Asphyxia Neonatorum
Definition
Asphyxia Neonatorum is a state of anoxia as a result of lack of oxygen and/or deficiency of perfusion to various organs arising from absence of normal respiratory function at birth.[1]
While there aren’t perfect synonyms for "Asphyxia Neonatorum," here are some related terms that capture different aspects of this condition:
Birth asphyxia:
- This is a broader term encompassing any condition where a newborn baby experiences oxygen deprivation during the birthing process.
Perinatal asphyxia:
- This term refers to oxygen deprivation occurring around the time of birth, including both before and after delivery.
Intrapartum asphyxia:
- This specifically refers to oxygen deprivation during labor and delivery.
Neonatal encephalopathy:
- This refers to brain damage caused by oxygen deprivation during birth.
Hypoxic-ischemic encephalopathy (HIE):
- This is a specific type of neonatal encephalopathy caused by a combination of oxygen deprivation and reduced blood flow to the brain.
It’s important to note that some of these terms have slightly different meanings and are used in specific contexts. If you’re unsure which term to use, it’s always best to consult with a medical professional.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do's & Don'ts
Terminology
References
Also Search As
Overview
Overview
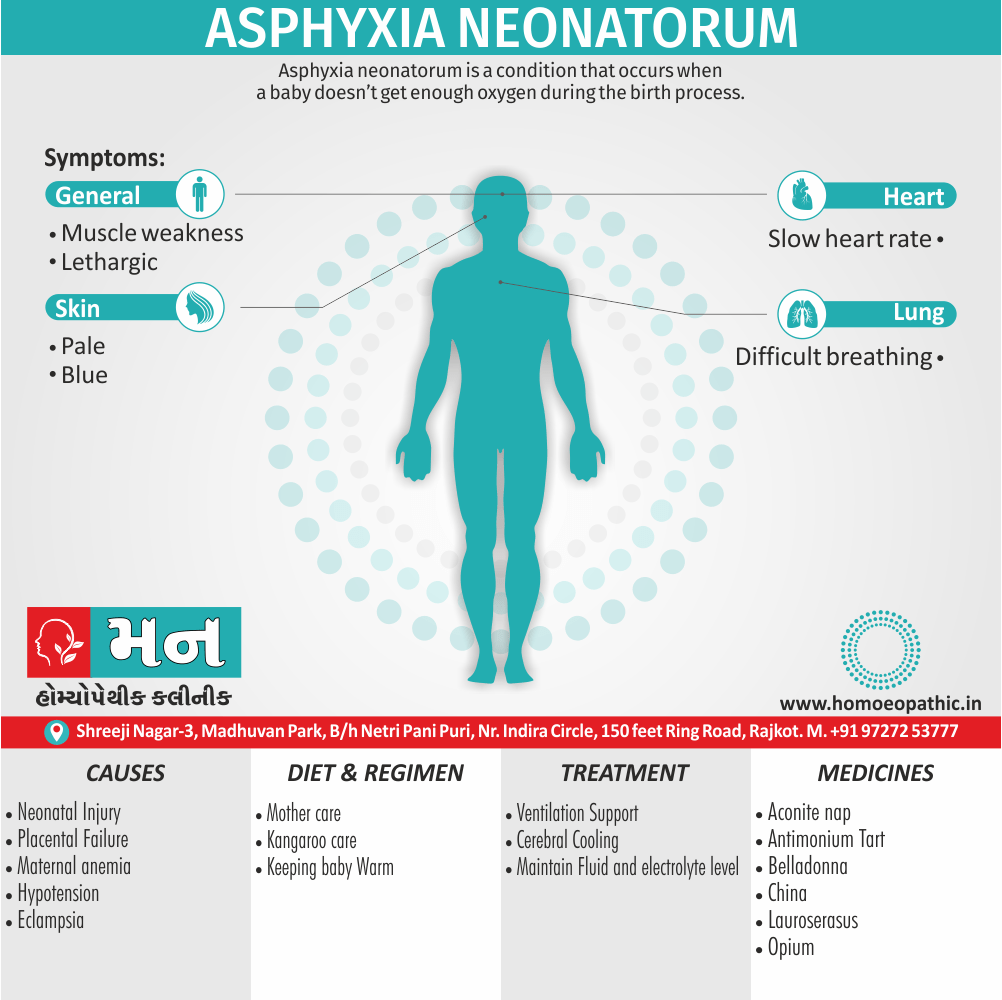
Asphyxia neonatorum is a condition that occurs when a baby doesn’t get enough oxygen during the birth process. It can be fatal. Another more common name for it is perinatal asphyxia, or birth asphyxia. Hypoxic-ischemic encephalopathy may be a result of severe asphyxia neonatorum.
Epidemiology
Epidemiology
The epidemiology of asphyxia neonatorum in India varies across studies, with the following references highlighting key findings:
- IJCMAAS, May 2018: In a rural tertiary care hospital in Tamil Nadu, the highest occurrence of perinatal asphyxia was in the 11-20 years age group (30.92%), followed by 21-30 years (29.21%).[8]
- IJARS, September 2023: Citing Singh A et al., the prevalence of birth asphyxia in the Indian population is approximately 8%, especially among individuals aged 10 to 30 years.[9]
- IJCMR: This study in a tertiary care hospital in North India found the least number of patients in the >50 years age group (4%). The mean age reported in various Indian studies ranges from 20.9 to 30.8 years.[10]
- ResearchGate: This study from a peripheral hospital in Maharashtra found the occurrence of birth asphyxia to be more common in males, with the highest rate in the 20-30 years age group.[11]
- International Journal of Medicine and Medical Research: A study from North-East India found birth asphyxia affected both sexes equally, with a slightly higher incidence in males and a peak during the second and third decades of life.[12]
- Indian Pediatrics, March 1997: Amongst 2371 births (55 fetal deaths and 2316 live births), there were 86 cases of perinatal asphyxia (35 fetal deaths and 51 live births), providing an asphyxia rate of 36.3/1000 births.[13]
- PubMed: Prevalence of birth asphyxia was estimated to be at least 2 per cent (39/1977). Case fatality in these cases was 74 per cent.[14]
Important Considerations:
- The prevalence and demographics of asphyxia neonatorum can vary depending on the region, healthcare setting, and study population.
- It is crucial to consult multiple sources and consider the specific context of each study for a comprehensive understanding.
Causes
Causes of Asphyxia Neonatorum
- Persistence of intrauterine hypoxia (major cause)
- Placental: Functional failure of placenta to function as respiratory organ, e.g. inefficient uteroplacental circulation, early separation of placenta, small size of placenta or its infarction, circumvallate placenta
- Maternal hypoxic states: Anemia, eclampsia, cardiac disease, severe bronchial asthma, hypotension
- Neonatal injury: Prolonged head compression, abnormal lie such as breech or oblique causing increased intracranial pressure and thus asphyxia
- Medications to mother (prenatal and intranasal, e.g. anaesthetic agents, sedatives) depress respiratory centres of the newborn, resulting in continuation of intrauterine asphyxia. [1]
Types
Types
Asphyxia Neonatorum is typically classified based on the timing and severity:
Timing:
- Primary Apnea: This occurs immediately after birth due to inadequate oxygenation during labor or delivery.[15]
- Secondary Apnea: This occurs minutes to hours after birth due to persistent hypoxia or underlying conditions.[16]
Severity:
- Mild Asphyxia: The newborn may require some resuscitation, but there are typically no long-term consequences.[17]
- Moderate Asphyxia: The newborn requires more extensive resuscitation and may experience some short-term complications.[18]
- Severe Asphyxia: The newborn requires prolonged resuscitation and may have significant short-term and long-term complications, including neurological damage.[19]
Additional Classification (Based on Cause):
- Antepartum Asphyxia: Caused by factors occurring before labor onset.[20]
- Intrapartum Asphyxia: Caused by factors during labor and delivery.[21]
It’s important to note that these classifications can overlap, and the severity and type of asphyxia can influence the management and potential outcomes for the newborn.
Risk Factors
Risk Factor of Asphyxia Neonatorum
Premature babies are at increased risk for this condition. Babies born to mothers with conditions that affect pregnancy, such as diabetes mellitus or preeclampsia, are also at greater risk.
Pathogenesis
Pathogenesis
The pathogenesis of asphyxia neonatorum is a complex process that involves multiple factors and pathways. Here are some of the key mechanisms described in reference textbooks:
- Asphyxia disrupts the normal gas exchange, leading to hypoxia (low oxygen) and hypercapnia (high carbon dioxide).
- Hypoxia triggers anaerobic metabolism, resulting in lactic acidosis and cellular energy depletion.
- The combination of acidosis, energy failure, and excitotoxicity (overactivation of neurons) leads to cell damage and organ dysfunction.
- The brain is particularly vulnerable to hypoxic-ischemic injury, which can result in long-term neurological impairment.[15]
- The initial response to asphyxia is primary apnea, characterized by cessation of breathing and bradycardia (slow heart rate).
- If asphyxia persists, gasping respirations may occur, followed by secondary apnea, which is more difficult to reverse.
- The pathophysiology of asphyxia involves a cascade of events, including:
- Decreased oxygen delivery to tissues
- Increased production of lactic acid
- Release of inflammatory mediators
- Cerebral edema and neuronal injury[16]
- Asphyxia can be caused by various factors, including placental insufficiency, umbilical cord compression, maternal hypotension, or airway obstruction.
- The severity of asphyxia depends on the duration and intensity of the insult.
- The pathophysiology involves multiple pathways, including:
- Hypoxic-ischemic encephalopathy (brain injury due to lack of oxygen)
- Multiorgan dysfunction syndrome (failure of multiple organs)
- Coagulopathy (abnormal blood clotting)[17]
Different Pathogenesis
- The pathogenesis of asphyxia is a dynamic process that can vary depending on the underlying cause and the individual response of the newborn.
- Early recognition and prompt intervention are crucial to minimize the long-term consequences of asphyxia.
- The pathophysiology involves a complex interplay between:
- Hypoxia and ischemia
- Inflammation and oxidative stress
- Excitotoxicity and apoptosis (programmed cell death)[18]
- Asphyxia can lead to a spectrum of clinical manifestations, ranging from mild respiratory distress to severe encephalopathy and multiorgan failure.
- The pathophysiology involves a cascade of events that can be triggered by various factors, including:
- Decreased oxygen delivery
- Increased carbon dioxide levels
- Acid-base disturbances
- Electrolyte imbalances[19]
Pathophysiology
Pathophysiology
The pathophysiology of asphyxia generally results from interruption of placental blood flow with resultant fetal hypoxia, hypercarbia, and acidosis.
Circulatory and non-circulatory adaptive mechanisms exist that allow the fetus to cope with asphyxia also preserve vital organ function. With severe and/or prolonged insults, these compensatory mechanisms fail, resulting in hypoxic ischemic injury, leading to cell death via necrosis and apoptosis.
Permanent brain injury is the most severe long-term consequence of perinatal asphyxia. The severity and location of injury is influenced by the mechanisms of injury, including degree also duration, as well as the developmental maturity of the brain.[3]
Clinical Features
Clinical Features
"The clinical features of perinatal asphyxia and HIE are nonspecific.
The most frequent signs are:
- Depressed level of consciousness
- Hypotonia
- Altered respiratory pattern (periodic breathing, gasping respirations, apnea)
- Seizures (often subtle)
- Pupillary and oculomotor abnormalities (unequal, dilated, or poorly reactive pupils)
- Abnormal tone and posture (decerebrate, decorticate)
- Autonomic dysfunction (bradycardia, variable heart rate, poor perfusion)
Signs of multisystem involvement are common and include:
- Renal (oliguria, acute tubular necrosis)
- Gastrointestinal (feeding intolerance, necrotizing enterocolitis)
- Cardiovascular (persistent pulmonary hypertension, myocardial dysfunction, tricuspid insufficiency)
- Hematologic (thrombocytopenia, disseminated intravascular coagulation)
The severity of HIE is classified based on the Sarnat staging system."[16]
Sign & Symptoms
Sign & Symptoms
Your baby may experience immediate symptoms after birth. These can include i.e.:
- Skin that appears pale or blue
- Difficulty breathing, which may cause symptoms such as nasal flaring or abdominal breathing
- A slow heart rate
- Weak muscle tone
The length of time your baby goes without oxygen affects the severity of symptoms. Additionally, The longer a baby is without oxygen, the more likely they are to experience symptoms. Besides this, More severe symptoms can include injury or failure of the:
- Lungs
- Heart
- Brain
- Kidneys
CNS i.e.
- Hypoxic ischemic damage (For instance cortical infarcts, damage to thalamus/ basal ganglia)
- Signs of increased intracranial tension
Renal i.e.
- Acute tubular necrosis
- ADH syndrome GI
- Necrotizing enterocolitis
- Liver damage
Cardiac i.e.
- Transient myocardial ischemia
- MR, TR Lung: e.g. Hemorrhage, oedema, respiratory distress syndrome, meconium aspiration
Hematological i.e.
DIC [1]
Clinical Examination
Clinical Examination
Physical Examination
Vitals
Respiratory Rate i.e.
Poor respiratory effort
Skin i.e.
Poor color (cyanosis)
Neurology i.e.
Poor muscle tone
Miscellaneous i.e.
Low Apgar score. If resuscitation is successful, the infant is usually transferred to a neonatal intensive care unit.[4]
Diagnosis
Diagnosis of Asphyxia Neonatorum
Diagnostic criteria for asphyxia neonatorum i.e.
- Signs of fetal distress
- Acute metabolic acidosis
- Apgar score at 5 minutes < 5
Your baby will receive an Apgar score about 1 to 5 minutes after birth.
The scoring system have factors i.e.:
- Breathing
- Pulse
- Appearance
- Response to stimulus
- Muscle tone
Each factor gets a score of 0, 1, or 2. The highest score possible is 10. A baby with a lower Apgar score after 5 minutes has a higher risk for asphyxia neonatorum. Furthermore, A score lower than 7 can indicate that a baby doesn’t have enough oxygen. The doctor may suspect your baby has asphyxia neonatorum if they have an Apgar score of 3 or lower for more than 5 minutes.
A doctor may also test a baby’s blood for high acid levels. This can indicate poor oxygenation. A doctor may also order blood tests to see if a baby’s kidneys, heart, and liver might be affected.
- Initiation of respiration > 5 minutes
- Features of ischemic hypoxic encephalopathy
- Multiorgan damage Note: Any four of the above
Factors of poor prognosis
- Prolonged duration also severe asphyxia
- Seizures
- Raised intracranial pressure
- Persistent oliguria
- CT brain shows hypodensities [1]
Differential Diagnosis
Differential Diagnosis of Asphyxia Neonatorum
- acute hemorrhage
- depression from maternal anesthesia or analgesia
- infection
- cardiac or pulmonary disorders
- trauma
- neurological disorders
- metabolic diseases.[6]
Complications
Complications
"The major complications of perinatal asphyxia and HIE include:
- Hypoxic-ischemic encephalopathy (HIE)
- Seizures
- Cerebral palsy
- Cognitive deficits
- Multiorgan dysfunction (renal, gastrointestinal, cardiovascular, hematologic)
- Death
The severity of the complications is related to the severity of the asphyxial insult and the effectiveness of resuscitation and supportive care."[16]
Investigations
Investigation
- Diagnostic techniques such as head ultrasound (HUS), CT scan and MRI will reveal areas of the brain that have been affected.
- An electroencephalogram (EEG) will be done to determine the amount and quality of brain activity. Additional tests may also be performed, focusing on the premature baby’s sensory responses.
- Tests on hearing and sight, for example, may give an indication that damage has or has not occurred to cells within the brain.[5]
Treatment
Treatment of Asphyxia Neonatorum
The severity of your baby’s symptoms influences the treatment. The timing of when your baby receives the diagnosis also affects their treatment. For example, mothers may receive additional oxygen before delivery to boost a baby’s oxygenation before birth. A cesarean delivery is a potential preventive measure in prolonged or difficult deliveries.
After birth, babies with the condition may need ventilation to support their breathing. Keeping babies warm has also been shown to reduce harmful effects. Doctors will also monitor the baby’s blood pressure and fluid intake to make sure they’re getting enough oxygen.
Some babies can experience seizures as a result of asphyxia neonatorum. Doctors should carefully treat these babies to avoid injury from seizures.
- IV fluids
- Warmth
- Management of cerebral oedema
- Symptomatic treatment of seizures, hypoglycemia, hypocalcemia
- Cerebral cooling [1]
Prevention
Prevention of Asphyxia Neonatorum
Preventing birth asphyxia can be difficult because the condition can happen suddenly and without warning.
According to a 2019 article, proper care and monitoring before and after every birth are vital, particularly in settings where fewer resources are available. Steps may include:
- effective resuscitation
- controlling body temperature
- ensuring that the correct equipment is available
- having properly trained and skilled healthcare providers present for every birth
- pretreatment with certain medications, such as barbiturates, to reduce the risk of brain injury
- treatments, such as body cooling, to prevent secondary complications from asphyxia due to damaged cells releasing toxins[7]
Homeopathic Treatment
Homeopathic Treatment of Asphyxia Neonatorum
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Asphyxia Neonatorum:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Aconite nap
Especially medicines for Asphyxia neonatorum. Apoplectic from, the babe is hot, purple-hued, pulseless also breathless, or nearly so.[2]
Antimonium Tart
Suffocative form; rattling of mucus in throat; child pale and breathless, although the cord still pulsates.
Belladonna
Apoplectic form; face very red, eyeballs injected, pupils dilated.
China
Syncope, after profuse hemorrhage
Lauroserasus
Face blue, with gasping for breath also nearly imperceptible breathing; twitching of muscles of the face.
Opium
Pale and breathless, cord still pulsates.[2]
Diet & Regimen
Diet & Regimen
Nutritional Support:
- Early initiation of enteral feeding (breast milk preferred) is crucial, but may be delayed if the infant has significant respiratory distress or neurological instability.
- Parenteral nutrition may be necessary if enteral feeding is not tolerated.
- Close monitoring of fluid and electrolyte balance is essential.
Neurological Support:
- Hypothermia therapy may be indicated for moderate to severe hypoxic-ischemic encephalopathy (HIE).
- Seizures should be treated promptly with anticonvulsants.
- Supportive care for other neurological complications, such as cerebral palsy, may be necessary.
Other Considerations:
- The infant’s respiratory and cardiovascular status should be closely monitored.
- Careful attention should be paid to maintaining a neutral thermal environment.
- The infant should be protected from infection.[16]
Do's & Don'ts
Do’s & Don’ts
Do’s
- Do initiate resuscitation promptly and effectively according to neonatal resuscitation guidelines.
- Do provide supportive care, including maintaining adequate oxygenation, ventilation, and perfusion.
- Do consider hypothermia therapy for moderate to severe HIE.
- Do monitor for and treat seizures promptly.
- Do initiate early enteral feeding (breast milk preferred) when the infant is stable.
- Do monitor for and manage complications, such as multiorgan dysfunction.
- Do provide ongoing developmental support and follow-up care.
Don’ts
- Don’t delay resuscitation or provide inadequate support.
- Don’t overstimulate the infant, as this can increase oxygen demand and worsen brain injury.
- Don’t neglect to monitor for and treat seizures, as they can cause further brain damage.
- Don’t delay initiation of feeding when the infant is stable, as early nutrition is crucial for recovery.
- Don’t overlook the potential for long-term complications and the need for ongoing care.[16]
Terminology
Terminology:
- Asphyxia Neonatorum: The condition where a newborn doesn’t receive enough oxygen around the time of birth.
- Anoxia: Complete absence of oxygen supply to an organ or tissue.
- Hypoxia: Reduced oxygen supply to an organ or tissue.
- Perfusion: The process of blood flow delivering oxygen and nutrients to organs and tissues.
- Primary Apnea: The initial cessation of breathing immediately after birth due to lack of oxygen.
- Secondary Apnea: Cessation of breathing occurring minutes to hours after birth due to persistent hypoxia.
- Hypoxic-Ischemic Encephalopathy (HIE): Brain damage resulting from a combination of oxygen deprivation and reduced blood flow.
- Apgar Score: A quick assessment of a newborn’s health at 1 and 5 minutes after birth, evaluating heart rate, breathing, muscle tone, reflexes, and color.
- Intrauterine: Within the uterus.
- Placental Insufficiency: When the placenta doesn’t function properly to provide oxygen and nutrients to the fetus.
- Umbilical Cord Compression: Pressure on the umbilical cord, restricting blood flow to the fetus.
- Maternal Hypotension: Low blood pressure in the mother, potentially reducing blood flow to the placenta.
- Excitotoxicity: Overactivation of neurons leading to cell damage.
- Apoptosis: Programmed cell death.
- Necrosis: Cell death due to injury.
- Parenteral Nutrition: Delivery of nutrients through a vein when a baby cannot be fed orally.
Additional Terms from the Overview and FAQ Sections:
- Birth Asphyxia: A broader term referring to any oxygen deprivation around the time of birth.
- Perinatal Asphyxia: Similar to birth asphyxia, referring to oxygen deprivation around the time of birth.
- Intrapartum Asphyxia: Oxygen deprivation specifically during labor and delivery.
- Neonatal Encephalopathy: Brain damage in newborns, often caused by oxygen deprivation.
References
References
- https://www.healthline.com/health/asphyxia-neonatorum#treatment
- Homoeopathic Therapeutics by Lilienthal
- https://pubmed.ncbi.nlm.nih.gov/27524444/#:~:text=The%20pathophysiology%20of%20asphyxia%20generally,and%20preserve%20vital%20organ%20function.
- https://wikidoc.org/index.php/Perinatal_asphyxia_physical_examination
- https://www.aboutkidshealth.ca/article?contentid=1808&language=english
- https://jpnim.com/index.php/jpnim/article/viewFile/030269/214
- https://www.medicalnewstoday.com/articles/birth-asphyxia#prevention
- IJCMAAS, May 2018
- IJARS, September 2023
- IJCMR
- ResearchGate
- International Journal of Medicine and Medical Research
- Indian Pediatrics, March 1997
- PubMed
- Nelson Textbook of Pediatrics, 21st Edition (2020), Robert Kliegman et al.
- Cloherty and Stark’s Manual of Neonatal Care, 8th Edition (2018), Anne R. Hansen et al.
- Fanaroff and Martin’s Neonatal-Perinatal Medicine, 11th Edition (2020), Richard J. Martin et al.
- Avery’s Diseases of the Newborn, 10th Edition (2018), Christine A Gleason et al.
- Neonatology: Management, Procedures, On-Call Problems, Diseases, and Drugs, 7th Edition (2018), Tricia Lacy Gomella et al.
- Williams Obstetrics, 25th Edition (2018), F. Gary Cunningham et al.
- Creasy and Resnik’s Maternal-Fetal Medicine: Principles and Practice, 8th Edition (2019), Robert Resnik et al.
Also Search As
Also Search As
People can search for the article "Asphyxia Neonatorum" using various methods:
1. Search Engines (Google, Bing, etc.):
- Directly type the term: Simply enter "Asphyxia Neonatorum" into the search bar.
- Use related terms: Search for "birth asphyxia," "perinatal asphyxia," or "neonatal encephalopathy."
- Specify the type of information: Add words like "homeopathic treatment," "causes," "symptoms," or "prevention" to your search query.
2. Online Medical Resources:
- Reputable websites: Look for articles on websites like the Mayo Clinic, WebMD, MedlinePlus, or the National Institutes of Health (NIH).
- Medical journals: Search databases like PubMed or Google Scholar for scientific articles and research papers.
3. Social Media:
- Hashtags: Look for relevant hashtags on platforms like Twitter, Facebook, or Instagram, such as #asphyxianeonatorum, #birthasphyxia, or #neonatalhealth.
4. Libraries:
- Medical textbooks: Consult textbooks like Cloherty and Stark’s Manual of Neonatal Care or Nelson Textbook of Pediatrics.
- Ask a librarian: They can assist you in finding relevant books or articles.
Tips for Effective Searching:
- Use specific keywords: Instead of just "Asphyxia Neonatorum," try "Asphyxia Neonatorum homeopathic treatment" or "Asphyxia Neonatorum risk factors."
- Combine terms: Use Boolean operators like AND, OR, and NOT to refine your search.
- Look for reliable sources: Prioritize websites and publications from reputable medical organizations or universities.
There are several ways to search for information on Asphyxia Neonatorum:
1. Online Search Engines:
Google: This is the most common way to search for information online. Simply type "Asphyxia Neonatorum" into the search bar and you’ll get a variety of results, including articles, research papers, and websites.
Other Search Engines: You can also use other search engines like Bing, DuckDuckGo, or Yahoo to find information.
2. Medical Websites and Databases:
Reputable Health Websites: Websites like Mayo Clinic, WebMD, MedlinePlus, and the National Institutes of Health (NIH) offer reliable information on medical conditions, including Asphyxia Neonatorum.
Medical Journals: PubMed and Google Scholar are excellent resources for finding scientific articles and research papers on the topic.
3. Social Media:
- Medical Groups and Forums: Facebook groups or online forums dedicated to neonatal health or parenting may have discussions or resources related to Asphyxia Neonatorum.
4. Libraries:
Medical Textbooks: Libraries often have medical textbooks, like Cloherty and Stark’s Manual of Neonatal Care or Nelson Textbook of Pediatrics, that provide detailed information on the condition.
Ask a Librarian: Librarians can help you find relevant books and articles on the topic.
Tips for Effective Searching:
Use Specific Keywords: Instead of just searching for "Asphyxia Neonatorum," use more specific terms like "Asphyxia Neonatorum causes," "Asphyxia Neonatorum treatment," or "Asphyxia Neonatorum complications."
Use Boolean Operators: Combine search terms using words like "AND," "OR," and "NOT" to refine your search. For example, search for "Asphyxia Neonatorum AND treatment" to find articles specifically about treatment options.
Evaluate the Source: Make sure the information you find comes from a credible source, such as a reputable medical organization, government website, or peer-reviewed journal. Be wary of information from personal blogs or websites that are not backed by medical professionals.
Frequently Asked Questions (FAQ)
What is Asphyxia Neonatorum?
Asphyxia Neonatorum is a state of anoxia as a result of lack of oxygen and/or deficiency of perfusion to various organs arising from absence of normal respiratory function at birth.
How is Asphyxia Neonatorum diagnosed?
Diagnosis
Diagnosis involves assessing the baby’s Apgar score, blood tests to check for acidosis (high acid levels), and sometimes imaging studies of the brain.
Can Asphyxia Neonatorum be prevented?
Prevention
While not all cases can be prevented, close monitoring during pregnancy and labor, prompt intervention during delivery, and effective resuscitation can significantly reduce the risk and severity of the condition.
Can homeopathy treat Asphyxia Neonatorum?
Homoeopathy for Asphyxia Neonatorum
Homeopathy is a complementary therapy that some parents explore for supporting newborns with asphyxia neonatorum. It aims to address the underlying causes and symptoms using natural remedies.
What are the causes of Asphyxia Neonatorum?
- Persistence of intrauterine hypoxia (major cause)
- Placental
- Maternal hypoxic states
- Neonatal injury
- Medications to mother
What are the symptoms of Asphyxia Neonatorum?
- Skin that appears pale or blue
- Difficulty breathing, which may cause symptoms such as nasal flaring or abdominal breathing
- A slow heart rate
- Weak muscle tone
Is homeopathy safe for newborns with Asphyxia Neonatorum?
Homeopathic remedies, when prescribed by a qualified practitioner, are generally considered safe for newborns. However, it’s crucial to consult with both a homeopathic practitioner and a medical doctor for a comprehensive treatment plan.
What are the potential complications of Asphyxia Neonatorum?
Complications
Complications can range from mild to severe and may include hypoxic-ischemic encephalopathy (brain damage), developmental delays, cerebral palsy, and in rare cases, death.
How does homeopathic treatment differ from conventional medical approaches?
Homeopathy
focuses on the whole individual, aiming to stimulate the body’s natural healing abilities, while conventional medicine typically focuses on addressing the immediate physiological issues.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Asphyxia Neonatorum?
Homoeopathic Medicine for Asphyxia Neonatorum
- Aconite nap
- Antimonium Tart
- Belladonna
- China
- Lauroserasus
- Opium
