Functional Enuresis
Definition
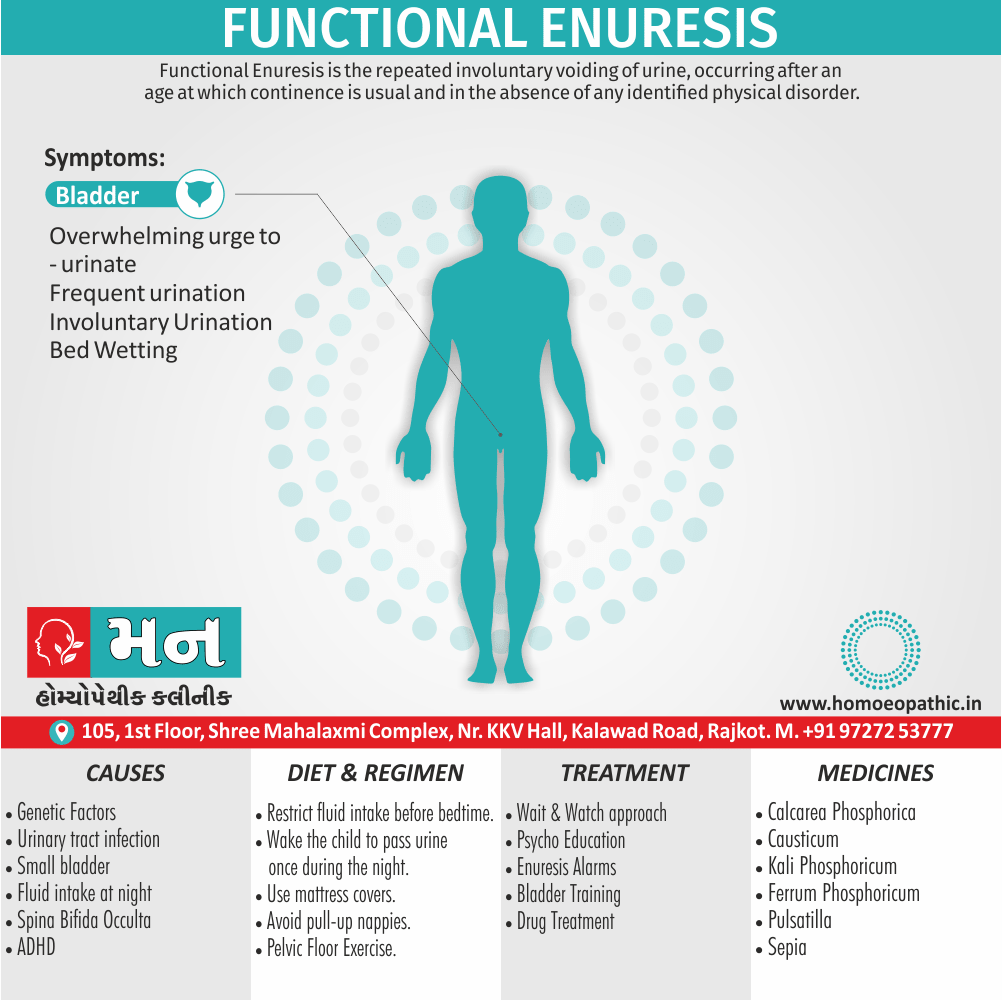
Functional Enuresis is the repeated involuntary voiding of urine, occurring after an age at which continence is usual and in the absence of any identified physical disorder. [1]
While there aren’t direct synonyms for "functional enuresis," here are some related terms you might find useful:
- Primary nocturnal enuresis: This describes bedwetting that occurs at night in a child who has never achieved bladder control.
- Non-monosymptomatic nocturnal enuresis: This refers to bedwetting at night that occurs alongside other lower urinary tract symptoms like daytime incontinence, urgency, or frequency.
- Idiopathic nocturnal enuresis: This term indicates bedwetting at night for which there is no identifiable medical cause.
These terms all share some characteristics with functional enuresis, but they may have slightly different nuances.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
The condition may be nocturnal (bed-wetting), diurnal (occurring during waking hours), or both.
Nocturnal enuresis is referred to as primary if there has been no preceding period of urinary continence, and secondary if there has been a preceding period of urinary continence.
There is no absolute period of continence needed to become secondary enuresis, but 6 months is a commonly used time frame.
Most children achieve regular daytime and night-time continence by 3 or 4 years of age, and 5 years is generally taken as the youngest age for the diagnosis.
Nocturnal enuresis can cause great unhappiness and distress, particularly if the parents blame or punish the child, and if the condition restricts staying with friends or going on holiday.
Nocturnal enuresis occurs in about;
- 10 % of children at 5 years of age,
- 4 % at 8 years,
- 1 % at 14 years,
- 0.5 % in adulthood.
The condition is more frequent in boys. [1]
Daytime enuresis has a lower prevalence and is more frequent in girls.
Epidemiology
Epidemiology
The epidemiology of functional enuresis (FE) in India is characterized by a prevalence rate ranging from 7% to 15% among children aged 5 to 10 years, with the numbers decreasing to 3% to 5% by the age of ten. This data comes from a study published in the Indian Journal of Clinical Pediatrics in 2018 titled "Prevalence of nocturnal enuresis among children aged 05 to 10 years" (1).
Additional studies in India have also explored the prevalence and factors associated with enuresis:
- A study published in the Indian Journal of Physiotherapy and Occupational Therapy in 2018 found prevalence rates of 12.6% and 11.3% in rural school children (2).
- Another study published in the Journal of Indian Association for Child and Adolescent Mental Health in 2011 found a prevalence of 7.61% among primary school children aged 6-10 years (3).
These studies highlight the importance of addressing enuresis in India, as it can significantly impact a child’s psychological well-being and quality of life. Further research is needed to better understand the underlying causes of enuresis in the Indian population and to develop effective treatment strategies.[3][4][5]
References:
- Prevalence of nocturnal enuresis among children aged 05 to 10 years (Indian Journal of Clinical Pediatrics, 2018)
- (PDF) Prevalence of Nocturnal Enuresis in 6–15 Years School Children and its Awareness among Parents in Dharwad – ResearchGate
- Prevalence and factors affecting enuresis amongst primary school children – ResearchGate
Causes
Causes
The majority of cases of nocturnal primary enuresis are idiopathic; there is simply a delay in maturation of the nervous system controlling the bladder.
These children often have a family history of enuresis, as children who have either one or two parents who were enuretic have a 44 and 70 % chance, respectively, of being enuretic themselves.
There are a range of other causes of enuresis, but these are more commonly associated with secondary nocturnal or diurnal enuresis.
Common causes of nocturnal primary enuresis:
- Idiopathic developmental delay
- Genetics
Less common causes of enuresis (consider in secondary nocturnal or diurnal cases):
- Urinary tract infection
- Diabetes mellitus
- Abnormalities of the urinary tract (e.g. small bladder, vesicoureteric reflux)
- Structural abnormalities of the nervous system (e.g. spina bifida occulta)
- Chronic constipation
- Diuretics: e.g. caffeine, alcohol
- ADHD
- Learning disorders or syndromes of developmental delay
- Behavioural: being too engaged in play or ‘leaving it too late’
- Psychological: i.e. a response to bereavement, stress, abuse, or bullying
- Obstructive sleep apnoea
- Epilepsy [1]
Other Causes:
- Fluid intake at night.
- The bladder is irritated by the bowels.
- Inability to know if the bladder is filled.
- Urinary tract infection.
- Stress also anxiety.
- Hyperactivity in children.
- Lack of attention.
Types
Types
Functional enuresis (FE) can be classified into two main types:
Monosymptomatic nocturnal enuresis (MNE):
This is the most common type, characterized by bedwetting only during sleep without any other lower urinary tract symptoms (LUTS) during the day.
Non-monosymptomatic nocturnal enuresis (NMNE):
This type includes bedwetting during sleep along with other LUTS during the day, such as urgency, frequency, or daytime incontinence.
This comprehensive textbook Clinical Pediatric Nephrology provides a detailed discussion of the different types of functional enuresis, their clinical presentation, diagnostic evaluation, and management strategies. The authors highlight the importance of differentiating between MNE and NMNE as it can guide the selection of appropriate treatment approaches.[6]
Risk Factors
Risk factors
The risk factors for functional enuresis (FE) can be classified into several categories:
Genetic Predisposition:
- A strong family history of enuresis is a major risk factor. If one parent had enuresis, the child’s risk is 44%, and if both parents had it, the risk increases to 77%.
- Certain gene variations have been linked to FE, particularly those affecting the production or response to antidiuretic hormone (ADH), which regulates urine production.
Sleep-Related Factors:
- Deep sleep and difficulty awakening in response to bladder signals can contribute to enuresis.
- Sleep disorders like obstructive sleep apnea may worsen enuresis due to disturbed sleep patterns.
Bladder and Urinary Tract Factors:
- Reduced functional bladder capacity, bladder overactivity, or delayed bladder maturation can increase the risk.
- Urinary tract infections may temporarily trigger enuresis.
Psychological and Social Factors:
- Stressful life events, family conflicts, or emotional problems can contribute to or worsen enuresis.
- Children with attention-deficit/hyperactivity disorder (ADHD) or other neurodevelopmental disorders are at higher risk.
Other Factors:
- Constipation can put pressure on the bladder and contribute to enuresis.
- Excessive fluid intake before bedtime can increase urine production during sleep.
This textbook Clinical Pediatric Nephrology provides a detailed discussion of the various risk factors associated with functional enuresis. The authors emphasize that the risk factors often interact and contribute to the development of enuresis in a complex manner. Understanding these risk factors is crucial for identifying children at risk and implementing appropriate preventive and treatment strategies.[6]
Pathogenesis
Pathogenesis
The pathogenesis of functional enuresis (FE) is multifactorial and involves a complex interplay of various factors. A comprehensive discussion on this topic can be found in the book "Clinical Pediatric Nephrology" by Ellis D. Avner, William E. Harmon, and Patrick Niaudet.
Pathogenesis:
The book outlines several key factors contributing to the pathogenesis of functional enuresis:
- Nocturnal Polyuria: Increased urine production during sleep due to inadequate suppression of antidiuretic hormone (ADH) or decreased renal responsiveness to ADH.
- Bladder Dysfunction: Reduced functional bladder capacity or bladder overactivity during sleep, leading to involuntary detrusor contractions and urgency.
- Sleep Arousal Dysfunction: Difficulty awakening from sleep in response to bladder signals, resulting in a failure to void appropriately.
- Genetics: A strong genetic predisposition is observed in functional enuresis, with a higher risk in children with a family history of the condition.
The book also discusses other potential contributing factors like constipation, psychological stress, and urinary tract infections. It emphasizes the importance of a comprehensive evaluation to identify the specific underlying causes in each individual and tailor the treatment accordingly.[6]
Pathophysiology
Pathophysiology
The pathophysiology of functional enuresis (FE) is multifactorial and involves a complex interplay of various factors. A comprehensive discussion on this topic can be found in the following book:
- Book: Clinical Pediatric Urology
Pathophysiology of Functional Enuresis:
The book outlines several key factors contributing to the pathophysiology of functional enuresis:
Nocturnal Polyuria:
Increased urine production during sleep due to inadequate suppression of antidiuretic hormone (ADH) or decreased renal responsiveness to ADH.
Bladder Dysfunction:
Reduced functional bladder capacity (small bladder) or bladder overactivity (overactive bladder) during sleep, leading to involuntary detrusor contractions and urgency.
Sleep Arousal Dysfunction:
Difficulty awakening from sleep in response to bladder signals, resulting in a failure to void appropriately.
Genetic Predisposition:
A strong genetic component is observed in functional enuresis, with a higher risk in children with a family history of the condition.
The book also discusses other potential contributing factors like constipation, psychological stress, and urinary tract infections. It emphasizes the importance of a comprehensive evaluation to identify the specific underlying causes in each individual and tailor the treatment accordingly.[7]
Clinical Features
Clinical Features
The clinical features of functional enuresis (FE) can be summarized as follows:
Primary Nocturnal Enuresis (PNE):
- Recurrent involuntary urination during sleep in a child who has never been consistently dry at night.
- Onset usually occurs before age 5.
- More common in boys.
- No associated daytime bladder symptoms.
Secondary Nocturnal Enuresis (SNE):
- Recurrent involuntary urination during sleep in a child who has previously been dry for at least six months.
- Onset typically occurs after age 5.
- May be associated with daytime bladder symptoms or other medical conditions.
Monosymptomatic Nocturnal Enuresis (MNE):
- Bedwetting without any other lower urinary tract symptoms (LUTS) during the day.
Non-monosymptomatic Nocturnal Enuresis (NMNE):
- Bedwetting with other LUTS during the day, such as urgency, frequency, or daytime incontinence.
This comprehensive textbook Clinical Pediatric Urology provides a detailed discussion of the clinical presentation and diagnostic evaluation of functional enuresis. The authors emphasize the importance of a thorough history and physical examination to differentiate between the different types of enuresis and identify any underlying medical conditions.[7]
Sign & Symptoms
Sign And Symptoms
The symptoms of bladder dysfunction include:
1. Urge incontinence:
In detail, The presence of an overwhelming urge to urinate, frequent urination, attempts to hold the urine and urinary tract infections.
2. Voiding postponement:
Delaying urination in certain situations such as school.
3. Stress incontinence:
Generally, Incontinence that occurs in situations when increased intra-abdominal pressure occurs such as coughing.
4. Giggling incontinence:
Basically, Incontinence that occurs when laughing.
Secondary incontinence usually occurs in the context of a new life event that is stressful such as abuse or parental divorce. [2]
Clinical Examination
Clinical Examination
The clinical examination for functional enuresis (FE) typically involves a comprehensive assessment to identify any underlying causes and rule out other medical conditions. This includes:
Physical Examination:
- Abdominal examination: Palpation to assess for a distended bladder or fecal impaction (constipation).
- Genital examination: To rule out anatomical abnormalities or signs of infection.
- Neurological examination: Assessment of reflexes, gait, and sensation to exclude neurological causes.
Voiding Diary:
- Parents/caregivers are asked to record the child’s fluid intake, voiding frequency, and episodes of enuresis over a few days.
- This helps assess voiding patterns and identify any potential triggers.
Additional Tests (if indicated):
- Urinalysis: To rule out infection or other urinary abnormalities.
- Uroflowmetry: Measures the rate of urine flow, helping to assess bladder function.
- Ultrasound: To visualize the kidneys, bladder, and ureters for any structural abnormalities.
This comprehensive urology textbook- Campbell-Walsh-Wein Urology provides a detailed overview of the clinical examination and diagnostic evaluation of enuresis in children. It emphasizes the importance of a thorough assessment to identify any underlying causes and tailor the treatment plan accordingly.[8]
Diagnosis
Diagnosis
The diagnosis of functional enuresis (FE) primarily relies on a detailed medical history, physical examination, and exclusion of other potential causes.
Diagnostic Criteria:
According to the International Children’s Continence Society (ICCS), the diagnostic criteria for FE include:
- Chronological or developmental age of at least 5 years.
- Recurrent involuntary urination during sleep (at least twice a week for three consecutive months).
- Absence of other underlying medical conditions (e.g., urinary tract infection, neurological disorders).
This comprehensive textbook- Clinical Pediatric Urology provides a detailed overview of the diagnostic process for functional enuresis. The authors emphasize the importance of a thorough history and physical examination to:
- Differentiate between primary and secondary enuresis.
- Identify any associated daytime symptoms (urgency, frequency, daytime incontinence).
- Rule out other potential causes like urinary tract infections, constipation, diabetes, or neurological disorders.
Additional Diagnostic Tests:
In some cases, additional tests may be recommended to further evaluate bladder function or rule out other conditions:
- Voiding diary: To track fluid intake, voiding patterns, and episodes of enuresis.
- Urinalysis: To check for infection or other urinary abnormalities.
- Ultrasound: To visualize the urinary tract for any structural abnormalities.
- Uroflowmetry: To measure the rate of urine flow.
By following these diagnostic steps and utilizing the information provided in the reference textbook, healthcare professionals can accurately diagnose functional enuresis and develop appropriate treatment plans for affected children.[7]
Differential Diagnosis
Differential Diagnosis
The differential diagnosis for functional enuresis (FE) involves ruling out other medical conditions that can cause or contribute to bedwetting. This includes:
Organic Causes:
- Urinary Tract Infections (UTIs): Can cause urgency, frequency, and bedwetting.
- Diabetes Mellitus or Insipidus: Increased urine production due to high blood sugar or hormonal imbalances.
- Constipation: Fecal impaction can press on the bladder, reducing its capacity.
- Anatomical Abnormalities: Structural problems in the urinary tract (e.g., posterior urethral valves) can obstruct urine flow.
- Neurological Conditions: Conditions affecting bladder control (e.g., spinal cord injury) can lead to enuresis.
Sleep Disorders:
- Obstructive Sleep Apnea (OSA): Disturbed sleep patterns can disrupt normal bladder function.
- Parasomnias: Sleepwalking or sleep terrors can be associated with bedwetting.
Psychological Factors:
- Stress and Anxiety: Emotional distress can trigger or worsen enuresis.
- Behavioral Problems: Attention-deficit/hyperactivity disorder (ADHD) or other behavioral issues can increase the risk.
This comprehensive pediatric textbook-Nelson Textbook of Pediatrics provides a detailed discussion of the differential diagnosis for enuresis, emphasizing the importance of ruling out other medical conditions before establishing a diagnosis of functional enuresis. The authors highlight the need for a thorough medical history, physical examination, and appropriate diagnostic tests to identify any underlying causes and guide treatment.[9]
Complications
Complications
While functional enuresis (FE) itself is not a life-threatening condition, it can lead to several complications, mainly psychosocial in nature.
These complications include:
Emotional Distress:
Feelings of shame, embarrassment, guilt, low self-esteem, and anxiety are common in children with enuresis. This can affect their social interactions, school performance, and overall well-being.
Social Isolation:
Children with enuresis may avoid sleepovers, camps, or other social activities due to fear of embarrassment. This can lead to social isolation and difficulty forming relationships.
Family Stress:
Enuresis can be a source of stress for the entire family, impacting family dynamics and parent-child relationships.
Behavioral Problems:
Some children with enuresis may develop behavioral problems, such as oppositional defiant disorder or attention deficit hyperactivity disorder (ADHD), as a way to cope with the emotional stress.
In rare cases, untreated enuresis may lead to physical complications, such as:
Urinary Tract Infections (UTIs):
Repeated episodes of bedwetting can increase the risk of UTIs.
Skin Problems:
Prolonged exposure to urine can cause skin irritation or rashes.
This comprehensive textbook-Clinical Pediatric Urology discusses the psychosocial and physical complications associated with functional enuresis. The authors emphasize the importance of early diagnosis and treatment to prevent these complications and improve the child’s quality of life.[7]
Investigations
Investigation
The investigation of functional enuresis (FE) aims to identify the underlying cause and rule out other medical conditions. The following investigations are typically recommended:
Detailed History:
- Age of onset and duration of enuresis
- Frequency and pattern of bedwetting episodes
- Daytime voiding symptoms (frequency, urgency, hesitancy, straining)
- Family history of enuresis or other voiding disorders
- Sleep patterns and any associated sleep disorders
- Medical history, including medications and previous treatments
- Psychosocial history, including stress, anxiety, or behavioral problems
Physical Examination:
- Abdominal examination (to assess for bladder distention or constipation)
- Genital examination (to rule out anatomical abnormalities)
- Neurological examination (to assess reflexes, gait, and sensation)
Additional Investigations (if indicated):
- Voiding Diary: To track fluid intake, voiding frequency, and episodes of enuresis over several days.
- Urinalysis: To rule out urinary tract infections or other abnormalities.
- Urine Culture: To identify specific bacteria causing a UTI.
- Blood Tests: To check for diabetes or other underlying medical conditions.
- Ultrasound: To visualize the kidneys, ureters, and bladder for structural abnormalities.
- Urodynamic Studies: To assess bladder function and identify any abnormalities in bladder storage or emptying.
This comprehensive textbook– Clinical Pediatric Urology provides a detailed discussion on the investigation of functional enuresis, outlining the steps involved and the rationale behind each investigation. The authors emphasize the importance of a systematic approach to identify the underlying cause and guide appropriate treatment.[7]
Treatment
Treatment
Assessment
- The majority of children who are bedwetting at 5 years will outgrow it in the next 2 years.
- Therefore, a watching and waiting approach is often the best option in this period.
- Many clinicians do not start to treat enuresis until 7 years unless it is causing functional, psychological, or social impairment.
- Most cases of primary enuresis can treat successfully in general practice.
Psychoeducation:
- The parents and their child should reassure that enuresis is common and the child is not to blame.
- The parents should told that punishment and disapproval are inappropriate and ineffective, and that they should reward success (e.g. with star charts), and not focus attention on failure.
- Reinforcing positives helps to increase self-esteem and also is a powerful tool in changing behaviour.
Practical advice:
Parents can be advised to:
- Restrict fluid intake before bedtime;
- Wake the child to pass urine once during the night;
- Use mattress covers;
- Avoid pull-up nappies (these can prolong the problem).
Enuresis alarms:
- A sensor to detect urine attached to the child’s pyjama trousers and a miniature alarm carry in the pocket or on the wrist.
- The child turns off the alarm and rises to complete emptying the bladder while the bed remade if necessary.
- In the past, before the necessary sensors were available, the passage of urine detect by two metal plates separated by a cotton pad.
- When the pad became wet, the current flowed and an alarm bell rang.
- The term pad and bell method is still in use to describe this approach to treatment.
- About 70 % of children improve within a month of this treatment, but a third relapse within a year.
Medication:
- The synthetic antidiuretic hormone analogue desmopressin (in other words, DDAVP) acts to reduce urine production whilst the child is asleep, and is effective at producing dry nights in 50 percent of children.
- It is available as an oral tablet or as a nasal spray, which is preferred by most children.
- Unfortunately, desmopressin has only a short-term effect and most children relapse as soon as they stop taking it.
- However, it can a useful method of allowing a child to attend a sleepover or camp.
- Tricyclic antidepressants, especially imipramine, are effective at reducing bedwetting when given at a low dose.
- Most children improve partially on the drug, and about a third stop completely, although most relapse when the drug stop.
- Because of this high relapse rate, the side effects of tricyclics, and the potential danger of accidental overdose, the use of antidepressant drugs limit mainly to enabling the child to dry over a short but important period, such as a school journey.
- It has a very limited longer-term role in those with persistent enuresis whose social, educational, or psychological development is being adversely affected by it.
Bladder training and pelvic floor exercises. [1]
Prevention
Prevention
While primary functional enuresis (PNE) cannot be entirely prevented, there are several strategies that can help reduce the risk or minimize the severity of bedwetting episodes:
Early Toilet Training:
Encourage toilet training during the day and establish a regular voiding schedule. Positive reinforcement and patience are key to successful toilet training.
Limiting Fluids Before Bedtime:
Avoid giving your child fluids in the two hours leading up to bedtime.
Encouraging Regular Voiding:
Remind your child to empty their bladder before bed and upon waking in the morning.
Positive Reinforcement:
Praise and reward your child for dry nights. Avoid punishment or shaming for wet nights, as this can worsen anxiety and stress.
Addressing Constipation:
If your child is constipated, address the issue with dietary changes, increased fluid intake, and/or laxatives as recommended by a healthcare professional.
Managing Stress:
If your child is experiencing stress or anxiety, provide emotional support and consider seeking professional help if necessary.
Treating Underlying Medical Conditions:
If enuresis is secondary to another medical condition (e.g., sleep apnea), treating the underlying condition can improve or resolve bedwetting.
This comprehensive textbook-Developmental-Behavioral Pediatrics discusses various strategies for preventing and managing enuresis in children. It emphasizes the importance of a multi-faceted approach that addresses both behavioral and medical factors. The authors also provide guidance on when to seek professional help for persistent or severe enuresis.[10]
Homeopathic Treatment
Homeopathic Treatment
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
The remedies contained in this preparation bring about an improvement in nervous and debilitated constitutions. They also have an affinity to the motor nerves controlling the bladder functions.
Calcarea phosphorica: Constitutionally indicated in the asthenic patient.
Pulsatilla: Incontinence of urine, particularly in girls.
Ferrum phosphoricum: Incontinence of urine, also during the day.
Kali phosphoricum: Nervous constitutions. General debility and weakness.
Sepia: Specific affinity to the bladder sphincter (insufficiency of). Nocturnal enuresis during first sleep. Close relationship to sexual sphere.
Diet & Regimen
Diet & Regimen
While there is no specific diet proven to cure functional enuresis (FE), certain dietary and lifestyle modifications may help reduce bedwetting episodes.
Limit Fluid Intake Before Bedtime:
Avoid caffeinated or sugary drinks in the evening as they can increase urine production and irritate the bladder.
Constipation Management:
Ensure adequate fiber intake through fruits, vegetables, and whole grains to prevent constipation, which can worsen enuresis.
Potential Bladder Irritants:
Some children may be sensitive to certain foods like citrus fruits, chocolate, spicy foods, or artificial sweeteners. Consider eliminating these if you notice a correlation with increased bedwetting.
Regimen Recommendations:
Regular Toilet Trips:
Encourage your child to urinate at regular intervals throughout the day, including before bedtime.
Double Voiding:
Have your child try to urinate again a few minutes after the initial void to empty the bladder completely.
Positive Reinforcement:
Reward your child for dry nights and avoid punishment for wet nights.
Manage Stress:
Help your child manage stress through relaxation techniques, exercise, or hobbies.
This book- Urinary and Fecal Incontinence: A Training Program for Children provides practical guidance on managing childhood incontinence, including dietary and behavioral strategies for reducing bedwetting. It emphasizes the importance of a positive and supportive approach to help children overcome this common challenge.[11]
Do’s and Don'ts
Do’s & Don’ts
Managing functional enuresis (FE) involves a combination of behavioral, lifestyle, and medical interventions. Here’s a list of do’s and don’ts to help your child:
Do’s:
- Do maintain a consistent bedtime routine and encourage regular sleep patterns.
- Do limit fluid intake in the evening, especially caffeinated and sugary drinks.
- Do encourage your child to urinate before bed and upon waking up.
- Do use positive reinforcement to reward dry nights, such as a sticker chart or small prizes.
- Do be patient and understanding, as overcoming enuresis takes time and effort.
- Do consult a healthcare professional if bedwetting persists or significantly impacts your child’s well-being.
- Do consider using a bedwetting alarm if behavioral strategies are unsuccessful.
- Do discuss any concerns or questions you have with your child’s doctor.
Don’ts:
- Don’t punish or shame your child for bedwetting accidents, as this can worsen anxiety and stress.
- Don’t restrict fluids during the day, as this can lead to dehydration and other health issues.
- Don’t wake your child up during the night to urinate, as this can disrupt their sleep and make them more tired.
- Don’t give up on treatment too soon, as some therapies may take weeks or months to show results.
- Don’t hesitate to seek professional help if you feel overwhelmed or need additional support.
This comprehensive textbook-Clinical Pediatric Urology provides a detailed discussion of the management strategies for functional enuresis, including behavioral, lifestyle, and medical interventions. The authors emphasize the importance of a collaborative approach between parents, children, and healthcare professionals to achieve optimal outcomes.[7]
Terminology
Terminology
Functional enuresis involves several terminologies that are important to understand for accurate diagnosis and treatment:
Enuresis:
The involuntary passage of urine in children who are expected to be toilet trained.
Functional Enuresis:
Enuresis that occurs in the absence of any underlying medical or structural cause. It is also known as primary nocturnal enuresis (PNE) if the child has never achieved night-time dryness, or secondary nocturnal enuresis (SNE) if bedwetting resumes after a period of dryness.
Monosymptomatic Nocturnal Enuresis (MNE):
Enuresis that occurs only during sleep, without any daytime bladder symptoms.
Non-monosymptomatic Nocturnal Enuresis (NMNE):
Enuresis that occurs during sleep along with daytime symptoms like urgency, frequency, or daytime incontinence.
Primary Nocturnal Enuresis (PNE):
Enuresis that has been present since early childhood and has never resolved.
Secondary Nocturnal Enuresis (SNE):
Enuresis that develops after a period of established continence (at least 6 months of dryness).
Nocturnal Polyuria:
Excessive urine production during the night, often due to decreased production of antidiuretic hormone (ADH) or decreased kidney response to ADH.
Bladder Capacity:
The maximum amount of urine the bladder can hold comfortably. Reduced bladder capacity can be a contributing factor to enuresis.
Overactive Bladder (OAB):
A condition characterized by urgency, frequency, and sometimes urge incontinence. OAB can contribute to both daytime and nighttime wetting.
Detrusor Overactivity:
Involuntary contractions of the detrusor muscle (the muscle that contracts to empty the bladder) during filling. This can lead to urgency and incontinence.
Urotherapy:
A behavioral therapy approach that includes education, bladder training, fluid management, and positive reinforcement to manage enuresis.
Enuresis Alarm:
A device that sounds an alarm when it detects moisture, helping to wake the child and interrupt the bedwetting episode.
Understanding these terminologies is crucial for healthcare professionals and parents to effectively communicate about functional enuresis, identify the specific subtype, and develop appropriate treatment plans.
In homeopathic literature on functional enuresis, you will often encounter the following terminologies:
Enuresis:
The involuntary discharge of urine, especially at night, in children beyond the age when bladder control is expected.
Nocturnal Enuresis:
Specifically refers to bedwetting that occurs during sleep.
Involuntary Urination:
The unintentional passing of urine without control.
Constitutional Remedy:
A homeopathic medicine chosen based on the individual’s overall physical, emotional, and mental characteristics, rather than just the specific symptoms of enuresis.
Repertory:
A comprehensive index of homeopathic symptoms and the corresponding remedies that are known to address them.
Materia Medica:
A collection of detailed descriptions of homeopathic remedies, including their characteristic symptoms and therapeutic applications.
Potency:
The strength or dilution of a homeopathic remedy. Higher potencies are believed to have a deeper and longer-lasting effect.
Aggravation:
A temporary worsening of symptoms after taking a homeopathic remedy, which is considered a positive sign of healing.
Miasm:
In homeopathy, a miasm refers to a predisposing factor or inherited tendency towards certain types of diseases. Identifying the underlying miasm is believed to be important for selecting the most effective remedy.
Proving:
A systematic process of testing a homeopathic substance on healthy individuals to determine its characteristic symptoms and therapeutic potential.
Understanding these terminologies will help you navigate homeopathic articles on functional enuresis and interpret the information presented. Remember, it’s crucial to consult with a qualified homeopathic practitioner for proper diagnosis and treatment.
References
Referenaces
- Psychiatry, Fourth Edition – Oxford Medical Publications -SRG-by John Geddes, Jonathan Price, Rebecca McKnight / Ch 32.
- https://en.wikipedia.org/wiki/Enuresis
- Prevalence of nocturnal enuresis among children aged 05 to 10 years (Indian Journal of Clinical Pediatrics, 2018)
- (PDF) Prevalence of Nocturnal Enuresis in 6–15 Years School Children and its Awareness among Parents in Dharwad – ResearchGate
- Prevalence and factors affecting enuresis amongst primary school children – ResearchGate
Book: Clinical Pediatric Nephrology,Edition: 5th edition
Writers: Ellis D. Avner, William E. Harmon, Patrick Niaudet
(2016),Publication: Lippincott Williams & Wilkins.- Book: Clinical Pediatric Urology
Edition: 4th edition,Writers: Stephen A. Koff, Douglas A. Canning, Lane S. Palmer,(2018),Publication: Wiley-Blackwell. - Book: Campbell-Walsh-Wein Urology,Edition: 12th edition
Writers: Alan J. Wein, Louis R. Kavoussi, Andrew C. Novick, Alan W. Partin, Craig A. Peters
(2021),Publication: Elsevier. - Book: Nelson Textbook of Pediatrics
Edition: 21st edition, Writers: Robert M. Kliegman, Bonita F. Stanton, Joseph St. Geme, Nina F. Schor, Richard E. Behrman,(2020),Publication: Elsevier. - Book: Developmental-Behavioral Pediatrics (4th Edition),Writers: William B. Carey, Helen C. Egger, Allen C. Crocker,(2009)
Publication: Saunders/Elsevier. - Book: Urinary and Fecal Incontinence: A Training Program for Children, Writers: Sean T. O’Leary, Steve J. Hodges,(2017),Publication: New Harbinger Publications.
Also Search As
Also Search As
To search for homeopathic articles on functional enuresis, you can use the following methods:
Online Databases:
Homeopathic Library (hpathy.com): This website contains a vast collection of homeopathic articles, cases, and resources. You can use the search bar to find articles specific to functional enuresis.
National Center for Homeopathy (NCH): This website provides access to homeopathic journals and publications. You can search their archives for relevant articles.
The American Institute of Homeopathy (AIH): This website offers a library of homeopathic resources, including journals and research articles. You can browse their collection or use the search function.
Search Engines:
Google Scholar: Search for academic articles and research papers on homeopathy and functional enuresis. Use specific keywords like "homeopathy," "functional enuresis," "bedwetting," and "case studies."
PubMed: This database includes a vast collection of biomedical literature. You can filter your search to include complementary and alternative medicine (CAM) articles, which may cover homeopathic research.
Homeopathic Libraries:
Visit your local homeopathic college or library to access their collection of books, journals, and articles. Librarians can guide you to relevant resources.
Homeopathic Forums and Communities:
Online forums and communities dedicated to homeopathy can be valuable resources. You can ask questions, share experiences, and learn from other practitioners and patients.
Tips for Effective Searching:
Use specific keywords and combinations of terms related to functional enuresis and homeopathy.
Filter your search results by date to find the most recent articles.
Look for articles published in reputable homeopathic journals.
Consider consulting with a homeopathic practitioner for personalized recommendations and guidance.
By utilizing these resources and strategies, you can find a wealth of information on the homeopathic approach to functional enuresis.
There are several ways to search for information on functional enuresis:
Medical Databases:
PubMed: A free resource developed by the National Center for Biotechnology Information (NCBI) at the U.S. National Library of Medicine (NLM). It comprises more than 35 million citations for biomedical literature from MEDLINE, life science journals, and online books.
Google Scholar: A freely accessible web search engine that indexes the full text or metadata of scholarly literature across an array of publishing formats and disciplines.
Clinical Guidelines and Reviews:
UpToDate: An evidence-based, physician-authored clinical decision support resource which clinicians trust to make the right point-of-care decisions.
International Children’s Continence Society (ICCS): This organization provides guidelines and resources on the diagnosis and management of enuresis in children.
Books and Textbooks:
Clinical Pediatric Urology: A comprehensive textbook covering various aspects of pediatric urology, including functional enuresis.
Nelson Textbook of Pediatrics: A widely used pediatric textbook that includes a chapter on enuresis.
Websites and Online Resources:
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Provides information on enuresis, including causes, diagnosis, and treatment options.
Mayo Clinic: Offers a patient-friendly overview of enuresis, including symptoms, risk factors, and treatment options.
Tips for Effective Searching:
Use specific keywords: Instead of just searching for "enuresis," try using more specific terms like "functional enuresis," "primary nocturnal enuresis," or "secondary enuresis."
Combine keywords: Use Boolean operators (AND, OR, NOT) to combine keywords and refine your search. For example, search for "functional enuresis AND treatment" to find articles specifically about treatment options.
Filter your results: Most databases allow you to filter your results by date, publication type, or other criteria. This can help you narrow down your search to the most relevant articles.
Consult a healthcare professional: If you have specific questions or concerns about functional enuresis, it’s always best to consult with a doctor or other healthcare professional. They can provide you with personalized advice and guidance based on your individual circumstances.
Frequently Asked Questions (FAQ)
What is Functional Enuresis?
Functional Enuresis is the repeated involuntary voiding of urine, occurring after an age at which continence is usual and in the absence of any identified physical disorder.
What causes Functional Enuresis?
- Idiopathic developmental delay
- Genetics
- Urinary tract infection
- Diabetes mellitus
- Abnormalities of the urinary tract
- Structural abnormalities of the nervous system
- Chronic constipation
- Diuretics: e.g. caffeine, alcohol
- ADHD
What are the types of functional enuresis?
There are two main types: primary nocturnal enuresis (PNE), where the child has never been dry at night, and secondary nocturnal enuresis (SNE), where bedwetting starts after a period of dryness.
What are the symptoms of Functional Enuresis?
- Urge incontinence
- Voiding postponement
- Stress incontinence
- Giggling incontinence
Can homeopathy help with bedwetting in children?
Yes, homeopathy offers a holistic approach to address functional enuresis (bedwetting) in children.It aims to treat the root cause, not just the symptoms, by considering the child’s individual constitution and emotional state., luctus nec ullamcorper mattis, pulvinar dapibus leo.
How does homeopathic treatment for functional enuresis work?
A homeopathic practitioner will conduct a detailed consultation with the child and parents, exploring the child’s medical history, sleep patterns, emotional state, and any other relevant factors. Based on this information, they will select a personalized remedy to address the individual’s needs.
How long does homeopathic treatment for functional enuresis take?
The response to treatment varies. Some children may experience improvement within a few weeks, while others may take longer. It is important to be patient and consistent with the treatment.
Can I combine homeopathic remedies with conventional treatments for functional enuresis?
It is generally safe to combine homeopathic remedies with conventional treatments, such as behavioral therapies or medications. However, it is essential to inform your child’s doctor and homeopath about all treatments being used.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Functional Enuresis?
Homeopathic Medicines for Functional Enuresis
- Calcarea phos
- Pulsatilla
- Ferrum phos
- Kali phos
- Sepia
