Psychiatric History Taking
Definition:
The amount of detail and the focus of the psychiatric history taking vary from case to case but the basic aims are the same it is not necessary to learn a separate interview for each condition.
Overview of Psychiatric History Taking:
When time is short, parts of the background history should be covered only in outline.
It is important to be flexible and able to adopt any of the following three approaches:
(i) to spend 2 minutes screening patients for mental disorder,
(ii) to spend 5–10 minutes undertaking a shortened, focused history in an emergency, or
(iii) to spend perhaps 30 minutes obtaining a full history.
Note that the most important investigation in psychiatry is always obtaining a corroborative history from someone who knows the patient well.
The elements of the psychiatric history taking:
- History of the presenting problems
- Background history
- Family history
- Personal history
- Social history
- Past medical history
- Past psychiatric history
- Medicines
- Personality
- Corroborative history
Screening Questions:
When a patient complains of symptoms of physical illness, for example, it is often appropriate to check for evidence of a psychiatric disorder, since this may be present as the cause or a consequence of the symptoms.
For this purpose, a brief screening interview is require to detect any symptoms and problems that have not complained of spontaneously.
The following five domains are helpful:
General well-being:
- Fatigue, irritability, poor concentration, poor sleep, and a feeling of being under pressure/ not coping.
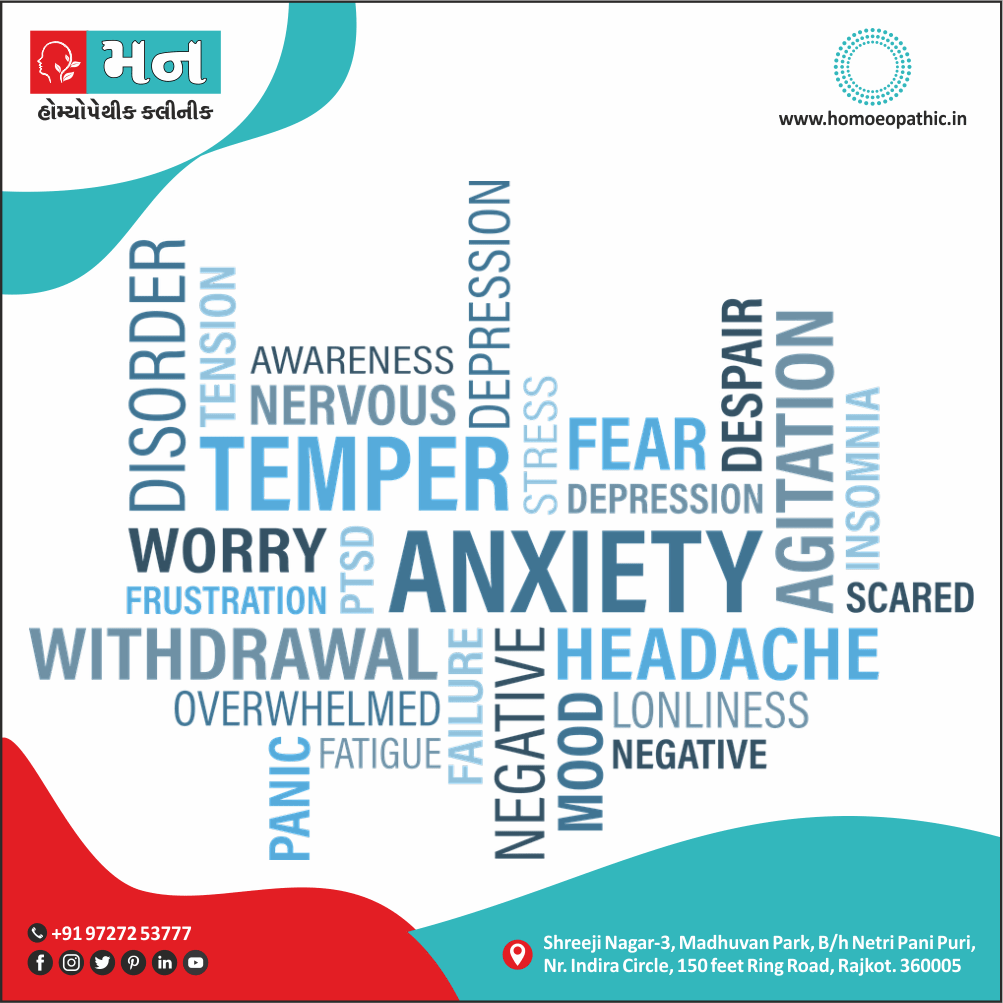
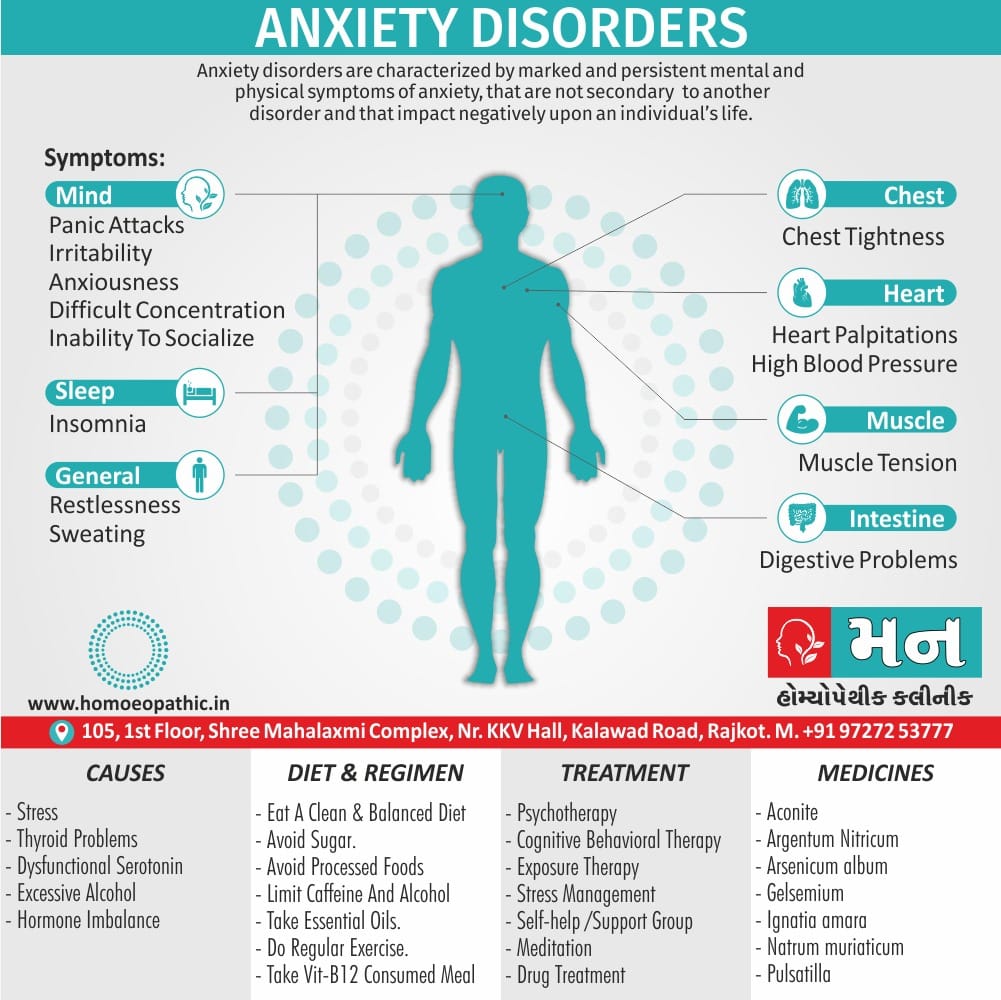
Anxiety:
- Tension, sweating, palpitations, and repeated worrying thoughts.
- If replies are positive, go on to systematic questions about anxiety disorders.
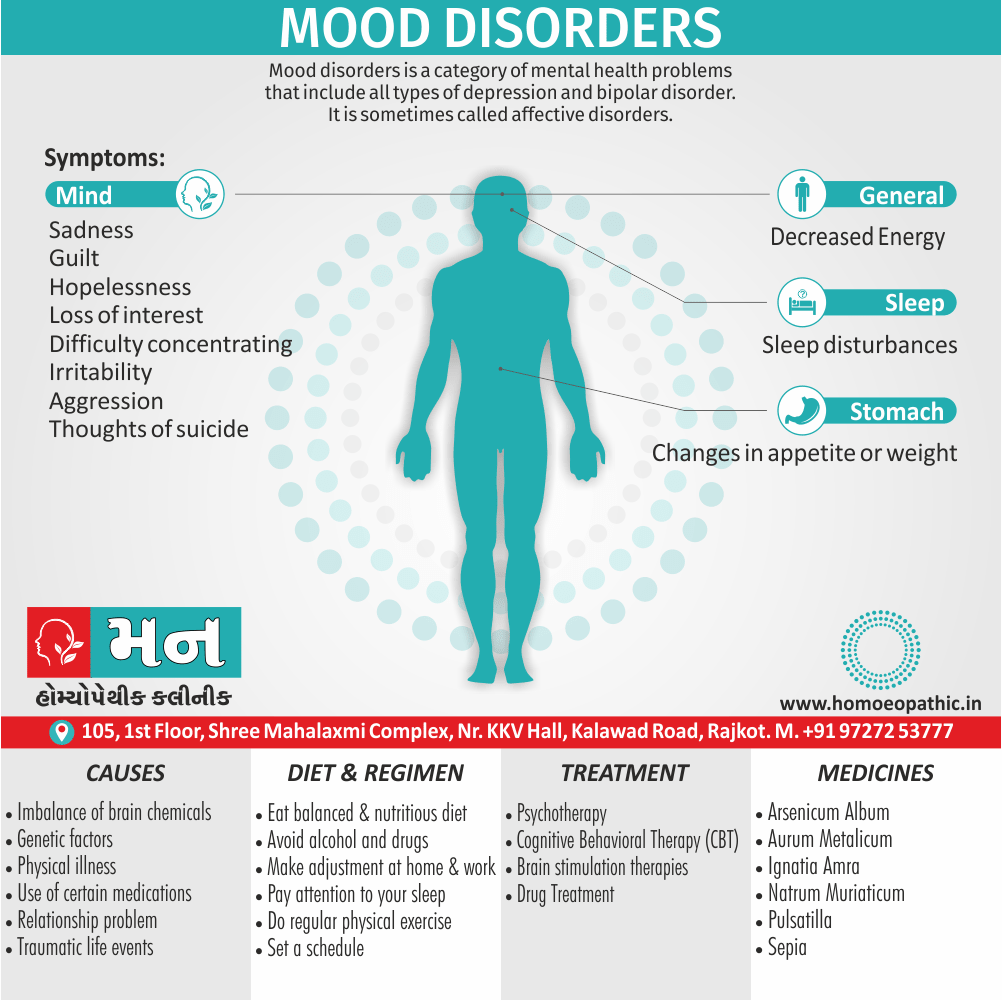
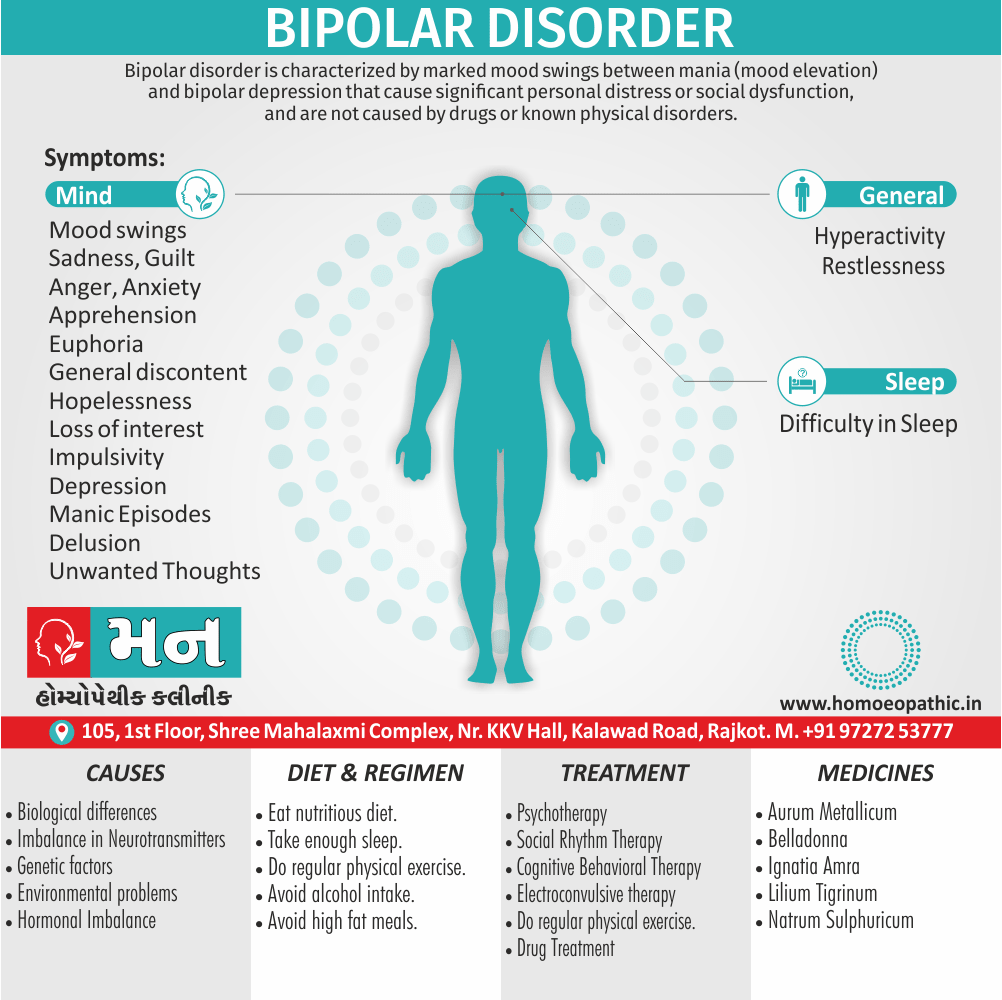
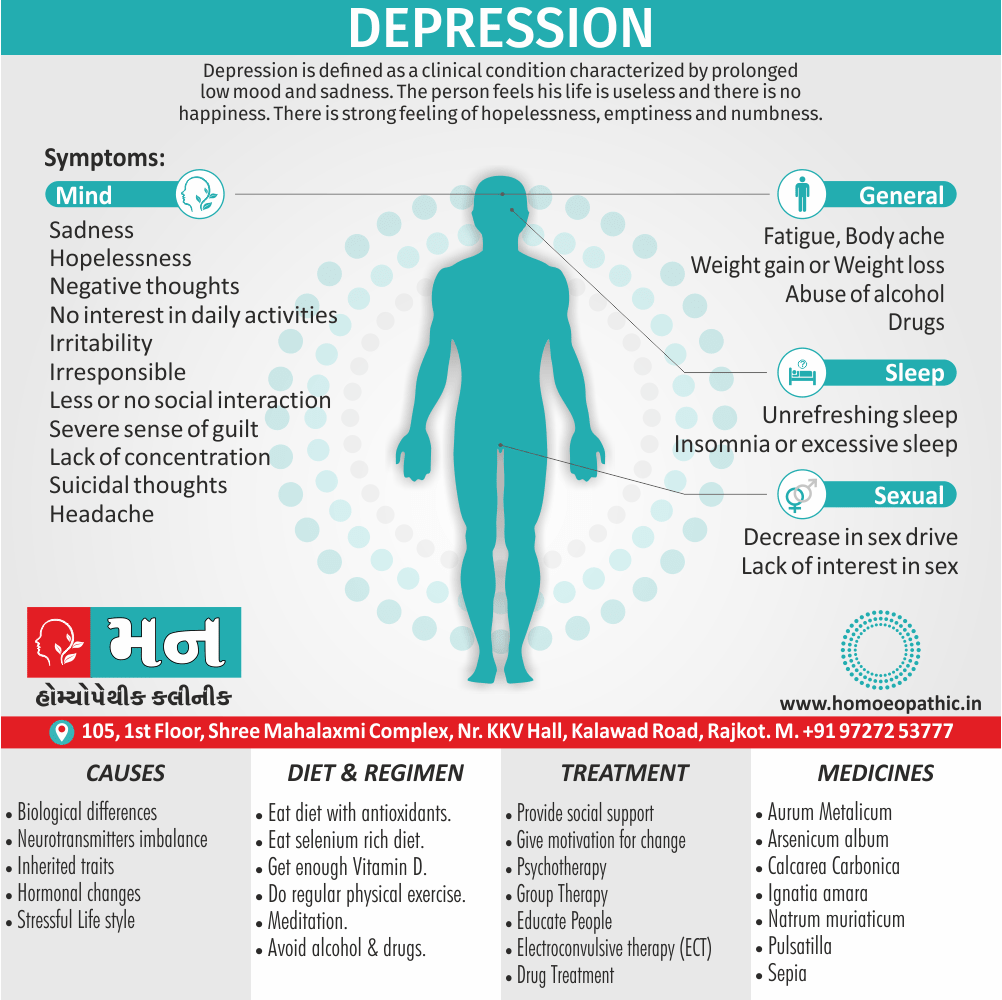
Depression:
- Persistent low mood, low energy, loss of interest, loss of confidence, and hopelessness.
- If these questions are answered positively, go on to questions concerning depressive disorder, including suicidal ideas.
Memory:
- Difficulty in recalling recent events.
- If difficulties are report or suspected, use simple tests of cognitive function.
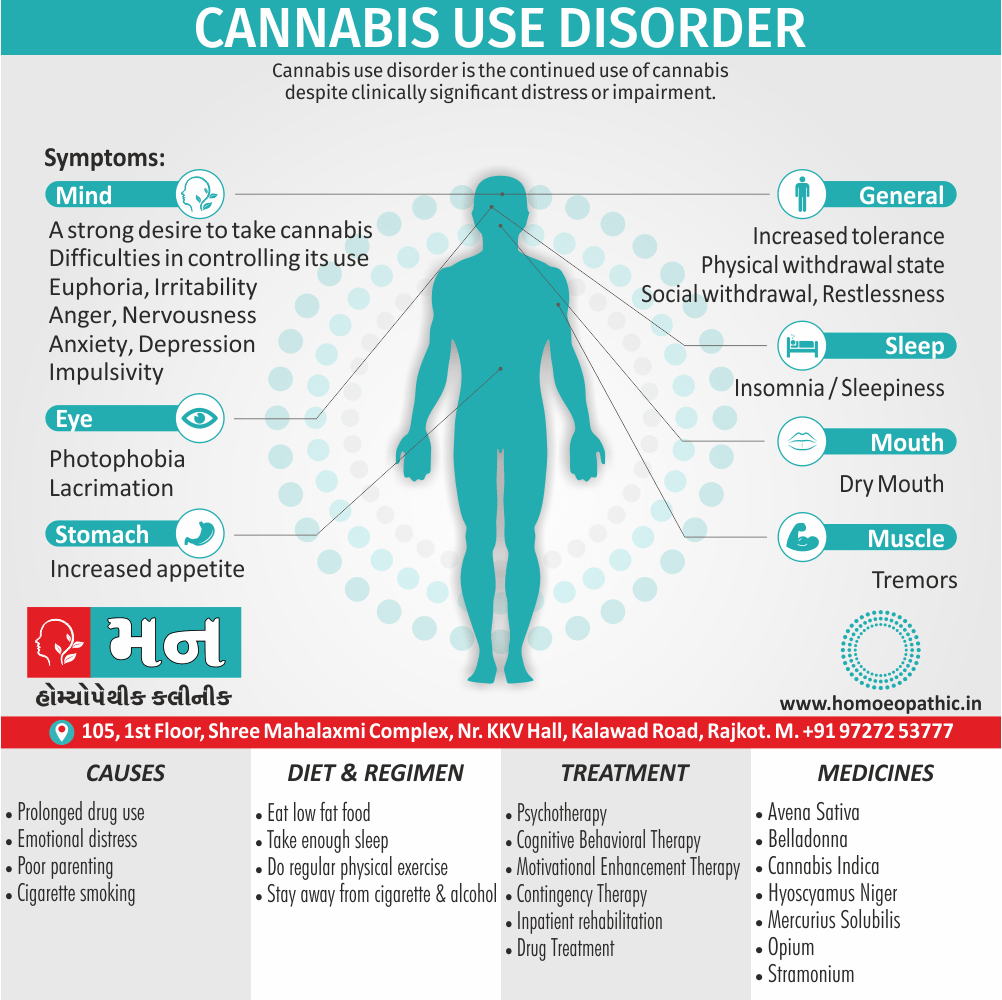
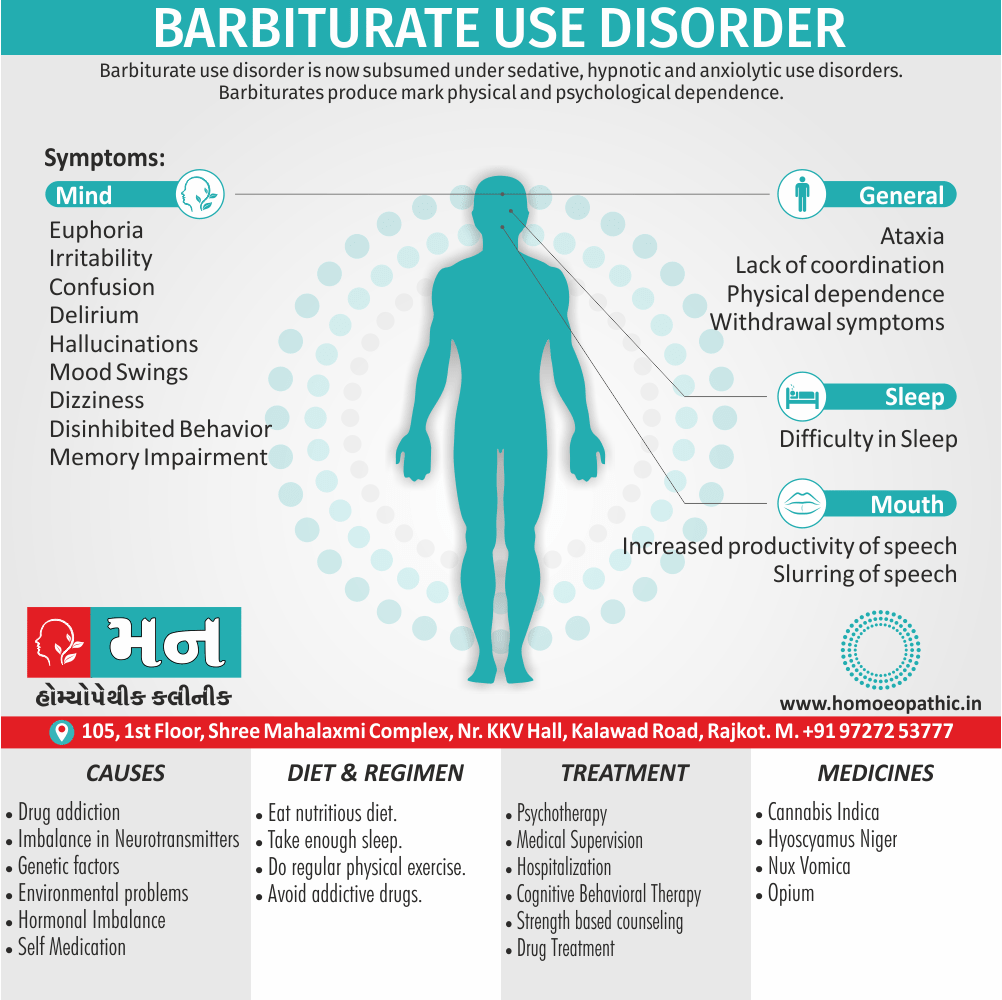
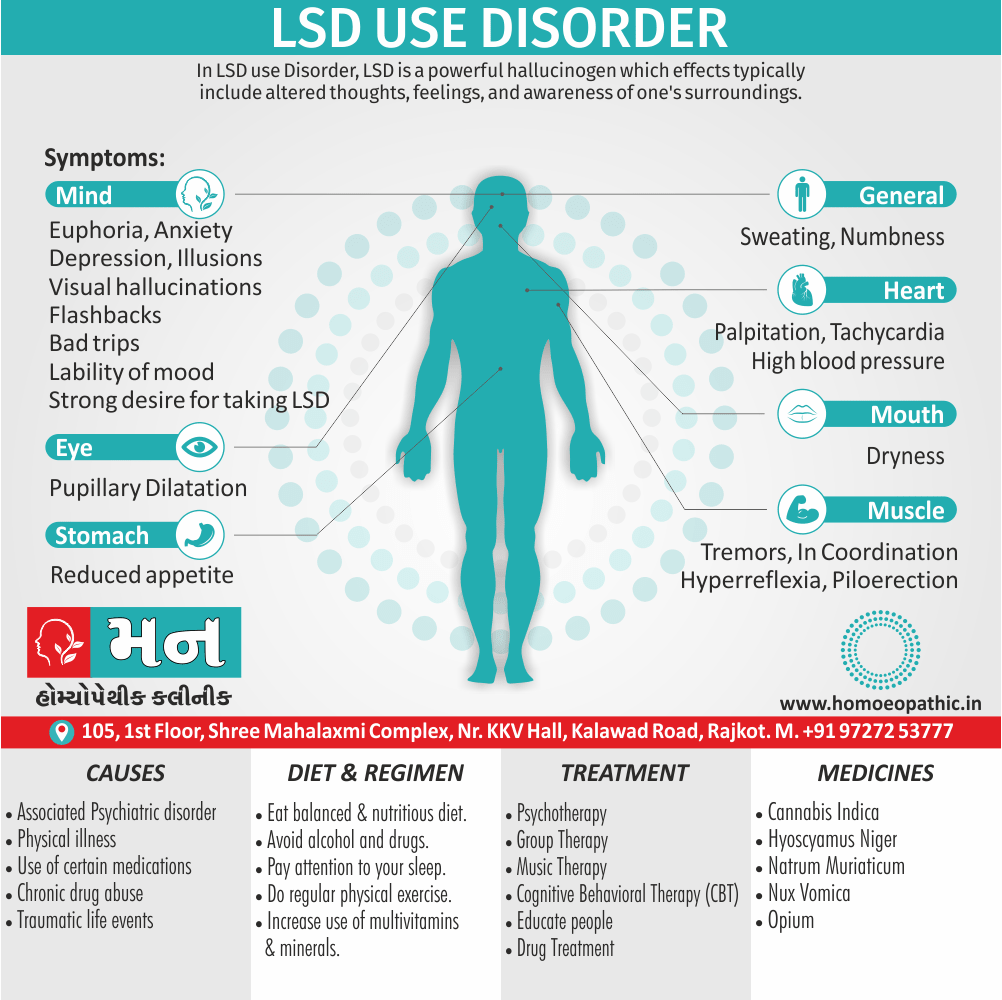
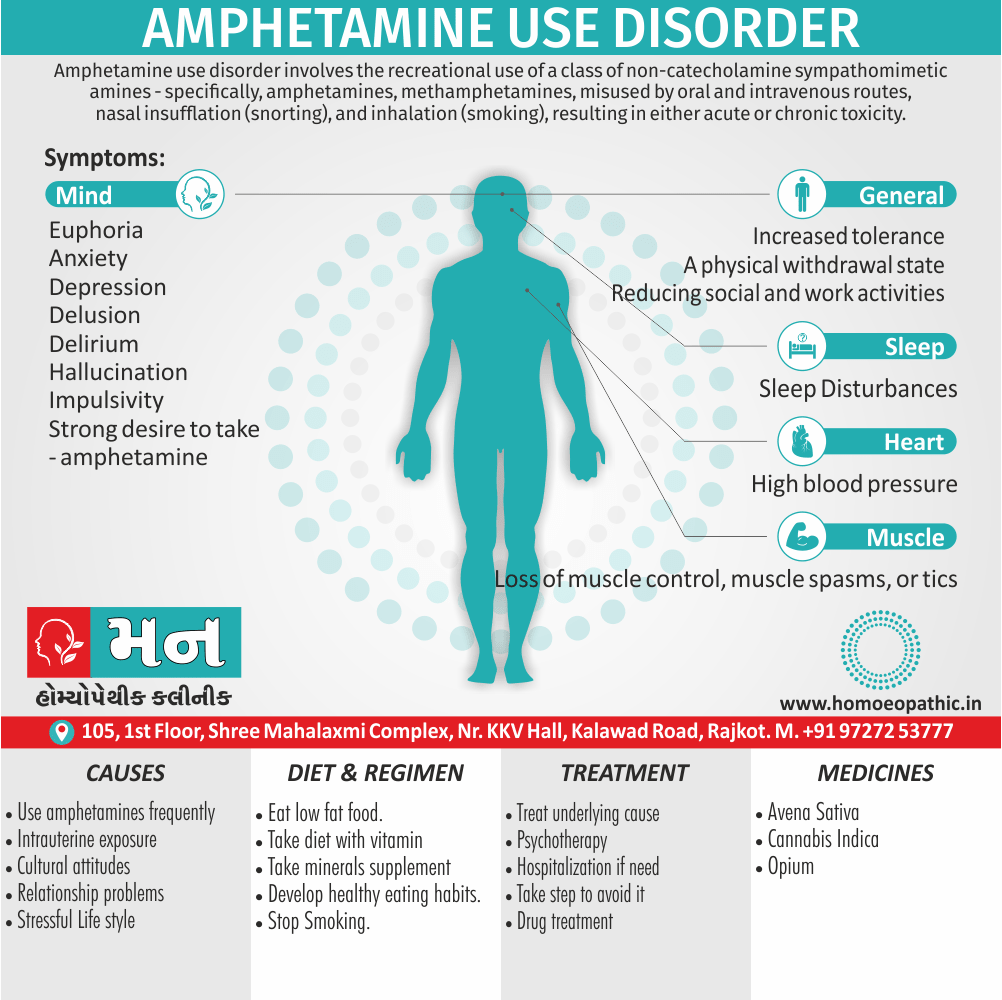
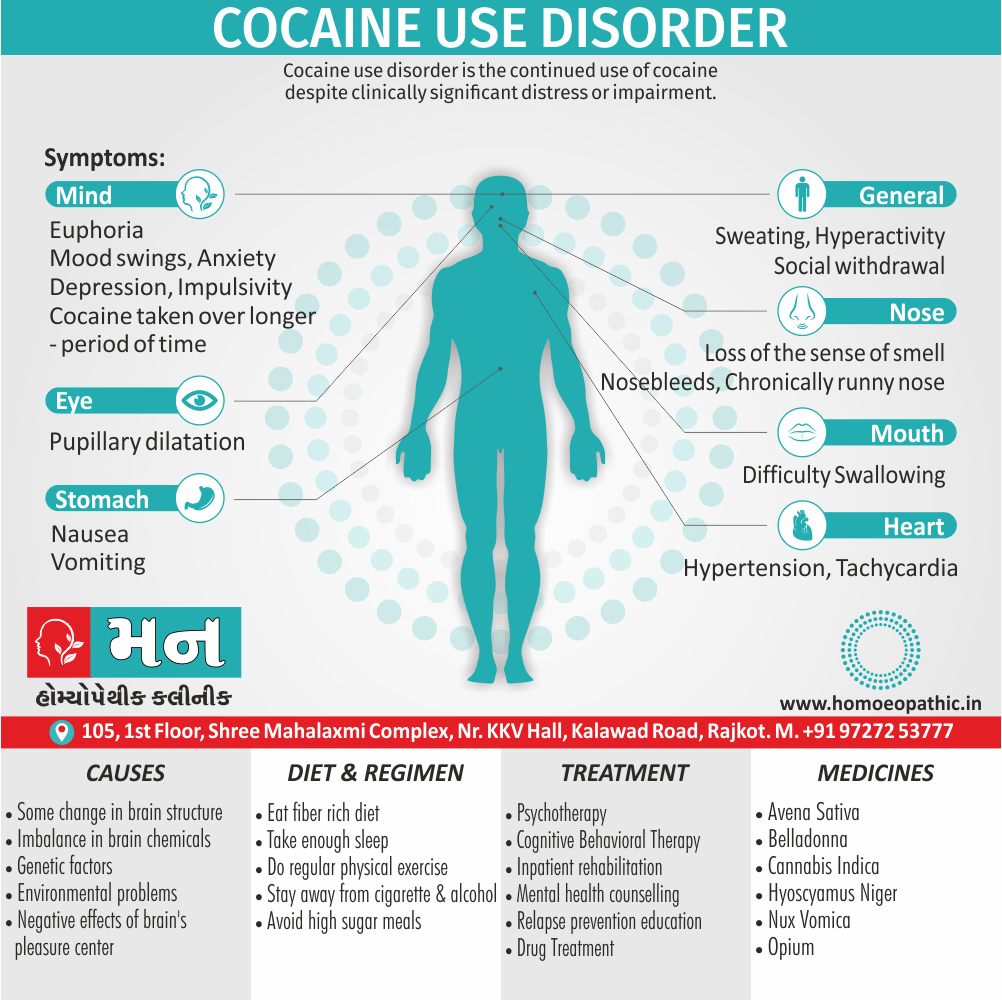
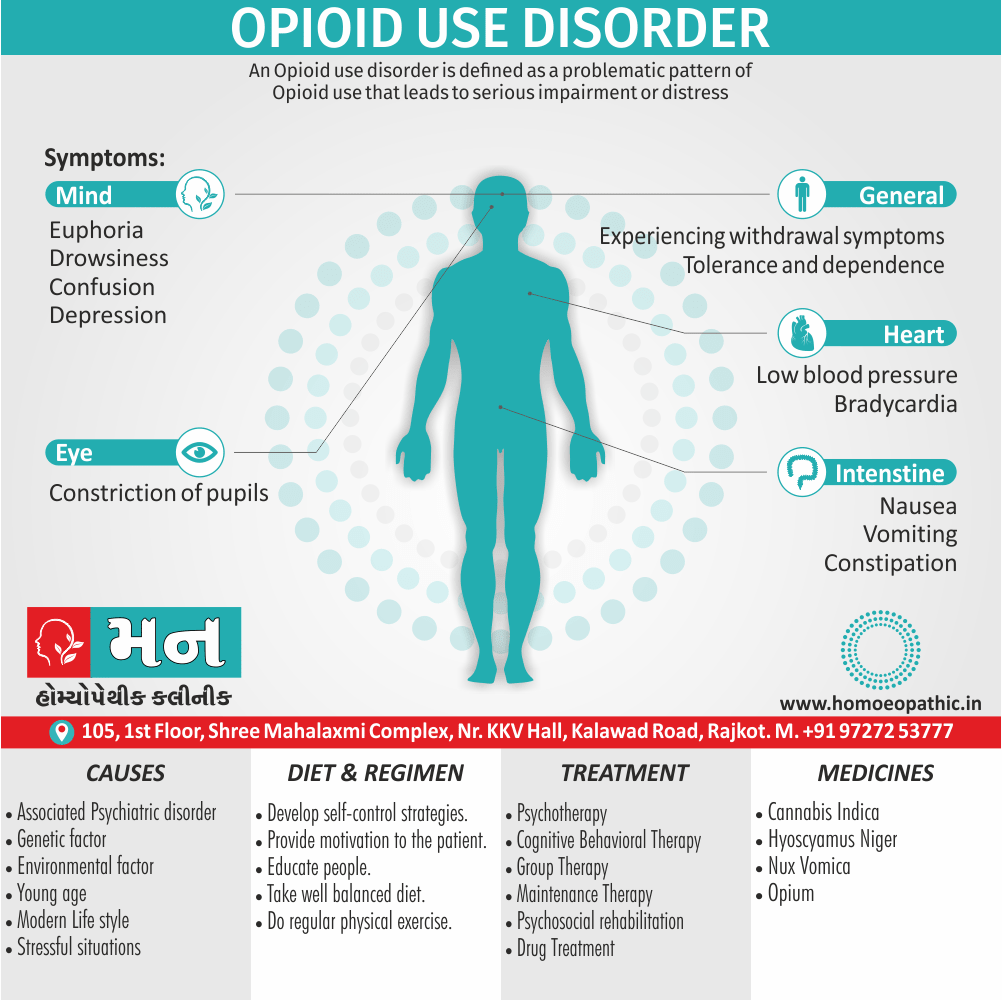
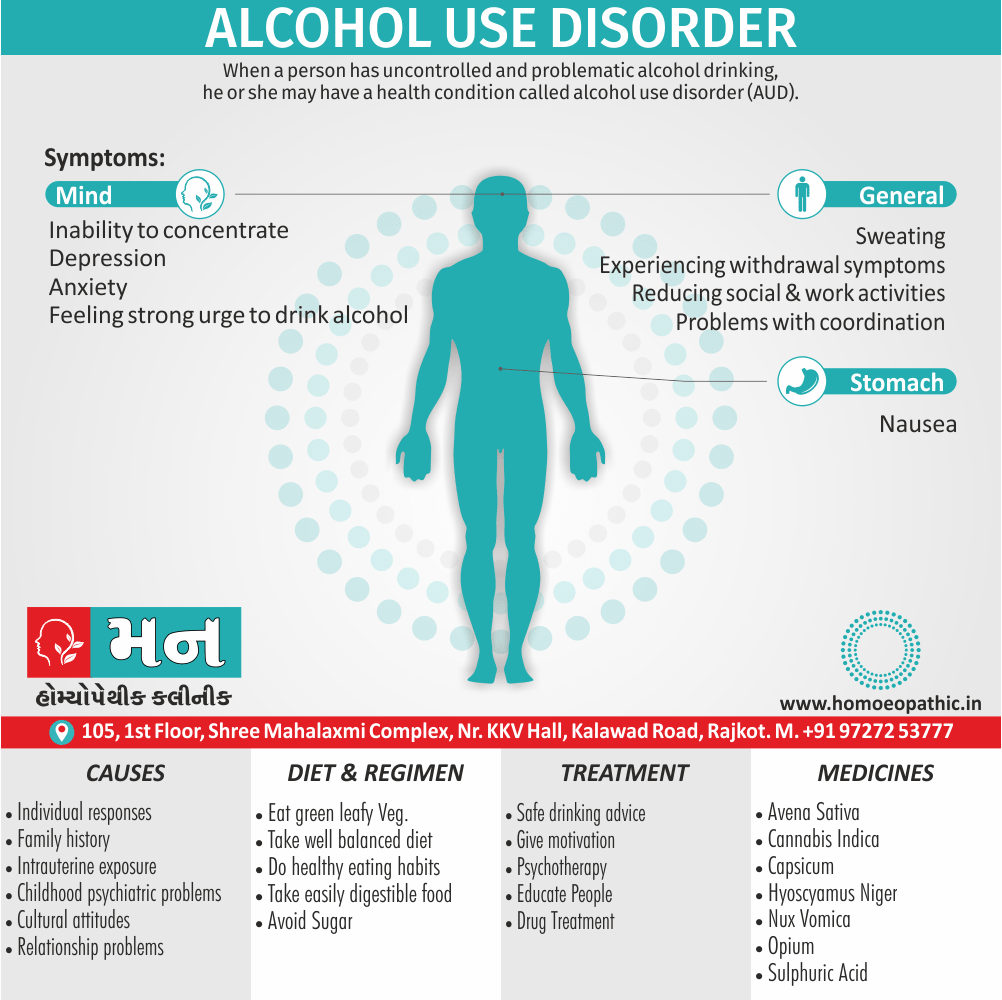
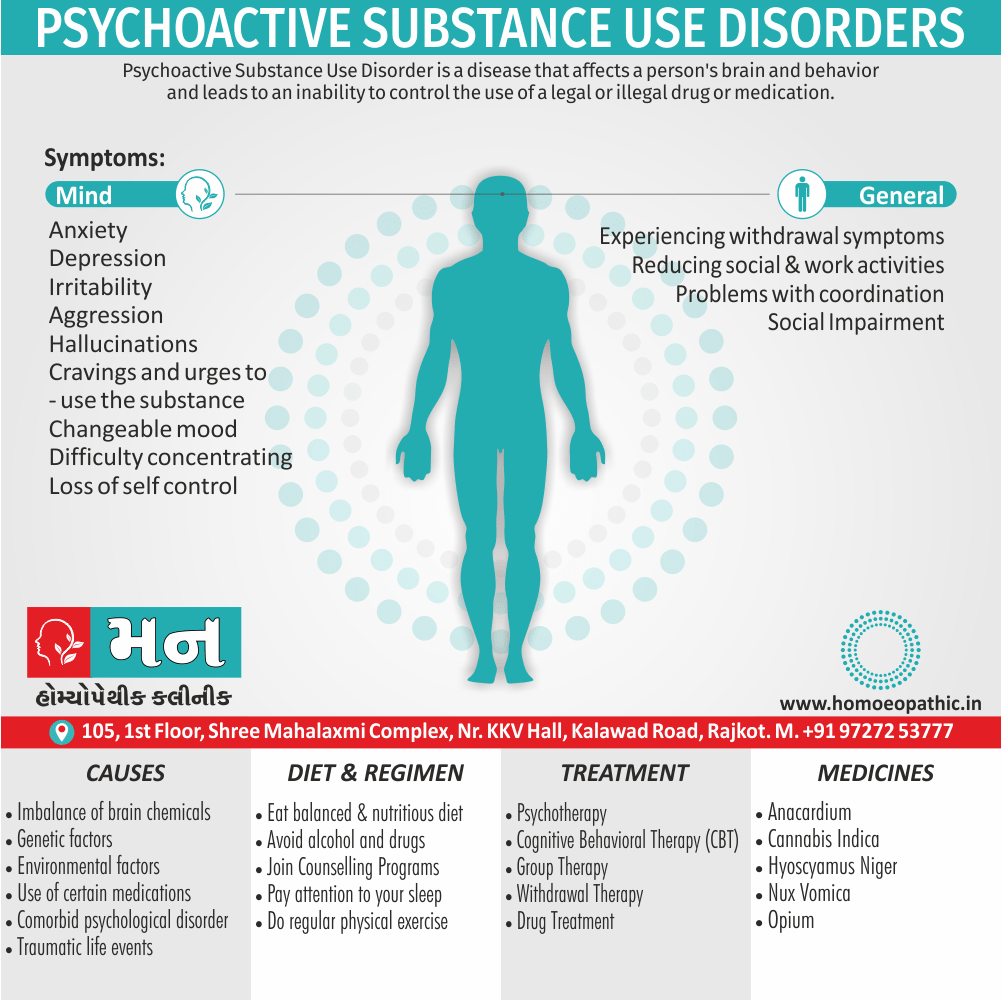
Alcohol and illicit drugs:
The extent of use of alcohol and drugs is note, and in appropriate cases the CAGE questions or the alcohol use disorders identification test are use.
When urgent action is required, the interview has to be brief (focused on the basic points set out above) and effective (leading to a provisional diagnosis and a plan of immediate action).
The information needed includes, at the least, the following points:
- The presenting problem in terms of symptoms or behaviours, together with their onset, course, and present severity;
- Other relevant symptoms with their onset, course, and severity, including an assessment of risks to self (e.g self-harm, suicide, neglect) and others (e.g. assault or homicide, childcare, driving, operating machinery);
- Stressful circumstances around the time of onset and at the present time;
- Previous and current physical or mental disorders and how the patient coped with them;
- Current medicines
- The use of alcohol and illicit drugs
- Family and personal history covered with a few salient questions;
- Social circumstances and the possibilities of support;
- Personality this is valuable, although it may be difficult to obtain this information in the circumstances of an emergency.
If the patient has had previous treatment, efforts should be made to contact a professional who knows the patient.
However short the time, the patient should feel that he has the interviewer’s undivided attention and an opportunity to say everything that is important.
Full Psychiatric History Taking:
Name, age, and address of the patient; name of any informants, and their relationship to the patient.
1. History of presenting problems:
- Patient’s description of the presenting problems; nature, severity, onset, factors that are making the problem worse or better
- Other problems and symptoms
- Treatment received to date
2. Background history:
Family history:
- Parents: age (now or at death), occupation, personality, and relationship with the patient
- Similar information about siblings
- Social position; atmosphere of the home
- Mental disorder in other members of the family, abuse of alcohol/drugs, suicide
Personal history:
- Mother’s pregnancy and birth
- Early development, separation, childhood illnesses
- Educational history
- Occupational history
- Intimate relationships
Social history:
- Living arrangements
- Financial problems
- Alcohol and illicit drug use
- Forensic history
Past medical history
Past psychiatric history
Medicines
Personality
3. Corroborative history
Patient’s description of the presenting problems:
- In this part of Psychiatric History Taking. The interviewer should allow patients adequate time to talk spontaneously before asking questions, otherwise they may not reveal all their problems.
- For example, a patient who begins by describing depression may also have a marital problem that she is hesitant to reveal.
- If the interviewer asks further questions about depression as soon as this is mention, the marital problem may not be revealed.
- To avoid overlooking problems, when patients have finished speaking spontaneously the interviewer should summarize the problems that have been mentioned, and ask if there are any others.
The interviewer’s subsequent questions are designed to understand the following issues:
Nature of the problem:
- For example, a patient who complains of worrying excessively could describing anxiety, obsessional symptoms, or intrusive thoughts occurring in a depressive disorder.
Severity of the problem:
It will be related to
- The amount of distress caused by the problem
- The amount of functional impairment/interference with day-to-day activities
Onset:
- How long ago it started, and whether this was spontaneous (‘out of the blue’) or related to stressful events.
Course of the problem:
- Whether it is static, worsening, improving, or fluctuating in severity, whether it has worsened gradually or in a stepwise fashion, and whether it is present continuously or intermittently.
Factors making the problem worse or better:
- For example, low mood might worse on work days, due to problems at work such as poor relationships with colleagues, and the presence of a supportive relationship at home.
- Alternatively, low mood might better on work days, due to the structure and sense of purpose that work can bring, and the presence of a difficult marital relationship at home.
Other problems and symptoms:
- The interviewer should now enquire about the symptoms and problems that he judges relevant and that have not yet volunteered by the patient.
- These further enquiries are guide by the interviewer’s knowledge of the disorders in which the presenting symptoms and problems can occur.
- For example, if the presenting problem is poor sleep, the interviewer would ask about the symptoms of depressive and anxiety disorders, and about pain, all of which can cause insomnia.
- If the presenting problem is depression, a variety of physical, psychological, and social symptoms should assessed.
- The date of onset and sequence of the various symptoms should also be noted.
- For example, whether obsessional symptoms began before or after depressive symptoms is relevant to diagnosis and treatment.
- The sequence of problems is similarly important, such as whether abuse of alcohol began before or after marital difficulties.
Treatment received to date:
- Finally, a note should made of any treatment already received, its effectiveness or ineffectiveness, side effects and adherence.
- For example, a patient may report that they took fluoxetine for low mood, for about 1 month, but this made them feel anxious and worsened their sleep, so they stopped taking it despite their GP advising them to continue, and that their GP also recommended that they read a named self-help book, but they have not yet obtained this.
Some specific symptoms:
- Pathological depression is a pervasive lowering of mood accompanied by feelings of sadness and a loss of the ability to experience pleasure (anhedonia).
- Pathological elation is a pervasive elation of mood accompanied by excessive cheerfulness, which in extreme cases may experienced as ecstasy.
- Pathologic anxiety is a feeling of apprehension that is out of proportion to the actual situation. This is usually associate with autonomic changes, manifested by pale skin and increased sweating of the hands, feet, and axilla.
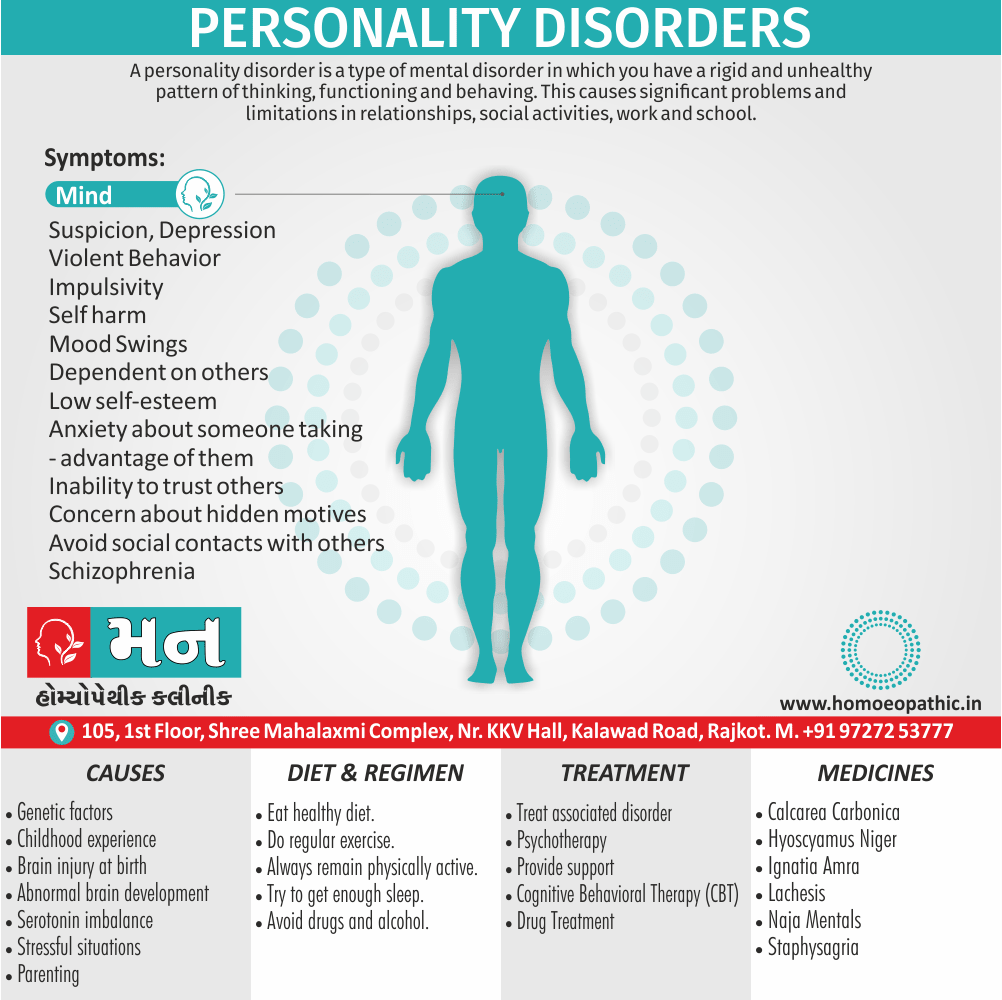
- Depersonalization and derealization are less easy to understand than anxiety and depression because they are less often experienced by healthy people. They are experience occasionally by healthy people, sometimes when they are very tired. They occur as symptoms of many kinds of psychiatric disorder, especially anxiety disorders, depressive disorders, and schizophrenia, and occur also in temporal lobe epilepsy.
- Depersonalization is the experience of being unreal, detached, and unable to feel emotion. Paradoxically, this lack of emotional responsiveness can extremely distressing. People who experience depersonalization often have difficulty in describing it and use similes such as ‘it feels as if I were cut off by a wall of glass’. An ‘as if’ description of this kind must not confused with a delusion, when the person lacks insight into their actual situation.
- Derealization is a similar experience, but occurs in relation to the environment rather than the self: for example, the feeling that other people seem ‘as if made of cardboard’ or that things no longer evoke any emotional response.
This part of Psychiatric History Taking divided into 7 category:
1. Family history:
This part of the background history concerns the patient’s father, mother, siblings, and other relatives.
Enquiries about the patient’s spouse or partner and children are made later.
The family history is important for several reasons:
- Psychiatric disorder in other family members may point to genetic causes.
- Past events in the family, such as the divorce of parents, are the background to the patient’s psychological development.
- Past events in the family may help to explain the patient’s concerns. For example, the discovery that a brother died of a brain tumour may help to explain a patient’s seemingly excessive concerns about headaches.
- Current events in the family may stressful.
- A history of completed suicide in a first-degree relative increases the patient’s risk of suicide.
A useful introduction to this part of the enquiry is:
- ‘I would like to ask about the family into which you were born. Let us start with your father. Is he still alive?’
- If the father is alive, his age, state of health, and job are recorded. If the father has died, the cause of death, and his age and that of the patient at the time of the death should be determined.
- ‘How do you get on now?’ Similar enquiries are made about the mother, siblings, and other important figures in the patient’s early life, such as a stepfather or a grandmother living with the patient.
The amount of detail required varies from case to case.
It is unlikely to profitable to spend time in detail enquiries about the childhood of an older people seeking help for poor memory, but it could highly relevant to obtain this information about a young adult whose behaviour is unusual.
2. Personal history:
The aims in taking the personal history are to describe and understand the following:
- The life story, including any influences that help to explain the patient’s personality, concerns, and preferences. For example, sexual abuse in childhood may help to explain a woman’s low self-esteem and sexual difficulties in adult life, and being the unwanted child of an unaffectionate mother may partly explain a man’s fear of rejection;
- Any stressful circumstances, including how the patient reacted to them.
The amount of detail required to achieve these aims varies from patient to patient.
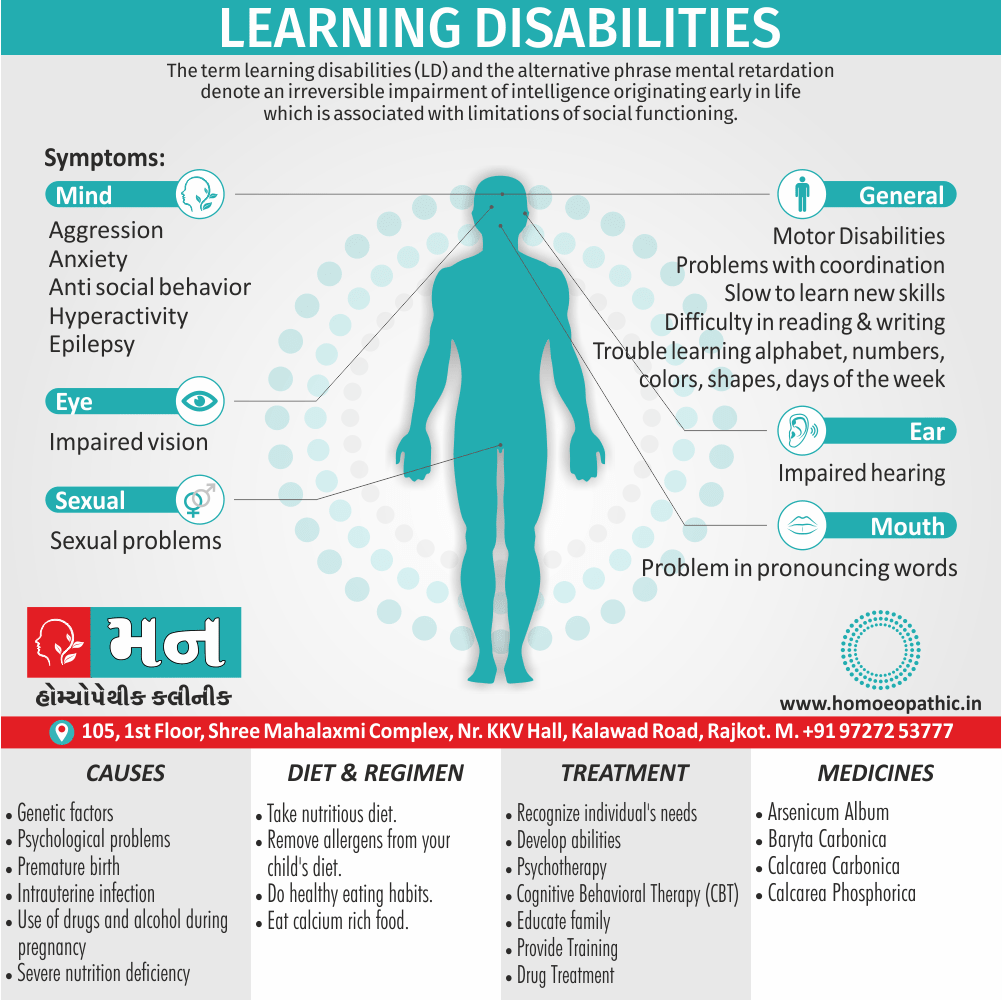
Pregnancy and Birth i.e.:
- The mother’s health during pregnancy and the nature of the patient’s delivery can be important in the context of learning disability.
- Information from the patient may be unreliable and should be checked whenever possible with the mother or with hospital records made at the time of the event.
- In most other cases, it is necessary to enquire only about any major problems.
Early development, separation, and childhood illnesses i.e.:
- The comments above about the relevance and reliability of information about pregnancy and delivery apply equally to developmental milestones, which are seldom important except when the patient is a child or an adult with learning disability.
- A note should be made of any prolonged separation from either parent for whatever reason.
- Since the effects of separation vary considerably, it is important to find out whether the patient was distress at the time and for how long.
- If possible, this information should be checked with the parents.
- Serious and prolonged childhood illnesses may have affected the patient’s emotional development.
- Diseases of the central nervous system in this period may be relevant to learning disability.
Educational History i.e.:
- The history of school and, if applicable, college and university education gives a general indication of intelligence and achievements, and contributes to an understanding of personality.
- As well as academic, artistic, and sporting achievement, enquiries are made about friendships, sociability, aggressive behaviour, bullying, leadership, and relationships with fellow students and with teachers.
Occupational History i.e.:
- The occupational history throws light on abilities and achievements, and on personality.
- Frequent changes of job, failure to gain promotion, or arguments with senior staff may reflect negative aspects of personality (although there are, of course, many other reasons for these events).
- Persistence with jobs or degrees that are poorly rewarded financially, and associate with frustrations and difficulties, may reflect more positive aspects of personality.
Intimate Relationships i.e.:
- This part of the history includes the success and failure of intimate relationships, as well as sexual preferences and behaviour.
- If the patient is sexually active, questions about their attitude to pregnancy and contraception are relevant.
- These are often relevant in patients with mental illness for example, depression is associate with low sexual interest, and antidepressants can have sexual side effects, including delayed orgasm.
- Women should ask about menstrual problems appropriate to their age, including psychological and other symptoms of the premenstrual syndrome and the menopause.
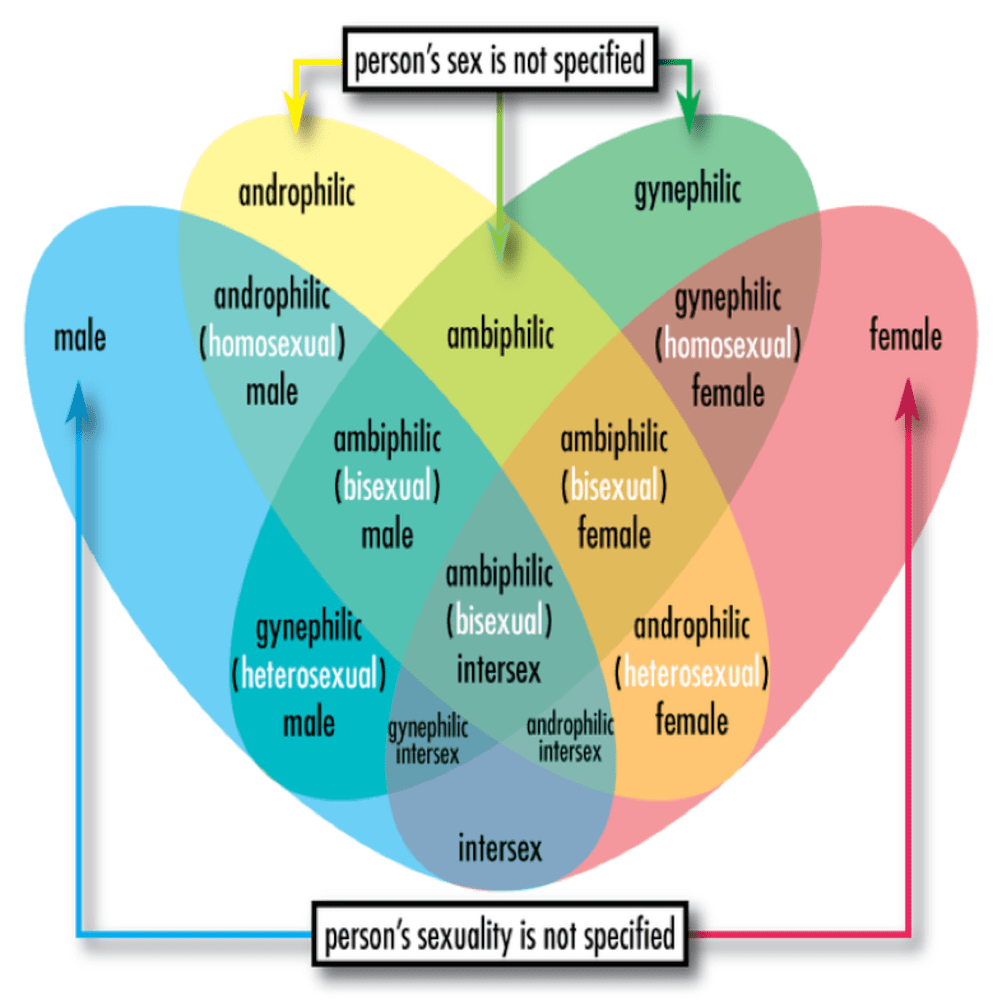
- The interviewer should ask about long-term relationships, including marriage and other partnerships, including same-sex partnerships.
- Ask whether the partnership is happy, how long it has lasted, about the partner’s work and personality, and about the sex, age, parentage, health, and development of any children.
- Similar enquiries are made about any previous partnership(s).
- If the partnership is unhappy, further questions should ask about the nature and causes of this unhappiness, how the couple came together, and any periods of separation or plans for future separation or divorce.
3. Social History in Psychiatric History Taking:
Without the following topics being addressed, an overview of the patient’s problems is not possible.
Living Arrangements i.e.:
- Potentially relevant enquiries include the size and quality of the patient’s home, whether it is owned or rented, who else lives with the patient, and how these people relate to one another, and to the patient.
Financial Problems i.e.:
- Does the patient have financial difficulties and, if so, what kind, and what steps are they taking to deal with them?
Alcohol and illicit drug use i.e.:
- These are often associated with mental disorder, and a careful alcohol and drugs history should take in every case. A screening question will often suffice for illicit drug use.
Forensic History i.e.:
- This concerns behaviour that breaks the law.
- Common sense should use to judge its relevance, but it is important in all cases of alcohol or drug misuse.
- For example, a young man who indulging drinks on Friday and Saturday nights may have convictions for assault and criminal damage while intoxicated with alcohol, and one or more convictions for drink driving, and yet denying that he has an alcohol problem.
- If the patient has a criminal record, note the charges and the penalties, and find out whether other such acts have gone undetected.
4. Past Medical History:
- Medical illnesses, past and current, should be asked about in every case.
- Medical problems are often a cause or a consequence of mental disorder.
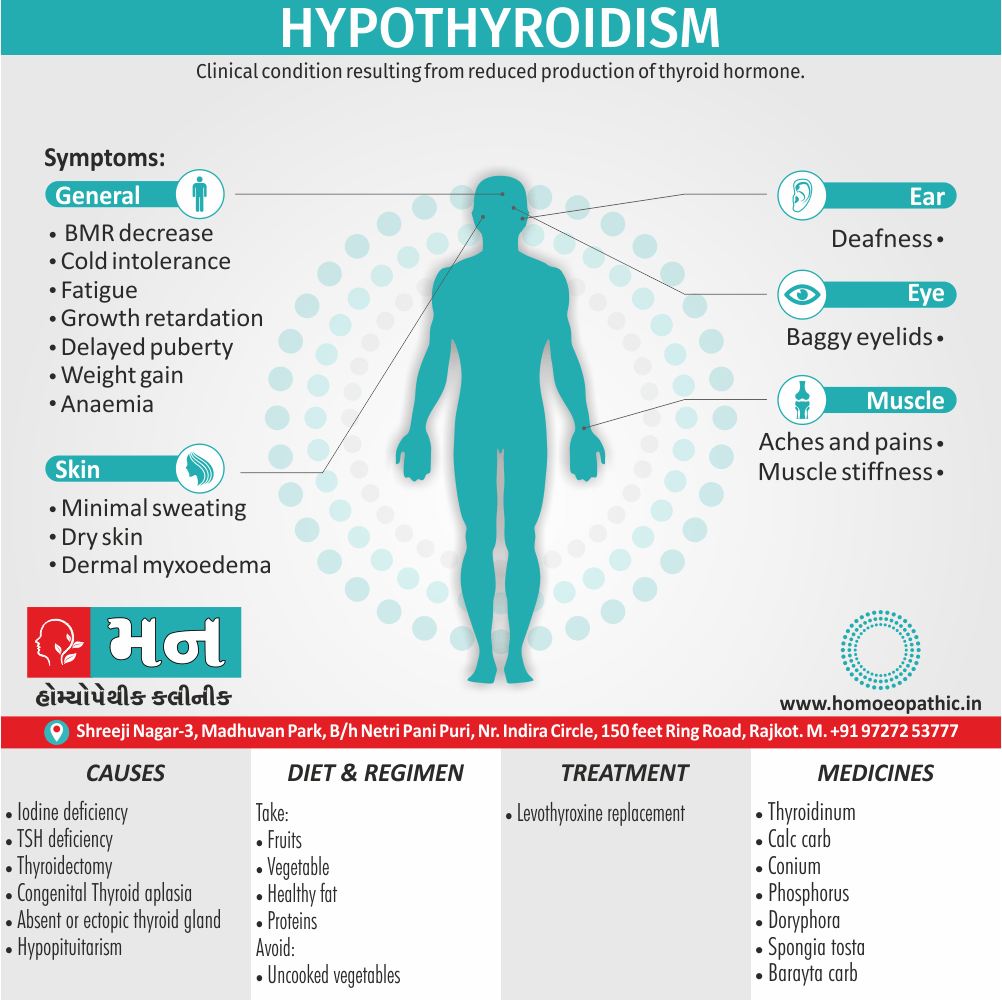
- For example, endocrine disorders such as hypothyroidism are associate with mental illness, and psychiatric medications such as antipsychotics have metabolic side effects.
5. Past psychiatric history:
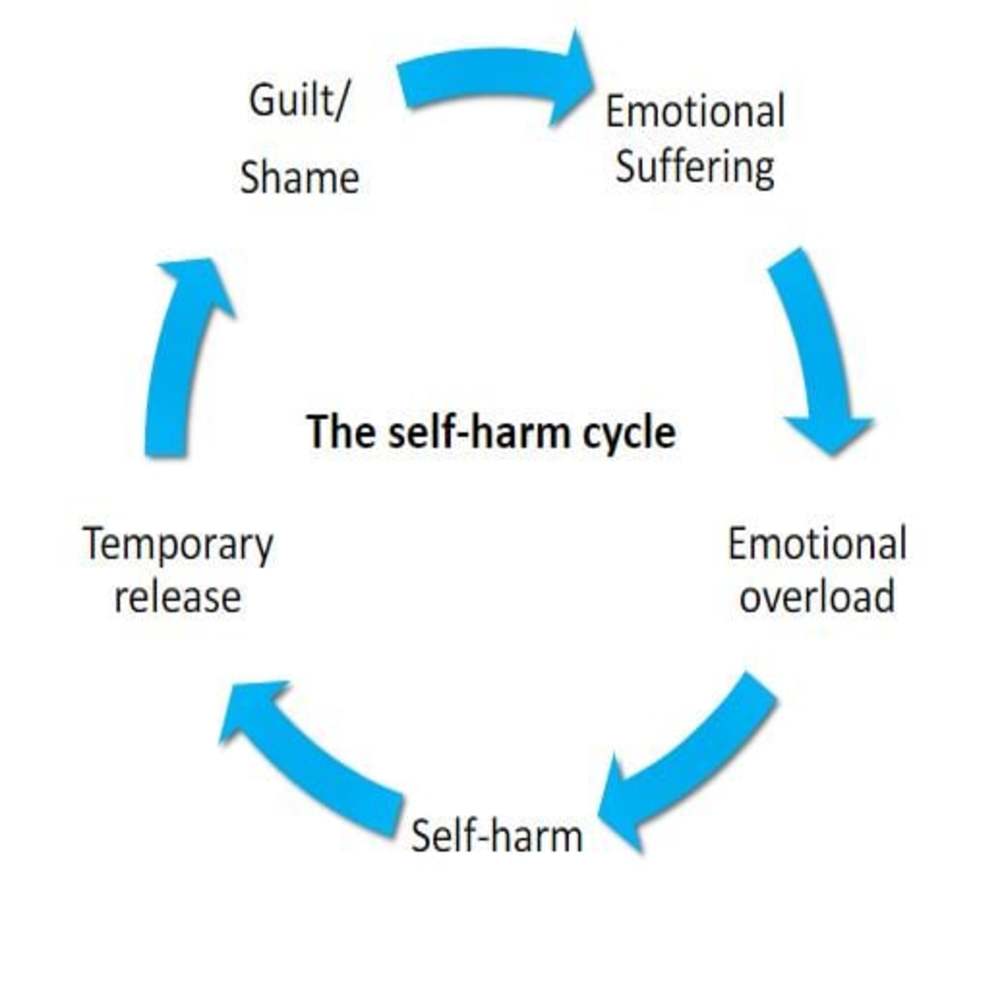
- When there is a past psychiatric history, careful notes should take of the nature of the illness, the number and severity of episodes, any association with risks to self (e.g. self-harm) or to others, including inpatient admission.
6. Medicines:
- A careful medicine history should record.
- Which medicines is the patient taking, at what dose, and at what frequency?
- Does the patient know why they are prescribe?
- Do the patient use tablets prescribed for someone else, such as using a relative’s antidepressants as an occasional pick-me-up, or benzodiazepines to calm nerves?
- Does the patient buy other pills or remedies from the chemist?
7. Personality:
- Enquiries should begin by asking patients to describe their personality.
- Subsequent questions are concern with education, work, social relationships, leisure activities, prevailing mood, character, attitudes and standards, and habits.
- Sometimes the interviewer’s impressions of the patient formed during the interview are useful, but these impressions can misleading, especially when the patient is very distress or suffering from a psychiatric disorder.
- General practitioners are able to build up a picture of their patients’ personalities over years of occasional medical contacts.
This part of Psychiatric History Taking include following information:
What informants can contribute:
In every case informants can provide useful information about the patient’s personality.
Their information is essential when the patient is unable or unwilling to reveal important information, for example when the patient:
- is unaware of the nature and extent of his abnormality (e.g. a demented patient);
- knows the extent of the problem but is unwilling to reveal it (e.g. a patient with an alcohol problem);
- cannot say reliably when the disorder started.
The need for consent:
With few exceptions, the patient’s consent should obtain before interviewing informants.
The interviewer should explain that the interview is to obtain information that will help to decide how best to help the patient, and that information given to the interviewer by the patient will not be revealed to the informant unless the patient has agreed.
The exceptions to the need for consent are when patients cannot provide an adequate history.
Because they are:
- confused, stuporose, extremely foolish, or mute;
- extremely agitated or violent; or
- depending on specific local mental health law, being assessed with a view to detention against their will. A further exception is usually made for children.
Arranging the interview:
- It is generally better to interview relatives or other informants after the interview with the patient.
- It is usually better to see them away from the patient so that they can speak freely: for example, a wife may be reluctant to talk in her husband’s presence about his heavy drinking.
- The purpose of the interview should be explained because relatives sometimes expect that they are about to be blamed for the patient’s problems, or asked to give help that they are not prepared to provide.
Confidentiality:
- Unless informants have agreed to disclosure, the interviewer should not tell the patient what they have said.
- This rule applies even when the relative has spoken of something that the interviewer needs to discuss with the patient, such as heavy drinking that has been denied.
- If the relative has refused permission for the information to be disclosed, the interviewer can only try to help the patient reveal the information himself.
- In view of this and because patients may ask to see their case notes, it is better to record the interview with the informant on a separate sheet.
The informants’ concerns:
- As well as asking for information about the patient, the interviewer should find out how the informants view the problem, how it affects them, and what help they are seeking.
Helping the informants:
- When the interview with informants reveals that they too have emotional problems, either as a result of the patient’s illness or for other reasons, the interviewer should either offer help or assist them to obtain help from another professional.
Frequently Asked Questions
How do you take History of Psychiatric patient?
- History of the presenting problems
- Background history
- Family history
- Personal history
- Social history
- Past medical history
- Past psychiatric history
- Medicines
- Personality
- Corroborative history
What are the 7 categories of Background History?
- Family history
- Personal history
- Social History
- Past Medical History
- Past psychiatric history
- Medicines
- Personality
What is presenting problems?
In this part of Psychiatric History Taking The interviewer should allow patients adequate time to talk spontaneously before asking questions, otherwise they may not reveal all their problems.
Name of the 5 domains which are helpful during screening interview?
- General well-being
- Anxiety
- Depression
- Memory
- Alcohol and illicit drugs