Acute Stress Disorder
Definition
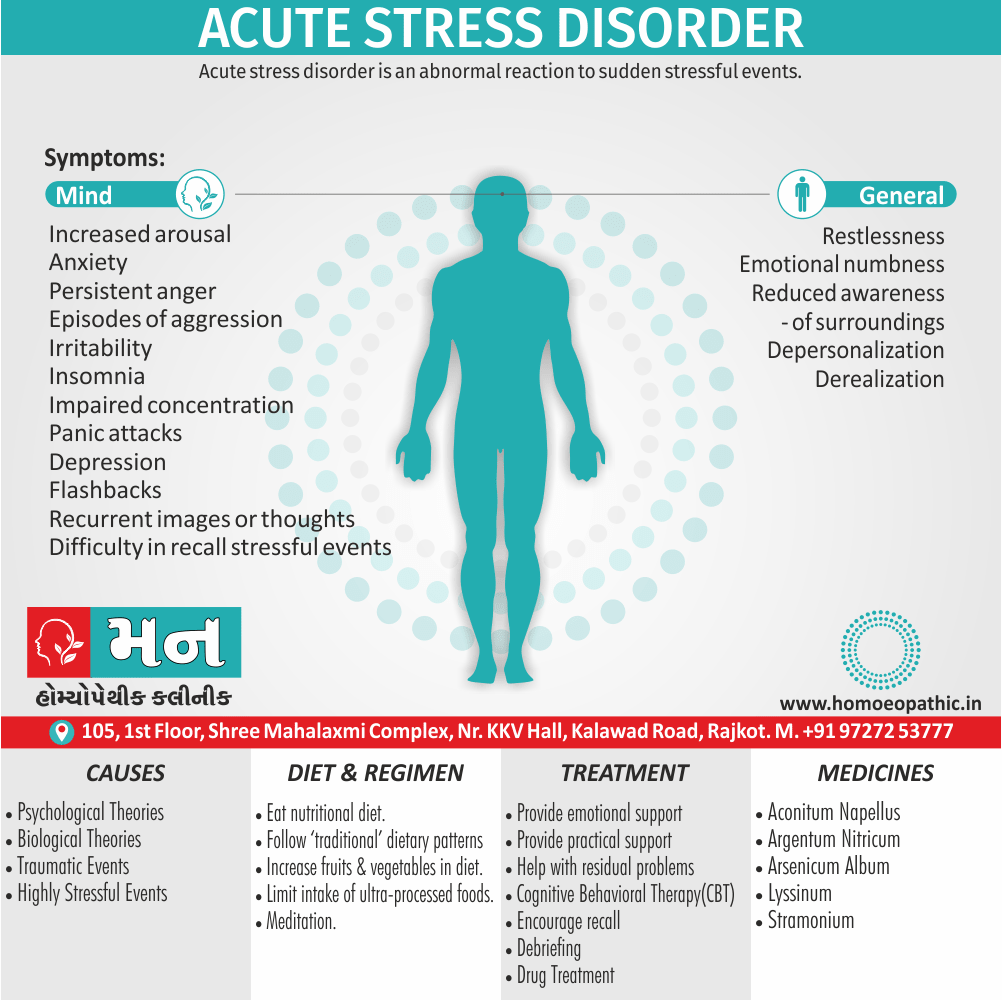
Acute stress disorder is an abnormal reaction to sudden stressful events. [1]
Here are some related terms that capture different aspects of ASD:
- Clinical diagnoses:
- Acute Stress Disorder (ASD) – for short-term stress reactions after a traumatic event.
- Post-traumatic Stress Disorder (PTSD) – for long-term effects of experiencing trauma.
- More general terms:
- Anxiety disorders – encompasses various conditions where anxiety is the main feature.
- Adjustment disorders – difficulty coping with a stressful life event.
- Informal terms:
- Traumatic stress reaction
- Emotional overwhelm
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do's & Don'ts
Terminology
References
Also Search As
Overview
Overview
The basic response of the body is the same as in the normal stress reaction, but the symptoms are more severe and last for a longer period.
Acute stress disorder lasts no more than 4 weeks.
It is generally accept that having symptoms after a stressful event is normal for up to about 48 hours, but after this point the majority of people will have recovered. [1]
Epidemiology
Epidemiology of Acute Stress Disorder (ASD) in India
The available research on the epidemiology of ASD in India is limited, but some studies provide insights into its prevalence and contributing factors.
- A Study of Prevalence and Contributory Factors of Acute Stress Disorder in a Train Accident in India (2015)
This study investigated the prevalence of ASD following a train accident in India. The researchers found that a significant proportion of survivors met the criteria for ASD, highlighting the impact of traumatic events on mental health.
- Epidemiology and factors associated with acute stress disorder in a population of burn patients in the city of Medellín: case-control study (2021)
While this study was conducted in Medellín, Colombia, it offers valuable insights that may be relevant to the Indian context. The study found that burn patients have a high incidence of ASD, with factors such as life threat, severe pain, and burn severity increasing the risk.
- Stress in India – statistics & facts – Statista (Accessed July 2024)
This resource provides a broader overview of stress in India, including statistics related to its prevalence and impact. While not specific to ASD, it highlights the significant burden of stress-related disorders in the country.
- Acute Stress Disorder – StatPearls – NCBI Bookshelf (Accessed July 2024)
This resource, while not specific to India, provides a comprehensive overview of ASD, including its diagnostic criteria, epidemiology, and treatment approaches. It can serve as a valuable reference for understanding ASD in the Indian context.
It is important to note that these are just a few examples, and more research is needed to fully understand the epidemiology of ASD in India. Further studies should explore the prevalence of ASD in different populations, identify risk and protective factors, and evaluate the effectiveness of interventions for preventing and treating ASD.
Causes
Causes
Many kinds of highly stressful event can provoke an acute stress disorder, for example involvement in an either accident or fire, physical assault, or rape.
Since the stress response does not become abnormal in everyone exposed to the same events, there must be some kind of personal predisposition, but it is not known what this is.
Acute stress disorder can occur among bystanders as well as those directly involved, and among those involved in rescuing or caring for others.
Psychological theories:
- A variety of psychological mechanisms are probably at work in acute stress disorder, but dissociation is the most studied.
- It is thought that dissociation reduces the negative consequences of trauma by restricting awareness of the event and thereby preventing the person from being overwhelmed by the traumatic experience.
- Unfortunately, this prevents recovery as it does not allow the experience to be processed also integrated into existing coping mechanisms.
- A similar problem occurs when a person uses avoidance strategies excessively.
Biological theories:
- The main theory is based upon classical conditioning.
- When a traumatic event occurs (an unconditioned stimulus), people respond with fear (unconditioned response).
- As reminders of the trauma occur (conditioned stimulus), people then respond with fear reactions (conditioned response).
- It is thought that in some people, the stress response becomes sensitized to repeated stimuli, and a larger response is produced to each stimulus.
- Those people who suffer a panic attack during a traumatic event are very likely to experience increasing panic attacks in the few weeks afterwards. [1]
Types
Types
Acute Stress Disorder (ASD) is not typically classified into distinct types. However, it can manifest with different symptom patterns and varying severity levels. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) outlines the following symptom clusters for ASD:
Intrusion Symptoms: Recurrent, involuntary, and distressing memories of the traumatic event, nightmares, flashbacks, or intense psychological distress or physiological reactions to reminders of the event.
Negative Mood: Persistent inability to experience positive emotions like happiness, satisfaction, or love.
Dissociative Symptoms: Altered sense of reality, inability to remember important aspects of the traumatic event, feeling detached from oneself or one’s surroundings.
Avoidance Symptoms: Efforts to avoid distressing memories, thoughts, feelings, or external reminders of the traumatic event.
Arousal Symptoms: Sleep disturbances, irritable behavior, hypervigilance, exaggerated startle response, problems with concentration, or reckless behavior.
The specific presentation of ASD can vary depending on individual experiences and the nature of the traumatic event.[6]
Please note that while the DSM-5 does not categorize ASD into distinct types, some researchers and clinicians may refer to subtypes based on predominant symptom clusters (e.g., predominantly dissociative ASD or predominantly hyperarousal ASD). However, these subtypes are not officially recognized in the DSM-5.
Risk Factors
Risk Factor
Pretrauma factors i.e.:
- Female gender
- Intellectual disability
- Lack of education
- History of traumatic events
- History of psychiatric disorder(s)
- Personality disorder(s)
- Genetics
Peritrauma factors i.e.:
- Trauma severity
- Assault
- Rape
- Physical injury
Posttrauma factors i.e.:
- Acute stress disorder (ASD)
- Tachycardia
- Poor socioeconomic status
- Physical pain severity
- ICU stay
- Brain injury
- Dissociative symptoms
- Disability
- Subsequent life stress[3]
Pathogenesis
Pathogenesis
The pathogenesis of Acute Stress Disorder (ASD) is complex and involves a combination of biological, psychological, and social factors. While no single book provides a comprehensive explanation, several resources offer valuable insights into the underlying mechanisms:
The DSM-5 outlines the diagnostic criteria for ASD and provides a framework for understanding its clinical presentation. It emphasizes the role of exposure to a traumatic event as a primary trigger for ASD.[6]
This section delves into the neurobiological and psychological underpinnings of trauma-related disorders, including ASD. It discusses the dysregulation of stress response systems, alterations in brain structures and function, and the impact of individual vulnerabilities.[9]
While not a textbook, this book provides a comprehensive overview of trauma’s impact on the brain and body. It explores the role of the autonomic nervous system, the limbic system, and the prefrontal cortex in the development of trauma-related disorders.
Key Points on ASD Pathogenesis:
- Exposure to a traumatic event: ASD is triggered by experiencing or witnessing a traumatic event that involves actual or threatened death, serious injury, or sexual violence.
- Dysregulation of stress response systems: The hypothalamic-pituitary-adrenal (HPA) axis, responsible for the stress response, becomes dysregulated, leading to heightened arousal and impaired emotional regulation.
- Neurobiological alterations: Trauma can alter brain structures and functions, particularly in the amygdala (responsible for fear processing) and the hippocampus (involved in memory consolidation).
- Psychological factors: Preexisting psychological vulnerabilities, coping mechanisms, and social support systems can influence the development and severity of ASD.
- Genetic predisposition: Research suggests that genetic factors may play a role in individual susceptibility to developing ASD after trauma exposure.
Understanding the pathogenesis of ASD is crucial for developing effective prevention and treatment strategies. Further research is needed to elucidate the complex interplay of biological, psychological, and social factors contributing to this disorder.
Pathophysiology
Pathophysiology of Acute stress disorder
The exact reason why most people recover after a traumatic event but few develop acute stress disorder (ASD) remains unknown. Various models were developed to explain the response to traumatic events. The majority of them are related to "fear conditioning." It is a form of Pavlovian learning that when a traumatic stimulus (e.g., explosion) occurs together with a neutral stimulus (e.g., smell) or context (e.g., night time), in the future encounters of the neutral stimulus or context, the brain, and the body exhibits the same fear responses (even in the absence of the traumatic stimulus)
Most healthy people adapt to fear conditioning by extinction learning – a gradual reduction in response to the traumatic stimulus. If this mechanism fails, the patient continues to re-experience fearful symptoms of the initial traumatic event.
Functional magnetic resonance imaging (fMRI) scans of PTSD patients have shown hypoactivity of the frontal cortex and hyperactivity of the temporal cortex, demonstrating the possibility of a correlation between PTSD and neural functioning. A more recent study showed hyperactivation of the superior prefrontal and cingulate cortex and medial posterior precuneus.[3]
Clinical Features
Clinical Features of Acute Stress Disorder
Acute Stress Disorder (ASD) is characterized by a constellation of clinical features that emerge within one month of exposure to a traumatic event. These features are categorized into five clusters, as described in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5):
Intrusion Symptoms:
- Recurrent, involuntary, and intrusive distressing memories of the traumatic event.
- Nightmares related to the traumatic event.
- Dissociative reactions (e.g., flashbacks) in which the individual feels or acts as if the traumatic event were recurring.
- Intense or prolonged psychological distress or marked physiological reactions in response to internal or external cues that symbolize or resemble an aspect of the traumatic event.
Negative Mood:
- Persistent inability to experience positive emotions (e.g., happiness, satisfaction, or loving feelings).
Dissociative Symptoms:
- An altered sense of the reality of one’s surroundings or oneself (e.g., feeling in a daze, time slowing).
- Inability to remember an important aspect of the traumatic event (typically dissociative amnesia and not due to head injury, alcohol, or drugs).
Avoidance Symptoms:
- Efforts to avoid distressing memories, thoughts, or feelings about or closely associated with the traumatic event.
- Efforts to avoid external reminders (people, places, conversations, activities, objects, situations) that arouse distressing memories, thoughts, or feelings about or closely associated with the traumatic event.
Arousal Symptoms:
- Sleep disturbance (e.g., difficulty falling or staying asleep, restless sleep).
- Irritable behavior and angry outbursts (with little or no provocation), typically expressed as verbal or physical aggression toward people or objects.
- Hypervigilance.
- Problems with concentration.
- Exaggerated startle response.
To meet the diagnostic criteria for ASD, an individual must experience a minimum number of symptoms from each cluster. The DSM-5 provides detailed criteria for the diagnosis of ASD.
Please note that this information is a summary of the clinical features of ASD as described in the DSM-5. For a comprehensive understanding, it is recommended to consult the DSM-5 or other authoritative sources.[6]
Sign & Symptoms
Sign & Symptoms of acute stress disorder are:
Increased arousal:
- Anxiety and panic attacks
- Restlessness, impaired concentration, and purposeless activity
- Irritability, depression, anger, or despair
- Insomnia
‘Dissociative’ symptoms:
- Emotional numbness and ‘being in a daze’
- Reduced awareness of surroundings
- Difficulty in recall of the stressful events
- Depersonalization and derealization
‘Re-experiencing’ symptoms":
- Flashbacks
- Recurrent images or thoughts
- Disturbing dreams
Avoidance of reminders of the stressful events
Maladaptive coping strategies
Acute stress disorder is diagnos when symptoms last from 2 days up to 4 weeks. [1]
Clinical Examination
Clinical Examination
Acute Stress Disorder (ASD) does not have specific physical examination findings. The diagnosis is primarily based on clinical interview and assessment of the patient’s history and symptoms. However, the clinical examination can help assess the patient’s overall mental and physical state, rule out other medical conditions, and identify any co-occurring disorders.
Mental Status Examination:
- Appearance and Behavior: Assess for signs of distress, agitation, or withdrawal.
- Mood and Affect: Assess for anxiety, depression, irritability, or emotional lability.
- Thought Content: Assess for intrusive thoughts, flashbacks, nightmares, or suicidal ideation.
- Perceptual Disturbances: Assess for hallucinations or dissociative experiences.
- Cognition: Assess for attention, concentration, and memory deficits.
- Insight and Judgment: Assess the patient’s understanding of their symptoms and their ability to make sound decisions.
Physical Examination:
- Vital Signs: Assess for elevated heart rate, blood pressure, and respiratory rate, which may be present due to anxiety.
- Neurological Examination: Assess for any neurological deficits that may mimic or contribute to ASD symptoms.
- General Physical Examination: Assess for any underlying medical conditions that may be contributing to or exacerbating the patient’s symptoms.
Assessment of Trauma History:
- Inquire about the nature of the traumatic event: Obtain a detailed account of the event, including the patient’s experience, emotions, and reactions.
- Assess the severity and duration of the trauma exposure: Determine the extent to which the event threatened the patient’s life or physical integrity and how long the exposure lasted.
- Identify any previous trauma history: Inquire about any previous traumatic experiences that may increase the patient’s vulnerability to ASD.
Additional Considerations:
- Collateral Information: If possible, obtain information from family members, friends, or witnesses to corroborate the patient’s self-report and gain a broader understanding of their functioning.
- Screening Tools: Consider using standardized screening tools for ASD, such as the Acute Stress Disorder Scale (ASDS) or the Acute Stress Disorder Interview (ASDI), to aid in diagnosis.
It is important to note that the clinical examination is just one component of the assessment process for ASD. A comprehensive evaluation also includes a thorough clinical interview, review of the patient’s medical and psychiatric history, and consideration of cultural and social factors that may influence the presentation of symptoms.[7]
Diagnosis
Diagnosis
DSM-IV diagnostic criteria for acute stress disorder:
1. Exposure to a traumatic event in which the following were present:
- Either Actual or threatened death or serious injury, or a threat to the physical integrity of self or others;
- The person’s response involved intense fear, helplessness, or horror.
2. Due to the distressing event, the individual has at least three of the following dissociative symptoms:
- A subjective sense of numbing, detachment, or absence of emotional responsiveness;
- A reduction in awareness of his or her surroundings;
- Derealization;
- Depersonalization;
- Dissociative amnesia.
3. The traumatic event is persistently re-experienced through recurrent images, thoughts, dreams, illusions, flashback episodes, or a sense of reliving the experience.
4. Marked avoidance of stimuli that arouse recollections of the trauma.
5. After that, Marked symptoms of anxiety or increased arousal.
6. The disturbance leads to, clinically significant distress.
7. The disturbance lasts for a minimum of 2 days and a maximum of 4 weeks and occurs within 4 weeks of the traumatic event.
8. The disturbance is not due to the direct physiological effects of a substance or a general medical condition, is not better accounted for by Brief Psychotic Disorder, and is not merely an exacerbation of a pre-existing Axis I or Axis II disorder. [1]
Differential Diagnosis
Differential Diagnoses
Adjustment Disorders
Brief Psychotic Disorder
Dissociative Disorders
Postconcussion Syndrome
Posttraumatic Stress Disorder
Substance abuse[4]
Complications
Complication
Acute Stress Disorder (ASD) can lead to several complications if left untreated or inadequately managed. These complications can affect various aspects of an individual’s life, including mental health, physical health, and overall well-being.
Complications of Acute Stress Disorder (ASD):
Development of Post-Traumatic Stress Disorder (PTSD): ASD is a precursor to PTSD, and individuals with untreated ASD are at a significantly higher risk of developing PTSD. PTSD is a chronic condition with more persistent and severe symptoms that can significantly impair functioning.
Other Mental Health Disorders: ASD can increase the risk of developing other mental health disorders, including:
- Major Depressive Disorder: Individuals with ASD may experience persistent feelings of sadness, hopelessness, and loss of interest in activities.
- Anxiety Disorders: ASD can trigger or worsen anxiety disorders, such as generalized anxiety disorder, panic disorder, or social anxiety disorder.
- Substance Use Disorders: Individuals may turn to substance use as a way to cope with the distressing symptoms of ASD, leading to addiction and dependence.
Physical Health Problems: The stress response associated with ASD can have negative impacts on physical health, including:
- Cardiovascular Problems: Increased risk of high blood pressure, heart disease, and stroke.
- Gastrointestinal Problems: Increased risk of irritable bowel syndrome, ulcers, and other digestive issues.
- Immune System Suppression: Stress can weaken the immune system, making individuals more susceptible to infections and illnesses.
Impaired Functioning: ASD can significantly impair an individual’s ability to function in daily life, affecting their work, relationships, and social interactions.
Suicidal Thoughts and Behaviors: In severe cases, individuals with ASD may experience suicidal ideation or engage in self-harming behaviors.
It is important to seek professional help if you or someone you know is experiencing symptoms of ASD. Early intervention can significantly improve outcomes and prevent the development of long-term complications.[7]
Investigations
Investigation
Acute Stress Disorder (ASD) is primarily diagnosed based on clinical interview and assessment of the patient’s history and symptoms following a traumatic event. There are no specific laboratory or imaging tests to definitively diagnose ASD. However, certain investigations may be helpful in ruling out other medical conditions that could mimic or contribute to the symptoms of ASD, as well as identifying any co-occurring disorders.
Clinical Interview and Assessment:
- A thorough clinical interview is the primary tool for diagnosing ASD. The clinician will inquire about the nature of the traumatic event, the patient’s symptoms, and their impact on daily functioning.
- The clinician may use structured or semi-structured interviews, such as the Clinician-Administered PTSD Scale (CAPS) or the Acute Stress Disorder Interview (ASDI), to assess the presence and severity of ASD symptoms.
Mental Status Examination:
- A comprehensive mental status examination is conducted to assess the patient’s overall mental state, including their appearance, behavior, mood, affect, thought content, perception, cognition, insight, and judgment.
Physical Examination:
- A physical examination may be performed to rule out any underlying medical conditions that could be contributing to the patient’s symptoms, such as head injury, substance intoxication, or withdrawal.
Laboratory Tests:
- Toxicology Screening: To rule out substance-induced symptoms.
- Complete Blood Count (CBC): To assess for anemia or infection.
- Thyroid Function Tests: To rule out hyperthyroidism or hypothyroidism, which can cause anxiety-like symptoms.
- Electrolyte Panel: To assess for electrolyte imbalances, which can affect neurological function.
Neuroimaging:
- Brain Imaging (e.g., MRI, CT): While not routinely used, brain imaging may be considered in cases where there is a suspicion of underlying neurological conditions or head trauma.
Psychological Assessment:
- Questionnaires and Scales: Standardized questionnaires, such as the PTSD Checklist for DSM-5 (PCL-5) or the Impact of Event Scale-Revised (IES-R), can be used to assess the severity of symptoms and monitor treatment progress.
It is important to note that these investigations are primarily aimed at ruling out other conditions and supporting the clinical diagnosis of ASD. The final diagnosis is based on a comprehensive assessment of the patient’s history, symptoms, and response to treatment.[7]
Treatment
Treatment
General measures:
Provide emotional support:
- Usually the person can be comforted effectively by relatives or friends, and can talk to them about the stressful experience.
- Meanwhile, If no close friend or relative is available, or if the response is severe, comfort may be offered by a healthcare professional.
- At last, It is important to explain the course and prognosis of an acute stress disorder.
Provide practical support:
- The period after a traumatic event is usually very busy and confusing.
- The person involved will need advice regarding police procedures, support in obtaining medical care, help with insurance claims, assistance with dealing with the media, additionally, help with domestic tasks.
Help with residual problems:
- Sometimes an acutely stressful situation results in lasting adversity to which the person has to adjust; for example, a serious car accident may lead to permanent disability.
- When this happens the treatment of an acute reaction should be followed by help in readjustment.
Psychological treatments:
Encourage recall i.e.:
- As anxiety is reduced, the person is usually able to recall and come to terms with the experience.
- When memories of the events remain fragmented, help may be needed to remember the events and integrate them into memory.
Develop more effective coping strategies i.e.:
- As explained above, in a time of crisis some people will use maladaptive coping strategies such as using substances.
- It is important to try and help them develop more productive strategies for example, provide a supportive atmosphere for working through problems, and encourage recall of events.
- Specific counselling is available in these situations and is called crisis intervention.
Debriefing i.e.:
- Until recently, a type of counselling know as debriefing was often make widely available after stressful events.
- The aim was to promote adaptation to the traumatic event, and it was usually gave within 24 to 72 hours of the trauma.
- Subjects talked about the stressful events and were encourage to express their thoughts and feelings at the time and since.
- A Cochrane review of randomized controlled trials found that whilst the majority of people said they found the counselling useful, additionally, it did not reduce the proportion of patients developing PTSD.
- UK guidance is now that debriefing should not routinely offered to patients.
Cognitive behavioural therapy i.e.:
- CBT differs from debriefing crucially in its emphasis on integrating recovered memories with existing ones, also on self-help.
- Evidence suggests the most effective strategy is a brief intervention, typically five sessions of individual therapy.
- Studies vary in their results but on average CBT reduces the proportion of people developing PTSD by 20 – 50 % .
Pharmacological treatments:
There has been very little research done on to which pharmacological interventions are effective in acute stress disorder.
Anxiolytics i.e.:
- A short course (3–5 days) of a benzodiazepine may be indicated in patients with a high level of anxiety immediately after the event.
- Occasionally, insomnia is severe, and a hypnotic drug (e.g. temazepam) should be given, but again only for a short period to avoid the development of tolerance and dependence.
Antidepressants i.e.:
- SSRIs are the most effective drug treatment for PTSD.
- Consider prescribing an SSRI if the symptoms continue to be severe, there is evidence of either depression, or the patient is too unwell to engage in psychological therapy.
- It is also an option for those patients who fail to improve after CBT. [1]
Prevention
Prevention
Research on prevention strategies for stress-related disorders has taken a number of avenues, including intervention before and after trauma and the use of both psychosocial and somatic approaches.
Despite advances in neurobiological understanding of response to trauma, clinical evidence for preventive interventions remains sparse. This review provides an overview of prevention approaches also summarizes the existing literature on prevention of ASD and PTSD, including clinical and preclinical studies.
Given the potential benefits to trauma survivors and society, the development of effective preventive interventions should be given greater priority.[5]
Early intervention and treatment of ASD are crucial to prevent the development of these complications. Effective treatments for ASD include:
- Cognitive Behavioral Therapy (CBT): CBT helps individuals identify and change negative thought patterns and behaviors associated with the traumatic event.
- Eye Movement Desensitization and Reprocessing (EMDR): EMDR uses bilateral stimulation (e.g., eye movements) to help individuals process traumatic memories and reduce associated distress.
- Medications: In some cases, medications such as antidepressants or anti-anxiety medications may be prescribed to manage specific symptoms of ASD.[7]
Homeopathic Treatment
Homeopathic Treatment of Acute Stress Disorder
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Acute Stress Disorder:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
1. Arsenicum album:
- This remedy covers a lot of fears and anxieties that lead to obsessive-compulsive behaviors. Your mind can’t stop playing the same trauma over and over again.
- You can only focus on the negative-worrying, perhaps, that something bad will happen either to you or a loved one. In addition, you may overly concerned about germs or your health, to the point of hypochondria.
2. Aconitum napellus:
- Often follows a sudden, unexpected trauma, such as an earthquake or car accident.
- A deep fear of death sends you into a panic state.
- You can feel your heart beating at a rapid pace that comes on all of a sudden.
- You may feel faint, along with perspiration and trembling.
- Things that would not have bothered you before can trigger panic attacks, such as driving on a freeway, getting into an elevator, or flying in an airplane.
- "I went to the supermarket and on the way in the car, I thought I would die," is the type of statement you might make.
3. Argentum nitricum:
- Very anxious, especially about health.
- I call it "Monkey Brain," when patients can only focus on their health or lack of it, convinced that every minor ache or ailment is the symptom of a fatal disease, and tend to go from doctor to doctor to get diagnoses.
- Lots of fear- for example heights, crowds, small spaces, etc.
- They have a need to express their feelings in an impulsive way with anyone who will listen.
- They have a feeling of impending doom, such as some evil force is coming for them.
4. Stramonium:
- Night fears and nightmares.
- Fear of the dark, animals, violence, especially when being alone.
- Terrifying nightmares, waking up panic-stricken and full of anxiety. Similarly, anxiety turns into destructive and malicious behavior, an out-of-control feeling, and anger.
- The fears are so deep that they bring on panic.
- Patients can’t stand to be alone. Their reaction to fear is violence.
- They feel they need to protect themselves, so are always on the attack.
5. Lyssinum:
- Hypersensitive to sound, light, smell, also even others’ emotions. Furthermore, their emotions are raw, like exposed nerves.
- They feel they are being torment or ridiculed, also have a dread that something bad will happen to them.
- May have many phobias, such as fear of driving, flying, injury, suffocation.
- May also fear being alone, even though they tend to do better by themselves in a quiet room without much light.
- They have an irrational fear of water, either seeing it or just thinking of it.
- They have bitten by an animal and had fears since then.
Diet & Regimen
Diet & Regimen
Foods that are promoted on the Mediterranean diet are the same foods that are good to eat when you’re stressed: fish, poultry, fruits, vegetables, fruits, whole grains, and healthy fats.
In fact, patients to adopt a Mediterranean diet for overall health and wellness, including stress relief.
The goal is to eat foods that reduce inflammation in your body, thus reducing cortisol levels.
In contrast, some foods raise cortisol levels. Foods that cause stress on your body include:
- Alcohol.
- Caffeine.
- High-sugar foods.
- Simple carbs, such as cakes and pastries.
- Soda.
Do's & Don'ts
Do’s & Don’ts
Managing Acute Stress Disorder (ASD) involves a combination of self-care strategies, professional support, and understanding the do’s and don’ts to facilitate recovery.
Do’s
- Do seek professional help: A mental health professional can provide accurate diagnosis, recommend appropriate treatment options (such as cognitive-behavioral therapy or EMDR), and offer ongoing support.
- Do practice relaxation techniques: Deep breathing exercises, meditation, mindfulness, and yoga can help reduce physiological arousal and manage stress.
- Do maintain a healthy lifestyle: Eat nutritious meals, exercise regularly, and get adequate sleep to support your overall well-being and resilience.
- Do connect with supportive people: Talk to trusted friends, family members, or support groups who can offer empathy, understanding, and encouragement.
- Do engage in enjoyable activities: Participating in hobbies and activities you enjoy can provide distraction, relaxation, and a sense of normalcy.
- Do be patient with yourself: Healing from trauma takes time, and it’s normal to experience setbacks. Be kind to yourself and acknowledge your progress.
Don’ts:
- Don’t isolate yourself: Withdrawing from social interactions can worsen feelings of loneliness and despair.
- Don’t use substances to cope: Alcohol or drugs may provide temporary relief, but they can exacerbate symptoms and hinder long-term recovery.
- Don’t blame yourself: ASD is a natural response to a traumatic event, and it’s not your fault. Avoid self-blame and focus on healing.
- Don’t avoid talking about the trauma: While it can be painful, discussing the traumatic event with a trusted person or therapist can be an important part of the healing process.
- Don’t make major life decisions: Trauma can impair judgment and decision-making abilities. Postpone significant decisions until you feel more emotionally stable.
Remember, everyone’s journey with ASD is unique, and what works for one person may not work for another. It’s essential to find strategies that resonate with you and seek professional guidance to develop a personalized recovery plan.[8]
Terminology
Terminology
Terminologies and Their Meanings
In the context of Acute Stress Disorder (ASD) and homeopathic treatment, several key terms are used:
Clinical Diagnoses:
- Acute Stress Disorder (ASD): A mental health condition characterized by intense emotional and physical reactions that develop within one month of experiencing or witnessing a traumatic event.
- Post-Traumatic Stress Disorder (PTSD): A long-term condition that may develop after experiencing a traumatic event, involving similar symptoms to ASD but lasting for more than one month.
More General Terms:
- Anxiety Disorders: A broad category of mental health conditions characterized by excessive worry, fear, and related behavioral disturbances.
- Adjustment Disorders: Difficulty coping with and adjusting to a stressful life event, often involving emotional or behavioral symptoms.
Informal Terms:
- Traumatic Stress Reaction: A general term referring to the psychological and physiological responses that occur after experiencing a traumatic event.
- Emotional Overwhelm: A state of intense emotional distress, often triggered by a traumatic event or ongoing stress, leading to difficulty coping and functioning.
Additional Terms:
- Dissociation: A mental process where a person disconnects from their thoughts, feelings, memories, or sense of self, often as a response to trauma.
- Depersonalization: A feeling of detachment or estrangement from oneself, as if observing one’s body or thoughts from a distance.
- Derealization: A feeling of unreality or detachment from one’s surroundings, as if the world is dreamlike or unreal.
- Flashback: A vivid, intrusive re-experiencing of a traumatic event, often accompanied by intense emotions and physiological reactions.
- Hypervigilance: A state of heightened alertness and sensitivity to potential threats, often seen in individuals with ASD or PTSD.
Miasmatic Tendency: In homeopathy, this refers to a person’s inherited or acquired predisposition to certain disease patterns, which can influence their overall health and response to treatment.
Key Homeopathic Terms:
- Remedies: Substances used in homeopathy to stimulate the body’s natural healing abilities.
- Potency: The strength or dilution of a homeopathic remedy.
- Constitutional Indications: The characteristic physical and mental traits of an individual, considered important in selecting the most appropriate homeopathic remedy.
References
References
- Psychiatry, Fourth Edition- Oxford Medical Publications – SRG- by Geddes, Jonathan Price, Rebecca McKnight / Ch 23.
- https://www.betternutrition.com/natural-rx/homeopathic-remedies-stress-anxiety-ptsd
- https://www.ncbi.nlm.nih.gov/books/NBK560815/
- https://emedicine.medscape.com/article/2192581-differential
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4677144/
- Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) Publisher: American Psychiatric Association Year of Publication: 2013
- Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry (11th Edition) ,Authors: Benjamin J. Sadock, Virginia A. Sadock, Pedro Ruiz ,Publisher: Wolters Kluwer, Year of Publication: 2014
- Coping with Trauma-Related Dissociation: A Practical Guide for Healing and Recovery (1st Edition,)Authors: Suzette Boon, Onno van der Hart, Ellert R.S. Nijenhuis,Publisher: W. W. Norton & Company,Year of Publication: 2012
- Trauma- and Stressor-Related Disorders (Section from Kaplan & Sadock’s Comprehensive Textbook of Psychiatry, 10th Edition)
Editors: Benjamin J. Sadock, Virginia A. Sadock, Pedro Ruiz
Publisher: Wolters Kluwer(2017) - The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma
Author: Bessel van der Kolk M.D.
Publisher: Viking
Year of Publication: 2014
Also Search As
Also Search as
Specific Search Terms:
- Acute Stress Disorder Homeopathy: This is the most direct and targeted search term for the article.
- Homeopathic Remedies for ASD: This focuses on the treatment aspect.
- Homeopathy for Trauma: This broader term could attract those looking for alternative treatments for trauma-related conditions.
- Natural Treatment for Acute Stress: This appeals to those interested in holistic or non-conventional approaches.
Related Search Phrases:
- Can homeopathy help with ASD?
- What are homeopathic remedies for emotional trauma?
- How to manage acute stress naturally?
- Alternative treatments for stress disorders
Additional Tips:
- Include location (if relevant): If the article is targeted towards a specific region (e.g., "Homeopathy for ASD in India"), including the location in the search can help.
- Use synonyms: Try different terms for stress (e.g., anxiety, trauma) or homeopathy (e.g., homeopathic medicine, natural remedies) to widen the search.
- Check related searches: Look at the "Searches related to…" section at the bottom of the search results page for more ideas.
Where to Optimize for Search:
- Title: Make sure the article’s title includes the main keywords (Acute Stress Disorder, Homeopathy).
- Meta Description: This short summary appears in search results and should entice users to click.
- Headers and Subheaders: Use H2 and H3 tags with relevant keywords throughout the article.
- Image Alt Text: Describe images using relevant keywords for better search engine indexing.
People can search for this article in several ways, depending on their needs and where the article is published:
Using Search Engines:
- Specific Keywords: Directly search on Google, Bing, or other search engines using phrases like "acute stress disorder homeopathy," "homeopathic remedies for ASD," or "natural treatment for acute stress."
- Broader Terms: Use more general terms like "homeopathy for trauma" or "alternative stress disorder treatments."
- Question Format: Type questions like "Can homeopathy help with ASD?" or "What are natural ways to manage acute stress?"
Within a Website or Publication:
- Site Search Bar: Most websites have a search bar. Use the same keywords mentioned above to search within the site where the article is published.
- Category or Tag Search: If the website organizes content by category or tags, look for sections related to homeopathy, mental health, or stress disorders.
Through Social Media:
- Hashtags: Search relevant hashtags on platforms like Twitter or Instagram (e.g., #homeopathy, #ASD, #stressrelief).
- Groups and Communities: Join online groups or communities focused on homeopathy or mental health, and search for discussions related to acute stress disorder.
Using Academic Databases:
- Google Scholar: This database is a great resource for finding scholarly articles. Search using keywords like "acute stress disorder homeopathic treatment" or similar phrases.
- Other Databases: If you have access to medical or academic databases, search them using relevant keywords.
By Referral:
- Word-of-Mouth: If someone recommends the article to you, they might tell you the specific title or author, making it easier to find.
Remember: The effectiveness of these methods depends on how well the article is optimized for search engines, the platform it’s published on, and the specific search terms used.
Frequently Asked Questions (FAQ)
What is Acute Stress Disorder?
Acute stress disorder is an abnormal reaction to sudden stressful events.
Causes of acute stress disorder?
Causes
ASD is caused by exposure to a traumatic event, such as accidents, natural disasters, violence, or combat. Not everyone who experiences trauma develops ASD, as individual resilience and coping mechanisms play a role.
Is homeopathic treatment for ASD safe?
Homeopathic remedies are generally safe and do not have significant side effects when used appropriately. However, it is essential to consult a qualified homeopath for proper diagnosis and treatment.
What are the symptoms of Acute Stress Disorder?
- Anxiety and panic attacks
- Restlessness, impaired concentration
- Purposeless activity
- Irritability, depression, anger, despair
- Insomnia
- Reduced awareness of surroundings
- Difficulty in recall of the stressful events
- Disturbing dreams
What are the risk factors for developing acute stress disorder?
Risk factors
- Severity and duration of the trauma
- Lack of social support
- History of previous trauma or mental health conditions
- Certain genetic predispositions
What can I expect during a homeopathic consultation for ASD?
During a homeopathic consultation, the homeopath will take a detailed case history, including the nature of the traumatic event, symptoms experienced, and overall health condition. This information helps in selecting the most appropriate homeopathic remedies.
Homeopathic Medicines use by Homeopathic Doctors in treatment of Acute Stress Disorder?
Homoeopathic Medicine For Acute Stress Disorder
- Arsenicum album
- Aconitum napellus
- Argentum nitricum
- Stramonium
- Lyssinum
