Gall Bladder Stones
Definition
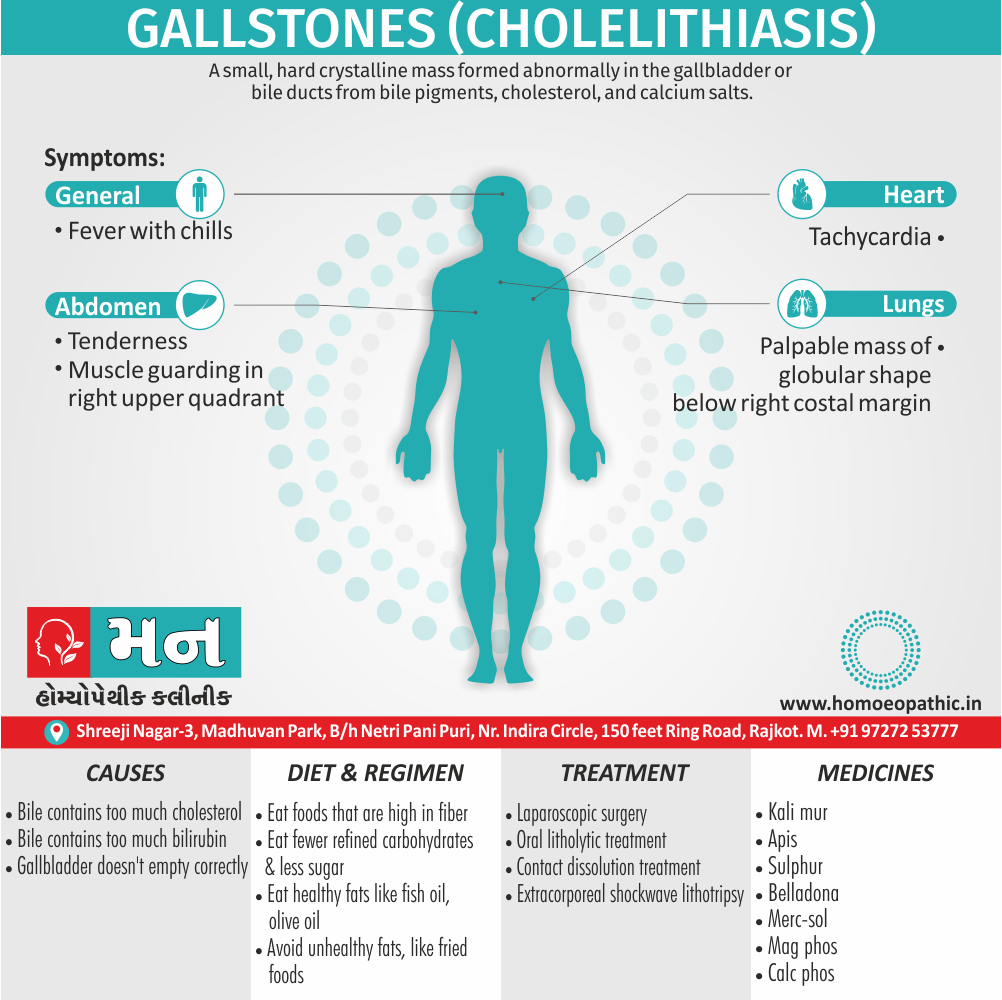
Galls Bladder Stones (Cholelithiasis) is a small, hard crystalline mass formed abnormally in the gall bladder or bile ducts from bile pigments, cholesterol, also calcium salts. Gall Bladder Stones can cause severe pain and blockage of the bile duct. [1]
Here are some synonyms for gall bladder stones:
- Cholelithiasis: This is the medical term for gallstones. It comes from the Greek words "chole" (bile), "lithos" (stone), and "-iasis" (condition).
- Biliary calculi: This term refers to any stones present in the biliary system, which includes the gallbladder and bile ducts.
- Gallbladder calculi: This term specifically refers to stones located in the gallbladder.
- Gallstones: This is the most common term used in everyday language.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
Generally, Gall Bladder Stone formation is the most common disorder of the biliary tree and it is unusual for the gallbladder to be diseased in the absence of gallstones. Moreover, In developed countries, gallstones occur in 7% of males and 15% of females aged 18–65 years, with an overall prevalence of 11%. Individuals under 40 years there is a 3:1 female preponderance, whereas in the people who are older in age the sex ratio is about equal.
In developed countries, the incidence of symptomatic gallstones appears to be increasing and they occur at an earlier age. Gallstones are less frequent in India, the Far East also Africa. There has been much debate over the role of diet in cholesterol gallstone disease; an increase in dietary cholesterol, fat, total calories and refined carbohydrate or lack of dietary fiber has been implicated. At present, the best data support an association between simple refined sugar in the diet and gallstones. [1]
Epidemiology
Epidemiology of Gall Bladder Stones
The estimated prevalence of gallstone disease in India has been reported as 2% to 9%. It is seven times more frequent in North India compared to South India.
Reference:
- Singh V, Singh R, Singh S, et al. Epidemiological study in operated patients with cholelithiasis and analysis of risk factors. International Journal of Recent Surgical and Medical Sciences. 2016;2(1):23-28. [6]
Causes
Causes
It’s not clear what causes gall bladder stones to form. Doctors think gallstones may result when:
- Your bile contains too much cholesterol. Normally, your bile contains enough chemicals to dissolve the cholesterol excreted by your liver. But if your liver excretes more cholesterol than your bile can dissolve, the excess cholesterol may form into crystals and eventually into stones.
- Your bile contains too much bilirubin. Bilirubin is a chemical that’s produced when your body breaks down red blood cells. Certain conditions cause your liver to make too much bilirubin, including liver cirrhosis, biliary tract infections and certain blood disorders. The excess bilirubin contributes to gallstone formation.
Your gallbladder doesn’t empty correctly. If your gallbladder doesn’t empty completely or often enough, bile may become very concentrated, contributing to the formation of gallstones [2]
Types
Types
- Cholesterol gallstones. The most common type of gallstone, called a cholesterol gallstone, often appears yellow in colour. Additionally, these gallstones are composed mainly of undissolved cholesterol, but may contain other components.
- Pigment gallstones. These either dark brown or black stones form when your bile contains too much bilirubin.[2]
Risk Factors
Risk factors of Gall Bladder Stones
- Obesity: Excess body weight, particularly central obesity, is a major risk factor, especially in women.
- Female sex: Women are two to three times more likely to develop gallstones than men.
- Age: The risk increases with age, particularly after 40.
- Ethnicity: Native Americans and Mexican Americans have a higher prevalence of gallstones.
- Rapid weight loss: Rapid weight loss, as seen after bariatric surgery or crash dieting, can increase the risk.
- Pregnancy: Hormonal changes and increased cholesterol saturation of bile during pregnancy can contribute to gallstone formation.
- Certain medications: Medications containing estrogen, such as oral contraceptives and hormone replacement therapy, can increase the risk.
- Family history: A family history of gallstones increases an individual’s risk.
- Medical conditions: Certain medical conditions, such as diabetes mellitus, Crohn’s disease, and cirrhosis, are associated with an increased risk of gallstones. [7]
Pathogenesis
Pathogenesis of Gall Bladder Stones
The pathogenesis of gallstones is a complex process involving various factors that lead to the formation of stones within the gallbladder. These factors can be broadly categorized into:
1. Cholesterol Supersaturation of Bile:
- The liver secretes cholesterol into bile, and when the concentration of cholesterol exceeds the solubilizing capacity of bile acids and phospholipids, bile becomes supersaturated with cholesterol.
- This supersaturation promotes the nucleation and crystallization of cholesterol, leading to the formation of cholesterol crystals, which eventually aggregate to form cholesterol stones.
- Factors that increase cholesterol secretion or decrease bile acid and phospholipid secretion can contribute to cholesterol supersaturation.
2. Gallbladder Hypomotility:
- Impaired gallbladder emptying (hypomotility) allows for the prolonged retention of bile within the gallbladder, providing more time for cholesterol crystals to form and aggregate into stones.
- Hypomotility can be caused by various factors, including hormonal imbalances, neural dysfunction, or intrinsic gallbladder muscle abnormalities.
3. Nucleation and Crystallization Promoters:
- Mucin glycoproteins, secreted by the gallbladder epithelium, can promote the nucleation and aggregation of cholesterol crystals.
- Abnormal mucin secretion or changes in mucin composition can contribute to stone formation.
4. Pigment Stone Formation:
- Pigment stones are primarily composed of calcium bilirubinate and can be black or brown.
- Black pigment stones are associated with chronic hemolysis, increased bilirubin turnover, and sterile bile.
- Brown pigment stones are often associated with bacterial infection within the biliary tract, leading to the release of enzymes that deconjugate bilirubin and promote stone formation. [7]
Pathophysiology
Pathophysiology
- Gall Bladder Stones are conveniently classified into cholesterol or pigment stones, although the majority is of mixed composition.
- Cholesterol stones are most common in developed countries, whereas pigment stones are more frequent in developing countries.
- Gall Bladder stones contain varying quantities of calcium salts, including calcium bilirubinate, carbonate, phosphate also palmitate, which simper radio-opaque.
- All in all, Gallstone formation is multifactorial, toms are not now recognized as being caused by and the factors involved are related to the type of gallstone [2]
Clinical Features
Clinical Features of Gall Bladder Stones
The clinical presentation of gallstones (cholelithiasis) is highly variable, ranging from asymptomatic to severe and life-threatening complications.
Asymptomatic Gallstones:
- The majority (80%) of individuals with gallstones are asymptomatic, meaning they do not experience any noticeable symptoms.
- These "silent" stones are often discovered incidentally during imaging studies performed for other reasons.
Symptomatic Gallstones:
- Biliary Colic: The most common symptom is biliary colic, a sudden onset of severe, steady pain in the upper right abdomen or epigastric region.
- The pain typically radiates to the right shoulder or back and may last for several hours.
- triggered by fatty meals and may be accompanied by nausea, vomiting, and sweating.
- Acute Cholecystitis: Inflammation of the gallbladder (cholecystitis) usually occurs due to a gallstone obstructing the cystic duct.
- It presents with persistent right upper quadrant pain, fever, and leukocytosis.
- Patients may also experience Murphy’s sign (increased tenderness on palpation of the right upper quadrant during inspiration).
- Choledocholithiasis: This refers to the presence of gallstones in the common bile duct, which can cause biliary obstruction.
- It may manifest with jaundice (yellowing of the skin and eyes), dark urine, pale stools, and pruritus (itching).
- Gallstone Pancreatitis: Obstruction of the pancreatic duct by a gallstone can lead to pancreatitis, characterized by severe epigastric pain radiating to the back, nausea, vomiting, and elevated pancreatic enzymes.
Chronic Cholecystitis:
- Repeated episodes of biliary colic or acute cholecystitis can result in chronic inflammation of the gallbladder.
- Patients may experience recurrent abdominal pain, dyspepsia, and intolerance to fatty foods. [7]
Sign & Symptoms
Sign & Symptoms
(I) General—Include fever with often chills at Onset, also tachycardia.
(II)Local—
(a) Tenderness and muscle guarding in right upper quadrant.
(b) Palpable mass of globular shape below right costal margin also moving on inspiration may be felt.
(c) Murphy’s sign – Patient complains of pain on taking a deep breath while the examiner’s hand is pressed below the right costal margin.
(d) Abdominal distension – may occur and if marked simulates intestinal obstruction.
(e)Boa’s sign – Area of hyperesthesia over right subscapular region.[2]
Clinical Examination
Clinical Examination of Gallbladder Stones
Physical examination findings in patients with gallstone disease can vary depending on the presence and severity of symptoms, as well as any complications that may have developed.
Asymptomatic Gallstones:
- Physical examination is often unremarkable in patients with asymptomatic gallstones.
- There may be no specific findings on abdominal palpation or other aspects of the exam.
Symptomatic Gallstones:
- Biliary Colic:
- Tenderness in the right upper quadrant (RUQ) or epigastric region during palpation.
- No peritoneal signs (e.g., guarding, rigidity, rebound tenderness) unless complications are present.
- Murphy’s sign may be positive (increased tenderness and sudden cessation of inspiration during deep palpation of the RUQ).
- Acute Cholecystitis:
- RUQ tenderness and guarding, with possible rebound tenderness.
- Fever and tachycardia may be present.
- Positive Murphy’s sign is often elicited.
- Choledocholithiasis:
- Jaundice (yellowing of the skin and sclera) may be present due to biliary obstruction.
- Palpable gallbladder (Courvoisier’s sign) may be present in cases of malignant obstruction.
- Gallstone Pancreatitis:
Chronic Cholecystitis:
- Physical examination findings may be similar to those of acute cholecystitis, but typically less severe.
- RUQ tenderness may be present, but fever and other systemic signs are less common. [7]
Diagnosis
Diagnosis
Tests and procedures used to diagnose gall bladder stones also complications of gallstones include:
- Abdominal ultrasound. This test is the one most commonly used to look for signs of gallstones. Abdominal ultrasound involves moving a device (in other words; transducer) back and forth across your stomach area. Additionally, the transducer sends signals to a computer, which creates images that show the structures in your abdomen.
- Endoscopic ultrasound (EUS). This procedure can help identify smaller stones that may be missed on an abdominal ultrasound. During EUS your doctor passes a thin, flexible tube (i.e. endoscope) through your mouth and through your digestive tract. A small ultrasound device (i.e. transducer) in the tube produces sound waves that create a precise image of surrounding tissue.
Other imaging tests.
- Additional tests may include oral cholecystography, a hepatobiliary iminodiacetic acid (i.e. HIDA) scan, computerized tomography (i.e. CT), magnetic resonance cholangiopancreatography (i.e. MRCP) or endoscopic retrograde cholangiopancreatography (in other words; ERCP). Gallstones discovered using ERCP can be removed during the procedure.
- Blood tests. In detail; Blood tests may reveal infection, jaundice, pancreatitis or other complications caused by gallstones.[3]
Differential Diagnosis
Differential Diagnosis of Gallbladder Stones
The differential diagnosis for gallstones (cholelithiasis) includes various conditions that can mimic its symptoms, particularly biliary colic and acute cholecystitis. These conditions often present with abdominal pain, making it essential to distinguish them from gallstone disease for accurate diagnosis and appropriate management.
Gastrointestinal Conditions:
- Peptic ulcer disease
- Gastritis
- Gastroesophageal reflux disease (GERD)
- Pancreatitis (acute or chronic)
- Appendicitis
- Irritable bowel syndrome (IBS)
- Diverticulitis
- Hepatitis
Hepatobiliary Conditions:
- Biliary dyskinesia (functional gallbladder disorder)
- Sphincter of Oddi dysfunction
- Cholangitis (infection of the bile ducts)
- Choledocholithiasis (gallstones in the common bile duct)
- Primary sclerosing cholangitis (PSC)
Cardiopulmonary Conditions:
- Myocardial infarction (heart attack)
- Pneumonia
- Pleurisy
- Pulmonary embolism
Other Conditions:
- Renal colic (kidney stones)
- Pyelonephritis (kidney infection)
- Herpes zoster (shingles)
- Fitz-Hugh-Curtis syndrome (pelvic inflammatory disease with liver capsule inflammation) [7]
Complications
Complications of Gallstones:
- Cholangitis: Infection of the bile ducts, which can be life-threatening.
- Gallbladder perforation: Rupture of the gallbladder, leading to peritonitis.
- Gallstone ileus: Obstruction of the small intestine by a large gallstone that has eroded into the intestine.
- Mirizzi syndrome: Impaction of a gallstone in the cystic duct or gallbladder neck, causing compression of the common hepatic duct. [7]
Investigations
Investigations of Gallbladder Stones
Laboratory Tests:
Liver Function Tests (LFTs):
- Elevated levels of bilirubin (especially conjugated bilirubin), alkaline phosphatase (ALP), and gamma-glutamyl transferase (GGT) may suggest biliary obstruction due to gallstones.
- Aspartate aminotransferase (AST) and alanine aminotransferase (ALT) may be elevated in cases of acute cholecystitis or choledocholithiasis.
Complete Blood Count (CBC):
- Leukocytosis (elevated white blood cell count) is common in acute cholecystitis.
Amylase and Lipase:
- Elevated levels may indicate gallstone pancreatitis.
Imaging Studies:
Abdominal Ultrasound:
- The first-line imaging modality for evaluating suspected gallstones.
- Highly sensitive and specific for detecting gallstones within the gallbladder.
- Can also assess gallbladder wall thickness, ductal dilatation, and pericholecystic fluid.
Magnetic Resonance Cholangiopancreatography (MRCP):
- Non-invasive imaging technique that visualizes the biliary tree and pancreatic duct without contrast dye.
- Useful for detecting choledocholithiasis and evaluating bile duct anatomy.
- Non-invasive imaging technique that visualizes the biliary tree and pancreatic duct without contrast dye.
Endoscopic Ultrasound (EUS):
- Combines endoscopy with ultrasound to provide detailed images of the biliary tree and surrounding structures.
- Can detect small gallstones and evaluate the gallbladder wall for signs of malignancy.
- Combines endoscopy with ultrasound to provide detailed images of the biliary tree and surrounding structures.
Computed Tomography (CT) Scan:
- Less sensitive than ultrasound for detecting gallstones, but can be useful for identifying complications like perforation or abscess.
Hepatobiliary Iminodiacetic Acid (HIDA) Scan:
- Nuclear medicine scan that evaluates gallbladder function and cystic duct patency.
- Can help diagnose acute cholecystitis when ultrasound is inconclusive.
- Nuclear medicine scan that evaluates gallbladder function and cystic duct patency.
Additional Investigations:
Endoscopic Retrograde Cholangiopancreatography (ERCP):
- Therapeutic and diagnostic procedure that uses an endoscope to visualize the biliary tree and remove gallstones from the common bile duct.
- Therapeutic and diagnostic procedure that uses an endoscope to visualize the biliary tree and remove gallstones from the common bile duct.
Percutaneous Transhepatic Cholangiography (PTC):
- Rarely used imaging technique that involves injecting contrast dye directly into the bile ducts through the skin.
- May be helpful in cases of complex biliary obstruction. [7]
- Rarely used imaging technique that involves injecting contrast dye directly into the bile ducts through the skin.
Treatment
Treatment
For Gall bladder stones, Surgical treatment—Laparoscopic or open cholecystectomy is the only radical procedure for symptomatic gallstones.
Non-surgical treatment
Oral litholytic treatment i.e.
- Bile acids Chenodeoxycholic acid 10–12 mg/kg/day, and Ursodeoxycholic acid 10–12 mg/kg/day, either alone or in combination (using one half of the dose of each) is suitable for radiolucent small stones (<10 mm in diameter). Pigment stones are not responsive to medical therapy. Lastly, the whole dose should preferably be taken at bed time.
Side effects –
Chenodeoxycholic acid: diarrhoea also hypertransaminasemia.
Ursodeoxycholic acid: in brief; gallstone calcification resulting in treatment failure.
Contact dissolution treatment—
- Percutaneous transhepatic gallbladder puncture followed by application of methyl-butyl ether (powerful cholesterol solvent) directly to the stones. Any number also size of stones can be treated. In detail, Complete dissolution is usually achieved within a few hours.
Side effects – Post-puncture severe abdominal pain also nausea, erosive duodenitis and biliary peritonitis.
Extracorporeal shockwave lithotripsy (ESWL)
- Fragments the stones using focused sound waves; the fragments are subsequently dissolved by bile acid therapy. The procedure is suitable for patients with up to three stones of diameter 10–30 mm.
Side effects –
Biliary colic, haemobilia and pancreatitis.
Recurrent stones—
are radiolucent and smaller, and can be redissolved with bile acids if detected early.[1]
Prevention
Prevention of Gallbladder Stones
While not all gallstones can be prevented, certain lifestyle modifications and dietary changes can help reduce the risk of their formation:
Maintain a Healthy Weight:
- Obesity is a significant risk factor for gallstone development.
- Gradual weight loss through a balanced diet and regular exercise can help prevent gallstone formation.
- Avoid rapid weight loss or crash diets, as they can actually increase the risk of gallstones.
Eat a Healthy Diet:
- Consume a diet rich in fiber from fruits, vegetables, whole grains, and legumes.
- Choose healthy fats like those found in olive oil, fish, and nuts.
- Limit saturated and trans fats from fried foods, processed foods, and fatty meats.
- Moderate your intake of refined carbohydrates and sugary drinks.
Regular Physical Activity:
- Engage in regular exercise, aiming for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity exercise per week.
- Regular physical activity helps maintain a healthy weight and promotes gallbladder emptying.
Manage Medical Conditions:
- If you have diabetes, keep your blood sugar levels well-controlled.
- Manage other medical conditions that may increase the risk of gallstones, such as high cholesterol or inflammatory bowel disease.
Consider Medications:
- In some cases, medications like ursodeoxycholic acid (UDCA) may be prescribed to dissolve small cholesterol gallstones or prevent their formation in high-risk individuals. [7]
Homeopathic Treatment
Homoeopathic Treatment:
Homeopathic Treatment of Cholelithiasis
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Cholelithiasis:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicine Gallstones (Cholelithiasis):
- Kali mur: Air-Chilly in the open air. Additionally; Back and neck–Shivering over the back and neck with warm feet.
- Apis: General oedema. Inflammation of knee joint.
- Sulphur: Rawness in the larynx, with hoarseness. Dry cough especially in the evening, waking at night, with dyspnoea, (<) night when lying on the back, with pressure and anxiety in the chest; suffocation. Cough dry at night, but loose in the day time from crawling in the larynx. Burning in the chest, extending upward to the face. Besides this, Sharp sticking pains in the sides, often extending to back, (<) night and lying on the back. Anxiety and oppression in the chest. Weakness when talking.
- Belladona: Persistent, dry, also burning hot (with thirst), followed by sweat only on the head. Chill alternates with heat, internal heat, with anxiety; internal chill with external burning heat. In detail, Heat of the head, with coldness of the extremities.
- Merc-sol: Raised considerable mucus from larynx and trachea (second day). Larynx and trachea free from mucus; generally collected there in the morning (second day). Sensation of heat in the larynx (first day). Sensation of roughness in the larynx, after breakfast (second day). Occasional hoarseness (second day). Unusual expectoration of mucus (second day). Mercurial fetor of the breath (second day); (third day).
- MAGN PHOS: For the pain
- CALC PHOS: To prevent formation.
- LYCOPODIUM: Symptoms characteristically on right side of body, < 4-8 pm. Poor circulation, cold extremities, craves everything warm. Pains come and go suddenly. Great weakness of digestion. Better – by motion, after midnight also from warm food and drink.
CHINCHONA OFFICINALIS: Much flatulent colic. > Bending double. Pain in right hypochondrium. Gallstone colic. Jaundice. Stool undigested. Worse – slightest touch, after eating. On the other hand Better – bending double, warmth.[5]
Diet & Regimen
Diet & Regimen
for Gall stones
Diet:
- Healthy Weight Management: Maintaining a healthy weight is key, as rapid weight loss can increase your risk. Aim for gradual weight loss if needed.
- Fiber-Rich Foods: A high-fiber diet helps keep bile flowing, reducing the chance of stone formation. Choose fruits, vegetables, whole grains (brown rice, oats, whole wheat bread), and legumes (beans, lentils).
- Healthy Fats: Include moderate amounts of olive oil, avocados, nuts and seeds, and fatty fish (salmon, tuna).
- Limit Unhealthy Fats: Reduce your intake of saturated and trans fats found in fried foods, processed snacks, and fatty meats.
- Stay Hydrated: Drink plenty of water throughout the day to aid digestion and bile flow.
- Coffee Consumption: Some studies suggest that moderate coffee consumption may lower gallstone risk.
Regimen:
- Regular Meals: Avoid skipping meals to prevent disrupting bile flow and increasing gallstone risk.
- Physical Activity: Regular exercise helps with weight management and overall health, indirectly reducing gallstone risk.
- Medication: In some cases, your doctor may prescribe medication to dissolve gallstones or prevent their formation.
- Surgery: If gallstones cause significant symptoms or complications, surgical removal of the gallbladder (cholecystectomy) may be necessary.
Do’s and Don'ts
The Do’s & Don’ts
Do’s:
Maintain a healthy weight: Obesity is a major risk factor for gallstone development. Gradual weight loss through a balanced diet and regular exercise is recommended.
Eat a high-fiber diet: Fiber helps to reduce cholesterol levels and promote regular bowel movements, which can help prevent gallstones. Include plenty of fruits, vegetables, whole grains, and legumes in your diet.
Choose healthy fats: Opt for unsaturated fats found in olive oil, fish, nuts, and seeds. Avoid saturated and trans fats found in fried foods, processed foods, and fatty meats.
Stay hydrated: Drink plenty of water throughout the day to help prevent gallstone formation.
Limit your intake of refined carbohydrates and sugars: These can increase cholesterol levels and contribute to gallstone formation.
Exercise regularly: Physical activity helps maintain a healthy weight and promotes gallbladder emptying. Aim for at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise per week.
Manage underlying medical conditions: If you have conditions like diabetes or high cholesterol, manage them effectively to reduce your risk of gallstones.
Discuss preventive medications with your doctor: If you have a high risk of gallstones, your doctor may recommend medications like ursodeoxycholic acid (UDCA) to help prevent their formation.
Don’ts:
Do not skip meals: Skipping meals or fasting can increase the risk of gallstones by promoting the accumulation of cholesterol in the gallbladder.
Not lose weight too quickly: Rapid weight loss, such as crash dieting, can trigger gallstone formation.
Don’t eat a high-fat diet: Foods high in saturated and trans fats can increase cholesterol levels and promote gallstone formation. Limit your intake of fried foods, fatty meats, processed foods, and high-fat dairy products.
Never consume excessive alcohol: Alcohol can contribute to gallbladder problems and increase the risk of gallstones.
Do Not ignore symptoms: If you experience symptoms like abdominal pain, nausea, vomiting, or jaundice, seek medical attention promptly. Early diagnosis and treatment can prevent complications.
Terminology
Terminology
- Cholelithiasis: The presence of gallstones in the gallbladder.
- Cholecystitis: Inflammation of the gallbladder, often caused by gallstones blocking the cystic duct.
- Biliary colic: Severe pain in the upper right abdomen or epigastric region, often caused by gallstones obstructing the cystic duct.
- Choledocholithiasis: The presence of gallstones in the common bile duct.
- Cholangitis: Infection of the bile ducts, often caused by gallstones obstructing the flow of bile.
- Gallstone pancreatitis: Inflammation of the pancreas caused by gallstones obstructing the pancreatic duct.
- ERCP (Endoscopic Retrograde Cholangiopancreatography): A procedure that uses an endoscope to visualize and remove gallstones from the bile ducts.
Cholecystectomy:
- Surgical removal of the gallbladder, often the treatment of choice for symptomatic gallstones.
- Laparoscopic cholecystectomy: A minimally invasive surgical technique for removing the gallbladder through small incisions.
- Open cholecystectomy: A traditional surgical technique for removing the gallbladder through a larger incision.
- Lithotripsy: A procedure that uses shock waves to break up gallstones into smaller pieces that can pass through the bile ducts.
- Ursodeoxycholic acid (UDCA): A medication that can be used to dissolve small cholesterol gallstones or prevent their formation in high-risk individuals.
Homoeopathic Terminologies
- Similimum: The most similar remedy to the patient’s overall symptom picture, chosen based on the totality of symptoms.
- Totality of Symptoms: The complete picture of a patient’s symptoms, including physical, mental, and emotional aspects, considered crucial in choosing a homeopathic remedy.
- Rubrics: Headings in the repertory that describe specific symptoms.
- Keynote: A unique or characteristic symptom of a remedy that helps to distinguish it from others.
- Modalities: Factors that make a symptom better or worse, such as time of day, temperature, or position.
- Potentization: The process of diluting and succussing (shaking) a remedy to enhance its therapeutic effect.
- Succussion: The act of forcefully shaking a homeopathic remedy during its preparation.
- Nosode: A remedy made from diseased tissue or product.
- Organon of Medicine: The foundational text of homeopathy written by Samuel Hahnemann.
You may also encounter specific remedy names commonly used in gallstone cases like:
- Berberis vulgaris: For biliary colic with stitching pain radiating to the back.
- Calcarea carbonica: For large, fair individuals with a tendency towards constipation and gallstones.
- Chelidonium majus: For right-sided abdominal pain radiating to the right shoulder and associated with liver problems.
- Lycopodium clavatum: For individuals with digestive complaints, gas, and bloating along with gallstones.
- Nux vomica: For irritable individuals with a tendency towards constipation, indigestion, and spasmodic pain.
References
References
- Davidsons Principles and Practice of Medicine (PDFDrive.com)
- Medicine Golwala
- https://www.healthgrades.com/right-care/gallbladder-removal-surgery/cholelithiasis
- https://www.niddk.nih.gov/health-information/digestive-diseases/gallstones/eating-diet-nutrition
- T.F.Allen
- Singh V, Singh R, Singh S, et al. Epidemiological study in operated patients with cholelithiasis and analysis of risk factors. International Journal of Recent Surgical and Medical Sciences. 2016;2(1):23-28.
- Sleisenger and Fordtran’s Gastrointestinal and Liver Disease Review and Assessment, 11th Edition, by Anthony Fauci, Dan Longo, Dennis Kasper, Stephen Hauser, J. Larry Jameson, Joseph Loscalzo, 2021, Elsevier Saunders
Also Search As
Also Search As
Online Search Engines:
- Use search engines like Google, DuckDuckGo, or Ecosia.
- Combine keywords like "homeopathy," "gallstones," "gallbladder stones," "homeopathic treatment," "homeopathic remedies," etc.
- Look for articles on reputable homeopathic websites, blogs, or forums.
Homeopathic Journals and Publications:
- Many homeopathic journals publish articles on specific conditions like gallstones.
- Look for well-established journals like "The Homeopathic Journal," "Homeopathy," "The American Homeopath," or "Simillimum."
- Check the archives or online databases of these journals for relevant articles.
Homeopathic Libraries or Resource Centers:
- Many cities have homeopathic libraries or resource centers where you can find books and articles on various topics, including gallstones.
- Consult with librarians or staff for assistance in finding relevant materials.
Homeopathic Practitioners:
- Consult with a qualified homeopathic practitioner. They often have access to resources and can provide you with articles or research papers on gallstones from a homeopathic perspective.
Homeopathic Organizations:
- National or regional homeopathic organizations often have websites or publications with resources on different conditions.
- Check their websites or contact them for information on gallstones.
Other ways
1. Online Search Engines:
- General search engines: Use search engines like Google, Bing, or DuckDuckGo and enter keywords such as "gallbladder stones," "gallstone symptoms," "gallstone treatment," etc.
- Medical websites: Reputable medical websites like Mayo Clinic, WebMD, Cleveland Clinic, and Healthline provide comprehensive information on gallstones, including causes, symptoms, diagnosis, and treatment options.
- Academic databases: If you’re looking for more in-depth or scholarly information, search academic databases like PubMed or Google Scholar for research articles and medical publications on gallstones.
2. Libraries and Bookstores:
- Medical textbooks: Consult medical textbooks on gastroenterology or surgery for detailed information on gallstone disease.
- Health books: Look for books specifically about gallstones or digestive health in your local library or bookstore.
3. Healthcare Professionals:
- Primary care physician: Your doctor can provide you with information about gallstones, answer your questions, and refer you to a specialist if needed.
- Gastroenterologist: A gastroenterologist specializes in digestive disorders and can provide expert advice on diagnosis and treatment of gallstones.
- Surgeon: If surgery is being considered, consult with a surgeon specializing in gallbladder surgery to discuss the best approach for your case.
4. Support Groups and Online Forums:
- Patient support groups: Connect with other people who have experienced gallstones to share experiences, ask questions, and gain support.
- Online forums: Many online forums dedicated to health and wellness have discussions about gallstones, where you can find information and connect with others.
Frequently Asked Questions (FAQ)
What is Gallstones?
A small, hard crystalline mass formed abnormally in the gall bladder or bile ducts from bile pigments, cholesterol, and calcium salts. Gallstones can cause severe pain and blockage of the bile duct.
What causes Gallstones?
Causes
- Bile contains too much cholesterol
- Bile contains too much bilirubin
- Gallbladder doesn’t empty correctly
How are gallstones diagnosed?
Gallstones are usually diagnosed using an abdominal ultrasound. Other tests, such as CT scans, MRI scans, or HIDA scans, may also be used.
Is homeopathy safe for gallstones?
Homeopathic remedies are generally considered safe when prescribed by a qualified practitioner. However, it’s important to consult with a homeopath before starting any treatment, especially if you have a history of gallstones or other health conditions.
Can homeopathy dissolve gallstones?
Some homeopathic remedies have been traditionally used to help dissolve small gallstones, but this is not the primary goal of homeopathic treatment. The focus is on improving overall gallbladder health and function, reducing the risk of further stone formation, and managing associated symptoms.
What are the symptoms of Gallstones?
Symptoms
- Fever with often chills at Onset, and tachycardia.
- Tenderness and muscle guarding in right upper quadrant.
- Murphy’s sign
- Abdominal distension
- Boa’s sign
What is the homeopathic approach to gallstones?
Homeopathy treats gallstones holistically, focusing on the individual’s unique symptom pattern and underlying imbalances. It aims to stimulate the body’s natural healing abilities to address the root cause of gallstone formation, not just the symptoms.
How long does homeopathic treatment take for gallstones?
The duration of treatment varies depending on the individual’s case, the severity of symptoms, and the response to the remedies. Some people may experience improvement within a few weeks, while others may require longer-term treatment.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Gallstones?
Homeopathic Medicines for Gall Bladder Stones
- Kali mur
- Apis
- Sulphur
- Belladona
- Merc-sol
- Mag Phos
- Calcarea Phos
