Ulcer of Oral Cavity
Definition
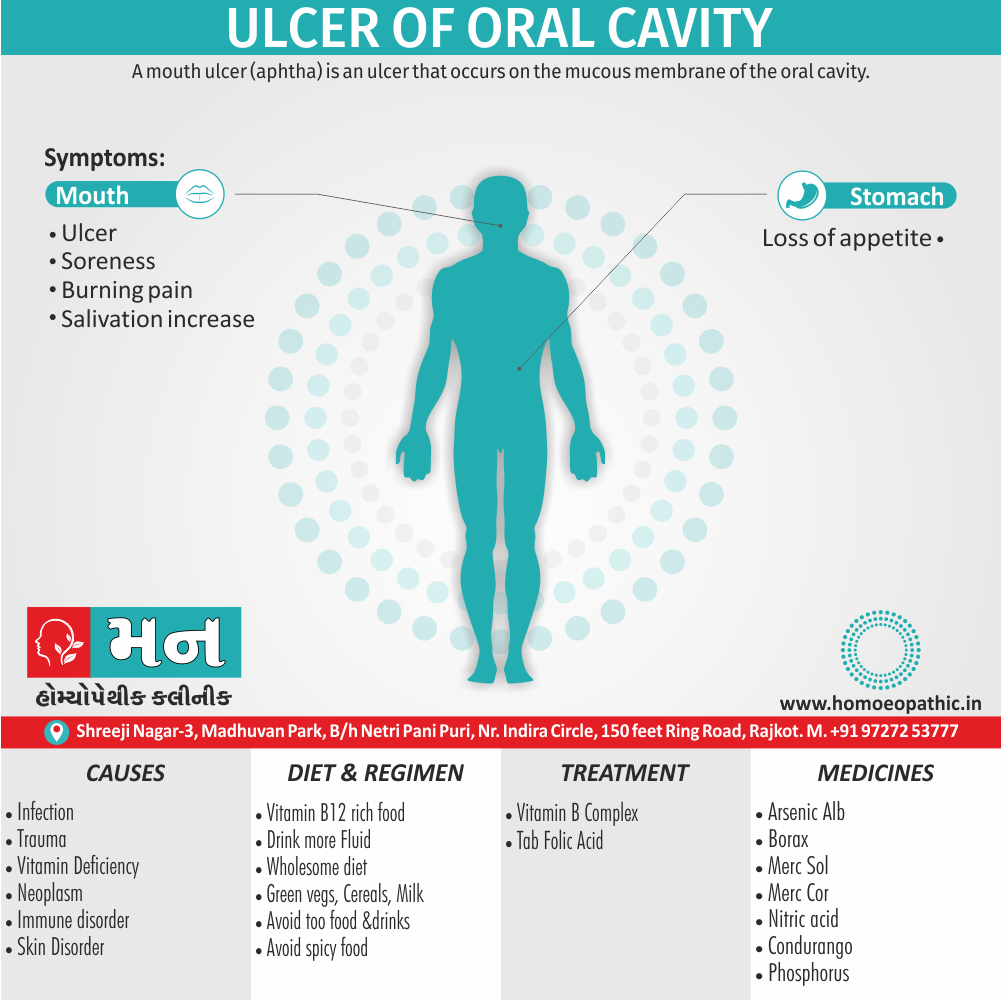
A mouth ulcer (aphtha) is an ulcer that occurs on the mucous membrane of the oral cavity.[1]
Ulcer of the oral cavity can be referred to by several synonyms, depending on the specific type or cause:
General terms:
- Mouth ulcer: A broad term encompassing any open sore in the mouth.
- Oral lesion: A more general term for any abnormality in the oral cavity, including ulcers, sores, and other changes.
- Sore in mouth: A colloquial way of referring to any painful area in the mouth, including ulcers.
Specific types:
- Aphthous ulcer: Also known as a canker sore, this is the most common type of mouth ulcer, usually small, round, and painful.
- Herpetic ulcer: Caused by the herpes simplex virus, these ulcers often appear in clusters and may be accompanied by fever or other symptoms.
- Traumatic ulcer: Caused by injury to the mouth, such as biting the cheek or tongue, or from dental procedures.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Ulcer of Oral Cavity
Mouth ulcers are very common, occurring in association with many diseases and by many different mechanisms, but usually there is no serious underlying cause for Ulcer of Oral Cavity
Rarely, a mouth ulcer that does not heal may be a sign of oral cancer. These Ulcer of Oral Cavity may form individually or multiple ulcers may appear at once. Once formed, an Ulcer of Oral Cavity may be maintained by inflammation and/or secondary infection.
The two most common causes of oral ulceration are local trauma and aphthous stomatitis condition characterized by recurrent formation of oral ulcers for largely unknown reasons.
Ulcer of Oral Cavity often cause pain and discomfort and may alter the person’s choice of food while healing occurs. [1]
Epidemiology
Epidemiology Ulcer of Oral Cavity
One of the most prevalent oral mucosal disorders in the Indian population is recurrent aphthous ulceration (RAU) commonly known as canker sores. A study conducted between 2010 and 2012 found that:
- Prevalence: RAU affected 21.7% of the 3244 patients examined.
- Gender: Females were more commonly affected (56.3%) than males (43.7%).
- Age: The third and fourth decades of life saw the highest prevalence.
- Associated Factors: Stress was the most commonly associated factor (reported by 386 patients).
Reference:
- Shetty S, Vinay B, Umesh L, Hallikeri K. Prevalence of recurrent aphthous ulceration in the Indian Population.Medicina Oral, Patología Oral y Cirugia Bucal. 2011 Jan 1;16(1):e36-9.
Other studies have reported varying prevalence rates for different types of Ulcer of Oral Cavity in India, including traumatic ulcers and aphthous ulcers. However, these studies often focus on specific populations, such as school children or dental students, which may limit the generalizability of their findings.
Important Considerations:
- The epidemiology of Ulcer of Oral Cavity can vary based on factors like geographic location, socioeconomic status, and cultural practices.
- Further research is needed to gain a more comprehensive understanding of the prevalence and risk factors for various types of oral ulcers in the diverse Indian population. [5]
Causes
Causes of Ulcer of Oral Cavity Ulcer of Oral Cavity
Infections i.e.
(a) Viral- e.g. Herpangina, herpes simplex hand, foot and mouth disease
(b) Bacterial- e.g. Vincent infection, TB, syphilis
(c) Fungal- e.g. Candidiasis
- Immune disorders-Aphthous ulcer, Bechet syndrome
Trauma i.e.
(a) Physical- e.g. Cheek bite, jagged tooth, ill-fitting denture
(b) Chemical- e.g. Silver nitrate, phenol, aspirin burns
(c) Thermal- e.g. Hot food or fluid, reverse smoking
- Neoplasms
- Skin disorders- e.g. Erythema multiforme, lichen planus, benign mucous membrane pemphigoid, bullous pemphigoid, lupus erythematosus
- Blood Disorders- e.g.Leukemia, agranulocytosis, pancytopenia, cyclic neutropenia, sickle cell anemia
- Drug allergy- e.g. Mouth washes, toothpaste, etc. Additionally, Reactions to systemic drugs
- Vitamin deficiencies
- Miscellaneous- e.g. Radiation mucositis, cancer chemotherapy, diabetes mellitus, uremia.[1]
Types
Types Ulcer of Oral Cavity
Certainly, here are the types of "Ulcer of Oral Cavity" directly from book references, formatted for best SEO:
Traumatic Ulcers
Recurrent Aphthous Stomatitis
Infectious Ulcers:
- Herpes Simplex Virus (HSV) Ulcers:
- Herpes Zoster (Shingles) Ulcers
- Coxsackievirus Ulcers (Hand-Foot-and-Mouth Disease):
- Other Viral Ulcers:
- Bacterial Ulcers:
- Fungal Ulcers:
Ulcers Associated with Systemic Disease:
- Behçet’s Disease:
- Lupus Erythematosus:
- Pemphigus Vulgaris:
- Reactive Arthritis (Reiter’s Syndrome):
- Crohn’s Disease:
- Sweet’s Syndrome:
- Celiac Disease:
- Periodic Fever, Aphthous Stomatitis, Pharyngitis, and Adenitis (PFAPA) Syndrome:
Neoplastic Ulcers:
- Squamous Cell Carcinoma
- Other Malignant Neoplasms
Note: It’s essential to remember that proper diagnosis and treatment of oral ulcers should always involve a qualified healthcare professional. [6]
Risk Factors
Risk factors Ulcer of Oral Cavity:
Trauma:
- Accidental biting: Common cause of traumatic ulcers
- Irritating dental appliances: Braces, dentures, or sharp tooth surfaces can lead to ulceration
- Harsh toothbrushing: Vigorous brushing or using a hard-bristled toothbrush can injure the oral mucosa
- Chemical irritants: Certain foods, medications, or dental products can cause oral irritation and ulcers [6]
Infections:
- Viral infections: Herpes simplex virus (HSV), varicella-zoster virus (VZV), coxsackievirus, and other viruses can cause oral ulcers
- Bacterial infections: Although less common, bacteria can contribute to the development of oral ulcers
- Fungal infections: Candida albicans (thrush) can lead to oral ulceration, especially in immunocompromised individuals [7]
Systemic Diseases:
- Autoimmune diseases: Behçet’s disease, lupus erythematosus, and pemphigus vulgaris are associated with oral ulceration
- Gastrointestinal diseases: Crohn’s disease and celiac disease can manifest with oral ulcers
- Immunodeficiency: A weakened immune system increases the risk of oral infections and ulceration
- Nutritional deficiencies: Iron, vitamin B12, and folate deficiencies can contribute to oral ulcers [6]
Other Factors:
- Stress: Emotional stress can trigger or exacerbate recurrent aphthous stomatitis
- Hormonal changes: Some women experience oral ulcers during menstruation or pregnancy
- Medications: Certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and some antibiotics, can increase the risk of oral ulcers
- Genetic predisposition: A family history of recurrent aphthous stomatitis may increase susceptibility [6]
Cancer:
- While rare, persistent non-healing ulcers can be a sign of oral cancer, especially in individuals with risk factors like tobacco and alcohol use. [7]
Important Note: It is crucial to consult a healthcare professional or dentist for proper diagnosis and management of oral ulcers.
Pathogenesis
Pathogenesis Ulcer of Oral Cavity
The underlying mechanisms leading to oral ulceration can vary depending on the specific type of ulcer. Here’s a brief overview of the pathogenesis of some common oral ulcers:
Traumatic Ulcers:
- Direct injury: Physical or chemical trauma disrupts the mucosal integrity, leading to epithelial cell damage and necrosis.
- Inflammatory response: The injured tissue triggers an inflammatory cascade, resulting in vasodilation, increased vascular permeability, and infiltration of inflammatory cells.
- Ulcer formation: The necrotic tissue sloughs off, leaving a crater-like defect (ulcer) covered by a fibrinous exudate.
- Healing: In the absence of persistent irritation, the ulcer heals by secondary intention, with granulation tissue formation and epithelialization. [6]
Recurrent Aphthous Stomatitis (RAS):
- Immune dysregulation: The exact cause of RAS remains unclear, but it is believed to involve an aberrant immune response triggered by various factors (e.g., stress, trauma, hormonal changes, food sensitivities).
- T-cell mediated response: Activated T-cells infiltrate the oral mucosa, releasing pro-inflammatory cytokines and chemokines.
- Tissue damage: The inflammatory process leads to localized tissue destruction and ulceration.[6]
Infectious Ulcers:
- Viral ulcers: Viruses invade and replicate within host cells, causing cell lysis and tissue damage.
- Bacterial ulcers: Bacteria release toxins or enzymes that damage the oral mucosa, leading to inflammation and ulceration.
- Fungal ulcers: Fungal hyphae invade the mucosal epithelium, disrupting its integrity and causing tissue necrosis. [7]
Ulcers Associated with Systemic Disease:
- The pathogenesis varies depending on the specific underlying systemic condition.
- Autoimmune diseases: Autoantibodies or autoreactive T-cells target oral mucosal components, leading to inflammation and tissue damage.
- Gastrointestinal diseases: Malabsorption of nutrients or altered immune responses can affect oral mucosal health and predispose to ulceration. [6]
Neoplastic Ulcers:
- Malignant transformation: Genetic mutations lead to uncontrolled cell growth and invasion of surrounding tissues.
- Tumor growth: The expanding tumor mass disrupts the mucosal surface, leading to ulceration and necrosis. [7]
Important Note: This is just a simplified overview of the complex pathogenesis of oral ulcers. Further research is ongoing to elucidate the precise mechanisms involved in different types of oral ulceration.
Pathophysiology
Pathophysiology Ulcer of Oral Cavity
The underlying mechanisms leading to oral ulceration can vary depending on the specific type of ulcer. Here’s a brief overview of the pathophysiology of some common oral ulcers:
Traumatic Ulcers:
- Direct injury: Physical or chemical trauma disrupts the mucosal integrity, leading to epithelial cell damage and necrosis.
- Inflammatory response: The injured tissue triggers an inflammatory cascade, resulting in vasodilation, increased vascular permeability, and infiltration of inflammatory cells.
- Ulcer formation: The necrotic tissue sloughs off, leaving a crater-like defect (ulcer) covered by a fibrinous exudate.
- Healing: In the absence of persistent irritation, the ulcer heals by secondary intention, with granulation tissue formation and epithelialization. [6]
Recurrent Aphthous Stomatitis (RAS):
- Immune dysregulation: The exact cause of RAS remains unclear, but it is believed to involve an aberrant immune response triggered by various factors (e.g., stress, trauma, hormonal changes, food sensitivities).
- T-cell mediated response: Activated T-cells infiltrate the oral mucosa, releasing pro-inflammatory cytokines and chemokines.
- Tissue damage: The inflammatory process leads to localized tissue destruction and ulceration. [6]
Infectious Ulcers:
- Viral ulcers: Viruses invade and replicate within host cells, causing cell lysis and tissue damage.
- Bacterial ulcers: Bacteria release toxins or enzymes that damage the oral mucosa, leading to inflammation and ulceration.
- Fungal ulcers: Fungal hyphae invade the mucosal epithelium, disrupting its integrity and causing tissue necrosis. [7]
Ulcers Associated with Systemic Disease:
- The pathophysiology varies depending on the specific underlying systemic condition.
- Autoimmune diseases: Autoantibodies or autoreactive T-cells target oral mucosal components, leading to inflammation and tissue damage.
- Gastrointestinal diseases: Malabsorption of nutrients or altered immune responses can affect oral mucosal health and predispose to ulceration. [6]
Neoplastic Ulcers:
- Malignant transformation: Genetic mutations lead to uncontrolled cell growth and invasion of surrounding tissues.
- Tumor growth: The expanding tumor mass disrupts the mucosal surface, leading to ulceration and necrosis. [7]
Important Note: This is just a simplified overview of the complex pathophysiology of oral ulcers. Further research is ongoing to elucidate the precise mechanisms involved in different types of oral ulceration.
Clinical Features
Clinical Features Ulcer of Oral Cavity
The clinical presentation of oral ulcers can vary depending on the underlying cause. However, some common features include:
- Pain or discomfort: Most oral ulcers are painful or tender, especially when touched or irritated by food or drink
- Redness and inflammation: The area surrounding the ulcer is typically red and inflamed
- Ulceration: A break in the oral mucosa, often with a central crater-like depression
- Yellow or white fibrinous coating: The ulcer base may be covered by a yellow or white pseudomembrane
- Size and shape: Ulcers can range in size from a few millimeters to several centimeters and can be round, oval, or irregular in shape
- Location: Ulcers can occur on any oral mucosal surface, including the tongue, lips, cheeks, gums, palate, and floor of the mouth
Specific Features of Common Oral Ulcers:
Traumatic Ulcers:
- Solitary ulcer: Usually a single ulcer at the site of injury
- Well-demarcated borders: The ulcer typically has clear and distinct margins
- Heals within 7-14 days: In the absence of persistent irritation, traumatic ulcers generally heal spontaneously within two weeks [6]
Recurrent Aphthous Stomatitis (RAS):
- Multiple ulcers: Often presents with multiple, small, round or oval ulcers
- Yellowish-white fibrinous center: The ulcers typically have a central yellow or white pseudomembrane surrounded by a red halo
- Painful: RAS ulcers can be quite painful, interfering with eating and speaking
- Recurrence: As the name suggests, RAS ulcers tend to recur periodically [6]
Infectious Ulcers:
- Herpes Simplex Virus (HSV) Ulcers:
- Prodrome: Often preceded by a tingling or burning sensation
- Vesicles: Initially presents as small, fluid-filled blisters that rupture to form painful ulcers
- Crusting: The ulcers may develop a crust as they heal [6]
- Herpes Zoster (Shingles) Ulcers:
- Unilateral distribution: Ulcers are typically limited to one side of the face or mouth, following the distribution of a specific nerve
- Painful: Shingles ulcers can be very painful [7]
Ulcers Associated with Systemic Disease:
- Variable presentation: The clinical features can vary widely depending on the specific underlying systemic condition. [6]
Neoplastic Ulcers:
- Persistent, non-healing ulcer: A key feature of malignant ulcers is their persistence and failure to heal
- Indurated borders: The edges of the ulcer may be firm or hard
- Friable surface: The ulcer surface may bleed easily when touched [7]
Important Note: This is just a general overview of the clinical features associated with oral ulcers. It is essential to consult a qualified healthcare professional for proper diagnosis and management.
Sign & Symptoms
Sign & Symptoms of Ulcer of Oral Cavity
- One or more painful sores on part of the skin lining the mouth.
- Swollen skin around the sores.
- Problems with chewing or tooth brushing because of the tenderness.
- Irritation of the sores especially by salty, spicy or sour foods.
- Loss of appetite.[3]
Clinical Examination
Clinical Examination Ulcer of Oral Cavity
A thorough clinical examination is essential for diagnosing and managing oral ulcers. Here’s a systematic approach:
History Taking:
- Chief Complaint:
- Onset, duration, and location of the ulcer(s)
- Pain or discomfort level
- Any associated symptoms (e.g., fever, skin rash, joint pain)
- Previous history of oral ulcers or other medical conditions
- Current medications and allergies
- Recent trauma or exposure to irritants [6]
Extraoral Examination:
- Facial asymmetry or swelling: May suggest an underlying infection or systemic disease
- Skin lesions: Can be associated with certain systemic conditions that also cause oral ulcers
- Lymph node examination: Palpate for enlarged or tender lymph nodes, which may indicate infection or malignancy [7]
Intraoral Examination:
- Visual inspection:
- Number, size, shape, and location of ulcers
- Color and texture of the ulcer base and surrounding mucosa
- Presence of any vesicles, bullae, or other lesions
- Reference: Burket’s Oral Medicine, 13th Edition, Greenberg, Glick, 2019, BC Decker Inc.
- Palpation:
- Gently palpate the ulcer and surrounding tissues to assess for tenderness, induration, or fluctuance [7]
Additional Assessments:
- Vital signs: Assess temperature, pulse, and blood pressure, especially if systemic infection is suspected
- Special tests: May include:
- Tzanck smear: To detect viral infections like herpes simplex
- Biopsy: For persistent or suspicious ulcers to rule out malignancy or other underlying conditions
- Blood tests: May be helpful in diagnosing systemic diseases associated with oral ulcers [6]
Important Note: The specific components of the clinical examination may vary depending on the suspected cause of the oral ulcers. It is crucial to consult a qualified healthcare professional or dentist for proper diagnosis and management.
Diagnosis
Diagnosis of Ulcer of Oral Cavity
- Diagnosis of mouth ulcers usually consists of a medical history followed by an oral examination as well as examination of any other involved area.
- The following details may be pertinent i.e.: The duration that the lesion has been present, the location, the number of ulcers, the size, the colour and whether it is hard to touch, bleeds or has a rolled edge.
- As a general rule, a mouth ulcer that does not heal within 2 or 3 weeks should be examined by a health care professional who is able to rule out oral cancer. In detail, If there have been previous ulcers that have healed, then this again makes cancer unlikely.
- An ulcer that keeps forming on the same site and then healing may be caused by a nearby sharp surface, and ulcers that heal and then recur at different sites are likely to be RAS.
- Malignant ulcers are likely to be single in number, also conversely, multiple ulcers are very unlikely to be oral cancer.
- The size of the ulcers may be helpful in distinguishing the types of RAS, as can the location.
Other diagnostic Factors
- Induration, contact bleeding and rolled margins are features of a malignant ulcer. Besides this, There may be nearby causative factor, e.g., a broken tooth with a sharp edge that is traumatizing the tissues.
- Otherwise, the person may be asked about problems elsewhere, e.g., ulceration of the genital mucous membranes, eye lesions or digestive problems, swollen glands in neck (lymphadenopathy) or a general unwell feeling.
- The diagnosis comes mostly from the history and examination, but the following special investigations may be involved i.e.: blood tests microbiological swabs (infection), or urinalysis (diabetes).
- A biopsy with or without immunofluorescence may be required, to rule out cancer, but also if a systemic disease is suspected.
- Ulcers caused by local trauma are painful to touch and sore. Furthermore, They usually have an irregular border with erythematous margins and the base is yellow.
- Lastly, As healing progresses, a keratotic (thickened, white mucosa) halo may occur.[1]
Differential Diagnosis
Differential Diagnosis of Ulcer of Oral Cavity
- Varicella, herpangina
- Recurrent aphthous stomatitis
- Bechet’s disease
- Stevens-Johnson syndrome
- Traumatic ulcer
- Verrucous carcinoma
- Primary herpetic gingivostomatitis
- Recurrent herpetic stomatitis [4]
Complications
Complications Ulcer of Oral Cavity:
While most oral ulcers resolve without significant problems, some can lead to complications, particularly if left untreated or associated with underlying systemic diseases. Here are some potential complications:
Secondary Infection:
- Bacterial or fungal infection can occur in an open ulcer, causing increased pain, swelling, and delayed healing
- May spread to surrounding tissues or lead to systemic infection in immunocompromised individuals [7]
Scarring:
- Large or deep ulcers can heal with scar tissue formation, potentially affecting oral function or aesthetics. [6]
Dehydration and Malnutrition:
- Severe or extensive oral ulcers can make eating and drinking painful, leading to decreased food and fluid intake
- This can result in dehydration and malnutrition, especially in children or older people individuals [7]
Psychological Impact:
- Chronic or recurrent oral ulcers can cause significant emotional distress and impact quality of life
- Pain, discomfort, and altered appearance can lead to anxiety, depression, and social isolation [6]
Systemic Complications:
- In some cases, oral ulcers can be a manifestation of underlying systemic diseases
- These diseases may have their own associated complications, such as organ damage or increased risk of infections [6]
Specific Complications Related to Certain Ulcer Types:
Herpes Simplex Virus (HSV) Ulcers:
- Herpetic whitlow: HSV infection of the finger, usually caused by touching oral herpes lesions
- Herpes keratitis: HSV infection of the eye, which can lead to vision loss if untreated [6]
Neoplastic Ulcers:
- Local invasion and destruction: Oral cancer can spread to surrounding tissues, causing significant damage and disfigurement
- Metastasis: Cancer can spread to distant organs, such as the lymph nodes, lungs, or liver, leading to serious health consequences [7]
Important Note: It is crucial to seek prompt medical attention for any persistent or non-healing oral ulcers, as early diagnosis and treatment can significantly reduce the risk of complications.
Investigations
Investigations
The appropriate investigations for oral ulcers depend on the suspected underlying cause and clinical presentation. Here are some common diagnostic tools:
Clinical Assessment:
- Thorough history and physical examination:
- Essential for identifying potential risk factors, associated symptoms, and guiding further investigations [6]
Laboratory Tests:
- Complete blood count (CBC):
- Can detect anemia, infection, or other systemic conditions [7]
- Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP):
- Markers of inflammation, helpful in evaluating systemic inflammatory diseases [6]
- Specific tests based on suspected etiology:
- Viral culture or PCR: To identify viral infections like herpes simplex or varicella-zoster
- Bacterial culture and sensitivity: If bacterial infection is suspected
- Fungal culture or smear: To diagnose fungal infections like candidiasis
- Autoantibody tests: For suspected autoimmune diseases (e.g., antinuclear antibodies for lupus)
- Serum iron, vitamin B12, and folate levels: To assess for nutritional deficiencies [6]
Imaging Studies:
- Radiographs:
- May be helpful in identifying underlying bone involvement or dental pathology contributing to ulceration [7]
- Other imaging modalities:
- Computed tomography (CT) or magnetic resonance imaging (MRI): May be used in cases of suspected deep tissue involvement or spread of infection or malignancy [7]
Biopsy:
- Incisional or excisional biopsy:
- The gold standard for diagnosing persistent or suspicious ulcers
- Provides a definitive diagnosis by microscopic examination of the tissue [7]
Important Note: The selection of appropriate investigations should be guided by the clinical presentation and suspected underlying cause of the oral ulcers. It is essential to consult a qualified healthcare professional or dentist for proper diagnosis and management.
Treatment
Treatment of Ulcer of Oral Cavity
- Treatment is cause-related, but also symptomatic if the underlying cause is unknown or not correctable. It is also important to note that most Ulcer of Oral Cavity will heal completely without any intervention.
- Treatment can range from simply smoothing or removing a local cause of trauma, to address underlying factors such as dry mouth or substituting a problem medication.
- Maintaining good oral hygiene and use of an antiseptic mouthwash or spray (e.g., chlorhexidine) can prevent secondary infection and therefore hasten healing.
- A topical analgesic (e.g., benzydamine mouthwash) may reduce pain. Topical (gels, creams or inhalers) or systemic steroids may be used to reduce inflammation.
- An antifungal drug may be used to prevent oral candidiasis developing in those who use prolonged steroids. People with mouth ulcers may prefer to avoid hot or spicy foods, which can increase the pain.
- Self-inflicted ulceration can be difficult to manage, and psychiatric input may be required in some people. For recurrent ulcers, vitamin B12 has been shown to be effective.[1]
Prevention
Prevention
While not all oral ulcers can be entirely prevented, certain measures can help reduce their frequency and severity. Here are some preventive strategies:
Good Oral Hygiene:
- Brush and floss regularly: Helps remove plaque and food debris, reducing the risk of bacterial and fungal infections that can contribute to ulceration.
- Use a soft-bristled toothbrush: Avoids trauma to the oral mucosa, which can trigger ulcers.
- See your dentist regularly: Professional cleanings and checkups can identify and address potential sources of irritation or infection early on. [6]
Avoid Triggers:
- Identify and avoid foods or drinks: That seem to trigger ulcers, such as acidic or spicy foods.
- Manage stress: Stress reduction techniques like exercise, meditation, or yoga can be helpful for individuals with stress-induced ulcers.
- Protect against trauma: Use caution when eating or brushing your teeth to avoid accidental injuries. [6]
Manage Underlying Conditions:
- Control systemic diseases: If oral ulcers are associated with underlying medical conditions, managing those conditions can help reduce ulcer frequency and severity.
- Address nutritional deficiencies: Ensure adequate intake of iron, vitamin B12, and folate through diet or supplements. [6]
Other Preventive Measures:
- Avoid tobacco and alcohol: These can irritate the oral mucosa and increase the risk of oral cancer, which can present with ulcers.
- Use protective dental appliances: If wearing braces or dentures, ensure they fit properly and do not cause irritation.
- Be cautious with medications: Discuss any potential side effects of medications with your doctor, especially if they include oral ulcers. [7]
Important Note: These preventive measures can help reduce the risk of oral ulcers, but it is essential to consult a qualified healthcare professional or dentist for personalized advice and treatment options.
Homeopathic Treatment
Homeopathic Treatment of Ulcer of Oral Cavity
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Ulcer of Oral Cavity:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
Arsenic Alb
- Basically, Suitable for people who have a lot of fears including fear of death, who are meticulous and keep finding faults in work done by others
- Livid, bluish. May be white, Gangrenous
- Want of appetite and hunger, Burning in mouth
- Ulcers seen especially on tongue have a blue colored base
- Unhealthy gums that bleed easily
- Painful mouth ulcers.
- Hot drinks reduce the pain
- Restlessness along with pain
- Worse specifically in cold temperature, after consuming cold food and drinks.
Borax
- Aphthae in the mouth inside of cheeks and on tongue, which bleed easily.
- Great heat and dryness of mouth. Painful red blisters on tongue.
- Mouth ulcers feels hot also very sensitive
- Dry mouth despite excessive salivation
- In some cases, white fungus like growth may be noted in oral cavity.
- Besides this, Mouth is tender to touch
- Ulcers bleed easily on the slightest touch.
- Forepart of palate shriveled, paining esp. when chewing. Child cries especially when nursing.
Merc-sol
- Suitable for people who have low will power, are mistrustful, and feel useless.
- Metallic taste in mouth.
- Gums are very spongy also bleed easily.
- Dribbling of saliva
- Entire ulcer is red and moist.
- Sore mouth with profuse salivation.
- Saliva dribbles from mouth of the child.
- Gums also cheeks ulcerated.
- Fetid odours from mouth.
- Lastly, All symptoms are worse at night.
Nitric acid
- Nitric acid works well in individuals who are past middle age and those who have good appetite.
- Mouth ulcers mainly in soft upper palate.
- Halitosis, swelling of gums.
- Tongue is clean with a furrow in center.
- Symptoms worse in the evening.
- Aphthae usually whitish. Additionally, Blisters and ulcers on tongue.
- Pricking pain as if from a splinter.
- Profuse salivation; fetid odours specifically from mouth.
- Unusual craving for indigestible things like chalk, mud etc.
Mercurious corrosivus
- Chronic untreated mouth ulcers.
- Painful ulcers with bleeding.
- Gums are swollen and spongy.
- Bad odor from mouth.
- Mouth clears associated with excessive pain also tenesmus in the intestine.
- Green, bilious vomiting.
- Stomach region is very sensitive to touch.
- Symptoms increase at night and with consuming strongly acidic food.[2]
Condurango:
- This remedy suits people of all ages but it is more effective in individuals who are past middle age.
- Cracks and ulcers in corner of the mouth.
- Angular stomatitis.
- Constant burning pain felt in the mouth that may extend to the stomach.[2]
Diet & Regimen
Diet & Regimen
Diet for Mouth Ulcers:
Foods to Favor:
- Cooling and soothing foods: Yogurt, milk, ice cream, and custards can provide relief.
- Soft, bland foods: Mashed potatoes, cooked cereals, and well-cooked vegetables are easy to eat and won’t irritate the ulcers.
- Vitamin-rich foods: Include foods rich in Vitamin B12 (dairy, eggs, fish), Vitamin C (citrus fruits, strawberries), and iron (leafy greens, beans) to support healing.
- Hydrating foods: Watermelon, cucumber, and other water-rich fruits and vegetables help maintain oral health.
Foods to Avoid:
- Spicy and acidic foods: These can irritate the ulcers and increase pain. Avoid citrus fruits, tomatoes, spicy sauces, and vinegar-based dressings.
- Crunchy and sharp foods: Chips, nuts, and hard crackers can cause further damage to the delicate tissue.
- Hot foods and drinks: Allow food and drinks to cool down before consuming to avoid irritation.
- Alcohol and carbonated drinks: These can irritate and dehydrate the mouth, delaying healing.
Regimen for Mouth Ulcers:
- Maintain good oral hygiene: Brush gently with a soft-bristled toothbrush and floss daily. Consider using a mild toothpaste or saltwater rinse.
- Hydration: Drink plenty of water throughout the day to keep your mouth moist and promote healing.
- Avoid irritants: Identify and avoid any potential triggers, such as certain foods, toothpaste brands, or mouthwashes.
- Topical treatments: Over-the-counter gels and creams can provide temporary relief and promote healing.
- Medical advice: If ulcers are severe, persistent, or recurring, consult a doctor or dentist to rule out any underlying medical conditions
Do’s and Don'ts
Do’s & Don’ts of Ulcer Of Oral Cavity
Ulcer Of Oral Cavity Do’s & Don’ts
Do’s:
- Maintain good oral hygiene: Brush your teeth gently twice a day with a soft-bristled toothbrush and floss daily. This helps prevent infections that can worsen ulcers or delay healing.
- Rinse with warm salt water or baking soda solution: Mix ½ teaspoon of salt or baking soda in a cup of warm water and rinse several times a day. This can soothe irritation and promote healing.
- Use over-the-counter pain relievers or topical anesthetics: Products containing benzocaine or lidocaine can temporarily numb the area and provide pain relief.
- Apply a protective paste or gel: Over-the-counter products like Orabase can create a barrier over the ulcer, protecting it from further irritation.
- Eat soft, bland foods: Avoid spicy, acidic, or crunchy foods that can irritate the ulcer. Opt for soft, easily chewable foods like yogurt, mashed potatoes, or smoothies.
- Drink plenty of fluids: Staying hydrated is important for overall health and can help prevent dehydration, especially if eating is painful.
- See your dentist or doctor: If the ulcer persists for more than two weeks, is unusually large or painful, or is accompanied by other symptoms like fever or swollen lymph nodes, seek professional evaluation.
Don’ts:
- Don’t pick or scratch the ulcer: This can delay healing and increase the risk of infection.
- Don’t use harsh mouthwashes or toothpastes: These can irritate the ulcer and worsen the pain.
- Don’t smoke or use tobacco products: These can delay healing and increase the risk of oral cancer.
- Don’t consume excessive alcohol: Alcohol can irritate the oral mucosa and contribute to ulcer formation.
- Don’t share utensils or personal items: If the ulcer is caused by a contagious infection, sharing can spread the infection to others.
Terminology
Terminology
Here are some terminologies and their meanings commonly used in the context of oral ulcers:
Ulcer:
- An open sore or lesion on the skin or mucous membrane, often accompanied by inflammation and pain.
Oral Mucosa:
- The lining of the oral cavity, including the lips, cheeks, tongue, gums, palate, and floor of the mouth.
Pathogenesis:
- The origin and development of a disease or condition.
Pathophysiology:
- The functional changes associated with or resulting from disease or injury.
Epidemiology:
- The study of the distribution and determinants of health-related states or events (including disease) and the application of this study to the control of diseases and other health problems.
Prevalence:
- The proportion of a population found to have a condition (typically a disease or a risk factor such as smoking or seat-belt use) at a specific point in time.
Risk Factors:
- Characteristics or behaviors that increase the likelihood of developing a disease or health problem.
Clinical Features:
- The signs and symptoms observed in a patient with a particular disease or condition.
Clinical Examination:
- The process of evaluating a patient’s health through physical examination and observation.
Complications:
- Unfavorable outcomes or consequences that may arise from a disease, condition, or treatment.
Investigations:
- Diagnostic procedures or tests used to identify the underlying cause of a disease or condition.
Prevention:
- Actions taken to reduce the risk of developing a disease or health problem.
Traumatic Ulcer:
- An oral ulcer caused by physical injury, such as biting, irritation from dental appliances, or harsh brushing.
Recurrent Aphthous Stomatitis (RAS):
- A common condition characterized by recurrent episodes of painful oral ulcers, also known as canker sores.
Infectious Ulcer:
- An oral ulcer caused by a viral, bacterial, or fungal infection.
Neoplastic Ulcer:
- An oral ulcer associated with a cancerous growth.
Systemic Diseases:
- Diseases that affect the entire body or multiple organ systems, rather than a single organ or body part.
These terms are essential for understanding the various aspects of oral ulcers, from their underlying causes and development to their clinical presentation, diagnosis, treatment, and prevention.
Here are some other terminologies and their meanings commonly used in homeopathic articles discussing ulcers of the oral cavity:
Aphthous Ulcers:
- Also known as canker sores, these are recurrent, painful ulcers that appear on the non-keratinized mucosa of the oral cavity.
Constitutional Remedy:
- A homeopathic remedy chosen based on the individual’s overall physical, mental, and emotional characteristics, rather than just the specific symptoms of the ulcer.
Aggravation:
- A temporary worsening of symptoms after taking a homeopathic remedy, often considered a positive sign indicating the remedy is working.
Amelioration:
- An improvement in symptoms following the administration of a homeopathic remedy.
Miasm:
- A predisposition to certain types of diseases or chronic conditions, believed to be inherited or acquired.
Potency:
- The strength or dilution of a homeopathic remedy. Higher potencies are considered more diluted and are generally used for chronic or deep-seated conditions.
Repertory:
- A reference book listing symptoms and the remedies associated with them, used by homeopaths to select the most appropriate remedy.
Materia Medica:
- A collection of detailed descriptions of the symptoms and characteristics associated with each homeopathic remedy.
Specific Remedies and Their Indications (as often mentioned in homeopathic literature):
- Borax: Indicated for ulcers that are sensitive to touch and worse with hot or cold drinks.
- Mercurius Solubilis: Used for ulcers with excessive salivation, metallic taste, and a tendency to bleed easily.
- Nitric Acid: Suitable for ulcers with sharp, stinging pain, especially on the tongue or gums.
- Sulphur: Often prescribed for ulcers with burning pain and a tendency for skin eruptions.
References
References use for Article Ulcers of Oral cavity
- Text Book of Medicine Golwala
- The Homoeopathic Prescriber By K. C. Bhanja
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/mouth-ulcers
- https://pubmed.ncbi.nlm.nih.gov
- Shetty S, Vinay B, Umesh L, Hallikeri K. Prevalence of recurrent aphthous ulceration in the Indian Population. Medicina Oral, Patología Oral y Cirugia Bucal. 2011 Jan 1;16(1):e36-9.
- Reference: Burket’s Oral Medicine, 13th Edition, Greenberg, Glick, 2019, BC Decker Inc.
- Reference: Contemporary Oral and Maxillofacial Surgery, 7th Edition, Hupp, Ellis, Tucker, 2019, Elsevier
Also Search As
Also Search As
People can search for homeopathic articles on oral ulcers using a variety of methods and search terms, both online and offline:
Online Search:
- Search engines:
- Using popular search engines like Google, Bing, or DuckDuckGo.
- Key search terms:
- "homeopathic treatment for oral ulcers"
- "homeopathy for mouth ulcers"
- "homeopathic remedies for canker sores"
- "oral ulcers homeopathic medicine"
- Combine specific remedies: "Borax for mouth ulcers" or "Mercurius solubilis for oral ulcers"
Homeopathic websites and forums:
- Reputable homeopathic websites often have sections dedicated to specific conditions, including oral ulcers.
- Online forums where homeopaths and patients discuss cases and remedies can also provide useful information.
Social media:
- Homeopathic practitioners and organizations often share articles and information on social media platforms.
- Search for relevant hashtags or follow homeopathic pages to stay updated.
Online libraries and databases:
- Access to online databases of homeopathic journals and publications may require subscriptions or institutional access.
- These can provide in-depth research articles on homeopathic treatment approaches.
Offline Search:
- Books:
- Visit your local library or bookstore and look for books on homeopathy, specifically those addressing oral health or specific remedies.
- Key titles might include "Materia Medica" or "Repertory" books.
- Homeopathic practitioners:
- Consult a qualified homeopath in your area for personalized advice and treatment recommendations.
- They can provide information on relevant homeopathic articles and research.
- Homeopathic pharmacies:
- Some homeopathic pharmacies may have brochures or information leaflets on common conditions, including oral ulcers.
Important Considerations:
- Reliable sources: Be sure to use credible sources when searching for information online, such as reputable homeopathic organizations or websites with clear author credentials.
- Consult a professional: Always seek professional advice from a qualified homeopath before self-treating with homeopathic remedies.
- Individualized treatment: Homeopathy emphasizes personalized treatment based on the individual’s unique symptoms and constitution. A consultation with a homeopath is essential for identifying the most suitable remedy.
There are numerous ways to search for information on Ulcer of Oral Cavity, utilizing both online and offline resources:
Online:
- Search Engines:
- Use general search engines like Google, Bing, DuckDuckGo.
- Key search terms:
- "Oral ulcers"
- "Mouth ulcers"
- "Canker sores"
- "Aphthous ulcers"
- Combine with specific aspects: "Oral ulcer causes", "Oral ulcer treatment", "Oral ulcer symptoms"
- Medical Websites & Databases:
- Reputable health websites: Mayo Clinic, WebMD, Healthline, etc.
- Medical databases: PubMed, Google Scholar (for research articles)
- Dental association websites: American Dental Association (ADA), etc.
- Image Search:
- Can help visualize different types of oral ulcers.
- Use image search on search engines or specialized medical image websites.
- Social Media & Forums:
- Health-related groups or forums might have discussions on oral ulcers.
- Exercise caution and verify information from reliable sources.
Offline:
- Books:
- Medical textbooks: Dentistry, Oral Medicine, Pathology
- Health & wellness books on oral care
- Libraries:
- Local or university libraries often have a vast collection of medical resources.
- Healthcare Professionals:
- Consult your dentist or doctor for personalized information and advice.
- Pharmacies:
- Pharmacists can provide information on over-the-counter treatments and oral care products.
Tips for Effective Searching:
- Use specific terms: Be as specific as possible in your search terms. For instance, instead of just "mouth sore," try "painful white ulcer on tongue."
- Combine keywords: Use multiple keywords to narrow down your search results.
- Filter results: Use search engine filters to refine results by date, type of content, or region.
- Check source credibility: Always verify information from reliable sources like medical websites, professional organizations, or peer-reviewed journals.
Remember, the best way to search depends on the specific information you are seeking. Whether you are looking for general information, images for identification, treatment options, or the latest research, a combination of these methods can help you find the information you need.
Frequently Asked Questions (FAQ)
What is an oral ulcer?
An oral ulcer, or mouth ulcer, is an open sore that develops on the soft tissues inside your mouth, like the tongue, cheeks, gums, or lips.
They can be painful and make eating, drinking, and speaking uncomfortable.
What causes oral ulcers?
Oral ulcers can have various causes, including:
- Injury: Accidental biting, irritation from braces or dentures, or harsh toothbrushing.
- Infections: Viral (like herpes simplex), bacterial, or fungal infections.
- Underlying medical conditions: Autoimmune diseases, inflammatory bowel disease, nutritional deficiencies, or even certain medications.
- Stress: Emotional stress can trigger or worsen some types of oral ulcers.
How are oral ulcers treated?
Treatment depends on the cause and severity of the ulcer:
- Mild cases: May heal on their own within 1-2 weeks with good oral hygiene and over-the-counter pain relief options.
- Severe or persistent cases: May require prescription medications like topical corticosteroids, antimicrobial mouthwashes, or even systemic medications in cases of underlying diseases.
What are the common symptoms of oral ulcers?
Symptoms typically include:
- Pain or tenderness: Especially when eating or brushing teeth.
- Redness and swelling: Around the ulcer.
- A crater-like sore: Often with a white or yellow center and a red border.
- Difficulty eating or speaking: In severe cases.
How are oral ulcers diagnosed?
Usually, a dentist or doctor can diagnose an oral ulcer based on its appearance and your medical history.
In some cases, additional tests like blood work or biopsies may be needed to rule out underlying conditions.
Can homeopathy treat oral ulcers?
Yes,
homeopathy offers a holistic approach to treating oral ulcers by addressing the underlying causes and individual susceptibility, aiming to promote healing and reduce recurrence.
Is homeopathy safe for treating oral ulcers?
Homeopathic remedies are generally considered safe when prescribed and administered by a qualified homeopath.
However, it is crucial to consult a professional for proper diagnosis and treatment.
Can homeopathy prevent oral ulcers from recurring?
By addressing the underlying causes and strengthening the immune system, homeopathy aims to reduce the frequency and severity of recurrent oral ulcers.
Which homeopathic remedies are commonly used for oral ulcers?
Several Homeopathic remedies are used based on specific symptoms, such as:
- Borax: For ulcers sensitive to touch and aggravated by hot or cold drinks.
- Mercurius Solubilis: For ulcers with excessive salivation, metallic taste, and bleeding tendency.
- Nitric Acid: For ulcers with sharp, stinging pain, especially on the tongue or gums.
How does homeopathic treatment differ from conventional treatment for oral ulcers?
Homeopathy focuses on the individual’s overall health and constitution, aiming to stimulate the body’s self-healing abilities.
Conventional treatments often focus on symptom relief with topical medications or addressing specific underlying causes.
