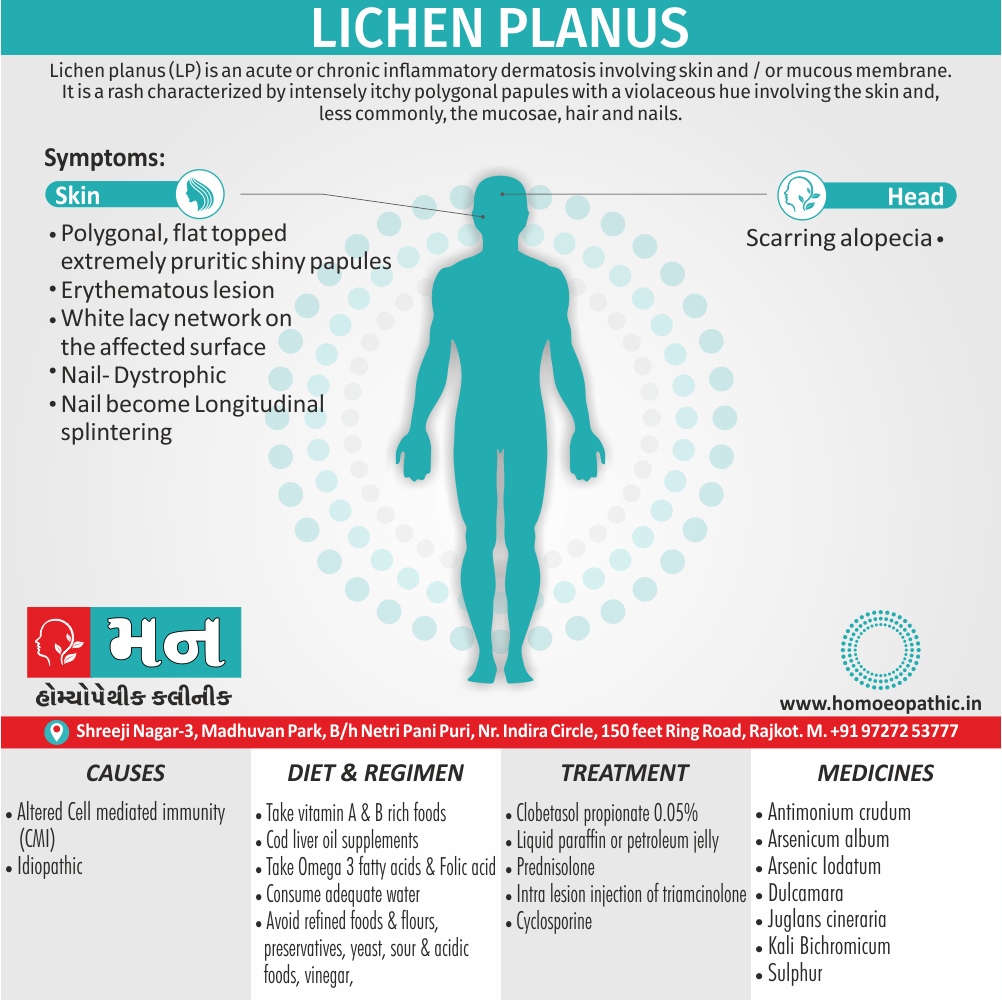
Definition:
Lichen planus (LP) is an acute or chronic inflammatory dermatosis involving skin and / or mucous membrane. Additionally, It is a rash characterized by intensely itchy polygonal papules with a violaceous hue involving the skin and, less commonly, the mucosae, hair also nails.[1]
Overview
Epidemiology xxx
Causes
Types
Risk Factors xxx
Pathogenesis xxx
Pathophysiology
Clinical Features xxx
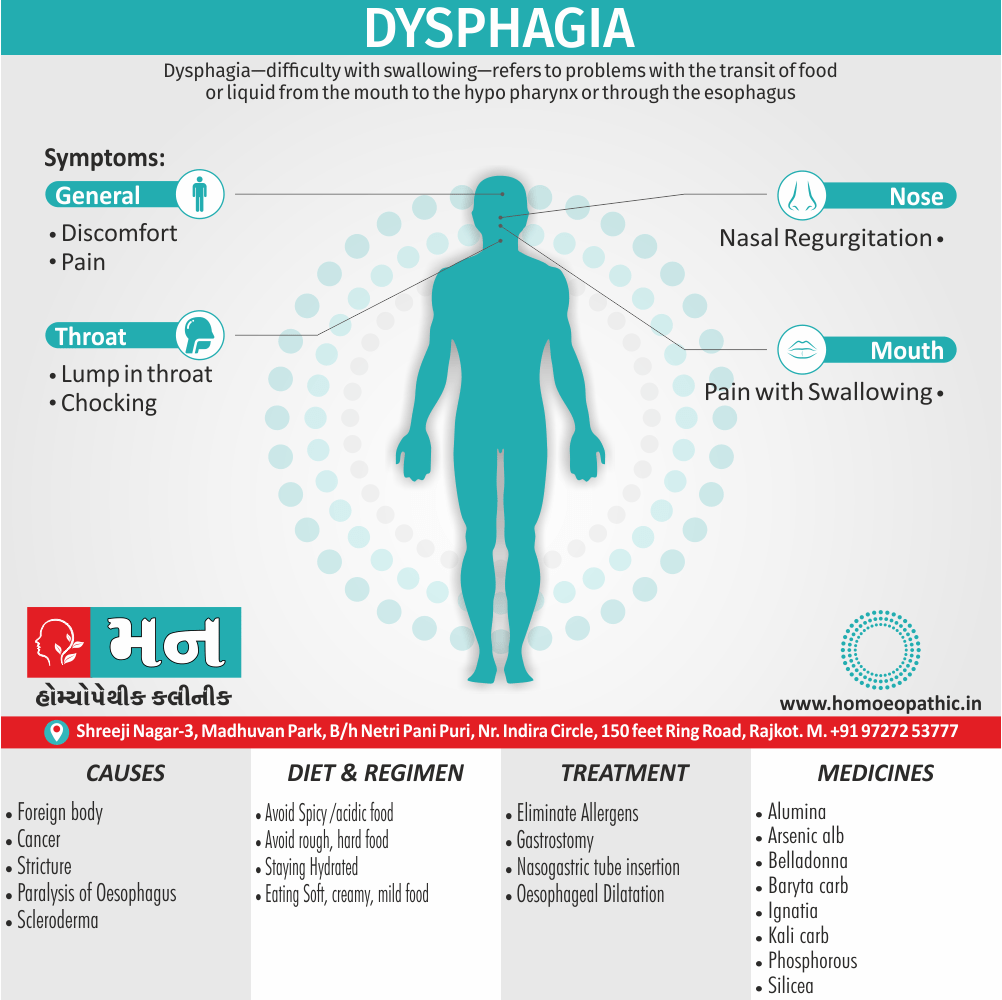
Sign & Symptoms
Clinical Examination xxx
Diagnosis
Differential Diagnosis
Complications xxx
Investigations xxx
Treatment
Prevention xxx
Homeopathic Treatment
Diet & Regimen
Do’s and Dont’s xxx
Terminology xxx
References
FAQ
Also Search As xxx
Overview
Overview of Lichen planus
In general, Lichen planus is a Autoimmune disorder. It is a recurrent, pruritic, inflammatory eruption characterized by small, discrete, polygonal, flat-topped, violaceous papules that may coalesce into rough scaly plaques, often accompanied by oral also genital lesions.
Moreover, Diagnosis is usually clinical and supported by skin biopsy. Besides this, Treatment generally requires topical or intralesional corticosteroids. Lastly, Severe cases may require phototherapy or systemic corticosteroids, retinoids, or immunosuppressants.[6]
Epidemiology xxx
Indian epidemiology then other
Causes
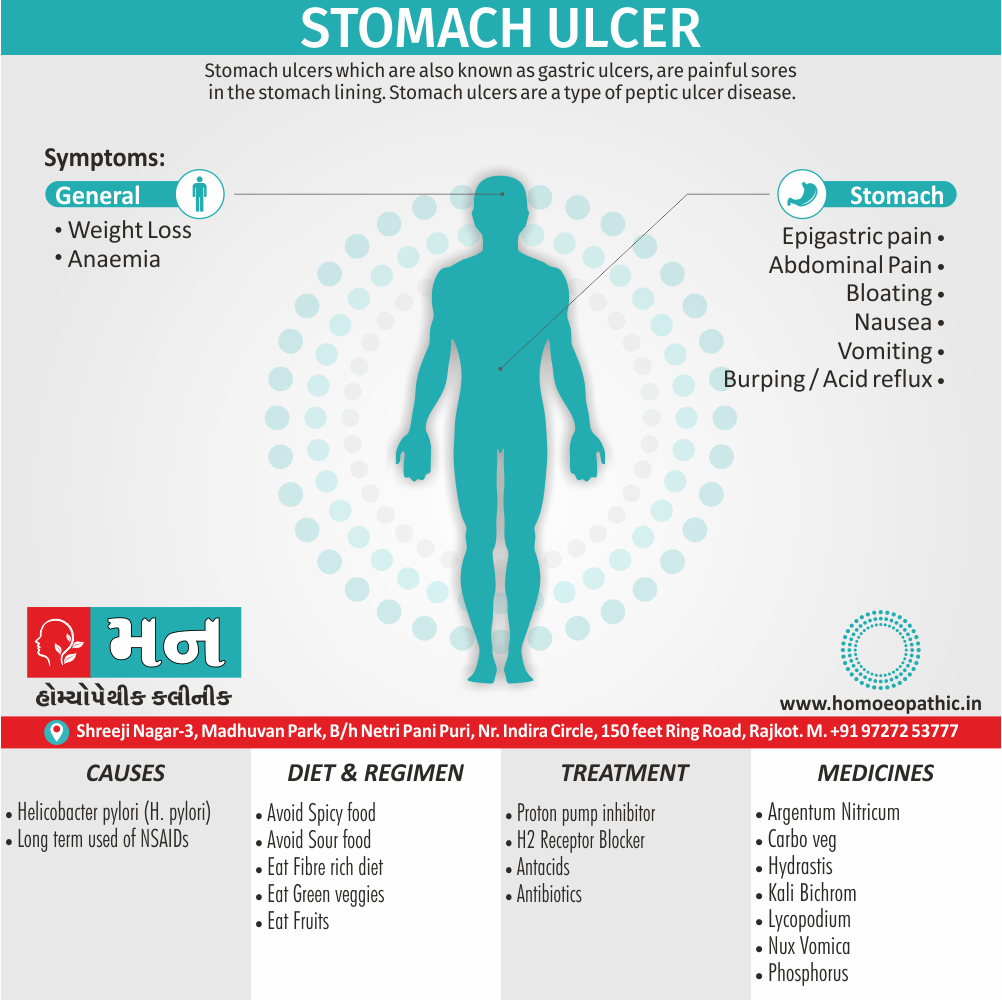
This refers to the initiating factors that trigger a disease
Causes of Lichen planus
- It is idiopathic in most cases.
- But it is evident that cell mediated immunity (in other words, CMI) plays a major role. Majority of the infiltrate contains CD 8+ and CD 45 RO+ memory cells.
- Drugs such as beta blockers, antimalarial, thiazides, gold also mercury salts and infection with hepatitis C virus result in altered cell mediated immunity. In detail, All these have been implicated as triggering factors for LP.[2]
Types
Classification of Lichen planus
- Hypertrophic lichen planus: – Presents as hyperkeratotic verrucous plaques especially on the lower parts of legs.
- Annular lesions: – It occur commonly on the glans penis.
- Linear violaceus papules of lichen planus: – It occur on the limbs also trunk .
- Follicular lesions: – It occur on the scalp.
- Graham Little syndrome: – It is the occurrence of follicular lesions also scarring alopecia of scalp with classical LP.
- Lichen planus actinicus: – the lesions are on the sites exposed to sunlight.
- Ulcerative lesions: – These are common on the soles also are resistant to therapy.[2]
Risk Factors xxx
Risk factors are things that make you more likely to develop a disease in the first place.
Pathogenesis xxx
Pathogenesis refers to the development of a disease. It’s the story of how a disease gets started and progresses.
This is the entire journey of a disease, encompassing the cause but going beyond it.
Pathophysiology
Pathophysiology of Lichen planus
- Pathology is quite characteristic.
- There is epidermal hyper keratosis, hyper granulosis, acanthosis, basal cell degeneration also a band like lymph histiocytic infiltrate in the upper dermis.[2]
Clinical Features xxx
Tab Content
Sign & Symptoms
Sign & Symptoms of Lichen planus
- Basically, The onset is usually insidious with the classical violaceous, polygonal, flat topped extremely pruritic shiny papules distributed symmetrically over the flexor aspect of forearms, wrists, lower parts of legs also genitalia.
- Furthermore, The initial lesions may be erythematous.
- Some lesions show a white lacy network (Wickham’s striae) on the surface.
- Koebner phenomenon (spread of lesions along the lines of trauma) is seen.
- In two thirds of cases, the buccal mucosa is involved.
- Sometimes scalp involvement leads to scarring alopecia.
- Nails become dystrophic with longitudinal splintering.[2]
Clinical Examination xxx
Tab Content
Diagnosis
Diagnosis of Lichen planus
A diagnosis of lichen planus based on your symptoms, your medical history, a physical examination and, if necessary, the results of lab tests. These tests may include i.e.:
- Biopsy: – Your doctor removes a small piece of affected tissue for examination under a microscope. Additionally, The tissue is analyzed to determine whether it has the cell patterns characteristic of lichen planus.
- Hepatitis C test: – You may have your blood drawn to test for hepatitis C, which is a possible trigger for lichen planus.
- Allergy tests: – Your doctor may refer you to an allergy specialist (in other words, allergist) or dermatologist to find out if you’re allergic to something that can trigger lichen planus.[3]
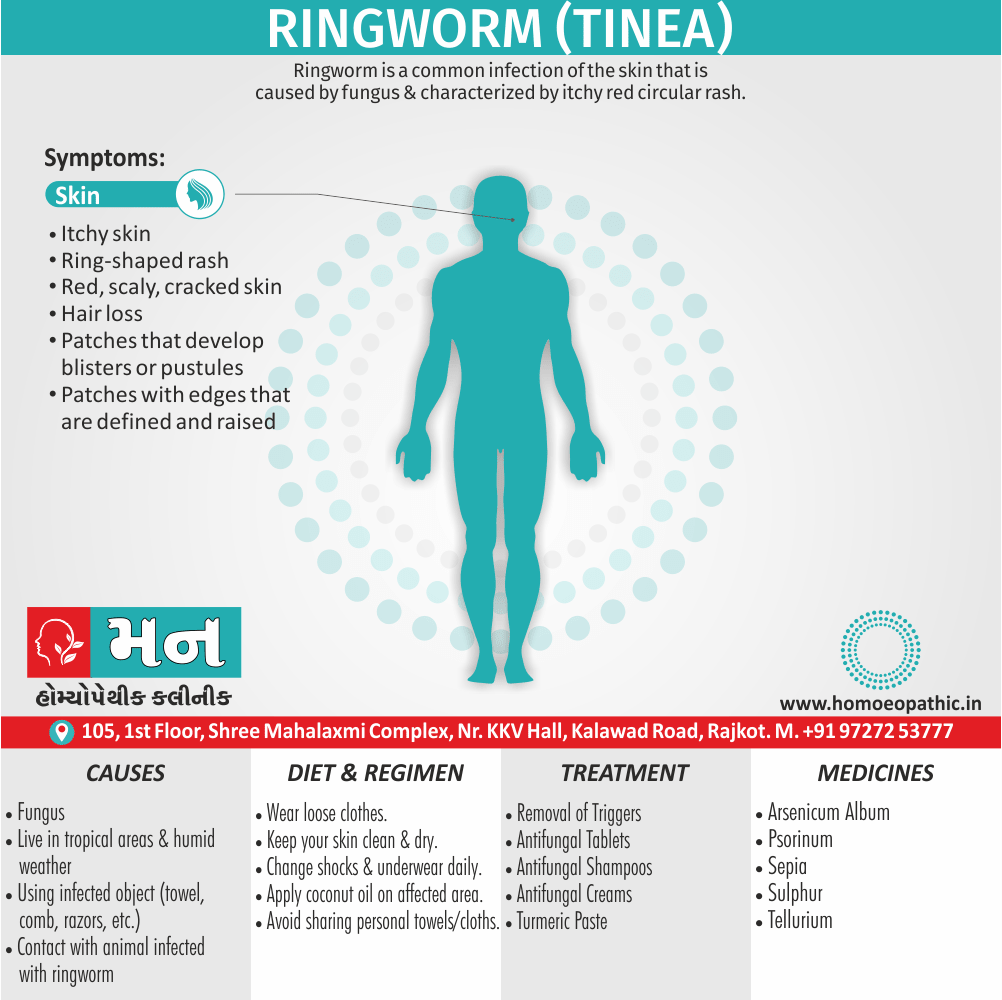
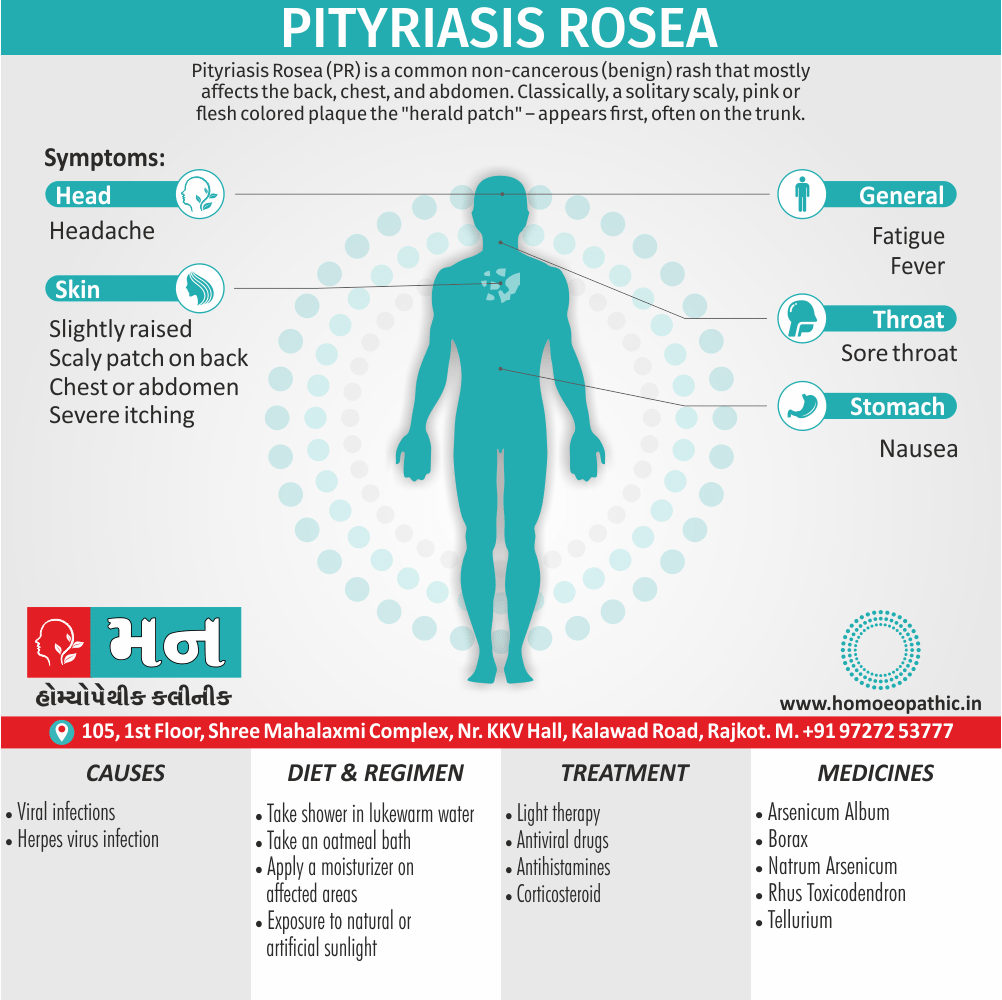
Differential Diagnosis
Differential Diagnosis of Lichen planus
- Lichen Nitidus
- Lichen Simplex Chronicus
- Pediatric Syphilis
- Pityriasis Rosea
- Plaque Psoriasis
- Tinea Corporis [9]
Complications xxx
Complications are what happen after you have a disease. They are the negative consequences of the disease process.
Investigations xxx
Tab Content
Treatment
Treatment of Lichen planus
- Classic LP can be treated with potent topical steroids such as Clobetasol propionate 0.05% twice daily for 2-3 weeks.
- Either Liquid paraffin or petroleum jelly should be applied 4-5 times daily.
- In acute generalized LP, oral corticosteroids such as Prednisolone 30-40 mg/day tapered over 1-3 months halt the rapid progression.
- Intra lesion injection of 0.1 ml of triamcinolone (10 mg/ml) is effective in hypertrophic LP.
- Cyclosporine in a dose of 3-5 mg/ kg orally for chronic LP induces long lasting remission.[2]
Prevention xxx
Tab Content
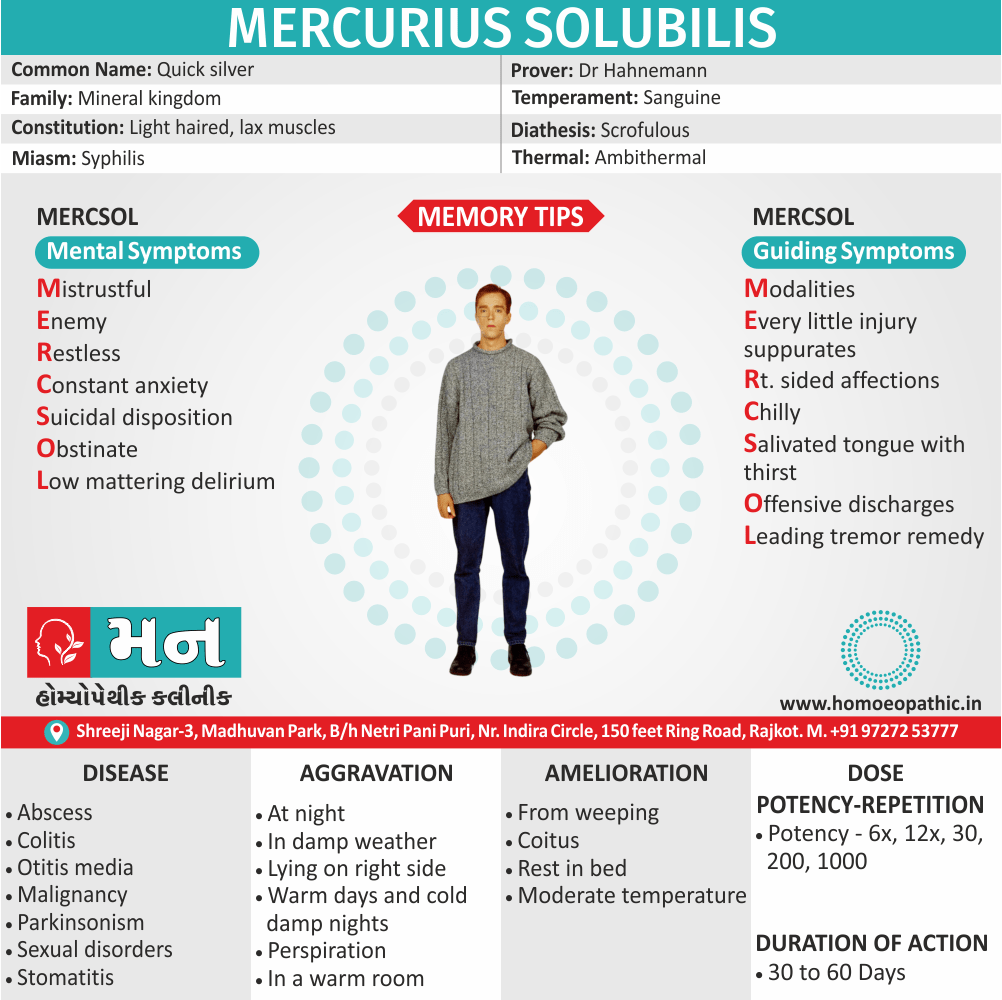
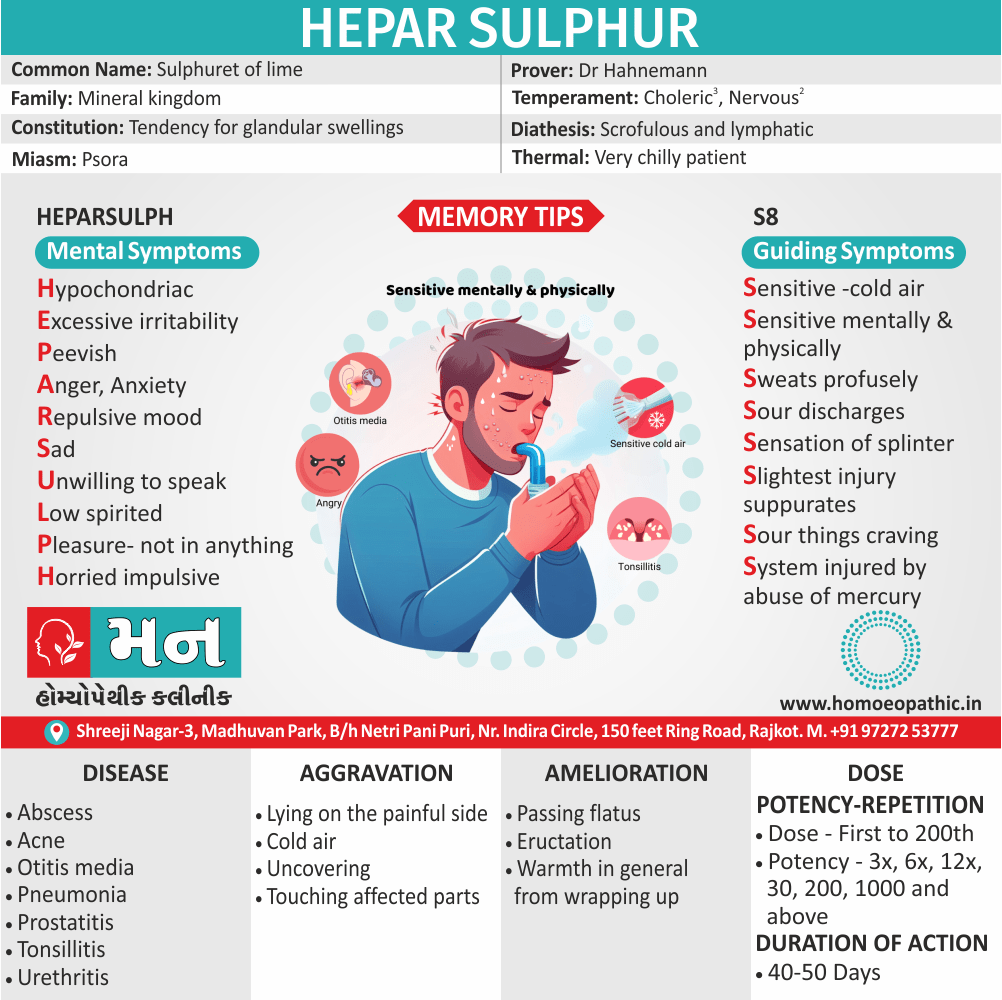
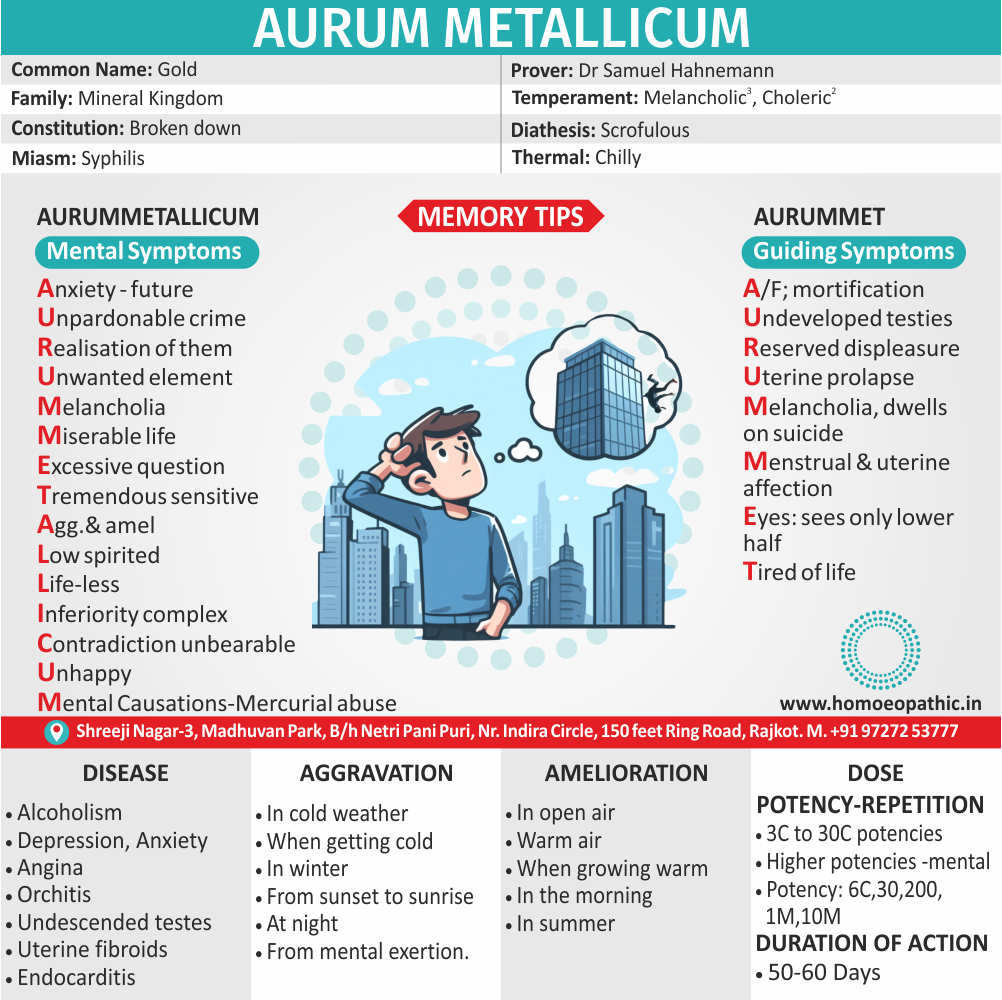
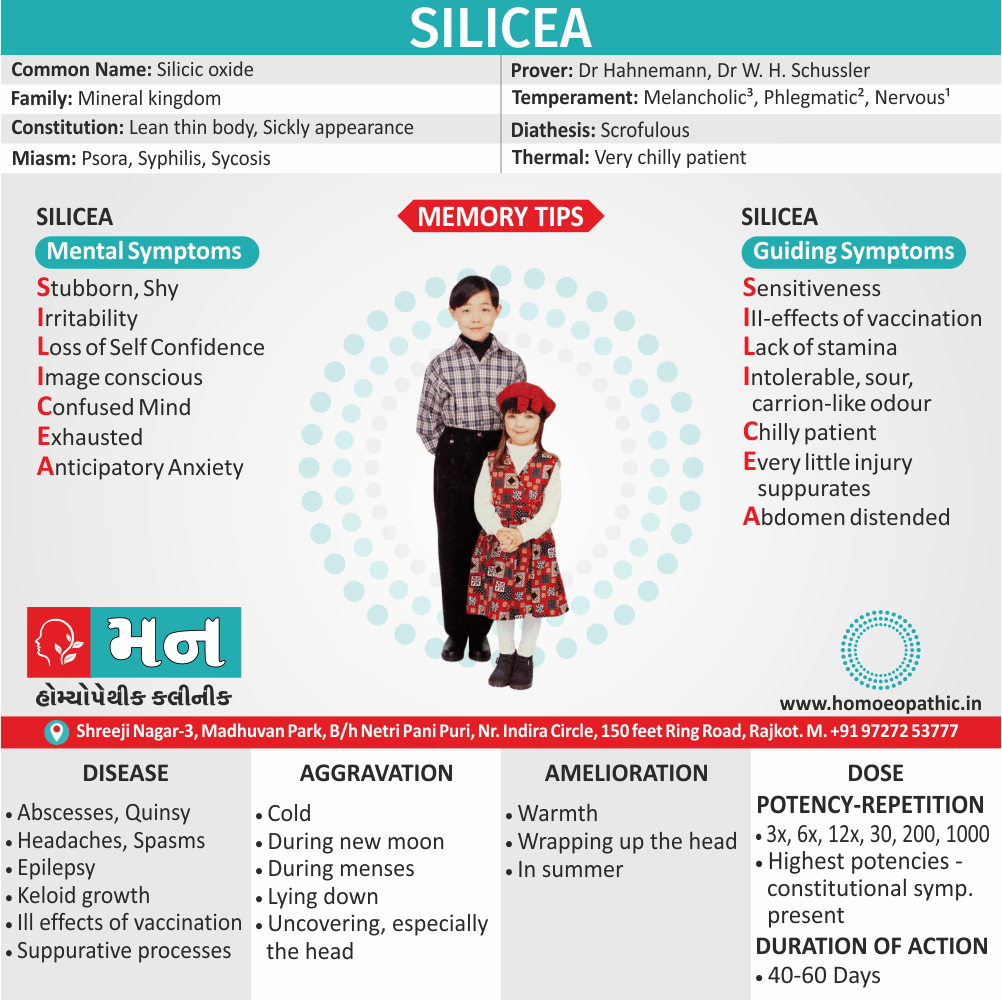
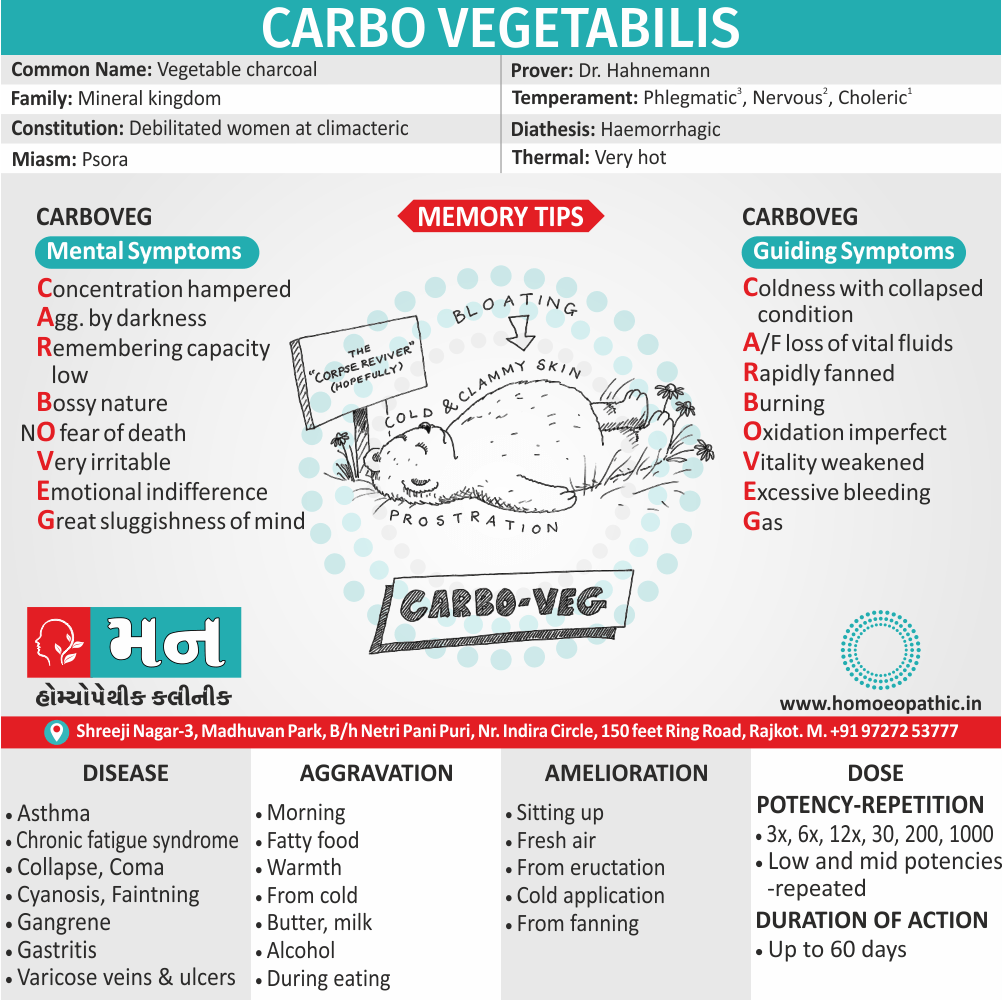
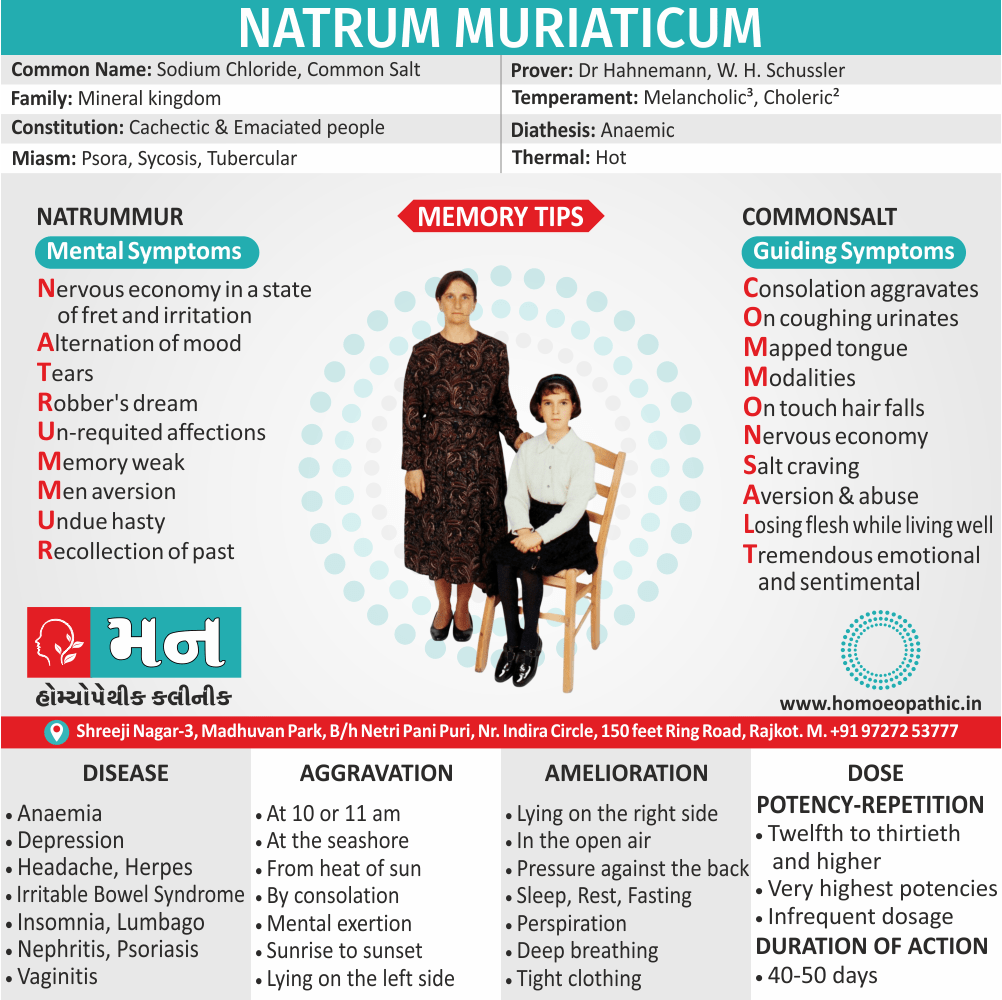
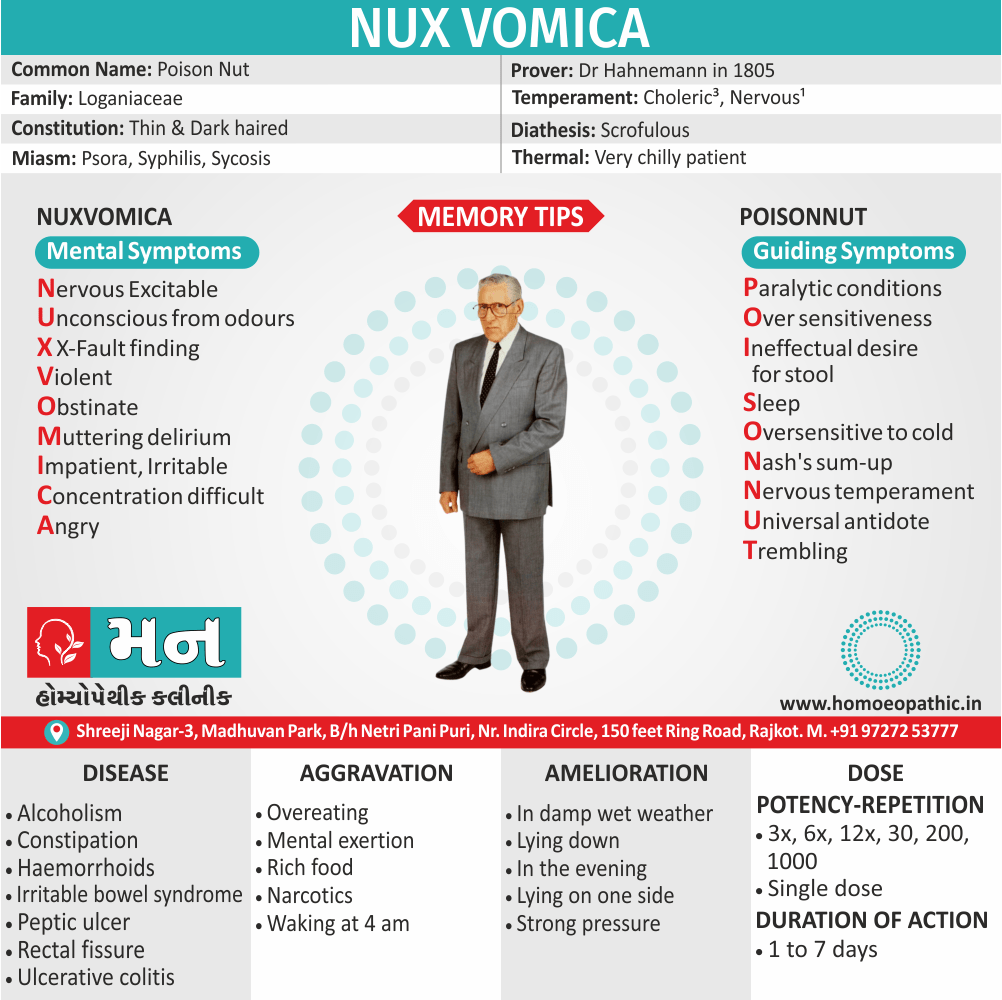
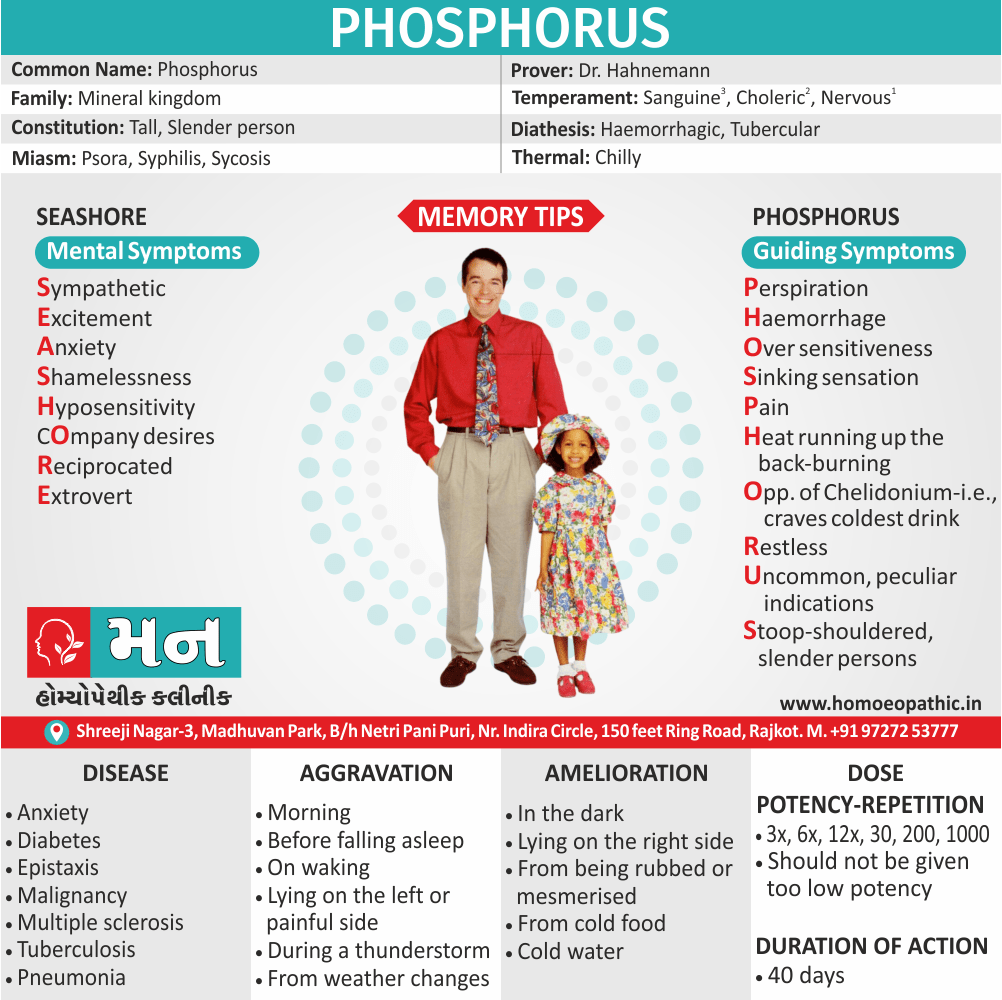
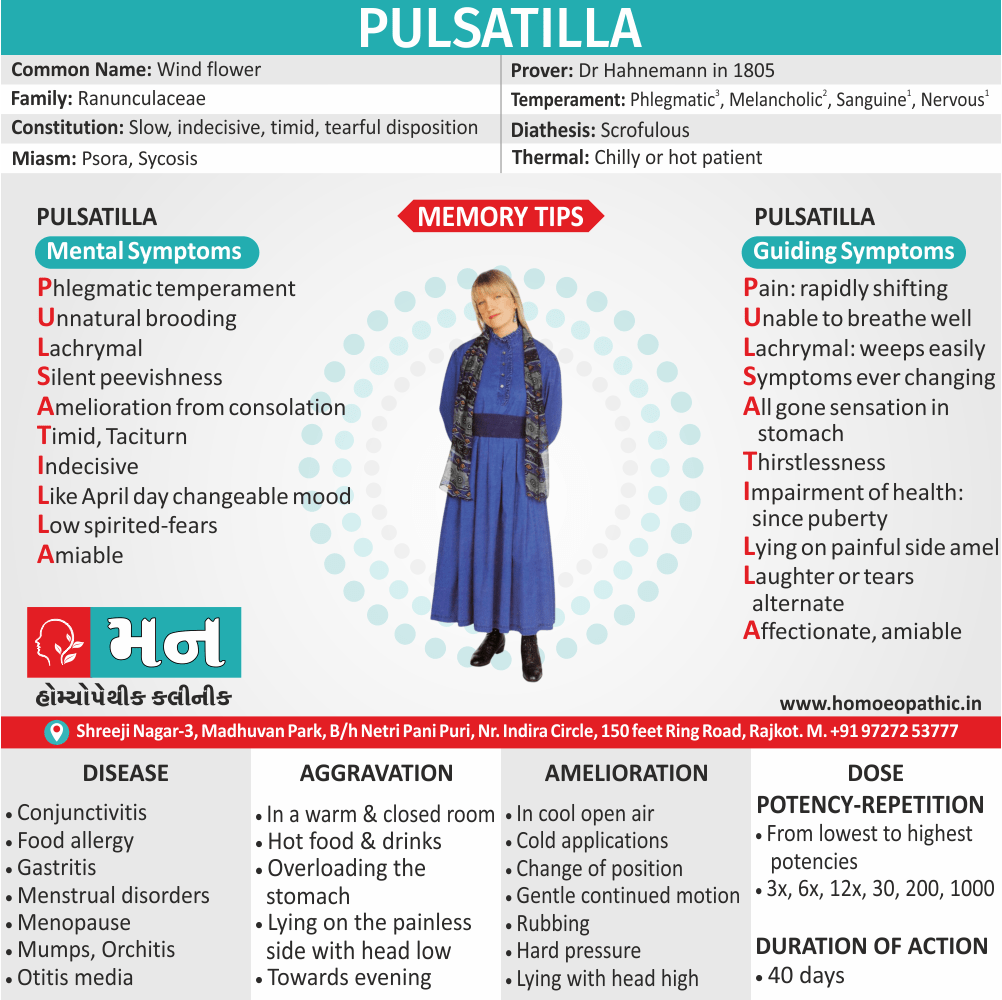
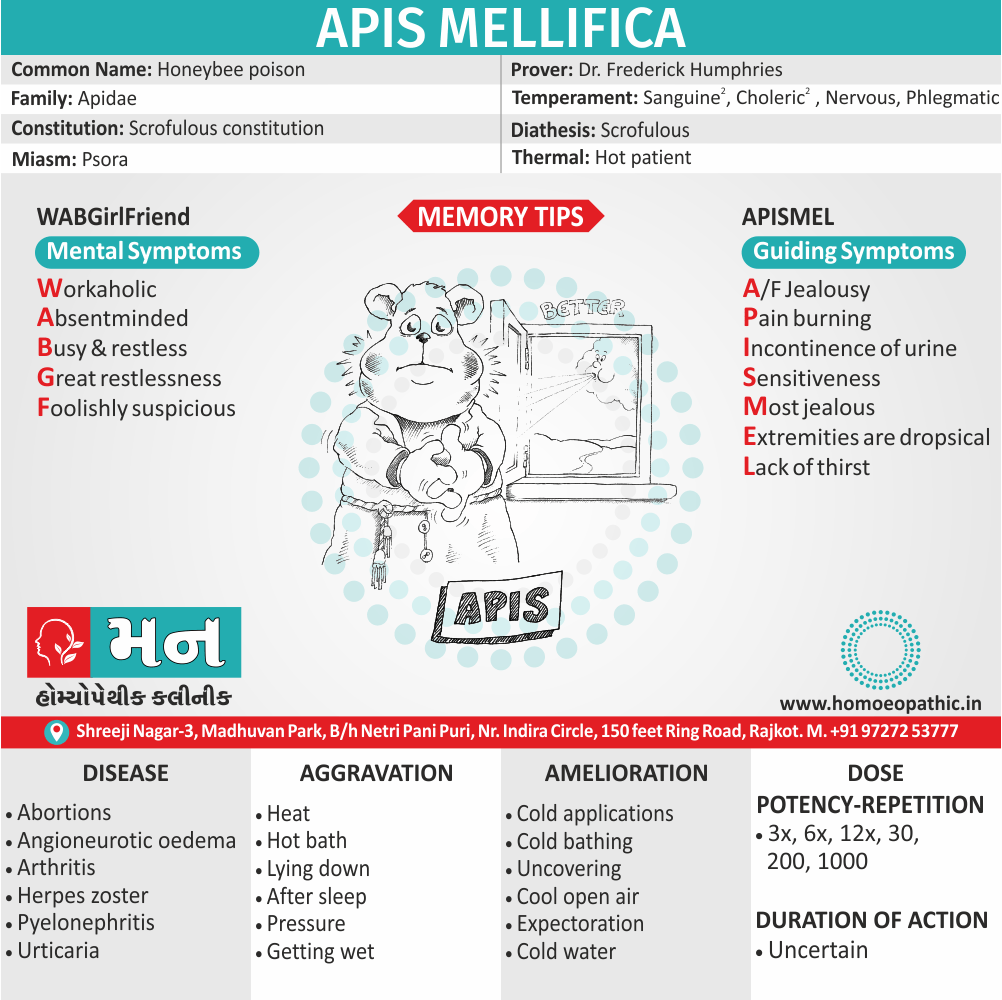
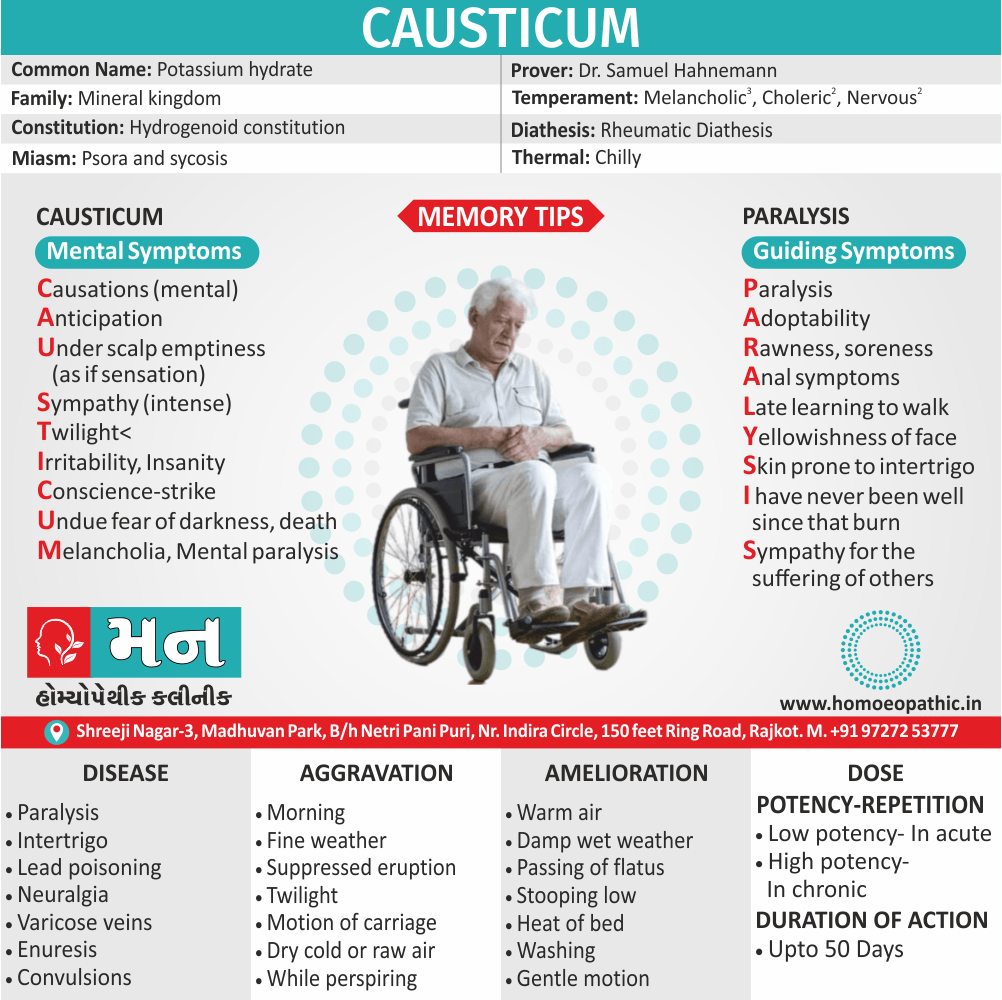
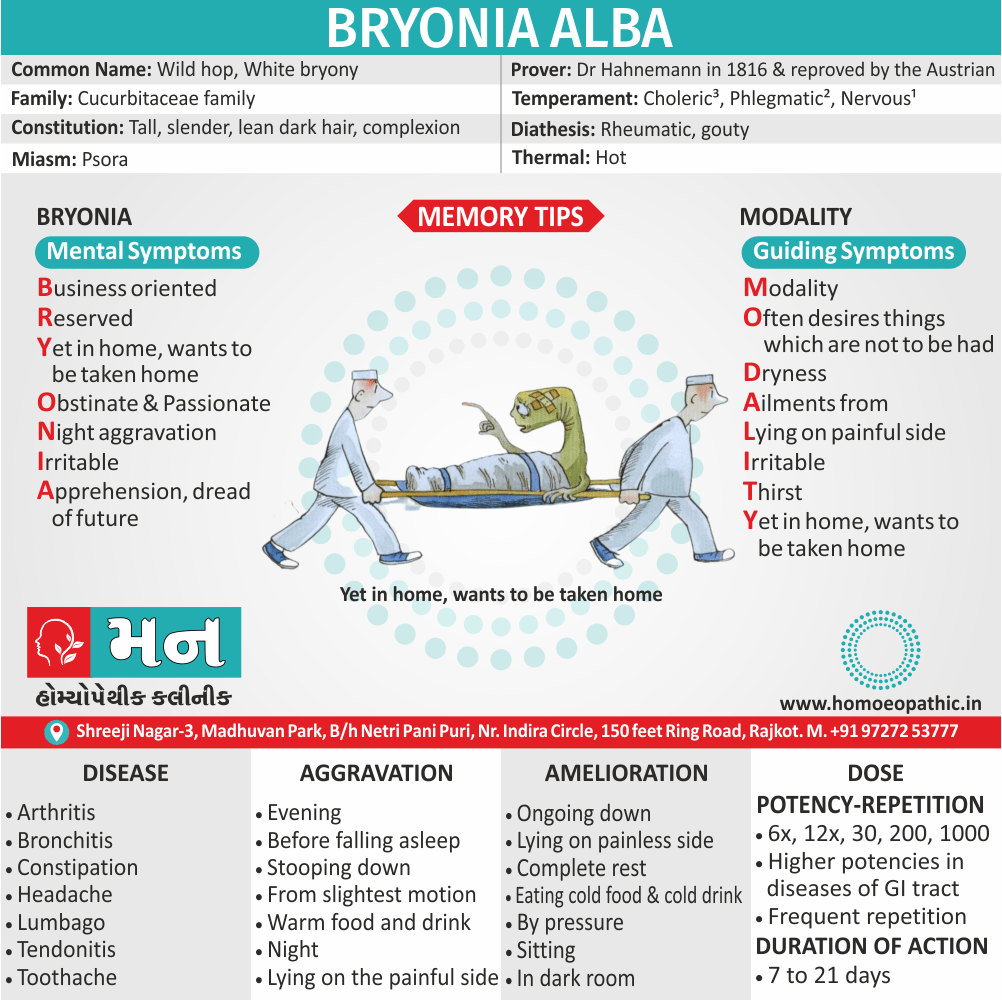
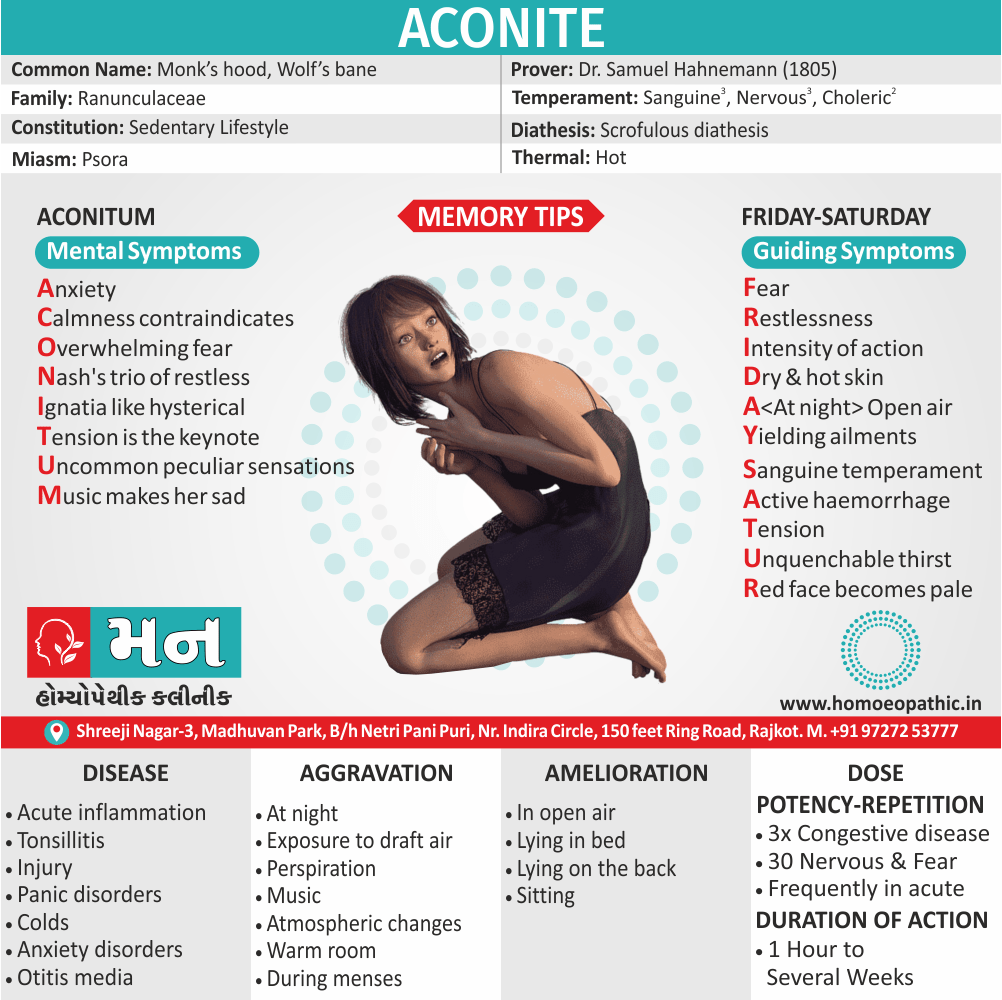
Homeopathic Treatment
Homeopathic Treatment of Lichen planus
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
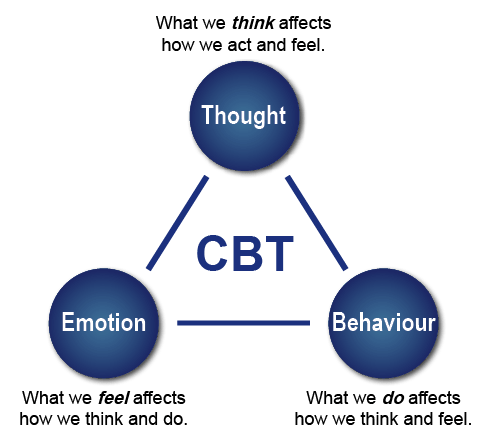
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Lichen planus:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicine:
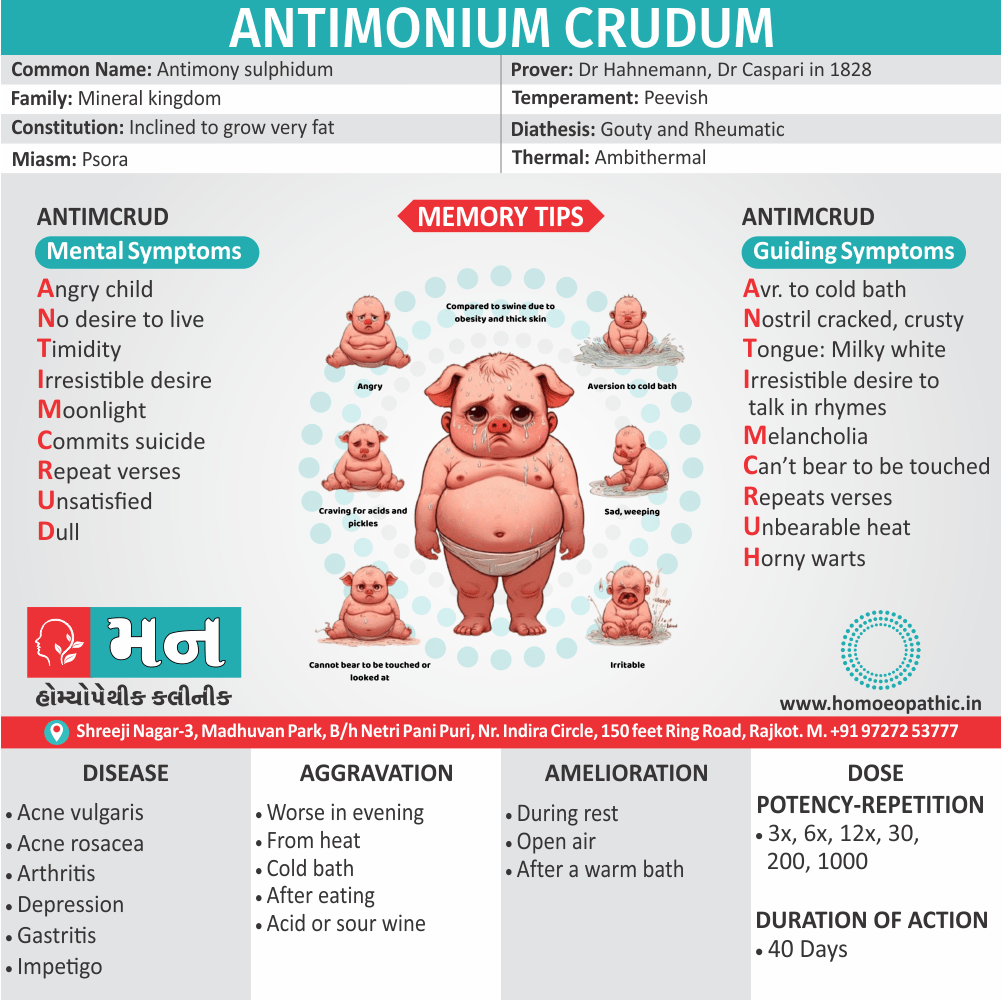
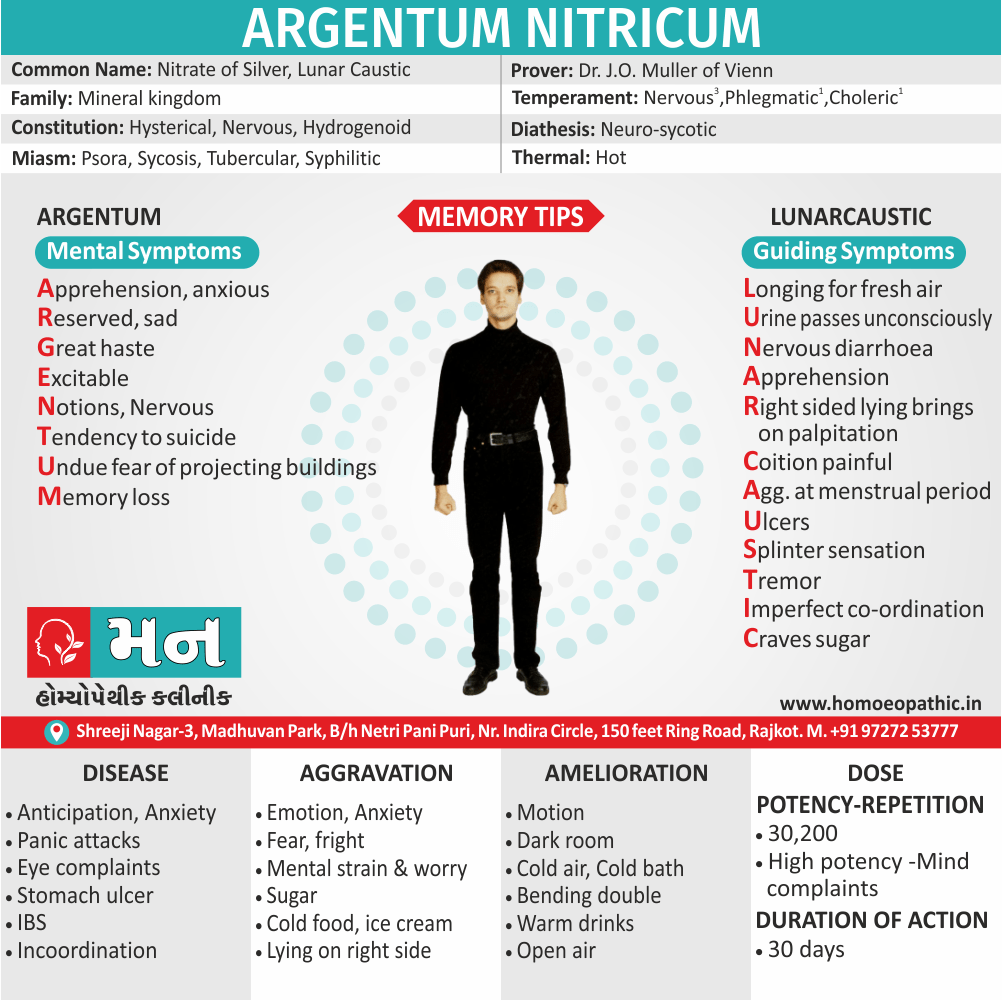
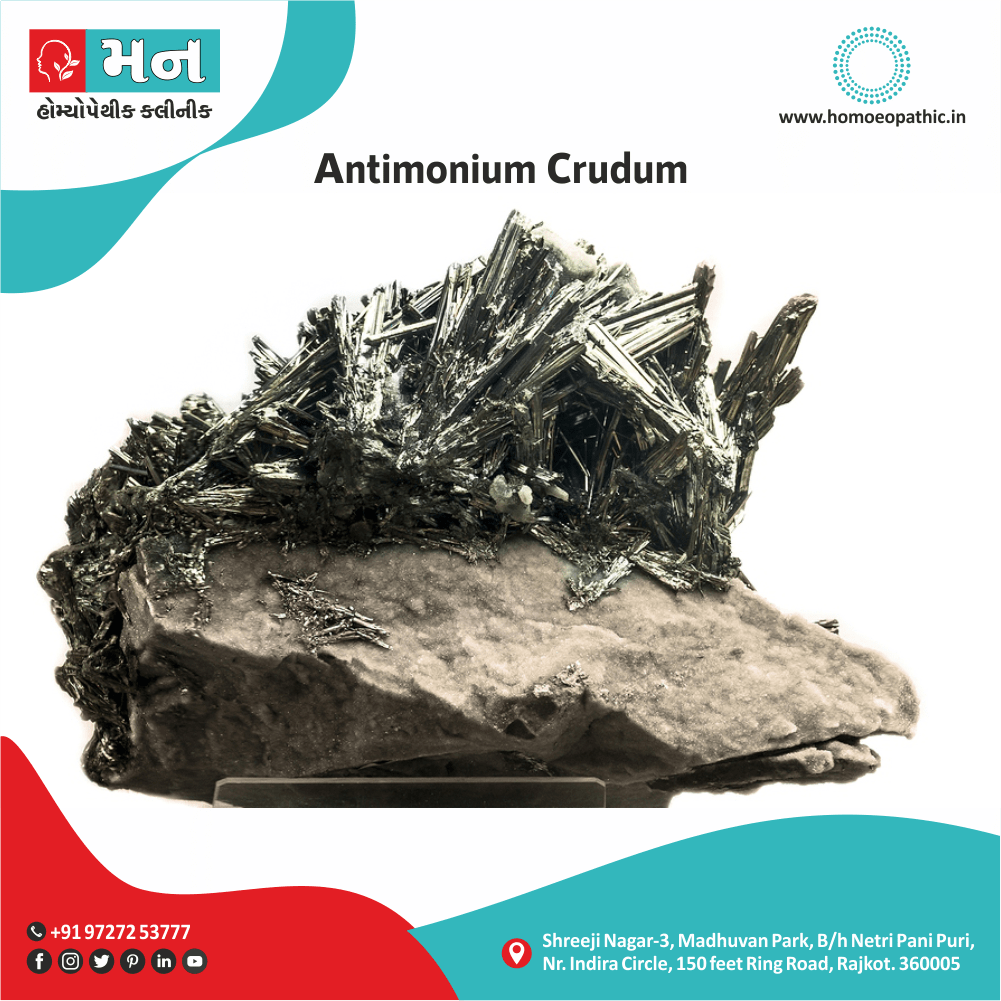
Antimonium crudum:
- Scaly, pustular eruption with burning and itching, worse especially at night.
- It is pre-eminently a scrofulous medicine, corresponding to gross constitutions with tendency to rough scaling skin with horny patches. Additionally, With these horny patches is great tenderness.
- A notable characteristic is the thickly coated tongue. Generally, it is thick and white; milky-white; or like whitewash evenly laid. In detail, The edges may be red and sore
- Sensitive to cold bathing.
- Thick, hard, honey-coloured scabs
- All in all, Itching when warm in bed.
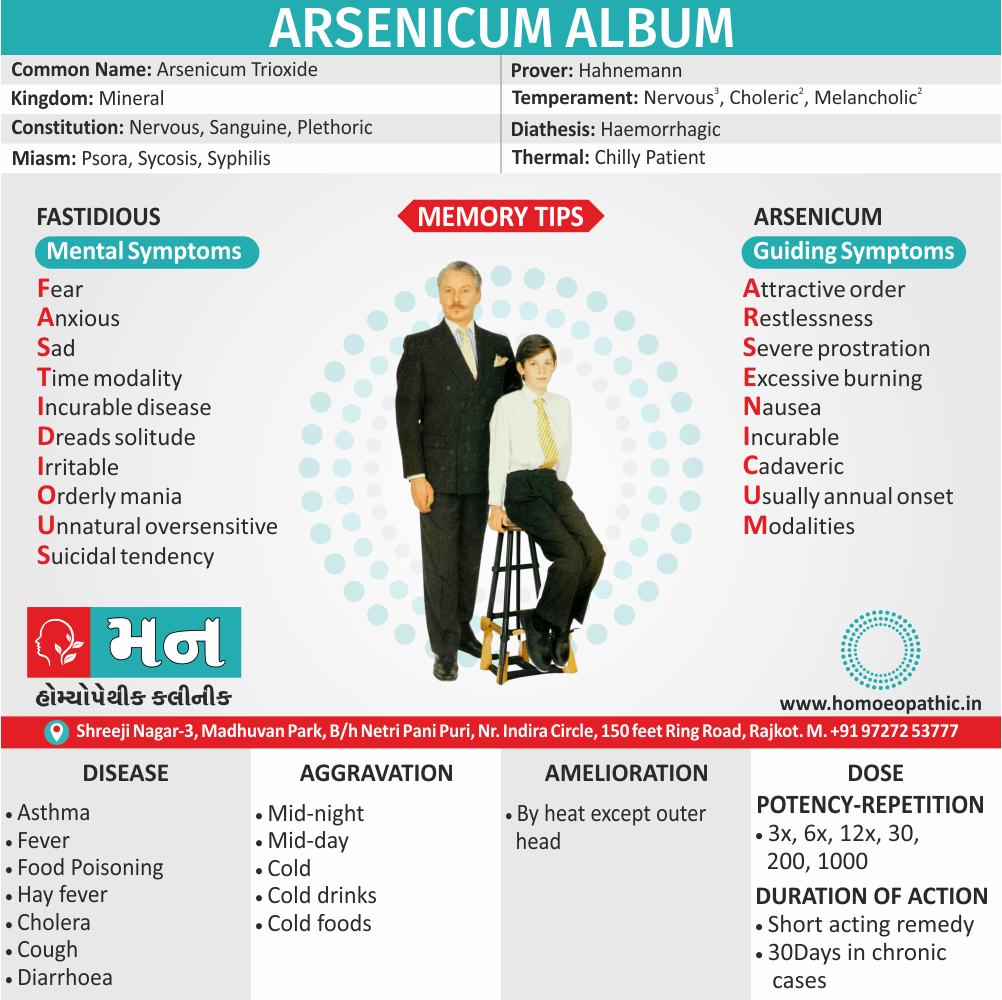
Arsenicum album:
- Itching, burning, swellings; edema, eruption, papular, dry, rough, scaly; worse cold also scratching.
- Ulcers with raised and hard edges, surrounded by a red and shining crown; with the bottoms like lard, or of a blackish-blue colour, with burning pains or shooting, when the parts affected become cold.
- Lastly, A very deep acting remedy, affecting every organ and tissue.
Arsenic Iodatum:
- Dry, scaly, itching.
- Marked exfoliation of skin in large scales, leaving a raw exuding surface beneath.
Dulcamara:
- Basically; Pruritus, always worse in cold, wet weather Humid eruptions on face, genitals, hands Warts, large, smooth, on face also palmar surface of hands.
- Thick, brown-yellow crusts, bleeding when scratched.
Juglans cineraria:
- Eruption resembling eczema simplex on upper chest, with itching pricking when heated by over-exertion.
- Furthermore, Pustules on thighs, hips, and nates, with itching and burning, a few pustules on body, face, and arms.
- Itching in spots, now here, now there, on head, neck, also shoulders, with pricking, burning and redness.
- Itching on arms > scratching.
Kali Bichromicum:
- Papular eruption.
- Hands become covered with deep, stinging cicatrice.
- Ulcer with punched-out edges, with tendency to penetrate and tenacious exudation.
Ledum palustre:
- Eruption of small pimple like red millet seed over the body.
- Excessive itching on the back of both feet worse especially after scratching and by warmth of bed > scratching.
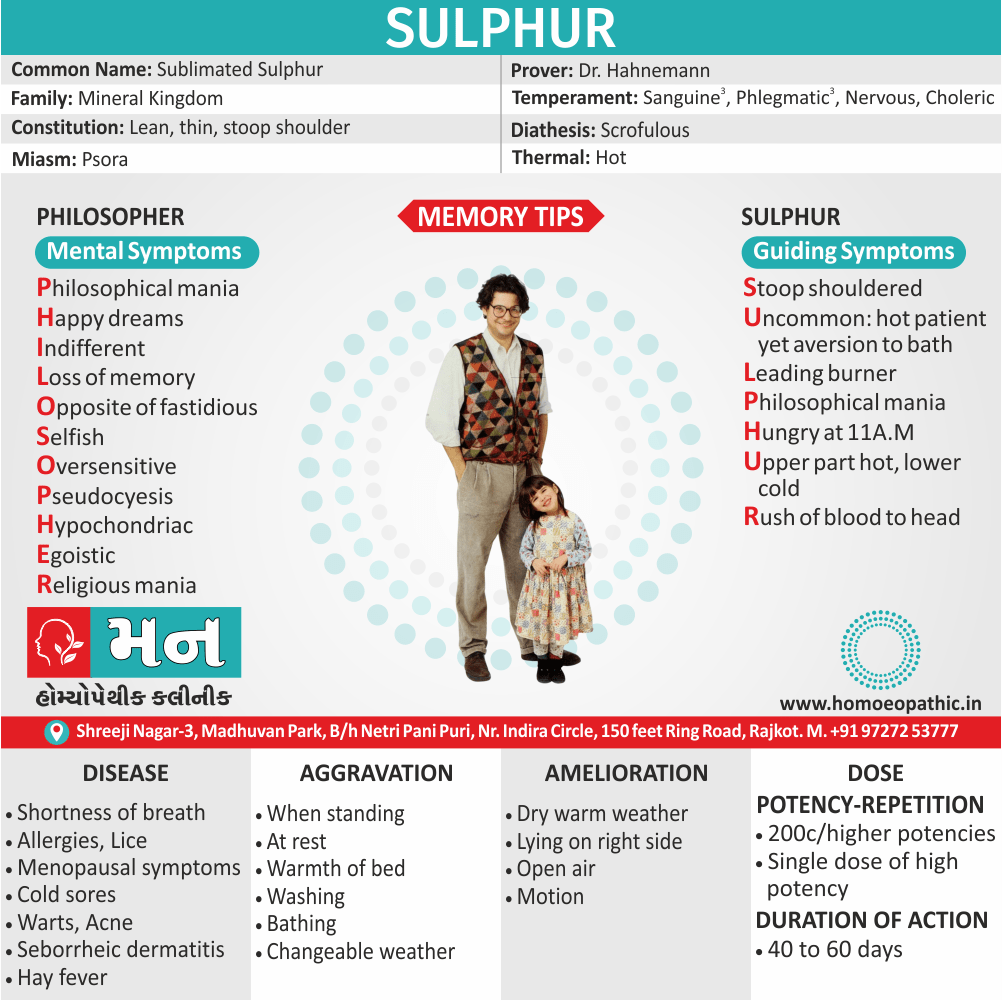
Sulphur:
- Dirty, filthy people, prone to skin affections. Aversion to being washed.
- Very red lips also face.
- Dry, scaly, unhealthy; every little injury suppurates. Itching, burning; worse scratching also washing.
- Skin affections after local medication. Pruritus, especially from warmth, is evening, often recurs in spring-time, in damp weather.[5]
Diet & Regimen
Diet & Regimen of Lichen planus
- Vitamin Brich foods like Eat green vegetables, sesame seeds, pulses, whole grain.
- Vitamin A rich foods like yellow orange fruits, vegetables, cereals, fortified foods can help.
- Cod liver oil supplements containing Vitamin A and D are also very helpful.
- Include Omega 3 fatty acids which are good for your skin such as flaxseed, olive oil, walnuts, corn.
- Green teas a great antioxidant, which can help in Lichen Planus.
- Folic acid rich foods like green vegetables prevent dry skin.
- Consume adequate water to maintain good hydration.
- Avoid excess of salt, sugar, refined foods, artificial foods, preservatives.
- Avoid yeast, sour and acidic foods, vinegar, tamarind, refined flours.
- Avoid foods which can cause allergy in you.
- Avoid very tight clothes.[4]
Do’s and Dont’s xxx
Tab Content
Terminology xxx
Tab Content
References
References use for Article Lichen planus
2] Textbook of Medicine, 5th Edition
3] https://www.mayoclinic.org/diseases-conditions/lichen-planus/diagnosis-treatment/drc-20351383
4] https://www.welcomecure.com/diseases/lichen-planus/diet-and-nutrition
5] https://www.homeobook.com/lichen-planus-and-its-homoeopathic-management/
6] https://www.msdmanuals.com/en-in/professional/dermatologic-disorders/psoriasis-and-scaling-diseases/lichen-planus
7] https://www.lybrate.com/topic/lichen-planus-everything-you-need-to-know/a248493cdb4740ba62436e4fbcde8ebc
8]https://www.researchgate.net/figure/Etiopathogenesis-of-oral-lichen-planus_fig1_346385208
9]https://emedicine.medscape.com/article/1123213-differential
FAQ
Frequently Asked Questions
What is Lichen planus ?
Lichen planus (LP) is an acute or chronic inflammatory dermatosis involving skin and / or mucous membrane. It is a rash characterized by intensely itchy polygonal papules with a violaceous hue involving the skin and, less commonly, the mucosae, hair and nails.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Lichen Planus?
- Antimonium crudum
- Arsenicum album
- Arsenic Iodatum
- Dulcamara
- Juglans cineraria
- Kali Bichromicum
- Ledum palustre
- Sulphur
What are the types of Lichen Planus ?
- Hypertrophic lichen planus
- Annular lesions
- Linear violaceus papules of lichen planus.
- Follicular lesions
- Graham Little syndrome
- Lichen planus actinicus
- Ulcerative lesions
Also Search As xxx
Frequently Asked Questions (FAQ)
XYZ
XXX
XYZ
XXX
XYZ
XXX