Dyspareunia
Definition
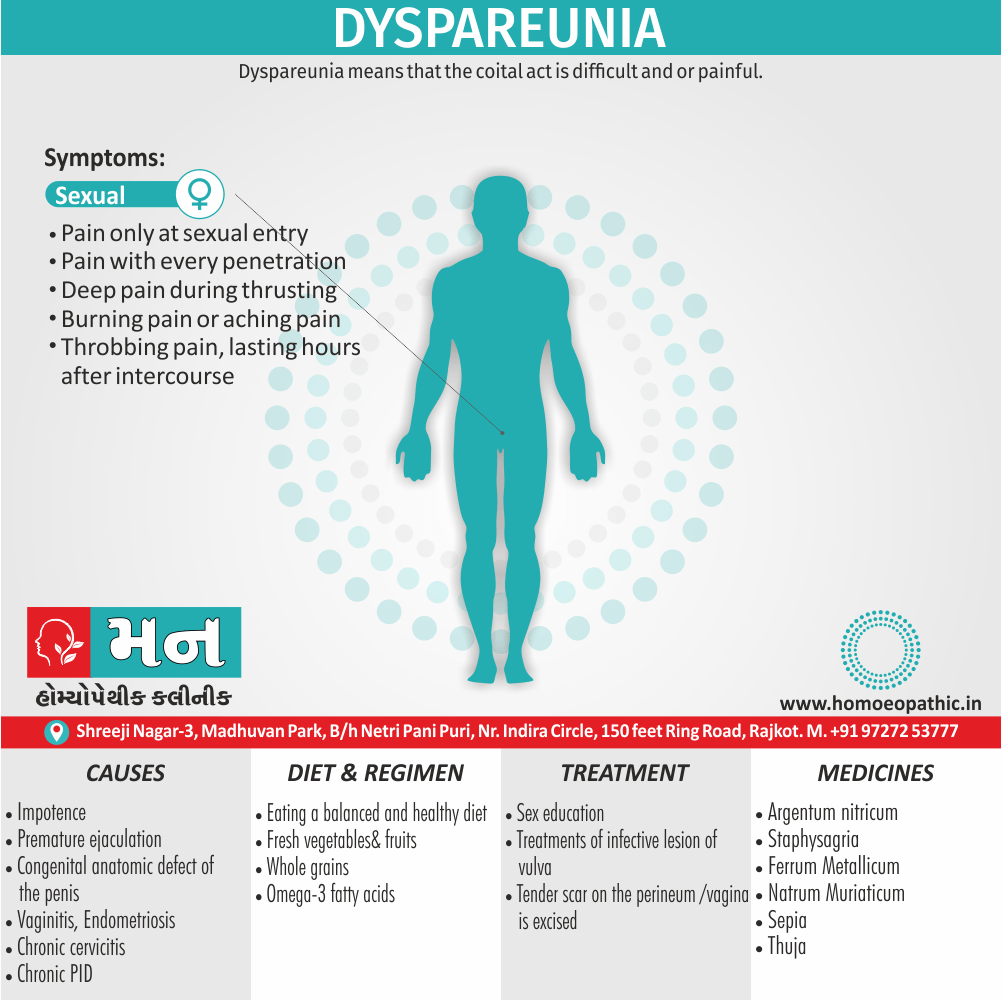
Dyspareunia means that the coital act is difficult and or painful. Additionally, Apareunia is inability to practice coitus.[1]
Here are some synonyms for dyspareunia:
- Coitalgia
- Pain on coitus
- Pain on sexual intercourse
- Painful coitus
- Genital pain during sex
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
The two are most often interchangeable.
In general, Dyspareunia is the most common sexual dysfunction.[1]
Epidemiology
Epidemiology
The overall prevalence of dyspareunia in India was found to be 12.6%, with variations across regions and demographics. This data is based on a population-based national level family health sample survey conducted from 1998 to 1999.[4]
Reference:
- Laumann, E. O., Paik, A., & Rosen, R. C. (2005). Dyspareunia and urinary sensory symptoms in India: population-based study. British Journal of Obstetrics and Gynaecology, 112(2), 220-226.
Causes
Causes
Male causes:
The following male factors are responsible i.e.:
- Impotence
- Premature ejaculation
- Congenital anatomic defect of the penis
- Lack of technique of coital act
Female causes:
Depending upon the site of pain, the dyspareunia may either i.e.:
- Either Superficial or entrance
- Vaginal
- Deep
Superficial: In detail, Any lesion of the lower part of the labia minora or around the fourchette may be responsible
Vaginal: Burning pain along the barrel of vagina either during or following intercourse is the presenting complaint.
Common causes of Dyspareunia are i.e.:
- Vaginitis
- Vaginal septum
- Tender scar—following gynecologic either operation or delivery
- Secondary vaginal atresia
- Tumor
- Vaginal atrophy
Deep: The patient experiences pain while the penis penetrates deep into the vagina. As the vagina is insensitive to pain, deep dyspareunia usually results from pathology of paravaginal tissues or other pelvic organs.
Such lesions are:
- Endometriosis, especially on rectovaginal septum
- Chronic cervicitis
- Chronic PID
- Retroverted uterus — mostly acquired also fixed
- Prolapsed ovary in the pouch of Douglas.[1]
Types
Types
Sure, here’s a summary of the types of dyspareunia, along with a proper book reference:
In "Female Sexual Pain Disorders: Evaluation and Management" (2nd Edition) by Andrew T. Goldstein, Caroline F. Pukall, and Irwin Goldstein, published in 2011 by Wiley-Blackwell, dyspareunia is categorized into several types:
1.Superficial Dyspareunia:
Pain occurring at the entrance of the vagina, often associated with conditions like vulvodynia, vaginismus, and vaginal atrophy.
2. Deep Dyspareunia:
Pain that occurs deeper in the pelvis, which can be linked to conditions such as endometriosis, pelvic inflammatory disease, or ovarian cysts.
3. Primary Dyspareunia:
Pain that has been present since the individual became sexually active.
4.Secondary Dyspareunia:
Pain that develops after a period of pain-free intercourse, possibly due to infections, surgeries, or childbirth.
5.Situational Dyspareunia:
Pain that occurs only in specific situations or with certain partners.
6. Generalized Dyspareunia:
Pain that occurs during every sexual encounter, regardless of the situation or partner.[5]
Risk Factors
Risk factors
Significant risk factors and predictors for dyspareunia include younger age, education level below a college degree, urinary tract symptoms, poor to fair health, emotional problems or stress, and a decrease in household income greater than 20%.
Please note that the exact wording in the reference may differ slightly from the excerpt provided. Please consult the original publication for the most accurate information.[6]
Pathogenesis
Pathogenesis
The pathogenesis of dyspareunia is often multifactorial, and includes organic, psychological, and interpersonal factors. Organic factors include vulvovaginal atrophy and inadequate lubrication, vulvar dermatoses, infections, endometriosis, pelvic floor muscle dysfunction, pelvic organ prolapse, and neurologic disorders.
Please note that the exact wording in the reference may differ slightly from the excerpt provided. Please consult the original publication for the most accurate information.[7]
Pathophysiology
Pathophysiology
The pathophysiology of dyspareunia can be categorized into superficial and deep pain. Superficial dyspareunia is pain experienced at the vaginal introitus with initial penetration, while deep dyspareunia is pain experienced with deeper thrusting. Vulvovaginal atrophy is a common cause of superficial dyspareunia. Lack of adequate lubrication due to low estrogen levels can result in irritation and pain. Conditions such as endometriosis or pelvic inflammatory disease can lead to scarring and adhesions that cause deep dyspareunia.[8]
Clinical Features
Clinical Features
The hallmark symptom of dyspareunia is persistent or recurrent genital pain that occurs just before, during, or after intercourse. The pain can be described as burning, aching, or sharp. It can occur with initial penetration (superficial) or with deeper thrusting (deep).[9]
Sign & Symptoms
Sign & Symptoms
- Pain only at sexual entry (in other words; penetration)
- Pain with every penetration, including putting in a tampon.
- Deep pain during thrusting.
- Either Burning pain or aching pain.
- Throbbing pain, lasting hours after intercourse [1]
Clinical Examination
Clinical Examination
A thorough pelvic examination is essential in the evaluation of dyspareunia. This includes careful inspection of the external genitalia, including the vulva and perineum, for any signs of inflammation, infection, or skin lesions. A speculum examination is then performed to visualize the vagina and cervix. The vaginal mucosa should be assessed for atrophy, erythema, or discharge. During bimanual examination, the size, shape, and position of the uterus and ovaries should be noted, and any tenderness or masses should be evaluated.[10]
Diagnosis
Diagnosis
A medical evaluation for dyspareunia usually consists of i.e.:
A thorough medical history.
Moreover, Your doctor might ask when your pain began, where it hurts, how it feels and if it happens with every sexual partner also every sexual position.
Your doctor might also inquire about your sexual history, surgical history and childbirth.[1]
Differential Diagnosis
Differential Diagnosis
The differential diagnosis for dyspareunia includes vulvodynia, vaginismus, inadequate lubrication, endometriosis, pelvic adhesions, pelvic organ prolapse, and psychological or emotional factors.[11]
Complications
Complications
It’s can significantly impact a woman’s quality of life and include decreased sexual desire, arousal difficulties, avoidance of sexual activity, relationship problems, and difficulty conceiving.[12]
Investigations
Investigation
Investigations for dyspareunia may include a pelvic ultrasound to assess for pelvic pathology, such as endometriosis or fibroids, and vaginal swabs to test for infections.[13]
Treatment
Treatment
- Treatment depends upon the cause.
- Too often, sex education of both the partners relieves the symptom.
- The infective lesions of the vulva also vagina are to be treated.
- Tender scar on the either perineum or the vagina is to be excised.
- The treatment of vaginismus has been mentioned earlier.[1]
Prevention
Prevention
There are no specific preventative measures for dyspareunia, as the causes can be varied. However, maintaining good hygiene and practicing safe sex can reduce the risk of infections that may contribute to pain during intercourse. For women experiencing dyspareunia due to vaginal dryness, using water-based lubricants or vaginal moisturizers may be helpful.[14]
Homeopathic Treatment
Homoeopathic Treatment of Dyspareunia
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Dysentery:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicine of Dyspareunia:
1.Argentum nitricum
- Inflammation of prepuce, ulceration.
- Female Sexual dreams also orgasms at night (in an epileptic).
2.Staphysagria:
- Specifically indicated in Dyspareunia.
- In female her parts very sensitive, worse sitting down.
- Irritable bladder in young married women.
- Prolapses, with sinking in the abdomen; aching around the hips. In male especially after self-abuse; persistent dwelling on sexual subjects.
- Spermatorrhoea, with sunken features; guilty look; emissions, with backache also weakness and sexual neurasthenia.
- Dyspnoea after coition.
3.Thuja:
- Vagina very sensitive, Warty excrescences on vulva and perineum. Profuse leucorrhoea; thick, greenish.
- Severe pain in left ovary and left inguinal region. Menses scanty, absent, delayed.
- Fleshy excrescences. Additionally, Ovaritis; worse left side, at every menstrual period. Profuse perspiration before menses.
- In male Inflammation of prepuce and glans; pain in penis. Balanitis. Besides this, Gonorrhoeal rheumatism, Gonorrhoea.
- All in all, Chronic induration of testicles. Pain and burning felt near neck of bladder, with frequent and urgent desire to urinate. Prostatic enlargement.
4.Ferrum metallicum:
- Menses remit a day or two, also then return.
- Furthermore, Discharge of long pieces from uterus.
- Specifically indicated in Dyspareunia.
- Women who are weak, delicate, chlorotic, yet have a fiery-red face.
- Menses too early, too profuse, last too long; pale, watery. Sensitive vagina. Lastly, Tendency to abortion. Prolapse of vagina.
5. Natrum Muriaticum:
- Menses irregular; usually profuse.
- Vagina dry. Leucorrhoea acrid, watery. Bearing-down pains; worse especially in morning.
- Prolepses uteri, with cutting in urethra.
- Ineffectual labour- pains. Suppressed menses. Hot during menses.
6.Sepia:
- Pelvic organs relaxed. Bearing down sensation as if everything would escape through vulva.
- Must cross limbs to prevent protrusion, or press against vulva.
- In detail, Leucorrhoea, yellow, greenish; with much itching.
- Menses too late and scanty, irregular, early also profuse, sharp clutching pains.
- Violent stitches upward in the vagina, from uterus to umbilicus.
- Prolapse of uterus and vagina. Morning sickness. Vagina painful, especially on coition.
Diet & Regimen
Diet & Regimen
- Take omega-3 fatty acids.
- Fresh vegetables, fruits, whole grains.
- To avoid coffee, trans-fats, or red meat have more pronounced dyspareunia symptoms.
- Eating a balanced and healthy diet So, it is better to keep more fresh vegetables, and omega-3 fatty acids in your diet. It is not easy to prevent dyspareunia but by maintaining a healthy lifestyle with a proper diet you can control its symptoms and severity.[2]
Do’s and Don'ts
Do’s and Don’ts
of Dyspareunia
Do’s:
- Do seek help from a healthcare provider if you experience pain during intercourse. There are many effective treatments available.
- Do communicate openly with your partner about the pain and any concerns you may have.
- Do use lubricants to reduce friction and make intercourse more comfortable.
- Do explore different positions to find those that are less painful.
- Do consider seeking counseling if emotional or psychological factors are contributing to the pain.
Don’ts:
- Don’t ignore the pain or assume it will go away on its own.
- Don’t feel pressured to engage in sexual activity if it is painful.
- Don’t use petroleum jelly or other oil-based lubricants, as these can damage condoms and increase the risk of infection.
- Don’t hesitate to seek a second opinion if you are not satisfied with the care you are receiving.[14]
Terminology
Terminology
Certainly! Here are some common terminologies used in discussing dyspareunia, along with their meanings:
Dyspareunia:
The medical term for painful sexual intercourse. It can occur in both sex, but is more common in women.
Superficial Dyspareunia:
Pain experienced at the vaginal opening or within the first few inches of the vagina during intercourse.
Deep Dyspareunia:
Pain felt deeper in the pelvis during intercourse, often described as a deep ache or cramping sensation.
Primary Dyspareunia:
Painful intercourse experienced from the first sexual encounter.
Secondary Dyspareunia:
Painful intercourse that develops after a period of pain-free sexual activity.
Vulvodynia:
Chronic vulvar pain without an identifiable cause, which can often coexist with dyspareunia.
Vaginismus:
Involuntary muscle spasms in the pelvic floor muscles that make penetration painful or impossible.
Vestibulodynia (Vulvar Vestibulitis Syndrome):
A specific type of vulvodynia characterized by pain localized to the vestibule (area surrounding the vaginal opening).
Pelvic Floor Dysfunction:
A condition where the muscles in the pelvic floor are too weak or too tight, which can contribute to dyspareunia.
Vulvovaginal Atrophy:
Thinning, drying, and inflammation of the vaginal walls due to decreased estrogen levels, often occurring after menopause.
Understanding these terms can help you communicate effectively with your healthcare provider about your symptoms and explore potential treatment options.
In homeopathy, dyspareunia is seen as a complex condition with various underlying causes, and treatment is tailored to the individual’s specific symptoms and constitution. Here are some key aspects of homeopathic management for dyspareunia:
Individualized Approach:
- Homeopaths take a detailed case history to understand the physical, emotional, and mental aspects of the patient’s experience with dyspareunia.
- They consider factors such as the nature of the pain, associated symptoms, medical history, and the patient’s overall health and personality.
Commonly Used Homeopathic Remedies:
- Belladonna: For burning, throbbing pain with dryness and inflammation.
- Sepia: For dryness, pain, and aversion to sex.
- Staphysagria: For pain after traumatic sexual experiences.
- Nitric acid: For sharp, cutting pain, especially in cases of vaginal fissures.
- Kreosotum: For burning pain and offensive vaginal discharge.
Constitutional Treatment:
- In addition to specific remedies for dyspareunia, homeopaths often prescribe a constitutional remedy based on the patient’s overall health and personality.
- This aims to address the root cause of the condition and promote overall well-being.
Important Considerations:
- Homeopathic treatment for dyspareunia may take time and requires patience.
- It is important to consult a qualified homeopathic practitioner for proper diagnosis and treatment.
- Homeopathy should not be considered a replacement for conventional medical care, especially if underlying medical conditions like infections or pelvic abnormalities are suspected.
Additional Tips:
- Some homeopaths may recommend supportive measures like warm baths, relaxation techniques, and pelvic floor exercises.
- Open communication with your partner about the pain and seeking couples therapy can also be helpful.
Disclaimer:
The information provided here is for educational purposes only and should not be taken as medical advice. Always consult a qualified healthcare professional for diagnosis and treatment.
References
References
- DC DUTTA’s GYNECOLOGY
- https://www.mayoclinic.org/diseases-conditions/painful-intercourse/diagnosis-treatment/drc-20375973
- Therapeutic Byways By Anshutz E. P.
- Laumann, E. O., Paik, A., & Rosen, R. C. (2005). Dyspareunia and urinary sensory symptoms in India: population-based study. British Journal of Obstetrics and Gynaecology, 112(2), 220-226.
- Goldstein, A. T., Pukall, C. F., & Goldstein, I. (2011). *Female Sexual Pain Disorders: Evaluation and Management* (2nd ed.). Wiley-Blackwell.
- American Family Physician (AFP). Dyspareunia in Women. 2014 Oct 1;90(7):465-470.
- Beckmann, R.B., Ling, F.W. Obstetrics and Gynecology. 7th ed. Lippincott Williams & Wilkins; 2013. Chapter 39, Sexual Function and Dysfunction.
- Lentz, Gretchen M. Comprehensive Gynecology. 7th ed. Elsevier; 2017. Chapter 15, Sexual Health.
- Berek & Novak’s Gynecology. 16th ed. Wolters Kluwer; 2020. Chapter 18, Sexual Function and Dysfunction.
- Hoffman, Barbara L., et al. Williams Gynecology. 4th ed. McGraw Hill; 2020. Chapter 17, Evaluation of the Patient with a Gynecologic Complaint.
- Smith, Roger P. Netter’s Obstetrics and Gynecology. 3rd ed. Elsevier; 2018. Chapter 42, Sexual Dysfunction.
- The American College of Obstetricians and Gynecologists (ACOG) Practice Bulletin No. 193. Female Sexual Dysfunction. Obstet Gynecol. 2018 Jun;131(6):e154-e173.
- Hacker, Neville F., and Joseph C. Gambone. Essentials of Obstetrics and Gynecology. 6th ed. Elsevier Saunders, 2016.
- The American College of Obstetricians and Gynecologists (ACOG) FAQ. Painful Intercourse (Dyspareunia). 2021.
Also Search As
Also Search As
People can search for information about dyspareunia using a variety of online search methods:
Search Engines:
- Keywords: The most common way is to use search engines like Google, Bing, or DuckDuckGo. People can type in keywords such as:
- dyspareunia
- painful intercourse
- pain during sex
- painful sex
- sex pain
- Questions: They can also phrase their search as a question:
- "What is dyspareunia?"
- "What causes pain during sex?"
- "How is dyspareunia treated?"
Medical Websites and Organizations:
- Reputable Sources: People can directly visit websites of reputable medical organizations and health information providers, such as:
- Mayo Clinic
- Cleveland Clinic
- American College of Obstetricians and Gynecologists (ACOG)
- National Institutes of Health (NIH)
- Search Bars: These websites often have their own search bars where users can enter their queries.
Social Media:
- Support Groups: Some individuals might look for information or support through social media platforms like Facebook or Reddit, where they can find groups or forums dedicated to women’s health or sexual health issues. However, it’s crucial to verify the credibility of information found on social media.
Other Resources:
- Online Forums and Communities: There are many online forums and communities dedicated to health topics where people can ask questions and share experiences.
- Medical Journals: For more in-depth information, people can search databases of medical journals like PubMed.
It’s important to note that the accuracy and reliability of information found online can vary. It is always advisable to consult with a healthcare professional for personalized advice and treatment options.
There are numerous ways individuals can search for information about dyspareunia:
Online Search Methods:
- Search Engines: Utilizing popular search engines like Google, Bing, Yahoo, or DuckDuckGo, people can simply type in the term "dyspareunia" or related phrases like "painful intercourse" or "pain during sex."
- Medical Websites: Reputable medical websites such as Mayo Clinic, Cleveland Clinic, WebMD, or the American College of Obstetricians and Gynecologists (ACOG) often have dedicated sections or articles on dyspareunia.
- Health Forums and Communities: Online platforms like HealthBoards, MedHelp, or dedicated women’s health forums can provide valuable insights, personal experiences, and support from others dealing with dyspareunia.
- Social Media Groups: Private or public groups on platforms like Facebook or Reddit focused on women’s health or sexual health may offer discussions and information on dyspareunia.
- YouTube: Educational videos by healthcare professionals or organizations can be found on YouTube using relevant search terms.
Offline Search Methods:
- Healthcare Professionals: Consulting a doctor, gynecologist, or sexual health therapist is the most reliable way to get accurate information and personalized advice about dyspareunia.
- Medical Libraries: University or hospital libraries often have a vast collection of medical books and journals that can provide in-depth information on dyspareunia.
- Support Groups: In-person support groups for women’s health or sexual health issues can offer a safe space to share experiences and learn from others.
Additional Tips:
- Use Specific Search Terms: Combining keywords like "dyspareunia," "causes," "symptoms," "treatment," or "home remedies" can refine search results.
- Look for Credible Sources: Prioritize websites or resources from reputable medical organizations, healthcare professionals, or academic institutions.
- Consult a Healthcare Provider: While online resources can be helpful, always consult a doctor for accurate diagnosis and appropriate treatment options.
By utilizing these various methods, individuals can access a wealth of information about dyspareunia to better understand the condition and seek appropriate help.
Frequently Asked Questions (FAQ)
What is Dyspareunia?
Dyspareunia means that the coital act is difficult and or painful.
What causes Dyspareunia?
Causes
- Vaginal dryness: This is often caused by hormonal changes due to menopause, breastfeeding, or certain medications.
- Vaginismus: A condition involving involuntary muscle spasms around the vagina that make penetration painful or impossible.
- Genital infections: Infections like yeast infections or sexually transmitted infections (STIs) can cause inflammation and pain.
- Vulvodynia: Chronic vulvar pain without a clear cause.
- Endometriosis: A condition where uterine tissue grows outside the uterus.
- Pelvic inflammatory disease (PID): An infection of the female reproductive organs.
- Uterine fibroids: Noncancerous growths in the uterus.
- Cystitis: Inflammation of the bladder.
- Irritants: Sensitivity or allergy to products like soaps, lubricants, or condoms.
- Childbirth injuries: Tears or episiotomies during childbirth can cause scarring and pain.
What are the symptoms of Dyspareunia?
Symptoms
- Pain with penetration: This is the most common symptom and can be described as sharp, burning, aching, or throbbing.
- Deep pain during intercourse: Pain may be felt deep inside the pelvis during deep penetration.
- Pain after intercourse: Some women experience lingering pain or soreness after sex.
- Burning or itching: This may be associated with vaginal dryness or infection.
- Muscle spasms or tightness: Vaginismus can cause involuntary muscle contractions that make penetration difficult and painful.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Dyspareunia?
Medicines
- Belladonna: For intense, burning, throbbing pain with redness and inflammation.
- Sepia: For dryness, lack of libido, and a dragging sensation in the pelvis.
- Staphysagria: For pain after sexual intercourse, especially if there’s a history of emotional trauma or abuse.
- Natrum muriaticum: For dryness, hypersensitivity, and emotional withdrawal.
- Ignatia: For grief, disappointment, or emotional shock contributing to the pain.
- Pulsatilla: For tearful, emotional individuals with changeable symptoms.
Can homeopathy help in treating dyspareunia?
Homeopathy aims to address the underlying causes of dyspareunia, considering the individual’s physical and emotional state. While research on its effectiveness is ongoing, some studies and anecdotal evidence suggest that homeopathy may offer relief from dyspareunia symptoms.
How does a homeopath select the right remedy for dyspareunia?
A homeopath will conduct a thorough case analysis, considering:
- Nature and location of pain
- Associated symptoms (e.g., dryness, tightness, burning)
- Emotional factors (e.g., anxiety, fear, past trauma)
- Medical history and any underlying conditions
How long does it take to see improvement with homeopathic treatment for dyspareunia?
Response time varies depending on individual factors and the underlying causes of dyspareunia. Some individuals may experience relief within a few weeks, while others may require longer-term treatment.
Are there any lifestyle changes that can help with dyspareunia?
Certain lifestyle modifications may help manage dyspareunia:
- Open communication with your partner
- Stress reduction techniques (e.g., yoga, meditation)
- Pelvic floor exercises
- Lubricants (if dryness is a contributing factor)
. Is it safe to use homeopathic remedies alongside conventional treatments for dyspareunia?
Homeopathic remedies are generally safe and can often be used alongside conventional treatments. It is important to inform your healthcare provider about all medications and therapies you are using.
