Rheumatoid Arthritis (RA)
Definition
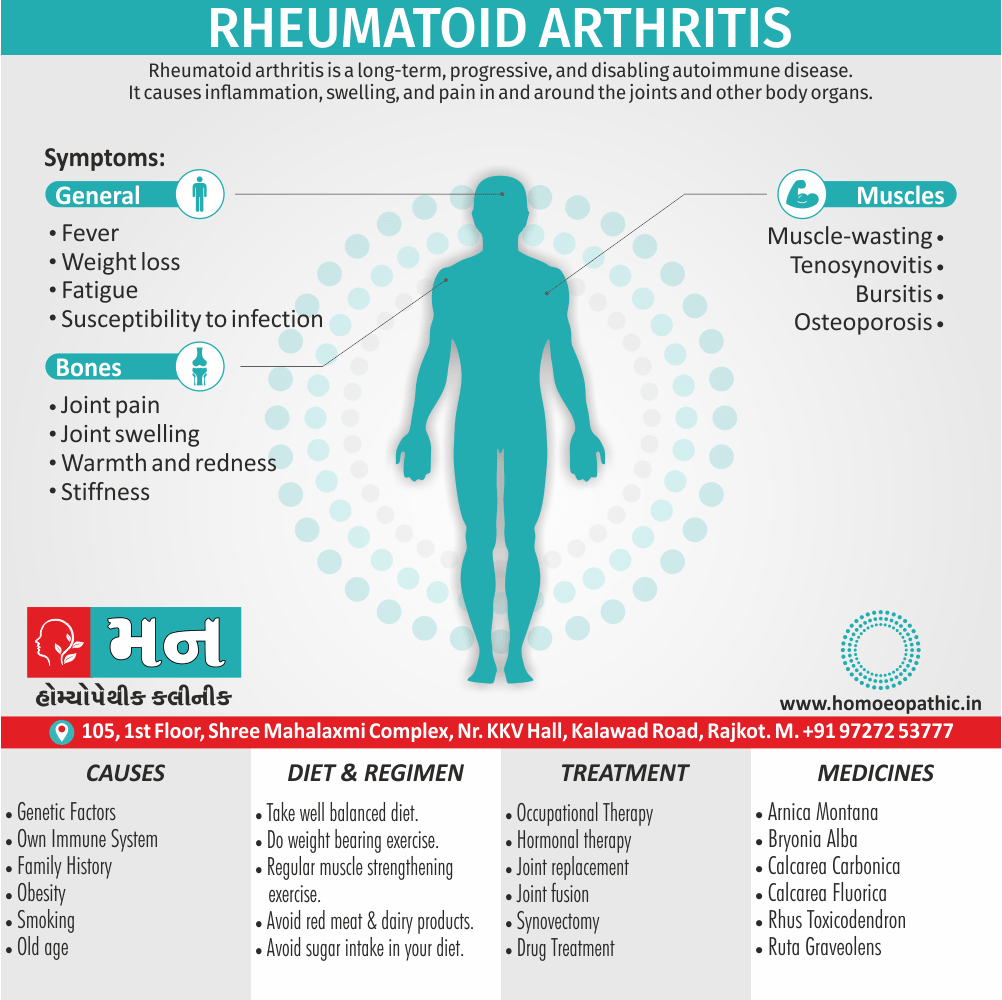
Rheumatoid Arthritis (RA) is a long-term, progressive, and disabling autoimmune disease. It causes inflammation, swelling, and pain in and around the joints and other body organs. [3]
There aren’t any true synonyms for Rheumatoid Arthritis since it’s a specific medical condition. However, here are some related terms you might encounter:
- Autoimmune arthritis: This term describes the fact that RA is an autoimmune disease, where the body’s immune system attacks healthy tissue.
- Inflammatory arthritis: This refers to the inflammation in the joints that’s a hallmark of RA.
- Chronic inflammatory polyarthritis: This term emphasizes that RA is a chronic condition (long-lasting) and affects multiple joints (polyarthritis).
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
- Rheumatoid arthritis (RA) is the most common persistent inflammatory arthritis, occurring throughout the world and in all ethnic groups.
- The prevalence is lowest in black Africans and Chinese, and highest in Pima Indians.
- The clinical course is prolonged, with intermittent exacerbations and remissions.
- Patients with RA have an increased mortality when compared with age matched controls, primarily due to an increased risk of cardiovascular disease.
- This is most marked in those with severe disease, with a reduction in expected lifespan by 8–15 years.
- Around 40% of RA patients are registered as disabled within 3 years of onset, and around 80% are moderately to severely disabled within 20 years.
- Functional capacity decreases most rapidly at the beginning of disease and the functional status of patients within their first year of RA is often predictive of long term outcome.
- Factors that associate with a poorer prognosis are disability at presentation, female gender, involvement of MTP joints, radiographic damage at presentation, smoking and a positive RF (Rheumatoid Factor).
Other Factors:
- In former years, around 25% of patients required a large joint replacement but rates are now falling, probably reflecting more aggressive and effective medical therapy. [1]
- Rheumatoid arthritis is a chronic inflammatory disorder that can affect more than just your joints. In some people, the condition can damage a wide variety of body systems, including the skin, eyes, lungs, heart and blood vessels.
- An autoimmune disorder, rheumatoid arthritis occurs when your immune system mistakenly attacks your own body’s tissues.
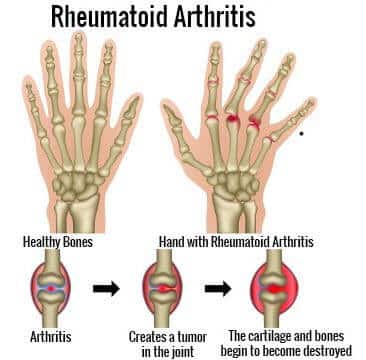
- Unlike the wear-and-tear damage of osteoarthritis, rheumatoid arthritis affects the lining of your joints, causing a painful swelling that can eventually result in bone erosion and joint deformity.
- The joint damage that RA causes usually happens on both sides of your body.
- So if a joint is affected in one of your arms or legs, the same joint in the other arm or leg will probably be affected, too. [2]
Epidemiology
Epidemiology
Prevalence:
- 0.7%: In India, the prevalence of RA is estimated to be 0.7%, which is higher than the global prevalence of 0.46%. (Household catastrophic health expenditures for rheumatoid arthritis: a single centre study from South India | Scientific Reports – Nature, 2023)
- 0.75%: A study published in 1993 found the prevalence of RA in India to be 0.75%. (Prevalence of rheumatoid arthritis in the adult Indian population – PubMed, 1993)
- 0.92%: Rheumatoid arthritis (RA) affects about 0.92% of the adult population in India. (Rheumatoid Arthritis, Arthritis India website)
- 0.31%: Roughly 42.19 million individuals in India, constituting around 0.31% of the populace, have been documented as having Rheumatic Arthritis (RA). (A Review of the Occurrence of Rheumatoid Arthritis and Potential Treatments through Medicinal Plants from an Indian Perspective – PubMed, 2023)
Comparison to global prevalence: The prevalence of RA in India is generally reported to be higher than the global average.
Impact: RA causes significant morbidity and mortality, affecting a substantial portion of the Indian population. It leads to long-lasting illnesses, reduced physical activity, and a negative impact on quality of life.[5][6][7][8]
Causes
Causes
- Nobody knows what causes the immune system to malfunction.
- Some people appear to have genetic factors that make it more likely.
- One theory is that bacteria or a virus triggers RA in people who have this genetic feature.
- In RA, the immune system’s antibodies attack the synovium, which is the smooth lining of a joint. When this happens, pain and inflammation result.
- Inflammation causes the synovium to thicken.
- Eventually, if left untreated, it can invade and destroy cartilage the connective tissue that cushions the ends of the bones.
- The tendons and ligaments that hold the joint together can also weaken and stretch.
- The joint eventually loses its shape and configuration.
- The damage can be severe. [3]
Types
Types of Rheumatoid Arthritis
While Rheumatoid Arthritis (RA) is a single disease entity, it can be classified into different types based on specific characteristics:
1. Seropositive RA vs. Seronegative RA
This classification is based on the presence or absence of certain antibodies in the blood:
- Seropositive RA: This type is characterized by the presence of antibodies like rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies. Seropositive RA is often associated with more severe disease, more joint damage, and a greater likelihood of extra-articular manifestations.
- Seronegative RA: In this type, RF and anti-CCP antibodies are absent. Although seronegative RA may present with milder symptoms initially, it can still progress and cause significant disability.[9]
2. Early RA vs. Established RA
This classification is based on the duration of symptoms:
- Early RA: This refers to RA with a symptom duration of fewer than six months. Early diagnosis and aggressive treatment are crucial in this stage to prevent joint damage and improve long-term outcomes.
- Established RA: This is RA with a symptom duration of more than six months. The focus of treatment in this stage is to control disease activity, prevent further joint damage, and manage complications.[10]
3. Other Subtypes
- Palindromic Rheumatism: This is a rare form of RA characterized by recurrent episodes of joint pain and swelling that last for a few days and then completely resolve. Some individuals with palindromic rheumatism may eventually develop classic RA.
- Juvenile Idiopathic Arthritis (JIA): This is a group of inflammatory arthritis conditions that affect children under the age of 16. While JIA is not technically a type of RA, it shares some similarities and can lead to long-term joint damage if not treated appropriately.
Risk Factors
Risk factors:
Factors that may increase your risk of rheumatoid arthritis include:
Sex i.e.:
- Women are more likely than men to develop rheumatoid arthritis.
Age i.e.:
- Rheumatoid arthritis can occur at any age, but it most commonly begins in middle age.
Family history i.e.:
- If a member of your family has rheumatoid arthritis, you may have an increased risk of the disease.
Smoking i.e.:
- Cigarette smoking increases your risk of developing rheumatoid arthritis, particularly if you have a genetic predisposition for developing the disease.
- Smoking also appears to be associated with greater disease severity.
Environmental exposures i.e.:
- Although poorly understood, some exposures such as asbestos or silica may increase the risk of developing rheumatoid arthritis.
- Emergency workers exposed to dust from the collapse of the World Trade Center are at higher risk of autoimmune diseases such as rheumatoid arthritis.
Obesity i.e.:
- People especially women age 55 and younger who are higher-weight person appear to be at a somewhat higher risk of developing rheumatoid arthritis. [2]
Pathogenesis
Pathogenesis
Rheumatoid Arthritis (RA) is a complex autoimmune disease with a multifactorial pathogenesis involving genetic, environmental, and immunologic factors. While the exact cause remains unknown, the following processes are believed to play a significant role in its development:
1. Genetic Predisposition
Certain genes, particularly those within the human leukocyte antigen (HLA) complex, increase an individual’s susceptibility to RA. These genes are involved in regulating the immune response, and variations in these genes can lead to immune system dysfunction and self-reactivity.[9]
2. Environmental Triggers
Environmental factors such as smoking, infections, and gut microbiome dysbiosis can trigger RA in genetically predisposed individuals. These triggers can lead to the activation of the immune system and the production of autoantibodies, which target the body’s own tissues.[10]
3. Synovial Inflammation
The synovium, a thin membrane lining the joints, becomes inflamed in RA. This inflammation is driven by the infiltration of immune cells, including T cells, B cells, and macrophages, into the synovium. These cells release pro-inflammatory cytokines and chemokines, which further amplify the inflammatory response.[11]
4. Pannus Formation
The inflamed synovium proliferates and forms a destructive tissue called pannus. The pannus invades the cartilage and bone within the joint, leading to joint damage, pain, and stiffness.[12]
5. Systemic Manifestations
RA is a systemic disease, meaning it can affect organs and tissues beyond the joints. This can lead to extra-articular manifestations such as fatigue, anemia, skin nodules, and lung involvement.[13]
Key Points
- RA pathogenesis involves a complex interplay of genetic, environmental, and immunologic factors.
- Early diagnosis and aggressive treatment are crucial to prevent joint damage and improve long-term outcomes.
- Current research focuses on identifying new therapeutic targets to better control disease activity and prevent complications.
Pathophysiology
Pathophysiology
Rheumatoid Arthritis (RA) is a chronic inflammatory disease primarily affecting the synovial joints, leading to pain, stiffness, swelling, and eventual joint destruction. Its pathophysiology involves a complex interplay of genetic, environmental, and immunologic factors.
Synovitis:
- The hallmark of RA is chronic inflammation of the synovium, the lining of the joint capsule.
- Activated immune cells, including T cells, B cells, and macrophages, infiltrate the synovium, releasing pro-inflammatory cytokines (e.g., TNF-alpha, IL-1, IL-6) and chemokines.
- This inflammatory cascade leads to synovial hyperplasia (thickening) and angiogenesis (new blood vessel formation), further fueling the inflammatory process.[9]
Pannus Formation:
- The inflamed synovium proliferates and forms a destructive tissue called pannus.
- Pannus invades and erodes adjacent cartilage and bone, leading to joint damage, deformity, and loss of function.[10]
Autoimmune Response:
- RA is characterized by the presence of autoantibodies, including rheumatoid factor (RF) and anti-citrullinated protein antibodies (ACPAs).
- These autoantibodies contribute to inflammation and tissue damage by forming immune complexes and activating complement pathways.
- Citrullination, a post-translational modification of proteins, is thought to play a key role in generating autoantigens that trigger the autoimmune response in RA.[11]
Bone and Cartilage Destruction:
- Activated osteoclasts, cells responsible for bone resorption, contribute to bone erosion.
- Inflammatory mediators and enzymes released by synovial cells and chondrocytes lead to cartilage degradation.[12]
Systemic Manifestations:
- RA can affect multiple organs and systems beyond the joints, leading to extra-articular manifestations.
- These include fatigue, anemia, rheumatoid nodules, vasculitis, pulmonary fibrosis, and cardiovascular disease.[13]
Conclusion:
Understanding the complex pathophysiology of RA is crucial for developing effective treatments. Current therapies target various aspects of the disease process, including inflammation, immune system modulation, and bone and cartilage protection. Early diagnosis and aggressive treatment are essential to prevent joint damage and improve long-term outcomes for individuals with RA.
Clinical Features
Clinical Features of Rheumatoid Arthritis (RA)
Rheumatoid Arthritis (RA) presents with a wide range of clinical features, impacting both the joints and various other organ systems. The following are the key clinical manifestations:
1. Joint Involvement
- Symmetrical Polyarthritis: RA typically affects multiple joints symmetrically, meaning the same joints on both sides of the body are involved.
- Small Joint Predominance: The small joints of the hands, wrists, and feet are most commonly affected initially.
- Morning Stiffness: Stiffness lasting for more than one hour in the morning is a characteristic feature of RA.
- Joint Swelling, Pain, and Tenderness: These are the cardinal symptoms of RA, often accompanied by warmth and redness over the affected joints.
- Joint Deformities: In advanced RA, joint deformities can occur, including swan-neck deformity, boutonniere deformity, and ulnar deviation of the fingers.[9]
2. Extra-articular Manifestations
- Rheumatoid Nodules: These are firm, subcutaneous nodules that often develop near pressure points like the elbows and fingers.
- Fatigue: A persistent feeling of tiredness and lack of energy is common in RA.
- Anemia: Chronic inflammation can lead to anemia, causing fatigue and shortness of breath.
- Vasculitis: Inflammation of blood vessels can occur in RA, affecting various organs like the skin, nerves, and eyes.
- Pulmonary Involvement: RA can lead to lung inflammation and scarring (interstitial lung disease) or pleural effusions (fluid around the lungs).
- Cardiac Involvement: RA can increase the risk of cardiovascular diseases like atherosclerosis and heart failure.[10]
3. Constitutional Symptoms
- Fever: Low-grade fever may occur, particularly during active disease flares.
- Weight Loss: Loss of appetite and chronic inflammation can contribute to weight loss.
- Malaise: A general feeling of discomfort and unwellness may be present.[11]
4. Other Features
- Dry Eyes and Mouth (Sjögren’s Syndrome): This can occur in some RA patients, causing dryness and discomfort in the eyes and mouth.
- Carpal Tunnel Syndrome: Compression of the median nerve in the wrist can lead to numbness and tingling in the hands.
- Osteoporosis: RA and its treatment can increase the risk of osteoporosis, leading to fragile bones and fractures.[12]
Key Points
- RA presents with a wide range of clinical features, impacting both the joints and various other organ systems.
- Early diagnosis and prompt treatment are crucial to prevent joint damage and other complications.
- Management of RA involves a multidisciplinary approach, including medications, physical therapy, and lifestyle modifications.
Sign & Symptoms
Sign and Symptoms
Rheumatoid Arthritis
Joints:
- Joint pain
- Joint swelling, warmth and redness
- Stiffness, especially first thing in the morning or after sitting still for a long time. [2]

Rheumatoid Arthritis In Hands
Extra-articular manifestations of rheumatoid disease:
Systemic e.g.:
- Fever
- Weight loss
- Fatigue
- Susceptibility to infection
Musculo-skeletal e.g.:
- Muscle-wasting
- Tenosynovitis
- Bursitis
- Osteoporosis
Hematological e.g.:
- Anemia
- Thrombocytosis
- Eosinophilia
Lymphatic e.g.:
- Felty’s syndrome
- Splenomegaly
Nodules e.g.:
- Sinuses
- Fistula
Ocula e.g.:
- Episcleritis
- Scleritis
- Scleromalacia
- Keratoconjunctivitis sicca
Vasculitis e.g.:
- Digital arteritis
- Ulcers
- Pyoderma gangrenosum
- Mononeuritis multiplex
- Visceral arteritis
Cardiac e.g.:
- Pericarditis
- Myocarditis
- Endocarditis
- Conduction defects
- Coronary vasculitis
- Granulomatous aortitis
Pulmonary e.g.:
- Nodules
- Pleural effusions
- Fibrosing alveolitis
- Bronchiolitis
- Caplan’s syndrome
Neurological e.g.:
- Cervical cord compression
- Compression neuropathies
- Peripheral neuropathy
- Mononeuritis multiplex
Amyloidosis [1]
Clinical Examination
Clinical Examination of Rheumatoid Arthritis (RA)
A thorough clinical examination is crucial for diagnosing and assessing the severity of Rheumatoid Arthritis (RA). It involves a detailed evaluation of the joints, as well as a search for extra-articular manifestations.
1. Joint Examination
- Inspection: Observe the joints for swelling, redness, warmth, and deformities.
- Palpation: Gently palpate the joints to assess for tenderness, warmth, and synovial thickening.
- Range of Motion: Evaluate the active and passive range of motion of each joint, noting any limitations or pain.
- Joint Stability: Assess for joint laxity or instability, which can occur in advanced RA.
- Specific Joint Assessments: Perform specific tests for individual joints, such as the squeeze test for hand joints or the McMurray test for the knee.[9]
2. Extra-articular Examination
- Skin: Look for rheumatoid nodules, vasculitis, or other skin manifestations.
- Eyes: Check for signs of dryness, inflammation, or scleritis.
- Lungs: Listen for crackles or decreased breath sounds, which can indicate lung involvement.
- Heart: Auscultate for murmurs or signs of heart failure.
- Neurological: Assess for any sensory or motor deficits, which can occur in peripheral neuropathy or nerve entrapment.[10]
3. General Examination
- Vital Signs: Check blood pressure, heart rate, respiratory rate, and temperature.
- Constitutional Symptoms: Assess for fatigue, malaise, or weight loss.
- Lymphadenopathy: Palpate for enlarged lymph nodes.
- Splenomegaly: Assess for an enlarged spleen.[11]
4. Functional Assessment
- Grip Strength: Measure grip strength using a hand dynamometer.
- Gait: Observe the patient’s gait for any abnormalities or limitations.
- Activities of Daily Living: Assess the patient’s ability to perform daily activities like dressing, bathing, and eating.[12]
Key Points
- A comprehensive clinical examination is essential for diagnosing and assessing the severity of RA.
- The examination should include a detailed evaluation of the joints, as well as a search for extra-articular manifestations.
- Functional assessment is important to evaluate the impact of RA on the patient’s daily life.
Diagnosis
Diagnosis of Rheumatoid Arthritis (RA)
To establish diagnosis:
- Clinical criteria
- ESR
- CRP
- Ultrasound
- MRI
- Rheumatoid factor
- Anti-citrullinated peptide antibodies
Monitor disease activity and drug efficacy:
- Pain (visual analogue scale)
- Early morning stiffness (minutes)
- Joint tenderness
- Joint swelling
- DAS28 score
- ESR and CRP
- Ultrasound
To monitor disease damage:
- X-rays
- Functional assessment
To monitor drug safety:
- Urinalysis
- Full blood count
- Urea
- Creatinine
- Liver function tests [1]
Erythrocyte sedimentation rate (ESR or sed rate):
- This test assesses levels of inflammation in the body.
- It measures how fast red blood cells in a test tube separate from blood serum over a set period.
- If the red blood cells settle quickly as sediment, inflammation levels are high.
- This test is not specific for RA and is a useful test for other inflammatory conditions or infections.
C-reactive protein (CRP):
- The liver produces CRP.
- A higher CRP level suggests that there is inflammation in the body.
- This test is not specific for RA and CRP can occur in other inflammatory conditions or infection.
Anemia:
- Many people with RA also have anemia.
- Anemia happens when there are too few red blood cells in the blood.
- Red blood cells carry oxygen to the tissues and organs of the body.
Rheumatoid factor:
- If an antibody known as rheumatoid factor is present in the blood, it can indicate that RA is present.
- However, not everyone with RA tests positive for this factor. [3]
Differential Diagnosis
Differential Diagnosis of Rheumatoid Arthritis (RA)
Rheumatoid Arthritis (RA) can mimic various other conditions, making its diagnosis challenging. The following are some key differential diagnoses to consider:
1. Other Inflammatory Arthritides
- Psoriatic Arthritis: This can present with joint pain and swelling, often accompanied by skin psoriasis.
- Ankylosing Spondylitis: This primarily affects the spine and sacroiliac joints, causing back pain and stiffness.
- Reactive Arthritis: This typically follows an infection and can cause arthritis, urethritis, and conjunctivitis.
- Gout: This causes acute, severe joint pain and swelling, often affecting the big toe.
- Pseudogout: This is similar to gout but involves calcium pyrophosphate crystals instead of uric acid crystals.[9]
2. Connective Tissue Diseases
- Systemic Lupus Erythematosus (SLE): This can cause joint pain, skin rash, and other systemic symptoms.
- Scleroderma: This leads to skin thickening and can also involve the joints and internal organs.
- Sjögren’s Syndrome: This causes dry eyes and mouth and can be associated with joint pain.
- Polymyositis/Dermatomyositis: These inflammatory muscle diseases can cause muscle weakness and pain, sometimes mimicking joint pain.[10]
3. Infectious Arthritis
- Septic Arthritis: This is a bacterial infection of the joint, causing severe pain, swelling, and fever.
- Lyme Arthritis: This can occur in Lyme disease and typically affects large joints like the knee.
- Viral Arthritis: Several viruses can cause joint pain and swelling, often resolving on their own.[11]
4. Degenerative Joint Diseases
- Osteoarthritis (OA): This is the most common form of arthritis, causing joint pain and stiffness, primarily in older adults.
- Spondyloarthropathy: This affects the spine and sacroiliac joints, often associated with inflammatory bowel disease.[12]
5. Other Conditions
- Fibromyalgia: This causes widespread pain and tenderness, often accompanied by fatigue and sleep disturbances.
- Chronic Fatigue Syndrome: This leads to persistent fatigue and other symptoms, sometimes including joint pain.
- Depression: This can cause various physical symptoms, including joint pain and fatigue.[13]
Key Points
- RA can mimic various other conditions, making its diagnosis challenging.
- A thorough clinical evaluation, laboratory tests, and imaging studies are crucial for differentiating RA from other diseases.
- Early diagnosis and prompt treatment are essential to prevent joint damage and other complications.
Complications
Complications
Rheumatoid Arthritis (RA), if left untreated or inadequately managed, can lead to a range of complications affecting various organ systems. These complications can significantly impact the quality of life and even increase mortality risk.
1. Joint Complications
- Joint Deformities: Chronic inflammation and joint destruction can lead to deformities like swan-neck deformity, boutonniere deformity, and ulnar deviation of the fingers.
- Joint Instability: Ligament and tendon damage can cause joint instability, leading to difficulty with movement and increased risk of falls.
- Joint Contractures: Limited joint movement due to scarring and inflammation can result in contractures, further impairing function.[9]
2. Extra-articular Complications
- Cardiovascular Disease: RA increases the risk of atherosclerosis, heart attack, stroke, and heart failure.
- Osteoporosis: Chronic inflammation and certain medications used to treat RA can contribute to bone loss and osteoporosis, increasing fracture risk.
- Lung Disease: RA can lead to interstitial lung disease (inflammation and scarring of the lungs) or pleural effusions (fluid around the lungs), causing breathing difficulties.
- Vasculitis: Inflammation of blood vessels can affect various organs, including the skin, nerves, and eyes.
- Eye Problems: Scleritis (inflammation of the white part of the eye) and dry eyes (Sjögren’s syndrome) can occur.
- Neurological Complications: Carpal tunnel syndrome (compression of the median nerve in the wrist), peripheral neuropathy (nerve damage), and cervical myelopathy (spinal cord compression) can occur.
- Kidney Disease: RA can rarely cause kidney problems, such as glomerulonephritis.
- Lymphoma: RA is associated with a slightly increased risk of developing lymphoma, a type of blood cancer.[10]
3. General Complications
- Anemia: Chronic inflammation can lead to anemia of chronic disease, causing fatigue and weakness.
- Infections: RA and its treatment can increase the risk of infections, particularly those affecting the lungs and skin.
- Depression and Anxiety: Chronic pain and disability associated with RA can contribute to mental health problems.[11]
4. Treatment-Related Complications
- Medication Side Effects: Medications used to treat RA can have various side effects, including gastrointestinal problems, liver damage, and increased risk of infections.
- Surgery Complications: Joint replacement surgery, while beneficial for some RA patients, carries risks like infection, bleeding, and implant failure.[12]
Investigations
Investigations of Rheumatoid Arthritis (RA)
A combination of clinical assessment, laboratory tests, and imaging studies is essential for diagnosing and monitoring Rheumatoid Arthritis (RA). These investigations help confirm the diagnosis, assess disease activity, and guide treatment decisions.
1. Laboratory Tests
- Rheumatoid Factor (RF): This antibody is present in about 70-80% of RA patients, but it can also be positive in other conditions.
- Anti-Cyclic Citrullinated Peptide (Anti-CCP) Antibodies: These antibodies are more specific for RA and often present earlier in the disease course.
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): These markers of inflammation are often elevated in active RA.
- Complete Blood Count (CBC): This can reveal anemia, which is common in RA.
- Liver and Kidney Function Tests: These are important to monitor for potential side effects of RA medications.[9]
2. Imaging Studies
- X-rays: These can show joint erosions, joint space narrowing, and other signs of joint damage in RA.
- Ultrasound: This can detect synovitis (inflammation of the joint lining) and erosions earlier than X-rays.
- Magnetic Resonance Imaging (MRI): This provides detailed images of the joints and surrounding tissues, allowing for early detection of synovitis and bone marrow edema.[10]
3. Other Investigations
- Synovial Fluid Analysis: This can help differentiate RA from other types of arthritis and rule out infection.
- Bone Densitometry: This measures bone density to assess for osteoporosis, a common complication of RA.
- Electrocardiogram (ECG) and Echocardiogram: These tests may be done to evaluate for cardiac involvement in RA.
- Pulmonary Function Tests: These can assess lung function in patients with suspected lung involvement.[11]
Treatment
Treatment of Rheumatoid Arthritis (RA)
There is no cure for rheumatoid arthritis.
But clinical studies indicate that remission of symptoms is more likely when treatment begins early with medications known as disease-modifying antirheumatic drugs (DMARDs).
Medications:
The types of medications recommended by your doctor will depend on the severity of your symptoms and how long you’ve had rheumatoid arthritis.
NSAIDs i.e.:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) can relieve pain and reduce inflammation.
- Over the counter NSAIDs include ibuprofen (Advil, Motrin IB) and naproxen sodium (Aleve).
- Stronger NSAIDs are available by prescription.
- Side effects may include stomach irritation, heart problems and kidney damage.
Steroids i.e.:
- Corticosteroid medications, such as prednisone, reduce inflammation and pain and slow joint damage.
- Side effects may include thinning of bones, weight gain and diabetes.
- Doctors often prescribe a corticosteroid to relieve acute symptoms, with the goal of gradually tapering off the medication.
Disease-modifying antirheumatic drugs (DMARDs) i.e.:
- These drugs can slow the progression of rheumatoid arthritis also save the joints and other tissues from permanent damage.
- Common DMARDs include methotrexate (Trexall, Otrexup, others), leflunomide (Arava), hydroxychloroquine (Plaquenil) and sulfasalazine (Azulfidine).
- Side effects vary but may include liver damage, bone marrow suppression and severe lung infections.
Biologic agents i.e.:
- Also known as biologic response modifiers, this newer class of DMARDs includes abatacept (Orencia), adalimumab (Humira), anakinra (Kineret), baricitinib (Olumiant), certolizumab (Cimzia), etanercept (Enbrel), golimumab (Simponi), infliximab (Remicade), rituximab (Rituxan), sarilumab (Kevzara), tocilizumab (Actemra) and tofacitinib (Xeljanz).
These drugs can target parts of the immune system that trigger inflammation that causes joint and tissue damage.
These types of drugs also increase the risk of infections.
In people with rheumatoid arthritis, higher doses of tofacitinib can increase the risk of blood clots in the lungs.
Biologic DMARDs are usually most effective when paired with a nonbiologic DMARD, such as methotrexate.
Occupational Therapy:
- Your doctor may send you to a physical or occupational therapist who can teach you exercises to help keep your joints flexible.
- The therapist may also suggest new ways to do daily tasks, which will be easier on your joints.
- For example, you may want to pick up an object using your forearms.
- Assistive devices can make it easier to avoid stressing your painful joints.
- For instance, a kitchen knife equipped with a hand grip helps protect your finger and wrist joints.
- Certain tools, such as buttonhooks, can make it easier to get dressed.
Surgery:
If medications fail to prevent or slow joint damage, you may consider surgery to repair damaged joints.
Surgery may help restore your ability to use your joint.
It can also reduce pain and improve function.
Rheumatoid arthritis surgery may involve one or more of the following procedures:
Synovectomy i.e.:
- Surgery to remove the inflamed lining of the joint (synovium) can be performed on knees, elbows, wrists, fingers and hips.
Tendon repair i.e.:
- Inflammation and joint damage may cause tendons around your joint to loosen or rupture.
- Your surgeon may be able to repair the tendons around your joint.
Joint fusion i.e.:
- Surgically fusing a joint may be recommended to stabilize or realign a joint and for pain relief when a joint replacement isn’t an option.
Total joint replacement i.e.:
- During joint replacement surgery, your surgeon removes the damaged parts of your joint and inserts a prosthesis made of metal and plastic.
- Surgery carries a risk of bleeding, infection and pain. [2]
Prevention
Prevention of Rheumatoid Arthritis (RA)
While there is no definitive way to prevent Rheumatoid Arthritis (RA), certain lifestyle modifications and interventions may help reduce the risk or delay its onset in genetically susceptible individuals.
1. Lifestyle Modifications
- Smoking Cessation: Smoking is a strong risk factor for RA development and progression. Quitting smoking can significantly reduce the risk.
- Healthy Diet: A balanced diet rich in fruits, vegetables, and omega-3 fatty acids may have anti-inflammatory effects and potentially lower the risk of RA.
- Regular Exercise: Moderate physical activity can help maintain joint health and overall well-being, potentially reducing the risk of RA.
- Weight Management: Maintaining a healthy weight can reduce stress on joints and potentially lower the risk of developing RA.[9]
2. Potential Preventive Interventions
- Periodontal Care: Studies suggest a link between periodontal disease and RA. Maintaining good oral hygiene and regular dental checkups may help reduce the risk.
- Breastfeeding: Some research indicates that breastfeeding may have a protective effect against RA development.
- Vitamin D Supplementation: Adequate vitamin D levels are important for immune system function. Maintaining optimal levels through sunlight exposure or supplementation may be beneficial.[10]
3. Early Intervention
- Prompt Treatment of Infections: Certain infections have been associated with triggering RA in susceptible individuals. Early diagnosis and treatment of infections may help prevent RA onset.[11]
Homeopathic Treatment
Homeopathic Treatment of Rheumatoid Arthritis (RA)
Arnica:
- Useful for chronic arthritis with a feeling of bruising also soreness.
- The painful parts feel worse especially from being moved or touched.
Bryonia:
- Helpful for stiffness also inflammation with tearing or throbbing pain, made worse by motion.
- The condition may have developed gradually, additionally it is worse in cold dry weather.
- Discomfort is aggravated specifically by being touched or bumped, or from any movement.
- Besides this, Relief can be had from pressure and from rest.
- Lastly, The person may want to stay completely still and not be interfered with.
Calcarea carbonica:
- Generally, Helpful for deeply aching arthritis involving node formation around the joints.
- Inflammation and soreness are worse especially from cold and dampness, and problems may be focused on the knees and hands.
- Common symptoms are: weakness in the muscles, easy fatigue from exertion, additionally a feeling of chilliness or sluggishness.
- The person who benefits from Calcarea is often solid and responsible, but tends to become extremely anxious and overwhelmed when ill or overworked.
Aurum metallicum:
- This remedy is often prescribed for wandering pains in the muscles and joints that are better from motion and warmth, and worse at night.
- The person may experience deep pain in the limbs when trying to sleep.
- Also may feel discomfort that may wake the person up.
- People who need this remedy have a tendency to feel depressed.
Causticum:
- Useful when deformities develop in the joints, in a person with a tendon problems, muscle weakness, and contractures.
- The hands and fingers may be most affected.
- Stiffness and pain are worse from being cold, and relief may come with warmth.
- The person often feels best in rainy weather and worse when the days are clear and dry.
Calcarea fluorica:
- Helpful when arthritic pains improve with heat and motion.
- Joints become enlarged and hard, and nodes or deformities develop.
- Arthritis after chronic injury to joints also responds to Calcarea fluorica.
Dulcamara:
- Indicated if arthritis flares up during cold damp weather.
- The person gets chilled and wet.
- They are often stout, with a tendency toward back pain, chronic stiffness in the muscles, and allergies.
Kali bichromicum:
- This is useful when arthritic pains alternate with asthma or stomach symptoms.
- Pains may suddenly come also go, or shift around.
- Discomfort and inflammation are aggravated by heat and worse when the weather is warm.
Kali carbonicum:
- Arthritis with great stiffness and stitching pains, worse especially in the early morning hours and worse from cold and dampness, may respond to Kali carbonicum.
- The joints may be becoming either thickened or deformed.
Kalmia latiflora:
- Basically, Useful for intense arthritic pain that flares up suddenly.
- The problems start in higher joints also extend to lower ones.
- Pain and inflammation may begin in the elbows, after that spreading downward to the wrists and hands.
- Discomfort is worse especially from motion and often worse at night.
Ledum palustre:
- Arthritis that starts in lower joints also extends to higher ones are candidate for this remedy.
- Furthermore, Pain and inflammation often begin in the toes and spread upward to the ankles and knees in RA.
- The joints may also make cracking sounds.
- Ledum is strongly indicated when swelling is significant and relieved by cold applications.
Pulsatilla:
- Applicable when rheumatoid arthritis pain is changeable in quality, or when the flare-ups move from place to place.
- The symptoms (and the person) feel worse from warmth, and better from fresh air and cold applications.
- Can benefit people who are emotional and affectionate, sometimes having teary moods.
Rhododendron:
- Strongly indicated if swelling and soreness flare up before a storm, continuing until the weather clears.
- Cold and dampness aggravate the symptoms.
- Discomfort is often worse toward early morning, or after staying still too long.
Rhus toxicodendron:
- Useful for rheumatoid arthritis, with pain and stiffness that is worse in the morning and worse on first motion, but better from continued movement.
- Hot baths or showers, and warm applications improve the stiffness and relieve the pain of RA.
- The condition is worse in cold, wet weather.
- The person may feel extremely restless, unable to find a comfortable position, and need to keep moving constantly.
- Continued motion also helps to relieve anxiety.
Ruta graveolens:
- Arthritis with a feeling of great stiffness and lameness, worse specifically from cold and damp and worse from exertion, may be helped by Ruta graveolens.
- Tendons and capsules of the joints can be either deeply affected or damaged by RA.
- The arthritis may have developed after overuse, from repeated wear also tear. [4]
Diet & Regimen
Diet & Regimen for Rheumatoid Arthritis (RA)
While there is no specific diet that can cure Rheumatoid Arthritis (RA), certain dietary and lifestyle choices can help manage symptoms, reduce inflammation, and improve overall well-being.
Diet Recommendations
- Anti-inflammatory Foods: Focus on a diet rich in fruits, vegetables, whole grains, and healthy fats, which have anti-inflammatory properties.
- Omega-3 Fatty Acids: Include fatty fish (salmon, tuna, sardines), flaxseeds, chia seeds, and walnuts in your diet, as they are rich in omega-3 fatty acids, which can help reduce inflammation.
- Antioxidant-rich Foods: Berries, cherries, citrus fruits, and green tea are high in antioxidants, which can help protect against cell damage and inflammation.
- Vitamin D: Ensure adequate vitamin D intake through sunlight exposure or supplements, as low levels have been linked to increased RA disease activity.
Foods to Limit or Avoid
- Processed Foods: Limit processed foods, refined sugars, and saturated fats, as they can increase inflammation.
- Red Meat: High consumption of red meat has been associated with increased inflammation and RA risk.
- Alcohol: Excessive alcohol intake can worsen inflammation and interact with RA medications.
- Potential Triggers: Some individuals may experience symptom flares after consuming certain foods, like nightshades (tomatoes, potatoes, peppers) or gluten. It’s essential to identify and avoid personal triggers.
Regimen Recommendations
- Regular Exercise: Engage in low-impact exercises like walking, swimming, or cycling, as they can help maintain joint mobility and reduce pain.
- Stress Management: Practice relaxation techniques like yoga, meditation, or deep breathing to help manage stress, which can worsen RA symptoms.
- Adequate Sleep: Aim for 7-8 hours of quality sleep each night, as sleep deprivation can increase inflammation and pain.
- Weight Management: Maintain a healthy weight to reduce stress on joints and improve overall health.
Additional Tips
- Hydration: Stay well-hydrated by drinking plenty of water throughout the day.
- Supplements: Consult your doctor before taking any supplements, as some can interact with RA medications.
- Regular Follow-ups: Maintain regular appointments with your rheumatologist to monitor disease activity and adjust treatment as needed.[9][10][11][12]
Do’s and Don'ts
Do’s and Don’ts of RA
Managing Rheumatoid Arthritis (RA) effectively requires a multifaceted approach encompassing lifestyle adjustments, medical interventions, and self-care strategies. Here’s a breakdown of essential do’s and don’ts to help you navigate life with RA:
- Do’s:
- Prioritize Regular Exercise: Engage in low-impact exercises like walking, swimming, or yoga to maintain joint mobility, muscle strength, and overall fitness. Reference: Kelley’s Textbook of Rheumatology, 11th Edition, Elsevier, 2023
- Maintain a Healthy Diet: Focus on anti-inflammatory foods, omega-3 fatty acids, and antioxidants to support joint health and overall well-being. Reference: Oxford Textbook of Rheumatology, 5th Edition, Oxford University Press, 2018
- Get Sufficient Sleep: Aim for 7-8 hours of quality sleep each night to reduce inflammation and pain. Reference: Harrison’s Principles of Internal Medicine, 21st Edition, McGraw Hill, 2022
- Manage Stress: Practice relaxation techniques like meditation, deep breathing exercises, or spending time in nature to alleviate stress and its impact on RA symptoms.
- Stay Hydrated: Drink plenty of water throughout the day to maintain joint lubrication and overall health.
- Use Assistive Devices: Utilize assistive devices like canes, walkers, or grab bars to facilitate daily activities and reduce stress on joints.
- Maintain Regular Follow-ups: Schedule regular appointments with your rheumatologist to monitor disease activity and adjust treatment as needed.
- Communicate Openly: Discuss any concerns or challenges related to RA with your healthcare team and loved ones.
Don’ts:
- Smoke: Smoking exacerbates RA symptoms and increases the risk of complications. Quitting smoking is crucial for managing RA effectively.
- Overexert Yourself: Avoid pushing yourself beyond your limits, especially during flares. Listen to your body and rest when needed.
- Neglect Oral Hygiene: Poor oral health has been linked to increased RA disease activity. Maintain good oral hygiene and schedule regular dental checkups.
- Ignore Mental Health: Seek support if you’re experiencing depression, anxiety, or other mental health challenges related to RA.
- Self-Medicate: Avoid taking over-the-counter medications or supplements without consulting your doctor, as they can interact with RA medications.
- Compare Yourself to Others: Everyone’s experience with RA is unique. Focus on your own progress and avoid comparing yourself to others.
By incorporating these do’s and don’ts into your daily life, you can effectively manage RA and improve your overall quality of life. Remember, a proactive approach to self-care and a strong partnership with your healthcare team are key to living well with RA.
Terminology
Terminology
- Autoimmune Disease: A condition where the body’s immune system mistakenly attacks its own healthy tissues.
- Inflammation: A protective response by the body to injury or infection, characterized by redness, swelling, heat, and pain. In RA, chronic inflammation affects the joints and can lead to damage.
- Synovium: The thin membrane lining the joints that produces synovial fluid, which nourishes and lubricates the joint. In RA, the synovium becomes inflamed and thickened.
- Pannus: An abnormal layer of tissue that forms in the inflamed synovium of people with RA. It can invade and damage cartilage and bone within the joint.
- Joint Erosion: The gradual destruction of bone and cartilage within a joint due to the inflammatory process in RA.
- Joint Deformity: Changes in the shape or alignment of a joint due to damage caused by RA.
- Rheumatoid Factor (RF): An antibody found in the blood of many people with RA. It can also be present in other conditions.
Other Terminologies
- Anti-Cyclic Citrullinated Peptide (Anti-CCP) Antibodies: Antibodies that are more specific for RA and often present earlier in the disease course than RF.
- Disease-Modifying Anti-Rheumatic Drugs (DMARDs): Medications that slow or stop the progression of RA by suppressing the immune system.
- Biologic DMARDs: A newer class of DMARDs that target specific molecules involved in the immune response.
- Remission: A state where RA disease activity is minimal or absent, and the patient experiences few or no symptoms.
- Flare: A period of increased RA disease activity, with worsening of symptoms and inflammation.
- Extra-articular Manifestations: Symptoms and complications of RA that affect organs and tissues beyond the joints.
- Comorbidities: Other health conditions that often coexist with RA, such as cardiovascular disease, osteoporosis, and depression.
References
References
- Davidson’s Principles and Practice of Medicine (22nd edition) Ch. 25
- https://www.mayoclinic.org/diseases-conditions/rheumatoid-arthritis/symptoms-causes/syc-20353648
- https://www.medicalnewstoday.com/articles/323361.php
- https://www.wellinghomeopathy.com/treatment-of-rheumatoid-arthritis/#Homeopathic_treatment_for_Rheumatoid_Arthritis
- Household catastrophic health expenditures for rheumatoid arthritis: a single centre study from South India | Scientific Reports – Nature, 2023.
- Prevalence of rheumatoid arthritis in the adult Indian population – PubMed, 1993.
- Rheumatoid Arthritis, Arthritis India website.
- A Review of the Occurrence of Rheumatoid Arthritis and Potential Treatments through Medicinal Plants from an Indian Perspective – PubMed, 2023.
- Kelley’s Textbook of Rheumatology, 11th Edition, Elsevier, 2023.
- Oxford Textbook of Rheumatology, 5th Edition, Oxford University Press, 2018.
- Harrison’s Principles of Internal Medicine, 21st Edition, McGraw Hill, 2022.
- Rheumatology, 7th Edition, Mosby, 2019.
- Goldman-Cecil Medicine, 26th Edition, Elsevier, 2020
Also Search As
Rheumatoid Arthritis Also Search As
People can search for homeopathic articles on RA in a variety of ways, using different combinations of keywords and phrases. Here are some effective search strategies:
General Search Terms
- "Homeopathy for rheumatoid arthritis"
- "Homeopathic treatment for RA"
- "Homeopathic remedies for RA"
- "RA and homeopathy"
More Specific Search Terms
- "Homeopathic medicines for RA pain"
- "Homeopathy for RA inflammation"
- "Homeopathic constitutional treatment for RA"
- "Homeopathy for RA case studies"
- "Research on homeopathy and RA"
Additional Tips for Effective Searching
- Use quotation marks to search for an exact phrase (e.g., "homeopathic treatment for RA").
- Use the minus sign to exclude certain terms (e.g., homeopathy for RA -arthritis).
- Use synonyms or related terms (e.g., homeopathy OR homeopathic medicine).
- Specify the type of information you’re looking for (e.g., homeopathy for RA research articles).
- Use advanced search options on search engines or databases to narrow down your results.
Where to Search
- Search engines: Google, Bing, DuckDuckGo, etc.
- Homeopathic websites and blogs: National Center for Homeopathy, Homeobook, etc.
- Medical databases: PubMed, Google Scholar, etc.
- Social media: Facebook groups, Twitter hashtags, etc.
Important Considerations
- It’s essential to critically evaluate the information you find online. Look for articles published in reputable sources and written by qualified professionals.
- Be aware that the scientific evidence supporting the effectiveness of homeopathy for RA is limited.
- Always consult with a qualified healthcare professional before starting any new treatment, including homeopathy.
By utilizing these strategies and considering these points, individuals can effectively search for and access reliable information about homeopathy and RA.
Frequently Asked Questions (FAQ)
What is Rheumatoid Arthritis ?
Definition
Rheumatoid arthritis is a long-term, progressive, also disabling autoimmune disease. Additionally, It causes inflammation, swelling, and pain in and around the joints and other body organs.
What causes Rheumatoid Arthritis ?
Causes of Rheumatoid Arthritis (RA)
- Genetic factors
- Either Bacteria or a virus
- Antibodies attack the synovium
- Inflammation causes the synovium to thicken
- The joint eventually loses its shape also configuration
- The damage can be severe
- Women are more likely than men
- Family history
What are the symptoms of Rheumatoid Arthritis ?
Symptoms of Rheumatoid Arthritis (RA)
- Joint pain
- Joint swelling, warmth also redness
- Stiffness
- Fever
- Weight loss
- Fatigue
- Susceptibility to infection
How is rheumatoid arthritis diagnosed?
Diagnosis involves a combination of medical history, physical examination, blood tests (like rheumatoid factor and anti-CCP antibodies), and imaging tests (like X-rays or MRIs).
What are the treatment options for rheumatoid arthritis?
Treatment aims to manage symptoms, slow disease progression, and prevent joint damage. Options include medications (like disease-modifying antirheumatic drugs or DMARDs), physical therapy, and lifestyle changes.
Can homeopathy help with rheumatoid arthritis?
Homeopathy offers a holistic and individualized approach to managing rheumatoid arthritis symptoms and improving overall well-being. It aims to address the root cause of the disease and stimulate the body’s natural healing abilities.
How does a homeopath select the right remedy for rheumatoid arthritis?
A detailed case analysis, considering the location and nature of pain, stiffness, swelling, and other associated symptoms, is crucial in selecting the most suitable remedy.
Can homeopathy help reduce inflammation and pain in rheumatoid arthritis?
Homeopathy aims to modulate the immune system and reduce inflammation, which may lead to a decrease in pain and stiffness.
How long does it take to see results with homeopathy for rheumatoid arthritis?
The response time varies depending on the individual and the severity of the condition. Some may experience improvement in symptoms within a few weeks, while others may require longer-term treatment.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Rheumatoid Arthritis ?
Homoeopathic Medicines for Rheumatoid Arthritis
- Arnica
- Bryonia
- Calcarea carb
- Aurum metallicum
- Causticum
- Calcarea fluorica
- Dulcamara
- Pulsatilla
