Opioid Use Disorder
Definition
Opioids are substances that mimic the effects of endogenous opioids (endorphins also enkephalins) by acting as agonists at the opioid receptors. [1]
Here are some synonyms for Opioid Use Disorder (OUD):
- Opioid addiction
- Problematic opioid use
- Opioid dependence
These terms all refer to a condition in which a person has an uncontrollable urge to use opioids, despite the negative consequences that this use may cause.
It’s important to note that some terms, like "opioid abuse," are considered outdated and less preferred by medical professionals. This is because "abuse" can carry a judgmental connotation. OUD is a medical condition and should be treated as such.
Overview
Opioid Derivatives
Physiological effects
Route of Administration
Acute Intoxication
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Withdrawal Syndrome
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
In the last few decades, opioid use disorder has increased markedly all over the world. [2]
The first record of opioid use by humans was in Mesopotamia in around 3400 BC, when people extracted the natural opioids from poppies and smoked them.
Originally it was marketed as a less addictive form of morphine, but unfortunately this turned out to be completely wrong. Diamorphine is the mostly widely used opioid, as it produces the most powerful euphoria. [1]
Dried exudate obtained from unripe seed capsules of Papaver somniferum has used also abused for centuries. Additionally; The natural alkaloids of opium and their synthetic preparations are highly dependence producing. [2]
Worldwide spread
The UN estimates that 15–20 million people worldwide are dependent upon diamorphine at any one time. As well as the desired euphoric effect of opioids, they also have a wide range of other effects upon the body, with the most commonly experienced being analgesia, constipation, anorexia, and loss of libido.
All in all; The high risk of respiratory depression makes the uncontrolled use of opioids very dangerous. [1]
Opioid Derivatives
Opioid Derivatives
A. Natural Alkaloids of Opium:
- Morphine
- Codeine
- Thebaine
- Noscapine
- Papaverine
B. Synthetic Compounds:
- Heroin
- Nalorphine
- Hydromorphone
- Methadone
- Dextropropoxyphene
- Meperidine (in other words; Pethidine)
- Cyclazocine
- Levallorphan
- Diphenoxylate
The most important dependence producing derivatives are morphine and heroin. They both like majority of dependence producing opioids bind to μ (mu) opioid receptors. The other opioid receptors are k (kappa, e.g. for pentazocine), δ (delta, e.g. for a type of enkephalin), σ (sigma, e.g. for phencyclidine), ε (epsilon) and λ (lambda). [2]
Physiological effects
Physiological effects
Psychological and neurological:
- Tolerance also dependence
- Anxiolysis
- Either Confusion or delirium
- Euphoria
- Drowsiness
- Analgesia
Cardiovascular:
Bradycardia
Hypotension
Respiratory:
Respiratory depression
Hypoventilation
Gastrointestinal:
Nausea also vomiting
Constipation
Dyspepsia
Miscellaneous:
Dry mouth
Pupil constriction
Urinary retention
Muscle spasticity
Itching. [1]
Route of Administration
Route of Administration
Opioids can be taken by mouth, intravenously, either by inhaling, or by smoking.
Mouth:
When diamorphine is taken orally it undergoes extensive first-pass metabolism, converting it to morphine and reducing the euphoric effects.
Intravenous (IV):
Intravenous (IV) use avoids this metabolism, and diamorphine crosses the blood–brain barrier quickly and produces a rapid powerful euphoria. IV use of heroin carries all of the risks discussed earlier in the chapter.
The antecubital fossa is usually the site first used for injecting, but eventually the veins become damaged and the user moves elsewhere.
- When venous access becomes extremely difficult, users may inject either subcutaneously (skin popping) or intramuscularly. [1]
- Apart from the parenteral mode of administration, heroin can also be smoked or ‘chased’ (chasing the dragon), often in an impure form (called ‘ smack’ or ‘ brown sugar’ in India). [2]
The form of heroin most commonly used in the UK will only dissolve if mixed with an acid and heated. The use of citric acid powder and lemon juice is typical, with heating occurring on a spoon over a heat source.
The use of acids is particularly troublesome because it causes immense damage to the veins. [1]
Heroin or di-acetyl-morphine is about two times more potent than morphine in inject-able form.
Duration
Heroin is more addicting than morphine and can cause dependence even after a short period of exposure. Tolerance to heroin occurs rapidly and can be increased to up to more than 100 times the first dose needed to produce an effect. [2]
Acute Intoxication
Acute Intoxication
Intoxication is characterised by apathy, bradycardia, hypotension, respiratory depression, subnormal core body temperature, also pin-point pupils.
Later, delayed reflexes, thready pulse and coma may occur in case of a large overdose. In severe intoxication, mydriasis may occur due to hypoxia. [2]
Epidemiology
Epidemiology
The 2019 study by Murthy et al. showed that the prevalence of opioid use in India is three times the global average. About 2.1% of India’s population use opioids.
(Murthy P, et al. Magnitude of substance use in India: National Survey, 2019. New Delhi: Ministry of Social Justice and Empowerment, Government of India; 2019.)[3]
Causes
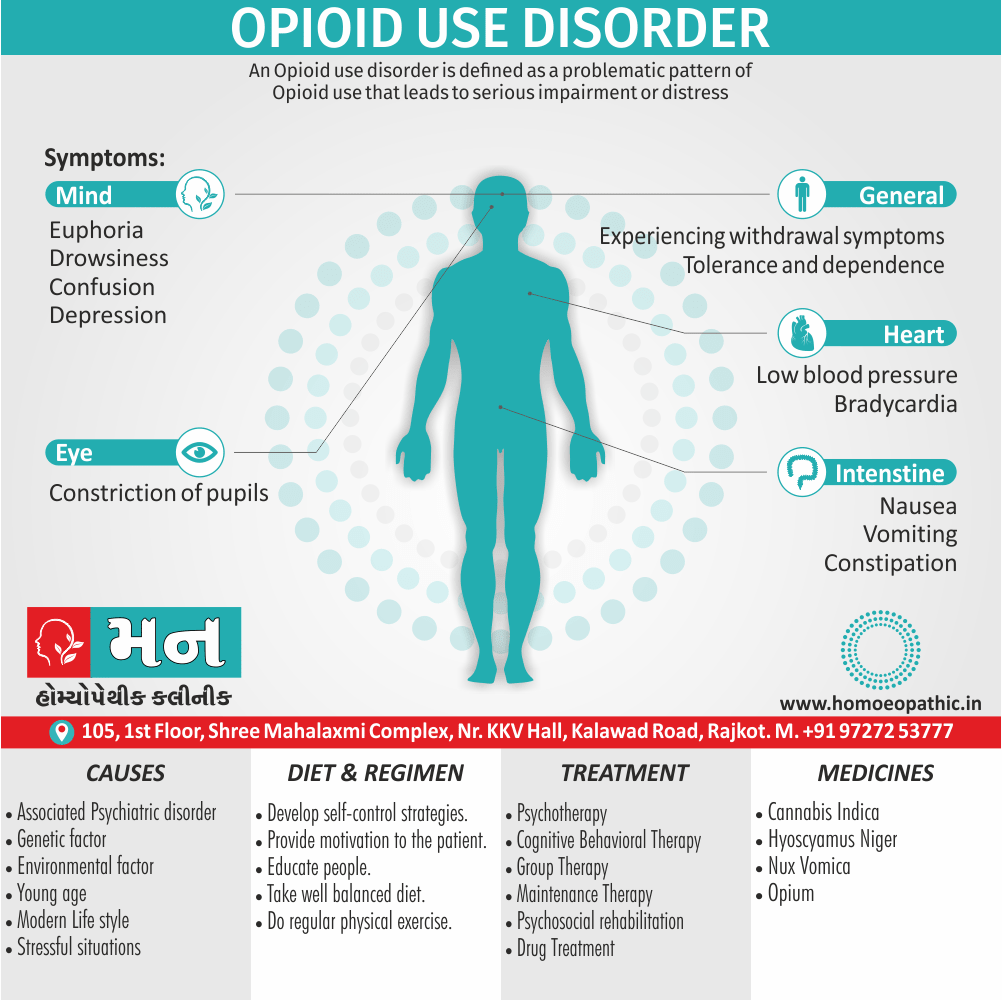
Causes of Opioid Use Disorder
Opioid use disorder (OUD) is a complex condition with various contributing factors. Some of the common causes include:
Chronic pain:
Long-term use of prescription opioids for pain management can increase the risk of developing OUD.
Genetic predisposition:
Family history of substance use disorders can increase an individual’s susceptibility to OUD.
Environmental factors:
Exposure to environments where opioid use is prevalent or easy access to opioids can increase the likelihood of developing OUD.
Psychological factors:
Mental health conditions such as depression, anxiety, or PTSD can increase the risk of opioid misuse and subsequent OUD.
Social factors:
Peer pressure, social isolation, and lack of support systems can contribute to the development of OUD.
It’s important to note that OUD often arises from a combination of these factors, and the specific causes can vary from person to person.[4]
Types
Types of Opioid Use Disorder
Opioid use disorder (OUD) itself is not typically categorized into distinct "types." However, it’s important to recognize that OUD can manifest in different ways and severity levels.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) outlines criteria for diagnosing OUD, which include a range of symptoms related to opioid use, such as:
Impaired control:
Taking larger amounts or over a longer period than intended, persistent desire or unsuccessful efforts to cut down or control use, and a great deal of time spent obtaining, using, or recovering from opioid use.
Social impairment:
Failure to fulfill major role obligations at work, school, or home, continued use despite persistent or recurrent social or interpersonal problems caused or exacerbated by opioid use, and important social, occupational, or recreational activities given up or reduced because of opioid use.
Risky use:
Recurrent opioid use in situations in which it is physically hazardous, continued use despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by opioid use.
Pharmacological criteria:
Tolerance (needing increased amounts to achieve desired effect or markedly diminished effect with continued use of the same amount) and withdrawal (characteristic withdrawal syndrome or opioid taken to relieve or avoid withdrawal symptoms).
The severity of OUD is then classified as mild (2-3 symptoms), moderate (4-5 symptoms), or severe (6 or more symptoms).
While OUD itself isn’t categorized into types, it’s crucial to consider the various factors that contribute to and influence its presentation, such as the specific opioid used, the individual’s history and circumstances, and any co-occurring mental or physical health conditions. This information can help inform appropriate treatment and support strategies.[5]
Risk Factors
Risk factors
Opioid use disorder (OUD) risk factors can be numerous and interconnected. Some prominent ones, as outlined in a reputable source, include:
Family History of Substance Abuse:
Having a family history of substance abuse, including alcohol or drug misuse, significantly increases the risk of developing OUD.
Personal History of Substance Abuse:
Prior personal experiences with substance abuse, particularly involving alcohol, illicit drugs, or prescription medications, elevate the risk for OUD.
Young Age:
Individuals between the ages of 16 and 45 are at a higher risk due to various factors, including increased exposure to opioids and greater susceptibility to peer influence.
History of Trauma:
Experiencing trauma, especially during childhood or adolescence, increases vulnerability to developing OUD as a coping mechanism.
Mental Health Conditions:
Co-occurring mental health disorders like depression, anxiety, or PTSD can increase the likelihood of opioid misuse and subsequent OUD.
It’s crucial to remember that these are just some of the risk factors. Other factors such as chronic pain, environmental factors, and social factors also play a significant role. Recognizing these risk factors can help in early identification and intervention for individuals at risk of developing OUD.[4]
Pathogenesis
Pathogenesis
The pathogenesis of Opioid Use Disorder (OUD) is a complex process involving both neurobiological and psychosocial factors.
Neurobiological Factors
Opioids primarily act on the brain’s reward system, particularly the mesolimbic dopamine pathway. Repeated opioid use leads to changes in this pathway, resulting in:
- Tolerance: The need for increasing doses to achieve the same effect.
- Dependence: The body adapts to the presence of opioids, leading to withdrawal symptoms upon cessation.
- Sensitization: Increased sensitivity to opioid-related cues, leading to cravings and relapse.
- Dysregulation of stress systems: Chronic opioid use disrupts the body’s stress response systems, contributing to anxiety and vulnerability to relapse.
Psychosocial Factors
These factors interact with the neurobiological changes to further contribute to the development and maintenance of OUD:
- Chronic pain: Individuals with chronic pain are at increased risk due to the reinforcing effects of opioids on pain relief.
- Mental health disorders: Co-occurring conditions such as depression, anxiety, and PTSD can increase the risk of opioid misuse and addiction.
- Environmental factors: Exposure to environments where opioid use is prevalent, or easy access to opioids, can increase the likelihood of developing OUD.
- Genetic predisposition: Family history of substance use disorders can increase an individual’s susceptibility.
It’s crucial to understand that OUD is a chronic, relapsing disorder. The combination of these neurobiological and psychosocial factors makes it challenging to treat, emphasizing the need for comprehensive and individualized approaches to management.[4]
Pathophysiology
Pathophysiology
The pathophysiology of Opioid Use Disorder (OUD) is a complex interplay of neurobiological adaptations and psychosocial factors that lead to compulsive drug-seeking and use despite harmful consequences.
Neurobiological Adaptations
Reward Pathway: Opioids bind to mu-opioid receptors in the brain’s reward pathway, triggering the release of dopamine, a neurotransmitter associated with pleasure and reinforcement. Repeated opioid use leads to downregulation of dopamine receptors, resulting in tolerance and the need for higher doses to achieve the same effect.
Stress Systems: Chronic opioid use disrupts the hypothalamic-pituitary-adrenal (HPA) axis, responsible for stress regulation. This dysregulation leads to heightened stress responses, anxiety, and increased vulnerability to relapse.
Neuroadaptations in the Brain: Opioids induce long-lasting changes in gene expression and neural circuitry, particularly in the prefrontal cortex and amygdala, affecting decision-making, impulse control, and emotional regulation.
Psychosocial Factors
Chronic Pain: Opioids are often prescribed for pain management, and prolonged use can increase the risk of developing OUD, especially in individuals with chronic pain conditions.
Mental Health Disorders: Co-occurring mental health conditions, such as depression, anxiety, and PTSD, increase the risk of opioid misuse and dependence.
Environmental Factors: Exposure to environments with high opioid availability, social pressures, and lack of support systems can contribute to the development and maintenance of OUD.
Genetic Predisposition: Family history of substance use disorders increases an individual’s vulnerability to OUD due to genetic and epigenetic factors.
Clinical Features
Clinical Features
Opioid use disorder (OUD) presents with a variety of clinical features that can be broadly classified into behavioral, physical, and psychological manifestations. These clinical features are vital in diagnosing and assessing the severity of the disorder.
Behavioral Features:
- Compulsive Drug-Seeking: The hallmark of OUD is the overwhelming desire to obtain and use opioids, often leading to significant time and effort spent in drug-seeking behaviors.
- Loss of Control: Individuals with OUD may experience difficulty controlling the amount and frequency of opioid use, often exceeding their intended limits.
- Continued Use Despite Consequences: OUD is characterized by persistent opioid use even in the face of adverse consequences, such as health problems, relationship difficulties, and legal issues.
- Neglect of Responsibilities: Individuals with OUD may neglect their responsibilities at work, school, or home due to the prioritization of opioid use.
Physical Features:
- Tolerance: The need for increasing doses of opioids to achieve the same effect, indicating physiological adaptation to the drug.
- Withdrawal: The experience of unpleasant physical and psychological symptoms upon cessation or reduction of opioid use, including nausea, vomiting, muscle aches, anxiety, and restlessness.
- Physical Signs of Opioid Use: These may include constricted pupils, drowsiness, slurred speech, and impaired coordination.
- Overdose: In severe cases, OUD can lead to opioid overdose, a potentially fatal condition characterized by respiratory depression, loss of consciousness, and coma.
Psychological Features:
- Cravings: Intense desires or urges to use opioids, often triggered by environmental cues or internal states.
- Mood Changes: OUD can contribute to mood swings, irritability, anxiety, and depression.
- Cognitive Impairment: Chronic opioid use can affect cognitive functions such as memory, concentration, and decision-making.[4]
Sign & Symptoms
Sign & Symptoms of Opioid Use Disorder
Opioid use disorder (OUD) manifests through a range of signs and symptoms, impacting an individual’s physical, psychological, and social well-being. These signs and symptoms can vary in intensity depending on the severity of the disorder and the individual’s specific circumstances.
Physical Signs and Symptoms
Tolerance:
The need for increasing amounts of opioids to achieve the desired effect or a markedly diminished effect with continued use of the same amount.
Withdrawal:
A characteristic withdrawal syndrome upon cessation or reduction of opioid use, including symptoms such as nausea, vomiting, muscle aches, diarrhea, sweating, insomnia, and anxiety.
Physical Signs of Opioid Use:
These can include constricted pupils, drowsiness, slurred speech, impaired coordination, and constipation.
Overdose:
In severe cases, OUD can lead to opioid overdose, a life-threatening condition characterized by respiratory depression, loss of consciousness, and coma.
Psychological Signs and Symptoms
Cravings:
Intense desires or urges to use opioids, often triggered by environmental cues or internal states.
Loss of Control:
Difficulty controlling the amount and frequency of opioid use, often exceeding intended limits.
Preoccupation with Opioids:
A significant amount of time spent obtaining, using, or recovering from opioid use.
Continued Use Despite Consequences:
Persistent opioid use despite negative consequences on health, relationships, work, or legal standing.
Mood Changes:
OUD can contribute to mood swings, irritability, anxiety, and depression.
Cognitive Impairment:
Chronic opioid use can affect cognitive functions such as memory, concentration, and decision-making.
Social Signs and Symptoms
Neglect of Responsibilities:
Failure to fulfill major role obligations at work, school, or home due to the prioritization of opioid use.
Social Isolation:
Withdrawal from social activities and relationships due to opioid use.
Financial Problems:
Spending excessive amounts of money on opioids, potentially leading to financial difficulties.
Legal Issues:
Engaging in illegal activities to obtain opioids or facing legal consequences related to opioid use.
Recognizing the signs and symptoms of OUD is crucial for early identification and intervention. If you or someone you know is exhibiting these signs, seeking professional help is essential. Remember, OUD is a treatable condition, and with appropriate support and treatment, individuals can achieve recovery and regain control of their lives.[6]
Clinical Examination
Clinical Examination
The clinical examination for Opioid Use Disorder (OUD) involves a comprehensive assessment of the patient’s medical, psychiatric, and social history, along with a thorough physical examination.
Medical History:
- Detailed substance use history: including the type of opioid used, route of administration, frequency, duration, and any prior attempts at cessation.
- Medical comorbidities: such as chronic pain, infectious diseases (e.g., HIV, hepatitis C), and psychiatric disorders (e.g., depression, anxiety).
- Current medications: including any prescribed or over-the-counter medications, as well as any potential interactions with opioids.
- Allergies: to medications or other substances.
- Family history: of substance use disorders or psychiatric illnesses.
Psychiatric History:
- Mental health conditions: including any history of depression, anxiety, bipolar disorder, or other psychiatric disorders.
- Prior treatment: for mental health or substance use disorders.
- Suicidal or homicidal ideation: assessment of current risk and any history of self-harm or violence.
Social History:
- Living situation: including family support, housing stability, and potential exposure to triggers for opioid use.
- Occupational and educational history: including any difficulties related to opioid use.
- Legal history: including any arrests or legal issues related to opioid use.
Physical Examination:
- Vital signs: including blood pressure, heart rate, respiratory rate, and temperature.
- General appearance: noting any signs of intoxication or withdrawal, such as constricted pupils, drowsiness, slurred speech, or agitation.
- Skin examination: checking for needle track marks or other signs of injection drug use.
- Neurological examination: assessing for any cognitive impairment or neurological deficits.
Additional Assessments:
- Urine drug screen: to confirm opioid use and identify other substances.
- Blood tests: to assess liver and kidney function, as well as screen for infectious diseases.
- Psychological assessments: to evaluate mental health status and any co-occurring psychiatric disorders.[7]
Diagnosis
Diagnosis of Opioid Use Disorder
Before treatment, a correct diagnosis must be made on the basis of history, examination (pin-point pupils during intoxication or withdrawal symptoms) and/or laboratory tests.
These tests are:
Naloxone challenge test (to precipitate withdrawal symptoms).
Urinary opioids testing:
With radioimmunoassay (RIA), free radical assay technique (FRAT), thin layer chromatography (TLC), gas-liquid chromatography (GLC), high pressure liquid chromatography (HPLC) or enzyme-multiplied immunoassay technique (EMIT). [2]
Differential Diagnosis
Diffrential Diagnosis
Opioid Use Disorder (OUD) requires a comprehensive differential diagnosis to ensure accurate identification and appropriate treatment.
Some key considerations, as highlighted in a reputable source, include:
Other Substance Use Disorders:
It’s important to ascertain if the patient is also misusing other substances like alcohol, benzodiazepines, or stimulants, as these can complicate the clinical picture and influence treatment decisions.
Pain Disorders:
Chronic pain conditions can mimic or coexist with OUD, necessitating careful assessment to determine the primary driver of opioid use and tailor treatment accordingly.
Mood Disorders:
Depression and anxiety often accompany or precede OUD, making it crucial to differentiate between primary mood disorders and those secondary to opioid use.
Medical Conditions:
Certain medical conditions, particularly those involving the gastrointestinal or endocrine systems, can present with symptoms similar to opioid withdrawal, emphasizing the importance of thorough medical evaluation.[4]
Withdrawal Syndrome
Withdrawal Syndrome of Opioid Use Disorder
The onset of withdrawal symptoms occurs typically within 12-24 hours, peaks within 24-72 hours, and symptoms usually subside within 7-10 days of the last dose of opioid.
The characteristic symptoms include i.e.:
- Lacrimation
- Intense craving for the drug
- Rhinorrhoea
- Pupillary dilation
- Sweating
- Diarrhoea
- Yawning
- Tachycardia
- Mild hypertension
- Insomnia
- Raised body temperature
- Muscle cramps
- Generalised bodyache
- Severe anxiety
- Piloerection
- Nausea
- Vomiting
- Anorexia
In detail; There are marked individual differences in presentation of withdrawal symptoms. Additionally, Heroin withdrawal syndrome is far more severe than the withdrawal syndrome seen with morphine. [2]
Complications
Complications
Biological:
Infections e.g.:
- Abscesses and cellulitis
- Sepsis
- HIV
- Hepatitis B or C
- Bacterial endocarditis
Cardiorespiratory e.g.:
- Deep vein thrombosis or embolism
- Aspiration
- Respiratory depression
- Cardiac arrhythmias
Complications of pregnancy
Death from overdose
Psychological:
Social:
- Unemployment
- Loss of accommodation
- Breakdown of relationships
- Loss of friends
- Criminal record [1]
Investigations
Investigations
The investigation of Opioid Use Disorder (OUD) involves a multi-faceted approach that combines clinical assessment, laboratory testing, and imaging studies to confirm the diagnosis and identify any underlying or co-occurring conditions.
Clinical Assessment
- Thorough History: A comprehensive history is crucial, including the patient’s opioid use patterns, medical and psychiatric history, family history, and social circumstances.
- Physical Examination: A physical exam should focus on identifying signs of opioid intoxication or withdrawal, as well as any physical complications associated with opioid use.
- Mental Status Examination: This evaluates the patient’s cognitive function, mood, and thought processes, which can be impacted by OUD and any co-occurring mental health disorders.
Laboratory Testing
- Urine Drug Screen: This is the most common test to detect recent opioid use and can identify other substances that might be contributing to the patient’s clinical presentation.
- Blood Tests: These may include liver function tests, kidney function tests, complete blood count, and tests for infectious diseases (e.g., HIV, hepatitis C) that can be associated with opioid use.
Imaging Studies
- Brain Imaging: Although not routinely used in the diagnosis of OUD, imaging studies like MRI or PET scans can be helpful in research settings to understand the neurobiological changes associated with opioid addiction. [8]
Treatment
Treatment of Opioid Use Disorder
The treatment can be divided into three main types:
1. Firstly; Treatment of overdose.
2. Secondly; Detoxification.
3. Thirdly; Maintenance therapy.
1. Treatment of Opioid Overdose:
The key clinical findings in a patient who has taken an overdose of opioids are:
- Respiratory depression (rate less than eight breaths per minute), possibly leading to respiratory arrest
- Unreactive pinpoint pupils
- Bradycardia
- Hypotension
- Snoring or other upper airway sounds
- Reduced level of consciousness.
Patients should be approached using the principles of airway, breathing, also circulation and treated with oxygen, respiratory support, fluids, and inotropes if necessary. [1]
An overdose of opioid can treated with narcotic antagonists (such as naloxone, naltrexone). Additionally; Usually an intravenous injection of 2 mg naloxone, followed by a repeat injection in 5-10 minutes, can cause reversal of overdose.
But as naloxone has a short half-life repeated doses may be needed every 1-2 hours. Lastly; This should combined with general care and supportive treatment. [2]
2. Detoxification (Planned withdrawal of opioids):
This is a mode of treatment in which the dependent person is ‘taken off’ opioids. In detail; This is usually done abruptly, followed by management of emergent withdrawal symptoms.
It is highly recommend that detoxification is conduct in a safe manner under expert guidance of a specialist.
The withdrawal symptoms can managed by one of the following methods i.e.:
Use of substitution drugs i.e.:
Such as methadone to ameliorate the withdrawal symptoms. The aim is to gradually taper off the patient from methadone (which is less addicting, has a longer half-life, decreases possible criminal behaviour, and has a much milder withdrawal syndrome).
However, relapses are common and its opponents argue that one type of dependence is often replaced by another (methadone).
Clonidine i.e.:
Basically; It is an α2 agonist that acts by inhibiting norepinephrine release at presynaptic α2 receptors. The usual dose is 0.3-1.2 mg/day, also drug is tapered off in 10-14 days.
It can be started after stoppage of either the opioid itself or the substitution drug (for example; methadone). The important side effects of clonidine are excessive sedation and postural hypotension.
Lastly; Clonidine treatment is usually started in an inpatient psychiatric or specialist alcohol and drug treatment center setting.
Naltrexone with Clonidine i.e.:
Naltrexone is an orally available narcotic antagonist which, when give to an opioid dependent individual, causes withdrawal symptoms. These symptoms are manage with the addition of clonidine for 10-14 days after which clonidine is withdraw and the patient is continue on naltrexone alone.
Now if the person takes an opioid, there are no pleasurable experiences, as the opioid receptors are block by naltrexone.
Therefore, this method is a combination of detoxification and maintenance treatment. The usual dose of naltrexone is 100 mg orally, administered on alternate days.
Other Drugs i.e.:
The other detoxification agents include LAAM (levo-alpha-acetyl-methadol), propoxyphene, diphenoxylate, buprenorphine (long acting synthetic partial μ-agonist which can be administered sublingually), and lofexidine (α2 agonist, similar to clonidine).
In particular, Buprenorphine has recently used widely for detoxification as well as for maintenance treatment in many parts of the World. Care must be exercised as there is potential for misuse with buprenorphine. [2]
When heroin is withdrawn, psychological support is particularly important to avoid immediate relapse. Withdrawal usually undertaken by substituting methadone (a longer-acting drug) for heroin.[1]
3. Maintenance Therapy:
After the detoxification phase is over, the patient is maintain on one of the following regimens:
Methadone maintenance (Agonist substitution therapy) i.e.:
This a very popular method use widely in the Western World. 20-50 mg/day of methadone is give to the patients to ‘shift’ them from ‘hard’ drugs, thus decreasing IV use and criminal behaviour.
Its use in India has not recommended by an expert committee for de-addiction services. Other drugs such as LAAM and buprenorphine can used for maintenance treatment.
Opioid antagonists i.e.:
Opioid antagonists have in use for a long time but they were either partial antagonists (such as n alorphine) or had to administer parenterally (such as naloxone).
Furthermore; The usual maintenance dose is 100 mg on Mondays and Wednesdays, and 150 mg on Fridays.
Naltrexone combine with clonidine, as describe above, is a very effective method for detoxification as well as for maintenance treatment.
Other methods i.e.:
These include individual psychotherapy, behaviour therapy, interpersonal therapy, cognitive behaviour therapy (CBT), motivational enhancement therapy, self-control strategies, psychotropic drugs for associated psychopathology, family therapy, and group therapy (e.g. in therapeutic communities such as Synanon, self-help groups such as Narcotic Anonymous or NA).
These methods have to tailored for use in an individual patient.
Psychosocial rehabilitation i.e.:
This is a very important step in the post-detoxification phase, in the absence of which relapse rates can very high. Rehabilitation should at both occupational and social levels. [2]
Prevention
Prevention
The prevention of Opioid Use Disorder (OUD) is a multifaceted approach that targets various levels of intervention, including individual, community, and policy-based strategies.
Individual-Level Prevention:
- Patient Education: Providing individuals with accurate information about the risks and potential consequences of opioid use can empower them to make informed decisions about pain management and avoid misuse.
- Screening and Brief Intervention: Healthcare providers can screen patients for risk factors and provide brief interventions to address any concerns or early signs of opioid misuse.
- Responsible Opioid Prescribing: Physicians should carefully assess the need for opioids, prescribe the lowest effective dose for the shortest duration, and monitor patients for signs of misuse or addiction.
- Mental Health Support: Addressing underlying mental health conditions, such as depression or anxiety, can reduce the risk of individuals turning to opioids for self-medication.
Community-Level Prevention:
- Public Awareness Campaigns: Raising awareness about the dangers of opioid misuse and the availability of treatment resources can help reduce stigma and encourage individuals to seek help.
- Drug Take-Back Programs: Providing safe and convenient disposal options for unused or expired medications can prevent them from falling into the wrong hands.
- Naloxone Distribution: Increasing access to naloxone, a medication that can reverse opioid overdose, can save lives and prevent overdose deaths.
- Community-Based Support Groups: Offering support groups and peer recovery programs can provide individuals with a safe space to connect with others and receive encouragement in their recovery journey.
Policy-Level Prevention:
- Prescription Drug Monitoring Programs (PDMPs): Implementing and strengthening PDMPs can help identify individuals who are at risk of opioid misuse or overdose by tracking prescription patterns and identifying potential "doctor shopping."
- Regulations on Opioid Manufacturing and Distribution: Stricter regulations on the manufacturing and distribution of opioids can help limit their availability and reduce the potential for diversion.
- Increased Funding for Treatment and Prevention Programs: Investing in evidence-based treatment and prevention programs can expand access to care and support for individuals struggling with OUD.[9]
Homeopathic Treatment
Homoeopathic Treatment of Opioid Use Disorder
While homeopathy is sometimes used as a complementary therapy for opioid use disorder (OUD), there’s no scientific evidence to support its effectiveness as a primary treatment. Conventional medicine, including medication-assisted treatment (MAT) and behavioral therapies, are considered the most effective approaches for OUD.
However, certain homeopathic remedies are suggested for addressing specific symptoms or aspects of OUD, as mentioned in some homeopathic texts. These include:
- Nux Vomica: Often suggested for managing withdrawal symptoms like nausea, vomiting, irritability, and sleep disturbances.
- Avena Sativa: Proposed to reduce cravings and anxiety associated with opioid withdrawal.
- Cannabis Indica: Sometimes used to alleviate restlessness and insomnia during detoxification.
Important note: It’s crucial to emphasize that these remedies lack rigorous scientific evidence and shouldn’t replace conventional treatment for OUD.[10]
Diet & Regimen
Diet & Regimen For Opioid Use Disorder
While there is no specific "Opioid Use Disorder Diet," maintaining a healthy and balanced diet can play a crucial role in supporting recovery and overall well-being for individuals with OUD.
Diet
- Nutrient-rich foods: Incorporate plenty of fruits, vegetables, whole grains, lean proteins, and healthy fats into your diet. These provide essential nutrients that support brain function, energy levels, and overall health.
- Regular meals: Eating regular meals and snacks throughout the day helps stabilize blood sugar levels and reduce cravings.
- Hydration: Staying adequately hydrated is crucial for physical and mental health. Aim to drink plenty of water throughout the day.
- Limit processed foods and sugary drinks: These can contribute to inflammation, mood swings, and energy crashes, which may trigger cravings and hinder recovery.
- Consider supplements: Consult with a healthcare professional about potential supplements that may support recovery, such as vitamin B complex, magnesium, and omega-3 fatty acids.
Regimen:
- Regular exercise: Engaging in regular physical activity can help reduce stress, improve mood, boost energy levels, and promote overall well-being.
- Adequate sleep: Getting enough sleep is essential for physical and mental health. Aim for 7-8 hours of sleep per night.
- Stress management: Incorporate relaxation techniques like meditation, deep breathing exercises, or yoga into your routine to manage stress and reduce the risk of relapse.
- Support groups: Joining a support group or attending therapy sessions can provide valuable support and encouragement during recovery.[11]
Do’s and Don'ts
Do’s & Don’ts
Opioid use disorder Do’s
- Do seek professional help: If you suspect you or someone you know has OUD, reach out to a healthcare provider, addiction specialist, or treatment center. Early intervention is crucial for successful recovery.
- Do be honest and open: During treatment, be honest about your opioid use and any co-occurring mental health conditions. This helps healthcare professionals develop an effective treatment plan.
- Do follow your treatment plan: Adhere to the prescribed medications, therapy sessions, and any other recommended interventions. Consistency is key to overcoming OUD.
- Do attend support groups: Connect with others in recovery through support groups or peer-led programs. Sharing experiences and receiving encouragement can be incredibly beneficial.
- Do practice self-care: Prioritize healthy habits like regular exercise, balanced nutrition, adequate sleep, and stress management techniques. These contribute to overall well-being and reduce the risk of relapse.
- Do be patient and persistent: Recovery is a journey, and setbacks may happen. Stay committed to your treatment plan and don’t give up.
Don’ts of Opioid Use Disorder
Avoiding Risks:
- Don’t self-medicate: Avoid using opioids or other substances to cope with pain, stress, or emotional distress. This can worsen the problem and lead to further complications.
- Don’t share or sell prescription opioids: Sharing or selling prescription medications is illegal and can contribute to the opioid epidemic.
- Don’t isolate yourself: Reach out to supportive friends, family, or professionals if you’re struggling. Isolation can increase the risk of relapse.
- Don’t be afraid to ask for help: If you’re experiencing cravings or struggling with recovery, don’t hesitate to seek help from your healthcare provider or support system.
- Don’t give up: Recovery is possible. Even if you experience setbacks, remember that treatment and support are available to help you get back on track.
Terminology
Terminology For Opioid Used Disorder
The article on Opioid Use Disorder (OUD) employs several key terminologies to describe various aspects of the condition. Here are some of them and their meanings:
Opioid Use Disorder (OUD)
This is the official diagnostic term used to describe a problematic pattern of opioid use leading to clinically significant impairment or distress.
Opioids
These are a class of drugs that include prescription pain relievers (e.g., oxycodone, hydrocodone), heroin, and synthetic opioids (e.g., fentanyl).
Tolerance
This refers to the body’s adaptation to opioids, requiring higher doses to achieve the same effect.
Withdrawal
This is a group of physical and psychological symptoms that occur when opioid use is stopped or decreased abruptly. Symptoms can include nausea, vomiting, muscle aches, anxiety, and insomnia.
Cravings
These are intense desires or urges to use opioids, often triggered by environmental cues or internal states.
Relapse
This refers to the recurrence of opioid use after a period of abstinence.
Medication-Assisted Treatment (MAT)
This is a treatment approach that combines medications (e.g., methadone, buprenorphine, naltrexone) with behavioral therapies to help individuals manage OUD.
Behavioral Therapies
These are therapeutic interventions that help individuals develop coping mechanisms, address underlying psychological issues, and modify behaviors associated with opioid use.
Overdose
This is a life-threatening condition that occurs when a person takes too much of an opioid, leading to respiratory depression and potentially death.
Naloxone
This is a medication that can rapidly reverse the effects of an opioid overdose, potentially saving lives.
Stigma
This refers to negative attitudes and beliefs about people with OUD, which can lead to discrimination and prevent individuals from seeking help.
Recovery
This is an ongoing process of managing OUD and achieving a healthier, more fulfilling life. It involves abstaining from opioid use, addressing underlying issues, and developing coping strategies to prevent relapse.
Understanding these terminologies is crucial for effective communication and collaboration among healthcare professionals, individuals with OUD, and their support systems. It also helps promote accurate information and reduce stigma surrounding OUD.
In homeopathic articles discussing Opioid Use Disorder (OUD), several terminologies are used that may differ from conventional medical terms. Here are some common ones and their meanings within the homeopathic context:
Vital Force
The fundamental energy or life force that animates and sustains the body. Homeopathy aims to stimulate and balance this vital force to promote healing.
Miasm
A predisposition to certain types of diseases or chronic conditions, believed to be inherited or acquired. Homeopaths consider miasms when selecting remedies for OUD, addressing underlying susceptibility.
Totality of Symptoms
The complete picture of the patient’s physical, emotional, and mental symptoms, which guides remedy selection. In OUD, this would include withdrawal symptoms, cravings, and associated psychological distress.
Proving
The process of testing a homeopathic remedy on healthy individuals to identify its characteristic symptoms. This information helps match remedies to patients based on symptom similarity.
Law of Similars
The central principle of homeopathy, stating that a substance that can produce symptoms in a healthy person can cure similar symptoms in a sick person.
Potentization
The process of diluting and succussing (vigorous shaking) a homeopathic remedy to increase its potency. Higher potencies are believed to have deeper and longer-lasting effects.
Constitutional Remedy
A remedy that matches the individual’s overall physical and mental constitution, rather than just specific symptoms. This is often used in chronic conditions like OUD to address underlying predispositions.
Aggravation
A temporary worsening of symptoms after taking a remedy, often considered a positive sign of the remedy’s action.
Detoxification
While similar to the conventional meaning, homeopathy might use remedies to support the body’s natural detoxification processes during withdrawal.
Mind Symptoms
The emotional and mental state of the patient is considered crucial in homeopathy, as it reflects the disturbance in the vital force. In OUD, this could include anxiety, depression, or irritability.
References
References
- Psychiatry, Fourth Edition- Oxford Medical Publications – SRG- by Geddes, Jonathan Price, Rebecca McKnight / Ch 29.
- A Short Textbook of Psychiatry by Niraj Ahuja / Ch 4
- Murthy P, et al. Magnitude of substance use in India: National Survey, 2019. New Delhi: Ministry of Social Justice and Empowerment, Government of India; 2019.
- "Kaplan & Sadock’s Comprehensive Textbook of Psychiatry, 11th Edition, Sadock, Benjamin J.; Sadock, Virginia A.; Ruiz, Pedro, 2019, Wolters Kluwer"
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
- Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), American Psychiatric Association, 2013, American Psychiatric Publishing.
- DSM-5 Clinical Cases, American Psychiatric Association, 2014, American Psychiatric Publishing.
- UpToDate. Opioid use disorder: Clinical features and diagnosis. (Accessed August 10, 2024).
- Substance Abuse: A Comprehensive Textbook, 5th Edition, Lowinson, Joyce H.; Ruiz, Pedro; Millman, Robert B.; Langrod, John G., 2005, Lippincott Williams & Wilkins.
- Homoeopathic Therapeutics in Psychiatry, Farokh J. Master, 2nd Edition, 1998, B. Jain Publishers.
- The Addiction Recovery Skills Workbook, Suzette Glasner-Edwards, 2013, New Harbinger Publications.
Also Search As
Also Search As
People can search for homeopathic articles on opioid use disorder using several methods:
Online Search Engines:
- Use specific keywords: Search for phrases like "homeopathy for opioid use disorder," "homeopathic treatment for opioid addiction," or "homeopathic remedies for opioid withdrawal."
- Include relevant terms: Add terms such as "case studies," "research," or "clinical trials" to narrow down the results to articles with a scientific focus.
Homeopathic Databases and Journals:
- Search specialized databases: Explore databases dedicated to homeopathic research and literature, such as the Homeopathy Research Institute (HRI) library or the National Center for Homeopathy (NCH) publications.
- Browse homeopathic journals: Look for articles in peer-reviewed homeopathic journals, although it’s important to critically evaluate the quality of the evidence presented.
Homeopathic Organizations and Websites:
- Visit websites of homeopathic organizations: Check websites of national or international homeopathic organizations for articles or resources on OUD.
- Consult homeopathic practitioners: Reach out to experienced homeopathic practitioners for recommendations on relevant articles or research.
Libraries and Bookstores:
- Search library catalogs: Use the library’s online catalog to find books or journals on homeopathy and OUD.
- Browse bookstores: Look for books on homeopathy and addiction in bookstores or online retailers.
Important Considerations:
- Critically evaluate sources: When searching for information on homeopathy and OUD, it’s crucial to assess the credibility and reliability of the sources. Look for evidence-based research and avoid relying solely on anecdotal evidence or personal testimonials.
- Consult with healthcare professionals: Before considering any homeopathic treatment for OUD, it’s essential to consult with qualified healthcare professionals, including both conventional and homeopathic practitioners, to ensure a comprehensive and safe approach to treatment.
Remember, homeopathy should not be considered a replacement for conventional medical treatment for OUD. It’s best used as a complementary therapy in conjunction with evidence-based approaches like medication-assisted treatment (MAT) and behavioral therapies.
There are numerous ways to search for information on Opioid Use Disorder (OUD), each offering different types of resources:
Search Engines:
- General Search Engines: Google, Bing, DuckDuckGo, etc. are excellent starting points for broad searches. Use keywords like "opioid use disorder," "opioid addiction," or "opioid treatment" to find a variety of resources, including news articles, websites, and scholarly articles.
- Specialized Search Engines: Consider using specialized search engines like PubMed or Google Scholar to filter your search for scholarly articles and research publications.
Government and Health Organization Websites:
- National Institutes of Health (NIH): The NIH website (https://www.nih.gov/) has a wealth of information on OUD, including research findings, treatment guidelines, and prevention resources.
- Substance Abuse and Mental Health Services Administration (SAMHSA): SAMHSA’s website (https://www.samhsa.gov/) provides resources on OUD, including treatment locators, prevention programs, and publications.
- Centers for Disease Control and Prevention (CDC): The CDC website (https://www.cdc.gov/) offers data and statistics on OUD, as well as prevention and treatment guidelines.
Medical and Academic Databases:
- PubMed: A free database of biomedical and life sciences literature, providing access to scholarly articles on OUD.
- Google Scholar: Another free resource for searching scholarly literature on OUD, including articles, theses, and books.
- University Libraries: University libraries often provide access to subscription-based databases and journals with in-depth information on OUD.
Non-Profit Organizations and Advocacy Groups:
- Shatterproof: This national non-profit organization focuses on ending the addiction crisis, offering resources and information on OUD prevention, treatment, and recovery.
- The Partnership to End Addiction: This organization provides support and resources for families affected by addiction, including OUD.
- National Alliance on Mental Illness (NAMI): NAMI offers information and support for individuals and families affected by mental health conditions, including those co-occurring with OUD.
Social Media and Online Communities:
- Support Groups: Online support groups and forums can provide a safe space for individuals with OUD and their loved ones to connect, share experiences, and offer mutual support.
- Hashtags: Following relevant hashtags on social media platforms like Twitter and Instagram can help you stay updated on the latest news and discussions about OUD.
Frequently Asked Questions (FAQ)
What is Opioid Use Disorder?
Opioids are substances that mimic the effects of endogenous opioids (endorphins and enkephalins) by acting as agonists at the opioid receptors.
Name of the derivatives of Opioid?
- Morphine
- Codeine
- Thebaine
- Noscapine
- Papaverine
- Heroin
- Nalorphine
- Hydromorphone
- Methadone
What are the long-term effects of OUD?
Untreated OUD can lead to serious health complications, including:
- Overdose: A potentially fatal condition requiring immediate medical attention.
- Infectious Diseases: Increased risk of HIV, hepatitis C, and other infections due to needle sharing.
- Cardiovascular Problems: Opioid use can contribute to heart problems and stroke.
- Mental Health Issues: OUD can worsen existing mental health conditions or lead to new ones, such as depression and anxiety.
What is Acute Intoxication of Opioid Use Disorder?
- Apathy
- Bradycardia
- Hypotension
- Respiratory depression
- Subnormal core body temperature
- Pin-point pupils
What is Withdrawal Syndrome of Opioid Use Disorder?
Can homeopathy help with opioid use disorder?
Homeopathy may offer supportive treatment for opioid use disorder by addressing withdrawal symptoms, cravings, and underlying emotional imbalances.
Is homeopathic treatment safe for opioid use disorder?
Homeopathic remedies are generally considered safe when prescribed by a qualified practitioner. However, it’s essential to consult a healthcare professional before starting any new treatment, especially if you’re currently on medication.
Are there specific homeopathic remedies for opioid use disorder?
Yes, remedies like Nux Vomica, Avena Sativa, and Sulphur are commonly used in homeopathy for opioid withdrawal and associated symptoms.
How long does homeopathic treatment for opioid use disorder take?
The duration of homeopathic treatment varies depending on individual needs and the severity of the condition. It’s best to discuss this with your homeopath.
Homeopathic remedies are commonly used for OUD.
Homoeopathic Medicine for Opioid use Disorder
- Nux Vomica: For managing withdrawal symptoms like nausea, vomiting, irritability, and sleep disturbances.
- Avena Sativa: To potentially reduce cravings and anxiety associated with opioid withdrawal.
- Cannabis Indica: To help alleviate restlessness and insomnia during detoxification.
However, it’s important to note that the effectiveness of these remedies lacks rigorous scientific evidence and they shouldn’t replace conventional treatment for OUD.
