Osteoarthritis (OA)
Definition
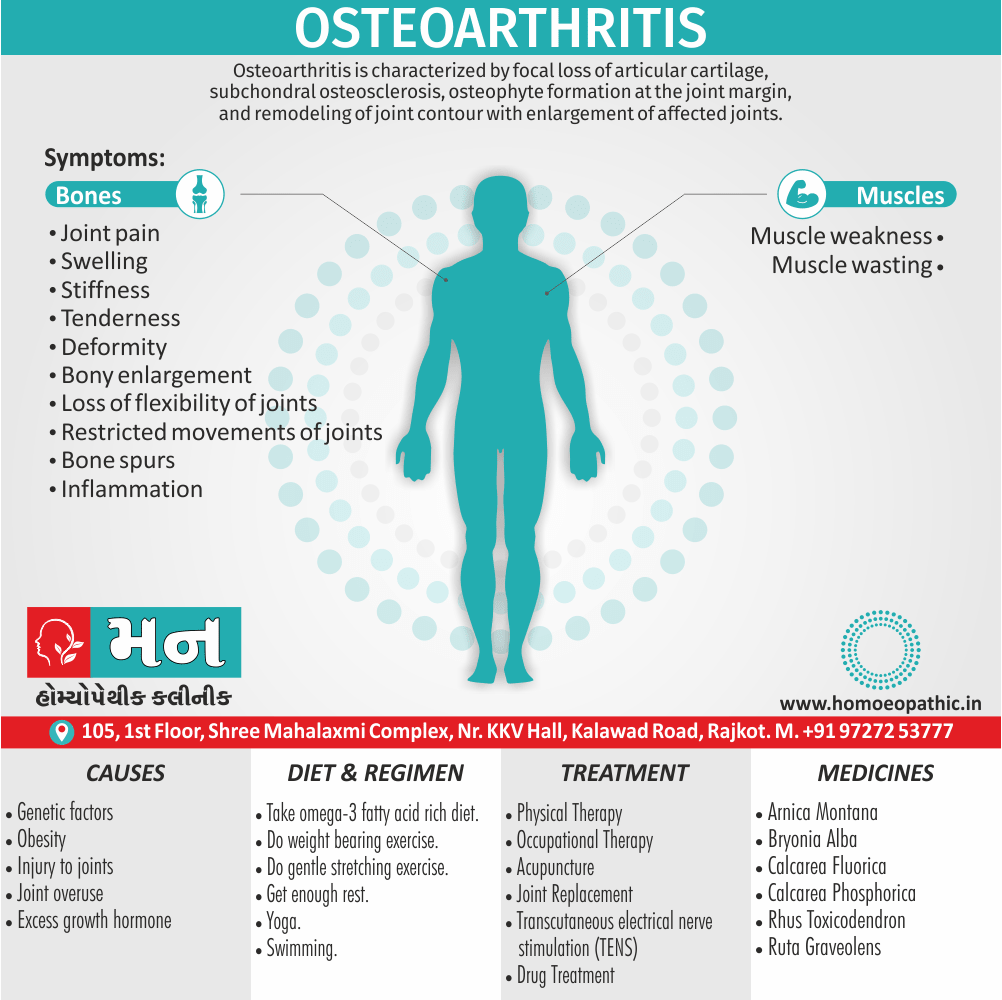
Osteoarthritis (OA) is characterized by focal loss of articular cartilage, subchondral osteosclerosis, osteophyte formation at the joint margin, and remodeling of joint contour with enlargement of affected joints. [1]
Here are some synonyms for osteoarthritis:
- Degenerative joint disease (DJD): This is the most common synonym and emphasizes the breakdown of joint cartilage.
- Osteoarthrosis: This term is less common than osteoarthritis but medically accurate.
- Wear-and-tear arthritis: This informal term describes the gradual breakdown of the joint from use.
Note: It’s generally best to use "osteoarthritis" in most contexts unless you’re specifically referring to the degenerative aspect (DJD) or want a more technical term (osteoarthrosis).
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview:
Osteoarthritis (OA) is the most common form of arthritis, affecting millions worldwide. It occurs when the protective cartilage that cushions the ends of your bones wears down over time.
Here’s a breakdown of OA:
- Cartilage Breakdown: OA is all about the deterioration of cartilage, the smooth, slippery tissue that allows bones to glide over each other in your joints. As cartilage breaks down, bones rub together, causing pain, stiffness, and loss of movement.
- Symptoms: These include joint pain (worsens with activity, improves with rest), stiffness (especially in the morning or after inactivity), limited range of motion, and sometimes swelling. You might also hear or feel a grating sensation in the joint.
- Risk Factors: Age is a big one, as cartilage tends to wear down over time. Other factors include genetics, obesity (puts extra stress on joints), joint injuries, and repetitive use of certain joints.
- Commonly Affected Joints: While OA can occur in any joint, it’s most often seen in the hands, knees, hips, and spine.
- No Cure, But Manageable: There’s no way to reverse the cartilage damage, but treatments focus on managing pain, improving function, and slowing the progression of the disease. This can involve medications, physical therapy, lifestyle changes (like weight loss and exercise), and in some cases, surgery.
Epidemiology
Epidemiology Of Osteoarthritis
The epidemiology of osteoarthritis (OA) in India reflects a substantial and growing burden of the disease.
Key findings from recent studies include:
Prevalence:
- The age-standardized prevalence of OA increased from 4,895 per 100,000 persons in 1990 to 5,313 per 100,000 persons in 2019. (Burden of osteoarthritis in India and its states, 1990-2019: findings from the Global Burden of disease study 2019, 2023) [7]
- An estimated 62.35 million individuals in India had OA in 2019. (POS1425 THE BURDEN OF OSTEOARTHRITIS ACROSS THE STATES OF INDIA, 1990–2019, 2022) [8]
- Knee OA is the most common form, followed by hand OA. (Burden of osteoarthritis in India and its states, 1990-2019: findings from the Global Burden of disease study 2019, 2023)
- Prevalence, incidence, and disease burden are consistently higher in females than males. (Burden of osteoarthritis in India and its states, 1990-2019: findings from the Global Burden of disease study 2019, 2023) [8]
Impact:
- OA was the 20th most common cause of years lived with disability (YLDs) in India in 2019, accounting for 1.48% of all YLDs. (Burden of osteoarthritis in India and its states, 1990-2019: findings from the Global Burden of disease study 2019, 2023) [8] [7]
- Disability-adjusted life years (DALYs) due to OA increased from 0.79 million in 1990 to 2.12 million in 2019. (Burden of osteoarthritis in India and its states, 1990-2019: findings from the Global Burden of disease study 2019, 2023) [7] [8]
Conclusion:
The burden of OA in India is substantial and increasing. Public health interventions targeting modifiable risk factors (obesity, injuries, occupational stress) are crucial to mitigate the current and future impact of OA in the country.
Causes
Causes of Osteoarthritis
There are several factors that increase a person’s chances of developing osteoarthritis.
Heredity i.e.:
- Some people have an inherited defect in one of the genes responsible for making cartilage.
- This causes defective cartilage, which leads to more rapid deterioration of joints.
- People born with joint abnormalities are more likely to develop osteoarthritis, and those born with an abnormality of the spine(such as scoliosis or curvature of the spine) are more likely to develop osteoarthritis of the spine.
Obesity i.e.:
- Obesity increases the risk for osteoarthritis of the knee, hip, and spine.
- Maintaining ideal weight or losing excess weight may help prevent osteoarthritis of these areas or decrease the rate of progression once Osteoarthritis-OA is established.
Injury i.e.:
- Injuries contribute to the development of osteoarthritis.
- For example, athletes who have knee-related injuries may be at higher risk of developing osteoarthritis of the knee.
- In addition, people who have had a severe back injury may predispose to develop osteoarthritis of the spine.
- People who have had a broken bone near a joint are prone to develop osteoarthritis in that joint.
Joint overuse i.e.:
- Overuse of certain joints increases the risk of developing osteoarthritis.
- For example, people in jobs requiring repeated bending of the knee are at increase risk for developing osteoarthritis of the knee.
Other diseases i.e.:
- People with rheumatoid arthritis, the second most common type of arthritis, are more likely to develop osteoarthritis.
- In addition, certain rare conditions, such as iron overload or excess growth hormone, increase the chance of developing Osteoarthritis-OA. [4]
Types
Types Of Osteoarthritis
Osteoarthritis is broadly classified into two main types:
Primary Osteoarthritis:
- This is the most common type, and its exact cause is unknown. It is often attributed to the wear and tear of joints over time, and it typically affects weight-bearing joints like knees, hips, and spine.
Secondary Osteoarthritis:
- This type occurs due to an underlying condition or injury that damages the joint. Some common causes include previous joint injuries, obesity, inflammatory arthritis, and genetic factors. [9]
Types:
Generalised nodal OA:
Characteristics of generalised nodal osteoarthritis i.e.:

Heberden’s Nodes
- Polyarticular finger interphalangeal joint Osteoarthritis (OA)
- Heberden’s (± Bouchard’s) nodes
- Marked female preponderance
- Peak onset in middle age
- Good functional outcome for hands
- Predisposition to Osteoarthritis (OA) at other joints, especially knees
- Strong genetic predisposition
Some patients are asymptomatic whereas others develop pain, stiffness and swelling of one or more PIP joints of the hands from the age of about 40 years onward.
Gradually, these develop posterolateral swellings on each side of the extensor tendon that slowly enlarge and harden to become Heberden’s (DIP) and Bouchard’s (PIP) nodes.
Typically, each joint goes through a phase of episodic symptoms (1–5 years) while the node evolves and OA develops.
Once OA is fully establish, symptoms may subside and hand function often remains good.
Affected joints are enlarge as the result of osteophyte formation and often show characteristic lateral deviation, reflecting the asymmetric focal cartilage loss of Osteoarthritis (OA).
Involvement of the first carpometacarpal joint (CMC) is also common, leading to pain on trying to open bottles and jars and functional impairment.
Clinically, it may detect by the presence of crepitus on joint movement, and squaring of the thumb base.
Generalised nodal OA has a very strong genetic component: the daughter of an affected mother has a 1 in 3 chance of developing nodal OA herself. [1]
Knee OA:
Osteoarthritis Of Knee
Location i.e.:
OA principally targets the patellofemoral and medial tibiofemoral compartments at this site but eventually spreads to affect the whole of the joint.
It may isolate or occur as part of generalised nodal OA.
Most patients, particularly women, have bilateral and symmetrical involvement.
With men, trauma is a more important risk factor and may result in unilateral OA.
Pain i.e.:
The pain is usually localised to the anterior or medial aspect of the knee and upper tibia.
Patellofemoral pain is usually worse going up and down stairs or inclines.
Posterior knee pain suggests the presence of a complicating popliteal cyst (Baker’s cyst).
Prolonged walking, rising from a chair, getting in or out of a car, or bending to put on shoes and socks may be difficult.
Local examination findings may include i.e.:
- A jerky, asymmetric (antalgic) gait with less time weight bearing on the painful side
- A varus, less commonly valgus, and/or fixed flexion deformity
- Joint line and/or periarticular tenderness (secondary anserine bursitis and medial ligament enthesopathy, causing tenderness of the upper medial tibia)
- Weakness and wasting of the quadriceps muscle
- Restricted flexion/extension with coarse crepitus
- Bony swelling around the joint line
Calcium pyrophosphate dihydrate (CPPD) crystal deposition in association with OA is most common at the knee. [1]
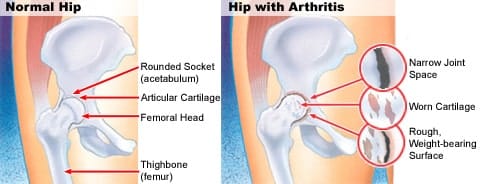
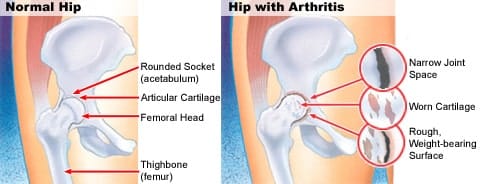
Hip OA:
Location i.e.:
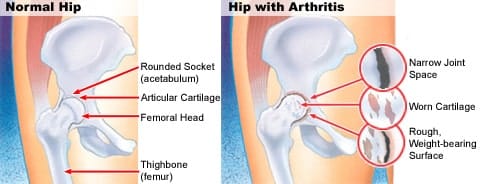
Osteoarthritis Of Hip
Hip OA most commonly targets the superior aspect of the joint.
This is often unilateral at presentation, frequently progresses with superolateral migration of the femoral head, and has a poor prognosis.
The less common central (medial) Osteoarthritis-OA shows more central cartilage loss and is largely confined to women.
It is often bilateral at presentation and may associate with generalised nodal OA.
It has a better prognosis than superior hip OA and progression to axial migration of the femoral head is uncommon.
Pain i.e.:
Hip pain is usually maximal deep in the anterior groin, with variable radiation to the buttock, anterolateral thigh, knee or shin.
Lateral hip pain, worse on lying on that side with tenderness over the greater trochanter, suggests secondary trochanteric bursitis.
Common functional difficulties are the same as for knee Osteoarthritis-OA; in addition, restricted hip abduction in women may cause pain on intercourse.
Examination may reveal i.e.:
- An antalgic gait
- Weakness and wasting of quadriceps and gluteal muscles
- Pain and restriction of internal rotation with the hip flexed the earliest and most sensitive sign of hip OA; other movements may subsequently restricted and painful
- Anterior groin tenderness just lateral to the femoral pulse
- Fixed flexion, external rotation deformity of the hip
- Ipsilateral leg shortening with severe joint attrition and superior femoral migration.
Although obesity is not a major risk factor for development of hip Osteoarthritis-OA, it is associated with more rapid progression.
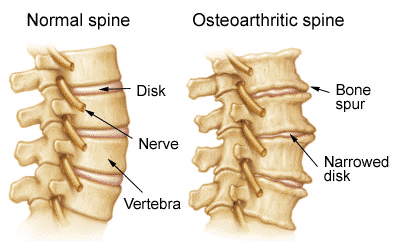
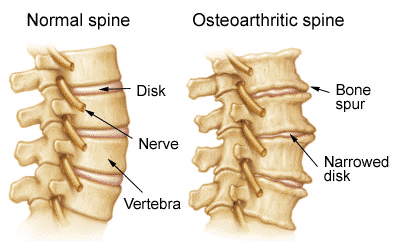
Spine OA:
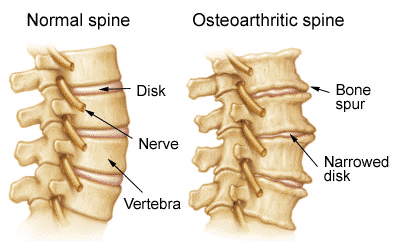
Osteoarthritis Of Spine
- The cervical and lumbar spine are predominantly targeted by OA, then referred to as cervical spondylosis and lumbar spondylosis, respectively.
- Spine OA may occur in isolation or as part of generalised OA.
- The typical presentation is with pain localised to the low back region or the neck, although radiation of pain to the arms, buttocks and legs may also occur due to nerve root compression.
- The pain is typically relieved by rest and worse on movement.
- On physical examination, the range of movement may be limited and loss of lumbar lordosis is typical.
- The straight leg raising test or femoral stretch test may be positive and neurological signs may be seen in the legs where there is complicating spinal stenosis or nerve root compression.
Early-onset OA:
- Unusually, typical symptoms and signs of Osteoarthritis-OA may present before the age of 45.
- In most cases, a single joint is affected and there is a clear history of previous trauma.
- However, specific causes of OA need to be considered in people with early onset disease affecting several joints, especially those not normally targeted by Osteoarthritis-OA, rare causes need to be considered.
- Kashin– Beck disease is a rare form of Osteoarthritis-OA that occurs in children, typically between the ages of 7 and 13, in some regions of China.
- The cause is unknown but suggested predisposing factors are selenium deficiency and contamination of cereals with mycotoxin producing fungi.
Causes of early-onset osteoarthritis:
Monoarticular e.g.:
- Previous trauma
- Localised instability
Pauciarticular or polyarticular e.g.:
- Juvenile idiopathic arthritis
- Metabolic or endocrine disease: for example Haemochromatosis, Ochronosis, Acromegaly
- Spondyloepiphyseal dysplasia
- Late avascular necrosis
- Neuropathic joint
- Kashin–Beck disease [1]
Risk Factors
Risk factors Of Osteoarthritis
Osteoarthritis is a multifactorial disease with several factors increasing an individual’s susceptibility. These include:
Age
- The risk of osteoarthritis increases significantly with age, primarily due to the natural wear and tear of joints over time.
Sex:
- Women are more likely to develop osteoarthritis than men, especially after menopause.
Obesity:
- Excess weight puts additional stress on weight-bearing joints like knees and hips, increasing the risk of osteoarthritis.
Joint Injury:
- Previous injuries to a joint, such as fractures or ligament tears, can increase the risk of developing osteoarthritis in that joint.
Genetics:
- A family history of osteoarthritis can increase an individual’s susceptibility to the condition.
Occupation:
Jobs that involve repetitive movements or heavy lifting can put extra stress on joints, raising the risk of osteoarthritis.
Other Factors:
- Certain medical conditions like rheumatoid arthritis, diabetes, and metabolic disorders can also contribute to the development of osteoarthritis. [10]
Pathogenesis
Pathogenesis of Osteoarthritis
Osteoarthritis is a complex disease characterized by the progressive degradation of articular cartilage, the smooth tissue covering the ends of bones in a joint. This breakdown results in pain, stiffness, and reduced joint function.
Key Processes in Osteoarthritis Pathogenesis:
Cartilage Degradation:
- Chondrocytes (cartilage cells) undergo changes in their gene expression and metabolic activity, leading to an imbalance between cartilage matrix synthesis and degradation.
- Enzymes like matrix metalloproteinases (MMPs) and aggrecanases break down cartilage components like collagen and proteoglycans.
- Loss of proteoglycans reduces the cartilage’s ability to absorb shock and distribute load, making it more susceptible to further damage.
Subchondral Bone Changes:
- The bone beneath the cartilage thickens and becomes sclerotic (hardened).
- Microfractures and cysts may form in the subchondral bone.
- In advanced stages, bone spurs (osteophytes) can develop at the joint margins.
Synovial Inflammation:
- The synovium (lining of the joint capsule) can become inflamed, leading to the release of inflammatory cytokines and enzymes that further contribute to cartilage destruction.
Other Factors:
- Oxidative stress, mechanical loading, and genetic predisposition also play roles in osteoarthritis pathogenesis. [11]
Pathophysiology
Pathophysiology Of Osteoarthritis
Key pathophysiological processes:
Cartilage Degradation:
- The primary event in OA is the breakdown of articular cartilage, a smooth, resilient tissue that covers the ends of bones in a joint, facilitating frictionless movement.
- This degradation is initiated by a disruption of the balance between anabolic (synthesis) and catabolic (breakdown) processes within the cartilage matrix.
- Chondrocytes, the cells responsible for maintaining cartilage, become activated and release enzymes like matrix metalloproteinases (MMPs) and aggrecanases, which degrade collagen and proteoglycans, the main structural components of cartilage.
- Loss of proteoglycans reduces the cartilage’s ability to retain water and resist compressive forces, leading to its progressive thinning and fissuring.
Subchondral Bone Changes:
- As the cartilage degenerates, the underlying subchondral bone becomes exposed and undergoes remodeling.
- Initially, the bone thickens and becomes sclerotic (hardened) in an attempt to compensate for the loss of cartilage support.
- However, this process can lead to the formation of microfractures and subchondral cysts, further compromising joint integrity.
- Osteophytes, or bone spurs, may also develop at the joint margins, contributing to pain and limited range of motion.
Synovial Inflammation:
- The synovium, a thin membrane lining the joint capsule, can become inflamed in OA, releasing inflammatory mediators and enzymes that exacerbate cartilage destruction.
- Synovitis can also lead to the formation of a pannus, an abnormal layer of tissue that can invade and erode cartilage.
Other Contributing Factors:
- Oxidative stress, mechanical overload, and genetic predisposition are also thought to play roles in the pathophysiology of OA.
- Aging, obesity, and joint injury are known risk factors that can accelerate cartilage degeneration and contribute to the development of OA. [12]
Clinical Features
Clinical Features of Osteoarthritis
Osteoarthritis is a prevalent joint disease characterized by a range of symptoms and physical findings. The typical clinical features include:
Pain: This is the most common symptom, often described as a deep, aching pain in the affected joint. Pain usually worsens with activity and improves with rest.
Stiffness: Joint stiffness is commonly experienced in the morning or after periods of inactivity. It typically resolves within 30 minutes of movement.
Reduced Range of Motion: As the disease progresses, joint movement becomes limited, affecting activities of daily living.
Crepitus: A grating or crackling sensation may be felt or heard when moving the affected joint.
Joint Enlargement: The joint may appear swollen or enlarged due to bone spurs (osteophytes) or thickening of the joint capsule.
Tenderness: The joint may be tender to touch, especially around the bony prominences.
Muscle Weakness: The muscles surrounding the affected joint may become weak due to disuse and pain. [13]
Sign & Symptoms
Sign & Symptoms Of Osteoarthritis
Pain:
- Insidious onset over months or years
- Either Variable or intermittent over time (‘good days, bad days’)
- Mainly related to movement and weight-bearing, relieve especially by rest
- Only brief (< 15 mins) morning stiffness also brief (< 5 mins) ‘gelling’ after rest
- Usually only one or a few joints painful
Clinical signs in Osteoarthritis (OA):
- Restricted movement due to capsular thickening, or blocking by osteophyte
- Furthermore; Palpable, sometimes audible, coarse crepitus due to rough articular surfaces
- Bony swelling around joint margins
- Deformity, usually without instability
- Either Joint-line or periarticular tenderness
- Muscle weakness also wasting
- Synovitis mild or absent
Clinical Examination
Osteoarthritis- Clinical Examination
It typically includes:
Inspection:
- Observe for joint swelling, deformity, erythema (redness), or muscle wasting.
- Look for signs of inflammation, such as warmth or redness around the joint.
- Assess the patient’s gait and posture for any abnormalities related to joint pain or stiffness.
Palpation:
- Gently palpate the joint for tenderness, warmth, and crepitus (a grating or crackling sensation).
- Feel for bony enlargements or osteophytes (bone spurs) at the joint margins.
- Assess the range of motion of the joint, both active (patient-initiated) and passive (examiner-assisted).
- Note any limitations in movement or pain during the examination.
Special Tests:
- Specific tests may be performed depending on the joint involved. For example:
- Knee: McMurray’s test, patellar grind test, varus/valgus stress tests.
- Hip: FABER test, Trendelenburg test.
- Hand: Heberden’s nodes, Bouchard’s nodes.
- Specific tests may be performed depending on the joint involved. For example:
Neurological Examination:
- Assess for any neurological deficits, such as muscle weakness, sensory loss, or reflex changes, that may indicate nerve compression or other complications.
Functional Assessment:
- Evaluate the patient’s ability to perform activities of daily living, such as walking, climbing stairs, dressing, and bathing.
- Use validated questionnaires or scales to assess pain severity, functional limitations, and quality of life. [14]
Diagnosis
Diagnosis Of Osteoarthritis
There is no blood test for the diagnosis of osteoarthritis.
Blood tests are performed to exclude diseases that can cause secondary osteoarthritis, as well as to exclude other arthritis conditions that can mimic osteoarthritis.
X-rays:
- X-rays of the affected joints can use to diagnose osteoarthritis.
- The common X-ray findings of Osteoarthritis-OA include loss of joint cartilage, narrowing of the joint space between adjacent bones, and bone spur formation.
- Simple X-ray testing can also very helpful to exclude other causes of pain in a particular joint as well as assisting the decision-making as to when surgical intervention might consider.
Arthrocentesis:
- Arthrocentesis is a procedure to remove joint fluid that is often performed in a health care professional’s office.
- During arthrocentesis, a sterile needle is use to remove joint fluid for analysis.
- Joint fluid analysis is useful in excluding gout, infection, and other causes of arthritis.
- Removal of joint fluid and injection of corticosteroids into the joints during arthrocentesis can help relieve pain, swelling, and inflammation.
Arthroscopy:
- Arthroscopy is a surgical technique whereby a doctor inserts a viewing tube into the joint space.
- Abnormalities of and damage to the cartilage and ligaments can detect and sometimes repair through the arthroscope.
- If successful, patients can recover from the arthroscopic surgery much more quickly than from open joint surgery.
Finally, a careful analysis of the location, duration, and character of the joint symptoms and the appearance of the joints helps the doctor in diagnosing osteoarthritis.
Bony enlargement of the joints from spur formations is characteristic of osteoarthritis.
Therefore, the presence of Heberden’s nodes, Bouchard’s nodes, and bunions of the feet can indicate to the doctor a diagnosis of osteoarthritis. [5]
Differential Diagnosis
Differential Diagnosis of Osteoarthritis
Osteoarthritis can present with symptoms similar to other musculoskeletal conditions, making a thorough differential diagnosis essential. Some common differential diagnoses include:
Rheumatoid Arthritis:
- Inflammatory arthritis affecting multiple joints symmetrically.
- Morning stiffness lasting more than 30 minutes.
- Systemic symptoms like fatigue, fever, and weight loss may be present.
Gout:
- Acute inflammatory arthritis caused by uric acid crystal deposition in joints.
- Severe pain, redness, and swelling in a single joint (often the big toe).
Pseudogout:
- Acute inflammatory arthritis caused by calcium pyrophosphate crystal deposition.
- Can mimic osteoarthritis or rheumatoid arthritis.
Infectious Arthritis:
- Joint infection caused by bacteria, viruses, or fungi.
- Acute onset of pain, swelling, redness, and warmth in a single joint.
- Fever and systemic symptoms may be present.
Avascular Necrosis:
- Bone death due to insufficient blood supply.
- Can cause pain and limited range of motion in affected joints (often the hip or shoulder).
Trauma:
- Fractures, sprains, or strains can cause joint pain and swelling.
- History of injury is usually present.
Fibromyalgia:
- Chronic pain syndrome characterized by widespread musculoskeletal pain, fatigue, and sleep disturbances.
Polymyalgia Rheumatica:
- Inflammatory condition causing pain and stiffness in the shoulders and hips.
- Usually affects older adults. [15]
Complications
Complications of Osteoarthritis
Osteoarthritis, while primarily a degenerative joint disease, can lead to various complications that significantly impact a patient’s quality of life. These complications include:
Chronic Pain: Persistent joint pain can lead to sleep disturbances, depression, anxiety, and reduced overall well-being.
Joint Deformity: As the disease progresses, joint damage can lead to deformities, particularly in the hands, knees, and hips. This can affect mobility and function.
Loss of Function: Reduced range of motion and joint stiffness can limit activities of daily living, making it difficult to perform routine tasks.
Muscle Weakness: Pain and limited joint movement can lead to muscle atrophy (wasting) and weakness, further impacting mobility.
Joint Instability: In severe cases, joint damage can lead to instability, increasing the risk of falls and fractures.
Nerve Compression: Osteophytes (bone spurs) can compress nearby nerves, causing pain, numbness, or tingling.
Depression and Anxiety: Chronic pain and disability can lead to psychological distress, including depression and anxiety.
Sleep Disturbances: Pain and discomfort can disrupt sleep, leading to fatigue and further exacerbating pain.
Reduced Quality of Life: The cumulative impact of pain, disability, and psychological distress can significantly reduce a person’s quality of life. [16]
Investigations
Investigations of Osteoarthritis
The diagnosis of osteoarthritis primarily relies on clinical assessment, but various investigations can aid in confirming the diagnosis, assessing disease severity, and excluding other conditions. These include:
Imaging Studies:
- X-rays: The most common imaging modality used to visualize joint changes associated with osteoarthritis. X-rays can reveal joint space narrowing, osteophytes (bone spurs), subchondral sclerosis (increased bone density), and subchondral cysts.
- MRI: Provides detailed images of soft tissues, including cartilage, ligaments, and tendons. It can detect early cartilage damage and other abnormalities not visible on X-rays.
- CT Scan: Can be helpful in assessing complex joint anatomy and evaluating the extent of bone damage in advanced cases.
Laboratory Tests:
- Blood Tests: Generally not specific for osteoarthritis but can help rule out other conditions like rheumatoid arthritis or gout.
- Erythrocyte Sedimentation Rate (ESR) and C-reactive protein (CRP): May be elevated in inflammatory arthritis but are usually normal in osteoarthritis.
- Rheumatoid Factor (RF) and Anti-CCP Antibodies: Negative in osteoarthritis but positive in rheumatoid arthritis.
- Uric Acid: Elevated in gout.
Joint Aspiration (Arthrocentesis):
- Involves withdrawing fluid from the affected joint for analysis.
- Can help rule out infection or inflammatory arthritis.
- Synovial fluid analysis in osteoarthritis typically shows a low white blood cell count and the absence of crystals. [17]
Treatment
Management of Osteoarthritis
OA treatment is centered upon symptom management.
The type of treatment that will help you the most will largely be determined by the severity of your symptoms and their location.
Often, lifestyle changes, over-the-counter (OTC) medication, and home remedies will be enough to provide you with relief from pain, stiffness, and swelling.
At-home treatments and lifestyle changes for Osteoarthritis-OA include:
Exercise i.e.:
- Physical activity strengthens the muscles around your joints and may help relieve stiffness.
- Aim for at least 20 to 30 minutes of physical movement, at least every other day.
- Choose gentle, low-impact activities, such as walking or swimming.
- Tai chi and yoga can also improve joint flexibility and help with pain management.
- Gentle stretching exercises can be very helpful for people with Osteoarthritis-OA, especially if you have stiffness or pain in your knees, hips, or back.
- Stretching can help improve mobility and range of motion.
Weight loss i.e.:
- Being higher-weight person can put strain on your joints and cause pain.
- Shedding excess pounds helps relieve this pressure and reduces pain.
- A healthy weight can also lower your risk of other health problems, such as diabetes and heart disease.
Adequate sleep i.e.:
- Resting your muscles can reduce swelling and inflammation.
- Be kind to yourself and don’t overdo it.
- Getting enough sleep at night can also help you to manage pain more effectively.
Heat and cold therapy i.e.:
- You can experiment with heat or cold therapy to relieve muscle pain and stiffness.
- Apply a cold or hot compress to sore joints for 15 to 20 minutes several times a day.
These practices can help take the edge off of your symptoms and improve your quality of life.
Medications of Osteoarthritis-OA:
There are a number of different types of Osteoarthritis-OA medications that can help provide relief from pain or swelling.
Oral analgesics i.e.:
- Tylenol (acetaminophen) and other pain relievers reduce pain but not swelling.
Topical analgesics i.e.:
- These OTC products are available as creams, gels, and patches.
- They help to numb the joint area and can provide pain relief, especially for mild arthritis pain.
NSAIDs (nonsteroidal anti-inflammatory drugs) i.e.:
- NSAIDs such as Advil (ibuprofen) and Aleve (naproxen) reduce swelling as well as pain.
Cymbalta i.e.:
- Your doctor may prescribe the antidepressant Cymbalta (duloxetine) for you off-label to help provide osteoarthritis(OA) pain relief.
Corticosteroids i.e.:
- These prescription medications are available in oral form.
- They may also be given by injection directly into a joint.
Natural treatments:
Alternative treatments and supplements may help to relieve symptoms such as inflammation and joint pain.
Some supplements or herbs that may help include:
- Fish oil
- Green tea
- Ginger
- Glucosamine
Other alternative treatment options include:
- Acupuncture
- Physical therapy
- Massage therapy
Other remedies can range from taking Epsom salt baths to using hot or cold compresses.
Diet:
There’s no downside to eating healthy, but if you have Osteoarthritis-OA, diet and nutrition are especially important.
Some types of Osteoarthritis-OA, such as osteoarthritis of the knee, respond positively to a diet high in flavonoids, which are nutrients found in fruits and vegetables.
Also, the antioxidants found in many fruits and vegetables may also help combat the free radicals produced by inflammation. Free radicals are molecules that can cause cell damage.
A high-quality diet may help provide relief from osteoarthritis (OA) symptoms by reducing inflammation and swelling.
Eating foods high in the following can be highly beneficial:
- Vitamin C
- Vitamin D
- Beta-carotene
- Omega-3 fatty acids
Increasing your intake of foods with anti-inflammatory properties will help, too. [3]
Prevention
Prevention of Osteoarthritis
While osteoarthritis cannot be completely prevented, there are several strategies to reduce its risk and slow its progression:
Weight Management:
- Maintaining a healthy weight reduces stress on weight-bearing joints, decreasing the risk of developing or worsening osteoarthritis.
- Even a small weight loss can have a significant impact on joint health.
Exercise:
- Regular physical activity helps strengthen muscles surrounding joints, improving joint stability and reducing pain.
- Low-impact exercises like swimming, cycling, and walking are particularly beneficial.
- Avoid high-impact activities or repetitive motions that put excessive stress on joints.
Injury Prevention:
- Take precautions to prevent joint injuries during sports or physical activities.
- Use proper protective gear and equipment.
- Warm up before exercise and cool down afterward.
- Listen to your body and avoid overexertion.
Proper Posture and Body Mechanics:
- Maintain good posture to reduce stress on joints.
- Use proper body mechanics when lifting heavy objects or performing repetitive tasks.
- Avoid prolonged sitting or standing.
Diet:
- A balanced diet rich in fruits, vegetables, and whole grains can help maintain a healthy weight and provide essential nutrients for joint health.
- Some studies suggest that foods rich in omega-3 fatty acids and antioxidants may have a protective effect against osteoarthritis.
Early Intervention:
- Seek medical attention if you experience persistent joint pain or stiffness.
- Early diagnosis and treatment can help slow disease progression and manage symptoms. [12]
Homeopathic Treatment
Homeopathic Treatment of Oesteoarthris
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’? The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition. The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for OA:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor. So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
Bryonia Alba:
- Excellent remedy which is useful in treatment of osteoarthritis, pain with inflammation which is aggravated by movement on the other hand relieved by moderate pressure and rest.
- There is inflammation of joints which are hot also swollen.
Rhus Toxicodendron:
- Recurring attacks due to getting chilled.
- Rheumatism caused by damp weather and worse in damp climate; there is restlessness and the pains are worse on first motion, better by continued motion.
Kali Carb:
- Pains stitching, stabbing and burning character relieved temporarily by cold application and not by rest or motion.
- The patient shrieks on account of pain.
- Backache accompanied by great weakness.
Arnica:
- Generally, Chronic arthritis with a feeling of bruised soreness can indicate a need for this remedy.
- Pain is worse specifically from touch, and may occur in joints that were injured in the past.
Ruta graveolens:
- Arthritis with a feeling of great stiffness and lameness, worse from cold and damp, and worse from exertion often is relieved by this remedy.
- Tendons and the capsules of the joints may be affected.
- Besides this; Arthritis may have developed after overuse, from repeated wear and tear.
Kalmia latifolia:
- Intense arthritic pain that appears quite suddenly may indicate this medicine especially when the problems start in higher joints and extend to lower ones.
- Pain and inflammation often start in the shoulder, moving to the elbow, wrist and hand.
- The knees are also frequently affected.
- Discomfort is worse from motion and often worse at night.
Apis mellifica:
- This remedy can be helpful in acute conditions with redness, tenderness, also swelling.
- Joints feel hot and have stinging pain.
- The hands and knees are often affected.
- Warmth can aggravate the symptoms and cool applications bring relief.
Calcarea fluorica:
- This medicine is often indicated for arthritic pains that are improved especially by heat and motion.
- Joints become enlarged also hard, and nodosities or bone spurs may develop.
- Arthritis after chronic injury to joints often responds to Calcarea fluorica.
Calcarea carbonica:
- This remedy is often useful for arthritis in a person who is flabby or higher-weight person , and easily tired by exertion.
- Inflammation and soreness are worse from cold and dampness, and weakness or cramping in the extremities are often seen.
- Problems often focus on the knees when Calcarea is needed.
Sticta Pulmonaria:
- Rheumatism of right shoulder blade or joint, wrist joint, ankle joint and knee joint.
- It also reduces fluid in the joints. [6]
Diet & Regimen
Diet:
Weight Management: Maintaining a healthy weight reduces stress on weight-bearing joints. Focus on a balanced diet with portion control and calorie restriction if necessary.
Anti-Inflammatory Foods: Include plenty of fruits, vegetables, and whole grains rich in antioxidants and phytochemicals that combat inflammation.
Omega-3 Fatty Acids: Found in fatty fish, flaxseeds, and walnuts, these healthy fats may have anti-inflammatory and cartilage-protective properties.
Vitamin D and Calcium: Ensure adequate intake to maintain bone health. Sun exposure, fortified foods, and supplements can help.
Limit Processed Foods: Minimize intake of sugary drinks, refined carbohydrates, and processed meats, which may contribute to inflammation.
Regimen:
Exercise: Engage in regular low-impact exercises like walking, swimming, and cycling to improve joint flexibility, strength, and range of motion.
Physical Therapy: Consult a physical therapist for personalized exercises and techniques to improve joint function and reduce pain.
Heat and Cold Therapy: Apply heat to relieve stiffness and cold to reduce inflammation and pain.
Assistive Devices: Use canes, walkers, or braces to support joints and improve mobility.
Weight Loss: If over-weight, weight loss can significantly reduce joint stress and pain.
Stress Management: Practice stress-reducing techniques like meditation and yoga, as stress can worsen pain perception. [18]
Do’s and Don'ts
Do’s:
- Stay Active: Engage in regular low-impact exercise like walking, swimming, or cycling to improve joint flexibility, strength, and range of motion.
- Maintain a Healthy Weight: Losing even a small amount of weight can significantly reduce stress on weight-bearing joints like knees and hips.
- Use Heat and Cold Therapy: Apply heat to relieve stiffness and cold to reduce inflammation and pain.
- Practice Good Posture: Maintain proper posture to reduce stress on joints and prevent further damage.
- Use Assistive Devices: Utilize canes, walkers, or braces to support joints and improve mobility if needed.
- Get Adequate Rest: Balance activity with rest to allow your joints to recover.
- Eat a Healthy Diet: Focus on a balanced diet rich in fruits, vegetables, and whole grains to support joint health and maintain a healthy weight.
- Consult a Healthcare Professional: Regularly see your doctor or a rheumatologist for check-ups and to discuss any concerns about your condition.
- Consider Physical Therapy: A physical therapist can teach you exercises and techniques to improve joint function and reduce pain.
- Manage Stress: Practice relaxation techniques like meditation and yoga, as stress can worsen pain.
Don’ts:
- Overexert Yourself: Avoid high-impact activities or repetitive motions that can put excessive stress on your joints.
- Ignore Pain: Persistent or worsening pain should be evaluated by a healthcare professional.
- Neglect Your Mental Health: Chronic pain can lead to depression and anxiety. Seek help if needed.
- Smoke: Smoking can worsen osteoarthritis and hinder its treatment.
- Overuse Painkillers: Relying solely on medication for pain relief can mask underlying problems and have side effects.
- Skip Doctor’s Appointments: Regular check-ups are important to monitor your condition and adjust treatment as needed.
- Give Up: While osteoarthritis can be challenging, staying positive and proactive in managing your condition can improve your quality of life.
Terminology
Terminology
- Osteoarthritis (OA): It is the most common form of arthritis, characterized by the breakdown of cartilage in joints, leading to pain, stiffness, and reduced mobility.
- Cartilage: A smooth, white tissue that covers the ends of bones where they meet to form a joint. It enables bones to glide over each other, reducing friction and absorbing shock during movement.
- Chondrocytes: The cells within cartilage responsible for producing and maintaining the cartilage matrix.
- Subchondral Bone: The layer of bone just beneath the cartilage. It becomes thickened and hardened in osteoarthritis.
- Synovium: The thin membrane lining the joint capsule that produces synovial fluid, which lubricates the joint. It can become inflamed in osteoarthritis.
- Osteophytes: Bony outgrowths or spurs that form around the margins of affected joints in osteoarthritis.
- Joint Space Narrowing: The reduction of space between the bones in a joint due to cartilage loss, visible on X-rays.
- Crepitus: A grating or crackling sensation or sound produced by the movement of a joint affected by osteoarthritis.
- Inflammation: The body’s response to injury or irritation, characterized by redness, swelling, warmth, and pain. In osteoarthritis, low-grade inflammation can contribute to disease progression.
- Pain: An unpleasant sensory and emotional experience associated with actual or potential tissue damage. It’s the primary symptom of osteoarthritis.
- Stiffness: A feeling of restricted movement or difficulty in moving a joint, often experienced in the morning or after periods of inactivity in osteoarthritis.
- Disability: Impairment in performing activities of daily living due to a health condition. Osteoarthritis can cause significant disability, affecting mobility and quality of life.
Commonly Used Homeopathic Remedies for Osteoarthritis:
- Rhus toxicodendron: Often recommended for joint pain and stiffness that worsen with initial movement but improve with continued motion, particularly in damp or cold weather.
- Bryonia: Indicated for pain aggravated by movement and relieved by rest, along with swelling and inflammation.
- Arnica: Considered for pain that feels like a bruise, especially after injury or overuse.
- Calcarea carbonica: May be used for individuals who are over-weight, chilly, and experience joint stiffness and cracking.
- Ledum: Often suggested for pain that feels cold and is relieved by cold applications.
References
References
- Davidson’s Principles and Practice of Medicine (22nd edition) Ch. 25
- https://www.mayoclinic.org/diseases-conditions/osteoarthritis/symptoms-causes/syc-20351925
- https://www.healthline.com/health/osteoarthritis#osteoarthritis-symptoms
- https://www.webmd.com/osteoarthritis/guide/osteoarthritis-basics#1
- https://www.medicinenet.com/osteoarthritis/article.htm#how_do_health_care_professionals_diagnose_osteoarthritis
- http://homeopathyclinic.co.in/10-best-homeopathic-medicines-treatment-osteoarthritis/
- Burden of osteoarthritis in India and its states, 1990-2019: findings from the Global Burden of disease study 2019, 2023
- POS1425 THE BURDEN OF OSTEOARTHRITIS ACROSS THE STATES OF INDIA, 1990–2019, 2022
Book Title: Kelley’s Textbook of Rheumatology, Edition: 11th Edition, Writer(s): Gary S. Firestein, Ralph C. Budd, Sherine E. Gabriel, Iain B. McInnes, James R. O’Dell
Year of Publication: 2023
Publisher: ElsevierBook Title: Harrison’s Principles of Internal Medicine Edition: 21st Edition, Writer(s): Dennis L. Kasper, Anthony S. Fauci, Stephen L. Hauser, Dan L. Longo, J. Larry Jameson, Joseph Loscalzo, Year of Publication: 2022, Publisher: McGraw-Hill Education
Book , Title: Robbins & Cotran Pathologic Basis of Disease, Edition: 10th Edition, Writer(s): Vinay Kumar, Abul K. Abbas, Jon C. Aster, Year of Publication: 2021, Publisher: Elsevier
- Rheumatology (Sixth Edition) by Marc C. Hochberg, Alan J. Silman, Josef S. Smolen, Michael E. Weinblatt, Michael H. Weisman, 2015 Published by Mosby (an imprint of Elsevier)
- Kumar and Clark’s Clinical Medicine(10th Edition)., by Parveen Kumar, Michael L. Clark (2021, Elsevier)
- Oxford Textbook of Rheumatology (4th Edition) by Peter Maddison, Will Dixon, Ravinder N. Maini, Paul Emery (2013, Oxford University Press)
- Rheumatology Secrets (Sixth Edition), by Sterling G. West (2015, Elsevier)
- Goldman-Cecil Medicine (26th Edition), by Lee Goldman, Andrew I. Schafer (2020, Elsevier)
- Davidson’s Principles and Practice of Medicine (24th Edition), by Brian R. Walker, Nicki R. Colledge, Stuart H. Ralston, Ian D. Penman (2022, Elsevier)
- The Duke Diet and Fitness Center Gluten-Free Cookbook (1st Edition) by Meggan Houlihan, 2014 Published by Grand Central Life & Style
Also Search As
Types Of Osteoarthritis
Osteoarthritis is broadly classified into two main types:
Primary Osteoarthritis:
- This is the most common type, and its exact cause is unknown. It is often attributed to the wear and tear of joints over time, and it typically affects weight-bearing joints like knees, hips, and spine.
Secondary Osteoarthritis:
- This type occurs due to an underlying condition or injury that damages the joint. Some common causes include previous joint injuries, obesity, inflammatory arthritis, and genetic factors. [9]
Types:
Generalised nodal OA:
Characteristics of generalised nodal osteoarthritis i.e.:

Heberden’s Nodes
- Polyarticular finger interphalangeal joint Osteoarthritis (OA)
- Heberden’s (± Bouchard’s) nodes
- Marked female preponderance
- Peak onset in middle age
- Good functional outcome for hands
- Predisposition to Osteoarthritis (OA) at other joints, especially knees
- Strong genetic predisposition
Some patients are asymptomatic whereas others develop pain, stiffness and swelling of one or more PIP joints of the hands from the age of about 40 years onward.
Gradually, these develop posterolateral swellings on each side of the extensor tendon that slowly enlarge and harden to become Heberden’s (DIP) and Bouchard’s (PIP) nodes.
Typically, each joint goes through a phase of episodic symptoms (1–5 years) while the node evolves and OA develops.
Once OA is fully establish, symptoms may subside and hand function often remains good.
Affected joints are enlarge as the result of osteophyte formation and often show characteristic lateral deviation, reflecting the asymmetric focal cartilage loss of Osteoarthritis (OA).
Involvement of the first carpometacarpal joint (CMC) is also common, leading to pain on trying to open bottles and jars and functional impairment.
Clinically, it may detect by the presence of crepitus on joint movement, and squaring of the thumb base.
Generalised nodal OA has a very strong genetic component: the daughter of an affected mother has a 1 in 3 chance of developing nodal OA herself. [1]
Knee OA:
Osteoarthritis Of Knee
Location i.e.:
OA principally targets the patellofemoral and medial tibiofemoral compartments at this site but eventually spreads to affect the whole of the joint.
It may isolate or occur as part of generalised nodal OA.
Most patients, particularly women, have bilateral and symmetrical involvement.
With men, trauma is a more important risk factor and may result in unilateral OA.
Pain i.e.:
The pain is usually localised to the anterior or medial aspect of the knee and upper tibia.
Patellofemoral pain is usually worse going up and down stairs or inclines.
Posterior knee pain suggests the presence of a complicating popliteal cyst (Baker’s cyst).
Prolonged walking, rising from a chair, getting in or out of a car, or bending to put on shoes and socks may be difficult.
Local examination findings may include i.e.:
- A jerky, asymmetric (antalgic) gait with less time weight bearing on the painful side
- A varus, less commonly valgus, and/or fixed flexion deformity
- Joint line and/or periarticular tenderness (secondary anserine bursitis and medial ligament enthesopathy, causing tenderness of the upper medial tibia)
- Weakness and wasting of the quadriceps muscle
- Restricted flexion/extension with coarse crepitus
- Bony swelling around the joint line
Calcium pyrophosphate dihydrate (CPPD) crystal deposition in association with OA is most common at the knee. [1]
Hip OA:
Location i.e.:
Osteoarthritis Of Hip
Hip OA most commonly targets the superior aspect of the joint.
This is often unilateral at presentation, frequently progresses with superolateral migration of the femoral head, and has a poor prognosis.
The less common central (medial) Osteoarthritis-OA shows more central cartilage loss and is largely confined to women.
It is often bilateral at presentation and may associate with generalised nodal OA.
It has a better prognosis than superior hip OA and progression to axial migration of the femoral head is uncommon.
Pain i.e.:
Hip pain is usually maximal deep in the anterior groin, with variable radiation to the buttock, anterolateral thigh, knee or shin.
Lateral hip pain, worse on lying on that side with tenderness over the greater trochanter, suggests secondary trochanteric bursitis.
Common functional difficulties are the same as for knee Osteoarthritis-OA; in addition, restricted hip abduction in women may cause pain on intercourse.
Examination may reveal i.e.:
- An antalgic gait
- Weakness and wasting of quadriceps and gluteal muscles
- Pain and restriction of internal rotation with the hip flexed the earliest and most sensitive sign of hip OA; other movements may subsequently restricted and painful
- Anterior groin tenderness just lateral to the femoral pulse
- Fixed flexion, external rotation deformity of the hip
- Ipsilateral leg shortening with severe joint attrition and superior femoral migration.
Although obesity is not a major risk factor for development of hip Osteoarthritis-OA, it is associated with more rapid progression.
Spine OA:
Osteoarthritis Of Spine
- The cervical and lumbar spine are predominantly targeted by OA, then referred to as cervical spondylosis and lumbar spondylosis, respectively.
- Spine OA may occur in isolation or as part of generalised OA.
- The typical presentation is with pain localised to the low back region or the neck, although radiation of pain to the arms, buttocks and legs may also occur due to nerve root compression.
- The pain is typically relieved by rest and worse on movement.
- On physical examination, the range of movement may be limited and loss of lumbar lordosis is typical.
- The straight leg raising test or femoral stretch test may be positive and neurological signs may be seen in the legs where there is complicating spinal stenosis or nerve root compression.
Early-onset OA:
- Unusually, typical symptoms and signs of Osteoarthritis-OA may present before the age of 45.
- In most cases, a single joint is affected and there is a clear history of previous trauma.
- However, specific causes of OA need to be considered in people with early onset disease affecting several joints, especially those not normally targeted by Osteoarthritis-OA, rare causes need to be considered.
- Kashin– Beck disease is a rare form of Osteoarthritis-OA that occurs in children, typically between the ages of 7 and 13, in some regions of China.
- The cause is unknown but suggested predisposing factors are selenium deficiency and contamination of cereals with mycotoxin producing fungi.
Causes of early-onset osteoarthritis:
Monoarticular e.g.:
- Previous trauma
- Localised instability
Pauciarticular or polyarticular e.g.:
- Juvenile idiopathic arthritis
- Metabolic or endocrine disease: for example Haemochromatosis, Ochronosis, Acromegaly
- Spondyloepiphyseal dysplasia
- Late avascular necrosis
- Neuropathic joint
- Kashin–Beck disease [1]
Types Of Osteoarthritis
Osteoarthritis is broadly classified into two main types:
Primary Osteoarthritis:
- This is the most common type, and its exact cause is unknown. It is often attributed to the wear and tear of joints over time, and it typically affects weight-bearing joints like knees, hips, and spine.
Secondary Osteoarthritis:
- This type occurs due to an underlying condition or injury that damages the joint. Some common causes include previous joint injuries, obesity, inflammatory arthritis, and genetic factors. [9]
Types:
Generalised nodal OA:
Characteristics of generalised nodal osteoarthritis i.e.:

Heberden’s Nodes
- Polyarticular finger interphalangeal joint Osteoarthritis (OA)
- Heberden’s (± Bouchard’s) nodes
- Marked female preponderance
- Peak onset in middle age
- Good functional outcome for hands
- Predisposition to Osteoarthritis (OA) at other joints, especially knees
- Strong genetic predisposition
Some patients are asymptomatic whereas others develop pain, stiffness and swelling of one or more PIP joints of the hands from the age of about 40 years onward.
Gradually, these develop posterolateral swellings on each side of the extensor tendon that slowly enlarge and harden to become Heberden’s (DIP) and Bouchard’s (PIP) nodes.
Typically, each joint goes through a phase of episodic symptoms (1–5 years) while the node evolves and OA develops.
Once OA is fully establish, symptoms may subside and hand function often remains good.
Affected joints are enlarge as the result of osteophyte formation and often show characteristic lateral deviation, reflecting the asymmetric focal cartilage loss of Osteoarthritis (OA).
Involvement of the first carpometacarpal joint (CMC) is also common, leading to pain on trying to open bottles and jars and functional impairment.
Clinically, it may detect by the presence of crepitus on joint movement, and squaring of the thumb base.
Generalised nodal OA has a very strong genetic component: the daughter of an affected mother has a 1 in 3 chance of developing nodal OA herself. [1]
Knee OA:
Osteoarthritis Of Knee
Location i.e.:
OA principally targets the patellofemoral and medial tibiofemoral compartments at this site but eventually spreads to affect the whole of the joint.
It may isolate or occur as part of generalised nodal OA.
Most patients, particularly women, have bilateral and symmetrical involvement.
With men, trauma is a more important risk factor and may result in unilateral OA.
Pain i.e.:
The pain is usually localised to the anterior or medial aspect of the knee and upper tibia.
Patellofemoral pain is usually worse going up and down stairs or inclines.
Posterior knee pain suggests the presence of a complicating popliteal cyst (Baker’s cyst).
Prolonged walking, rising from a chair, getting in or out of a car, or bending to put on shoes and socks may be difficult.
Local examination findings may include i.e.:
- A jerky, asymmetric (antalgic) gait with less time weight bearing on the painful side
- A varus, less commonly valgus, and/or fixed flexion deformity
- Joint line and/or periarticular tenderness (secondary anserine bursitis and medial ligament enthesopathy, causing tenderness of the upper medial tibia)
- Weakness and wasting of the quadriceps muscle
- Restricted flexion/extension with coarse crepitus
- Bony swelling around the joint line
Calcium pyrophosphate dihydrate (CPPD) crystal deposition in association with OA is most common at the knee. [1]
Hip OA:
Location i.e.:
Osteoarthritis Of Hip
Hip OA most commonly targets the superior aspect of the joint.
This is often unilateral at presentation, frequently progresses with superolateral migration of the femoral head, and has a poor prognosis.
The less common central (medial) Osteoarthritis-OA shows more central cartilage loss and is largely confined to women.
It is often bilateral at presentation and may associate with generalised nodal OA.
It has a better prognosis than superior hip OA and progression to axial migration of the femoral head is uncommon.
Pain i.e.:
Hip pain is usually maximal deep in the anterior groin, with variable radiation to the buttock, anterolateral thigh, knee or shin.
Lateral hip pain, worse on lying on that side with tenderness over the greater trochanter, suggests secondary trochanteric bursitis.
Common functional difficulties are the same as for knee Osteoarthritis-OA; in addition, restricted hip abduction in women may cause pain on intercourse.
Examination may reveal i.e.:
- An antalgic gait
- Weakness and wasting of quadriceps and gluteal muscles
- Pain and restriction of internal rotation with the hip flexed the earliest and most sensitive sign of hip OA; other movements may subsequently restricted and painful
- Anterior groin tenderness just lateral to the femoral pulse
- Fixed flexion, external rotation deformity of the hip
- Ipsilateral leg shortening with severe joint attrition and superior femoral migration.
Although obesity is not a major risk factor for development of hip Osteoarthritis-OA, it is associated with more rapid progression.
Spine OA:
Osteoarthritis Of Spine
- The cervical and lumbar spine are predominantly targeted by OA, then referred to as cervical spondylosis and lumbar spondylosis, respectively.
- Spine OA may occur in isolation or as part of generalised OA.
- The typical presentation is with pain localised to the low back region or the neck, although radiation of pain to the arms, buttocks and legs may also occur due to nerve root compression.
- The pain is typically relieved by rest and worse on movement.
- On physical examination, the range of movement may be limited and loss of lumbar lordosis is typical.
- The straight leg raising test or femoral stretch test may be positive and neurological signs may be seen in the legs where there is complicating spinal stenosis or nerve root compression.
Early-onset OA:
- Unusually, typical symptoms and signs of Osteoarthritis-OA may present before the age of 45.
- In most cases, a single joint is affected and there is a clear history of previous trauma.
- However, specific causes of OA need to be considered in people with early onset disease affecting several joints, especially those not normally targeted by Osteoarthritis-OA, rare causes need to be considered.
- Kashin– Beck disease is a rare form of Osteoarthritis-OA that occurs in children, typically between the ages of 7 and 13, in some regions of China.
- The cause is unknown but suggested predisposing factors are selenium deficiency and contamination of cereals with mycotoxin producing fungi.
Causes of early-onset osteoarthritis:
Monoarticular e.g.:
- Previous trauma
- Localised instability
Pauciarticular or polyarticular e.g.:
- Juvenile idiopathic arthritis
- Metabolic or endocrine disease: for example Haemochromatosis, Ochronosis, Acromegaly
- Spondyloepiphyseal dysplasia
- Late avascular necrosis
- Neuropathic joint
- Kashin–Beck disease [1]
Also Search As
People can search for homeopathic articles on Osteoarthritis in a variety of ways:
Online:
- Search engines: Use popular search engines like Google, DuckDuckGo, or Bing. Be specific with your search terms, such as "homeopathic remedies for osteoarthritis" or "homeopathic treatment of osteoarthritis research".
- Specialized databases: Explore databases like PubMed or the National Center for Biotechnology Information (NCBI) that index scientific literature, including homeopathic research.
- Homeopathic websites and journals: Search for reputable homeopathic organizations or journals that publish articles related to osteoarthritis.
Offline:
- Libraries: Visit your local library or university library and ask a librarian for assistance in finding relevant books or journals.
- Homeopathic practitioners: Consult a qualified homeopathic practitioner who may have access to resources and be able to provide information on homeopathic approaches to osteoarthritis.
Here are some possible interpretations of "OA" and how to search for each one effectively:
Osteoarthritis:
- General search terms:
- Osteoarthritis
- OA
- Degenerative joint disease
- Wear and tear arthritis
- Specific searches:
- Osteoarthritis symptoms
- Osteoarthritis causes
- Osteoarthritis treatment
- Osteoarthritis exercises
- Osteoarthritis diet
- Osteoarthritis research
- You can also add the specific joint you’re interested in (e.g., "knee osteoarthritis") or demographic factors (e.g., "osteoarthritis in elders").
Open Access:
- General search terms:
- Open access
- OA publishing
- Open science
- Free access journals
- Specific searches:
- Open access repositories
- Open access mandates
- Open access vs. traditional publishing
- Benefits of open access
- Challenges of open access
Other possible meanings:
- Office Automation:
- Office automation software
- OA tools
- OA systems
- Organizational Agility:
- Organizational agility
- Agile organizations
- Business agility
- Olympic Airways:
- Olympic Airways history
- Olympic Airways flights
- Other acronyms: depending on the context, OA could also stand for other things. Consider adding additional keywords to specify your search.
Frequently Asked Questions (FAQ)
What is Osteoarthritis?
Osteoarthritis (OA) is the most common form of arthritis, affecting millions worldwide.
It is a degenerative joint disease characterized by the breakdown of cartilage, the smooth tissue that cushions the ends of bones in a joint. This breakdown leads to pain, stiffness, and reduced mobility.
What causes Osteoarthritis?
OA is a multifactorial disease, meaning several factors can contribute to its development.
These include:
- Heredity
- Age: The risk of OA increases with age
- Sex: Women are more likely to develop OA than men
- Obesity – Excess weight puts additional stress on joints
- Injury
- Joint overuse
- Other diseases
How is osteoarthritis diagnosed?
Diagnosis typically involves:
- Medical history and physical examination
- Imaging tests like X-rays, MRI, or CT scans to visualize joint damage
- Blood tests to rule out other conditions like rheumatoid arthritis
Give the types of Osteoarthritis?
Types:
- Generalised nodal OA
- Knee OA
- Hip OA
- Spine OA
- Early-onset OA
What are the symptoms of Osteoarthritis?
Symptoms:
- Pain: Insidious onset, intermittent, morning stiffness
- Restricted movement
- Palpable, sometimes audible, coarse crepitus
- Bony swelling around joint margins
- Deformity, usually without instability
- Either Joint-line or periarticular tenderness
- Muscle weakness also wasting
- Synovitis mild or absent
Can homeopathy help with osteoarthritis?
Some people believe homeopathy can help manage osteoarthritis symptoms like pain and stiffness.
However, scientific evidence supporting its effectiveness is limited. It’s essential to consult with a qualified healthcare professional before considering homeopathic treatment.
How does homeopathy work for osteoarthritis?
Homeopathy follows the principle of "like cures like," using highly diluted substances that supposedly cause symptoms similar to the disease.
The aim is to stimulate the body’s self-healing abilities.
Is homeopathic treatment safe for osteoarthritis?
Homeopathic remedies are generally considered safe when used under the guidance of a qualified practitioner. However, it’s important to inform your doctor about any homeopathic remedies you’re taking, especially if you’re also on conventional medications.
How do I find a qualified homeopathic practitioner?
Look for practitioners who are registered with a recognized homeopathic association or board. Ask for their qualifications and experience in treating osteoarthritis.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Osteoarthritis?
Homoeopathic Medicines for Osteoarthrits
- Bryonia Alba
- Rhus Tox
- Kali Carb
- Arnica
- Ruta graveolens
- Kalmia latifolia
- Apis mellifica
- Calcarea fluorica
- Calcarea carbonica
- Sticta Pulmonaria
