Bulimia Nervosa
Definition
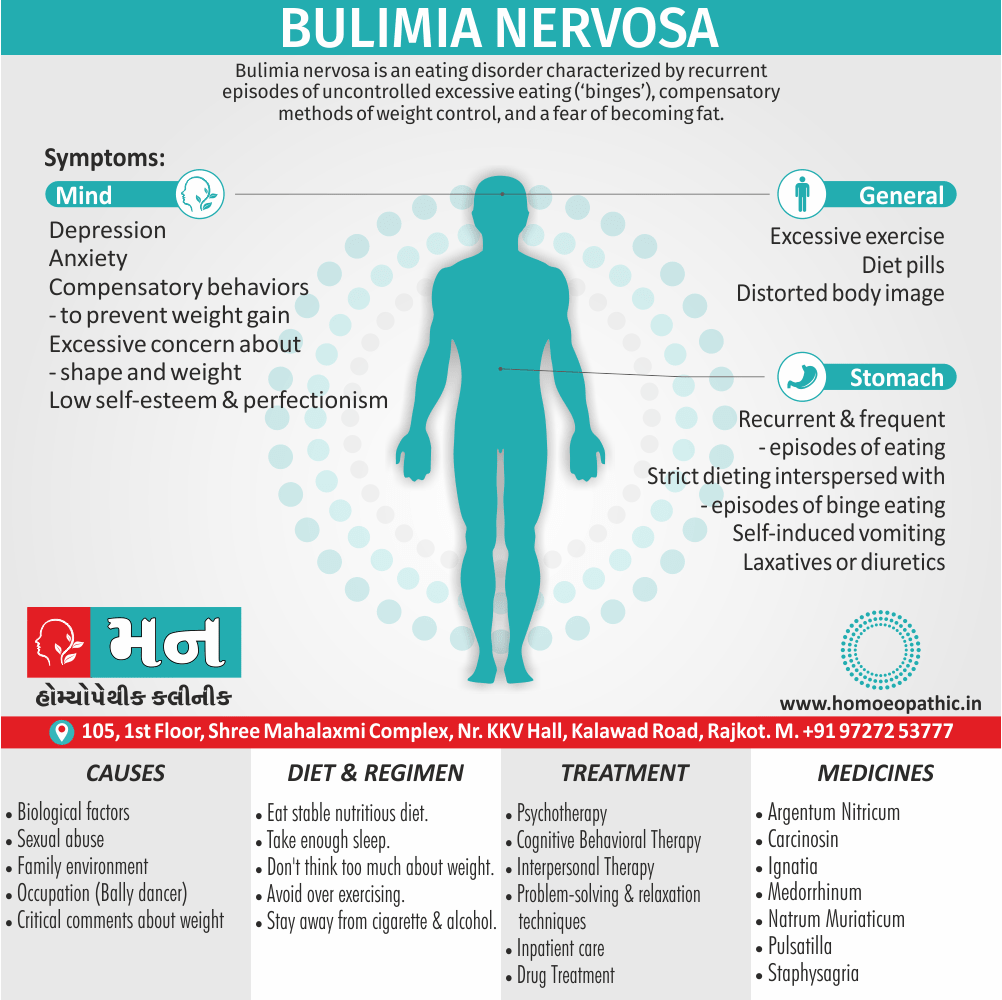
Bulimia nervosa is an eating disorder characterized by recurrent episodes of uncontrolled excessive eating , compensatory methods of weight control, and a fear of becoming fat. [1]
Bulimia nervosa has a few related terms, but true synonyms are limited in the medical field due to the specific characteristics of the eating disorder. Here’s a breakdown of some options depending on the context:
Formal Contexts:
- Purge disorder: This emphasizes the cycle of indulge eating followed by purging behaviors.
- Bulimic disorder (less common): This is a shorter version of bulimia nervosa but might be less widely recognized.
Informal Contexts (use with caution):
- Bulimia: This is a shortened version of bulimia nervosa, but it’s important to note that "bulimia" alone can be confused with other eating disorders.
- Purging syndrome: While descriptive, it’s not a formal diagnosis.
Important Considerations:
- In a medical setting, "bulimia nervosa" is the most precise and recognized term.
- "Purge disorder" might be appropriate for technical discussions but prioritize clarity for a general audience.
- Avoid informal terms like "bulimic" as a noun to describe someone with the condition.
Additional Options:
- You could describe specific aspects of bulimia nervosa, such as "experiencing cycles of indulge eating and purging." This wouldn’t be a synonym but could be helpful in some contexts.
Remember, accurate communication is crucial when discussing eating disorders. "Bulimia nervosa" is the most precise term for most contexts
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
The term ‘bulimia’ refers only to the episodes of uncontrollable excessive eating, and may also be present in other forms of eating disorder.
Moreover, Unlike anorexia nervosa, for which there are historical accounts dating back to medieval times, bulimia nervosa was first described as a distinct clinical entity in 1979.
Gerald Russell, a British psychiatrist, published a case series of 30 patients with bulimia nervosa also used them to describe the defining features of the condition.
Since Russell’s initial work, it has been realized that bulimia nervosa is a common condition, additionally, effective treatments have since been developed to treat it. [1]
Epidemiology
Epidemiology
The epidemiology of bulimia nervosa in India is not well-established due to limited research and varying methodologies. However, available studies suggest the following:
Shah M. Eating Disorders in India: A Systematic Review. Acta Neurophysiol 2023, 4(3): 180022:
This review mentions a study by Bhugra D, et al. that found a prevalence of 0.4% of bulimia nervosa in North India. It also highlights the wide range of disparities in prevalence estimates due to differences in gender, age, culture, and diagnostic methods.[9]
Incidence of Bulimia Nervosa – Medindia:
This source reports that the prevalence of bulimia nervosa among women aged 16-40 years in India is estimated to be around 1-3%. It also notes that this disorder is less common in men and is primarily recognized in developed countries.[10]
Eating Disorder Awareness Week in India 2023 – Skooc:
This article mentions various studies with differing prevalence rates of eating disorders in India, ranging from 2% to 6.5% in specific populations. While it doesn’t specifically state the prevalence of bulimia nervosa, it suggests that eating disorders are a growing concern in India.[11]
It is important to note that these are just a few examples, and the actual prevalence of bulimia nervosa in India may vary. Further research with standardized methods is needed to obtain more accurate and comprehensive data.
Causes
Causes
Biological i.e.:
- Female sex Age (15–40 years)
- Family history of:
- Mood disorders
- Substance abuse
- Eating disorder
- Obesity
- Type 1 diabetes
- Early menarche
Psychological i.e.:
- Critical comments in early life about eating, either shape, or weight
- Family environment with a focus on shape also dieting
- either Sexual or physical abuse in childhood
- Low self-esteem
- Perfectionism
Social i.e.:
- Living in a developed country
- Cultures that encourage dieting and value thinness
- Occupation (e.g. ballet dancer) [1]
Types
Types of Bulimia Nervosa
Bulimia of purging type
- This type is characterised by the use of self-induced vomiting or excessive usage of laxatives to purge food in order to prevent weight gain. Some patients may use diuretics.
2. Bulimia of non-purging type
- This type is characterised by using means, other than the self-induced methods, to avoid weight gain, like extreme degrees of fasting or excessive exercising that are both inappropriate. (6)
Risk Factors
Risk factors of Bulimia Nervosa
- Social isolation
- Change in mood or personality
- Refusing to eat in front of people
- Constantly talking about weight or food
- Impulsive behaviors
- Excessive or new substance or alcohol use
- Striving for perfectionism
- Intense fear of weight gain
- Obsession with body image
- Compulsive behaviors such as counting calories and tracking weight
- Distorted body image
- Participating in ritualistic behaviors while eating a meal
- Frequently weighing oneself
- Isolating oneself from the outside world
- Refusing to wear revealing or bright colored clothing
- Food hiding or hoarding
- Obsession with neutral and baggy clothing (4)
Pathogenesis
Pathogenesis
The pathogenesis of bulimia nervosa as a multifactorial interplay of biological, psychological, and sociocultural factors.
Biological Factors:
- Genetic Predisposition: Increased risk in first-degree relatives suggests a genetic component.
- Neurotransmitter Dysregulation: Alterations in serotonin, dopamine, and norepinephrine systems are implicated.
- Hypothalamic-Pituitary-Adrenal (HPA) Axis Dysfunction: Increased cortisol levels and stress response contribute.
- Neurobiological Changes: Structural and functional brain changes, particularly in areas related to reward and impulse control.
Psychological Factors:
Low Self-Esteem:
Negative body image and dissatisfaction with oneself.
Perfectionism:
Unrealistic expectations and striving for flawlessness.
Impulsivity:
Difficulty controlling urges and acting on impulse.
Emotional Dysregulation:
Difficulty managing emotions and coping with stress.
History of Trauma or Abuse:
Increased vulnerability to developing the disorder.
Sociocultural Factors:
Cultural Emphasis on Thinness:
Societal pressure to conform to unrealistic beauty standards.
Media Influence:
Exposure to idealized images of thinness and dieting behaviors.
Family Dynamics:
Overprotective or critical family environments can contribute.
Peer Pressure:
Influence from friends and social circles.
These factors interact in a complex manner, and the exact mechanisms leading to bulimia nervosa are still under investigation. The book Kaplan & Sadock’s Synopsis of Psychiatry emphasizes the importance of a comprehensive approach to understanding and treating the disorder, addressing both the biological and psychosocial aspects.[12]
Pathophysiology
Pathophysiology of Bulimia nervosa
- Bulimia is related to deep psychological issues and feelings of lack of control.
- Sufferers often use the destructive eating pattern to feel in control over their lives.
- They may hide or hoard food and overeat when stressed or upset.
- They may feel a loss of control during a satiete, and consume great quantities of food.
- There are higher rates of eating disorders in groups involved in activities that emphasize thinness and body type such as gymnastics, dance and cheerleading, figure skating.
- Bulimia is more prevalent among Caucasians but is increasing among African Americans and Hispanics.
- In one study, diagnosis of bulimia was correlated with high testosterone and low oestrogen levels, and normalizing these levels with combined oral contraceptive pills reduced craving for fat and sugar. (5)
Clinical Features
Clinical Features
The clinical features of bulimia nervosa as follows:
Core Features:
Recurrent Episodes of Indulge Eating:
Characterized by consuming a large amount of food in a discrete period (e.g., within 2 hours) and a sense of lack of control over eating during the episode.
Recurrent Inappropriate Compensatory Behaviors:
To prevent weight gain, such as self-induced vomiting, misuse of laxatives, diuretics, or other medications, fasting, or excessive exercise.
Frequency and Duration:
Indulge eating and inappropriate compensatory behaviors occur, on average, at least once a week for 3 months.
Self-Evaluation:
Unduly influenced by body shape and weight.
Associated Features:
Physical Symptoms:
- Electrolyte imbalances (e.g., hypokalemia)
- Dehydration
- Acid reflux and esophagitis
- Dental erosion
- Swollen salivary glands
- Irregular menstruation
- Gastrointestinal problems (e.g., constipation, irritable bowel syndrome)
Psychiatric Symptoms:
- Mood swings
- Depression
- Anxiety
- Substance abuse
- Personality disorders (e.g., borderline personality disorder)
Behavioral Symptoms:
- Impulsivity
- Social withdrawal
- Obsessive-compulsive behaviors
- Self-harm
Important Considerations:
- Normal or Heigherweight: Individuals with bulimia nervosa are typically normal weight or heigher weight, unlike those with anorexia nervosa who are underweight.
- Secrecy and Shame: Indulge eating and purging are often done in secret due to shame and embarrassment.
- Comorbidity: Bulimia nervosa often co-occurs with other mental health disorders, making diagnosis and treatment complex.
Please note that this is a summary of the clinical features mentioned in the book. For a comprehensive understanding, it is recommended to refer to the full text.[12]
Sign & Symptoms
Sign & Symptoms
It is characterized by recurrent also frequent episodes of eating unusually large amounts of food also feeling a lack of control over these episodes.
This satiate-eating is followed by behavior that compensates for the overeating for instance; forced vomiting, excessive use of laxatives or diuretics, fasting, excessive exercise, or a combination of these behaviors. [3]
There is an intense fear of becoming higher-weight person . There may be an earlier history of anorexia nervosa.
It is usually body-image disturbance and the person is unable to perceive own body size accurately. [2]
There is a persistent preoccupation with eating, also an irresistible craving for food. Besides this, There are episodes of overeating in which large amounts of food are consumed within short periods of time. [2]
Fascinated by food they sometimes buy magazines also cookbooks to read recipes, and enjoy discussing dieting issues. [3]
Weight control e.g.:
- Strict dieting interspersed with episodes of indulging eating
- Compensatory behaviours to prevent weight gain
- Self-induced vomiting
- either Laxatives or diuretics
- Excessive exercise
- Diet pills
Psychopathology e.g.:
- Excessive concern about shape and weight
- Distorted body image
- Low self-esteem also perfectionism
Physical consequences of weight control behaviours i.e.:
- Normal body weight
- Hypokalaemia, hyponatraemia, hypochloremia
- Menstrual abnormalities
- Swollen parotid glands
- Erosion of dental enamel
- Calluses of the dorsal aspect of the fingers (in other words, Russell’s sign)
- Peripheral oedema
- Increased plasma amylase
Other comorbid psychiatric conditions e.g.:
- Depression
- Anxiety
- Deliberate self-harm
- Misuse of either alcohol or drugs
- Borderline personality disorder [1]
Clinical Examination
Clinical Examination
The following components for a clinical examination of a patient suspected of having bulimia nervosa:
Physical Examination:
Vital Signs:
Assess blood pressure (may be low due to dehydration), heart rate (may be irregular), and temperature.
Weight and BMI:
Note that individuals with bulimia nervosa are typically normal weight or higher weight.
General Appearance:
Observe for signs of malnutrition (e.g., dry skin, brittle hair) or dehydration (e.g., dry mucous membranes).
Head and Neck:
- Oral Cavity: Check for dental erosion, caries, and enlarged salivary glands (parotid enlargement).
- Throat: Look for pharyngeal erythema or Russell’s sign (calluses on the knuckles from self-induced vomiting).
Abdominal Examination:
Assess for tenderness, distension, or bowel sounds indicative of gastrointestinal problems.
Cardiovascular and Respiratory:
Auscultate for any abnormalities in heart or lung sounds.
Neurological Examination:
Assess for any neurological deficits.
Laboratory Tests:
Complete Blood Count (CBC):
To evaluate for anemia or other blood cell abnormalities.
Electrolytes:
To check for imbalances, particularly hypokalemia (low potassium) due to purging behaviors.
Liver Function Tests (LFTs):
To assess for liver damage.
Kidney Function Tests:
To evaluate kidney function.
Thyroid Function Tests:
To rule out thyroid disorders.
Additional Investigations (if indicated):
Electrocardiogram (ECG):
To assess for cardiac arrhythmias related to electrolyte imbalances.
Bone Density Scan:
To evaluate for osteoporosis, a potential complication of bulimia nervosa.
Dental Examination:
To assess for dental erosion and caries.
Mental Status Examination:
- Assess for mood disturbances (e.g., depression, anxiety) and cognitive impairments.
- Evaluate for any comorbid psychiatric disorders (e.g., personality disorders, substance abuse).
The book Kaplan & Sadock’s Synopsis of Psychiatry emphasizes the importance of a thorough clinical examination and laboratory tests to assess the physical and psychological health of individuals with bulimia nervosa, as well as to identify any potential complications or comorbidities.[12]
Diagnosis
Diagnosis
The formal diagnostic criteria for bulimia nervosa are i.e.:
- Recurrent episodes of indulging eating, characterized by eating a large amount of food and by a sense of lack of control over eating
- Recurrent inappropriate behavior to prevent weight gain
- Evaluation of self-worth primarily based on weight also shape
- Symptoms do not occur exclusively during episodes of anorexia nervosa.
The last point means that a diagnosis of anorexia nervosa effectively ‘trumps’ bulimia nervosa; additionally, if the patient has a BMI of less than 17.5, the diagnosis is always anorexia nervosa. [1]
Differential Diagnosis
Differential Diagnosis
1. Anorexia nervosa:
It can be differentiated from bulimia nervosa principally by a low body weight (BMI <17.5). Indulge eating may occur in anorexia nervosa, but must be present for a diagnosis of bulimia nervosa.
2. EDNOS:
It describes those patients with disordered eating which is clinically significant, but which does not fit criteria for a specific eating disorder; for example, a patient with all the features of bulimia nervosa, except for the use of compensatory behaviors to prevent weight gain.
3. Klein–Levin syndrome:
In brief, This is a sleep disorder seen in adolescent males, characterized by recurrent episodes of indulging eating also hypersomnia.
4. Mood disorder such as:
Core features include low mood, fatigue, also anhedonia. Weight gain and indulging eating may occur, but the patient will not show the specific psychopathology and other weight control behaviours seen in bulimia nervosa.
5. Iatrogenic drugs such as:
Many drugs may cause weight gain, either through increased appetite or a direct effect on metabolism; for example, antipsychotics, lithium, steroids.
6. Organic disorders:
These can usually be identified by a clear history and lack of associated core psychopathology, but specific investigations may need to be done; for example, upper GI disorders with associated vomiting, brain tumours. [1]
Complications
Complication
The following complications of bulimia nervosa:
Medical Complications:
Metabolic:
- Electrolyte abnormalities (hypokalemia, hypochloremia, hyponatremia, metabolic alkalosis)
- Dehydration
- Acid-base disturbances
Gastrointestinal:
- Salivary gland hypertrophy
- Esophageal tears (Mallory-Weiss syndrome)
- Gastric dilatation or rupture
- Constipation, diarrhea, abdominal pain
- Pancreatitis
Dental:
- Erosion of dental enamel
- Caries
- Periodontal disease
Cardiac:
- Arrhythmias (due to electrolyte imbalances)
- Cardiomyopathy
- Ipecac cardiomyopathy (if ipecac is used to induce vomiting)
Endocrine:
- Menstrual irregularities or amenorrhea
- Osteoporosis (due to malnutrition and hormonal changes)
Psychiatric Complications:
Depression and anxiety:
Common comorbidities of bulimia nervosa.
Substance use disorders:
Increased risk of developing substance abuse problems.
Self-harm and suicidal ideation:
May occur in severe cases.
Personality disorders:
Particularly borderline personality disorder, may coexist with bulimia nervosa.
Social Complications:
Impaired social functioning:
Difficulty maintaining relationships and fulfilling social roles.
Occupational problems:
Absenteeism, decreased productivity, and difficulty concentrating at work.
Financial problems:
Due to the cost of food, medical care, and treatment.
Investigations
Investigation of Bulimia Nervosa
- serum electrolytes
- serum creatinine
- serum magnesium
- urine pregnancy test
- ECG
- serum ferritin
- serum B12
- serum red blood cell folate (6)
Treatment
Treatment of Bulimia Nervosa
- When you have bulimia, you may need several types of treatment, although combining psychotherapy with antidepressants may be the most effective for overcoming the disorder.
- Treatment generally involves a team approach that includes you, your family, your primary care provider, a mental health professional and a dietitian experienced in treating eating disorders. You may have a case manager to coordinate your care.
Psychotherapy
Psychotherapy, also known as talk therapy or psychological counseling, involves discussing your bulimia and related issues with a mental health professional. Evidence indicates that these types of psychotherapy help improve symptoms of bulimia:
- Cognitive behavioral therapy to help you normalize your eating patterns and identify unhealthy, negative beliefs and behaviors and replace them with healthy, positive ones
- Family-based treatment to help parents intervene to stop their teenager’s unhealthy eating behaviors, to help the teen regain control over his or her eating, and to help the family deal with problems that bulimia can have on the teen’s development and the family
- Interpersonal psychotherapy, which addresses difficulties in your close relationships, helping to improve your communication and problem-solving skills
Ask your mental health professional which psychotherapy, will use and what evidence exists that shows it’s beneficial in treating bulimia.
Medications
- Antidepressants may help reduce the symptoms of bulimia when used along with psychotherapy. The only antidepressant specifically approved by the Food and Drug Administration to treat bulimia is fluoxetine (Prozac), a type of selective serotonin reuptake inhibitor (SSRI), which may help even if you’re not depressed.
Nutrition education
- Dietitians can design an eating plan to help you achieve healthy eating habits to avoid hunger and cravings and to provide good nutrition. Eating regularly and not restricting your food intake is important in overcoming bulimia.
Hospitalization
- Bulimia can usually be treated outside of the hospital. But if symptoms are severe, with serious health complications, you may need treatment in a hospital. Some eating disorder programs may offer day treatment rather than inpatient hospitalization. (8)
Prevention
Prevention of Bulimia Nervosa
- Education about and awareness of the disorder and associated risk factors
- Early intervention if risk factors are identified
- Knowledge and maintenance of healthy eating habits
- Cultivation of a positive self-image of the body
- Maintenance of good mental health
- Counseling as needed to identify and resolve areas of conflict and stress
- Balancing school, work, social life, rest, and exercise (7)
Homeopathic Treatment
Homeopathic Treatment of Bulimia Nervosa
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Bulimia Nervosa
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
Argentum nit:
Satieting especially with chocolate, fixed ideas, impulsive behaviour, anticipation, overriding impulses for certain foods, chocolate, salty foods, they will eat a whole box of chocolates until they get sick.
Carcinosin:
Obsessive compulsive disorder. Moreover, Perfectionism, fear of becoming fat, fear of rejection. Etiology-abuse, grief or fears, often related to weight.
Ignatia:
Perfectionism, fear of becoming fat, fear of rejection. Hysteria-loss of control of emotions, fainting. Besides this, Etiology-grief or big disappointment, often related to weight.
Medorrhinum:
Ups and down in the person’s energy, very outgoing for 2 or 3 days than wiped out for several days and with that their diets fluctuate from good to satieting. Bulimia also with alcohol and drugs.
Natrum mur:
Often indicated remedy in anorexia, a lot of guilt. Furthermore, Fear of being rejected, hurt easily. Very self-conscious of their weight.
Pulsatilla:
Fear of being abandoned also unloved. Fixed ideas about food, their weight, they gain and lose weight easily, eat also indulging to console themselves, satiets out of loneliness, or depression, then they get guilt and fear about it and then suppress it.
Staphysagria:
indulging out of guilt, depression. Additionally, Poor self-confidence and worthlessness. It is out of self-denial, they do not deserve that -lemon meringue pie so they suppress their desire for it, and then indulging on it. [3]
Diet & Regimen
Diet & Regimen of Bulimia Nervosa
- Eat stable nutritious diet.
- Take enough sleep.
- Don’t think too much about weight.
- Avoid over exercising.
- Stay away from cigarette & alcohol.
Do’s and Don'ts
The Do’s & Don’ts
Do’s:
- Seek professional help: Early diagnosis and treatment are crucial for recovery. Consult a mental health professional specializing in eating disorders.
- Engage in therapy: Cognitive behavioral therapy (CBT) and other evidence-based therapies can help address the underlying psychological issues and develop healthier coping mechanisms.
- Follow a balanced meal plan: Work with a registered dietitian to establish regular eating patterns and avoid restrictive dieting, which can trigger indulge eating.
- Build a support system: Surround yourself with understanding and supportive friends, family, or support groups.
- Practice self-care: Engage in activities that promote relaxation, reduce stress, and improve self-esteem.
- Be patient with yourself: Recovery takes time and effort. Celebrate small victories and be kind to yourself during setbacks.
Don’ts:
- Don’t isolate yourself: Avoid withdrawing from social interactions and activities.
- Don’t compare yourself to others: Focus on your own progress and avoid comparing yourself to unrealistic body ideals.
- Don’t engage in negative self-talk: Challenge negative thoughts about yourself and your body.
- Don’t skip meals or restrict food: This can increase the risk of indulge eating.
- Don’t weigh yourself obsessively: Focus on overall health and well-being rather than just the number on the scale.
- Don’t give up: Recovery is possible with the right treatment and support.
Remember, these are general guidelines. A personalized treatment plan tailored to your specific needs and circumstances is essential for successful recovery from bulimia nervosa.[12]
Terminology
Terminology
Here’s a breakdown of the terminologies used in your homeopathic article on Bulimia Nervosa and their meanings:
Bulimia Nervosa:
An eating disorder characterized by recurrent episodes of indulge eating (consuming large amounts of food in a short period with a loss of control) followed by compensatory behaviors (purging, fasting, excessive exercise) to prevent weight gain.
Indulge Eating:
The consumption of a large amount of food in a short period with a sense of loss of control.
Compensatory Behaviors:
Actions taken after indulge eating to prevent weight gain, such as self-induced vomiting, misuse of laxatives or diuretics, fasting, or excessive exercise.
Purging:
The act of self-induced vomiting or misuse of laxatives or diuretics to rid the body of food consumed during a indulge.
Pathogenesis:
The origination and development of a disease. In the context of bulimia nervosa, it refers to the various biological, psychological, and sociocultural factors that contribute to the development of the disorder.
Pathophysiology:
The disordered physiological processes associated with a disease. In bulimia nervosa, this includes the physical effects of indulge eating and purging, such as electrolyte imbalances, gastrointestinal issues, and dental problems.
Comorbidity:
The simultaneous presence of two or more medical conditions or diseases in a patient. Bulimia nervosa is often associated with other mental health disorders like depression, anxiety, and substance abuse.
Homeopathic Remedies:
Natural substances used in homeopathy to treat various ailments. The principle of homeopathy is "like cures like," meaning a substance that can cause symptoms in a healthy person can be used in a diluted form to treat similar symptoms in a sick person.
Miasm:
A predisposition to chronic disease in homeopathy. Homeopathic practitioners consider the individual’s miasmatic tendency when selecting remedies.
By understanding these terms, readers can better comprehend the information presented in your article and make informed decisions about their health and treatment options.
References
References
- Psychiatry, Fourth Edition- Oxford Medical Publications – SRG- by Geddes, Jonathan Price, Rebecca McKnight / Ch 27.
- A Short Textbook of PSYCHIATRY 7th edition by Niraj Ahuja / ch 12.
- Homeopathy in treatment of Psychological Disorders by Shilpa Harwani / ch 15.
- https://www.medainc.org/causes-and-risk-factors-for-bulimia-nervosa-2/
- https://www.wikidoc.org/index.php/Bulimia_nervosa_pathophysiology
- https://bestpractice.bmj.com/topics/en-gb/441
- https://bulimiaguide.org/prevention-cure-triggers/
- https://www.mayoclinic.org/diseases-conditions/bulimia/diagnosis-treatment/drc-20353621
- Shah M. Eating Disorders in India: A Systematic Review. Acta Neurophysiol 2023, 4(3): 180022
- Incidence of Bulimia Nervosa – Medindia.
- Eating Disorder Awareness Week in India 2023 – Skooc:
- Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry, 12th Edition by Benjamin J. Sadock, Virginia A. Sadock, and Pedro Ruiz (2022).
Also Search As
- Also Search As
General Search Terms:
- Bulimia nervosa homeopathic treatment
- Homeopathy for bulimia
- Natural remedies for bulimia
- Eating disorder homeopathic remedies
- Homeopathic medicine for bulimia
Specific Remedy Searches:
- Pulsatilla for bulimia
- Natrum Muriaticum for bulimia
- Antimonium Crudum for bulimia
- Ignatia for bulimia
- Homeopathic remedies for indulge eating
- Homeopathic remedies for purging
Long-Tail Keywords:
- How can homeopathy help with bulimia nervosa?
- Is homeopathic treatment safe for bulimia?
- What are the best homeopathic remedies for bulimia?
- Can homeopathy cure bulimia nervosa?
Additional Tips:
- Use synonyms: Include terms like "alternative medicine," "complementary therapy," or "holistic treatment" in your article.
- Incorporate questions: Use the FAQs provided earlier in the article and in the title to match common search queries.
- Optimize meta descriptions: Write clear and concise meta descriptions that accurately summarize your article and include relevant keywords.
- Promote on social media: Share your article on social media platforms and homeopathic forums to reach a wider audience.
By incorporating these keywords and strategies into your article and its metadata, you can improve its visibility in search engine results and attract readers who are interested in exploring homeopathic options for bulimia nervosa.
People can search for your article using various methods:
Search Engines:
- Use relevant keywords: People will likely search using terms like "bulimia nervosa homeopathy," "homeopathic remedies for bulimia," or specific remedy names like "Pulsatilla for bulimia."
- Include long-tail keywords: These are more specific phrases like "how can homeopathy help with bulimia nervosa."
- Use search engine suggestions: As people type, search engines offer suggestions. This can help you understand common search terms.
Social Media Platforms:
- Share your article on platforms like Facebook, Twitter, or Instagram.
- Use relevant hashtags: #homeopathy, #bulimianervosa, #eatingdisorders, etc.
- Join homeopathic groups and forums: Share your article in these communities.
Homeopathic Websites and Directories:
- Submit your article to homeopathic websites and blogs that accept guest posts.
- List your article on directories that cater to homeopathic practitioners and patients.
Direct Traffic:
- If you have a website or blog, promote your article through newsletters, social media, or other channels.
- Share the article link directly with individuals or groups interested in homeopathy.
Other Online Platforms:
- Consider platforms like Reddit (in relevant subreddits) or Quora, where you can answer questions related to bulimia and homeopathy, linking to your article when appropriate.
Remember:
- Optimize your article’s title, meta description, and headers to make it more search engine friendly.
- Include relevant keywords throughout your article.
- Encourage social sharing by adding social media sharing buttons to your article.
By utilizing these different search methods, you can increase the visibility of your article and reach a wider audience interested in homeopathic approaches to bulimia nervosa.
Frequently Asked Questions (FAQ)
What is Bulimia Nervosa?
Bulimia nervosa is an eating disorder characterized by recurrent episodes of uncontrolled excessive eating, compensatory methods of weight control, and a fear of becoming fat.
How is bulimia nervosa treated?
Treatment typically involves a combination of psychotherapy (such as cognitive behavioral therapy), nutritional counseling, and sometimes medication to manage underlying mental health conditions like depression or anxiety.
What are the causes of Bulimia Nervosa?
Causes
- Female sex Age (15–40 years)
- Family history
- Type 1 diabetes
- Early menarche
- Family environment with a focus on shape and dieting
- Sexual or physical abuse in childhood
- Low self-esteem
- Perfectionism
What are the symptoms of Bulimia Nervosa?
Symptoms
- Strict dieting interspersed with episodes of indulging eating
- Compensatory behaviours to prevent weight gain
- Self-induced vomiting
- Laxatives or diuretics
- Excessive exercise, Diet pills
- Excessive concern about shape and weight
- Distorted body image
- Menstrual abnormalities
- Depression, Anxiety
- Deliberate self-harm
Homeopathic Medicines used by Homeopathic Doctors in treatment of Bulimia Nervosa?
Homoeopathic Medicines For Bulimia Nervosa
- Argentum nit
- Carcinosin
- Ignatia
- Medorrhinum
- Natrum mur
- Pulsatilla
- Staphysagria
Can homeopathy help with bulimia nervosa?
Homeopathy is a complementary therapy that some individuals find helpful in managing the emotional and physical aspects of bulimia nervosa. Homeopathic remedies are selected based on individual symptoms and constitutional type.
