Examination Of The Respiratory System
Examination Of The Respiratory System is carried out with a simultaneous general assessment. For the examination the patient should resting comfortably on a bed or couch, supported by pillows so that they can lean back comfortably at an angle of 45 °.
OBSERVATION IN RESPIRATORY SYSTEM EXAMINATION:
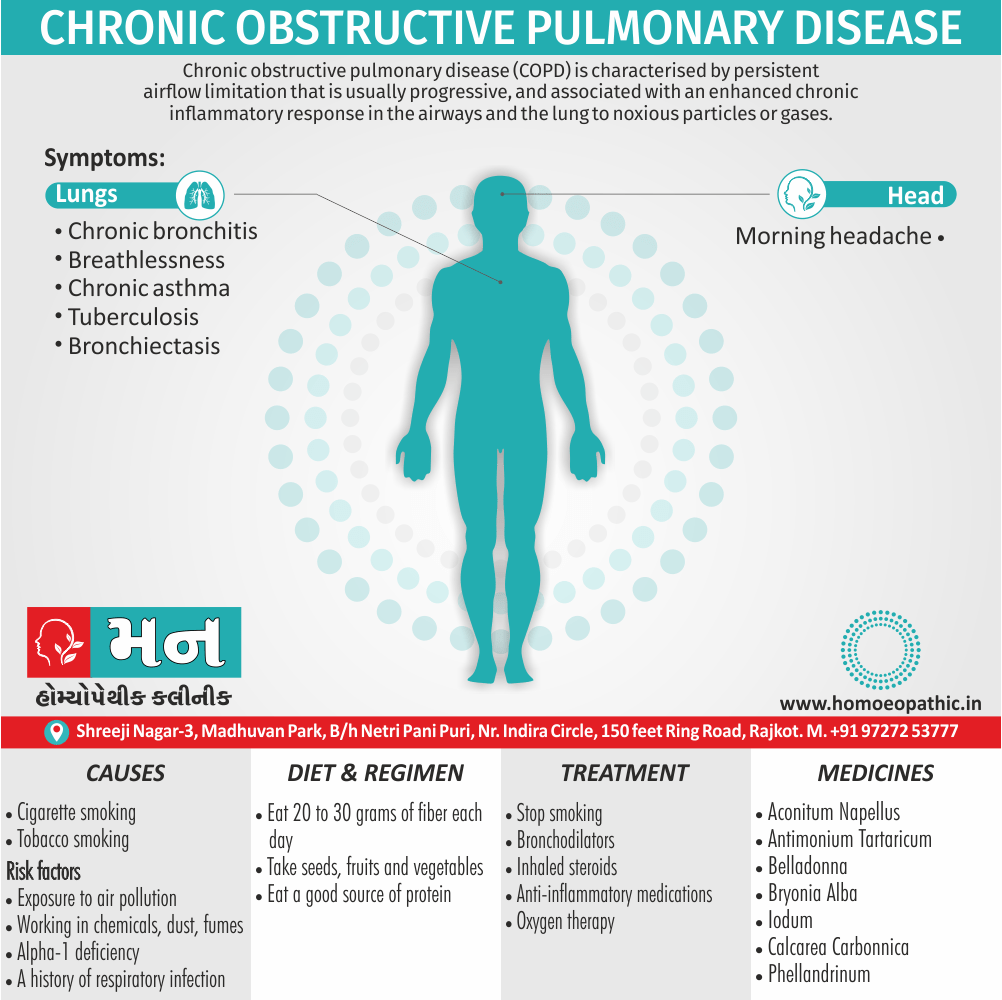
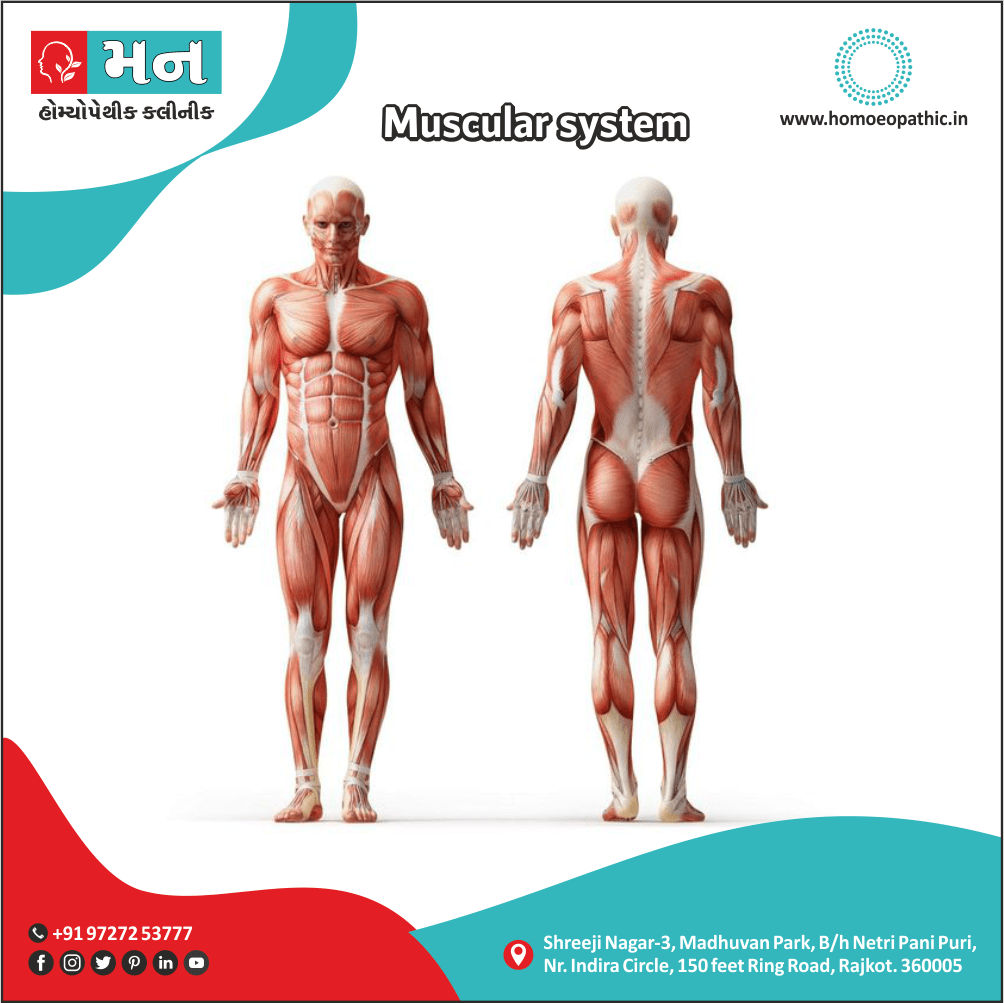
During Examination Of The Respiratory System the hands should inspect for clubbing, pallor or cyanosis. The lips and tongue should inspect for central cyanosis. Additionally, A breathless patient may be using the accessory muscles of respiration. Overall, Breathing out through pursed lips observe in patients suffering from severe COPD.
INSPECTION IN RESPIRATORY SYSTEM EXAMINATION:
In brief, A careful inspection must done in respiratory system examination to look out for any visible scars as a result of previous injury or previous surgery, lumps under the skin or any lesions on the skin. Furthermore, Chest should inspect for it shape and its movement.
SHAPE OF THE CHEST:
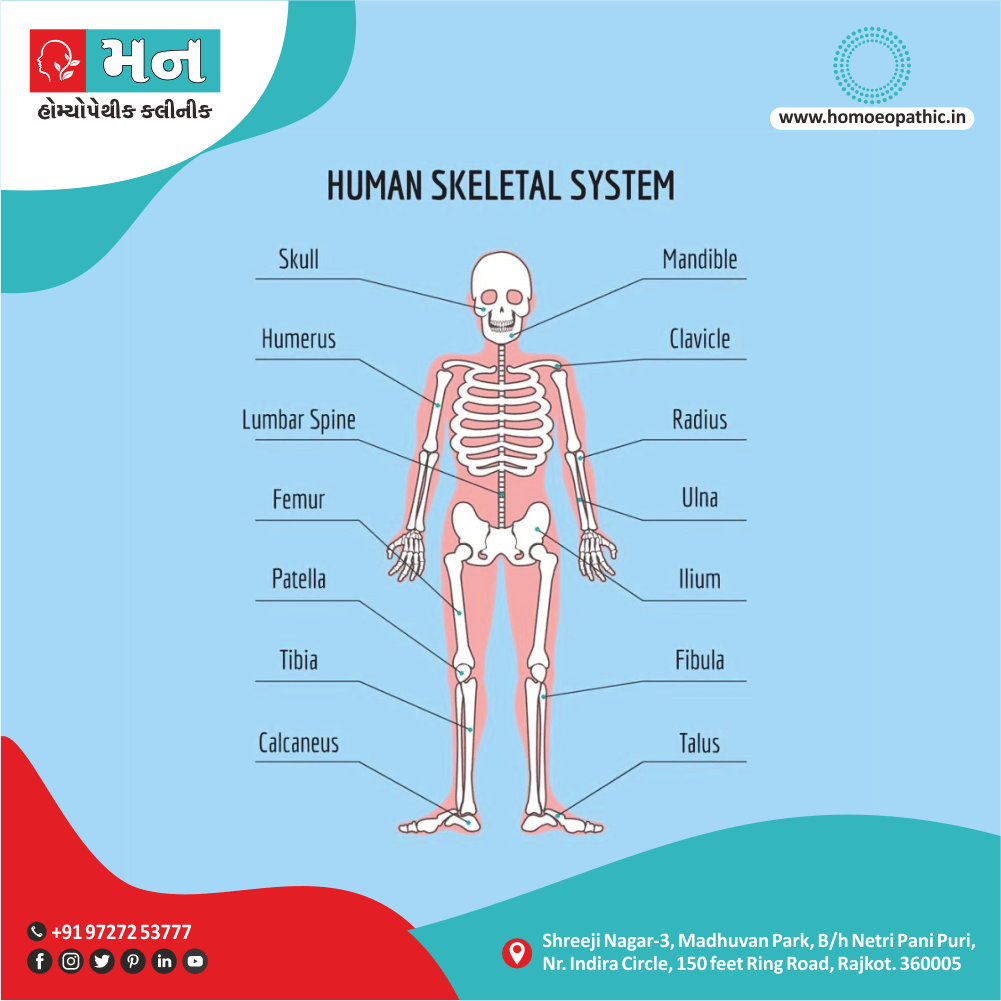
The normal chest is bilaterally symmetrical, with smooth contours and elliptical in cross-section with a slight recession below the clavicle. Additionally, Its transverse diameter is greater than the anterior posterior diameter with the ratio being 7:5. The chest may distort by disease of the either ribs or spinal vertebrae, or by underlying lung disease.
Barrel Chest:
It most easily appreciate as increased anteroposterior diameter. The sub-costal angle is wide, angle of Louis unduly prominent, sternum more arched, ribs show less obliquity also spine is concave forward. It occurs as a result of over-inflated lungs seen in case of COPD, usually emphysema, but may seen normally during infancy also accompanying normal aging.
Funnel Chest (i.e. Pectus Excavatum or Cobbler’s chest):
It characterize by a depression in the lower portion of the sternum. It may congenital as a consequence of Rickets in either childhood or may be occurring as an occupational deformity in cobblers. Due to the sternal depression, the normal cardiac shadow may appear enlarged on X-ray chest (Known as Pomfret’s heart.)
Pigeon Chest (Keeled chest or Pectus Carinatum):
Sternum displace anteriorly, increasing the anteroposterior diameter and the costal cartilages adjacent to the protruding sternum depress. It often associate with bead like enlargement at the costochondral junction, known as Rickety Rosary and a transverse groove seen passing outwards from the xiphisternal junction to the mid-axillary line, known as Harrison’s Sulcus.
Traumatic Flail Chest:
In case of multiple ribs fracture, paradoxical movements of the thorax may seen. Furthermore, As downward movement of the diaphragm during respiration decreases the intrathoracic pressure on inspiration, the injured area arches inward and on expiration, it arches outward.
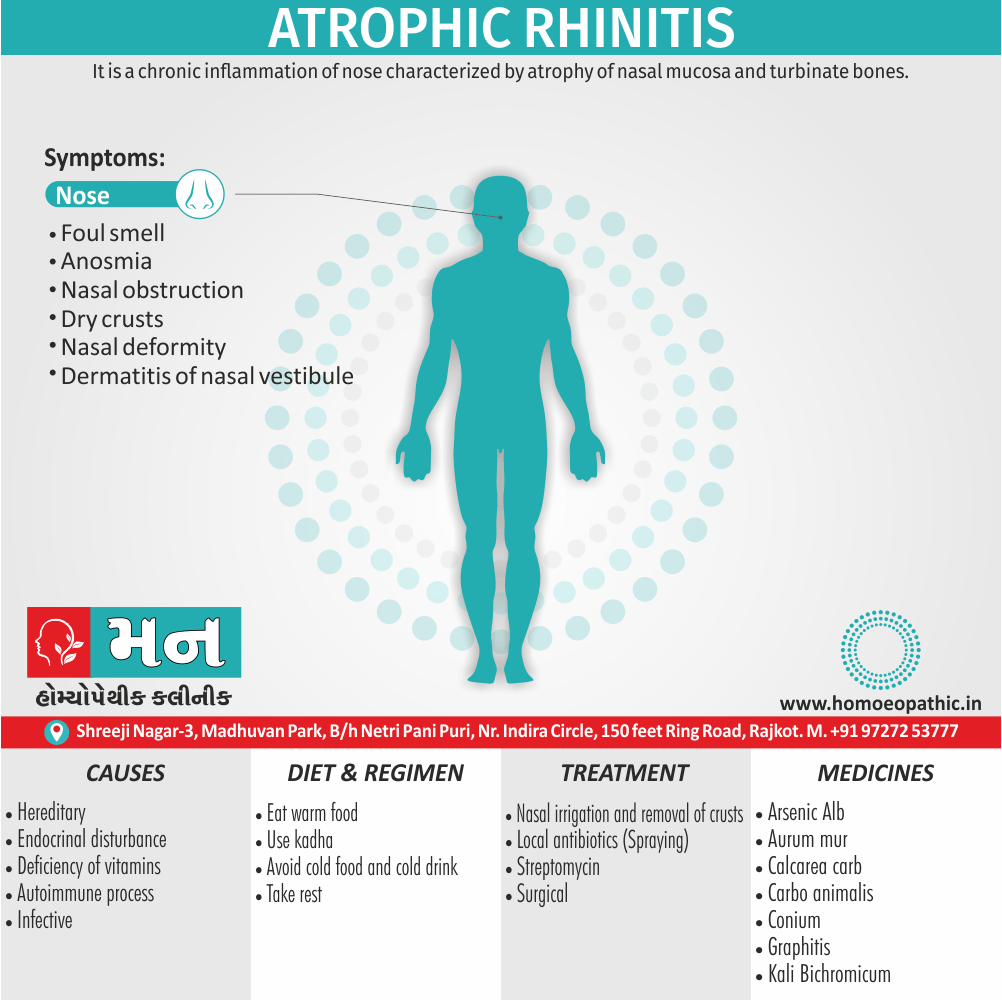
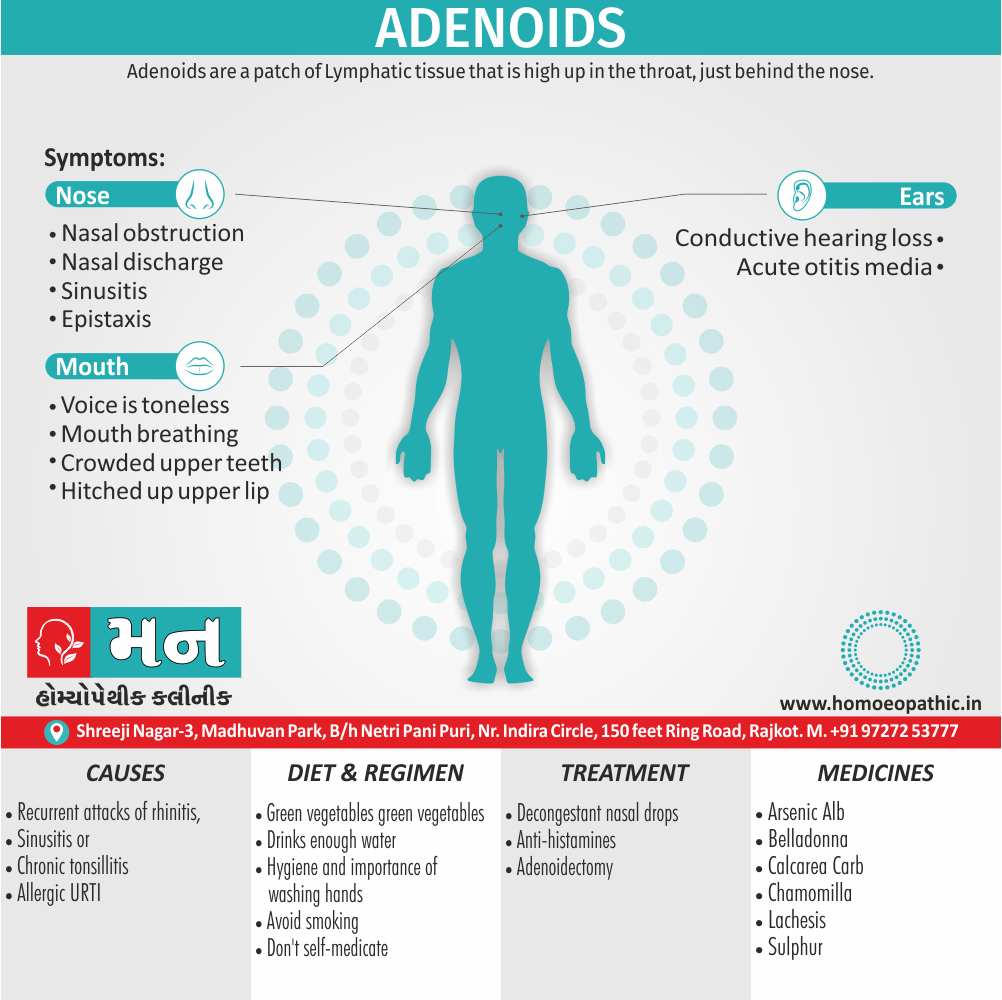
Flat Chest (Phthinoid chest):
In chronic nasal obstructive diseases like adenoid lymphoid hypertrophy or bilateral Pulmonary Koch’s or childhood rickets, due to obstruction to the airway, the anteroposterior diameter is reduced.
Thoracic Kyphoscoliosis:
Kyphosis (forward bending of spine) or scoliosis (lateral bending of spine) can lead to asymmetry of the chest, and if severe may significantly restrict lung movement.
Bulging, Depression or Flattening:
It may observe that one side of the chest may bulge outwards. Additionally, This usually observe in pleural effusion, pneumothorax, tumors, aneurysms, cardiomegaly, etc. Specific localized bulging seen in aortic aneurysm, pericardial effusion, liver abscess, chest wall tumors, etc.
Similarly, one side of the chest may flattened or depressed. It usually seen associated with either fibrosed or collapsed lungs, pleural adhesions or one sided muscle wasting as seen in poliomyelitis.
MOVEMENT OF THE CHEST:
Movements of the chest should well observe for their symmetry, rate, rhythm also type of respiration. Normally both the sides of the chest wall move uniformly without bulging or in-drawing of the interspaces. Intercostal recession, a drawing-in of the intercostal spaces with inspiration may indicate severe upper airways obstruction, or tumours of the trachea. In COPD the lower ribs usually move inwards on inspiration instead of the normal outwards movement.
DIMINISHED MOVEMENTS:
Basically, Unilaterally diminished movements seen in conditions such as obstruction to the main bronchus, fibrosis of lungs, pleural adhesions, severe lung collapse, consolidations, pleural effusion, hydropneumothorax, etc.
On the other hand, Bilaterally diminished movements seen in cases of emphysema, bilateral fibrosis, bilateral collapse, bilateral consolidation, hydropneumothorax, bronchial asthma, etc.
RESPIRATORY RATE:
To view details about respiratory rate kindly refer to the General Examination Section.
DYSPNOEA:
Dyspnoea define as difficult or labored breathing. It is a normal symptom of heavy exertion but becomes pathological if it occurs in unexpected situations.
Dyspnoea can be graded as follows:
GRADE 0 DEGREE None
No shortness of breath on either leveled road or uphill.
GRAD 1 DEGREE Mild
Trouble of shortness of breath on either leveled road or walking uphill.
GRAD 2 DEGREE Moderate
Comparatively, Walking pace slower than the person of his same age.
GRAD 3 DEGREE Severe
Has to stop after walking a distance of about 100 yards.
GRAD 4 DEGREE Very Severe
Shortness of breath even on rest.
RESPIRATORY RHYTHM:
Normal process of respiration involves a regular rhythm of inspiration also expiration with inspiration being longer than expiration.
Irregularities in Respiratory Rhythm can be of following types:
TYPE : Kussmaul’s respiration (in other words, Air hunger)
Characterized by deep also rapid respiration.
Seen in Diabetic ketoacidosis, alcoholics, uremia also starvation ketoacidosis.
TYPE : Cheyne-Stokes respiration
Cyclical deepening and quickening of respiration (in other words; hyperapnoea), followed by diminishing respiratory effort and rate, sometimes with a short period of complete apnea.
Seen in Severely ill patients, left ventricular failure, narcotic drug poisoning especially by either opium or barbiturates, conditions of increased intra-cranial pressure, damage to either cerebrum or diencephalon and neurological disorders; occasionally seen in elderly patients during sleep, without any obvious serious disease.
TYPE : Biot’s respiration
Irregularly regular respiration.
Lastly, Seen in Meningitis and raised intra-cranial pressure.
TYPE : Stridor
Prolonged, high pitched, inspiratory sound through the obstructed upper airway.
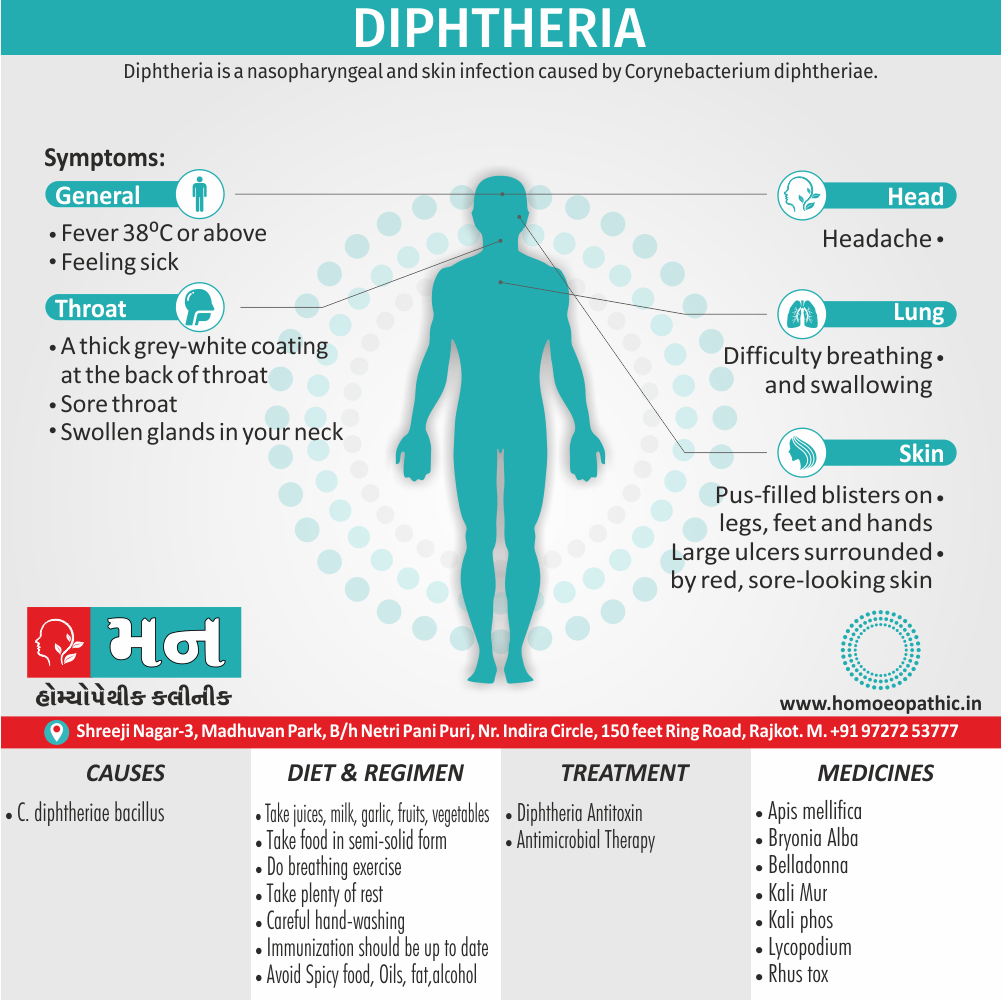
Furthermore, Seen in Laryngeal or tracheal obstruction, laryngeal diphtheria, mediastinal growths or tumors.
TYPE : Wheezing
Prolonged expiration through an obstructed lower airway, bronchi or bronchioles, reflecting narrowing of smaller airways.
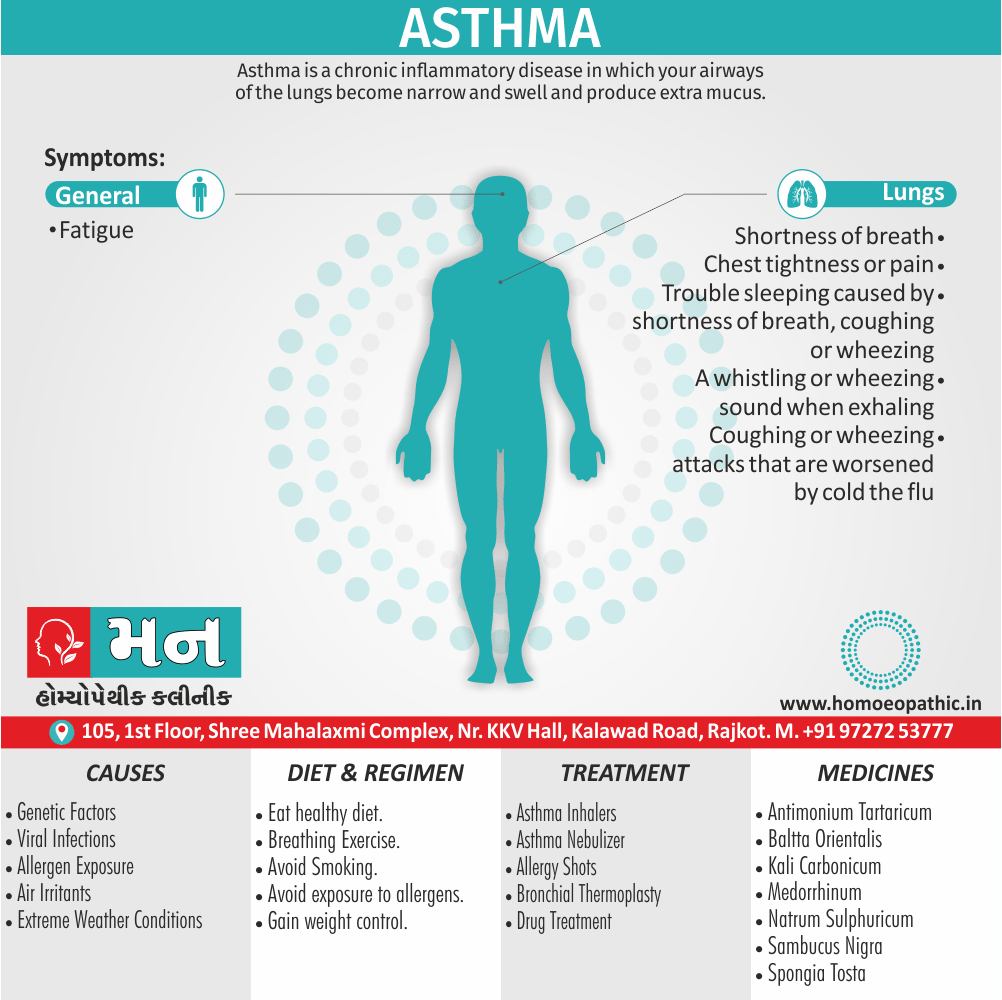
Seen in Bronchial asthma, cardiac asthma, renal asthma.
TYPE : Stertor
Death Rattle; commonly occurring in a dying person.
Seen in Coma or deep sleep.
TYPE OF BREATHING:
In males and some females breathing normally is abdominothoracic. In case of thoracoabdominal breathing, thoracic movements are more prominent as compared to abdominal movements.
TYPE : ABDOMINAL
Abdominal movements are predominant and thoracic movements are diminished.
Seen in Pleurisy, Lung collapse.
TYPE : THORACIC
Thoracic movements are predominant and abdominal movements are diminished.
Additionally, Seen in Diaphragmatic paralysis, peritonitis, severe ascites.
INSPECTION OF MEDIASTINUM
A normal mediastinum is central. The shift of mediastinum can be detected by noting the respective position of trachea and apex beat. In case of shift in mediastinum, the sternocleidomastoid becomes more prominent on the side to which trachea is shifted. This phenomenon is known as Trail Sign.
The position of mediastinum in various respiratory diseases is given as follows:
CENTRAL MEDIASTINUM i.e.-
- Emphysema
- Pneumonia
- Interstitial fibrosis
- Lung abscess
- Bronchial asthma
- Bronchitis
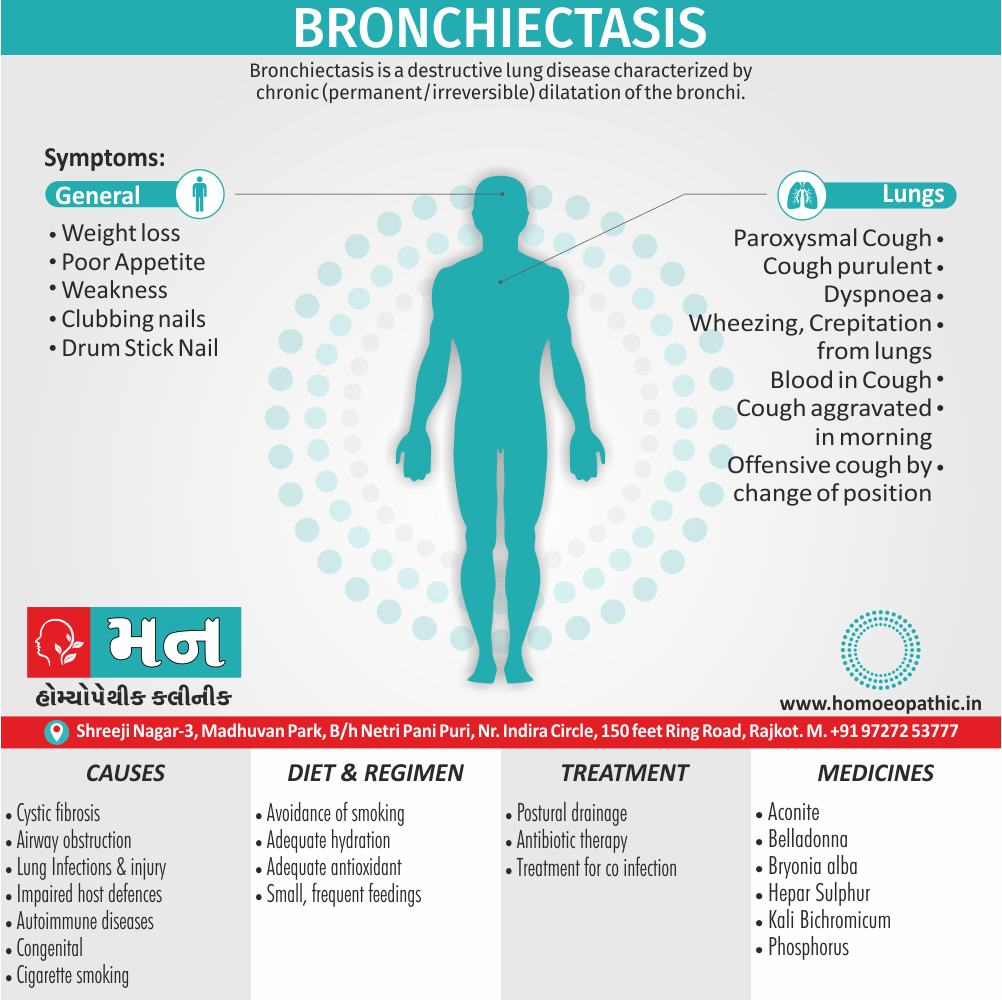
- Bronchiectasis
MEDIASTINUM – SHIFTED TO THE SAME SIDE i.e.
- Collapse
- Pleural thickening
- Fibrosis
MEDIASTINUM – SHIFTED TO THE OPPOSITE SIDE i.e.
- Pneumothorax
- Pleural effusion
- Hydropneumothorax
PALPATION IN RESPIRATORY SYSTEM EXAMINATION
IDENTIFY TENDER AREAS:
Carefully palpate any area where pain has been reported or where lesions or bruises are evident. Assess any observed abnormalities either masses or sinus tracts (e.g. blind, inflammatory, tube-like outlets opening onto the skin).
TEST CHEST EXPANSION:
Place your thumbs at about the level of the 10th ribs, with your fingers loosely grasping and parallel to the lateral rib cage and slide them medially just enough to raise a loose fold of skin on either side between your thumb and the spine. Moreover; Ask the patient to inhale deeply. Besides this, Observe the distance between your thumbs as they move apart during inspiration and feel for the range and symmetry of the rib cage as it expands and contracts.
LYMPH NODES PALPATION:
The lymph nodes in the supraclavicular fossae, cervical regions and axillary regions should be palpated. If they are enlarged this may be as a result of secondary spread of malignancy from the chest.
TRACHEA AND HEART PALPATION:
The positions of the cardiac impulse and trachea should be determined. Putting the second and fourth fingers of the examining hand on each edge of the sternal notch, use the third finger to assess whether the trachea is central or deviated to any side. Displacement of the cardiac impulse without displacement of the trachea may be due to scoliosis, congenital funnel depression of the sternum or enlargement of the left ventricle. In the absence of these conditions a significant displacement of the cardiac impulse or trachea, or of both together, suggests that the position of the mediastinum has been altered by disease of the lungs or pleura.
TACTILE VOCAL FREMITUS:
It is defined as tactile perception of vibrations communicated to the chest wall from the bronchopulmonary tree during the act of phonation.
To detect fremitus, use either the ball of the palm, base of the fingers or the ulnar surface of your hand to optimize the vibratory sensitivity of your hand. Ask the patient to repeat the words like “ninety-nine” or “one-one-one.” Palpate and compare bilaterally symmetric areas of the lungs for its fremitus. Identify and locate any areas of increased, decreased, or absent fremitus.
TACTILE VOCAL FREMITUS : INCREASED
Seen in
- Pyogenic consolidation
- Tuberculous consolidation
- Pulmonary infarction
- Surrounding a malignant lesion
TACTILE VOCAL FREMITUS : DECREASED
Seen in
- Emphysema
- Pulmonary fibrosis
- Lung collapse
- Bronchial asthma
- Bronchial obstruction
- Pleural effusion
- Pneumothorax
- Hydropneumothorax
ABNORMAL VIBRATIONS:
PLEURAL FRICTION RUB – It a vibration felt as a rub usually during the peak of inspiration or early expiration, commonly seen in case of pleurisy.
BRONCHIAL FREMITUS – It is a vibration that can palpate on the chest wall over a bronchus. It often feel in diseases like bronchitis, bronchial asthma and COPD.
PALPABLE RALES – They are felt in conditions like bronchiectasis, pulmonary fibrosis and pulmonary congestion.
PERCUSSION IN RESPIRATORY SYSTEM EXAMINATION
In Respiratory System examination percussion helps you to access whether the underlying tissues air-fill, fluid-fill, or solid.
ABNORMAL NOTES:
In conditions when the amount of air in the alveoli decreases, the lungs fail to vibrate sufficiently to the percussion stroke. This occurs in conditions such as
- Consolidations
- Infiltrations
- Fibrosis
- Lung Collapse
DULL NOTES:
An impaired note of a higher degree is called a dull note.
It is felt in conditions like –
- Consolidations
- Infiltrations
- Fibrosis
- Lung Collapse
- Pleural Thickening
STONY DULL NOTES:
It is a type of percussion note which is completely devoid of resonance or it may express extreme level of dullness. This is mainly due to underlying fluid, as fluid dampens the vibrations or due to underlying fibrosis, mass or thickening. It is a common associate in conditions like –
- Pleural Effusion
- Lung Fibrosis
- Pleural Thickening
- Solid Intrathoracic tumor
TYMPANY:
Tympany a hollow drum-like resonant sound produced when a gas-containing cavity tapped sharply. It may felt over the chest wall in following conditions –
- Emphysema
- Pneumothorax
- Superficial empty cavities
SUB TYMPANY:
It also known as Skodaic resonance. It is a hype resonant note of a boxy quality occurring due to relaxed lungs, felt just above the levels of pleural effusion.
HYPER-RESONANCE:
It is a note of a loud intensity, low pitch and lasts for a longer time, ranging between normal resonance and tympany and may well elicited with the chest in full inspiration while percussing.
It occurs in conditions e.g.–
- Pneumothorax
- Emphysema
- Large Cavities
- Congenital Lung Cyst
- Emphysematous Bullae
- Eventration of diaphragm
BELL TYMPANY:
Generally, This a high pitch tympanic sound heard over the chest wall in cases of massive pneumothorax. In detail, This sound heard by placing a silver coin on the affected side and percussion carried out with a second coin. Besides this, The ear or stethoscope may held over the opposite side of the chest to hear the emitted sound. At last, A clear bell-like sound resembling the sound of a ‘Hammer stroked on an anvil’ is heard.
KRONIG’S ISTHMUS:
Kronig’s Isthmus is a band of resonance approximating to about 5-7 cm. in width, which connects lung resonance of the anterior also posterior aspects of each side of the chest. Moreover, It is bounded medially by dullness of the neck muscles also laterally by the dullness of pectoral muscles. Absence of this sound on either side suggests pulmonary fibrosis as a consequence of TB. Lastly, Increased width of resonance is suggestive of emphysema.
LIVER AND CARDIAC DULLNESS:
Normal liver dullness is present in the right 5th intercostal space in the mid-clavicular line, 7th space in the anterior axillary line and 9th space in scapular line.
LIVER DULLNESS RAISED
Seen in i.e.
- Amoebic Liver Abscess
- Pyogenic Liver Abscess
- Diaphragmatic Paralysis
- Lower Lobe Collapse of lungs
LIVER DULLNESS LOWERED
Seen in i.e.
- Emphysema
- Right-sided Pneumothorax
- Terminal Cirrhosis
- Air in the Peritoneal Cavity
Cardiac dullness felt on the left side of the lung field due to the presence of the heart. Furthermore, It felt normally in the 3rd and 4th parasternal line and 5th left mid-clavicular line.
CARDIAC DULLNESS INCREASED
Seen in i.e.:
- Cardiomegaly
- Shift of heart to the left
CARDIAC DULLNESS DECREASED
Seen in i.e.:
- Emphysema
- Left-sided Pneumothorax
TIDAL PERCUSSION:
Percussion done of the upper border of the liver with dullness on the right side anteriorly on inspiration and expiration helps to determine the range of lung expansion.
It restricted in conditions e.g.–
- Pulmonary disease at the base of the lung
- Pulmonary Fibrosis
- Empyema
- Hepatic Amoebiasis
- Sub-diaphragmatic abscess
TRAUBE’S AREA:
This area bound above by lung resonance, below by costal margins, on the right by the left border of liver and on the left by spleen. Moreover, It normally occupy by stomach and the note developed is tympanic. All in all, Dull note in Traube’s area suggests pleural effusion on the left side.
SHIFTING DULLNESS:
In patients with hydropneumothorax in sitting position, there is a hype resonant note felt above followed by a note of dullness felt below. On changing the patient’s posture to supine, this area of dullness of the fluid changes as air and fluid levels shift.
AUSCULTATION IN RESPIRATORY SYSTEM EXAMINATION
BREATH SOUNDS:
Normal breath sounds are vesicular, bronchial and Broncho-vesicular.
VESICULAR:
These sounds are soft and low pitched, heard through inspiration, continue without pause through expiration, fading about one third of the way through expiration. It is typically rustling due to the passage through alveoli which selectively transmit sounds of lower frequency and dampen the higher frequency sounds. It is normally heard over the chest.
BRONCHIAL:
These sounds are louder and higher in pitch, with a short silence between inspiratory and expiratory sounds. Expiratory sounds last longer than inspiratory sounds. In this type, both higher and lower frequency sounds are conducted as alveolar phase is absent. They may be normally heard over the manubrium if at all heard.
There are 3 types of bronchial breath sounds i.e.–
FIRSTLY, TYPE : TUBULAR
High pitched bronchial sound
Seen in Consolidations, above the level of pleura and above the cavities
SECONDLY, TYPE : CAVERNOUS
Low pitched bronchial sound
Seen in Irregular cavity
THIRDLY, TYPE : AMPHORIC
Low pitched bronchial sound with high pitched over tones
Seen in Smooth walled cavity, open pneumothorax
BRONCHO-VESCICULAR:
These sounds are with inspiratory and expiratory sounds about equal in length, at times separated by a silent interval. It is normally heard over the 1st and 2nd interspaces anteriorly and between the scapulae. It may be heard as an abnormal component in cases of i.e.–
- Asthma
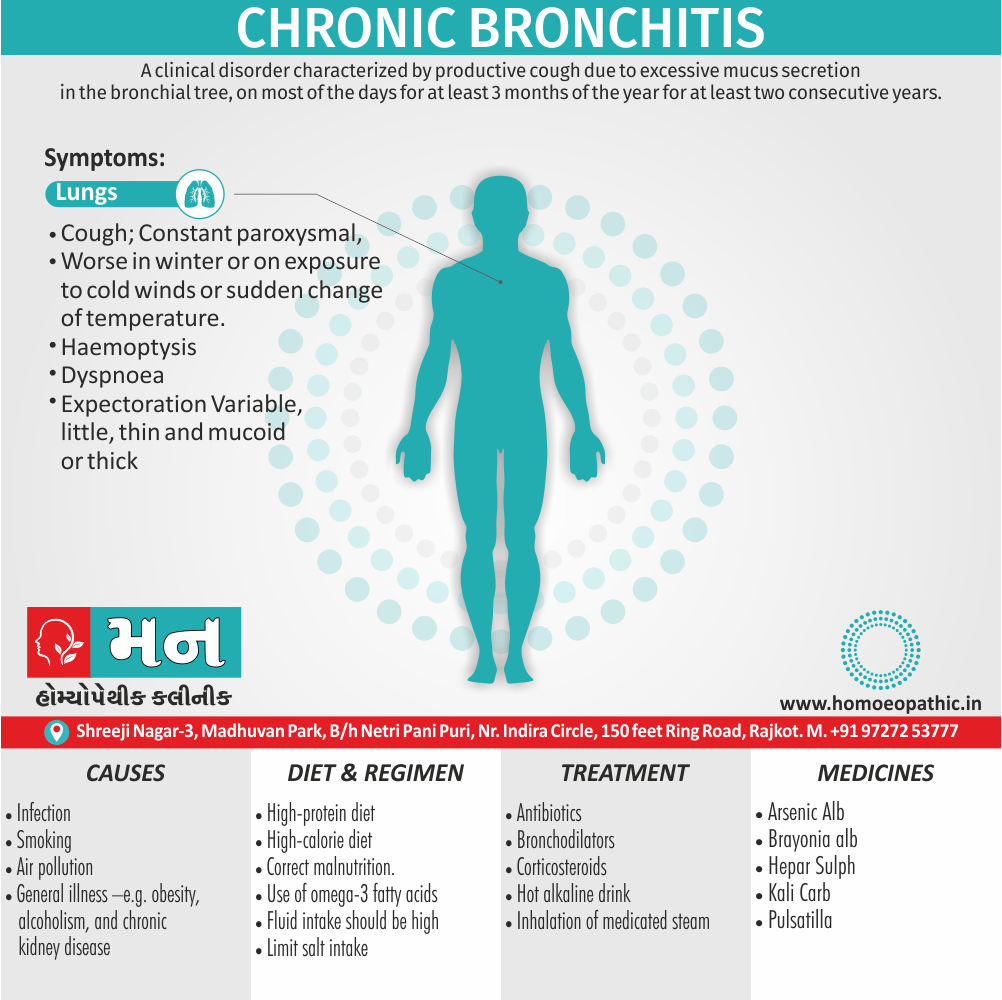
- Chronic Bronchitis
- Emphysema
ABNORMAL/ FOREIGN SOUNDS:
RALES (IN OTHER WORDS, CRACKLES):
They are crackling sounds originating in the smaller airways and alveoli as a result of an explosive opening of the airways (especially, during inspiration) in that particular part of the lung that is deflated (specifically, during expiration). Crackles result from air bubbles flowing through secretions or lightly closed airways during respiration.
Types of Rales:
EARLY INSPIRATORY
Result from openings of large airways being closed by air-trapping mechanism during the previous expiration, appear soon after inspiration, also are often coarse and few in number.
Seen in Chronic bronchitis
MID-INSPIRATORY
Seen in Bronchiectasis
LATE INSPIRATORY
May begin in the first half of inspiration but must continue into late inspiration. They are usually fine and fairly profuse.
Seen in Interstitial lung disease (e.g. fibrosis), early congestive heart failure.
EXPIRATORY
Associated with severe airway obstruction.
Seen in Chronic bronchitis and Asthma
RHONCHI (WHEEZE):
They occur when air flows rapidly through bronchi that are narrowed to an extent of closure.
Causes of wheezes that are generalized throughout the chest include –
- Bronchial Asthma
- Chronic Bronchitis
- COPD
- Congestive heart failure (in other words; Cardiac Asthma)
- Malignancy
In asthma, during respiratory system examination wheezes may be heard only in expiration or in both phases of the respiratory cycle. In severe COPD, the patient is no longer able to force enough air through the narrowed bronchi to produce wheezing. A persistent localized wheeze suggests a partial obstruction of a bronchus, as by a tumor or foreign body. It may be inspiratory, expiratory, or both.
Types of Rhonchi:
- Firstly, Polyphonic – This type of rhonchi consists of expiratory sound containing several notes of different pitch. It results from simultaneous oscillatory movement of several large bronchi.
- Secondly, Monophonic – It a sound emit from a single airway which constricted. It seen in conditions like chronic bronchitis and emphysema.
STRIDOR:
Stidor a loud inspiratory sound heard over the airways due to obstruction of the respiratory tract.
- Laryngeal Stridor – It a high pitched sound audible over the larynx due to the obstruction of larynx by a foreign body or diphtheria. It regarded as a medical emergency.
- Tracheal Stridor – It a low pitched sound heard over the trachea due to tracheal obstruction.
VOCAL RESONANCE:
Vocal resonance is the resonance in the chest occurring due to the sounds made by the voice as a result of laryngeal vibrations. While testing vocal resonance, you are detecting vibrations transmitted to the chest from the vocal cords as the patient repeats a phrase, usually the words ‘ninety-nine’.
Vocal Resonance may increased or altered as follows:
TYPE : WHISPERING PECTORILOQUY
Resonance increase and the sounds heard louder and clearer in a consolidate lung more than an air-filled lung. Thus, even when the patient whispers a phrase the sounds may be heard clearly.
Seen in Lung Consolidation
TYPE : AEGOPHONY
Nasal or bleating character of voice when auscultated.
Seen in Pleural effusion (above its level), Lung consolidation.
TYPE : BRONCHOPHONY
Increased vocal resonance wherein the sounds heard loud and clear but the words spoken are indistinguishable.
Seen in Lung consolidation
TYPE : SUCCUSSION SPLASH
Splashing sound audible over the chest wall by a stethoscope or an unaided ear, when the patient shaken suddenly by the examiner.
Seen in Hydropneumothorax, large cavity containing fluid and air or herniation of stomach or colon into the thorax.
TYPE : POST-TUSSIVE SUCTION
Suction sound heard over the chest wall during the long inspiratory spell that follows a bout of cough.
Seen in Thin walled compressible lung cavity communicating with the bronchus.
TYPE : POST-TUSSIVE RALES
Rales are not audible during normal respiration but are audible after making the patient cough. They suggest cavity fill with thick material which dislodged during coughing allowing the air to bubble out through the remaining fluid, thus producing the rales.
Seen in Lung cavity filled with fluid (most commonly lung abscess).
Frequently Asked Questions
What is Examination Of The Respiratory System?
Examination Of The Respiratory System carry out with a simultaneous general assessment. For the examination the patient should be resting comfortably on a bed or couch, supported by pillows so that they can lean back comfortably at an angle of 45 °.
Give the name of methods of Examination Of The Respiratory System?
- Observation
- Inspection
- Palpation
- Percussion
- Auscultation
What should be inspected in Examination Of The Respiratory System?
- Shape of the chest
- Movement of the chest
- Respiratory Rhythm
- Type of breathing
What is percussion in Examination Of The Respiratory System?
In Respiratory System examination percussion helps you to access whether the underlying tissues air-filled, fluid-filled, or solid.