Pneumothorax
Definition
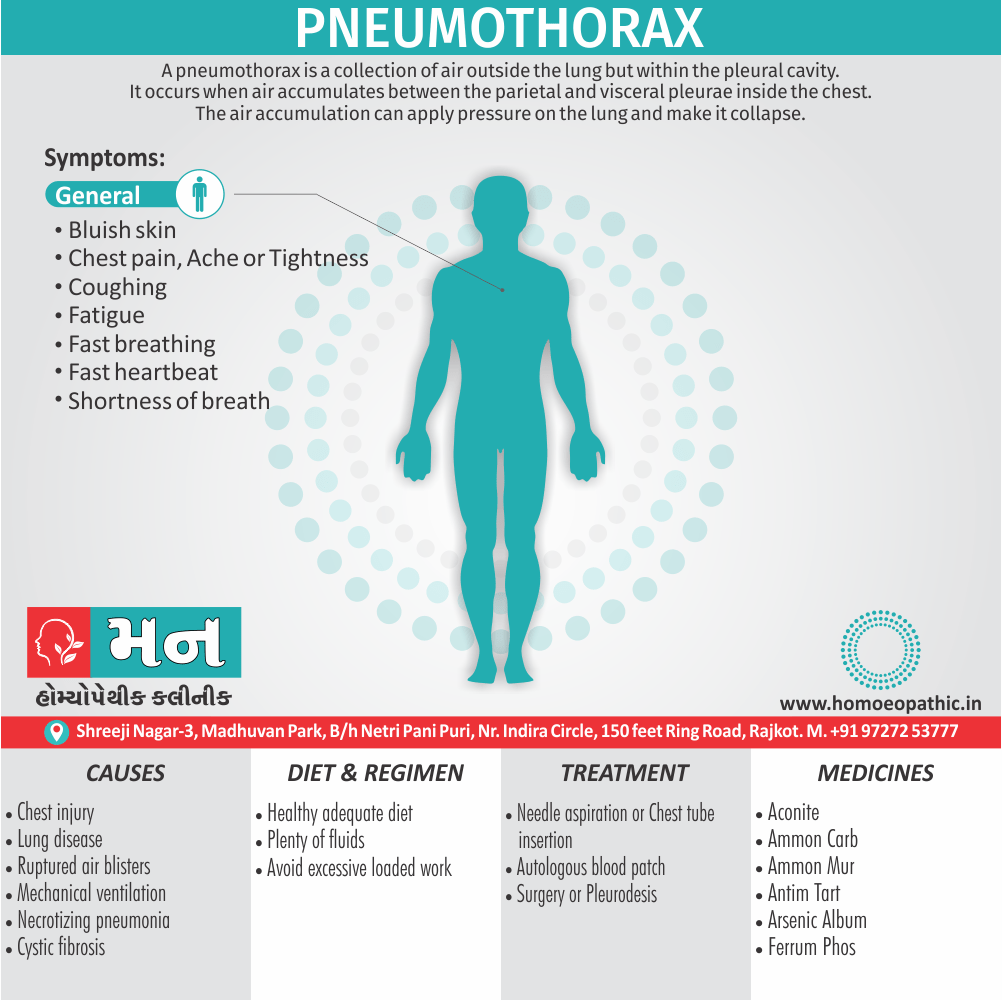
- A pneumothorax is a collection of air outside the lung but within the pleural cavity.
- It occurs when air accumulates between the parietal and visceral pleurae inside the chest.
- The air accumulation can apply pressure on the lung and make it collapse. (1)
There aren’t many true synonyms for pneumothorax in everyday language, but some related terms you might encounter include:
- Collapsed lung: This is a common way to describe pneumothorax for easier understanding by the general public. Air in the pleural space causes the lung to collapse partially or completely.
- Punctured lung: This term refers specifically to pneumothorax caused by a physical injury that punctures the lung tissue, allowing air to enter the pleural space.
In the medical field, there are a few other terms used depending on the specific type of pneumothorax:
- Simple pneumothorax: This is the most common type, where air enters the pleural space but isn’t constantly leaking in.
- Tension pneumothorax: This is a life-threatening condition where air continues to enter the pleural space without escaping, putting pressure on the lung and other organs.
- Open pneumothorax: This occurs when there’s a large opening in the chest wall that allows air to enter the pleural space.
- Spontaneous pneumothorax: This type develops without a clear cause or injury.
- Secondary pneumothorax: This occurs in people with underlying lung conditions like COPD or cystic fibrosis.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
- It is the most common cause of respiratory insufficiency following chest trauma.
- Usually if there is a rib fracture and evidence of subcutaneous emphysema, pneumothorax is certainly present.
- Pneumothorax can be closed (simple), open and tension.
- Small simple pneumothorax does not need any treatment.
- A repeat chest X-ray after 12-24 hours is essential to confirm that it is not progressing.
- It can be confused for a large bullae.
- Small pneumothorax can be missed easily.
- Bilateral pneumothorax is an emergency.
- Late pneumothorax can also occur.
- Open chest wound will produce complete collapse of lung and paradoxical shift of the mediastinum with each respiration (mediastinal flutter) causing hypoventilation and reduced cardiac output. (2)
Epidemiology
Epidemiology of Pneumothorax in India
The epidemiology in India is characterized by a few key points:
Higher incidence of Secondary Spontaneous Pneumothorax (SSP): Studies suggest that SSP is more common in India compared to Primary Spontaneous Pneumothorax (PSP). This is likely due to the higher prevalence of underlying lung diseases such as tuberculosis and chronic obstructive pulmonary disease (COPD).
Male Predominance: It affects males more frequently than females in India, with a male-female ratio ranging from 4:1 to 9:1 in various studies.
Young to middle-aged adults most affected: The most affected age group is typically young to middle-aged adults.
Regional Variations: The incidence and etiology can vary across different regions of India, possibly influenced by factors like environmental pollution, smoking habits, and the prevalence of specific lung diseases.
References:
- Clinical Profile of Spontaneous Pneumothorax in Adults: A Retrospective Study (Indian J Chest Dis Allied Sci 2016;58:95-9) – This study found that the annual incidence of spontaneous pneumothorax was 1590 per 100,000 hospital admissions, with SSP being more common than PSP. The most common cause of SSP was tuberculosis. [9]
- Profile of patients of spontaneous pneumothorax of North Gujarat region, India: a prospective study at GMERS medical college, Dharpur-Patan (Int J Res Med Sci 2017;5:1620-4) – This study reported an annual incidence of spontaneous pneumothorax of 99.9 per 100,000 hospital admissions, with a male predominance and a majority of patients being above 40 years of age. [10]
Causes
Causes of Pneumothorax:
Chest injury:
- Any blunt or penetrating injury to your chest can cause lung collapse.
- Some injuries may happen during physical assaults or car crashes, while others may inadvertently occur during medical procedures that involve the insertion of a needle into the chest.
Lung disease:
- Damaged lung tissue is more likely to collapse.
- Lung damage can be caused by many types of underlying diseases, such as chronic obstructive pulmonary disease (COPD), cystic fibrosis, lung cancer or pneumonia.
- Cystic lung diseases, such as lymphangioleiomyomatosis and Birt-Hogg-Dube syndrome, cause round, thin-walled air sacs in the lung tissue that can rupture, resulting in pneumothorax.
Ruptured air blisters:
- Small air blisters (blebs) can develop on the top of the lungs.
- These air blisters sometimes burst allowing air to leak into the space that surrounds the lungs.
Mechanical ventilation:
- A severe type of pneumothorax can occur in people who need mechanical assistance to breathe.
- The ventilator can create an imbalance of air pressure within the chest.
- The lung may collapse completely. [3]
Types
Types
It can be classified into several types based on its underlying cause and characteristics. Here’s a breakdown with references:
1. Spontaneous Pneumothorax
Primary Spontaneous Pneumothorax (PSP): Occurs in individuals without any known lung disease, often due to the rupture of small air sacs (blebs) on the lung surface. [11]
- Secondary Spontaneous Pneumothorax (SSP): Develops in individuals with pre-existing lung conditions, such as chronic obstructive pulmonary disease (COPD), asthma, or tuberculosis. [12]
2. Traumatic Pneumothorax
Open Pneumothorax: Results from a penetrating chest injury, such as a gunshot or stab wound, allowing air to enter the pleural space from the outside. [13]
- Closed Pneumothorax: Occurs due to blunt chest trauma, such as a rib fracture, causing air to leak from the lung into the pleural space without an external wound. [14]
- Iatrogenic Pneumothorax: A complication of medical procedures, such as central line insertion, lung biopsy, or mechanical ventilation. [15]
3. Tension Pneumothorax
- A life-threatening condition where air enters the pleural space but cannot escape, leading to a buildup of pressure that compresses the lungs and shifts the mediastinum. [16]
Risk Factors
Risk factors of Pneumothorax
- In general, men are far more likely to have a pneumothorax than women are.
- The type of pneumothorax caused by ruptured air blisters is most likely to occur in people between 20 and 40 years old, especially if the person is very tall and underweight.
- Underlying lung disease or mechanical ventilation can be a cause or a risk factor for a pneumothorax.
Other risk factors include:
- Smoking. The risk increases with the length of time and the number of cigarettes smoked, even without emphysema.
- Genetics. Certain types of pneumothoraxes appear to run in families.
- Previous pneumothorax. Anyone who has had one pneumothorax is at increased risk of another. (3)
Pathogenesis
Pathogenesis of Pneumothorax
This results from air entering the pleural space, the normally airtight cavity between the lung and the chest wall. This influx of air disrupts the negative pressure that keeps the lung inflated, causing it to collapse partially or completely.
The specific mechanisms behind pneumothorax development vary depending on the underlying cause. Here’s a breakdown of the pathogenesis associated with different types of pneumothorax, along with relevant book references for further reading:
1. Spontaneous Pneumothorax
Primary Spontaneous Pneumothorax (PSP):
- The most widely accepted theory is that PSP arises from the rupture of subpleural blebs or bullae, small air-filled sacs that form on the lung surface. These blebs are more common in tall, thin individuals and smokers. [11]
Secondary Spontaneous Pneumothorax (SSP):
- In SSP, pneumothorax occurs as a complication of underlying lung diseases. These conditions can create areas of weakness or inflammation in the lung tissue, increasing the risk of air leaks. [12]
2. Traumatic Pneumothorax
Open Pneumothorax:
- A penetrating chest injury creates a direct communication between the pleural space and the external environment. Air rushes into the pleural cavity with each inspiration, leading to lung collapse. [13]
Closed Pneumothorax:
- Blunt trauma can cause rib fractures or lung lacerations, allowing air to escape from the airways or lung parenchyma into the pleural space. [14]
Iatrogenic Pneumothorax:
- Medical procedures that involve the chest or lungs can inadvertently introduce air into the pleural space. [15]
3. Tension Pneumothorax
- This is a medical emergency where air enters the pleural space but cannot escape, creating a one-way valve effect. With each breath, more air becomes trapped, increasing intrapleural pressure and compressing the lung, heart, and great vessels. [16]
Pathophysiology
Pathophysiology
Pneumothorax Pathophysiology includes
- The pressure gradient inside the thorax changes with a pneumothorax.
- Usually, the pressure of the pleural space is negative when compared to atmospheric pressure. When the chest wall expands outwards, the lung also expands outwards due to surface tension between the parietal and visceral pleurae.
- Lungs tend to collapse due to elastic recoil.
- When there is communication between the alveoli and the pleural space, air fills this space changing the gradient, lung collapse unit equilibrium is achieved, or the rupture is sealed. Pneumothorax enlarges, and the lung gets smaller due to this vital capacity, and oxygen partial pressure decreases.
- Clinical presentation of a pneumothorax can range anywhere from asymptomatic to chest pain and shortness of breath.
- A tension pneumothorax can cause severe hypotension (obstructive shock) and even death.
- Increased central venous pressure can result in distended neck veins and hypotension.
- Patients may have tachypnoea, dyspnoea, tachycardia, and hypoxia.
Spontaneous pneumothorax:
- In most patients occurs due to the rupture of bullae or blebs.
- Primary spontaneous pneumothorax is defined as occurring in patients without underlying lung disease, but these patients had asymptomatic bullae or blebs on thoracotomy.
- Primary spontaneous pneumothorax occurs in tall and thin young people due to increased shear forces or more negative pressure at the apex of the lung.
- Lung inflammation and oxidative stress are essential to the pathogenesis of primary spontaneous pneumothorax.
- Current smokers have increased inflammatory cells in small airways and are at increased risk of pneumothorax.
Secondary spontaneous Pneumothorax:
- It Occurs in the presence of underlying lung disease, primarily chronic obstructive pulmonary disease; others may include tuberculosis, sarcoidosis, cystic fibrosis, malignancy, idiopathic pulmonary fibrosis, and pneumocystis jiroveci pneumonia.
Iatrogenic pneumothorax:
- It Occurs due to a complication of a medical or surgical procedure.
- Thoracentesis is the most common cause.
Traumatic pneumothoraces:
- It can result from blunt or penetrating trauma; these often create a one-way valve in the pleural space (letting the airflow in but not flow out) and hence hemodynamic compromise.
- Tension pneumothorax most commonly occurs in ICU settings in positive- pressure ventilated patients. (1)
Imagine a car accident. Pathogenesis would be like understanding how the accident happened – what caused it, the sequence of events (e.g., one car ran a red light, then hit another car). Pathophysiology would be like understanding the damage caused by the accident – the bent fenders, deployed airbags, and any injuries to the passengers.
In simpler terms, pathogenesis is about the "why" of a disease, while pathophysiology is about the "how" of the disease’s effects.
Clinical Features
Clinical Features
The clinical presentation of pneumothorax can vary depending on the size of the air leak, the underlying lung function, and the presence of any complications. However, some common signs and symptoms are frequently encountered:
1. Chest Pain
- Sudden onset: Often described as sharp or stabbing.
- Pleuritic in nature: Worsens with deep breathing or coughing.
- Location: Typically on the affected side, but can radiate to the shoulder or back. [11]
2. Shortness of Breath
- Dyspnea: Difficulty or labored breathing.
- Severity: Can range from mild to severe, depending on the extent of lung collapse.
- Exacerbation: May worsen with exertion or lying flat. [12]
3. Cough
- Dry and nonproductive: Usually without sputum.
- Triggered by: Irritation of the pleural lining. [15]
4. Physical Exam Findings
- Decreased breath sounds: Over the affected side.
- Hyperresonance to percussion: Due to increased air in the pleural space.
- Decreased tactile fremitus: Reduced transmission of vibrations through the chest wall.
- Tracheal deviation: Away from the affected side in tension pneumothorax. [13]
5. Other Symptoms
- Tachycardia: Rapid heart rate.
- Tachypnea: Rapid breathing.
- Hypoxemia: Low oxygen levels in the blood.
- Anxiety or restlessness: Due to difficulty breathing. [16]
Sign & Symptoms
Sign & Symptoms of Pneumothorax:
Symptoms can range from mild to dangerous. If your case is mild, you may not notice a problem. That’s why it’s important to tell your doctor what’s happening. Common symptoms include:
- Bluish skin
- Chest pain, ache, or tightness
- Coughing
- Fatigue
- Fast breathing
- Fast heartbeat
- Shortness of breath (6)
Clinical Examination
Clinical Examination of Pneumothorax
Key findings can help guide diagnosis and determine the severity of the condition. Here’s a breakdown of the physical exam components and their significance:
1. Inspection
- Respiratory Distress: Observe for increased respiratory rate, use of accessory muscles, or nasal flaring, indicating compromised respiratory function.
- Asymmetric Chest Expansion: Compare the movement of both sides of the chest during breathing. Reduced expansion on the affected side suggests lung collapse.
- Cyanosis: Bluish discoloration of the skin or lips due to decreased oxygen levels. [17]
2. Palpation
- Decreased Tactile Fremitus: Vibrations felt on the chest wall during speech are reduced over the affected side due to decreased lung transmission.
- Tracheal Deviation: In tension pneumothorax, the trachea may shift away from the affected side due to increased pressure in the pleural space.
- Subcutaneous Emphysema: Crackling sensation under the skin due to air leakage into the subcutaneous tissues.[18]
3. Percussion
- Hyperresonance: A drum-like sound elicited over the affected side due to increased air in the pleural cavity. [19]
4. Auscultation
- Decreased or Absent Breath Sounds: Over the collapsed lung area. [20]
5. Vital Signs
- Tachycardia: Increased heart rate due to decreased oxygen delivery.
- Tachypnea: Rapid breathing to compensate for reduced lung function.
- Hypotension: Low blood pressure in severe cases or tension pneumothorax. [13]
Diagnosis
Diagnosis of Pneumothorax
Accurate and timely diagnosis of this, is crucial for effective management and preventing complications. A combination of clinical evaluation and imaging studies is typically employed to confirm the presence and extent of lung collapse.
1. Chest X-ray
- Upright Posterior-Anterior (PA) View: The most common initial imaging study.
- Findings: A visible visceral pleural line separated from the chest wall by a radiolucent zone (air) indicates pneumothorax.
- Limitations: May miss small pneumothoraces or be difficult to interpret in supine patients. [11]
2. Ultrasound
- Point-of-Care: Can be used at the bedside for rapid assessment.
- Findings: Absence of lung sliding and the presence of a "barcode sign" or "lung point" suggest pneumo..
- Advantages: Useful in critically ill or immobile patients. [16]
3. Computed Tomography (CT) Scan
- High Sensitivity: Can detect even small pneumothoraces and underlying lung pathology.
- Indications: When chest X-ray is inconclusive or further evaluation of lung disease is needed. [12]
4. Other Tests
- Electrocardiogram (ECG): May show signs of right heart strain in tension pneumothorax.
- Arterial Blood Gas (ABG): Can reveal hypoxemia and respiratory alkalosis. [15]
Differential Diagnosis
Complications
Complications of Pneumothorax
Tension Pneumothorax:
A life-threatening condition where air trapped in the pleural space builds up pressure, compressing the lung and mediastinal structures. This can lead to decreased cardiac output, respiratory failure, and even death if not promptly treated.
Recurrence:
The risk of pneumothorax recurrence varies depending on the underlying cause. Primary spontaneous pneumothorax has a recurrence rate of up to 50%, while secondary spontaneous pneumothorax carries a higher risk due to persistent lung disease.
Persistent Air Leak:
Continued air leakage into the pleural space despite interventions like chest tube placement. May necessitate surgical procedures such as pleurodesis or bullectomy.
Hemothorax:
Blood accumulation in the pleural space, frequently associated with traumatic pneumothorax. May require drainage and, in severe cases, surgical intervention.
Infection (Empyema):
Pus collection in the pleural space, usually due to bacterial contamination. Risk factors include pre-existing lung infections and prolonged chest tube placement. Treatment involves antibiotics and drainage.
Respiratory Failure:
Inability of the lungs to maintain adequate oxygenation or carbon dioxide removal. Can occur in large pneumothoraces, with underlying lung disease, or as a result of complications like tension pneumothorax. May require mechanical ventilation and supportive care.
Long-Term Lung Impairment:
In some cases, especially with recurrent or complicated pneumothoraces, residual lung damage or reduced lung function can persist. [16]
Investigations
Investigations of Pneumothorax:
- Start with a physical examination listen breathing through a stethoscope and tap on chest to find out if it sounds hollow.
- X-rays is for your doctor so that he can see the outline of your lung.
- A CT scan, a series of X-rays that a computer turns into a detailed image of your lung.
- Arterial blood gas or pulse oximetry, to measure how much oxygen is in your blood.
- EKG, to check how well your heart is working. (6)
Treatment
Treatment of Pneumothorax:
- Initial management may involve aspiration, or the insertion of a chest drain connected to an underwater seal into the pleural space.
- This allows the lung to re-expand.
- In most cases of primary pneumothorax, air leakage stops within 48 hours or so, after which the drain can be removed.
- If the pneumothorax recurs or the air leakage does not stop, thoracoscopic surgery is indicated.
- The lung is inspected, and any blebs or bullae are stapled.
- These are usually found at the apices of the upper or lower lobes.
- Pleurodesis is then performed either by using an abrasion technique to scarify the parietal pleura, or a pleural strip (pleurectomy), or by insufflation of kaolin.
- Bullectomy and abrasion or pleurectomy carry about an 8% risk of further recurrent pneumothorax.
- This is reduced to 1–2% with kaolin insufflation, but as this technique involves leaving foreign material in the chest of a young person, it is usually kept in reserve for recurrent pneumothorax or for patients with no obvious culprit bulla or bleb.
- Secondary pneumothorax may not settle rapidly, owing to the poor quality of the underlying lung tissue.
- It typically occurs in individuals who are poor candidates for general anaesthesia and major thoracic surgery.
- It is customary, therefore, to wait for 1–2 weeks to see if the air leak will stop spontaneously.
- If not, videothoracoscopy is undertaken in better-risk patients to inspect the lung for a leaking bulla, which can be closed by stapling.
- Alternatively, kaolin mixed with local anaesthetic can be inserted as slurry up the drain.
- This option avoids general anaesthesia but results in significant pain.
- Either treatment is associated with an appreciable mortality of 5–10%, owing to respiratory and cardiovascular Complications. (4)
Prevention
Prevention of Pneumothorax:
Pneumothorax, a condition where air leaks into the pleural space, can be a serious complication of various medical procedures and underlying lung diseases. Prevention strategies are crucial in minimizing the risk of pneumothorax.
Key Preventive Measures:
Careful Technique During Procedures: Medical professionals should exercise meticulous care during procedures that involve the chest or lungs, such as thoracentesis, central line placement, and lung biopsies. Using ultrasound guidance can significantly reduce the risk of complications.
Management of Underlying Lung Diseases: Individuals with conditions like COPD, asthma, and cystic fibrosis should receive appropriate treatment to manage their lung health and reduce the likelihood of pneumothorax.
Smoking Cessation: Smoking weakens lung tissue and increases the risk of pneumothorax. Quitting smoking is essential for preventing this and other respiratory complications.
Avoidance of High-Altitude Activities: People at risk of pneumothorax should avoid activities that involve rapid changes in air pressure, such as scuba diving and high-altitude flying. [21]
Homeopathic Treatment
Homoeopathic treatment for Pneumothorax
- Homeopathy treats the person as a whole.
- It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition.
- The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
- A homeopathy doctor tries to treat more than just the presenting symptoms.
- The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
- The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses.
- Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic.
- The correct homeopathy remedy tries to correct this disease predisposition.
- The focus is not on curing the disease but to cure the person who is sick, to restore the health.
- If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Pneumothorax:
- The homeopathic remedies (medicines) given below indicate the therapeutic affinity, but this is not a complete and definite guide to the homeopathy treatment of this condition.
- The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
- So, here we describe homeopathic medicine only for reference and education purpose.
- Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
ACONITE
- Very useful for pneumothorax with constant pressure in left chest.
- There is oppressed breathing on least motion.
- Useful for hoarse, dry, croupy cough with loud, labored breathing.
- Given when child grasps at throat every time he coughs.
- Useful for dry, short, hacking cough which worse at night and after midnight.
AMMON CARB
- Useful for pneumothorax when there is cough every morning about three o’clock, with dyspnœa, palpitation and burning in chest.
- Helpful when chest feels tired with much oppression in breathing which is worse after any effort, and entering warm room, or ascending even a few steps.
AMMON MUR for Pneumothorax
- Useful for pneumothorax with hoarseness and burning in larynx.
- There is dry, hacking, scraping cough which is worse lying on back or right side.
- Given when cough loose in afternoon, with profuse expectoration and rattling of mucus.
ANTIM TART
- Useful for pneumothorax with great rattling of mucus, but very little is expectorated.
- There is Velvety feeling in chest. Useful for burning sensation in chest, which ascends to throat.
- There is Rapid, short, difficult breathing; seems as if he would suffocate.
ARSENIC ALBUM
- Useful for pneumothorax when patient is unable to lie down.
- There is fear of suffocation with constricted air passage Air passage.
- There is burning in chest with Suffocative catarrh. Useful for scanty, frothy expectoration with Darting pain through upper third of right lung.
FERRUM PHOS
- Useful in pneumothorax in First stage of all inflammatory affections.
- Useful for hard, dry cough, with sore chest. (7)
Diet & Regimen
Diet & Regimen:
- Water, fatty fish, apricots, apples, broccoli, walnuts, poultry, beans, berries [8]
While there’s no specific diet that directly prevents or treats pneumothorax, maintaining good overall nutrition and lung health is crucial for recovery and reducing the risk of complications.
Recommended Dietary Guidelines:
- Antioxidant-rich Foods: Include plenty of fruits and vegetables, especially those rich in vitamins C and E, like citrus fruits, berries, leafy greens, and nuts. These help protect lung tissue from damage.
- Whole Grains: Opt for whole-grain bread, pasta, and rice over refined carbohydrates. These provide sustained energy and fiber, aiding digestion and overall health.
- Lean Protein: Choose lean sources like fish, poultry, beans, and lentils. Protein is essential for tissue repair and immune function.
- Healthy Fats: Incorporate sources like avocados, nuts, seeds, and olive oil. These provide essential nutrients and support lung function.
- Hydration: Drink plenty of water to keep mucus thin and airways clear.
Foods to Limit:
- Processed Foods: Limit intake of highly processed foods, sugary drinks, and unhealthy fats. These can contribute to inflammation and hinder recovery.
- Salty Foods: Excess sodium can cause fluid retention, making breathing more difficult.
- Alcohol and Caffeine: These can dehydrate the body and negatively impact lung health.
Lifestyle Recommendations:
- Smoking Cessation: If you smoke, quitting is the most crucial step you can take for your lung health.
- Regular Exercise: Engage in moderate exercise as tolerated to strengthen respiratory muscles and improve overall fitness.
- Stress Management: Practice relaxation techniques like deep breathing and meditation to reduce stress and improve lung function.
- Adequate Sleep: Aim for 7-8 hours of sleep per night to support healing and immune function. [22,23,24]
Remember, always consult your doctor or a registered dietitian for personalized dietary advice based on your individual needs and medical condition.
Do’s and Don'ts
Do’s & Don’ts
Pneumothorax do’s & don’ts
Do’s
- Seek medical attention immediately if you experience sudden chest pain, shortness of breath, or a persistent cough.
- Follow your doctor’s treatment plan. This may include observation, needle aspiration, chest tube placement, or surgery, depending on the severity of your pneumothorax.
- Rest and take it easy while recovering. Avoid strenuous activity and heavy lifting until your doctor clears you.
- Take pain medications as prescribed to manage any discomfort.
- Practice deep breathing exercises as instructed by your healthcare provider.
- Quit smoking, if you smoke. Smoking increases your risk of pneumothorax and can delay healing.
- Attend follow-up appointments with your doctor to monitor your progress and address any concerns.
- Get vaccinated against respiratory infections, such as influenza and pneumonia, which can increase the risk of complications.
- Be aware of the signs and symptoms of recurrence, such as sudden chest pain or shortness of breath, and seek medical attention immediately if they occur.
Don’ts
- Don’t ignore chest pain or shortness of breath. These are serious symptoms and could indicate a pneumothorax or other medical emergency.
- Don’t engage in strenuous activity or heavy lifting until your doctor clears you. This can worsen the air leak and delay healing.
- Don’t smoke or be around secondhand smoke. Smoking damages your lungs and increases your risk of complications.
- Don’t fly in an airplane or scuba dive until your doctor gives you the okay. Changes in air pressure can worsen a pneumothorax.
- Don’t travel to high altitudes without consulting your doctor. The decreased air pressure at high altitudes can also exacerbate a pneumothorax.
- Don’t drive if you’re experiencing shortness of breath or chest pain.
- Don’t hesitate to ask your doctor any questions you have about your condition or treatment.
Terminology
Terminology
Pleural Space:
The normally airtight cavity between the lung and the chest wall, lined by two thin membranes called the pleura.
Visceral Pleura:
The inner membrane that covers the lung surface.
Parietal Pleura:
The outer membrane that lines the chest wall.
Spontaneous Pneumothorax:
Occurs without any apparent cause or injury.
- Primary Spontaneous Pneumothorax (PSP): Happens in individuals without pre-existing lung disease.
- Secondary Spontaneous Pneumothorax (SSP): Occurs in people with underlying lung conditions.
Traumatic Pneumothorax:
Results from an injury to the chest, such as a rib fracture or penetrating wound.
Iatrogenic Pneumothorax:
Occurs as a complication of medical procedures.
Tension Pneumothorax:
A life-threatening type where air enters the pleural space but cannot escape, causing increased pressure and compression of vital organs.
Blebs:
Small air-filled sacs on the lung surface that can rupture and cause pneumothorax.
Bullae:
Larger air spaces within the lung tissue that can also rupture.
Chest Tube:
A tube inserted into the pleural space to drain air or fluid.
Needle Aspiration:
A procedure where a needle is used to remove air from the pleural space.
Pleurodesis:
A procedure to create adhesions between the pleura, preventing future pneumothorax.
Bullectomy:
Surgical removal of bullae to reduce the risk of recurrence.
Hypoxemia:
Low oxygen levels in the blood.
Dyspnea:
Shortness of breath or difficulty breathing.
Tachypnea:
Rapid breathing.
Tachycardia:
Fast heart rate.
Hypotension:
Low blood pressure.
Subcutaneous Emphysema:
Air trapped under the skin, causing a crackling sensation.
Mediastinal Shift:
Displacement of the central chest structures (heart, trachea, etc.) due to pressure in the pleural space.
Homeopathic Remedies
Homeopathic remedies for pneumothorax are selected based on the individual’s unique symptom picture, including:
- Physical Symptoms: Chest pain, shortness of breath, cough, anxiety, etc.
- Mental & Emotional State: Fear, restlessness, anxiety, etc.
- Underlying Cause: Whether the pneumothorax is spontaneous, traumatic, or iatrogenic.
Some commonly used homeopathic remedies for pneumothorax include:
Aconitum Napellus:
For sudden onset with intense fear and anxiety.
Arnica Montana:
For traumatic pneumothorax with bruising and soreness.
Carbo Vegetabilis:
For shortness of breath and a feeling of suffocation.
Phosphorus:
For tall, slender individuals with a tendency to bleed easily.
Kali Carbonicum:
For sharp chest pain and stitching sensations.
References
References
- Pneumothorax – StatPearls – NCBI Bookshelf (nih.gov)
- Manipal Manual Of Surgery Fourth Edition Chapter 44
- Pneumothorax – Symptoms and causes – Mayo Clinic
- Principles Practice Surgery 6th Edition Chapter 22
- Pneumothorax (Collapsed Lung): Symptoms & Treatment (clevelandclinic.org)
- Pneumothorax (Collapsed Lung): Symptoms, Causes, Diagnosis and Treatment (webmd.com)
- homeopathic treatment for Pneumothorax in homeopathy, Pneumothorax Treatment in Patna & Ranchi (rajeevclinic.com)
- Pneumothorax – Types, Causes, Symptoms, Diet And Treatment (lybrate.com)
- Clinical Profile of Spontaneous Pneumothorax in Adults: A Retrospective Study (Indian J Chest Dis Allied Sci 2016;58:95-9)
- Profile of patients of spontaneous pneumothorax of North Gujarat region, India: a prospective study at GMERS medical college, Dharpur-Patan(Int J Res Med Sci 2017;5:1620-4)
- Murray and Nadel’s Textbook of Respiratory Medicine, 7th Edition by Robert J. Mason, John F. Murray, Jay A. Nadel, et al. (2022, Elsevier)
- Fishman’s Pulmonary Diseases and Disorders, 6th Edition by Michael A. Grippi, Robert M. Senior, et al. (2023, McGraw Hill)
- Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 9th Edition by Judith E. Tintinalli, J. Stephan Stapczynski, et al. (2019, McGraw Hill)
Sabiston Textbook of Surgery, 21st Edition by Courtney M. Townsend, Jr., et al. (2022, Elsevier)
- Harrison’s Principles of Internal Medicine, 21st Edition by Dennis L. Kasper, Anthony S. Fauci, et al. (2022, McGraw Hill)
- Rosen’s Emergency Medicine: Concepts and Clinical Practice, 10th Edition by Robert S. Hockberger, et al. (2023, Elsevier)
- Bates’ Guide to Physical Examination and History Taking, 13th Edition by Lynn S. Bickley, Peter G. Szilagyi (2022, Wolters Kluwer).
- DeGowin’s Diagnostic Examination, 11th Edition by Richard F. LeBlond, Donald D. Brown, Richard A. DeGowin (2020, McGraw Hill).
- Mosby’s Physical Examination Handbook, 9th Edition by Seidel, Ball, Dains, Benedict, et al. (2015, Mosby).
- The Oxford Textbook of Clinical Examination and Practical Skills, 2nd Edition by Talley, O’Connor (2017, Oxford University Press).
Murray and Nadel’s Textbook of Respiratory Medicine, 7th Edition ,Robert J. Mason, John F. Murray, Jay A. Nadel, et al. 2023, Elsevier
- Nutrition and COPD American Lung Association
- 20 Foods to Promote Lung Health and 5 to Avoid
- Best and Worst Foods for Lung Health – WebMD
Also Search As
Also Search As
People can search for homeopathic articles on pneumothorax using a variety of online resources and strategies. Here are some effective ways:
Online Search Engines:
- Use specific keywords: Combine terms like "homeopathy," "treatment," "remedies," and "case studies" to refine your search.
- Include relevant phrases: Search for phrases like "homeopathic approach to pneumothorax," "homeopathic management of collapsed lung," or "homeopathic remedies for pneumothorax."
- Use advanced search operators: Utilize operators like quotation marks (""), minus sign (-), and site: to narrow down your search results. For example: "homeopathy pneumothorax" -conventional site:.edu
Homeopathic Websites and Databases:
- Explore reputable homeopathic websites: Many homeopathic organizations and practitioners have websites that offer articles, case studies, and research related to homeopathy. Search their archives or use their search functions to find information on pneumothorax.
- Search homeopathic databases: Several online databases specialize in homeopathic literature, including journals, books, and clinical trials. These can provide access to more in-depth information and research on the homeopathic treatment of pneumothorax.
Social Media and Forums:
- Join homeopathic groups and communities: Engage with other homeopathic practitioners and enthusiasts on social media platforms and online forums. Ask for recommendations on relevant articles or case studies on disease.
- Follow homeopathic experts and organizations: Stay updated on the latest research and developments in homeopathy by following key figures and institutions in the field. They may share links to relevant articles on it.
There are several ways to search for information on pneumothorax, depending on the level of detail and type of resources you’re looking for:
General Search:
- Search engines: Use Google, Bing, or other search engines with keywords like "pneumothorax," "collapsed lung," or "air in chest." This is a great starting point for general information and overview.
- Online encyclopedias: Websites like Wikipedia or Britannica can provide basic information on the condition, its causes, symptoms, and treatment.
Medical Websites and Databases:
- Reputable health organizations: Organizations like the Mayo Clinic, Cleveland Clinic, or American Lung Association have dedicated sections on pneumothorax with detailed explanations and patient resources.
- Medical literature databases:Databases like PubMed or Google Scholar allow you to search for scientific articles and research studies on pneumothorax, providing more in-depth and specialized information.
Image and Video Search:
- Image search engines: Search for "pneumothorax x-ray" or "pneumothorax ultrasound" to see visual representations of the condition and how it’s diagnosed.
- Video platforms: Search YouTube or other video platforms for educational videos on pneumothorax, its symptoms, and treatment options.
- Specific Search Queries:
- Focus on a particular aspect: Use specific search queries like "pneumothorax treatment options," "pneumothorax symptoms," "pneumothorax causes," or "pneumothorax complications" to find targeted information.
- Include demographics or medical history: Search for "pneumothorax in smokers," "pneumothorax in children," or "pneumothorax after surgery" to find information tailored to specific populations or risk factors.
Frequently Asked Questions (FAQ)
What is a pneumothorax?
A pneumothorax occurs when air leaks into the pleural space, the area between the lung and chest wall, causing the lung to collapse partially or completely. This can lead to sudden chest pain and difficulty breathing.
What causes a pneumothorax?
- Chest injury or trauma
- Lung diseases like COPD, asthma, or cystic fibrosis
- Ruptured air blisters (blebs) on the lung surface
- Medical procedures like lung biopsies or central line placement
- Sometimes, it can occur spontaneously without an apparent cause
How is a pneumothorax diagnosed?
A pneumothorax is typically diagnosed through a physical examination and chest X-ray. In some cases, a CT scan may be needed for a more detailed view of the lungs.
What are the symptoms of a pneumothorax?
Common symptoms include sudden chest pain, shortness of breath, rapid breathing, and a racing heartbeat. In some cases, a pneumothorax may cause a bluish tint to the skin due to decreased oxygen levels.
What are the potential complications of a pneumothorax?
If left untreated, a pneumothorax can lead to serious complications, including:
- Tension pneumothorax, a life-threatening condition where air trapped in the chest cavity puts pressure on the heart and other organs.
- Respiratory failure, where the lungs can’t provide enough oxygen to the body.
- Recurrence of pneumothorax
Can homeopathy help with pneumothorax?
While homeopathy may offer supportive care by addressing associated symptoms and promoting overall well-being, it’s crucial to understand that pneumothorax is a medical emergency requiring immediate conventional treatment.
How long does it take to see improvement with homeopathy for pneumothorax-related symptoms?
Homoeopathic treatment
The response to homeopathic treatment varies depending on the individual and the severity of symptoms. Conventional medical treatment is the priority for addressing the pneumothorax itself.
Can homeopathy be used alongside conventional treatment for pneumothorax?
Yes, homeopathy can potentially be used as a complementary therapy alongside conventional medical treatment, but only under the supervision of a healthcare professional.
What homeopathic remedies are sometimes considered for pneumothorax symptoms?
Some remedies that might be considered, depending on individual symptoms and constitution, include
Aconitum napellus (for sudden onset, anxiety),
Arnica montana (for trauma),
and Bryonia alba (for sharp, stitching pains worsened by movement). However, consulting a qualified homeopath is essential.
How does a homeopath choose the right remedy for pneumothorax-related symptoms?
A skilled homeopath will conduct a detailed case analysis, considering the patient’s physical, mental, and emotional state, as well as their medical history, to select the most suitable remedy.
