Paralysis
Definition
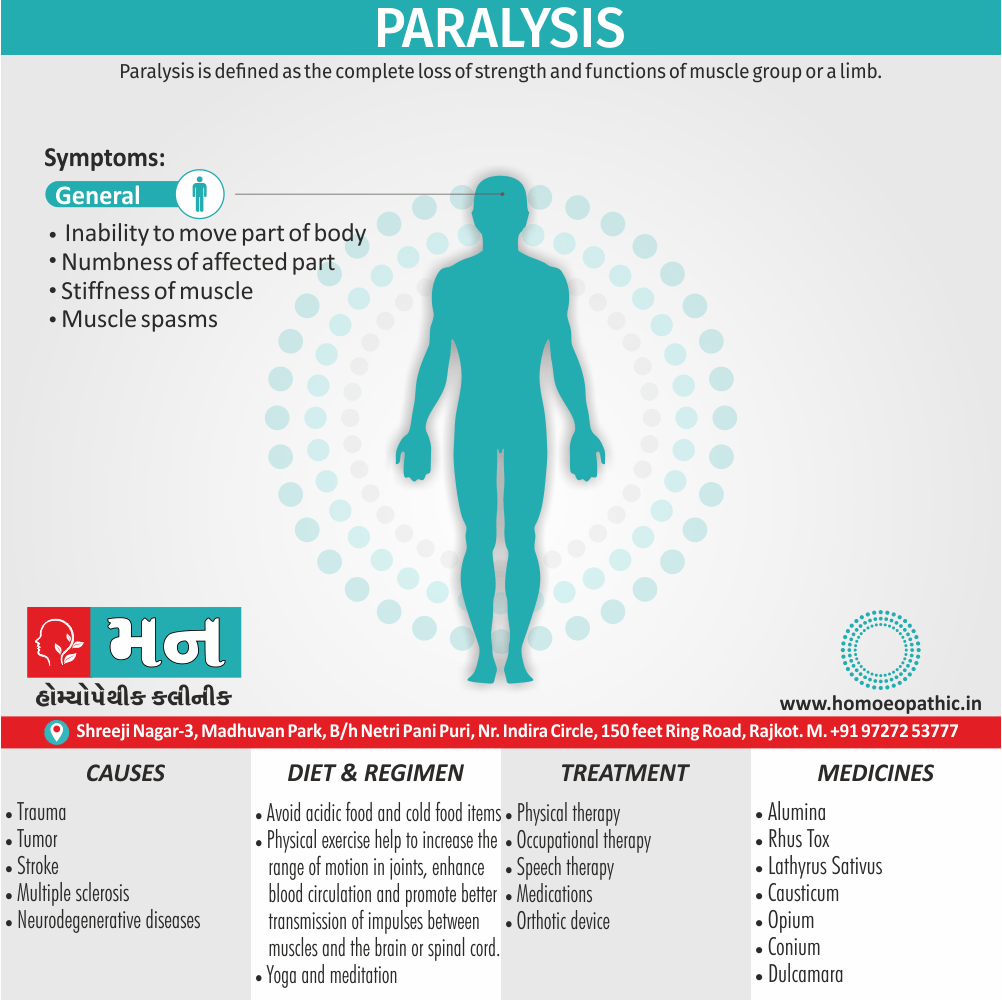
Paralysis is defined as the complete loss of strength and functions of muscle group or a limb. [1]
The best synonym for paralysis depends on the specific aspect you want to emphasize. Here are some options:
General loss of movement:
- Disability
- Impairment
- Immobility
- Immobilization
- Weakness
Medical terms for paralysis:
- Palsy (an older term for paralysis)
- Paresis (partial paralysis)
- Hemiplegia (paralysis affecting one side of the body)
- Paraplegia (paralysis affecting both legs and sometimes the torso)
- Quadriplegia (tetraplegia) – paralysis affecting all four limbs
Remember, some of these terms have a more negative connotation than others. Choose the one that best fits your context.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
Paralysis is the loss of muscle function, ranging from temporary to permanent and partial to complete.
It can impact any body part. Paralysis significantly impacts physical, emotional, and social well-being. However, with support and treatment, individuals can lead fulfilling lives.
Causes:
Nervous System Damage: Most commonly due to:
- Stroke
- Spinal Cord Injury
- Traumatic Brain Injury
- Multiple Sclerosis
- Cerebral Palsy
- Nerve Disorders (e.g., Guillain-Barré syndrome)
- Infections (e.g., polio, meningitis)
- Tumors
Types:
- Monoplegia: One limb affected
- Hemiplegia: One side of the body affected
- Paraplegia: Lower body, including both legs, affected
- Quadriplegia: All four limbs affected
Symptoms:
- Loss of muscle function and movement
- Numbness, tingling
- Muscle stiffness or spasms
- Loss of sensation
- Difficulty breathing/swallowing (if relevant muscles are affected)
Epidemiology
Epidemiology
The epidemiology of paralysis in India is complex and multifaceted, reflecting the country’s diverse population and varied health challenges. While significant progress has been made in reducing the incidence of polio-related paralysis, non-polio acute flaccid paralysis (NPAFP) remains a significant concern.
Key references on the epidemiology of paralysis in India include:
Trends in Nonpolio Acute Flaccid Paralysis Incidence in India 2000 to 2013 (Pediatrics, 2014) – This study highlights the increasing trend of NPAFP in India, even as polio cases decline. It underscores the need for further research into the causes and risk factors of NPAFP to develop effective prevention and control strategies. [5]
- Acute flaccid paralysis surveillance in India – A road ahead (ResearchGate, 2015) – This paper discusses the challenges and opportunities in AFP surveillance in India. It emphasizes the importance of strengthening surveillance systems to accurately track the burden of NPAFP and identify emerging trends. [6]
Key points on the epidemiology of paralysis in India:
- Polio: India achieved polio-free status in 2014, a remarkable feat attributed to widespread vaccination efforts. However, continued vigilance is crucial to prevent the re-emergence of poliovirus.
- NPAFP: The incidence of NPAFP has increased in recent years, surpassing the expected rate. The causes of NPAFP are diverse and include Guillain-Barré syndrome, enteroviruses, and other infectious and non-infectious conditions.
- Regional variations: The burden of paralysis varies across different regions of India, influenced by factors such as socioeconomic conditions, access to healthcare, and environmental factors.
- Challenges: The accurate diagnosis and surveillance of NPAFP pose challenges due to limited laboratory capacity and the need for improved clinical awareness.
Causes
Causes
Common causes are i.e.
- Trauma
- Tumor
- Stroke
- Cerebral palsy (condition caused by brain injury immediately after birth)
- Multiple sclerosis
- Neurodegenerative diseases.[1]
Types
Types/ Classification
- Partial – Only some muscle groups do not work.
- Complete – the whole body is immobile.
- Temporary – The condition is either medically induced or affected by neurotoxins by biting of venomous snakes or the sting of jellyfish.
- Permanent – Paralysis as an irreversible condition is usually caused especially by the damage of the nerve cells in the brain or spinal cord.
- Flaccid – In this condition, the muscles become flaccid also shrink.
- Spastic – In this condition, the muscles show erratic movements like jerking. These conditions are not totally inter-related; but, they can be used for understanding the severity of the condition.
Depending on the affected regions in the body
- Monoplegia – Affecting only one limb;
- Hemiplegia – Affecting only one side of the body;
- Diplegia – Affecting the same area of both sides of the body like only both arms or both legs;
- Paraplegia – Affecting both legs,
- Quadriplegia – Sometimes also called tetraplegia, it affects both arms and legs, and, in some cases, the whole torso is affected, while the inner organs are unaffected.
Secondary Condition
- Paralysis may lead to other medical conditions; if there is no proper assistance provided, and then a bed-ridden patient may develop bedsores which can even lead to severe infection in the body.
- Besides, due to complete loss of tactile sensation (sensation of the touch), the patient may not realize any skin or muscle-related problem like infection, itching, burning, etc. until it is too late.
- Some patients who are completely immobile for years also show signs like fragility and fracturing of the bones.
- Therefore, the secondary conditions are more life-threatening to the affected persons than paralysis itself. [2]
Risk Factors
Risk Factors
- Age: The risk of paralysis generally increases with age, particularly for conditions like stroke and neurodegenerative diseases.
- Underlying Medical Conditions: Certain medical conditions significantly elevate the risk of paralysis, including:
- Stroke
- Spinal Cord Injury
- Traumatic Brain Injury
- Multiple Sclerosis
- Cerebral Palsy
- Guillain-Barré Syndrome
- Polio
- Brain Tumors
- Spinal Tumors
- Infections (e.g., meningitis, encephalitis)
- Lifestyle Factors: Unhealthy lifestyle choices can contribute to conditions that increase the risk of paralysis:
Other Factors
- Smoking
- Excessive Alcohol Consumption
- Physical Inactivity
- Unhealthy Diet
- Genetic Predisposition: Some individuals may have a genetic predisposition to certain conditions that can lead to paralysis.
- Environmental Factors: Exposure to certain toxins or pollutants may increase the risk of neurological damage and paralysis. [7]
Pathogenesis
Pathogenesis of Paralysis
The pathogenesis of paralysis, or the mechanisms by which it develops, is intricate and can vary widely depending on the underlying cause. However, the fundamental principle revolves around the disruption of communication between the nervous system and the muscles. This disruption can occur at different levels:
Upper Motor Neuron Lesions:
- Damage to the brain or spinal cord, particularly the motor cortex or the descending motor pathways, leads to upper motor neuron lesions.
- This results in:
- Spasticity: Increased muscle tone and stiffness due to loss of inhibitory control.
- Hyperreflexia: Exaggerated reflexes.
- Weakness or paralysis: Loss of voluntary muscle control.
Lower Motor Neuron Lesions:
- Damage to the spinal cord’s anterior horn cells, nerve roots, or peripheral nerves causes lower motor neuron lesions.
- This manifests as:
- Flaccid paralysis: Decreased or absent muscle tone and reflexes.
- Muscle atrophy: Wasting of muscles due to lack of nerve stimulation.
- Fasciculations: Involuntary muscle twitches.
Neuromuscular Junction Disorders:
- Diseases affecting the neuromuscular junction, like myasthenia gravis, disrupt the transmission of nerve signals to muscles, leading to fluctuating muscle weakness and fatigue.
Muscle Diseases:
- Inherited or acquired muscle diseases (e.g., muscular dystrophies) directly affect muscle fibers, leading to progressive weakness and paralysis. [8]
Pathophysiology
Pathophysiology
The pathophysiology of paralysis, or the mechanisms by which it develops, is intricate and can vary widely depending on the underlying cause. However, the fundamental principle revolves around the disruption of communication between the nervous system and the muscles. This disruption can occur at different levels:
Upper Motor Neuron Lesions:
- Damage to the brain or spinal cord, particularly the motor cortex or the descending motor pathways, leads to upper motor neuron lesions.
- This results in:
- Spasticity: Increased muscle tone and stiffness due to loss of inhibitory control.
- Hyperreflexia: Exaggerated reflexes.
- Weakness or paralysis: Loss of voluntary muscle control.
- Positive Babinski sign: An abnormal reflex response indicating upper motor neuron dysfunction.
Lower Motor Neuron Lesions:
- Damage to the spinal cord’s anterior horn cells, nerve roots, or peripheral nerves causes lower motor neuron lesions.
- This manifests as:
- Flaccid paralysis: Decreased or absent muscle tone and reflexes.
- Muscle atrophy: Wasting of muscles due to lack of nerve stimulation.
- Fasciculations: Involuntary muscle twitches.
Neuromuscular Junction Disorders:
- Diseases affecting the neuromuscular junction, like myasthenia gravis, disrupt the transmission of nerve signals to muscles, leading to fluctuating muscle weakness and fatigue.
Muscle Diseases:
- Inherited or acquired muscle diseases (e.g., muscular dystrophies) directly affect muscle fibers, leading to progressive weakness and paralysis. [8]
Clinical Features
Clinical Features of Paralysis
The clinical presentation of paralysis can vary significantly depending on the underlying cause, location, and extent of the neurological damage. However, the core features revolve around the loss or impairment of motor function, often accompanied by sensory and autonomic disturbances.
Motor Features:
- Loss of Voluntary Movement: The hallmark of paralysis is the inability to initiate or control movement in the affected body part(s). This can range from mild weakness (paresis) to complete paralysis (plegia).
- Muscle Tone Abnormalities:
- Spasticity: Increased muscle tone and stiffness, often associated with upper motor neuron lesions.
- Flaccidity: Decreased or absent muscle tone, typically seen with lower motor neuron lesions.
Reflex Changes:
- Hyperreflexia: Exaggerated reflexes, characteristic of upper motor neuron lesions.
- Hyporeflexia or Areflexia: Diminished or absent reflexes, associated with lower motor neuron lesions.
- Muscle Atrophy: Wasting of muscles due to lack of nerve stimulation or disuse, commonly observed in chronic paralysis.
- Fasciculations: Involuntary muscle twitches, sometimes seen with lower motor neuron lesions.
Sensory Features:
- Numbness: Loss or decreased sensation in the affected area, often accompanied by tingling or pins-and-needles sensations.
- Pain: May be present due to nerve damage, muscle spasms, or secondary complications.
- Loss of Proprioception: Impaired sense of joint position and movement.
Autonomic Features:
- Bladder and Bowel Dysfunction: Difficulty with urination or defecation, ranging from incontinence to retention.
- Sexual Dysfunction: Erectile dysfunction or decreased libido may occur.
- Cardiovascular Instability: Orthostatic hypotension (drop in blood pressure upon standing) or autonomic dysreflexia (sudden increase in blood pressure) may be present in cases of spinal cord injury.
Additional Features:
- Respiratory Difficulties: May occur with paralysis affecting the diaphragm or chest muscles.
- Speech and Swallowing Impairments: May be present with paralysis involving the muscles controlling speech or swallowing.
- Emotional and Psychological Effects: Depression, anxiety, and adjustment difficulties are common in individuals with paralysis. [9]
Sign & Symptoms
Sign & Symptoms
- The main symptom is the inability to move part of body, or not being able to move at all.
- It can start suddenly or gradually.
- Sometimes it comes and goes.
- It can affect any part of the body, including:
- Face
- Hands
- One arm or leg (monoplegia)
- One side of the body (hemiplegia)
- Both legs (paraplegia)
- Both arms and legs (tetraplegia or quadriplegia)
The affected part of your body may also be:
Clinical Examination
Clinical Examination of Paralysis
A comprehensive clinical examination is crucial to assess the extent and nature of paralysis, identify the underlying cause, and guide management. The examination typically involves a detailed history and physical examination, with a focus on the neurological system.
History:
- Onset and Progression: The timing and pattern of paralysis onset (sudden vs. gradual), progression (stable vs. worsening), and any associated symptoms (pain, sensory changes, bowel/bladder dysfunction) are vital clues.
- Medical and Family History: Past medical conditions, surgeries, medications, family history of neurological disorders, and recent illnesses or injuries can help identify potential causes.
- Social and Occupational History: Exposure to toxins, recent travel, and occupational hazards may offer clues about potential environmental or infectious causes.
Physical Examination:
- Mental Status: Assessing cognitive function, language, and mood can reveal associated brain involvement.
- Cranial Nerves: Evaluating cranial nerve function (eye movements, facial sensation, tongue movement, etc.) helps localize lesions in the brainstem or cranial nerves.
- Motor System:
- Inspection: Observing muscle bulk, symmetry, and any involuntary movements (fasciculations, tremors).
- Tone: Assessing muscle tone (spasticity vs. flaccidity) helps differentiate between upper and lower motor neuron lesions.
- Power: Testing muscle strength in various muscle groups using a standardized scale (e.g., Medical Research Council scale) helps quantify the degree of weakness.
- Reflexes: Examining deep tendon reflexes (e.g., knee jerk, biceps reflex) and superficial reflexes (e.g., plantar response) aids in localizing lesions.
- Sensory System: Assessing pain, temperature, light touch, vibration, and proprioception in various dermatomes helps identify sensory deficits and their distribution.
- Coordination and Gait: Evaluating coordination (finger-nose test, heel-shin test) and observing gait patterns can reveal cerebellar or motor pathway dysfunction.
- Other Systems: Depending on the suspected cause, additional examinations (e.g., cardiovascular, respiratory, gastrointestinal) may be necessary. [9]
Diagnosis
Diagnosis of Paralysis
The diagnosis of paralysis involves a systematic approach that integrates a detailed clinical history, a comprehensive neurological examination, and appropriate investigations to identify the underlying cause.
Clinical History:
- A thorough history helps elucidate the onset, progression, and associated symptoms of paralysis, providing crucial clues for diagnosis.
- Key aspects to explore include:
- Timing and pattern of paralysis onset (sudden vs. gradual)
- Progression of symptoms (stable vs. worsening)
- Associated symptoms (pain, sensory changes, bowel/bladder dysfunction)
- Past medical history (trauma, surgeries, medications)
- Family history of neurological disorders
- Recent illnesses or exposures
Neurological Examination:
- A meticulous neurological examination helps localize the lesion responsible for paralysis and assess its extent.
- Key components include:
- Mental status assessment
- Cranial nerve examination
- Motor system evaluation (muscle tone, power, reflexes)
- Sensory system assessment
- Coordination and gait analysis
Investigations:
- The choice of investigations depends on the suspected cause of paralysis.
- Common investigations include:
- Imaging studies (MRI, CT scan, X-ray)
- Electrophysiological tests (electromyography, nerve conduction studies)
- Blood tests (complete blood count, inflammatory markers, autoimmune antibodies)
- Lumbar puncture (cerebrospinal fluid analysis)
- Genetic testing [10]
Differential Diagnosis
Differential Diagnosis of Paralysis
The differential diagnosis for paralysis is extensive, as numerous conditions can lead to loss or impairment of motor function. A systematic approach is crucial to identify the underlying cause accurately. Here’s a breakdown of some common considerations:
Central Nervous System Disorders:
- Stroke: Ischemic or hemorrhagic stroke can cause sudden-onset paralysis, often affecting one side of the body (hemiplegia).
- Spinal Cord Injury: Trauma, tumors, or infections affecting the spinal cord can lead to paralysis below the level of injury, with varying degrees of sensory and autonomic dysfunction.
- Brain Tumors: Tumors compressing or infiltrating the motor cortex or descending pathways can cause progressive weakness or paralysis.
- Multiple Sclerosis: This autoimmune disease affecting the central nervous system can cause various neurological symptoms, including weakness, numbness, and paralysis.
- Cerebral Palsy: This group of disorders affecting movement and posture, often arising from brain injury during early development, can cause varying degrees of paralysis.
Peripheral Nervous System Disorders:
- Guillain-Barré Syndrome: This autoimmune disorder affecting peripheral nerves can cause rapidly progressive weakness and paralysis, often starting in the legs and ascending.
- Chronic Inflammatory Demyelinating Polyneuropathy (CIDP): This chronic inflammatory disorder of peripheral nerves can cause slowly progressive weakness and sensory loss.
- Diabetic Neuropathy: Nerve damage due to diabetes can lead to numbness, tingling, and weakness, particularly in the feet and hands.
- Radiculopathy: Compression or irritation of nerve roots (e.g., herniated disc) can cause pain, weakness, and numbness in the corresponding dermatome.
- Peripheral Nerve Injuries: Trauma or compression of peripheral nerves can cause weakness or paralysis in the affected muscles.
Neuromuscular Junction Disorders:
- Myasthenia Gravis: This autoimmune disorder affects the neuromuscular junction, causing fluctuating muscle weakness and fatigue.
- Lambert-Eaton Myasthenic Syndrome: This rare autoimmune disorder also affects the neuromuscular junction, causing muscle weakness that often improves with exercise.
- Botulism: This rare but serious illness caused by a bacterial toxin can cause muscle weakness and paralysis.
Muscle Diseases:
- Muscular Dystrophies: This group of inherited disorders causes progressive muscle weakness and wasting.
- Myopathies: Various acquired muscle diseases (e.g., inflammatory myopathies, metabolic myopathies) can cause muscle weakness and fatigue. [8]
Complications
Complications of Paralysis
Paralysis can lead to a wide range of complications that significantly impact physical and mental well-being.
These complications can be broadly categorized into physical, psychological, and social aspects.
Physical Complications:
Musculoskeletal:
- Muscle atrophy and contractures (shortening and tightening of muscles) due to disuse
- Joint deformities and stiffness
- Osteoporosis (bone loss) due to reduced weight-bearing and mobility.
Respiratory:
Cardiovascular:
- Deep vein thrombosis (blood clots) and pulmonary embolism due to immobility
- Orthostatic hypotension (drop in blood pressure upon standing)
- Autonomic dysreflexia (sudden increase in blood pressure) in cases of spinal cord injury
Skin:
- Pressure ulcers (bedsores) due to prolonged pressure on skin areas
- Skin infections
Gastrointestinal:
- Constipation due to immobility and decreased bowel motility
- Fecal impaction
- Urinary tract infections due to bladder dysfunction and urinary retention
Psychological Complications:
- Depression: Feelings of sadness, hopelessness, and loss of interest, often associated with the significant life changes caused by paralysis.
- Anxiety: Excessive worry and fear about the future and potential complications.
- Adjustment Disorders: Difficulty coping with the emotional and practical challenges of paralysis.
- Post-traumatic Stress Disorder (PTSD): In cases where paralysis results from trauma, individuals may experience flashbacks, nightmares, and emotional distress.
Social Complications:
- Social isolation: Withdrawal from social activities and relationships due to physical limitations or emotional distress.
- Reduced employment opportunities: Difficulty finding or maintaining employment due to physical limitations and potential discrimination.
- Financial difficulties: Increased healthcare costs and potential loss of income can lead to financial strain.
- Relationship challenges: Paralysis can impact intimate relationships and family dynamics. [11]
Investigations
Investigation
- X-ray
- CT Scan
- Myelography
- MRI
- Spinal tap
- Electromyography (EMG) [2]
Treatment
Treatment
Physical Therapy
- Physical therapy focuses on improving mobility through targeted exercise.
- If paralysis is mild and patient is not able to move the affected regions on his own, he should continue to actively practice movement.
- If his paralysis is complete and he does not have any control over his movements, then have a therapist or trained caregiver move his body. This is called passive movement.
- Although he is not actively performing the movement, the movement itself will continue to stimulate the central nervous system.
- Consistent and repetitive stimulation of the brain and spinal cord help reinforce demand for those functions and promotes neuroplasticity.
- The more you practice, the greater your chances of recovery.
Occupational Therapy
- Occupational therapy helps you develop the skills necessary to perform self-care tasks, return to school or work, and minimize the risk of secondary complications.
- It involves practicing activities of daily living such as grooming or eating to provide practical, real-world training.
- An occupational therapist can also recommend effective ways to compensate for limited movement and develop your functional independence.
- For example, they may teach you how to use adaptive tools to help you perform everyday activities you may otherwise not be able to on your own.
Speech Therapy
- Speech therapy helps individuals with facial paralysis strengthen their oral motor muscles.
- Paralysis of these muscles can significantly impair an individual’s ability to speak, breathe, chew, and swallow.
- By practicing speech therapy exercises and activities, individuals can improve their feeding and communication skills.
- Individuals with more severe facial paralysis may be taught how to utilize augmentative and alternative communication (AAC) devices such as voice generators to communicate with others.
Mobility Aids
- Due to paralysis, individuals may struggle to walk, stand, and sit upright.
- To compensate for limited mobility, therapists may recommend mobility aids such as wheelchairs, crutches, walkers, and canes.
- They’ll help you move around, stay balanced, and minimize the risk of falling.
Orthotic Devices
- If left unmanaged, spastic muscles can progressively tighten and further restrict your range of motion.
- Orthotic devices such as braces and splints help provide structural support and resist against abnormal muscle tone.
- By holding your affected limbs in place, they passively stretch muscles with high tone (spasticity) and help reduce your risk of injury.
Medications
- Often, secondary complications of paralysis such as pain, high muscle tone, and depression can interfere with one’s motivation to pursue rehabilitation.
- Medications may be prescribed to help treat secondary complications.
- If you believe secondary effects of paralysis are impacting your mental health, speak to your doctor about medications that may help.
- Individuals who experience high muscle tone may have very limited range of motion due to severely contracted muscles.
- To allow you to participate more actively in physical therapy, nerve blockers like Botox injections or muscle relaxants like baclofen may be recommended to temporarily relieve high muscle tone.
Psychotherapy
- Individuals who develop mental health disorders such as depression or anxiety and those who are struggling to adapt to life with paralysis may benefit from psychotherapy.
- This treatment involves identifying what is causing your negative thoughts and behaviors and practicing more effective ways to cope.
- Because each individual experiences paralysis differently, paralysis treatment will vary from person to person.
- What works for one person may not be as effective for another.
- Therefore, taking a personalized approach to paralysis treatment is ideal.[3]
Prevention
Prevention of Paralysis
Preventing paralysis involves a multi-pronged approach targeting various risk factors and underlying causes. While complete prevention may not always be possible, adopting healthy lifestyle choices and managing underlying medical conditions can significantly reduce the risk.
Lifestyle Modifications:
- Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins provides essential nutrients for nerve and muscle health.
- Regular Exercise: Engaging in regular physical activity helps maintain cardiovascular health, strengthens muscles, and improves overall well-being, reducing the risk of stroke and other conditions that can lead to paralysis.
- No Smoking: Smoking damages blood vessels and increases the risk of stroke and other vascular diseases. Quitting smoking significantly reduces the risk of paralysis.
- Moderate Alcohol Consumption: Excessive alcohol consumption can lead to nerve damage and increase the risk of accidents and injuries.
- Fall Prevention: Taking precautions to prevent falls, especially in older adults, can reduce the risk of traumatic brain injury and spinal cord injury.
Medical Management:
- Control Blood Pressure and Cholesterol: Managing high blood pressure and cholesterol levels reduces the risk of stroke.
- Manage Diabetes: Keeping blood sugar levels under control can help prevent diabetic neuropathy and other complications.
- Treat Infections Promptly: Prompt treatment of infections, especially those affecting the nervous system (e.g., meningitis, encephalitis), can prevent neurological damage and paralysis.
- Vaccinations: Vaccinations against polio and other infectious diseases can prevent paralysis caused by these illnesses.
- Injury Prevention: Using safety measures like seatbelts, helmets, and protective gear during sports and activities can reduce the risk of traumatic brain injury and spinal cord injury. [12]
Homeopathic Treatment
Homeopathic Treatment of Paralysis
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Paralysis
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
Rhus Tox:
- Generally, Paralysis of the lower extremities and proved it to exceedingly useful.
- It specifically corresponds to all forms of paralysis which are of a rheumatic origin or brought on by exposure to dampness or by getting wet.
- Paralysis is caused by nervous fever also typhus accompanied by a dragging gait and much stiffness in the limbs from damp cold.
- Lastly, Paralysis of muscles of the eyes and face.[4]
Gelsemium:
- Complete motor paralysis which rather functional than organic in origin.
- Paralysis from emotions Paralysis of either ocular or laryngeal muscles, the speech is thick from paretic condition of the tongue.
- Weakness in the lower body, heaviness, completes relaxation also lack of muscular coordination.
- It is one of the best remedies specifically for post-diphtheric and infantile paralysis.
Causticum:
- Especially adapted to paralysis of single parts of the body and facial paralysis from exposure to dry cold weather including.
- paralysis of the right side of the face, tongue, pharynx etc.
- Useful for vocal paralysis associated with weakness of vocal cords, and paralysis of muscles of deglutition of the tongue, eyelids, face, bladder and extremities.[4]
Lathyrus Sativus:
- It is adapted to spastic paralysis, infantile paralysis and paralysis which affects the lower extremities associated with heaviness,
- Much weakness and slow process recovery of nerve power.
- Rheumatic paralysis is also there.
- Tendency for excessive rigidity of the legs; also the patient is unable to extend or cross legs while sitting.
- The patient can easily sir or bend forwards, but straightens up with much difficulty.[4]
Dulcamara
- Worse from cold damp weather, or by sudden changes from hot to cold weather;
- Paralysis of tongue with impaired speech; paresis and Hyperaemia of spinal cord from lying on damp cold weather;
- Palsy of bladder from the same cause; urine offensive loaded with mucus.[4]
Conium:
- Paralysis caused due to suppressed sexual desire in widows, widowers and bachelors; gradually progressing, ascending paralysis, ending in death by failure of respiration;
- Painless paralytic conditions; paralytic weakness of hips and legs resulting in difficult gait,
- Trembling and loss of strength while walking;
- Weakness of muscles of face, upper lids etc.
- Paralytic conditions are attended with numbness;
- Vertigo when turning the eyes, when lying down or when looking at moving object.[4]
Opium:
- One side of the body paralyzed due to cerebral apoplexy;
- Great spoor, painless and patient complaints of nothing and wants nothing.
- Lying in deep sleep with stertorous breathing, jaw dropped, and face red, eyes half closed, skin covered with hot sweat; pupils usually contracted but may be dilated.
- Insensibility and partial or complete paralysis from fright or bad effects of fear still remaining.
- Mental and physical sluggishness.
- Paralysis of the bowels and rectum causing constipation with black, hard, round balls or involuntary stools due to paralysis of sphincter ani.
- Paralysis of bladder causing retention of urine with full bladder.[4]
Arnica:
- Paralysis due to concussion, cerebrovascular accident especially cerebral thrombosis.
- in case of hemiplegia due to cerebral thrombosis in case of hypertension arnica is the first medicine to be used.
- It helps by controlling haemorrhages and aids absorption.
- other symptoms are sore bruised feeling; everything on which patient lies seems hard. Involuntary faeces and urine due to paralysis of sphincters after injury.
- Mainly left sided paralysis, pulse full and strong, singing and muttering.[4]
Plumbum met:
- Paralysis of single muscles; it generally begins in the extensors.
- Wrist drop is prominent.
- Patient is unable to lift anything with the hand.[4]
Diet & Regimen
Diet & Regimen
- Avoid acidic food also cold food items
- Furthermore, Physical exercise help to increase the range of motion in joints, enhance blood circulation and promote better transmission of impulses between muscles and the brain or spinal cord.
- Lastly, Yoga and meditation.[3]
Do’s and Don'ts
The Do’s & Don’ts
Do’s:
- Seek medical attention immediately: At the first signs of paralysis or weakness, seek immediate medical attention. Early diagnosis and treatment can be crucial in managing the underlying cause and preventing further complications.
- Follow the prescribed treatment plan: Adhere to the medications, therapies, and lifestyle recommendations provided by your healthcare team. Consistency is key to managing the condition and maximizing recovery potential.
- Maintain a healthy lifestyle: Eat a balanced diet rich in fruits, vegetables, and whole grains. Engage in regular physical activity as advised by your healthcare team. Avoid smoking and excessive alcohol consumption.
- Practice good skin care: Regularly inspect your skin for any signs of pressure sores or breakdown. Keep your skin clean and dry, and use pressure-relieving devices as recommended.
- Manage bowel and bladder function: Follow a bowel and bladder program as advised by your healthcare team. This may include dietary changes, medications, or catheterization.
- Stay socially connected: Engage in social activities and maintain relationships with friends and family. Social support is essential for emotional well-being and coping with the challenges of paralysis.
- Seek emotional support: If you’re struggling with the emotional impact of paralysis, don’t hesitate to seek help from a therapist or counselor.
- Explore assistive devices and technologies: Utilize assistive devices (wheelchairs, walkers, etc.) and adaptive technologies (voice-activated devices, smart home systems) to enhance independence and quality of life.
- Join support groups: Connect with other individuals with paralysis through support groups or online communities. Sharing experiences and receiving support can be invaluable.
- Stay informed: Educate yourself about paralysis, its management, and available resources. Knowledge empowers you to make informed decisions about your health and well-being.
Context-Specific Considerations for India:
- Accessibility: Advocate for improved accessibility in public spaces, transportation, and healthcare facilities.
- Affordable healthcare: Explore government schemes and non-profit organizations offering affordable healthcare and rehabilitation services.
- Community support: Leverage community resources and support networks to access care and overcome social barriers.
Don’ts:
- Don’t ignore symptoms: Delaying medical attention can worsen outcomes.
- Don’t neglect skin care: Pressure sores can lead to serious infections.
- Don’t isolate yourself: Social connection is essential for emotional health.
- Don’t give up: Focus on your abilities and strive for progress, no matter how small.
- Don’t hesitate to ask for help: Reach out to family, friends, or healthcare professionals when you need assistance.
Terminology
Terminology
Paralysis: The complete loss of muscle function in one or more parts of the body.
Paresis: Partial or incomplete paralysis, characterized by muscle weakness.
Plegia: Suffix indicating paralysis; often combined with prefixes to specify the affected body part. For example:
Spasticity: Increased muscle tone and stiffness, often associated with upper motor neuron lesions.
Flaccidity: Decreased or absent muscle tone, typically seen with lower motor neuron lesions.
Upper Motor Neuron (UMN) Lesion: Damage to the brain or spinal cord, leading to spasticity, hyperreflexia, and weakness.
Lower Motor Neuron (LMN) Lesion: Damage to the spinal cord’s anterior horn cells, nerve roots, or peripheral nerves, leading to flaccidity, muscle atrophy, and fasciculations.
Neuropathy: Damage or dysfunction of one or more nerves, often causing numbness, tingling, weakness, or pain.
Myopathy: Disease of the muscle tissue, leading to muscle weakness and wasting.
Rehabilitation: The process of helping individuals with paralysis regain function and independence through physical therapy, occupational therapy, and other interventions.
Assistive Devices: Tools and technologies that help individuals with paralysis perform daily activities, such as wheelchairs, walkers, and communication devices.
Spinal Cord Injury (SCI): Damage to the spinal cord resulting in varying degrees of paralysis and sensory loss below the level of injury.
Stroke: A sudden interruption of blood flow to the brain, often causing paralysis on one side of the body.
Traumatic Brain Injury (TBI): Injury to the brain caused by an external force, potentially leading to paralysis and other neurological impairments.
Multiple Sclerosis (MS): A chronic autoimmune disease affecting the central nervous system, causing a wide range of symptoms, including paralysis.
Homoeopathy
- Causticum: Often recommended for paralysis following exposure to cold or injuries, with symptoms like muscle weakness, stiffness, and difficulty swallowing.
- Gelsemium: Suggested for paralysis associated with emotional stress, fear, or anxiety, presenting with trembling, weakness, and heavy eyelids.
- Nux Vomica: Considered for paralysis related to digestive issues or overexertion, with symptoms like muscle spasms, constipation, and irritability.
- Rhus Toxicodendron: Often used for paralysis caused by dampness or overexertion, with stiffness, pain, and restlessness.
References
References used for Article
- K. Sembuligam Textbook of Medical Physiology
- www.vedantu.com/biology/paralysis
- www.nhs.uk/conditions/paralysis
- Homoeopathic Therapeutics by Lilienthal
- Trends in Nonpolio Acute Flaccid Paralysis Incidence in India 2000 to 2013 (Pediatrics, 2014)
- Acute flaccid paralysis surveillance in India – A road ahead (ResearchGate, 2015)
- Neurological Rehabilitation (6th Edition), by Darcy Umphred (2012, Elsevier Health Sciences)
- Adams and Victor’s Principles of Neurology (11th Edition) by Allan H. Ropper, Martin A. Samuels, Joshua P. Klein, Sashank Prasad (2019, McGraw-Hill Education / Medical)
- DeJong’s The Neurologic Examination (8th edition), by William W. Campbell, (2019, Wolters Kluwer)
- Bradley’s Neurology in Clinical Practice (7th Edition), by Robert B. Daroff, Joseph Jankovic, Scott L. Pomeroy, Michael J. Aminoff, (2016, Elsevier)
- Textbook of Physical Medicine and Rehabilitation, 4th Edition, by Randall L. Braddom, (2015, Elsevier)
- Stroke Prevention, Treatment, and Rehabilitation, 4th Edition, by Louis R. Caplan, José Biller, Marc Fisher,(2016, Cambridge University Press)
Also Search As
Also Search As
People can search for homeopathic articles on paralysis through various channels:
Online Search Engines:
- Use specific keywords: Try searching for "homeopathy for paralysis," "homeopathic remedies for paralysis," or "homeopathic treatment for paralysis" on popular search engines like Google, DuckDuckGo, or Bing.
- Include additional terms: To narrow down your search, include specific types of paralysis (e.g., "homeopathy for facial paralysis" or "homeopathy for post-stroke paralysis").
- Specify the source: You can also include phrases like "homeopathic journal articles on paralysis" or "homeopathic research on paralysis" to find scholarly publications.
Homeopathic Websites and Databases:
- Visit reputable homeopathic organizations’ websites: Many homeopathic organizations have resources and articles available on their websites. Some well-known organizations include:
- The National Center for Homeopathy (NCH)
- The Homeopathic Research Institute (HRI)
- The British Homeopathic Association (BHA)
- Search homeopathic databases: Several online databases specialize in homeopathic literature. One example is HomBRex, which allows you to search for articles based on keywords and remedies.
Homeopathic Libraries and Bookstores:
- Visit a local homeopathic library: If you have access to a homeopathic library, you can browse their collection or ask a librarian for assistance.
- Check homeopathic bookstores: Homeopathic bookstores often carry books and journals on various topics, including paralysis.
Here are some common approaches:
Online Search Engines:
- General Search: Use broad keywords like "paralysis," "causes of paralysis," or "treatment for paralysis" on popular search engines (Google, Bing, DuckDuckGo). This will yield a wide range of results, including general information, news articles, and medical websites.
- Specific Searches: To narrow down your search, include more specific terms. For instance, you could search for "paralysis after stroke," "spinal cord injury paralysis," or "facial paralysis treatment."
- Scholarly Articles: If you’re looking for in-depth research and medical literature, try using Google Scholar or PubMed. You can use similar keywords or search for specific medical terms like "hemiplegia" or "quadriplegia."
Medical Websites and Databases:
- Reputable Health Organizations: Visit the websites of well-known health organizations like the World Health Organization (WHO), the Mayo Clinic, or the National Institutes of Health (NIH). They often provide reliable information on various health conditions, including paralysis.
- Specialized Organizations: There are organizations dedicated to specific types of paralysis or neurological conditions (e.g., the Christopher & Dana Reeve Foundation for spinal cord injury). Their websites offer valuable resources and information.
Libraries and Bookstores:
- Medical Libraries: If you have access to a medical library, you can find textbooks, journals, and other resources on paralysis. Librarians can assist you in finding relevant materials.
- Bookstores: Look for books on neurology, rehabilitation, or specific conditions related to paralysis.
Consult Healthcare Professionals:
- Doctors: Your primary care physician or a neurologist can provide personalized information and guidance on paralysis, including diagnosis, treatment options, and preventive measures.
- Therapists: Physical therapists, occupational therapists, and speech therapists can offer valuable insights on rehabilitation and managing daily life with paralysis.
Support Groups and Online Communities:
- Connect with Others: Joining support groups or online communities for people with paralysis or their families can provide emotional support and practical advice.These platforms can also be a source of information and resources.
Frequently Asked Questions (FAQ)
What is Paralysis?
Definition
Paralysis is defined as the complete loss of strength and functions of muscle group or a limb.
Can paralysis be cured?
The potential for recovery from paralysis depends on the underlying cause and severity. Some individuals may experience complete recovery, while others may have permanent limitations.
Rehabilitation therapies play a crucial role in maximizing function and independence.
What are the types of Paralysis?
Types
- Partial
- Complete
- Temporary
- Permanent
- Flaccid
- Spastic
- Monoplegia
- Hemiplegia
- Diplegia
- Paraplegia
- Quadriplegia
Give the symptoms of Paralysis?
Symptoms
- Inability to move part of body, or not being able to move at all.
- It can start either suddenly or gradually.
- Sometimes it comes and goes.
- It can affect any part of the body, including:
- Face
- Hands
- Either One arm or leg
- One side of the body
- Both legs
- Both arms and legs
What is the main cause of Paralysis?
- Trauma
- Tumor
- Stroke
- Cerebral palsy
- Multiple sclerosis
- Neurodegenerative diseases
Can homeopathy help with paralysis?
Homeopathy proponents suggest that certain remedies may stimulate the body’s healing response and potentially improve nerve function and muscle control in cases of paralysis. However, it’s crucial to remember that scientific evidence supporting homeopathy’s effectiveness in treating paralysis is limited.
Should I consult a homeopath for paralysis?
If you’re interested in exploring homeopathy as a complementary therapy for paralysis, consulting a qualified homeopathic practitioner is recommended. They can assess your individual needs and suggest appropriate remedies. However, it’s crucial to continue conventional medical treatment for paralysis alongside any homeopathic interventions.
Is homeopathy a safe treatment option for paralysis?
Homeopathic remedies are generally considered safe when used as directed by a qualified homeopathic practitioner.
However, it’s crucial to inform your doctor about any homeopathic remedies you’re taking, especially if you are also undergoing conventional medical treatment for paralysis.
