Coma
Definition
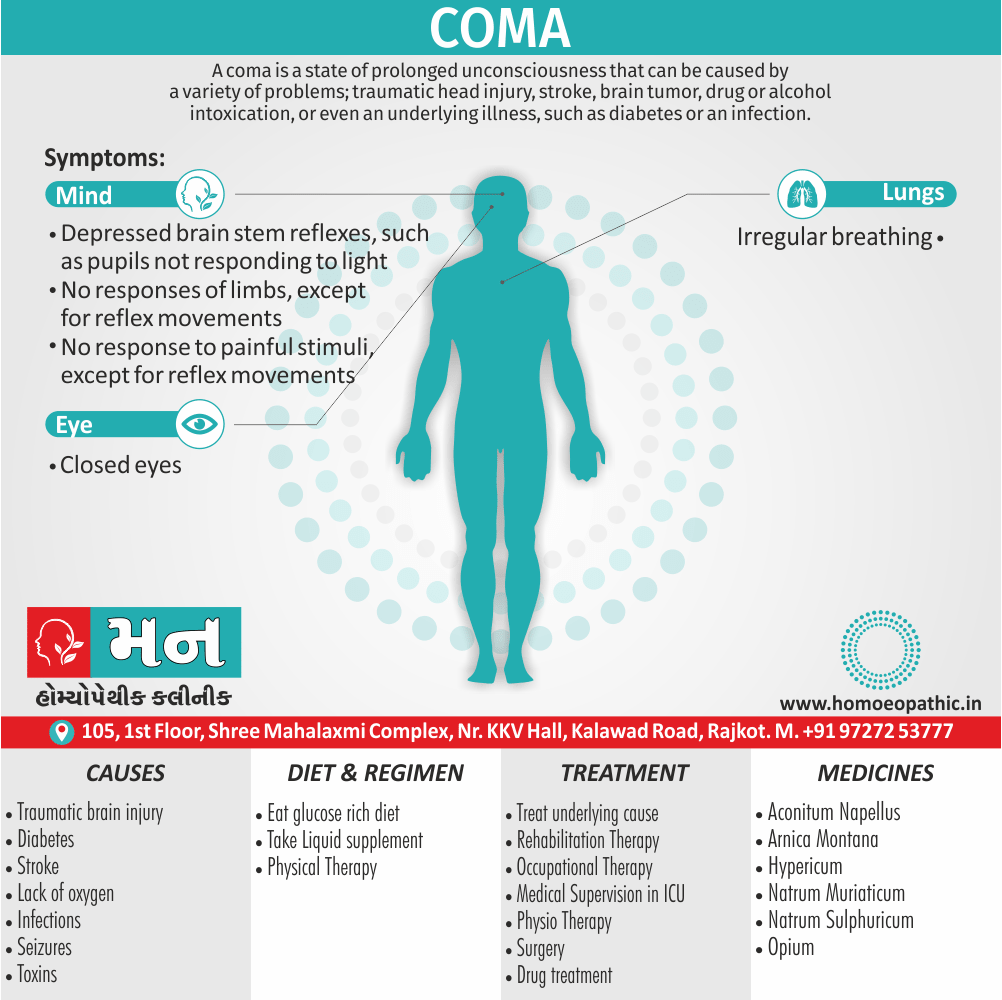
A coma is a state of prolonged unconsciousness that can be caused by a variety of problems; traumatic head injury, stroke, brain tumor, drug or alcohol intoxication, or even an underlying illness, such as diabetes or an infection. [1]
The best synonym for coma depends on the specific aspect you want to emphasize. Here are some options:
State of unconsciousness:
- Oblivion
- Stupor
- Trance
- Blackout
- Insensibility
Deep sleep-like state:
- Slumber
- Sleep
- Somnolence
Suspended animation:
- Dormancy
- Torpor
- Hibernation
- Suspended animation
Figurative (non-medical):
- Stagnant
- Impasse
- Dormancy
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
- Coma is different from sleep because the person is unable to wake up.
- Moreover, It is not the same as brain death. The person is alive, but they cannot respond in the normal way to their environment.
- Whether or not they are conscious, or how many people are conscious during a coma, or the level of consciousness, is a question that scientists are currently investigating.
- Levels of consciousness also responsiveness will depend on how much of the brain is functioning.
- A coma often lasts for a few days or weeks. occasionally, it can last for several years.
Medical Emergency
- In general, If a person enters a coma, this is a medical emergency.
- Rapid action may be needed to preserve life also brain function.
- They do not respond to pain, either light, or sound in the usual way, and they do not make voluntary actions.
- Although they do not wake up, their body follows normal sleep patterns.
- Automatic functions, for example, breathing and circulation, normally continue to function, but the person’s thinking ability is suppressed.
- According to the National Institutes of Neurological Disorders and Stroke (in other words, NINDS), the person may sometimes grimace, laugh, or cry as a reflex. [2]
Epidemiology
Epidemiology
A recent national survey published in 2023 in Neurocritical Care examined the epidemiology of coma in India. The study, titled "A National Survey on Coma Epidemiology, Evaluation, and Therapy in India: Revisiting the Curing Coma Campaign Come Together Survey," found that traumatic brain injury (TBI) was the most common cause of coma, followed by ischemic stroke and intracerebral hemorrhage. The survey also revealed that the Glasgow Coma Scale (GCS) and neurological examination were the most commonly used tools for assessing coma in India.[12]
Additionally, a 2020 article in the Indian Journal of Critical Care Medicine titled "The Curing Coma Campaign®: Concerns in the Indian Subcontinent" highlighted the lack of comprehensive epidemiological data on coma and disorders of consciousness (DOC) in India. The article emphasized the need for further research to better understand the prevalence and etiology of coma in the Indian population.[13]
Causes
Causes
Many types of problems can cause coma. Some examples are:
Traumatic brain injuries:
- Road traffic accidents, sports injuries, also violent attacks that involve a blow to the head can cause coma. [2]
- When the brain swells as a result of trauma, the fluid pushes up against the skull.
- The swelling may eventually cause the brain to push down on the brain stem, which can damage the RAS (Reticular Activating System) a part of the brain that’s responsible for arousal and awareness. [3]
Stroke:
- Reduced or interrupted blood supply to the brain (i.e. stroke), which may be caused by blocked arteries or a burst blood vessel, can result in a coma.
Tumors:
- Tumors either in the brain or brain stem can cause a coma. [1]
Diabetes:
- In people with diabetes, blood sugar levels that become too high (hyperglycemia) or too low (hypoglycemia) can cause a coma. [1]
- This type of coma is usually reversible once the blood sugar is corrected. [3]
Lack of oxygen:
- Oxygen is essential for brain function.
- Cardiac arrest causes a sudden cut off of blood flow and oxygen to the brain, called hypoxia or anoxia.
- After cardiopulmonary resuscitation (in other words, CPR), survivors of cardiac arrest are often in comas.
- Oxygen deprivation can also occur with drowning or choking. [3]
Infections:
- Infections such as encephalitis and meningitis cause swelling (in other words, inflammation) of the brain, spinal cord or the tissues that surround the brain.
- Severe cases of these infections can result in either brain damage or a coma. [1]
Bleeding:
- Bleeding in the layers of the brain may cause coma due to swelling and compression on the injured side of the brain.
- This compression causes the brain to shift, causing damage to the brain stem also the RAS.
- High blood pressure, cerebral aneurysms, also tumors are non-traumatic causes of bleeding in the brain. [3]
Seizures:
- A single seizure rarely produces coma. But continuous seizures called status epilepticus can produce coma.
- Repeated seizures can prevent the brain from recovering in between seizures.
- This will cause prolonged unconsciousness also coma. [3]
Toxins:
- Substances that are normally found in the body can accumulate to toxic levels if the body fails to dispose of them correctly.
- As an example, ammonia due to liver disease, carbon dioxide from a severe asthma attack, or urea from kidney failure can accumulate to toxic levels in the body.
Drugs and alcohol:
- Drugs and alcohol in large quantities can also disrupt neuron functioning in the brain. [3]
Types
Types of coma
- Toxic-metabolic encephalopathy- This is an acute condition of brain dysfunction with symptoms of confusion and/or delirium. The condition is usually reversible. The causes of toxic-metabolic encephalopathy are varied. They include systemic illness, infection, organ failure, and other conditions.
- Persistent vegetative state- This is a state of severe unconsciousness. The person is unaware of their surroundings and incapable of voluntary movement. With a persistent vegetative state, someone may progress to wakefulness but with no higher brain function. With persistent vegetative state, there is breathing, circulation, and sleep-wake cycles.
- Medically induced: This type of temporary coma, or deep state of unconsciousness, is used to protect the brain from swelling after an injury – and allow the body to heal. The patient receives a controlled dose of an anesthetic, which causes lack of feeling or awareness. Doctors then closely watch the person’s vitals. This happens only in hospital intensive care units.(7)
Risk Factors
Risk factor of Coma
- A hemorrhagic or ischemic stroke
- A severe head injury
- Seizures
- Brain tumor
- Brain infections
- Hypoxia for a long time
- Metabolic abnormalities, such as diabetic hyperosmolar coma, hypoglycemia
- Toxins, including poisons, alcohol and other drugs (barbiturates, sedatives, amphetamines,cocaine)
- Liver failure or kidney failure (6)
Pathogenesis
Pathogenesis
The pathogenesis of coma is described as a result of bilateral dysfunction of the cerebral hemispheres or dysfunction of the ascending reticular activating system (ARAS) in the brainstem.
The book "Plum and Posner’s Diagnosis and Treatment of Stupor and Coma" explains that coma can arise from various causes, including:
- Structural lesions: These can be supratentorial (e.g., bilateral hemispheric strokes, tumors, or traumatic brain injury) or infratentorial (e.g., brainstem strokes, tumors, or hemorrhage).
- Metabolic disturbances: These can be caused by hypoxia, hypoglycemia, hyperglycemia, electrolyte imbalances, liver failure, kidney failure, or toxic ingestions.
- Infections: These can affect the brain (encephalitis, meningitis) or the systemic circulation (sepsis).
- Other causes: These include seizures, hypothermia, hyperthermia, and severe hypotension.
The book emphasizes that understanding the underlying pathophysiology of coma is crucial for accurate diagnosis and appropriate management.[14]
Pathophysiology
Pathophysiology of Coma
Clinical Features
Clinical Features
The clinical features of coma are described as follows:
- Loss of consciousness: The patient is unresponsive to external stimuli, including verbal commands, pain, or light.
- Alterations in breathing patterns: Breathing may be irregular, slow, or rapid. Specific patterns like Cheyne-Stokes respiration or central neurogenic hyperventilation may be observed.
- Pupillary abnormalities: Pupils may be dilated, pinpoint, or unequal in size. They may also be unreactive to light.
- Ocular movements: Eyes may be roving, fixed in a certain position, or exhibit specific movements like ocular bobbing or skew deviation.
- Motor responses: Motor responses to pain can vary from flaccid paralysis to decorticate or decerebrate posturing.
- Reflex changes: Deep tendon reflexes may be increased, decreased, or absent. Pathological reflexes like the Babinski sign may be present.
The book "Adams and Victor’s Principles of Neurology" emphasizes that the specific clinical features of coma can vary depending on the underlying cause and the extent of brain dysfunction. A thorough neurological examination is essential for accurate diagnosis and appropriate management.[15]
Sign & Symptoms
Sign & Symptoms
The signs and symptoms of a coma commonly i.e.:
- Closed eyes
- Depressed brain stem reflexes, such as pupils not responding to light
- Furthermore, No responses of limbs, except for reflex movements
- Besides this, No response to painful stimuli, except for reflex movements
- Irregular breathing [1]
Before entering a coma, a person with worsening hypoglycemia (low blood sugar), or hypercapnia (higher blood CO2 levels), for example, will first experience mild agitation.
Without treatment, their ability to think clearly will gradually decrease.
Finally, they will lose consciousness. [2]
Clinical Examination
Clinical examination of Coma
- The severity of coma impairment is categorized into several levels. Patients may or may not progress through these levels. In the first level, the brain responsiveness lessens, normal reflexes are lost, the patient no longer responds to pain and cannot hear.
- Contrary to popular belief, a patient in a coma does not always lie still and quiet. They may move, talk, and perform other functions that may sometimes appear to be conscious acts but are not.
- Two scales of measurement often used in TBI diagnosis to determine the level of coma are the Glasgow Coma Scale (GCS) and the Ranchos Los Amigos Scale(RLAS).
- The GCS is a simple 3 to 15-point scale (3 being the worst and 15 being that of a typical person) used by medical professionals to assess severity of neurologic trauma, and establish a prognosis.
- The RLAS is a more complex scale that has eight separate levels, and is often used in the first few weeks or months of coma while the patient is under closer observation, and when shifts between levels are more frequent.(6)
Diagnosis
Diagnosis
A medical and recent history, blood tests, physical tests, also imaging scans can help find out the cause of a coma, also this helps decide which treatment to apply.
Medical history:
Friends, family, police, and witnesses, if appropriate, may be asked:
- Whether the coma or symptoms beforehand started either slowly or suddenly
- If the person had or appeared to have any vision problems, dizziness, stupor or numbness before the coma
- Whether the patient has diabetes, any history of seizures or stroke, or any other condition or disease
- What medications or other substances the patient may have been taken
Physical tests i.e.:
- Generally, the aim is to check the person’s reflexes, how they respond to pain, also their pupil size.
- Tests may involve squirting either very cold or warm water into the ear canals.
- These tests will trigger varying reflexive eye movements.
- The type of response varies according to the cause of the coma.
Blood tests:
These will be taken to determine i.e.:
- Blood count
- Signs of carbon monoxide poisoning
- Presence and levels of either legal or illegal drugs or other substances
- Levels of electrolytes
- Glucose levels
- Liver function
Lumbar puncture (in other words, spinal tap):
This can check for any infection or disorder of the CNS.
The doctor inserts a needle into the patient’s spinal canal, measures pressure, also extracts fluid to send for tests.
Imaging scans of the brain:
- These will help determine whether there is any either brain injury or damage, and where.
- A CT or CAT scan or an MRI will check for blockages or other abnormalities.
- An electroencephalography (in other words, EEG) will measure electrical activity within the brain.
Glasgow Coma Scale:
- The scale is used as part of the initial evaluation of a patient, but does not assist in making the diagnosis as to the cause of coma.
- Since it "scores" the level of coma, the GCS can be used as a standard method for any health-caregiver to assess change in patient status. [4]
- The Glasgow Coma Scale (in other words, GCS) can be used to assess the severity of brain damage following a head injury.
- It gives patients a score, according to verbal responses, physical responses, also how easily they can open their eyes.
Glasgow Coma Scale | |
Eye Opening | |
| Spontaneous | 4 |
| To loud voice | 3 |
| To pain | 2 |
| None | 1 |
Verbal Response | |
| Oriented | 5 |
| Confused, Disoriented | 4 |
| Inappropriate words | 3 |
| Incomprehensible words | 2 |
| None | 1 |
Motor Response | |
| Obeys commands | 6 |
| Localizes pain | 5 |
| Withdraws from pain | 4 |
| Abnormal flexion posturing | 3 |
| Extensor posturing | 2 |
| None | 1 |
[4]
Differential Diagnosis
Differential diagnosis of Coma
- Structural abnormality
- Seizure
- Encephalitis
- Metabolic derangements
- Toxicologic etiologies.(9)
Complications
Complications
The complications of coma are described as follows:
Respiratory complications: These include aspiration pneumonia, atelectasis, and respiratory failure due to impaired airway protection and decreased respiratory drive.
Cardiovascular complications: These include hypotension, arrhythmias, and deep vein thrombosis due to immobility and autonomic dysfunction.
Neurological complications: These include pressure ulcers, seizures, and muscle contractures due to prolonged immobility and altered neurological function.
Nutritional complications: These include malnutrition and dehydration due to the inability to eat or drink.
Infections: These include urinary tract infections, pneumonia, and sepsis due to impaired immune function and the use of invasive devices.
The book "Critical Care Medicine: Principles of Diagnosis and Management in the Adult" emphasizes that the risk of complications in coma patients is high and requires vigilant monitoring and preventive measures to minimize morbidity and mortality. Early mobilization, nutritional support, and meticulous skin care are essential components of coma management.[16]
Investigations
Investigations
Blood tests:
These will be taken to determine i.e.:
- Blood count
- Signs of carbon monoxide poisoning
- Presence and levels of either legal or illegal drugs or other substances
- Levels of electrolytes
- Glucose levels
- Liver function
Lumbar puncture (in other words, spinal tap):
This can check for any infection or disorder of the CNS.
The doctor inserts a needle into the patient’s spinal canal, measures pressure, also extracts fluid to send for tests.
Imaging scans of the brain:
- These will help determine whether there is any either brain injury or damage, and where.
- A CT or CAT scan or an MRI will check for blockages or other abnormalities.
- An electroencephalography (in other words, EEG) will measure electrical activity within the brain.
Glasgow Coma Scale:
- The scale is used as part of the initial evaluation of a patient, but does not assist in making the diagnosis as to the cause of coma.
- Since it "scores" the level of coma, the GCS can be used as a standard method for any health-caregiver to assess change in patient status. [4]
- The Glasgow Coma Scale (in other words, GCS) can be used to assess the severity of brain damage following a head injury.
- It gives patients a score, according to verbal responses, physical responses, also how easily they can open their eyes.
Glasgow Coma Scale | |
Eye Opening | |
| Spontaneous | 4 |
| To loud voice | 3 |
| To pain | 2 |
| None | 1 |
Verbal Response | |
| Oriented | 5 |
| Confused, Disoriented | 4 |
| Inappropriate words | 3 |
| Incomprehensible words | 2 |
| None | 1 |
Motor Response | |
| Obeys commands | 6 |
| Localizes pain | 5 |
| Withdraws from pain | 4 |
| Abnormal flexion posturing | 3 |
| Extensor posturing | 2 |
| None | 1 |
Treatment
Treatment of Coma
- Treatment for a coma depends on the cause.
- Moreover, People close to the comatose patient should give doctors as much information as possible to help the doctors determine the cause of coma.
- Prompt medical attention is vital to treat potentially reversible conditions.
- For example, if there is an infection that’s affecting the brain, antibiotics may be needed.
- Glucose may be required in the event of a diabetic shock.
- Surgery may also be necessary to relieve the pressure on the brain due to swelling or to remove a tumor.
- Certain drugs may also help relieve the swelling.
- Medication may also be given to stop seizures if necessary.
- In general, treatment for a coma is supportive.
- People in comas are looked after in an intensive care unit and may often require full life support until their situation improves. [3]
- For patients in a prolonged coma, or persistent vegetative state, the focus is on preventing infections, providing nutrition, also maintaining the patient’s physical health.
- This includes proper nutrition and prevention of infections such as pneumonia (a common cause of death in those in a long-term coma) also bedsores.
- Sometimes, physical therapy is administered to prevent bone, joint, or muscle deformities.
Prevention
Prevention of Coma
- Proper blood glucose management.
- Sticking to your diet
- Regular exercise
- Moderating alcohol and eating when drinking alcohol
- Staying hydrated, preferably with water (10)
Homeopathic Treatment
Homeopathic Treatment of Coma
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Coma:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Homeopathic remedies for coma due to acute head injury:
- Generally, Immediately after a severe head injury, the focus should be on life-saving emergency care.
- Even at this time homeopathic medicines are important in stimulating recovery.
- The sooner these medicines are given the better.
- Then, depending on response I will change remedy or potency or frequency of repetition.
- Generally, Aconite is indicated within the first few minutes or hours after injury, where the person is restless and terrified, even panic-stricken, by the fear of imminent death.
- Those needing Arnica generally, deny that they need any help, saying that they feel quite well. Additionally, they may be severely bruised.
- Besides this, Opium is valuable for someone who is in a daze or even a coma after the head injury, with a flushed and bloated-looking face. Lastly, They may have severe injuries elsewhere, yet not complain of pain.
Homeopathic remedies for coma due to chronic head injury:
The following remedies can be valuable in many of those suffering from the long-term consequences of head injuries.
Natrum sulphuricum:
- It will be in indicated in those with persistent emotional and personality changes, in particular irritability also depression.
- These may be so severe that the person feels suicidal.
- There may be ringing in the ears, as well as vertigo.
- All the symptoms will be worse in damp, wet weather.
Natrum muriaticum:
- This may be valuable in those who after a head injury become sad also withdrawn.
- They may also have chronic headaches that are worse in direct sunlight and develop a marked craving for or dislike of salt.
- When they are at the seaside the symptoms may change, becoming dramatically worse or better.
Hyoscymus Niger:
- It is helpful when there is a change in behaviour, with the person becoming more talkative and excitable.
- Signs of dis inhibition such as laughing inappropriately or handling their genitals may be present.
- Epilepsy, twitches, muscle spasms, hiccoughs, and unusual repetitive gestures, such as picking at their clothes, may also be a problem.
Helleborus:
- This should be thought of when the person seems more dull or slowed since the head injury.
- The person almost seems shut off from the world, with eyes “that do not see” and ears “that do not hear”.
- They may seem almost indifferent to either pain or pleasure.
Hypericum:
- It is indicated when the person has convulsions soon after the injury.
- There may also be spinal injury.
- Later on the person may complain of nerve pain or pins also needles. [5]
Diet & Regimen
Diet & Regimen of Coma
- Eat modest portions. Eating large portions is linked to sleepiness, so keep portions moderate and be mindful of your fullness levels.
- Choose balanced meals.
- Limit alcohol intake.
- Stay hydrated.
- Get a good night’s sleep.
- Use bright light.
- Take a nap.
- Drink water and non-caffeinated tea.
- Do some aerobic exercise.
- Eat smaller meals for the rest of the day.
- Also eat some probiotics.
- Eat carbs that are low on the glycemic index. (11)
Do’s and Don'ts
Do’s & Don’ts
While "Critical Care Medicine: Principles of Diagnosis and Management in the Adult" does not explicitly list "Do’s and Don’ts" in bullet point format for coma management, it does provide comprehensive guidelines that can be interpreted as such:
Do’s:
- Do establish and maintain a patent airway, ensuring adequate oxygenation and ventilation.
- Do initiate neuroprotective measures promptly, such as controlling intracranial pressure and optimizing cerebral perfusion pressure.
- Do identify and treat the underlying cause of coma, whether it be traumatic, metabolic, infectious, or toxic.
- Do monitor and manage potential complications diligently, including respiratory, cardiovascular, neurological, nutritional, and infectious issues.
- Do provide supportive care, including adequate nutrition, skin care, and prevention of deep vein thrombosis.
Don’ts:
- Don’t delay in initiating appropriate diagnostic and therapeutic measures, as prompt intervention can significantly impact patient outcomes.
- Don’t overlook the possibility of multiple contributing factors to coma, as a thorough evaluation is essential for comprehensive management.
- Don’t neglect the psychological and emotional needs of the patient and family, as effective communication and support can significantly improve their experience.
- Don’t underestimate the importance of a multidisciplinary approach to coma management, involving neurologists, intensivists, nurses, therapists, and other healthcare professionals.
- Don’t withhold or withdraw life-sustaining treatment without careful consideration of the patient’s prognosis and wishes, as ethical and legal principles must be adhered to.[17]
Terminology
Terminology
Term | Meaning |
|---|---|
Coma | State of prolonged unconsciousness where a person is unresponsive to external stimuli. |
Traumatic Head Injury | Severe head injury caused by external force, often leading to brain damage. |
Stroke | Sudden loss of brain function due to disrupted blood supply to the brain. |
Brain Tumor | Abnormal growth of cells in the brain, which can be benign (non-cancerous) or malignant (cancerous). |
Intoxication | State of being poisoned by a drug or other substance, leading to altered mental or physical state. |
Hyperglycemia | High blood sugar levels, often seen in diabetes. |
Hypoglycemia | Low blood sugar levels, often seen in diabetes. |
Reticular Activating System (RAS) | A network of nerve pathways in the brainstem responsible for regulating wakefulness and sleep-wake transitions. |
Encephalitis | Inflammation of the brain, usually caused by a viral infection. |
Meningitis | Inflammation of the meninges, the protective membranes covering the brain and spinal cord. |
Cerebral Aneurysm | A weakened area in the wall of a blood vessel in the brain that balloons and may rupture. |
Status Epilepticus | A dangerous condition in which epileptic seizures follow one another without recovery of consciousness in between. |
Anoxia | Complete lack of oxygen to the body tissues. |
Hypoxia | Reduced oxygen supply to the body tissues. |
Additional Terms:
- Homeopathic Remedies: Substances used in homeopathic medicine to treat various ailments.
- Potency: A measure of the dilution of a homeopathic remedy.
- Miasmatic Tendency: A predisposition or susceptibility to certain diseases in homeopathy.
Note: These are just some of the terms used in the article. You can refer to the article itself for a more comprehensive understanding of the terminology and its context.
References
References
- https://www.mayoclinic.org/diseases-conditions/coma/diagnosis-treatment/drc-20371103
- https://www.medicalnewstoday.com/articles/173655.php
- https://www.webmd.com/brain/coma-types-causes-treatments-prognosis#1-2
- https://www.emedicinehealth.com/coma/article_em.htm#what_is_the_glasgow_coma_scale
- https://www.britishhomeopathic.org/charity/how-we-can-help/articles/conditions/h/a-little-bump-or-a-major-injury/
- examination
- https://www.webmd.com/brain/coma-types-causes-treatments prognosis#091e9c5e8027d4dc-2-3
- https://www.google.com/search?q=pathophysiology++of+coma&newwindow
- https://www.google.com/search?q=differntial+diagnosis+of+coma&newwindow
- https://www.healthline.com/health/understanding-and-preventing-diabetic-coma#prevention
- https://www.healthline.com/nutrition/food-coma
- National Survey on Coma Epidemiology, Evaluation, and Therapy in India.
- the Indian Journal of Critical Care Medicine titled "The Curing Coma Campaign®".
- "Plum and Posner’s Diagnosis and Treatment of Stupor and Coma" (Fourth Edition, Jerome B. Posner, Fred Plum, Nicholas J. Schiff, 2007, Oxford University Press).
- "Adams and Victor’s Principles of Neurology" (11th Edition, Allan H. Ropper, Martin A. Samuels, Joshua P. Klein, 2019, McGraw Hill Professional).
- "Critical Care Medicine: Principles of Diagnosis and Management in the Adult" (Fourth Edition, Joseph E. Parrillo, R. Phillip Dellinger, 2008, Elsevier Saunders).
- "Critical Care Medicine: Principles of Diagnosis and Management in the Adult" (Fourth Edition, Joseph E. Parrillo, R. Phillip Dellinger, 2008, Elsevier Saunders).
Also Search As
Also Search As
To find the article about homeopathic treatment of coma, people can use various search terms and strategies:
General Search Terms:
Specific Remedy Searches:
Long-Tail Keywords:
- Can homeopathy help someone in a coma?
- Is homeopathic treatment safe for coma patients?
- How to find a homeopathic practitioner for coma?
Social Media and Forums:
Sharing the article on social media platforms and relevant online forums can attract readers who are interested in homeopathy and alternative medicine.
Additional Tips:
- Look for the article on websites or blogs dedicated to homeopathy or alternative medicine.
- Use quotation marks around specific phrases to get more precise results.
- Include the word "article" in the search query to filter out non-article results.
- Consider using advanced search options to narrow down the results.
There are several ways to search for an article on the homeopathic treatment of coma:
Search Engines:
Use major search engines like Google, Bing, or DuckDuckGo with relevant keywords and phrases. You can try various combinations of the following:
- "homeopathy for coma"
- "homeopathic remedies for coma"
- "homeopathic treatment of coma"
- "coma and homeopathy"
- Specific remedies like "Arnica for coma", "Opium for coma", etc.
- Questions like "Can homeopathy help someone in a coma?"
Specialized Homeopathic Websites:
Look for websites or blogs dedicated to homeopathy or alternative medicine. Many of these platforms publish articles and case studies on various health conditions, including coma.
Homeopathic Journals and Publications:
Search academic databases or online libraries for articles published in homeopathic journals. These resources often contain research and clinical case reports on homeopathic treatments for different ailments.
Social Media:
Explore social media platforms like Facebook, Twitter, or Reddit for groups or communities focused on homeopathy. You can post questions or search for discussions about homeopathic treatments for coma.
Homeopathic Forums:
Participate in online forums dedicated to homeopathy. These forums often have sections for discussing specific health conditions or remedies, and you might find relevant information or discussions about coma treatment.
Homeopathic Practitioner Websites:
Visit the websites of homeopathic practitioners or clinics. They may have blogs or articles discussing their approach to treating coma and other neurological conditions.
Libraries:
Check your local library or university library for books or journals on homeopathy that might contain information on coma treatment.
- Tips for Effective Searching:
- Use quotation marks around specific phrases for more precise results.
- Include the word "article" in your search query to filter out non-article results.
- Combine different keywords and phrases to broaden your search.
- Try using synonyms or related terms for "coma" (e.g., unconsciousness, brain injury).
- Consider using advanced search options to narrow down the results.
- By utilizing these various methods, you can increase your chances of finding the information you need on the homeopathic treatment of coma.
Frequently Asked Questions (FAQ)
What is a coma?
A coma is a state of prolonged unconsciousness in which a person is unresponsive to external stimuli. It’s a medical emergency caused by various factors like traumatic brain injury, stroke, or metabolic disturbances.
How is a coma diagnosed?
Diagnosis
Diagnosis involves a thorough physical examination, neurological assessment, and imaging tests like CT scans or MRI to identify the underlying cause.
What are the different types of coma?
What are the signs and symptoms of a coma?
The primary sign is a complete lack of consciousness. Additional symptoms include closed eyes, irregular breathing, lack of response to pain or light, and altered reflexes.
