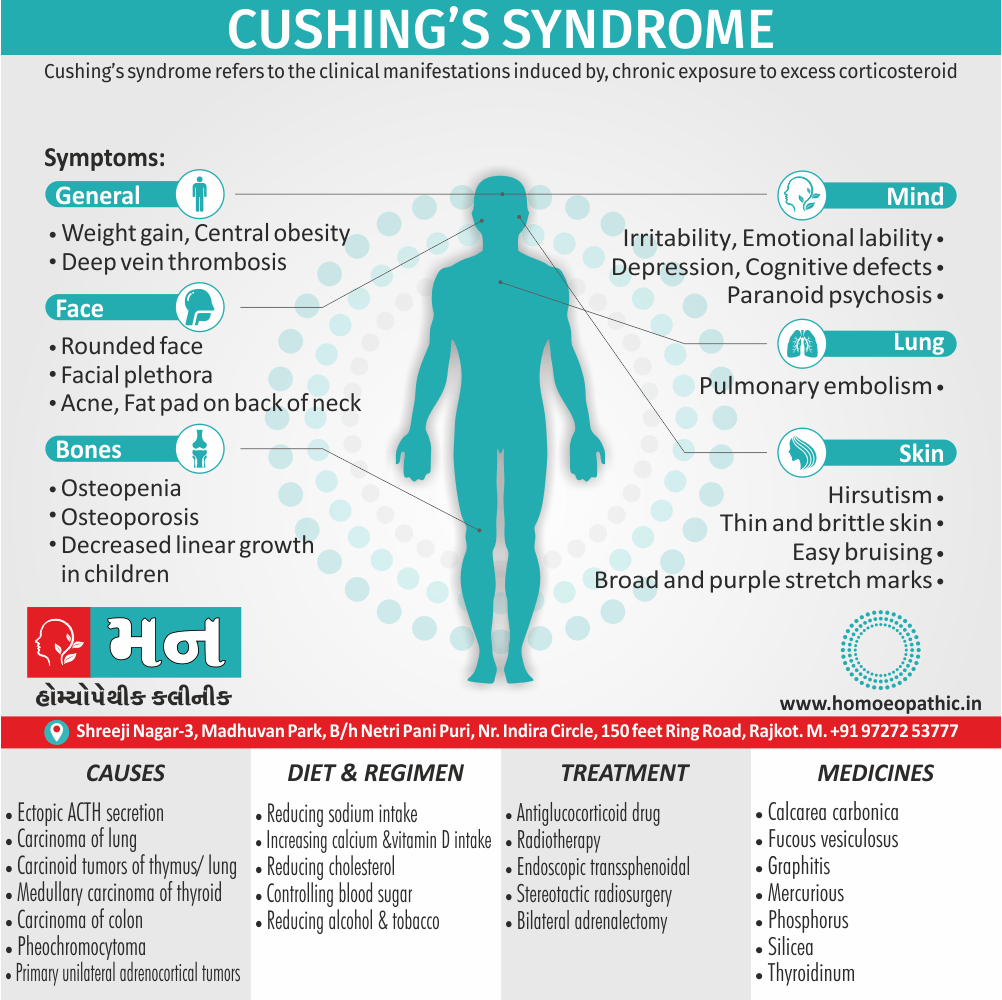
such as hypothyroidism or Cushing’s syndrome
Fat appearance.
Weight of 20% or more than ideal for height and body frame. In detail; Some heavier person have no physical symptoms but may have associated emotional problems and poor exercise tolerance.
Others may possibly experience:
Abdominal discomfort
Aching
Swollen ankles and joints
Breathlessness
Sweating
Increased fatigue
Clinical assessment
- quantify the problem
- exclude an underlying cause
- identify complications
- reach a management plan
Severity of obesity can be quantified using the BMI.
How to measure BMI i.e.:
- Body Mass Index is a simple calculation using a person’s height and weight. The formula is BMI = kg/m2 where kg is a person’s weight in kilograms and m2 is their height in metres squared.A BMI of 25.0 or more is overweight, while the healthy range is 18.5 to 24.9. BMI applies to most adults 18-65 years.
- making healthier food choices
- drink plenty of water
- limit intake of foods containing saturated fat, added salt, added sugars and alcohol
- Avoid junk food such as burgers cheese fries
- Avoid fad diets such as meat, fish, wheat or dairy products
|
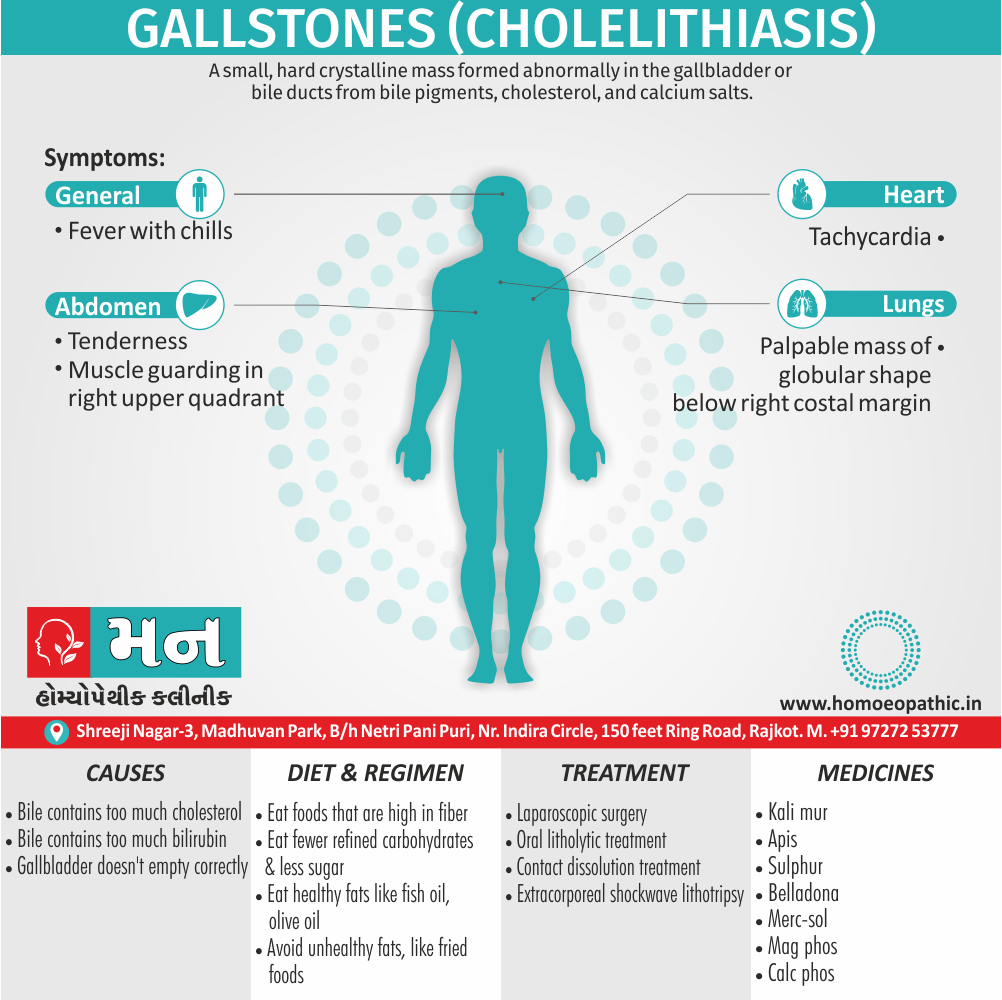
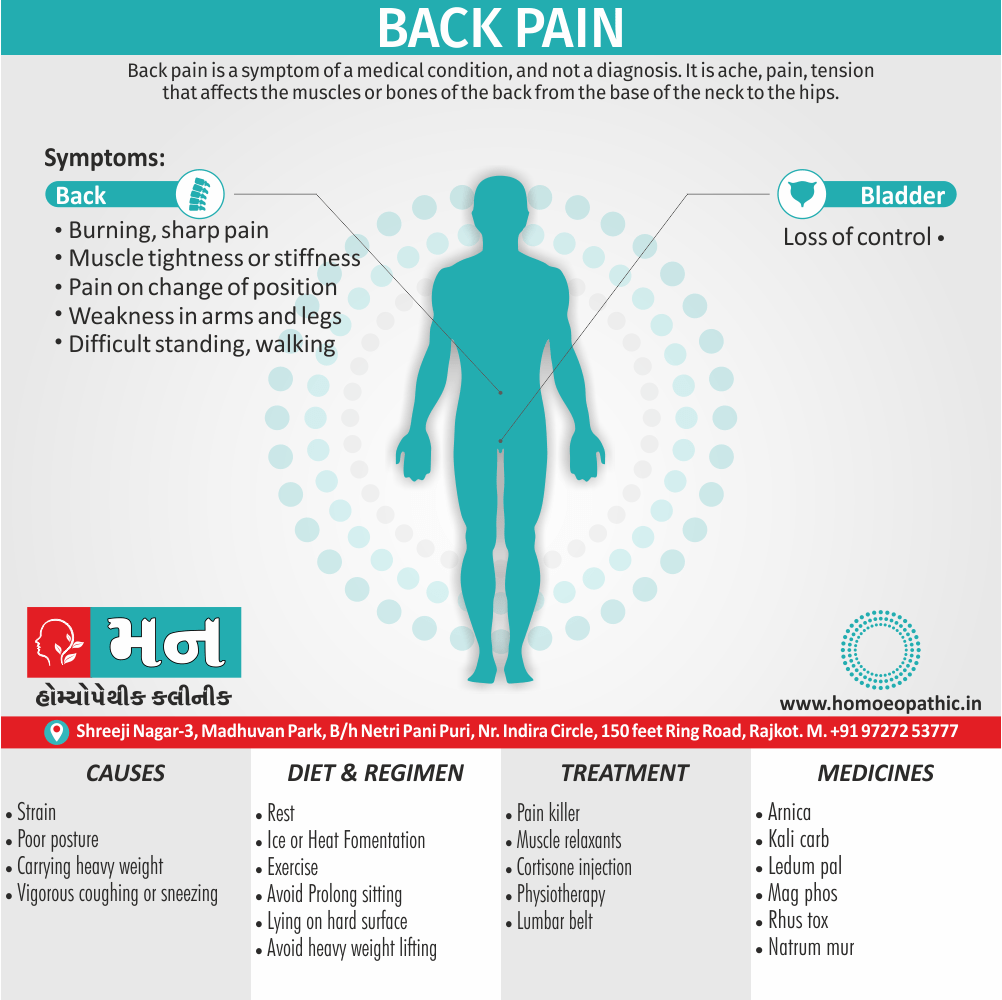
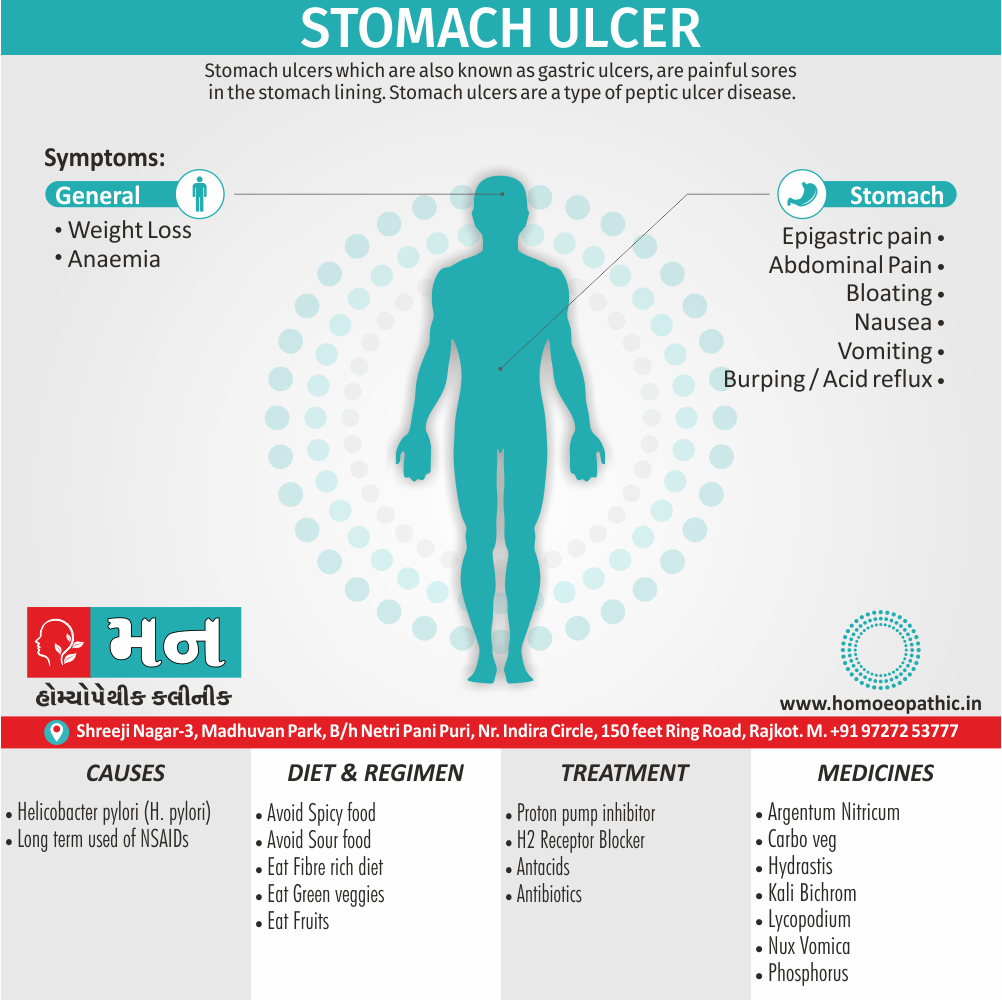
Risk factors
|
Outcome |
| ‘Metabolic syndrome’
Type 2 diabetes Hypertension Hyperlipidaemia Liver fat accumulation |
Coronary heart Disease Stroke Diabetic Complications Non-alcoholic steatohepatitis Cirrhosis |
| Restricted ventilation | Exertional dyspnoea
Obstructive sleep apnoea Obesity hypoventilation syndrome (in other words; Pickwickian syndrome) |
| Mechanical effects of weight
|
Urinary incontinence
Osteoarthritis |
| Increased peripheral steroid interconversion in adipose tissue
|
Hormone-dependent cancers
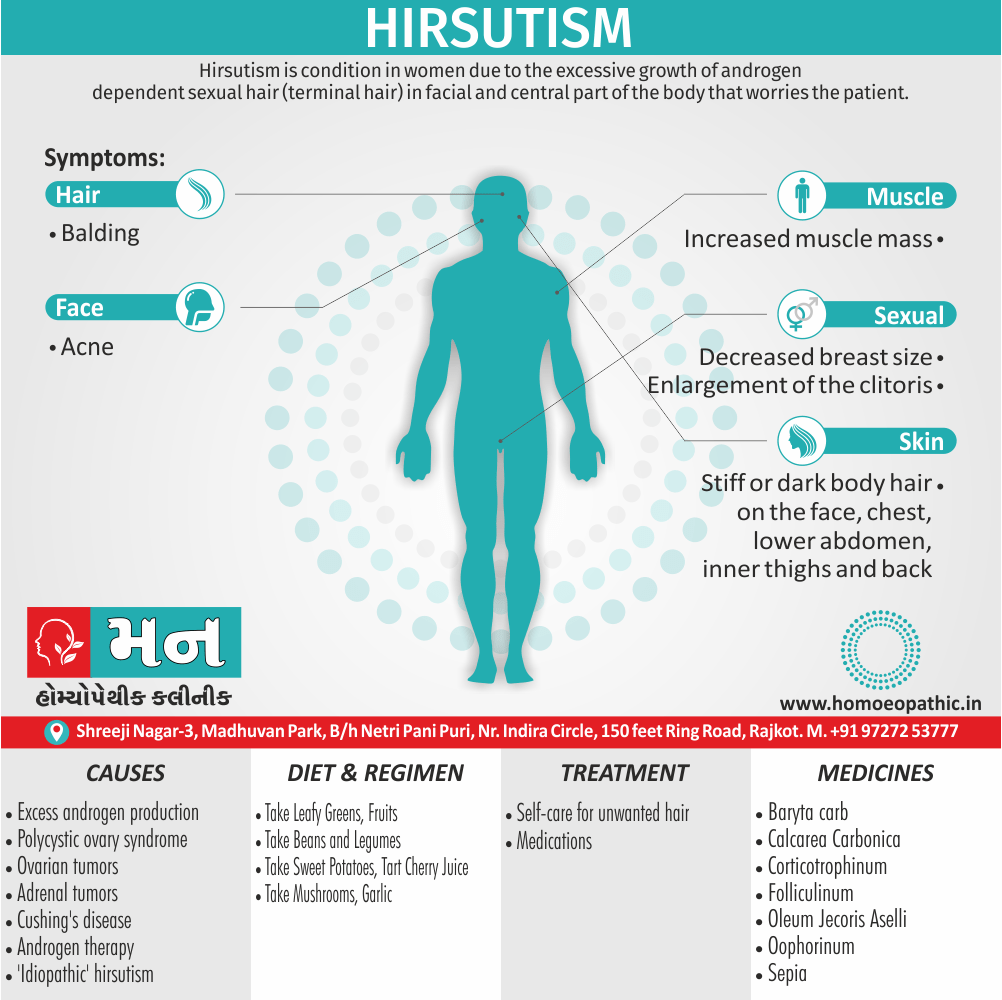
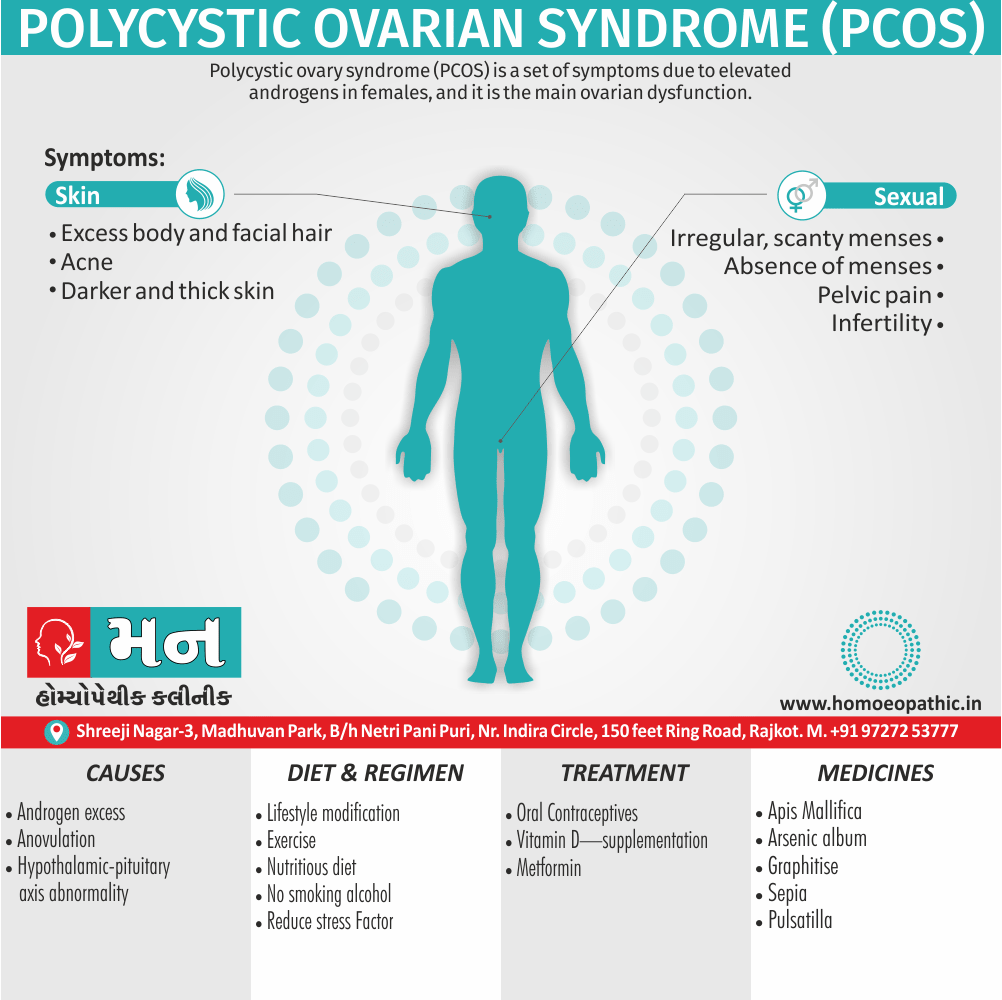
(breast, uterus) Polycystic ovarian syndrome (for example; infertility, hirsutism) |
| Others | Psychological morbidity
(for example; low self-esteem, depression) Socioeconomic disadvantage (lower income, less likely to be promoted) Gallstones Colorectal cancer Skin infections (groin and sub mammary candidiasis; hidradenitis) |
Therapeutic option for obesity
1st level management i.e.:
↑Exercise
Eating behaviour modification
including food selection, portion size control, avoidance of snacking, regular meals to encourage satiety, also substitution of sugar with artificial sweeteners. Regular support from a dietitian or attendance at a weight loss group may be helpful.
Treat cardiovascular risk factors
2nd level management i.e.:
Supervised low-calorie diet
The composition of the diet should ensure a minimum of 50 g of protein each day for men and 40 g for women to minimise muscle degradation. Energy content should be a minimum of 1.65 MJ (in other words; 400 kcal) for women of height < 1.73 m, and 2.1 MJ (in other words; 500 kcal) for all men and for women taller than 1.73 m.
3rd level management i.e.:
Drugs for example; sibutramine, rimonabant, orlistat
Drug therapy is usually reserved for patients with high risk of complications from obesity
4th level management i.e.:
surgery i.e. laparoscopic bariatric surgical procedures (i.e. ‘Bariatric’ surgery)
Generally, Cosmetic surgical procedures may be considered in heavier person after successful weight loss. Besides this; This operation is of no value for long-term weight reduction if food intake remains unrestricted.
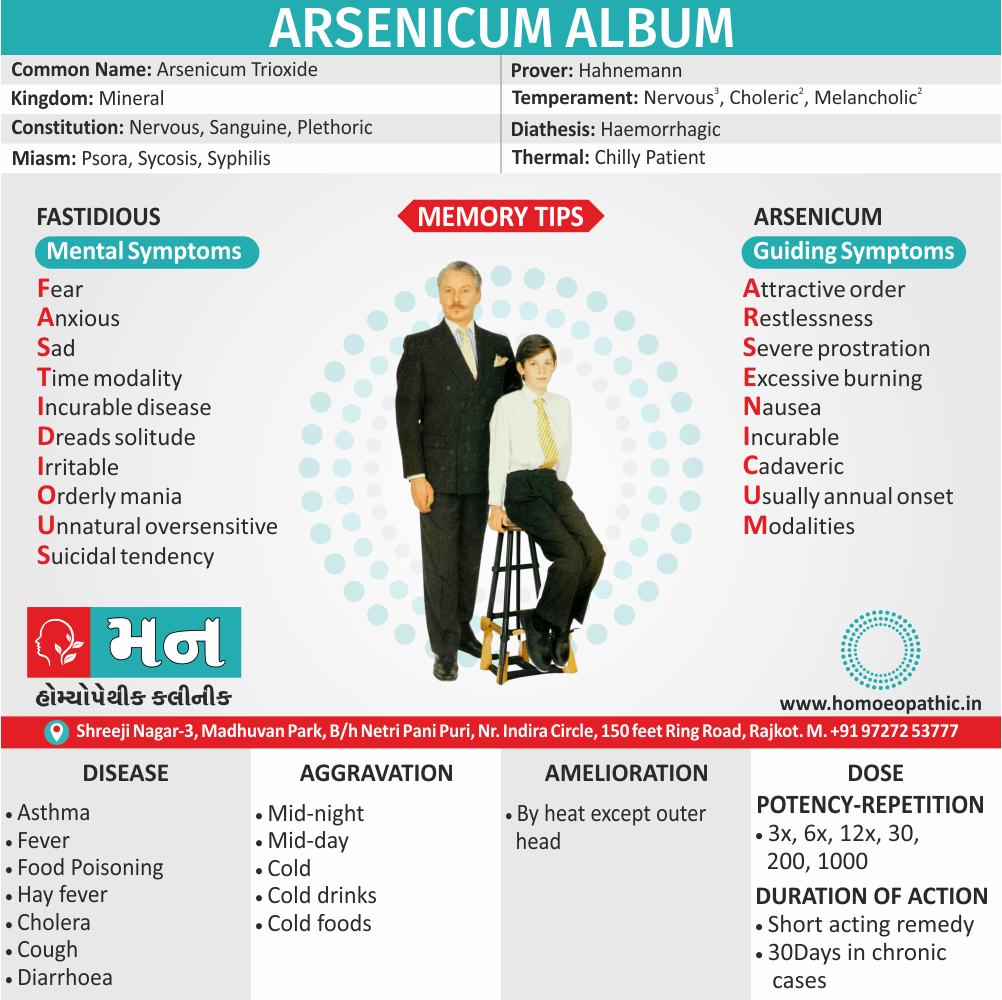
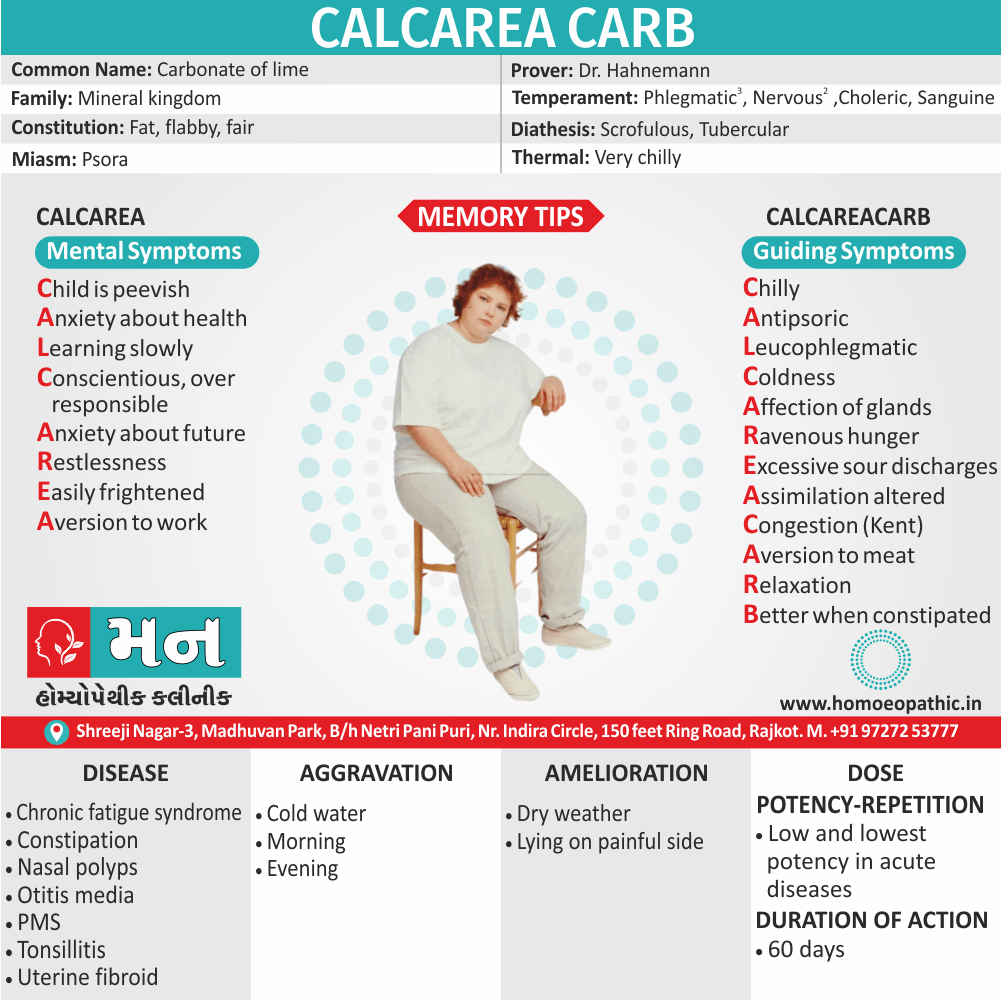
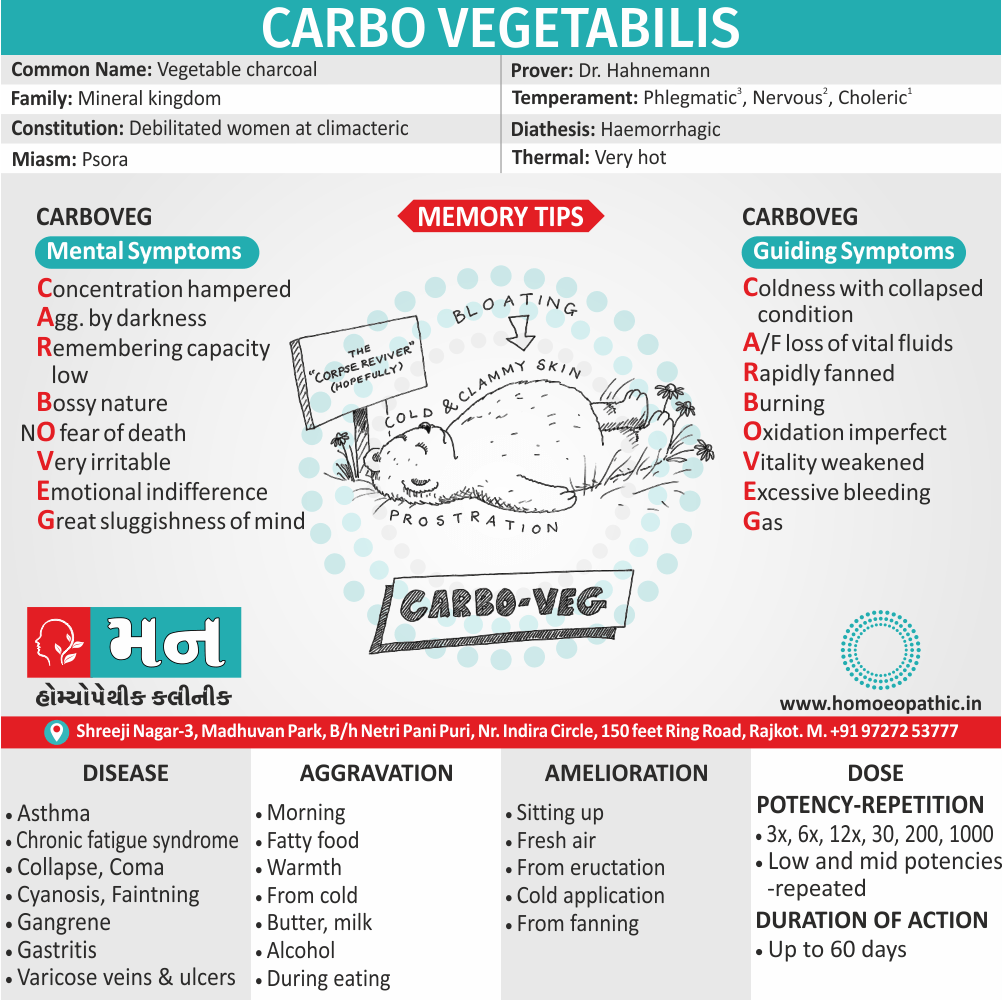
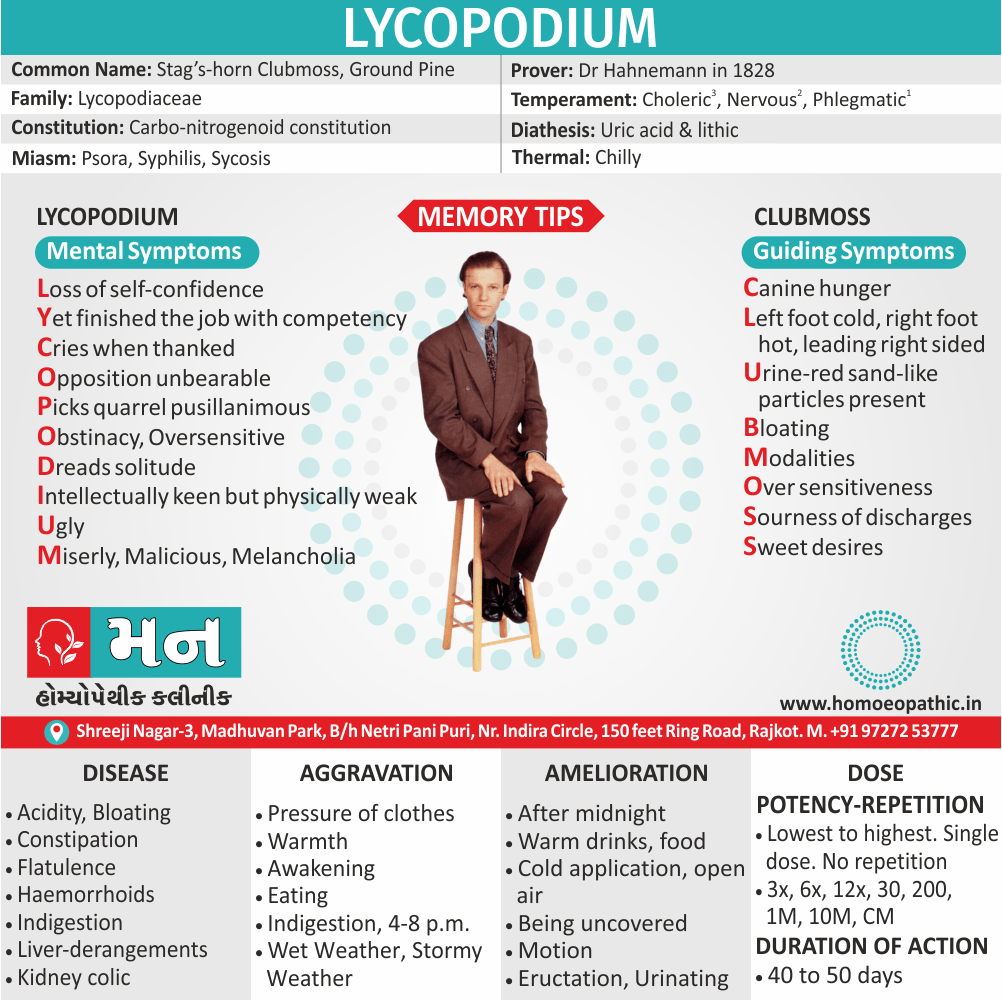
Calcarea Carbonica:
This medicine is mainly given when there is excess fat in the abdomen and the metabolism is working at a very low pace, resulting in obesity and weight gain. A patient requiring this medicine is fatty and flabby. In order to be eligible to use this medicine to lose weight, the constitutional symptoms shown by the patient are given utmost importance. The eating habits include craving for boiled eggs, and strange things like chalk, clay, pencils, lime etc. Due to a sluggish metabolic activity, the patients are almost always constipated. This medicine can also be considered if the excess weight gain is due to thyroid problems.
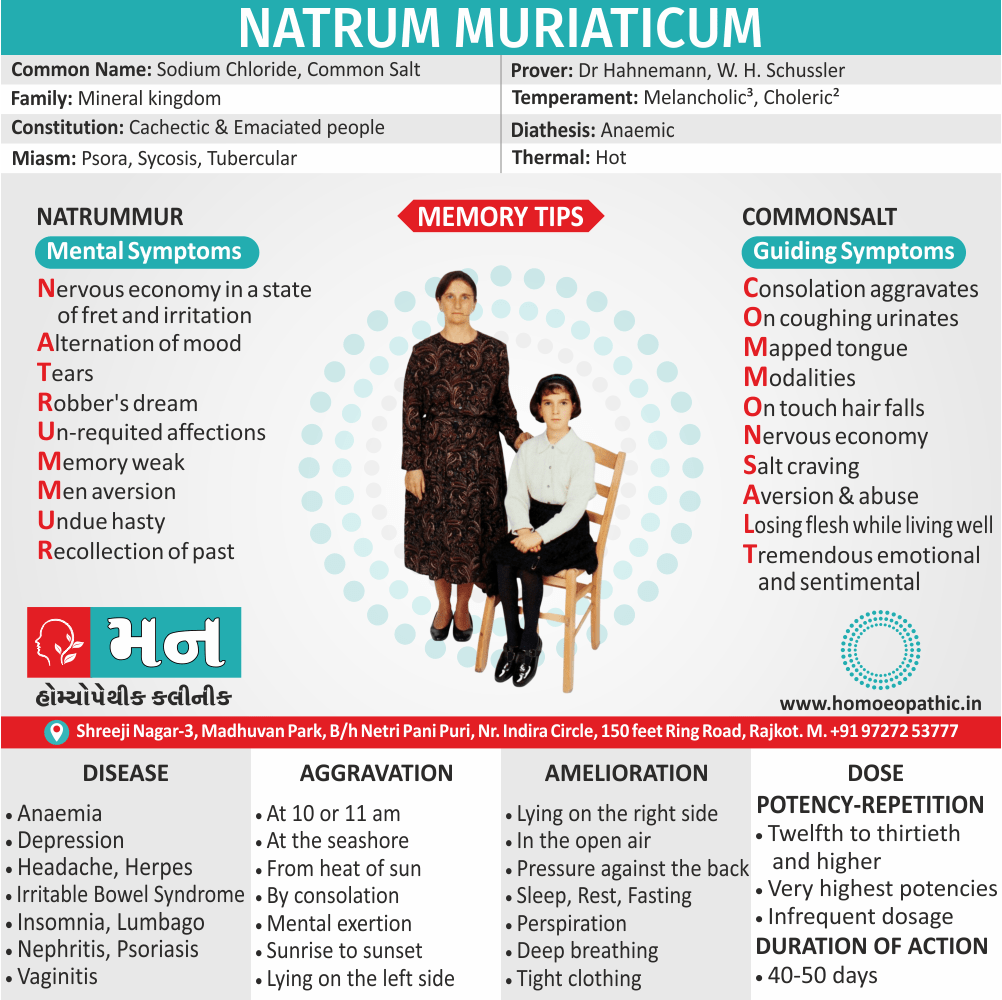
Natrum Mur:
This medicine is recommended when there is an excess of fat mainly in the thighs and buttocks as compared to other parts of the body. This medicine gives wonderful results if the person has gained excess weight due to long continued stress or depression. The patients who require this medicine usually suffer from anaemia. Another important symptom seen in patients suited to this medicine is the craving for extra salts in diet. A person eligible for this medicine comes across as a person with weeping tendencies, especially when alone, worsens when someone consoles him / her and reserved nature.
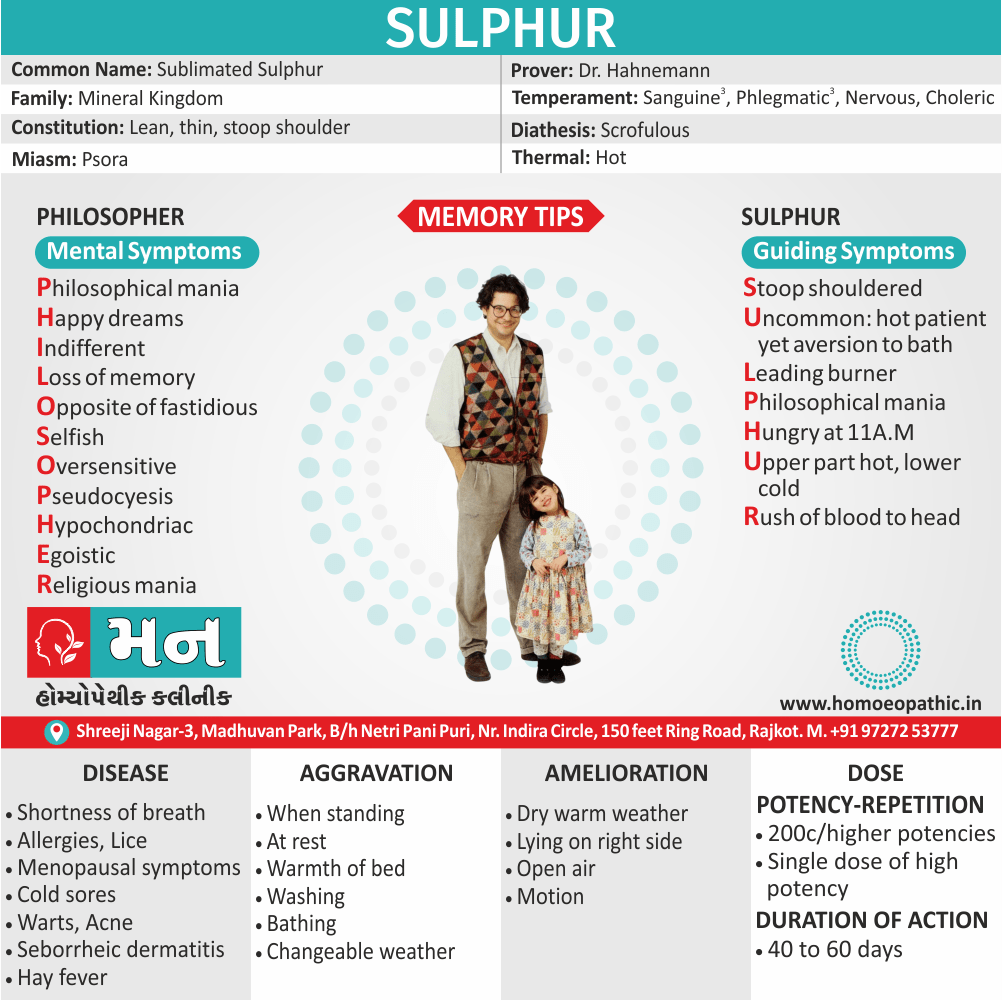
Lycopodium
The patients who require Lycopodium are chronic sufferers of gastric troubles like flatulence and constipation. Lycopodium have a tendency to crave for sweet foods. They also indulge in hot drinks and hot food. They show a tendency to eat far beyond their capacity with resulting bloated abdomen and weight gain. Mentally, the person requiring this medicine very irritable and easily rouse to anger, especially on being contradicted.
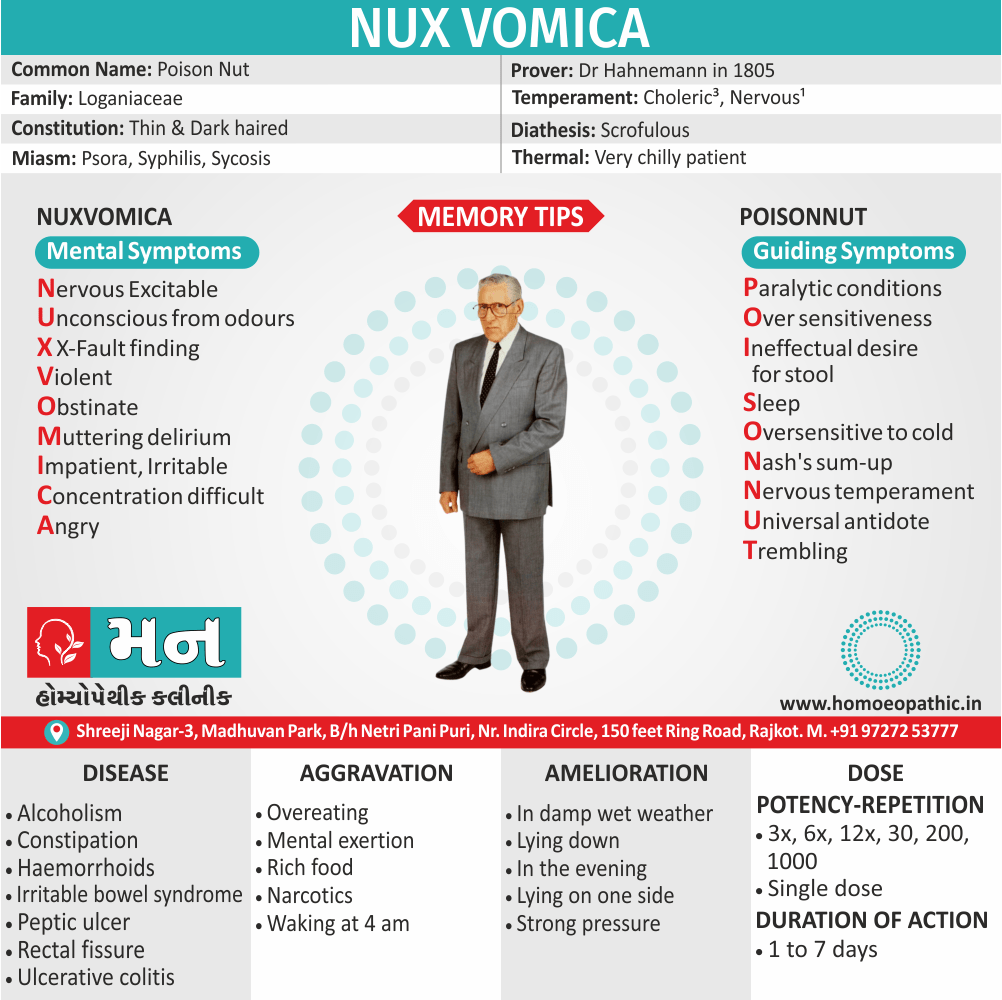
Nux Vomica:
Homeopathic medicine Nux Vomica recommend for persons who have gained excess weight due to sedentary habits. The first important symptom in persons requiring this medicine is that they are chronic sufferers of the most obstinate constipation. most important symptom is the eating habit – a person in need of Nux Vomica homeopathic medicine for losing weight likes spicy food, fatty food and stimulants like coffee or alcoholic drinks. Mentally, the person is extremely sensitive to external impressions and gets angry to an extreme degree too.
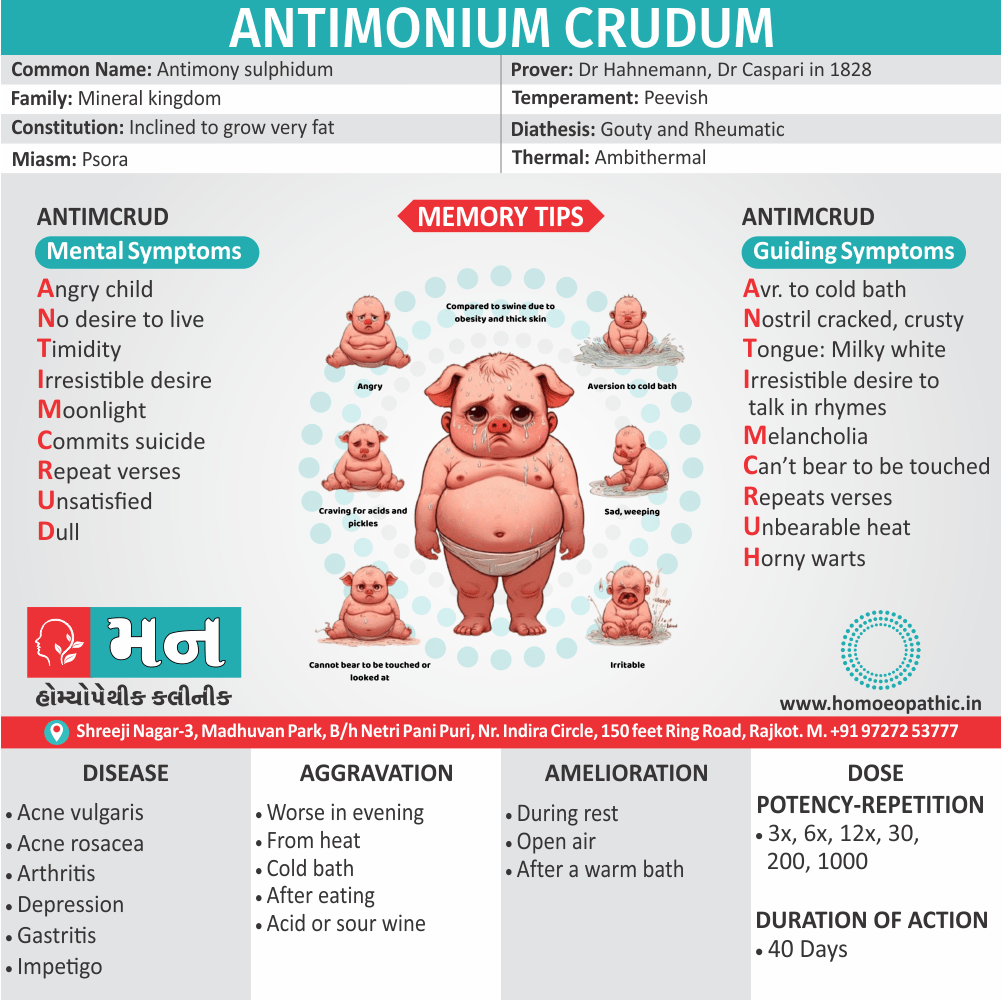
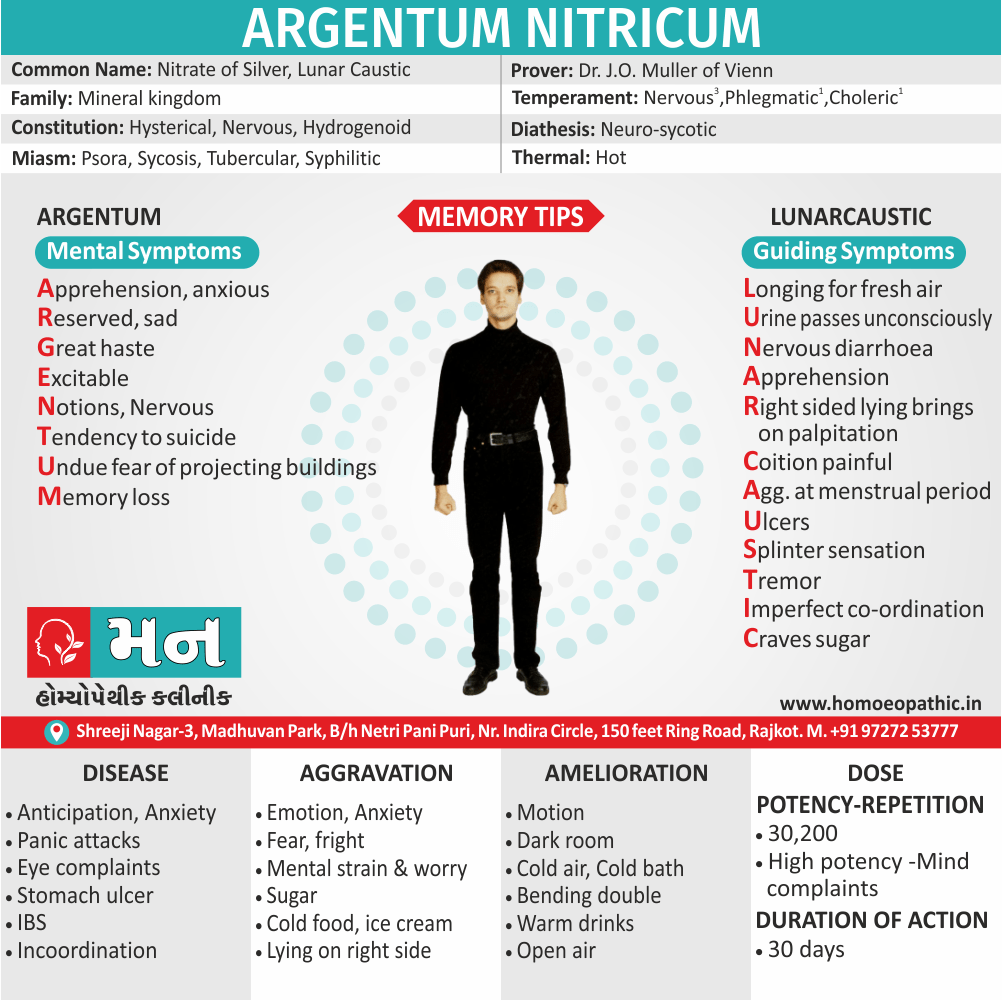
Antimonium Crudum:
This mainly a homeopathic medicine prescribe for heavier person in order to help them lose weight. A suitable candidate for this medicine is a child who possesses extreme irritability, very cross nature, and an aversion to touch or look at. These children also have a marked aversion to cold bathing. The significant indicator for using this medicine to lose weight is a craving for acidic things like pickles in the child. The child’s tongue in this case is usually thickly white coated and the stomach is deranged with alternate diarrhoea and constipation due to a habit of overeating.
CAPSICUM:
Lax fibre, weak; diminished vital heat. Fat, indolent, opposed to physical exertion. In detail; General uncleanliness of body. Homesickness. Worse – while eating, especially from heat, On the other hand Better – open air, uncovering, draughts.
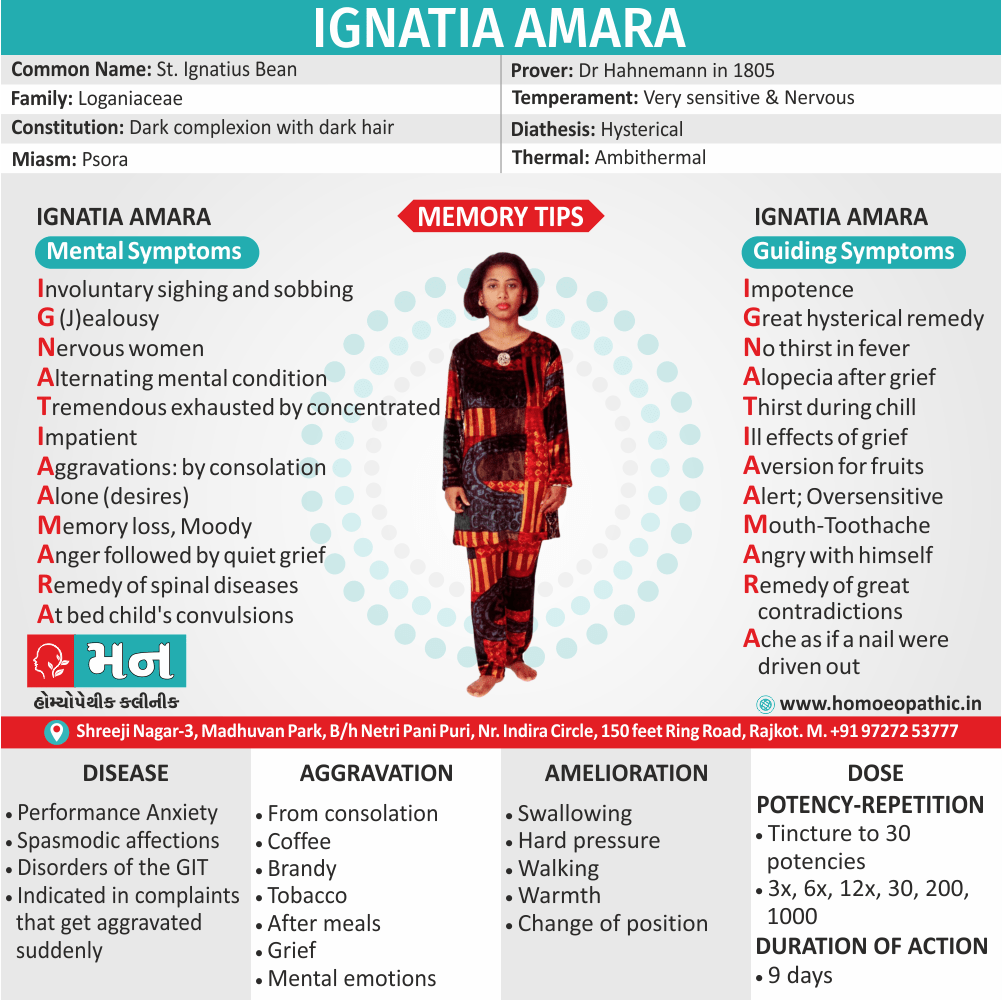
GRAPHITES:
Stout, fair complexion with tendency to skin affections and constipation, fat, chilly also costive. Additionally, Tendency to obesity. Aversion specifically to meat. Sweets nauseate. Besides this; Hot drinks disagree. Burning in stomach causing hunger. Worse – warmth, especially at night, during and after menstruation, whereas Better – dark, from wrapping up.
THYROIDINUM:
Thyroid exercise a general regulating influence over the mechanism of the organs of nutrition, growth also development. In detail; Thyroid weakness causes decided craving for large amounts of sweets. Excessive obesity. Best with pale patients. Weak; tachycardia; Palpitation especially from least exertion.
FUCUS VESICULOSUS:
"For obesity also non – toxic goitre." Digestion is furthered and flatulence is diminished. In addition; Obstinate constipation; forehead feels as if compressed by iron ring. All in all; Thyroid enlargement in heavier person.
Frequently Asked Questions
What is Obesity?
It is a condition characterized by an excess of body fat. In its simplest terms, obesity can be considered to result from an imbalance between the amount of energy consumed in the diet and the amount of energy expended through exercise and bodily functions.
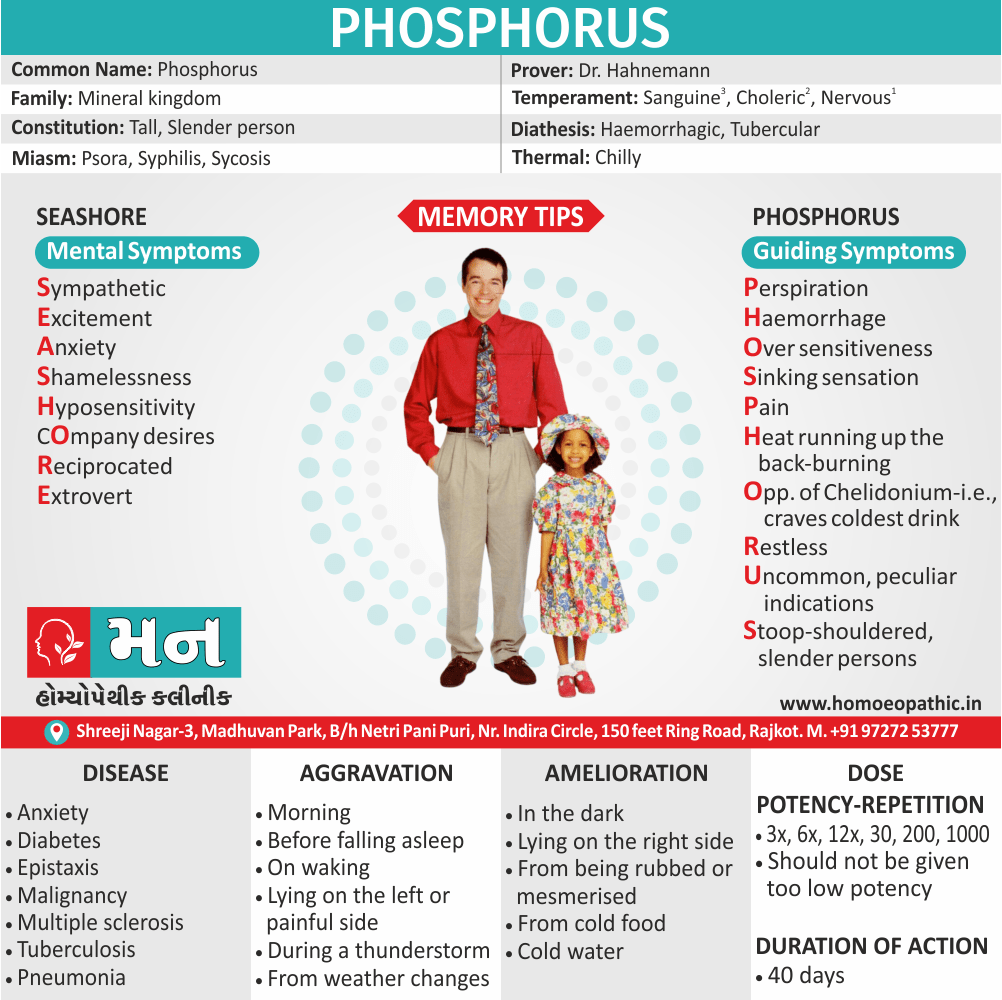
Homeopathic Medicines used by Homeopathic Doctors in treatment of Obesity?
- Calcarea Carb
- Natrum Mur
- Lycopodium
- Nux Vomica
- Antimonium Crud
- Capsicum
- Graphites
- Thyrodinum
What causes Obesity?
- Socio-economic Factor
- Energy dense foods
- Sedentary life
- Genetic role
- A few rare single gene
- Defects in the enzymes
- Mutations
- Additional genetic conditions
- Underlying disorder
What are the symptoms of Obesity?
- Fat appearance
- Emotional problems and poor exercise tolerance.
- Others may possibly experience:
- Abdominal discomfort
- Aching
- Swollen ankles and joints
- Breathlessness
- Sweating
Obesity
Definition
It is a condition characterised by an excess of body fat. Additionally, In its simplest terms, obesity can be considered to result from an imbalance between the amount of energy consumed in the diet and the amount of energy expended through exercise also bodily functions.
Overview
Epidemiology
Causes
Risk Factors
Pathogenesis
Pathophysiology
Types
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Dont’s
Terminology
References
FAQ
Also Search As
Overview
In brief, Obesity is widely regarded as a pandemic, with potentially disastrous consequences for human health.
Demography
In developing countries, average national rates of heavier person are low, but these figures may disguise high rates of heavier person in urban communities; for example, nearly one quarter of women in urban India are higher weight body. In detail, There is increasing public awareness of the health implications of obesity. Many patients will seek medical help for their obesity, on other hand others will present with one of the complications of obesity.
In countries like the USA also the UK, fat deposition is affecting almost the entire population. Additionally, The weight distribution of almost the whole population is shifting upwards – the slim are becoming less slim while the fat is getting fatter. Specifically, In the UK, this translates into a 1-kilogram increase in weight per adult per year (on average over the adult population).
Epidemiology
Indian epidemiology then other
Causes
This refers to the initiating factors that trigger a disease process.
- Examples of causes include:
- Pathogens: Viruses, bacteria, fungi, parasites (infectious diseases)
- Genetic mutations: Inherited or spontaneous changes in genes (genetic diseases)
- Environmental factors: Toxins, radiation, nutritional deficiencies
- Lifestyle choices: Smoking, unhealthy diet, lack of exercise (contributing factors)
Causes
A continuous small daily positive energy balance of only 0.2–0.8 MJ (50–200 kcal; < 10% of intake) would lead to weight gain of 2–20 kg over a period of 4–10 years.
Age i.e.:
Basically; heavier person usually become higher weight body adults. In detail, Weight tends to increase throughout adult life, as BMR and physical activity decrease.
Socio-economic Factor i.e.:
Generally, India it is estimated that 5% of the population receives 40% of the available food energy, leading to obesity in the urban population in parallel with persisting undernutrition in some rural communities
Energy dense foods i.e.:
For example; drinks with highly refined sugar content and salty snacks.
Sedentary life i.e.:
In brief, Decrease in physical activity levels in recent years correlated positively with the number of hours spent watching television. inversely with levels of physical activity (e.g. stair climbing).
Genetic role i.e.:
Twin also adoption studies confirm a genetic influence on obesity.
A few rare single gene disorders i.e.:
This disorders have been identified that lead to severe childhood obesity i.e. melanocortin4 receptor (in other words; MC4R)
Defects in the enzymes processing proopiomelanocortin (POMC, the precursor for adrenocorticotrophic hormone (in other words; ACTH)) in the hypothalamus.
mutations in the leptin gene.
Additional genetic conditions i.e.:
like Prader– Willi also Lawrence–Moon–Biedl syndromes.
underlying disorder i.e.:
such as hypothyroidism or Cushing’s syndrome
Risk Factors
Risk factors are things that make you more likely to develop a disease in the first place.
- Availability of cheap also heavily marketed energy rich foods
- Increase in labour saving devices (e.g. lifts and remote controls)
- Increase in passive transport (for example, cars as opposed to walking, cycling, or walking to public transport hubs).
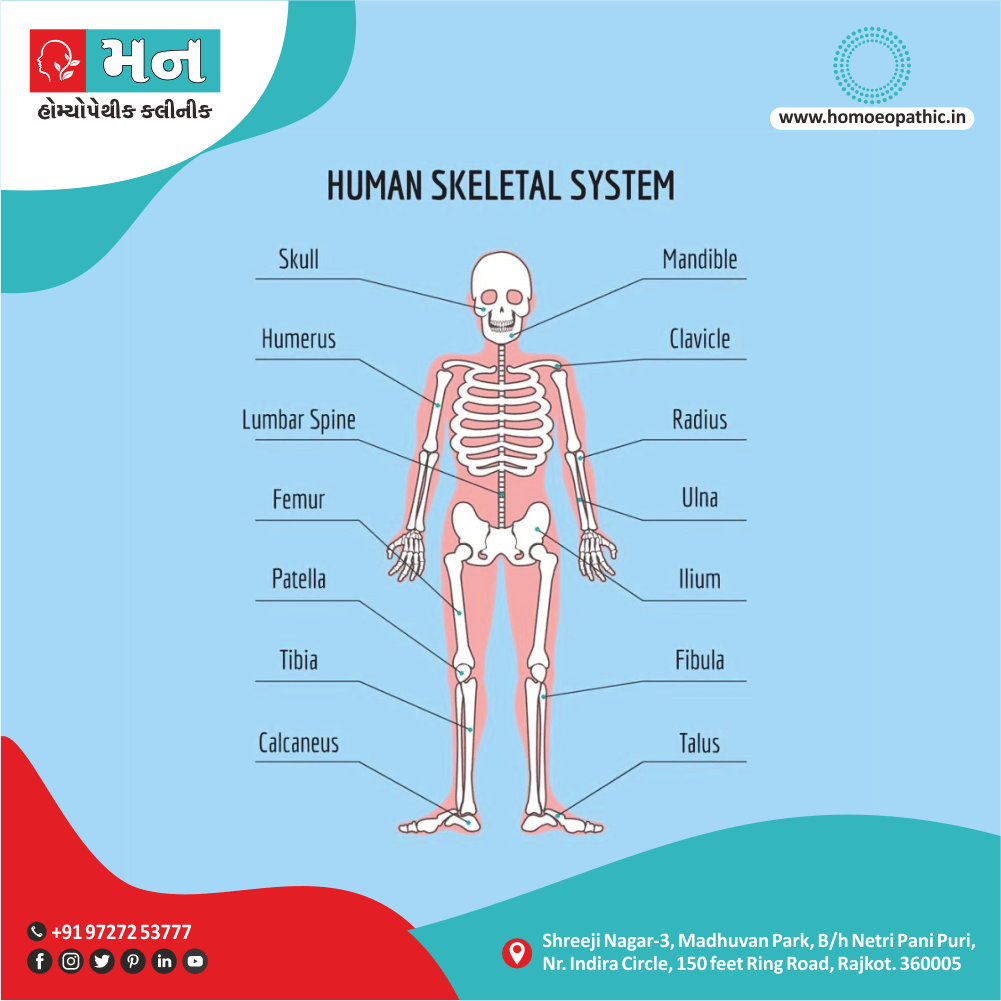
Body Fat Distribution
Increased intra abdominal fat causes ‘central’ (for example; ‘abdominal’, ‘visceral’, ‘android’ or ‘apple shaped’) obesity, which contrasts with subcutaneous fat accumulation causing ‘generalised’ (either ‘gynoid’ or ‘pear-shaped’) obesity; the former is more common in men and is more closely associated with type 2 diabetes, the metabolic syndrome also cardiovascular disease .
Besides this; The key difference between these depots of fat may lie in their vascular anatomy, with intra abdominal fat draining into the portal vein and thence directly to the liver.
Pathogenesis
Pathogenesis refers to the development of a disease. It’s the story of how a disease gets started and progresses.
This is the entire journey of a disease, encompassing the cause but going beyond it.
Pathophysiology
Pathophysiology, on the other hand, focuses on the functional changes that occur in the body due to the disease. It explains how the disease disrupts normal physiological processes and how this disruption leads to the signs and symptoms we see.
Imagine a car accident. Pathogenesis would be like understanding how the accident happened – what caused it, the sequence of events (e.g., one car ran a red light, then hit another car). Pathophysiology would be like understanding the damage caused by the accident – the bent fenders, deployed airbags, and any injuries to the passengers.
In simpler terms, pathogenesis is about the "why" of a disease, while pathophysiology is about the "how" of the disease’s effects.
Types
AAA
Clinical Features
Tab Content
Sign & Symptoms
Fat appearance.
Weight of 20% or more than ideal for height and body frame. In detail; Some heavier person have no physical symptoms but may have associated emotional problems and poor exercise tolerance.
Others may possibly experience:
Abdominal discomfort
Aching
Swollen ankles and joints
Breathlessness
Sweating
Increased fatigue
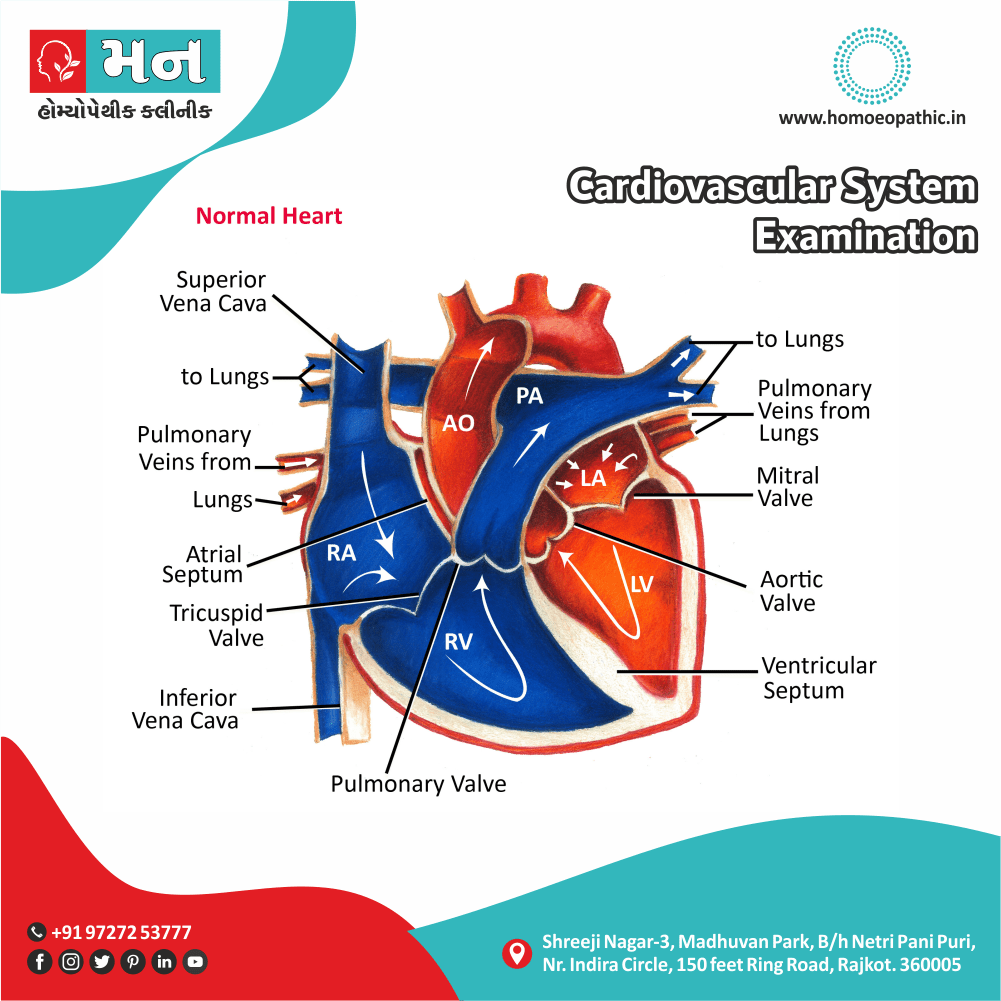
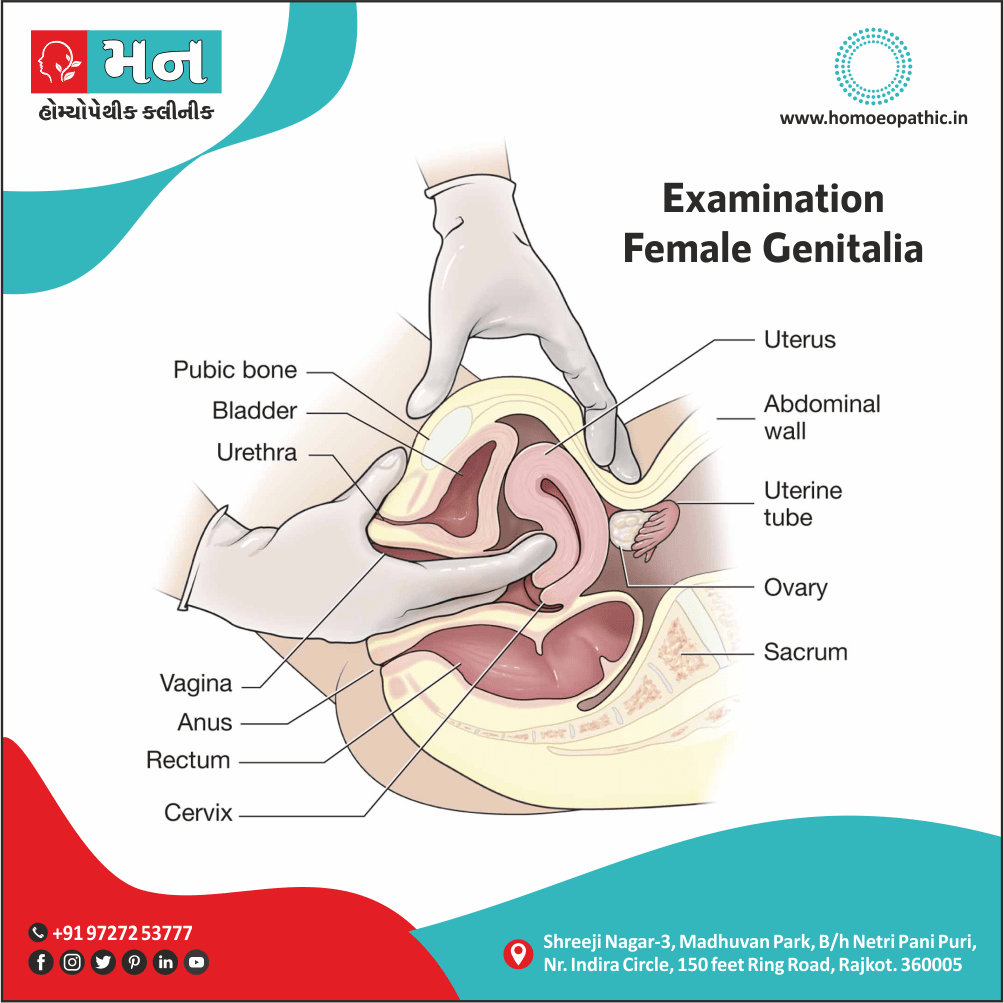
Clinical Examination
Tab Content
Diagnosis
Tab Content
Differential Diagnosis
Complications
Complications are what happen after you have a disease. They are the negative consequences of the disease process.
Risk factors
| Outcome |
‘Metabolic syndrome’
Type 2 diabetes Hypertension Hyperlipidaemia Liver fat accumulation |
Coronary heart Disease Stroke Diabetic Complications Non-alcoholic steatohepatitis Cirrhosis |
| Restricted ventilation | Exertional dyspnoea Obstructive sleep apnoea Obesity hypoventilation syndrome (in other words; Pickwickian syndrome) |
Mechanical effects of weight
| Urinary incontinence Osteoarthritis |
Increased peripheral steroid interconversion in adipose tissue
| Hormone-dependent cancers (breast, uterus) Polycystic ovarian syndrome (for example; infertility, hirsutism) |
| Others | Psychological morbidity (for example; low self-esteem, depression) Socioeconomic disadvantage (lower income, less likely to be promoted) Gallstones Colorectal cancer Skin infections (groin and sub mammary candidiasis; hidradenitis) |
Investigations
Clinical assessment
- quantify the problem
- exclude an underlying cause
- identify complications
- reach a management plan
Severity of obesity can be quantified using the BMI.
How to measure BMI i.e.:
- Body Mass Index is a simple calculation using a person’s height and weight. The formula is BMI = kg/m2 where kg is a person’s weight in kilograms and m2 is their height in metres squared.A BMI of 25.0 or more is overweight, while the healthy range is 18.5 to 24.9. BMI applies to most adults 18-65 years.
Treatment
Therapeutic option for obesity
1st level management i.e.:
↑Exercise
Eating behaviour modification
including food selection, portion size control, avoidance of snacking, regular meals to encourage satiety, also substitution of sugar with artificial sweeteners. Regular support from a dietitian or attendance at a weight loss group may be helpful.
Treat cardiovascular risk factors
2nd level management i.e.:
Supervised low-calorie diet
The composition of the diet should ensure a minimum of 50 g of protein each day for men and 40 g for women to minimise muscle degradation. Energy content should be a minimum of 1.65 MJ (in other words; 400 kcal) for women of height < 1.73 m, and 2.1 MJ (in other words; 500 kcal) for all men and for women taller than 1.73 m.
3rd level management i.e.:
Drugs for example; sibutramine, rimonabant, orlistat
Drug therapy is usually reserved for patients with high risk of complications from obesity
4th level management i.e.:
surgery i.e. laparoscopic bariatric surgical procedures (i.e. ‘Bariatric’ surgery)
Generally, Cosmetic surgical procedures may be considered in heavier person after successful weight loss. Besides this; This operation is of no value for long-term weight reduction if food intake remains unrestricted.
Prevention
Tab Content
Homeopathic Treatment
Calcarea Carbonica:
This medicine is mainly given when there is excess fat in the abdomen and the metabolism is working at a very low pace, resulting in obesity and weight gain. A patient requiring this medicine is fatty and flabby. In order to be eligible to use this medicine to lose weight, the constitutional symptoms shown by the patient are given utmost importance. The eating habits include craving for boiled eggs, and strange things like chalk, clay, pencils, lime etc. Due to a sluggish metabolic activity, the patients are almost always constipated. This medicine can also be considered if the excess weight gain is due to thyroid problems.
Natrum Mur:
This medicine is recommended when there is an excess of fat mainly in the thighs and buttocks as compared to other parts of the body. This medicine gives wonderful results if the person has gained excess weight due to long continued stress or depression. The patients who require this medicine usually suffer from anaemia. Another important symptom seen in patients suited to this medicine is the craving for extra salts in diet. A person eligible for this medicine comes across as a person with weeping tendencies, especially when alone, worsens when someone consoles him / her and reserved nature.
Lycopodium
The patients who require Lycopodium are chronic sufferers of gastric troubles like flatulence and constipation. Lycopodium have a tendency to crave for sweet foods. They also indulge in hot drinks and hot food. They show a tendency to eat far beyond their capacity with resulting bloated abdomen and weight gain. Mentally, the person requiring this medicine very irritable and easily rouse to anger, especially on being contradicted.
Nux Vomica:
Homeopathic medicine Nux Vomica recommend for persons who have gained excess weight due to sedentary habits. The first important symptom in persons requiring this medicine is that they are chronic sufferers of the most obstinate constipation. most important symptom is the eating habit – a person in need of Nux Vomica homeopathic medicine for losing weight likes spicy food, fatty food and stimulants like coffee or alcoholic drinks. Mentally, the person is extremely sensitive to external impressions and gets angry to an extreme degree too.
Antimonium Crudum:
This mainly a homeopathic medicine prescribe for heavier person in order to help them lose weight. A suitable candidate for this medicine is a child who possesses extreme irritability, very cross nature, and an aversion to touch or look at. These children also have a marked aversion to cold bathing. The significant indicator for using this medicine to lose weight is a craving for acidic things like pickles in the child. The child’s tongue in this case is usually thickly white coated and the stomach is deranged with alternate diarrhoea and constipation due to a habit of overeating.
CAPSICUM:
Lax fibre, weak; diminished vital heat. Fat, indolent, opposed to physical exertion. In detail; General uncleanliness of body. Homesickness. Worse – while eating, especially from heat, On the other hand Better – open air, uncovering, draughts.
GRAPHITES:
Stout, fair complexion with tendency to skin affections and constipation, fat, chilly also costive. Additionally, Tendency to obesity. Aversion specifically to meat. Sweets nauseate. Besides this; Hot drinks disagree. Burning in stomach causing hunger. Worse – warmth, especially at night, during and after menstruation, whereas Better – dark, from wrapping up.
THYROIDINUM:
Thyroid exercise a general regulating influence over the mechanism of the organs of nutrition, growth also development. In detail; Thyroid weakness causes decided craving for large amounts of sweets. Excessive obesity. Best with pale patients. Weak; tachycardia; Palpitation especially from least exertion.
FUCUS VESICULOSUS:
"For obesity also non – toxic goitre." Digestion is furthered and flatulence is diminished. In addition; Obstinate constipation; forehead feels as if compressed by iron ring. All in all; Thyroid enlargement in heavier person.
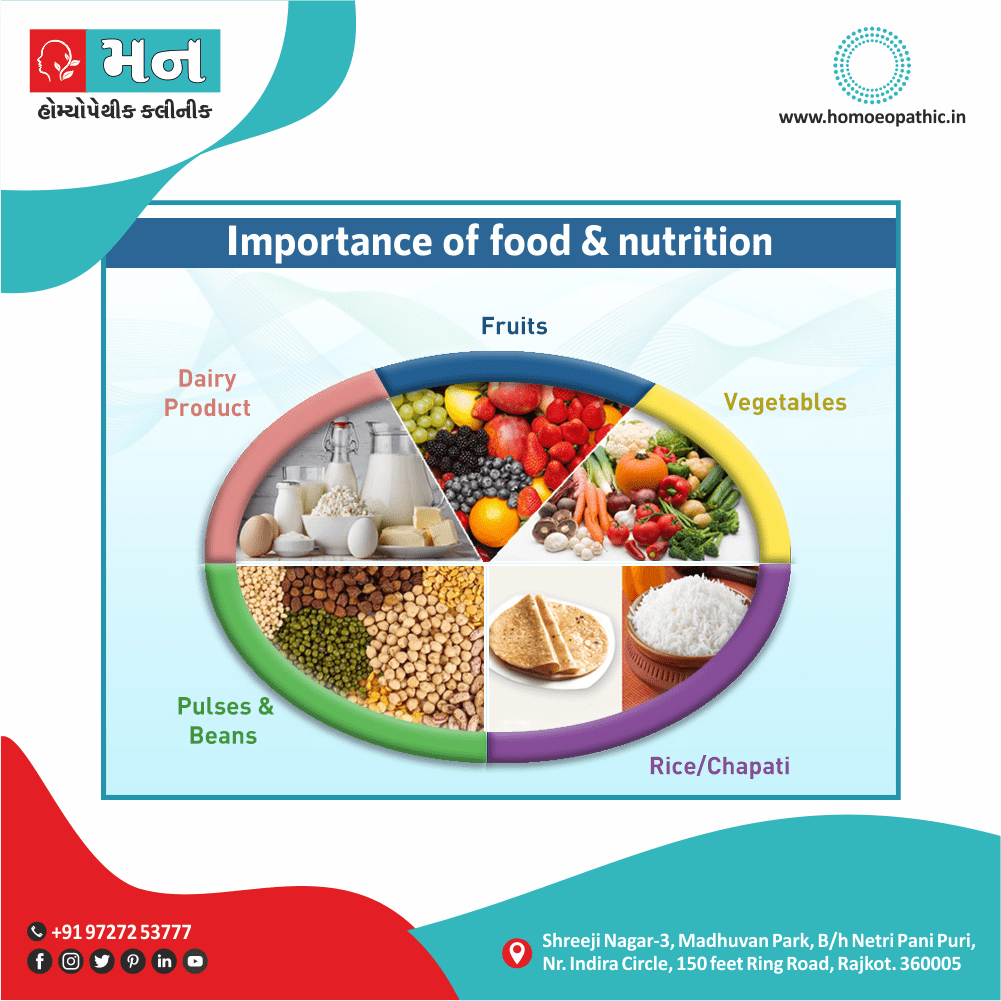
Diet & Regimen
- making healthier food choices
- drink plenty of water
- limit intake of foods containing saturated fat, added salt, added sugars and alcohol
- Avoid junk food such as burgers cheese fries
- Avoid fad diets such as meat, fish, wheat or dairy products
Do’s and Dont’s
Tab Content
Terminology
Tab Content
References
- Davidson’s Principles and Practice of Medicine (22nd edition)
- Department of Health (Obesity Guidelines)
- https://www.oxfordhandbooks.com/view/10.1093/oxfordhb/9780199736362.001.0001/oxfordhb-9780199736362-e-003
- https://www.emedicinehealth.com/obesity/article_em.htm
FAQ
Frequently Asked Questions
What is Obesity?
It is a condition characterized by an excess of body fat. In its simplest terms, obesity can be considered to result from an imbalance between the amount of energy consumed in the diet and the amount of energy expended through exercise and bodily functions.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Obesity?
- Calcarea Carb
- Natrum Mur
- Lycopodium
- Nux Vomica
- Antimonium Crud
- Capsicum
- Graphites
- Thyrodinum
What causes Obesity?
- Socio-economic Factor
- Energy dense foods
- Sedentary life
- Genetic role
- A few rare single gene
- Defects in the enzymes
- Mutations
- Additional genetic conditions
- Underlying disorder
What are the symptoms of Obesity?
- Fat appearance
- Emotional problems and poor exercise tolerance.
- Others may possibly experience:
- Abdominal discomfort
- Aching
- Swollen ankles and joints
- Breathlessness
- Sweating
Also Search As
Frequently Asked Questions (FAQ)
XYZ
XXX
XYZ
XXX
XYZ
XXX
How can I find reputable homeopathy clinics or homeopathic doctors in my area?
You can found Homeopathic Clinic For XXXX by searching for
Specific city Examples are
You can also search for near you Examples are