Addison’s Disease
Definition
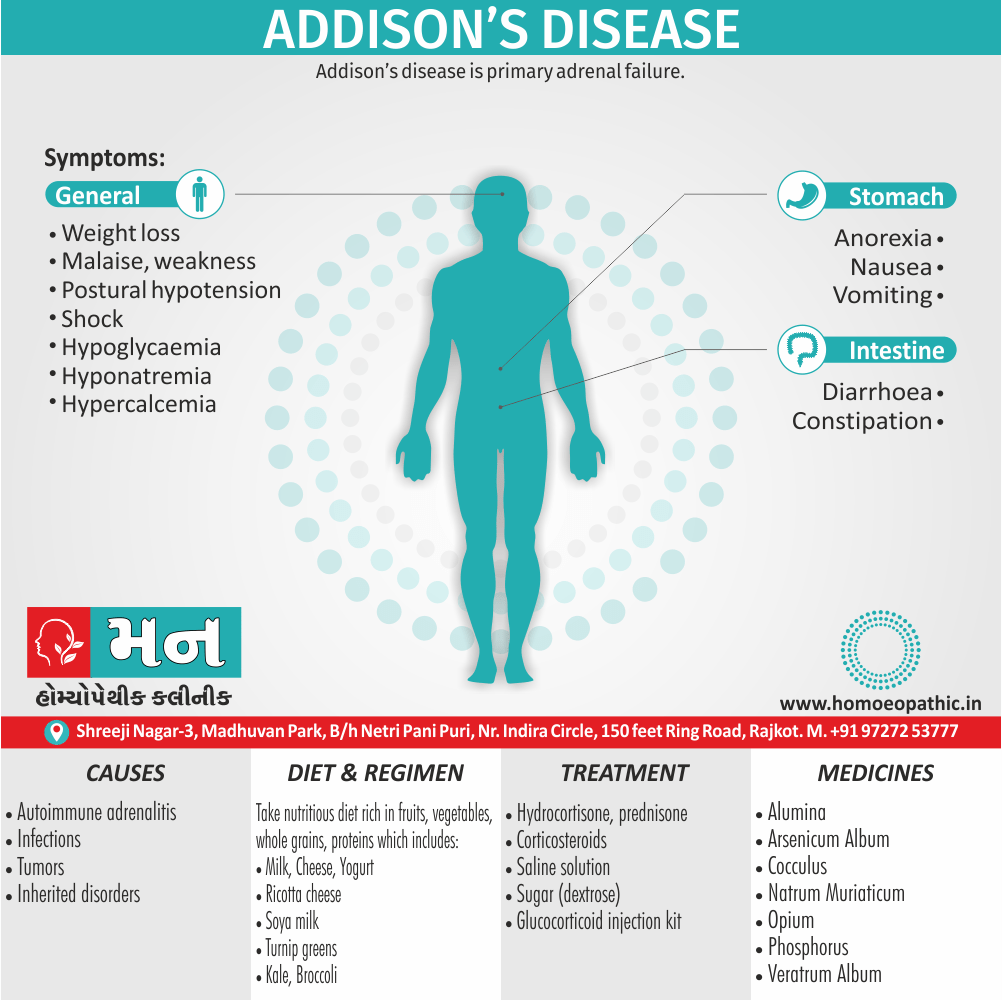
Addison’s disease is primary adrenal failure.[1]
Addison’s Disease does have a few synonyms, depending on the emphasis you want to convey:
- Primary adrenal insufficiency: This term focuses on the insufficient hormone production by the adrenal glands.
- Chronic adrenocortical insufficiency: This emphasizes the long-term nature of the condition and the affected part of the adrenal gland (adrenal cortex).
- Primary failure adrenocortical insufficiency: This is a more specific term highlighting both the primary cause (adrenal gland) and the insufficiency.
These synonyms are mainly used in medical contexts. For informal situations, you might simply say "adrenal gland failure".
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do's & Don'ts
Terminology
References
Also Search As
Overview
Overview:
- Adrenal insufficiency results from inadequate secretion of cortisol and/or aldosterone.
- It is potentially fatal and notoriously variable in its presentation. A high index of suspicion is therefore required in patients with unexplained fatigue, hyponatraemia or hypotension.
- Congenital adrenal hyperplasias and Addison’s disease (primary adrenocortical failure) are rare causes. [2]
Epidemiology
Epidemiology
The epidemiology of Addison’s disease in India differs from that in developed countries, with tuberculosis remaining a significant cause. A study published in the Journal of the Association of Physicians of India in 2001 ("Clinical profile and prognosis of Addison’s disease in India") found that 47% of Addison’s disease cases in their study cohort were attributed to tuberculosis.
Another source, ORD India, states that Addison’s disease affects approximately 1 in 100,000 people in India ("Addison’s Disease – ORD India"). This is slightly lower than the global prevalence, which is estimated to be around 40-60 people per million.
It’s important to note that these are older references, and more recent epidemiological data on Addison’s disease in India may be available. However, they provide a valuable starting point for understanding the unique characteristics of this condition in the Indian population.[13][14]
Causes
Causes of Addison’s Disease:
- Autoimmune adrenalitis
- Infections – Tuberculosis. Cytomegalovirus also fungal infections associated with AIDS.
- Tumours – Metastatic disease (notably from breast)
- Inherited disorders – e.g. adreno leukodystrophies and familial isolated glucocorticoid deficiency.
- Secondary deposits,
- Granulomatous disease, amyloidosis
- Haemochromatosis, fungal disease (e.g. histoplasmosis)
- Congenital adrenal hyperplasia,
- Meningococcal septicaemia, haemorrhage into adrenals, e.g. in new born or as complication of anticoagulant therapy, adrenal vein thrombosis after trauma or adrenal venography.
- Drugs, e.g. rifampicin, ethionamide, ketoconazole.[1]
Types
Types
Primary Adrenal Insufficiency
Secondary Adrenal Insufficiency
Tertiary Adrenal Insufficiency
Risk Factors
Risk Factor
You may be at a higher risk for Addison’s disease if you I.E.:
- have cancer
- take anticoagulants (blood thinners)
- have chronic infections like tuberculosis
- had surgery to remove any part of your adrenal gland
- have an autoimmune disease, like type 1 diabetes or Graves’ disease[6]
Pathogenesis
Pathogenesis
The pathogenesis of Addison’s disease involves the destruction or dysfunction of the adrenal cortex, leading to a deficiency of cortisol and aldosterone. Several factors can contribute to this:
Autoimmune Adrenalitis:
- The most common cause worldwide (approximately 70-90% of cases).
- The immune system mistakenly attacks the adrenal cortex, leading to gradual destruction.
- Associated with other autoimmune diseases and certain genetic predispositions (HLA-DR3 and HLA-DR4).[15]
Infections:
- Tuberculosis (TB) is a major cause in developing countries like India.
- Other infections like fungal infections (histoplasmosis, coccidioidomycosis) and HIV can also damage the adrenal glands.[16}
Other Causes:
- Adrenal hemorrhage (due to anticoagulant therapy, trauma, or sepsis)
- Infiltrative diseases (amyloidosis, sarcoidosis)
- Metastatic cancer
- Genetic disorders (congenital adrenal hyperplasia)
- Drug-induced adrenal insufficiency (e.g., ketoconazole)[17]
Key Pathophysiological Consequences:
- Cortisol Deficiency: Leads to fatigue, weakness, weight loss, hypotension, hypoglycemia, and impaired stress response.
- Aldosterone Deficiency: Causes salt wasting, dehydration, hyperkalemia, hyponatremia, and metabolic acidosis.
I hope this comprehensive explanation with book references is helpful. Please let me know if you have any further questions.
Pathophysiology
Pathophysiology
Primary Adrenal Insufficiency
In primary adrenal insufficiency, although the above mentioned causes lead to gradual destruction of the adrenal cortex, the symptoms and signs of the disease appear when the loss of adrenocortical tissue is higher than 90%.
At the molecular and cellular level, a viral infection, even subclinical, or an excessive tissue response to inflammatory signals may potentially lead to apoptosis or necrosis of adrenocortical cells. Cellular components, such as 21OH-derived peptides, trigger the activation of local dendritic cells, which then transport and present these antigens to CD4+ Th1 cells.
Upon activation, CD4+ Th1 cells help the committed clonal expansion of cytotoxic lymphocytes and autoreactive B cells releasing antibodies against 21-hydroxylase and possibly other antibodies.
The gradual destruction of adrenocortical tissue seems to be mediated by four distinct and complementary molecular mechanisms:
(a) direct cytotoxicity by lymphocytes that induce apoptosis; (b) direct cytotoxic actions by IFN-γ and lymphotoxin-α released by activated CD4+ Th1 cells; (c) cellular cytotoxicity by autoantibodies or by autoantibody-mediated activation of the complement system; and (d) cytotoxic effects of inflammatory cytokines (IL-1β, TNF-α) and free radicals (superoxide, NO) secreted by monocytes/macrophages or by the adrenal cells (51).
In the initial phase of chronic gradual destruction, the adrenal reserve is decreased and although the basal steroid secretion is normal, the secretion in response to stress is suboptimal. Consequently, any major or even minor stressor can precipitate an acute adrenal crisis. With further loss of adrenocortical tissue, even basal steroid secretion is decreased, leading to the clinical manifestations of the disease. Low plasma cortisol concentrations result in the increase of production and secretion of ACTH due to decreased negative feedback inhibition (37). The elevated plasma ACTH concentrations are responsible for the well-recognized hyperpigmentation observed in these patients.
Secondary and Tertiary Adrenal Insufficiency
In secondary or tertiary adrenal insufficiency, the resultant ACTH deficiency leads to decreased secretion of cortisol and adrenal androgens, while mineralocorticoid production remains normal. In the early stages, basal ACTH secretion is normal, while stress-induced ACTH secretion is impaired. With further loss of basal ACTH secretion, there is atrophy of zonae fasciculata and reticularis of the adrenal cortex. Therefore, basal cortisol secretion is decreased, but aldosterone secretion by the zona glomerulosa is preserved.[7]
Clinical Features
Clinical Features
The clinical features of Addison’s disease can be subtle and nonspecific, often developing insidiously over months or years. However, some classic manifestations may raise suspicion of this condition:
1. Hyperpigmentation:
- Increased pigmentation of the skin and mucous membranes, especially in sun-exposed areas, palmar creases, knuckles, elbows, knees, and sites of friction.
- This is due to increased adrenocorticotropic hormone (ACTH) secretion, which also stimulates melanocyte activity.[15]
2. Fatigue and Weakness:
- Generalized weakness and fatigue are almost universal complaints.
- The fatigue is often profound and out of proportion to the patient’s activity level.[17]
3. Gastrointestinal Symptoms:
- Anorexia, nausea, vomiting, abdominal pain, and weight loss are common.
- Salt craving may be present due to mineralocorticoid deficiency.[16]
4. Hypotension and Orthostasis:
- Low blood pressure, often exacerbated by standing (orthostatic hypotension), can lead to dizziness and syncope.[18]
5. Other Manifestations:
- Hyponatremia, hyperkalemia, hypoglycemia, and metabolic acidosis (due to aldosterone deficiency).
- Muscle and joint pain, depression, irritability, and menstrual irregularities.
- Vitiligo (autoimmune destruction of melanocytes) may coexist.
Important Note:
In addition to these chronic features, acute adrenal insufficiency (Addisonian crisis) can occur, presenting with severe hypotension, shock, abdominal pain, fever, and altered mental status. It is a life-threatening emergency requiring immediate medical attention.
I hope this information is helpful. Please let me know if you have any other questions.
Sign & Symptoms
Sign & Symptoms of Addison’s Disease
- Weight loss also anorexia
- Malaise, weakness
- Nausea, vomiting
- Diarrhoea
- Constipation
- Postural hypotension
- Shock
- Hypoglycaemia
- Hyponatraemia
- Hypercalcaemia
Onset – usually insidious, Rarely first manifestation may be acute crisis.
- Pigmentation of skin and mucous membranes – Varieties –
- Bluish black discoloration, or brownish patches or streaks on lips, gums, inside of cheeks.
- Hyper pigmentation of extensor surfaces such as face, neck, dorsum of hands also of forearms.
- Multiple black freckles especially on the forehead, face, neck, shoulders also arms.
- Gastrointestinal symptoms – for example, Anorexia, often with nausea and vomiting, Constipation with intermittent diarrhoea, Salt craving, Abdominal pain, Irritation of the diaphragm.
- Cardio-vascular system – such as Postural hypotension, Faintness ,Dyspnoea, Heart sounds feeble.
- Muscular system – Muscular weakness, and wasting with Creatinuria, Muscle cramps.
- Mental and nervous – Lassitude and muscle weakness are invariable and the first symptom to appear in majority of cases, additionally, Loss of memory, drowsiness.
- Genital system – Impotence and amenorrhoea, Symptoms may be aggravated at the time of menstruation or menopause.
- Kidneys –Kidney function is severely impaired, the excretion of urine is diminished and it contains granular casts and albumin, also the blood urea and creatinine rise above normal.
- Miscellaneous – Subnormal temperature, anemia,Loss of body hair in females.
- Other autoimmune disease – Such as vitiligo, thyroiditis, hypothyroidism, pernicious anaemia, hyperparathyroidism, insulin-dependent diabetes mellitus, mucocutaneous candidiasis.
- Increased secretion of ACTH- Pigmentation of skin in areas exposed to light, in oral mucosa, gums.
- Deficiency of adrenal cortisol secretion,Cortisol,Aldosterone, Androgens- Asthenia Pigmentation of points of pressure (e.g. elbows and mucus membrane, e.g. genital regions, mouth) Anorexia, nausea Weight loss Decreased tolerance to stressful situation Hypotension, postural syncope, Diminished axillary and pubic hair growth in females.
Clinical Examination
Clinical Examination
Appearance i.e.
The patient may be dehydrated and lethargic.
Vitals i.e.
- Low blood pressure
- Orthostatic hypotension
- Fever
Skin i.e.
- Pigmented skin and mucous membranes – darkening (hyperpigmentation) of the skin, including areas not exposed to the sun; characteristic sites are skin creases (e.g. of the hands), nipples, and the inside of the cheek (buccal mucosa), also old scars may darken.
- Vitiligo may be present.
- Absence of axillary and pubic hair in females as a result of loss of adrenal androgens.
- Pallor may be present.
Neck i.e.
- Goiter may be present.
Extremities i.e.
- Weakness
Neurologic i.e.
- Confusion may be present
- Seizures may be present.[8]
Diagnosis
Diagnosis of Addison’s Disease
First about to take medical history an signs and symptoms. You may undergo some of the following tests:
- Blood test
- ACTH stimulation test
- Insulin-induced hypoglycemia test
- Imaging tests [1]
Differential Diagnosis
Differential Diagnosis
Secondary adrenal insufficiency (pituitary failure) i.e.:
- Long-term steroid use
- Pituitary apoplexy
- Pituitary infiltrative disorders
Tertiary adrenal insufficiency (hypothalamic failure) i.e.:
- Pituitary stalk transection
- Hypothalamic stroke
- Central nervous system radiation
Diseases that manifest with hyperpigmentation must be differentiated from Addison disease i.e.
- Scleroderma
- Hemochromatosis
- POEMS syndrome
- Primary biliary cirrhosis
- Drug-induced pigmentation
- Erythema dyschromicum perstans
- Metastatic melanoma [11]
Complications
Complications
Addison’s disease, if left untreated or inadequately managed, can lead to several complications:
- Addisonian Crisis (Acute Adrenal Insufficiency):
- A life-threatening emergency characterized by severe hypotension, shock, abdominal pain, vomiting, fever, and altered mental status.
- Precipitated by stress (infection, surgery, trauma), abrupt discontinuation of glucocorticoid therapy, or untreated Addison’s disease.
- Requires immediate intravenous administration of hydrocortisone, fluids, and electrolytes.[15]
Infections:
- Patients with Addison’s disease are more susceptible to infections due to impaired immune function caused by cortisol deficiency.[17]
- Metabolic Disturbances:
- Hyponatremia (low sodium), hyperkalemia (high potassium), hypoglycemia (low blood sugar), and metabolic acidosis can occur due to aldosterone deficiency.
- These imbalances can lead to cardiac arrhythmias, muscle weakness, and neurological symptoms.[16]
Psychiatric and Neurological Complications:
- Depression, anxiety, irritability, and cognitive impairment may occur due to hormonal imbalances and the stress of chronic illness.[19]
Other Complications:
- Osteoporosis due to long-term glucocorticoid deficiency.
- Anemia and other hematologic abnormalities.
- Increased risk of autoimmune diseases (e.g., Hashimoto’s thyroiditis, type 1 diabetes).
It’s important to note that with proper diagnosis and treatment, many of these complications can be prevented or effectively managed, allowing individuals with Addison’s disease to lead fulfilling lives.
Investigations
Investigations
If Addison’s disease is suspected, blood tests will be carried out to measure the levels of sodium, potassium and cortisol in your body. A low sodium, high potassium or low cortisol level may indicate Addison’s disease.
You may need to see a hospital hormone specialist (endocrinologist) for your blood to be tested for the following:
- a low level of the hormone aldosterone
- a high level of adrenocorticotrophic hormone (in other words, ACTH)
- a low level of glucose (sugar used for energy)
- positive adrenal antibodies (antibodies designed to attack the adrenal gland)
Any of the above could be a sign of Addison’s disease.[9]
Treatment
Treatment
All treatment for Addison’s disease involves medication. You will be given hormone replacement therapy to correct the levels of steroid hormones your body isn’t producing.
Some options for treatment include oral corticosteroids such as i.e.:
- Hydrocortisone, prednisone or methylprednisolone to replace cortisol.
- Fludrocortisone acetate to replace aldosterone.
Treatment for an Addisonian crisis, which is a medical emergency, typically includes intravenous injections of i.e.:
- Corticosteroids
- Saline solution
- Sugar (dextrose)[1]
Prevention
Prevention
1. Do not stop taking steroids suddenly.
2. Do not miss daily steroid doses for more than 24 hours (accidentally missing a dose, vomiting more than 24 hours, hospitalization without continuation of medication, etc.).
3. Know when stress doses should be given (severe illness, surgery, or trauma).[12]
Homeopathic Treatment
Homeopathic Treatment of Addison’s Disease
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic medicines for Addison’s Disease:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Alumina:
- Dryness of mucous membranes.
- Eructation in spare, dry, but thin.
- Old people or prematurely aged. No desire to eat. Can swallow but small morsels at a time.
- Especially, indicated when confused as to personal identity. Low-spirited. Constipation. Menses scanty, pale.
- Worse – cold air, after eating, standing. On the other hand, Better – warmth, fasting, resting in bed.
Arsenic album:
- Gradual loss of weight from impaired nutrition.
- Great anguish also restlessness.
- General sensibility increased.
- Cannot bear either the sight or smell of food.
- Nausea, retching, vomiting after eating or drinking. Particularly, in anxiety in pit of stomach.
Cocculus:
- For travel nausea and sickness.
- Fever is gone but the patient does not rally, there is much nervous trembling, numbness, twitching of muscles and great weakness.
- Violent attacks of gastralgia, due to violent cramp of the stomach. Griping, pinching, constrictive pain.
- From grief ,anxiety, and from prolonged loss of sleep. Also in Headache, vertigo, nausea.
- The woman is emaciated, and grows more and more sickly and chlorotic. [5]
Natrum Muriaticum:
- Great weakness and weariness.
- Especially indicated when oversensitive to all sorts of influences.
- Depressed particularly in chronic diseases. Hungry, yet loose flesh.
- Unquenchable thirst.
- Sweats while eating. Wants to be alone to cry.
- Tears with laughter.
- Menses either irregular or suppressed. Additionally, heart fluttering or palpitation
Opium:
- With either coma or complete inactivity.
- Extremities and face are either bluish or a livid colour.
- Loud breathing, convulsions also trembling.
Phosphorus:
- Firstly, A picture of phosphorus for Addison’s Disease is, destructive metabolism.
- Secondly, thin, transparent skin weakened by loss of animal-fluids, with great nervous debility and emaciation.
- Then, Great lowness of spirits. Easily vexed. Fearful.
- Throws up ingest by mouthfuls.
- The food scarcely swallowed, comes up again. Additionally, pain in stomach relieved by cold food.
- Long, narrow, hard stools difficult to expel. Also, Amenorrhoea.
- At last, heart violent palpitations with anxiety.[4]
Veratrum album:
- Cold sweat on forehead also body.
- Marked by violence and destructiveness; wants to destroy, to tear something; tears the clothes from the body. In Addition, always wants to be busy, to carry on his daily work.
- Vomiting forcible and excessive.
- After that, nausea with weakness; is obliged to lie down
- intense cramps in the stomach; similarly, cramps in the muscles of the abdomen like colic. [5]
Diet & Regimen
Diet & Regimen of Addison’s Disease
Regimen for Addison’s Disease:
In addition to diet, a proper regimen is crucial for managing Addison’s disease effectively:
- Medication Adherence: The cornerstone of Addison’s management is hormone replacement therapy. Take medications as prescribed by your doctor and never skip doses.
- Stress Management: Stress can trigger adrenal crises in people with Addison’s. Practice stress-reducing techniques like yoga, meditation, or deep breathing exercises.
- Regular Monitoring: Regular checkups with your doctor are essential to monitor hormone levels, adjust medication dosages, and address any concerns.
- Emergency Preparedness: Carry an emergency kit containing hydrocortisone injections and a medical alert card with information about your condition.
- Lifestyle Adjustments: Get adequate sleep, engage in regular physical activity, and avoid extreme temperatures to maintain overall well-being.
- Education and Support: Learn as much as you can about Addison’s disease and connect with support groups or online communities to share experiences and gain valuable insights.
Diet for Addison’s Disease
A balanced diet is essential for individuals with Addison’s to ensure adequate nutrient intake and maintain overall health. Here are some key dietary recommendations:
- Increased Sodium Intake: Due to aldosterone deficiency, people with Addison’s may lose excessive sodium through urine. It’s crucial to consume enough sodium to maintain electrolyte balance and prevent low blood pressure. This can be achieved by adding salt to meals, consuming salty snacks, and choosing foods naturally high in sodium.
- Adequate Carbohydrate Intake: Cortisol plays a role in regulating blood sugar levels. Individuals with Addison’s may experience hypoglycemia (low blood sugar), so consuming sufficient carbohydrates throughout the day is crucial. Focus on complex carbohydrates like whole grains, fruits, and vegetables.
- Sufficient Protein Intake: Protein is essential for cell growth and repair. Include lean protein sources like poultry, fish, beans, and lentils in your diet.
- Increased Fluid Intake: Dehydration is a common concern in Addison’s disease. Drink plenty of water and electrolyte-rich fluids throughout the day, especially during hot weather or exercise.
- Frequent Meals: Consuming smaller, more frequent meals can help maintain stable blood sugar levels and prevent fatigue.
- Limit Alcohol and Caffeine: These substances can worsen dehydration and interfere with medication absorption
Do's & Don'ts
Do’s and Don’ts
Do’s:
Take Medications as Prescribed:
- Adhere strictly to the prescribed dosage and schedule of glucocorticoid (hydrocortisone or prednisone) and mineralocorticoid (fludrocortisone) replacement therapy.[16]
Wear a Medical Alert Bracelet or Necklace:
- This can inform healthcare professionals about your condition in case of emergencies.[17]
Carry an Emergency Kit:
- Include an injectable form of hydrocortisone and instructions for its use in case of an Addisonian crisis.[15]
Adjust Medication During Stressful Events:
- Increase glucocorticoid dosage temporarily during illness, surgery, or other stressors.
- Consult your doctor for specific instructions.[18]
Maintain a Healthy Lifestyle:
- Eat a balanced diet, exercise regularly, and manage stress to optimize your overall health and well-being.[20]
Don’ts:
Don’t Skip or Discontinue Medications Abruptly:
- This can precipitate an Addisonian crisis.
- Always consult your doctor before making any changes to your medication regimen.
Don’t Ignore Signs of Adrenal Insufficiency:
- Seek medical attention promptly if you experience symptoms like severe fatigue, weakness, nausea, vomiting, abdominal pain, or dizziness.
Don’t Neglect Regular Follow-up Visits with Your Doctor:
- Regular monitoring of hormone levels and overall health is essential to ensure optimal management of Addison’s disease.
Don’t Overexert Yourself Physically:
- Listen to your body’s signals and avoid pushing yourself beyond your limits.
Don’t Self-medicate:
- Consult your doctor before taking any over-the-counter medications or supplements, as some may interact with your prescribed medications or worsen your condition.
Terminology
Terminology
- Adrenal Insufficiency: The inability of the adrenal glands to produce adequate amounts of hormones, primarily cortisol and aldosterone.
- Primary Adrenal Insufficiency: Adrenal insufficiency caused by damage or dysfunction of the adrenal glands themselves.
- Secondary Adrenal Insufficiency: Adrenal insufficiency caused by a problem with the pituitary gland, which controls the adrenal glands.
- Tertiary Adrenal Insufficiency: Adrenal insufficiency caused by a problem with the hypothalamus, which controls the pituitary gland.
- Autoimmune Adrenalitis: An autoimmune condition where the body’s immune system attacks and destroys the adrenal glands.
- Hyperpigmentation: Increased pigmentation or darkening of the skin and mucous membranes, often a sign of Addison’s disease.
- Hypotension: Low blood pressure.
- Hyponatremia: Low levels of sodium in the blood.
- Hyperkalemia: High levels of potassium in the blood.
- ACTH (Adrenocorticotropic Hormone): A hormone produced by the pituitary gland that stimulates the adrenal glands to produce cortisol.
Specific Terms from the Homeopathic Context:
- Miasmatic Tendency: A predisposition or susceptibility to certain types of diseases, according to homeopathic theory.
- Therapeutic Affinity: The tendency of a homeopathic remedy to act on specific organs or systems of the body.
- Materia Medica: A reference book containing information about homeopathic remedies, their properties, and their uses.
Additional Notes:
- The section on "Pathophysiology" goes into detail about the cellular and molecular mechanisms involved in Addison’s disease, which may be more technical than necessary for a general audience.
- The homeopathic treatment section could benefit from clearer explanations of how homeopathic remedies are chosen and used for this condition. It might also be helpful to include information about the limitations of homeopathic treatment and the importance of working with a qualified practitioner.
References
References use for Article Addison’s disease
- Davidson’s principles and practice of medicine-Churchill Livingstone Elsevier (2014)
- Medicine Golwala
- The Bhanja Homoeopathic Prescriber By K. C.
- https://www.mayoclinic.org/diseasesconditions/addisons-disease/diagnosis-treatment/drc-20350296
- Australian Homoeopathic Home Prescriber Part 1
- Kent’s_Homeopathy_Materia_Medica
- https://www.healthline.com/health/addisons-disease#risk-factors
- https://www.ncbi.nlm.nih.gov/books/NBK279083/
- https://www.wikidoc.org/index.php/Addison%27s_disease_physical_examination
- https://www.nhs.uk/conditions/addisons-disease/diagnosis/#:~:text=If%20Addison’s%20disease%20is%20suspected,level%20may%20indicate%20Addison’s%20disease.
- https://www.visualdx.com/visualdx/diagnosis/addison+disease?diagnosisId=51066&moduleId=101
- https://www.parentprojectmd.org/care/care-guidelines/by-area/steroids/risk-for-adrenal-crisis/
- Bhansali, A., et al. (2001). Clinical profile and prognosis of Addison’s disease in India. Journal of the Association of Physicians of India, 49(2), 165-170.
- Addison’s Disease – ORD India. Retrieved from https://ordindia.in/about-rd/rare-disease-in-india/addisons-disease/addisons-disease-2/
- Harrison’s Principles of Internal Medicine, 20th Edition (2018), Kasper, D.L., Fauci, A.S., Hauser, S.L., Longo, D.L., Jameson, J.L., & Loscalzo, J. (Eds.). McGraw Hill Education.
- Williams Textbook of Endocrinology, 14th Edition (2020), Melmed, S., Polonsky, K.S., Larsen, P.R., & Kronenberg, H.M. (Eds.). Elsevier.
- Endocrinology: Adult and Pediatric, 7th Edition (2016), Jameson, J.L., De Groot, L.J., de Kretser, D.M., Giudice, L.C., Grossman, A.B., Melmed, S., … & Wierman, M.E. (Eds.). Elsevier Saunders.
- Katzung & Trevor’s Pharmacology Examination & Board Review, 12th Edition (2020), Trevor, A.J., Katzung, B.G., & Kruidering-Hall, M. (Eds.). McGraw Hill Education.
- Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry, 12th Edition (2021), Sadock, B.J., Sadock, V.A., & Ruiz, P. (Eds.). Wolters Kluwer.
- The Merck Manual Professional Version, Merck & Co., Inc. (Continuously updated online resource).
Also Search As
Also Search As
Primary Keywords:
- Addison’s Disease
- Homeopathy for Addison’s Disease
- Adrenal Insufficiency
- Homeopathic Remedies for Addison’s
- Natural Treatment for Addison’s
Secondary Keywords:
- Addison’s Symptoms
- Addison’s Causes
- Adrenal Fatigue
- Homeopathic Medicine
- Holistic Treatment
Long-Tail Keywords (More Specific Phrases):
- Can homeopathy cure Addison’s Disease?
- Best homeopathic remedies for adrenal insufficiency
- Homeopathic approach to managing Addison’s symptoms
- Safe and natural treatment for Addison’s Disease
- Diet and lifestyle tips for Addison’s patients
Additional Tips for Search Optimization:
- Use keywords naturally throughout the article: Incorporate these keywords into your title, headings, body text, and meta descriptions.
- Create a comprehensive FAQ section: Include common questions people might search for (as you’ve already done).
- Optimize images: Use descriptive file names and alt text for images.
- Internal linking: Link relevant sections within your website or blog to the article.
- Promote the article: Share it on social media, forums, and other relevant online platforms.
Direct Search on Your Website/Blog:
- If the article is hosted on your platform, users can simply use the search bar within your site.
- Ensure the article is properly indexed for internal search.
Search Engines (Google, Bing, etc.):
- Using any of the keywords and phrases mentioned earlier.
- Combining keywords, e.g., "Addison’s Disease homeopathic treatment."
- Searching for specific questions, e.g., "Can homeopathy help with Addison’s?"
Social Media:
- If you’ve shared the article on platforms like Facebook, Twitter, or LinkedIn, people can find it through hashtags or your profile/page.
- Encourage sharing to increase its reach.
Homeopathic Forums and Communities:
- Share your article in relevant online communities and forums focused on homeopathy or adrenal health.
- Participate in discussions and link to your article where appropriate.
Other Websites and Blogs:
- If other websites or blogs link to your article, people can discover it through those backlinks.
- Consider outreach to other sites in the health and wellness niche for potential collaborations.
Direct Links and Referrals:
- Share the direct link to your article with friends, family, colleagues, or anyone who might find it useful.
- Healthcare professionals (including homeopathic practitioners) might refer patients to your article.
Email Newsletters:
- If you have an email list, include a link to the article in your newsletter to reach your subscribers.
Frequently Asked Questions (FAQ)
What is Addison's disease?
Addison’s disease is primary adrenal failure.
How is Addison's disease diagnosed?
Diagnosis
Diagnosis involves a combination of medical history, physical examination, blood tests (to check hormone levels), and sometimes imaging studies of the adrenal glands. The ACTH stimulation test is a key diagnostic tool.
What are the causes of Addison's disease?
- Infections
- Tumours – Metastatic disease
- Inherited disorders
- Granulomatous disease, amyloidosis
- Fungal disease (histoplasmosis)
- Congenital adrenal hyperplasia,
- Drugs (rifampicin)
What are the symptoms of Addison's disease?
- Weight loss, anorexia
- Malaise, weakness
- Nausea, vomiting
- Diarrhoea
- Constipation
- Postural hypotension
- Shock
- Hypoglycaemia
Can homeopathy help with Addison's disease?
Homeopathy offers a supportive approach to Addison’s disease by potentially alleviating symptoms and improving overall well-being alongside conventional hormone replacement therapy.
What should people with Addison's disease do in case of an emergency?
- They should wear a medical alert bracelet or necklace and carry an emergency kit containing injectable hydrocortisone. It’s also crucial to inform family and friends about the condition.
Homeopathic Medicines use by Homeopathic Doctors in treatment of Addison's disease?
Homoeopathic Medicine For Addison’s Disease
- Alumina
- Arsenic album
- Cocculus
- Natrum Muriaticum
- Opium
- Phosphorus
- Veratrum album
