Insomnia
Definition
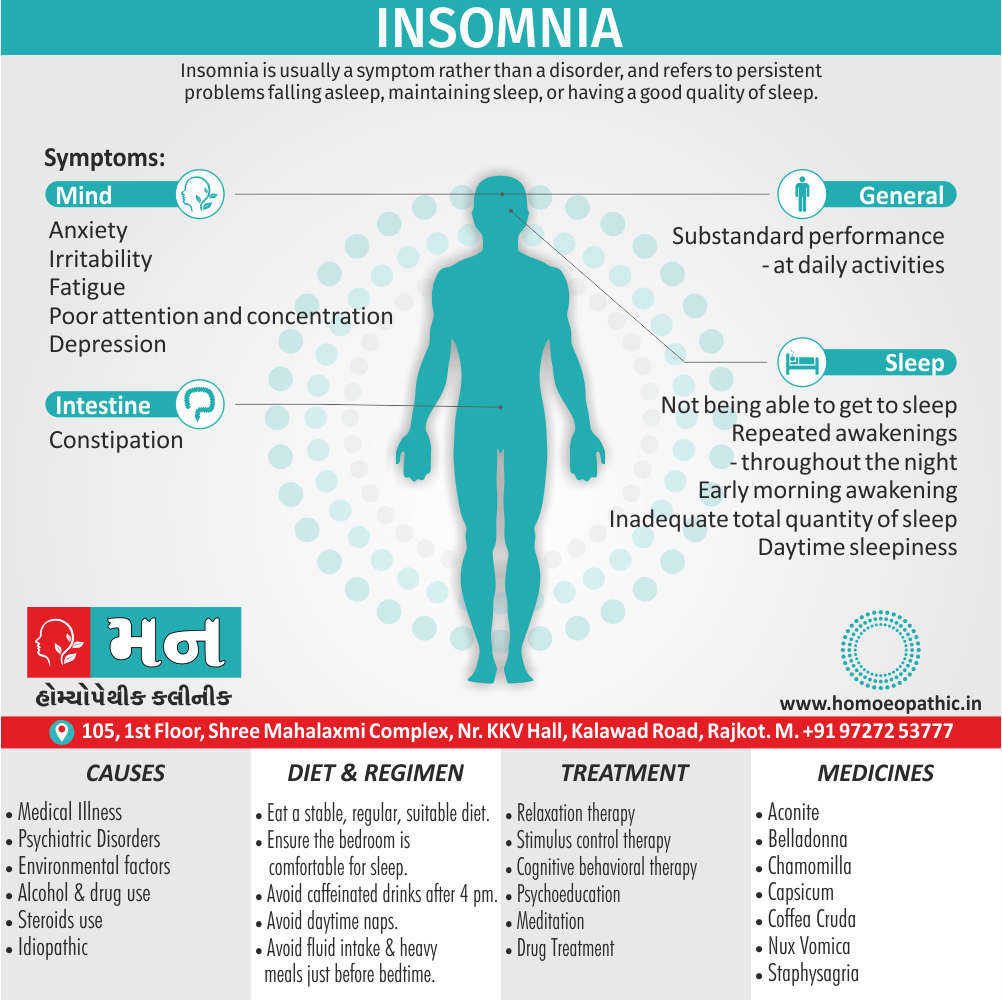
Insomnia is usually a symptom rather than a disorder, and refers to persistent problems falling asleep, maintaining sleep, or having a good quality of sleep.
It is extremely common, with one-third of adults experiencing significant insomnia at some point.
Sleep disruption may be a primary disorder, but is more often secondary to another medical or psychiatric condition. [1]
Here are some synonyms for insomnia depending on the nuance you want to convey:
- Sleeplessness: This is the most common and straightforward synonym.
- Sleep difficulties: This is a broader term that encompasses various problems with sleep, not just the inability to fall asleep.
- Wakefulness: This emphasizes the state of being awake when you should be sleeping.
- Restlessness: This highlights the inability to relax and settle down for sleep.
Less common synonyms:
- Insomnolence: This is a more formal term for insomnia.
- Agrypnia: This is a more technical term, rarely used in everyday conversation.
Informal options:
- Can’t catch any Zzz’s: This is a playful way to say you’re having trouble sleeping.
- Tossing and turning: This describes physical restlessness during sleep attempts.
Choosing the best option:
- For most contexts, "sleeplessness" is a good choice.
- If you want to emphasize specific aspects like difficulty falling asleep or staying asleep, "sleep difficulties" or "wakefulness" might be better.
- In formal writing, "insomnolence" might be appropriate.
- Use informal options cautiously, depending on the audience and tone.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Insomnia
Insomnia is also known as the Disorder of Initiation and/or Maintenance of Sleep ( DIMS).
Insomnia means one or more of the following:
1. Difficulty in initiating sleep (going-off to sleep).
2. Difficulty in maintaining sleep (remaining asleep).
This can include both:
a. Frequent awakenings during the night, and
b. Early morning awakening.
3. Non-restorative sleep where despite an adequate duration of sleep, there is a feeling of not having rested fully (poor quality sleep).
Insomnia is very common, with nearly 15-30% of general population complaining of a period of insomnia per year requiring treatment.
It is required for diagnosis that sleep disturbance occurs at least three times a week for at least 1 month, and that it causes either marked distress or interferes with social and occupational functioning.
The ICD-10 classification defines non-organic insomnia as a condition of unsatisfactory quantity also quality of sleep, which persists for a considerable period of time, including difficulty falling asleep, difficulty staying asleep, or early final wakening. [2]
Epidemiology
Epidemiology
The epidemiology of insomnia in India is a complex issue, with various factors contributing to its prevalence and presentation. A key reference in this field is:
Epidemiology of insomnia: A review of the Global and Indian scenario by D Bhattacharya, M K Sen, and J C Suri (2013).
This review, published in the Indian Journal of Sleep Medicine, offers a comprehensive overview of the burden of insomnia in India, highlighting the following key points:
- Prevalence: Insomnia is a highly prevalent disorder in India, although exact figures vary depending on the diagnostic criteria used. The review notes that several factors, including age, gender, and psychiatric comorbidities, influence the prevalence rates.
- Risk Factors: The study identifies various risk factors for insomnia in the Indian context, such as increasing urbanization, stress associated with modern life, and the presence of other medical or psychiatric conditions.
- Impact: The review emphasizes the significant impact of insomnia on an individual’s quality of life, including increased work absenteeism, accidents, family problems, and overall economic burden.
The authors conclude by calling for more research to understand the specific needs of the Indian population and develop culturally appropriate interventions to address this growing public health concern. [3]
Causes
Causes
1. Medical illnesses:
- Any painful or uncomfortable condition
- Heart diseases
- Respiratory diseases
- Rheumatic and musculoskeletal disease
- Old age
- Either Brain stem or hypothalamic lesions
- Delirium
- PMS ( in other words, Periodic movements in sleep)
2. Alcohol and drug use:
- Drug or alcohol withdrawal syndrome
- Delirium tremens
- Amphetamine or other stimulants, e.g. caffeine
- Chronic alcoholism
3. Current medication:
Such as: fluoxetine, steroids, theophylline, propranolol
4. Psychiatric disorders:
- Mania (may not complain of decrease in sleep, as there is often a decreased need for sleep)
- Major depression (diffi culty in maintenance of sleep is more prominent, although diffi culty in initiating sleep is also present)
- Dysthymia (difficulty in initiating sleep is characteristic)
- Anxiety disorder (difficulty in initiating sleep is common)
- Stressful life situation (may cause temporary insomnia)
5. Idiopathic insomnia [2]
Others:
Primary (idiopathic) insomnia i.e.:
No cause found (very rare)
Paradoxical insomnia i.e.:
Complaint of poor sleep despite normal patterns
Psychophysiological insomnia i.e.:
Learned sleep prevention behaviours
Sleep apnoea syndromes, e.g. obstructive sleep apnoea i.e.:
Central alveolar hypoventilation syndrome (Ondine’s curse)
Restless leg syndrome i.e.:
Painful sensations in legs which prevent sleep (in other words, Ekbom’s syndrome)
Periodic limb movement syndrome i.e.:
Episodes of repeated, stereotyped leg movements which prevent sleep, common over 60 years
Environmental i.e.:
Poor sleep hygiene, also stress
Hormonal i.e.:
Menstruation or menopause related
Circadian rhythm disturbance i.e.:
Jet lag, shift work
Rebound insomnia from overuse of hypnotics [1]
Types
Types
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), published by the American Psychiatric Association in 2013, outlines the following types of insomnia:
Chronic Insomnia Disorder: This is characterized by difficulty initiating or maintaining sleep, or nonrestorative sleep, occurring at least three nights per week for at least three months.
Short-Term Insomnia Disorder: This involves the same sleep difficulties as chronic insomnia but lasts for less than three months.
Other Insomnia Disorder: This category encompasses sleep disturbances that do not meet the criteria for chronic or short-term insomnia but still cause significant distress or impairment. [4]
Risk Factors
Risk factors for insomnia
Several risk factors for insomnia:
Age: The risk of insomnia increases with age. Older adults are more likely to experience changes in sleep patterns, medical conditions, and medications that can disrupt sleep.
Sex: Women are more prone to insomnia than men, possibly due to hormonal fluctuations throughout their lives, including menstruation, pregnancy, and menopause.
Genetics: Family history of insomnia increases the likelihood of developing the disorder. Certain genes may influence sleep regulation and predispose individuals to insomnia.
Mental Health Conditions: Mental health disorders like anxiety, depression, and post-traumatic stress disorder (PTSD) are strongly associated with insomnia.
Medical Conditions: Chronic pain, respiratory problems, heart disease, and neurological disorders can disrupt sleep and contribute to insomnia.
Medications: Certain medications, such as antidepressants, stimulants, and corticosteroids, can interfere with sleep.
Lifestyle Factors: Irregular sleep schedules, caffeine and alcohol consumption, nicotine use, and excessive screen time before bed can negatively impact sleep. [5]
Pathogenesis
Pathogenesis of Insomnia
- Hyperarousal: This is a core feature, involving heightened physiological and cognitive activation. This can manifest as increased heart rate, metabolism, and brain activity, alongside racing thoughts and worries.
- Dysregulated Sleep-Wake System: The body’s natural sleep-wake cycle is disrupted. This can involve alterations in the timing and release of sleep-promoting substances like melatonin, as well as imbalances in brain regions controlling sleep.
- Neurotransmitter Imbalance: Neurotransmitters like GABA (calming), glutamate (excitatory), and orexin (wake-promoting) are implicated. Imbalances in these can impair the ability to relax and fall asleep, or maintain sleep throughout the night.
- Conditioning Factors: Negative associations with bedtime or the bedroom can develop, where cues that should promote sleep instead trigger anxiety and wakefulness. This can be exacerbated by maladaptive behaviors like excessive time in bed while awake. [6]
Pathophysiology
Pathophysiology of Insomnia
- . Hyperarousal:Insomnia is often associated with a state of hyperarousal, both physically and mentally.This heightened arousal can manifest as increased heart rate, body temperature, and muscle tension. It can also involve cognitive processes like racing thoughts, worry, and rumination.
- Dysregulation of Sleep-Wake Cycle:Insomnia can be linked to disruptions in the body’s natural sleep-wake cycle, also known as the circadian rhythm.This can involve problems with the production and regulation of sleep-promoting hormones like melatonin, as well as imbalances in other neurotransmitters like serotonin and norepinephrine.
- Neurobiological Changes:Research suggests that insomnia may involve changes in brain activity and structure.These changes can affect areas of the brain responsible for regulating sleep, arousal, and emotions. For example, studies have shown increased activity in the amygdala, a region associated with fear and anxiety, and decreased activity in the prefrontal cortex, which is involved in cognitive control and decision-making.
- Psychological Factors:Psychological factors such as stress, anxiety, depression, and trauma can contribute to insomnia.These factors can trigger or exacerbate hyperarousal, disrupt the sleep-wake cycle, and lead to changes in brain activity.
- Medical and Environmental Factors:Various medical conditions, such as chronic pain, respiratory problems, and hormonal imbalances, can contribute to insomnia.Environmental factors like noise, light, and uncomfortable temperatures can also disrupt sleep. [6]
Clinical Features
Clinical Features of Insomnia
Difficulty initiating sleep: This refers to the struggle to fall asleep at the desired bedtime. It can involve prolonged periods of lying awake before sleep onset.
Difficulty maintaining sleep: This is characterized by frequent awakenings during the night, often with difficulty returning to sleep. It can lead to fragmented and non-restorative sleep.
Early morning awakening: This involves waking up earlier than desired, with an inability to fall back asleep. This can leave individuals feeling unrefreshed and tired throughout the day.
Daytime impairment: This encompasses a wide range of symptoms resulting from poor sleep quality or quantity. These can include fatigue, difficulty concentrating, irritability, mood disturbances, and impaired cognitive function. [7]
Sign & Symptoms
Sign & Symptoms
The patient may complain of:
- Not being able to get to sleep
- Repeated awakenings throughout the night
- Early morning awakening
- Inadequate total quantity of sleep
- Daytime sleepiness
- Irritability
- Fatigue
- Poor attention and concentration
- Substandard performance at daily activities
The patient is usually distressed and preoccupied by sleep problems, and in severe cases social or occupational functioning is negatively affected.
Rarely, the consequences will have been severe; for example, loss of a job due to poor performance secondary to fatigue.
There are often comorbid symptoms of anxiety related to the attempts to obtain adequate sleep.
Clinical Examination
Clinical Examination
While insomnia is primarily diagnosed through clinical history and sleep diaries, a physical examination can help rule out underlying medical conditions contributing to sleep disturbances.
General Observation: Look for signs of fatigue, anxiety, or depression, which are often associated with insomnia.
Vital Signs: Measure blood pressure, heart rate, and respiratory rate to detect any abnormalities that could affect sleep.
Head and Neck Examination: Check for signs of nasal congestion, enlarged tonsils, or a deviated septum, which can contribute to sleep apnea.
Cardiovascular Examination:
Listen for murmurs or irregular heartbeats, which could be associated with sleep disturbances.
Respiratory Examination: Look for signs of respiratory distress or wheezing, which could indicate asthma or other breathing problems affecting sleep.
Abdominal Examination: Palpate for masses or tenderness, which could suggest gastrointestinal issues contributing to sleep problems.
Neurological Examination: Assess reflexes, muscle strength, and coordination to rule out any neurological conditions affecting sleep. [8]
Diagnosis
Diagnosis
According to DSM-IV criteria, the following criteria must be met irrespective of the type of insomnia:
- The predominant complaint is difficulty initiating or maintaining sleep.
- It has been present for at least 1 month.
- It is accompanied by daytime fatigue or impaired daytime functioning.
- Sleep disturbance causes clinically significant distress in social or occupational functioning.
- The disturbance is not better accounted for by another sleep disorder.
Severe and chronic insomnia requires a minimum duration of 6 months with problems on at least three nights of the week. [1]
Differential Diagnosis
Differential Diagnosis
Psychiatric Disorders:
Mood disorders (e.g., major depressive disorder, bipolar disorder)
Anxiety disorders (e.g., generalized anxiety disorder, panic disorder)
Post-traumatic stress disorder (PTSD)
Obsessive-compulsive disorder (OCD)
Neurological Disorders:
Restless legs syndrome (RLS)
Periodic limb movement disorder (PLMD)
Sleep-related breathing disorders (e.g., obstructive sleep apnea)
Narcolepsy
Circadian rhythm sleep-wake disorders
Central nervous system hypersomnia
Medical Conditions:
Chronic pain (e.g., fibromyalgia, arthritis)
Gastrointestinal disorders (e.g., gastroesophageal reflux disease)
Endocrine disorders (e.g., hyperthyroidism)
Respiratory disorders (e.g., asthma)
Cardiovascular disorders (e.g., congestive heart failure)
Substance-Related Disorders:
Stimulant use (e.g., caffeine, amphetamines)
Alcohol withdrawal
Medication-induced sleep disturbances
Other Sleep Disorders:
Parasomnias (e.g., sleepwalking, sleep terrors)
Sleep-related movement disorders (e.g., bruxism) [9]
Complications
Complications of Insomnia
- Mental Health Disorders: Insomnia can exacerbate existing mental health conditions like depression and anxiety, or increase the risk of developing these disorders.
- Cognitive Impairment: Chronic sleep deprivation can lead to difficulties with attention, concentration, memory, and decision-making.
- Increased Risk of Accidents: Insomnia can impair daytime functioning, leading to slowed reaction times and an increased risk of accidents, especially while driving.
Cardiovascular Problems:
- Insomnia has been linked to an increased risk of hypertension, heart disease, and stroke.
- Metabolic Disorders: Chronic insomnia may contribute to the development of type 2 diabetes and obesity.
- Weakened Immune System: Sleep deprivation can weaken the immune system, making individuals more susceptible to infections and illnesses.
- Reduced Quality of Life: Insomnia can significantly impact an individual’s overall quality of life, leading to fatigue, irritability, and difficulty performing daily tasks. [7]
Investigations
Investigations for Insomnia
Sleep Diary: A self-reported record of sleep patterns, including bedtime, wake time, total sleep time, and any factors that may have affected sleep.
Actigraphy: A wrist-worn device that measures movement and can provide an objective assessment of sleep-wake patterns over several days or weeks.
Polysomnography (PSG): An overnight sleep study that records brain waves, eye movements, muscle activity, heart rate, and breathing patterns to rule out other sleep disorders like sleep apnea.
Multiple Sleep Latency Test (MSLT): A daytime test that measures how quickly a person falls asleep under standardized conditions. This can be helpful in diagnosing narcolepsy, a condition characterized by excessive daytime sleepiness.
Blood tests: May be ordered to rule out underlying medical conditions that can contribute to insomnia, such as thyroid problems or anemia.
Imaging studies (rare): In some cases, brain imaging like MRI or CT scan may be ordered to rule out structural abnormalities that could be affecting sleep.
Additional Considerations:
Psychiatric Evaluation: If a mood or anxiety disorder is suspected as a contributing factor to insomnia, a referral to a mental health professional may be necessary.
Medication Review: It’s essential to review all current medications, including over-the-counter drugs and supplements, as some can interfere with sleep. [6]
Treatment
Treatment
General measures:
- Identification also treatment of the cause of insomnia
- Psychoeducation
Improve sleep hygiene Psychological treatments (first line)
- Relaxation therapy
- Stimulus control therapy
- Sleep restriction
- Cognitive behavioural therapy
Pharmacological treatments (second line)
- Hypnotics: e.g. Benzodiazepines, Non-benzodiazepines
- Antihistamines
- Antidepressants
Sleep Hygiene:
- Ensure the bedroom is comfortable; additionally control light, temperature, and noise.
- Furthermore, Relax away from the day’s stresses for at least 1 hour before bed.
- Avoid caffeinated drinks (also other stimulants) after 4 pm.
- Avoid smoking for an hour before bed.
- Ensure regular exercise (although not late at night).
- Eat a stable, regular, also suitable diet.
- Besides this, Moderate alcohol consumption.
- Have a milky (or other tryptophan-containing) snack before bed.
- Do not take daytime naps.
- Avoid fluid intake also heavy meals just before bedtime.
- Avoid either reading or watching television while in bed.
- Regular times for going to sleep also waking-up [1]
Prevention
Prevention of Insomnia
Maintain a Consistent Sleep Schedule: Go to bed and wake up at the same time each day, even on weekends, to regulate your body’s natural sleep-wake cycle.
Create a Relaxing Bedtime Routine: Engage in calming activities before bed, such as taking a warm bath, reading, or listening to soothing music.
Optimize Your Sleep Environment: Ensure your bedroom is dark, quiet, cool, and comfortable.
Limit Exposure to Light at Night: Avoid bright lights and electronic devices before bed, as the blue light they emit can interfere with sleep.
Avoid Stimulants and Alcohol Before Bed: Caffeine, nicotine, and alcohol can disrupt sleep, so it’s best to avoid them in the hours leading up to bedtime.
Get Regular Exercise: Regular physical activity can improve sleep quality, but avoid exercising too close to bedtime.
Manage Stress: Practice relaxation techniques like deep breathing or meditation to reduce stress and promote relaxation. [10]
Homeopathic Treatment
Homeopathic Treatment
Coffea cruda:
Drinking coffee causes a wakeful, somewhat excited state, and homeopathically prepared coffee is indicated for persons in just that same state.
This state is sometimes caused by joy, pleasurable excitement, or sudden happy surprises as well as by unexpected bad news.
Such a state may also be found in those who drink too much wine or in those over-fatigued from long journeys. When the person lies down to attempt to sleep, the mind is simply awake with a flow of ideas.
Nux vomica:
In the classic Nux vomica type of insomnia, the patient can often fall asleep early, but awakens at 3:00 or 4:00 a.m. with great mental activity or worries.
When the time to rise rolls around, the patient finally feels able to sleep but instead must get up in a tired, irritable state. This type of acute insomnia is commonly brought on by the overuse of drugs and/or stimulants including alcohol, coffee, and wine, or by overwork or excess studying.
The typical Nux vomica patient is irritable, easily angered, and impatient—in short, a grump. They are often chilly, nervous, and excitable.
Aconite:
The patient needing Aconite is restless and excited with an anguished kind of fear. Such a state often comes on in the early stages of a sudden acute illness, often after a chill.
But this state may also be caused by a shock or fright, such as a serious accident, natural disaster, or operation.
Chamomilla:
Those needing Chamomilla are usually in an irritable, uncivil state. They are often frantic with pain or irritability and say they "cannot stand it."
They may have the peculiar symptom of being drowsy during the day, but unable to sleep in spite of sleepiness. This irritability is often found in teething infants who insist on being carried, or in adults who will walk the floor.
Arnica:
This is a well-known remedy for those with bruises and other sorts of trauma, and those needing this remedy for insomnia have often been in a recent accident or had recent exertion and strain.
Such a state is known to travelers as "jet lag." Many of my patients routinely use Arnica for jet lag with great success.
The patient is overtire but cannot sleep and may feel bruised, or the bed may feel too hard. Remember Arnica for those who have nightmares of the accidents or the injuries that they have suffered.
Cocculus:
In generally, Those needing this remedy are sleepless from exhaustion. Additionally, this often comes on from loss of sleep associated with night watching or nursing ill persons.
Their sleep may interrupted by waking and starting. In detail, Patients needing this remedy are often emotionally sensitive, easily offended, also intolerant of contradiction, or they may be extremely sad.
All in all, Motion sickness is a symptom often see in those who will respond to this remedy.
Belladonna:
Patients who need this remedy may sleepy, yet unable to sleep. They often start or jerk suddenly during sleep or when falling asleep.
Teeth-grinding during sleep is a common symptom. They are often restless. This type of sleepless state is often see in those coming down with an acute illness or fever.
Gelsemium:
Those needing this remedy for insomnia are often dull and drowsy, may even trembling.
Yet they cannot get fully to sleep; their bodies are still and they may appear asleep from the outside, but they are on the edge of sleep internally.
Sometimes they start on falling asleep. When finally asleep they may have restless sleep , heavy sleep.
Or, conversely, they may have a sort of nervous irritation, much like the Coffea patient, that comes on from anticipation of an upcoming event.
Capsicum:
Think of homeopathic Capsicum for those with sleeplessness from homesickness or similar emotional states, especially if they have red cheeks.
Staphysagria:
Consider this remedy for those who are sleepless after a fit of anger or after a dispute in which their honor wounded and they suppressed their anger.
Some of the other remedies mentioned, such as Nux vomica, Aconite, Chamomilla, and Coffea also may have sleeplessness after a fit of anger. Look at other characteristics to distinguish one from the other. [3]
Diet & Regimen
Diet & Regimen
Diet
Foods that May Promote Sleep:
- Tryptophan-rich foods: This amino acid helps produce serotonin and melatonin, which are involved in sleep regulation (turkey, milk, nuts, seeds).
- Complex carbohydrates: Can increase tryptophan availability in the brain (whole grains, oatmeal).
- Magnesium-rich foods: May help relax muscles and promote sleep (leafy greens, nuts, seeds).
- Tart cherries or tart cherry juice: Naturally contain melatonin.
- Warm milk: Contains tryptophan and calcium, which can aid relaxation.
- Tryptophan-rich foods: This amino acid helps produce serotonin and melatonin, which are involved in sleep regulation (turkey, milk, nuts, seeds).
Foods and Drinks to Limit or Avoid:
- Caffeine: A stimulant that can interfere with sleep (coffee, tea, soda, chocolate).
- Alcohol: While it may initially make you feel sleepy, it can disrupt sleep later in the night.
- Large meals or sugary snacks before bed: Can interfere with digestion and sleep.
- Spicy foods: May cause heartburn or indigestion that disrupts sleep.
- Caffeine: A stimulant that can interfere with sleep (coffee, tea, soda, chocolate).
Regimen
- Establish a regular sleep schedule: Go to bed and wake up around the same time each day, even on weekends.
- Create a relaxing bedtime routine: A warm bath, reading, or listening to calming music can signal to your body that it’s time to sleep.
- Optimize your sleep environment: Make sure your bedroom is dark, quiet, and cool.
- Get regular exercise: Physical activity can improve sleep quality, but avoid exercising too close to bedtime.
- Manage stress: Engage in relaxation techniques like meditation, deep breathing, or yoga.
- Limit screen time before bed: The blue light emitted from electronic devices can interfere with melatonin production.
- Avoid napping during the day: Naps can disrupt your sleep-wake cycle.
Do’s and Don'ts
Do’s & Dont’s
Insomnia do’s & don’ts
Do’s of Insomnia Management:
Maintain a regular sleep schedule: Go to bed and wake up at the same time every day, even on weekends.
Create a relaxing bedtime routine: Engage in calming activities like reading, taking a warm bath, or listening to soothing music before bed.
Optimize your sleep environment: Make sure your bedroom is dark, quiet, cool, and comfortable.
Limit exposure to light at night: Avoid bright lights and electronic devices in the hours leading up to bedtime.
Avoid stimulants and alcohol before bed: Caffeine, nicotine, and alcohol can disrupt sleep.
Get regular exercise: Regular physical activity can improve sleep quality, but avoid exercising too close to bedtime.
Manage stress: Practice relaxation techniques like deep breathing or meditation to reduce stress and promote relaxation.
See a doctor if insomnia persists: If self-help measures don’t work, consult a healthcare professional for diagnosis and treatment.
Don’ts of Insomnia Management:
- Don’t stay in bed if you can’t sleep: If you’re struggling to fall asleep after 20 minutes, get out of bed and do something relaxing until you feel tired.
- Don’t nap during the day: Napping can disrupt your nighttime sleep.
- Don’t consume caffeine or alcohol before bed: These substances can interfere with sleep.
- Don’t eat heavy meals or sugary snacks close to bedtime: These can cause indigestion and disrupt sleep.
- Don’t watch TV or use electronic devices in bed: The blue light emitted from screens can suppress melatonin production and make it harder to fall asleep.
- Don’t worry about not sleeping: Anxiety about sleep can make insomnia worse. Instead, focus on relaxation techniques.
- Don’t self-medicate with sleep aids: Over-the-counter or prescription sleep aids should only be used under the guidance of a healthcare professional.
Terminology
Terminology
General Terms:
Insomnia: A sleep disorder characterized by difficulty falling asleep, staying asleep, or experiencing non-restorative sleep despite adequate opportunity for sleep.
Sleep Latency: The time it takes to fall asleep from the moment you lie down to try to sleep.
Sleep Efficiency: The percentage of time spent asleep while in bed.
Wake After Sleep Onset (WASO): The total time spent awake after initially falling asleep.
Sleep Architecture: The pattern of sleep stages (light sleep, deep sleep, REM sleep) throughout the night.
Related Conditions:
Comorbid: Co-occurring with another condition, such as depression or anxiety.
Hypersomnolence: Excessive daytime sleepiness.
Parasomnia: Abnormal behaviors or experiences during sleep, like sleepwalking or sleep terrors.
Treatment Terms:
Cognitive Behavioral Therapy for Insomnia (CBT-I): A non-pharmacological treatment that focuses on changing thoughts and behaviors related to sleep.
Sleep Hygiene: Practices that promote good sleep, like maintaining a regular sleep schedule, avoiding caffeine before bed, and creating a relaxing sleep environment.
Hypnotics: Medications that induce sleep, such as benzodiazepines or non-benzodiazepine hypnotics.
Melatonin: A hormone that helps regulate the sleep-wake cycle.
Phototherapy: Exposure to bright light, often used to treat circadian rhythm sleep disorders.
Here are some commonly used homeopathic remedies for insomnia, along with their indications:
Coffea cruda: For insomnia caused by overstimulation, racing thoughts, or excitement. The person may feel restless and have difficulty calming down.
Nux vomica: For insomnia due to overwork, stress, or overindulgence in stimulants like coffee or alcohol. The person may experience irritability, digestive complaints, and difficulty falling asleep after midnight.
Ignatia amara: For insomnia caused by grief, loss, emotional upset, or suppressed emotions. The person may have a tendency to sigh or weep, and experience mood swings.
Arsenicum album: For insomnia with anxiety, restlessness, and fear. The person may wake up frequently, feel chilly, and have a desire for warm drinks.
Pulsatilla: For insomnia in people who are gentle, emotional, and crave attention. They may feel warm and stuffy, and prefer open air.
References
- Psychiatry, Fourth Edition- Oxford Medical Publications – SRG- by Geddes, Jonathan Price, Rebecca McKnight / Ch 28.
- A Short Textbook of Psychiatry by Niraj Ahuja / Ch 11.
- Epidemiology of insomnia: A review of the Global and Indian scenario by D Bhattacharya, M K Sen, and J C Suri (2013).
- The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), published by the American Psychiatric Association in 2013
- Why We Sleep: Unlocking the Power of Sleep and Dreams by Matthew Walker, published in 2017 by Scribner
- Principles and Practice of Sleep Medicine by Kryger, Roth, and Dement. 7th edition, published in 2023 by Elsevier
- UpToDate article Insomnia by A team of expert physicians
- Clinical Examination A Practical Guide by Nicholas J Talley and Simon O’Connor (9th edition, Elsevier, 2018)
- Sleep Disorders Medicine: Basic Science, Technical Considerations, and Clinical Aspects (4th edition, Elsevier, 2017) by Sudhansu Chokroverty
- Say Good Night to Insomnia by Gregg D. Jacobs, Ph.D. (Revised edition, Owl books,2008)
- The Sleep Diet: A Novel Approach to Insomnia by Shawn Stevenson, published in 2017 by Rodale Books
Also Search As
Also search as
There are several ways people can search for homeopathic articles on insomnia:
Online Databases:
Homeopathic Educational Services (HES): This database offers a wide range of homeopathic articles, including clinical cases, research studies, and provings. You can search for "insomnia" within the database to find relevant articles.
The National Center for Homeopathy (NCH): This organization provides resources and information on homeopathy, including articles and publications. Their website might have a search function or a dedicated section on insomnia.
Homeopathic Journals and Publications:
The American Journal of Homeopathic Medicine: This peer-reviewed journal features research articles, case reports, and reviews on various homeopathic topics, including insomnia.
Homeopathy: This journal published by Thieme Medical Publishers covers a broad spectrum of homeopathic research and clinical practice.
Homeopathy Links: This online magazine offers articles, interviews, and news related to homeopathy. They may have a section dedicated to sleep disorders or insomnia.
Homeopathic Libraries:
The British Homeopathic Library: This library houses a vast collection of homeopathic books, journals, and historical documents. They may have a catalog or search function to help you find relevant articles on insomnia.
The National Library of Medicine (NLM): The NLM’s PubMed database includes some homeopathic journals and articles, although the coverage is not as extensive as other databases.
Websites of Homeopathic Organizations:
The Council for Homeopathic Certification (CHC): This organization certifies homeopathic practitioners in the United States. Their website may have educational resources or articles on insomnia.
The North American Society of Homeopaths (NASH): This professional organization for homeopaths might have a member-only section with articles and resources, including those on insomnia.
General Search Engines:
Google Scholar: You can search for "homeopathy insomnia" or "homeopathic treatment for insomnia" to find research articles and scholarly publications.
Google: A general search using keywords like "homeopathic remedies for insomnia" or "homeopathic articles on insomnia" can yield a variety of results, including blog posts, articles, and websites dedicated to homeopathy.
There are several ways to search for information on insomnia, depending on your needs and preferences:
Online Search Engines:
Use search terms like "insomnia," "sleeplessness," "trouble sleeping," or "sleep problems."
Include specific terms to narrow down your search, such as "causes of insomnia," "insomnia treatment," or "insomnia in elders."
Utilize search operators like "AND," "OR," and "NOT" to refine your search. For example, "insomnia AND natural remedies."
Reputable Health Websites:
Mayo Clinic: Provides comprehensive information on insomnia causes, symptoms, diagnosis, and treatment options.
Sleep Foundation: Offers expert-backed information on sleep health, including insomnia, with articles, quizzes, and tools.
National Sleep Foundation: Features resources on sleep disorders and treatment, including a searchable database of sleep centers.
WebMD: Provides information on insomnia, including risk factors, symptoms, diagnosis, treatment, and lifestyle changes.
Cleveland Clinic: Offers detailed information on insomnia, including causes, types, symptoms, diagnosis, and treatment.
Scientific Databases:
PubMed: A free resource developed by the National Center for Biotechnology Information (NCBI) that provides access to medical literature, including research articles on insomnia.
Google Scholar: A search engine that indexes scholarly literature across various disciplines, including medicine. You can find research articles on insomnia here.
Books and Publications:
"Why We Sleep" by Matthew Walker: A comprehensive book on the science of sleep and its importance, including discussions on insomnia and its consequences.
"Say Good Night to Insomnia" by Gregg D. Jacobs: A practical guide to understanding and overcoming insomnia using cognitive behavioral therapy (CBT-I) techniques.
"The Promise of Sleep" by William C. Dement: A classic book on sleep and its disorders, including insomnia, with information on diagnosis and treatment options.
Medical Professionals:
Consult your doctor or a sleep specialist for personalized advice and treatment recommendations. They can assess your specific situation and help you develop a plan to manage insomnia.
Frequently Asked Questions (FAQ)
What is Insomnia?
Insomnia is usually a symptom rather than a disorder, and refers to persistent problems falling asleep, maintaining sleep, or having a good quality of sleep.
Give the types of Insomnia?
How is insomnia diagnosed?
Doctors typically diagnose insomnia based on a person’s sleep history, medical history, and a physical exam.
A sleep diary and sleep studies may also be recommended to rule out other sleep disorders.
What is the main cause of Insomnia?
- Heart diseases
- Respiratory diseases
- Rheumatic and musculoskeletal disease
- Old age
- Alcohol and drug use
- Current medication
- Mania
- Dysthymia
- Anxiety disorder
What are the symptoms of Insomnia?
- Not being able to get to sleep
- Repeated awakenings throughout the night
- Early morning awakening
- Inadequate total quantity of sleep
- Daytime sleepiness
- Irritability
- Fatigue
- Poor attention and concentration
- Substandard performance at daily activities
Can homeopathy help with insomnia?
Yes, homeopathy can be a helpful approach for managing insomnia by addressing the underlying causes of sleep disturbances and promoting natural sleep regulation.
How does homeopathy work for insomnia?
Homeopathic remedies are chosen based on the individual’s unique symptom pattern and constitutional type. The aim is to stimulate the body’s natural healing abilities and restore balance to promote restful sleep.
What are some tips for improving sleep and preventing insomnia?
Maintain a regular sleep schedule, create a relaxing bedtime routine, avoid caffeine and alcohol before bed, create a sleep-conducive environment, and manage stress through relaxation techniques or exercise.
How long does it take to see results with homeopathic treatment for insomnia?
The response to homeopathic treatment varies for each individual. Some people may experience improvement within a few days, while others may take weeks or months to see significant changes in their sleep patterns.
Is it safe to use homeopathic remedies alongside conventional medications for insomnia?
It’s important to consult with both your homeopathic practitioner and your regular doctor to ensure the safe and effective use of homeopathic remedies alongside any other medications you may be taking.
