Fibromyalgia
Definition
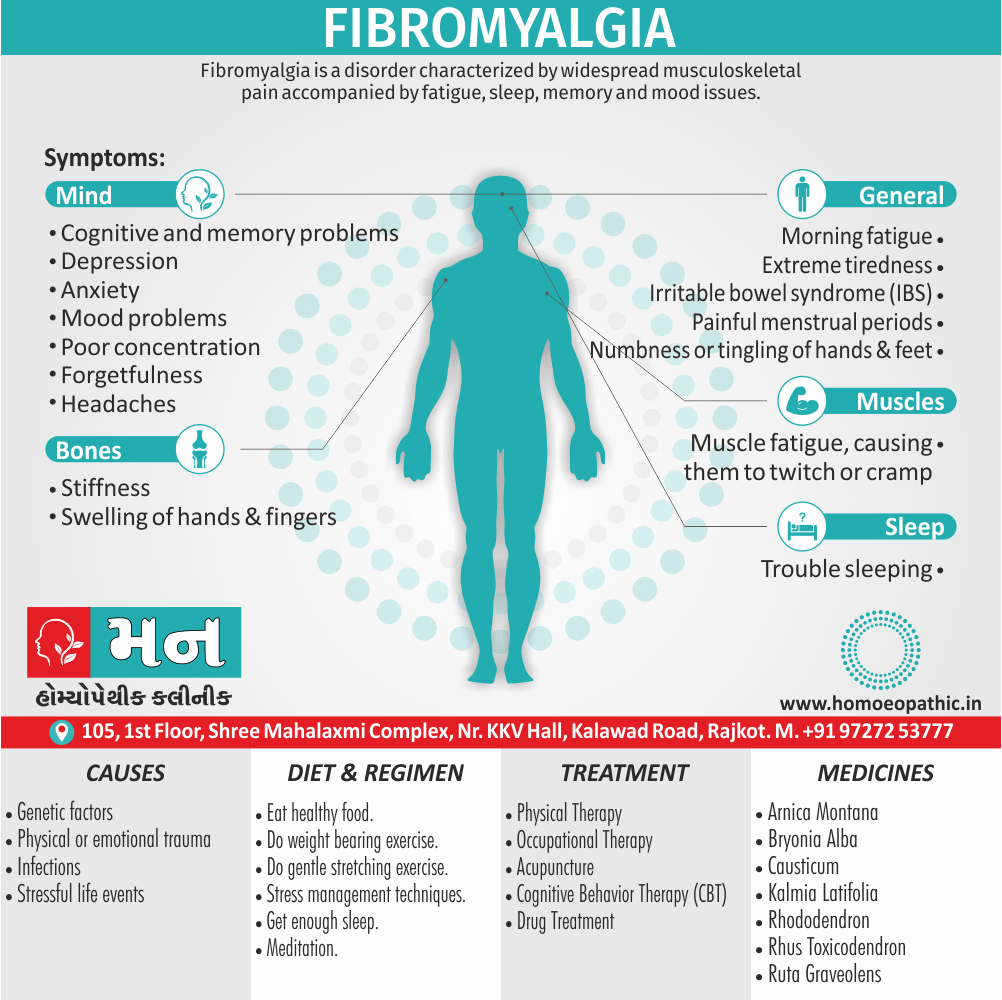
Fibromyalgia is a disorder characterized by widespread musculoskeletal pain accompanied by fatigue, sleep, memory also mood issues. [2]
There aren’t many exact synonyms for fibromyalgia, but here are some related terms used in the medical field:
- Diffuse myofascial pain syndrome: This term focuses on the widespread muscle pain characteristic of fibromyalgia.
- Fibromyalgia syndrome: This term emphasizes the constellation of symptoms associated with fibromyalgia, including fatigue, sleep problems, and cognitive difficulties.
- Fibromyalgia-fibromyositis syndrome: This is an older term that is no longer widely used. Fibromyalgia does not involve inflammation of the muscles (myositis).
- Fibromyositis: This term refers to inflammation of the muscles and connective tissues. It is not the same as fibromyalgia, although some people may use the terms interchangeably.
- Muscular rheumatism: This is a general term for pain in the muscles and joints, and it is not specific to fibromyalgia.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
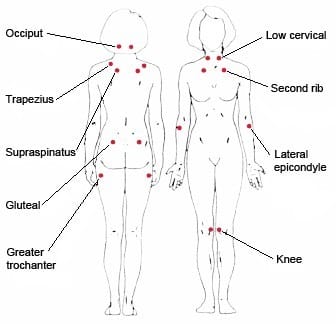
Fibromyalgia trigger points
Generally; This is a common cause of generalized regional pain and disability, and is frequently associated with medically unexplained symptoms in other systems.
Although fibromyalgia can occur at any age, including adolescence, additionally it increases in prevalence with age, to reach a peak of 7% in women aged over 70.
There is a strong female predominance of around 10 : 1.
Risk factors include life events that cause toxic social distress, such as marital disharmony, alcoholism in the family, injury or assault, low income and self reported childhood abuse.
It occurs in a wide variety of races also cultures. [1]
Symptoms resemble those of arthritis, but fibromyalgia affects the soft tissue, not the joints. [3]
Epidemiology
Epidemiology
The prevalence of fibromyalgia (FM) in India has been reported to be around 15% in patients with rheumatoid arthritis (RA) as per older American College of Rheumatology (ACR) FM Criteria (Dhir V, 2017). In a study using the 2016 revised ACR FM criteria, the prevalence was found to be 31% in RA patients and 4% in healthy controls (Dhir V, 2017).
Another study found a higher prevalence of FM in people with higher educational status (Clinical Features, Socio-cultural Characteristics, Sleep Patterns, and Depression in Fibromyalgia Patients from India: A Cross-Sectional Study, 2023).
However, in patients with systemic lupus erythematosus (SLE), FM was found to be distinctly uncommon (8.2%) (Fibromyalgia in Indian patients with SLE, 1998).
References:
- Dhir V. AB0281 THE 2016 REVISED ACR FIBROMYALGIA CRITERIA IDENTIFY A HIGHER PREVALENCE OF FIBROMYALGIA IN RHEUMATOID ARTHRITIS PATIENTS: A CROSS-SECTIONAL STUDY FROM INDIA. | Annals of the Rheumatic Diseases (2017) [5]
- Clinical Features, Socio-cultural Characteristics, Sleep Patterns, and Depression in Fibromyalgia Patients from India: A Cross-Sectional Study – The Open Rheumatology Journal (2023) [6]
- Fibromyalgia in Indian patients with SLE – PubMed (1998) [7]
Please note that these are just a few examples and the prevalence of fibromyalgia may vary depending on the population studied and the criteria used for diagnosis.
Causes
Causes
These factors include:
Infections:
- In general, Prior illnesses may trigger fibromyalgia or make symptoms of the condition worse.
Genetics:
- Fibromyalgia often runs in families.
- Furthermore; If you have a family member with this condition, your risk for developing it is higher.
- In detail, Researchers think certain genetic mutations may play a role in this condition.
- Lastly, Those genes haven’t yet been identified.
Trauma:
- People who experience either physical or emotional trauma may develop fibromyalgia.
- All in all, The condition has been linked with post-traumatic stress disorder.
Stress:
- Like trauma, stress can create long-reaching effects your body deals with for months and years.
- In detail, Stress has been linked to hormonal disturbances that could contribute to fibromyalgia.
Basically, Some theories suggest it may be that the brain lowers the pain threshold.
Another theory suggests that the nerves and receptors in the body become more sensitive to stimulation.
That means they may overreact to pain signals also cause unnecessary or exaggerated pain. [4]
Types
Types
While fibromyalgia itself is a specific syndrome, it doesn’t have distinct "types." However, fibromyalgia pain can manifest in different ways and affect various body areas. [8]
Risk Factors
Risk factors
- Gender: Women are more likely to develop fibromyalgia than men.
- Family History: Having a family member with fibromyalgia increases the risk.
- Other Conditions: Preexisting conditions like rheumatoid arthritis, lupus, or osteoarthritis can increase susceptibility.
- Stressful or Traumatic Events: Physical or emotional trauma can trigger fibromyalgia.
- Sleep Problems: Chronic sleep disturbances can increase the risk.
- Certain Infections: Some infections may trigger the onset of fibromyalgia.
In addition to these risk factors, the book also discusses other contributing factors, such as genetics, hormonal imbalances, and central nervous system dysfunction. [9]
Pathogenesis
Pathogenesis
The exact pathogenesis of fibromyalgia is still not fully understood, but it is believed to involve a complex interplay of genetic, neurological, hormonal, and environmental factors. A helpful resource that delves into the current understanding of fibromyalgia‘s pathogenesis is:
Fibromyalgia (1st Edition)
- Editors: Daniel Clauw, M.D. and Muhammad Yunus, M.D.
- Year of Publication: 2008
- Publisher: Lippincott Williams & Wilkins
This book provides a comprehensive overview of the various factors implicated in the development of fibromyalgia, including:
- Central Sensitization: This is a key mechanism where the central nervous system becomes overly sensitive to pain signals, leading to amplified pain perception.
- Dysregulation of Neurotransmitters: Imbalances in neurotransmitters like serotonin, norepinephrine, and dopamine can contribute to pain and other symptoms.
- Hormonal Abnormalities: Changes in hormone levels, particularly stress hormones like cortisol, may play a role.
- Genetic Predisposition: There is evidence to suggest a genetic component to fibromyalgia, although specific genes have not been identified.
- Environmental Triggers: Physical or emotional trauma, infections, and other stressors can potentially trigger or worsen fibromyalgia.
The book also discusses other potential mechanisms, such as abnormalities in the hypothalamic-pituitary-adrenal (HPA) axis, immune system dysfunction, and small fiber neuropathy.
While the book provides valuable insights into the current understanding of fibromyalgia‘s pathogenesis, it’s important to note that research in this area is ongoing, and new findings are continually emerging. Consulting with your healthcare provider is crucial for staying informed about the latest developments and receiving personalized guidance. [10]
Pathophysiology
Pathophysiology
Overview of the various factors implicated in the pathophysiology of fibromyalgia, including:
- Central Sensitization: This is a key mechanism where the central nervous system (brain and spinal cord) becomes overly sensitive to pain signals, leading to amplified pain perception.
- Dysregulation of Neurotransmitters: Imbalances in neurotransmitters like serotonin, norepinephrine, and dopamine, which are involved in pain regulation, mood, and sleep, can contribute to the diverse symptoms of fibromyalgia.
HPA Axis Dysfunction:The hypothalamic-pituitary-adrenal (HPA) axis, which plays a crucial role in the stress response, is often dysregulated in fibromyalgia, leading to abnormal stress hormone levels.
Autonomic Nervous System Dysfunction: The autonomic nervous system, which controls involuntary bodily functions like heart rate and digestion, can be disrupted in fibromyalgia, contributing to fatigue, sleep problems, and other symptoms
Neuroinflammation: There is growing evidence to suggest that low-grade inflammation in the nervous system may play a role in fibromyalgia.
Genetic Predisposition: While no specific gene has been identified, research suggests that genetic factors can increase susceptibility to fibromyalgia. [11]
Clinical Features
Clinical Features
- Widespread Pain: The hallmark symptom of fibromyalgia is widespread pain, often described as a constant dull ache lasting for at least three months. The pain can affect various body regions, including the muscles, joints, and soft tissues.
- Fatigue: People with fibromyalgia often experience persistent fatigue, even after adequate sleep. This fatigue can be debilitating and significantly impact daily functioning.
- Cognitive Difficulties: Often referred to as "fibro fog," cognitive difficulties are common in fibromyalgia and can include problems with memory, concentration, attention, and mental clarity.
- Sleep Disturbances: Many individuals with fibromyalgia have trouble falling asleep, staying asleep, or experiencing restorative sleep. This can further exacerbate fatigue and pain.
- Other Symptoms: Other common symptoms of fibromyalgia can include headaches, irritable bowel syndrome (IBS), anxiety, depression, numbness or tingling in the extremities, and sensitivity to light, noise, or temperature changes. [12]
Sign & Symptoms
Usual symptoms
- Multiple regional pain
- Marked fatigability
- Marked disability
- Broken, non-restorative sleep
- Low affect, irritability, also weepiness
- Poor concentration, forgetfulness
- Depression, Anxiety
Variable locomotor symptoms:
- Early morning stiffness
- Swelling of hands, also fingers
- Numbness, tingling of all fingers
Additional, variable, non-locomotor symptoms:
- Non-throbbing bifrontal headache (in other words; tension headache)
- Colicky abdominal pain, bloating, variable bowel habit (irritable bowel syndrome)
- Bladder fullness, nocturnal frequency (i.e. irritable bladder)
- Hyperacusis, dyspareunia, discomfort when touched (i.e. allodynia)
- Frequent side-effects with drugs (i.e. chemical sensitivity) [1]
Clinical Examination
Clinical Examination
While there is no specific clinical examination test to definitively diagnose fibromyalgia, a thorough physical examination and assessment of the patient’s history are crucial in establishing the diagnosis. [13]
Diagnosis
Diagnosis
There are no abnormalities on routine blood tests or imaging, but it is important to screen for other conditions that could contribute to some of the patient’s symptoms.
Minimum investigation screen in fibromyalgia:
Test | Condition screened |
Full blood count | Anaemia, Lymphopenia of SLE |
Erythrocyte sedimentation rate, C-reactive protein | Inflammatory disease |
Thyroid function | Hypothyroidism |
Calcium, Alkaline phosphate | Hyperparathyroidism also osteomalacia |
Antinuclear antibodies | SLE |
[1]
Differential Diagnosis
Differential Diagnosis
- Rheumatologic Conditions: Rheumatoid arthritis, lupus, ankylosing spondylitis, and polymyalgia rheumatica can present with similar symptoms like widespread pain, fatigue, and sleep disturbances.
- Infectious Diseases: Chronic infections like Lyme disease, hepatitis C, and HIV can also mimic the symptoms of fibromyalgia.
- Endocrine Disorders: Hypothyroidism, hyperparathyroidism, and Cushing’s syndrome can present with fatigue, muscle pain, and cognitive difficulties.
- Neurological Conditions: Multiple sclerosis, Parkinson’s disease, and peripheral neuropathy can cause pain, fatigue, and sensory disturbances.
- Psychiatric Disorders: Depression, anxiety, and somatic symptom disorder can often coexist with fibromyalgia, making it essential to differentiate between these conditions. [14]
Complications
Complications
Increased Pain and Fatigue: Fibromyalgia pain and fatigue can worsen over time, leading to increased disability and reduced functional capacity.
Sleep Problems: Chronic sleep disturbances associated with fibromyalgia can lead to daytime fatigue, cognitive impairment, and mood problems.
Depression and Anxiety: The chronic pain and fatigue of fibromyalgia often trigger or worsen depression and anxiety, creating a vicious cycle.
Reduced Quality of Life: The combination of pain, fatigue, sleep problems, and emotional distress can significantly impact a person’s quality of life, affecting their ability to work, socialize, and engage in activities they enjoy.
Cognitive Difficulties: Fibromyalgia is often associated with cognitive problems, including difficulty concentrating, memory problems, and mental fog, which can interfere with daily functioning.
Other Health Problems: People with fibromyalgia may be more likely to develop other health conditions, such as irritable bowel syndrome (IBS), migraines, interstitial cystitis, and temporomandibular joint (TMJ) disorders. [15]
Investigations
Investigations
There are no specific laboratory or imaging tests that can definitively diagnose fibromyalgia. However, certain investigations can help rule out other conditions and support the diagnosis.
Blood Tests: These can help rule out other conditions with similar symptoms, such as rheumatoid arthritis, lupus, thyroid problems, and vitamin D deficiency. Common blood tests include:
- Complete Blood Count (CBC): To check for anemia or infection.
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): To assess for inflammation.
- Thyroid Function Tests: To evaluate thyroid hormone levels.
- Vitamin D Levels: To check for deficiency.
Sleep Studies: Polysomnography or other sleep studies can help identify sleep disorders like sleep apnea or restless leg syndrome, which can contribute to fibromyalgia symptoms.
Imaging Studies: While imaging studies like X-rays, MRI scans, or CT scans are not routinely used to diagnose fibromyalgia, they can help rule out other conditions that may be causing pain or other symptoms.
Other Tests: Depending on the individual’s symptoms, other tests like nerve conduction studies, electromyography (EMG), or tilt table tests may be recommended to assess for neurological or autonomic nervous system dysfunction. [16]
Treatment
Treatment of Fibromyalgia
Medications:
Medications can help reduce the pain of fibromyalgia also improve sleep.
Common choices include:
Pain relievers:
- Over-the-counter pain relievers such as acetaminophen (e.g. Tylenol, others), ibuprofen (e.g. Advil, Motrin IB, others) or naproxen sodium (e.g. Aleve, others) may be helpful.
- Your doctor might suggest a prescription pain reliever such as tramadol (i.e. Ultram).
- Narcotics are not advised, because they can lead to dependence and may even worsen the pain over time.
Antidepressants:
- Duloxetine (Cymbalta) and milnacipran (Savella) may help ease the pain and fatigue associated with fibromyalgia.
- Your doctor may prescribe either amitriptyline or the muscle relaxant cyclobenzaprine to help promote sleep.
Anti-seizure drugs:
- Medications designed to treat epilepsy are often useful in reducing certain types of pain.
- Gabapentin (Neurontin) is sometimes helpful in reducing fibromyalgia symptoms, while pregabalin (Lyrica) was the first drug approved by the Food and Drug Administration to treat fibromyalgia.
Therapy:
Basically, A variety of different therapies can help reduce the effect that fibromyalgia has on your body and your life.
Examples include:
Physical therapy:
- A physical therapist can teach you exercises that will improve your strength, flexibility also stamina.
- Water-based exercises might be particularly helpful.
Occupational therapy:
- In general, An occupational therapist can help you make adjustments to your work area or the way you perform certain tasks that will cause less stress on your body.
Counseling:
- Talking with a counselor can help strengthen your belief in your abilities also teach you strategies for dealing with stressful situations. [2]
Exercise:
- A combination of aerobic exercise and resistance training, or strength training, has been linked to a reduction in pain, tenderness, stiffness, also sleep disturbance, in some patients.
- If exercise is helping with symptoms, it is important to maintain consistency in order to see progress.
- Working out with a either partner or personal trainer may help to keep the exercise program active.
Acupuncture:
- Generally, Some patients have experienced improvements in their quality of life after starting acupuncture therapy for fibromyalgia.
- The number of sessions required will depend on the symptoms also their severity.
- Besides this, One study found that 1 in 5 people with fibromyalgia use acupuncture within 2 years of diagnosis.
- All in all, The researchers concluded that it may improve pain also stiffness.
Behavior modification therapy:
- Behavior modification therapy is a form of cognitive behavioral therapy (in other words; CBT) that aims to reduce negative, either stress or pain increasing behaviors and improve positive, mindful behaviors.
- It includes learning new coping skills also relaxation exercises. [3]
Prevention
Prevention
As the exact cause of fibromyalgia is unknown, there is no definitive way to prevent it. However, some lifestyle modifications and proactive measures may help reduce the risk or minimize the severity of symptoms in predisposed individuals. [09]
Homeopathic Treatment
Homeopathic treatment of Fibromyalgia
Rhus toxicodendron:
- This is the rheumatism remedy.
- It is effective for pain and stiffness which is worse when having been still and gets better for getting moving, particularly bad after over doing things or in cold damp weather, eased by warmth and moderate exercise.
Ruta Graveolens:
- The remedy picture is similar to Rhus tox except that the stiffness is, if anything, more marked also less susceptible to improvement with gentle movement.
- In detail, There is often involvement of the tendons or the places where tendons meet bone (e.g. heels, elbows etc).
- Besides this, There is often a bruised feeling.
- Pains are worse for cold damp weather but without the definite benefit from warmth which is seen in Rhus tox.
Rhododendron:
- In brief, The picture is very similar to Rhus tox except that the pains are very much worse for changes in the weather, especially if there is an impending storm or thunderstorm.
Arnica:
- This medicine is best known for its action on injuries to reduce bruising also swelling.
- However, it is useful whenever the body feels bruised and sore, especially if markedly worse after exertion.
- A characteristic feeling described is of “the bed feeling too hard”, in other words, soreness and bruised feeling is worse if the part is lain upon.
- Arnica can be a good medicine to start treatment of fibromyalgia with, if there is not a clear picture suggesting another medicine at the onset.
Causticum:
- Again, soreness, weakness and stiffness, worse with exertion and cold, better for warm applications and being warm in bed.
- The unusual thing that might suggest Causticum is that the symptoms are worse especially in dry weather whereas better when it rains !
Bryonia Alba:
- For Bryonia to work, the pain must be very much worse especially for the slightest movement (the opposite of Rhus tox).
- Heat will aggravate the pain and pressure on the relevant part alleviates, possibly by preventing movement.
Kalmia Latifolia:
- This medicine is especially helpful for severe shooting pains in muscles, also there is often an accompanying numbness or cold sensation.
- Always make sure that there is no suggestion of either nerve pressure or damage, if these symptoms are present.
Cimicifuga:
- This medicine is used where the pains, soreness and stiffness are mostly in the neck and upper back muscles.
- These may have been preceded by an injury and are generally worse for cold or drafts.
- Symptoms are often accompanied by headaches, especially on the top of the head or radiating up from the neck. [4]
Diet & Regimen
Diet & Regimen
Stress Management: Chronic stress can exacerbate fibromyalgia symptoms. Practicing stress management techniques such as meditation, yoga, or mindfulness can help reduce stress levels and potentially lower the risk of developing fibromyalgia or experiencing flare-ups.
Regular Exercise: Engaging in regular physical activity, even low-impact exercises like walking or swimming, can help improve overall health, reduce pain, and enhance sleep quality.
Adequate Sleep: Prioritizing good sleep hygiene and aiming for 7-9 hours of quality sleep each night can help prevent fatigue and manage fibromyalgia symptoms.
Healthy Diet: Eating a balanced diet rich in fruits, vegetables, and whole grains can help maintain overall health and potentially reduce inflammation, which may play a role in fibromyalgia.
Early Intervention: If you experience persistent pain, fatigue, or other symptoms suggestive of fibromyalgia, seeking early medical evaluation and treatment can help prevent the condition from worsening. [9]
Do’s and Don'ts
The Do’s & Don’ts :
Do’s:
- Seek professional help: Consult with a doctor to get a proper diagnosis and create a personalized treatment plan.
- DO prioritize sleep: Aim for 7-9 hours of quality sleep each night, and establish a consistent sleep routine.
- DO exercise regularly: Engage in low-impact exercises like walking, swimming, or yoga, but listen to your body and avoid overexertion.
- Manage stress: Practice relaxation techniques such as meditation, deep breathing exercises, or spending time in nature.
- DO maintain a healthy diet: Eat a balanced diet rich in fruits, vegetables, whole grains, and lean protein, and avoid processed foods, sugar, and caffeine.
- DO connect with others: Join a support group or talk to a therapist to share your experiences and learn coping strategies.
- Pace yourself: Balance activity with rest, and avoid pushing yourself beyond your limits.
- DO track your symptoms: Keep a journal to track your pain, fatigue, and other symptoms, as well as any factors that may trigger or worsen them.
Don’ts:
- Not ignore your symptoms: If you are experiencing persistent pain, fatigue, or other symptoms, don’t dismiss them. Seek medical advice as soon as possible.
- DON’T compare yourself to others: Everyone experiences fibromyalgia differently. Don’t feel discouraged if your symptoms or treatment plan differ from others.
- DON’T give up: Fibromyalgia can be challenging, but it is manageable. Don’t lose hope, and keep trying different strategies until you find what works for you.
- Not isolate yourself: Social support is essential for coping with fibromyalgia. Don’t hesitate to reach out to friends, family, or support groups for help.
- DON’T self-medicate: Avoid using alcohol, drugs, or over-the-counter medications to cope with your symptoms. Talk to your doctor about safe and effective treatment options.
- DON’T overexert yourself: While exercise is important, it’s crucial to avoid pushing yourself too hard. Listen to your body and rest when needed.
- Not neglect your mental health: Fibromyalgia can take a toll on your emotional well-being. Don’t hesitate to seek help from a therapist or counselor if you are struggling with anxiety, depression, or other mental health concerns.
Terminology
Terminology
Core Terminology:
- Fibromyalgia (FM): A chronic pain disorder characterized by widespread musculoskeletal pain, fatigue, sleep disturbances, and cognitive difficulties.
- Chronic Widespread Pain (CWP): Pain that is experienced in multiple areas of the body for a prolonged period.
- Tender Points: Specific areas of the body that are painful to touch in individuals with fibromyalgia. While no longer the primary diagnostic criteria, they can still be clinically relevant.
- Widespread Pain Index (WPI): A scoring system used to assess the number of body areas where a person experiences pain.
- Symptom Severity (SS) Scale: A scale used to assess the severity of fatigue, waking unrefreshed, and cognitive symptoms in fibromyalgia.
Pathophysiology Terminology:
- Central Sensitization: A key mechanism in fibromyalgia where the central nervous system becomes overly sensitive to pain signals, leading to amplified pain perception.
- Neurotransmitters: Chemical messengers in the brain that play a role in pain regulation and other functions. Imbalances in neurotransmitters like serotonin, norepinephrine, and dopamine are often observed in fibromyalgia.
- HPA Axis: The hypothalamic-pituitary-adrenal axis, a complex system that regulates the body’s stress response. Dysregulation of the HPA axis is implicated in fibromyalgia.
- Neuroinflammation: Low-grade inflammation in the nervous system, which may contribute to fibromyalgia symptoms.
Other Relevant Terms:
- Comorbidities: Additional medical conditions that often coexist with fibromyalgia, such as irritable bowel syndrome (IBS), migraines, or anxiety disorders.
- Fibro Fog: A term used to describe the cognitive difficulties experienced by people with fibromyalgia, including problems with memory, concentration, and mental clarity.
- Flare-Up: A temporary worsening of fibromyalgia symptoms.
- Multidisciplinary Treatment: An approach to fibromyalgia management that involves a combination of medication, physical therapy, cognitive behavioral therapy (CBT), and other interventions.
Core Homeopathic Terms:
- Remedy: A substance, often diluted and potentized, used in homeopathy to treat a specific condition based on the principle of "like cures like."
- Potency: The number of times a homeopathic remedy has been diluted and succussed (shaken), indicating its strength.
- Constitutional Type: The individual’s unique physical, mental, and emotional characteristics, which guide the selection of the most appropriate remedy.
- Repertorization: The process of analyzing a patient’s symptoms and matching them to remedies listed in a homeopathic repertory (a reference book of symptoms and corresponding remedies).
- Aggravation: A temporary worsening of symptoms after taking a remedy, which can be a sign that the remedy is working.
- Amelioration: An improvement in symptoms after taking a remedy.
Fibromyalgia-Specific Terms:
- Vital Force: The innate energy that governs the body’s healing processes, which homeopaths believe can be disrupted in fibromyalgia.
- Miasm: A predisposition to certain types of diseases, including chronic conditions like fibromyalgia, that is believed to be inherited and can influence the choice of remedies.
- Suppression: The suppression of symptoms by conventional medicine, which homeopaths believe can push the disease deeper and create more chronic problems.
Examples of Homeopathic Remedies Used in Fibromyalgia:
- Arnica: For muscle pain, soreness, and bruising.
- Rhus Toxicodendron: For pain that is worse with rest and better with movement.
- Bryonia: For pain that is worse with the slightest movement.
- Caulophyllum: For menstrual cramps and hormonal imbalances that can worsen fibromyalgia symptoms.
- Kali Phosphoricum: For fatigue, anxiety, and depression associated with fibromyalgia.
Additional Terms in Homeopathic Literature:
- Proving: A systematic study of a substance’s effects on healthy individuals to determine its potential as a homeopathic remedy.
- Law of Similars: The principle that a substance that can cause symptoms in a healthy person can cure similar symptoms in a sick person.
- Individualization: The process of tailoring treatment to the specific needs of each patient, based on their unique symptoms and constitutional type.
References
References
- Davidson’s Principles and Practice of Medicine (22nd edition) Ch. 25
- https://www.mayoclinic.org/diseases-conditions/fibromyalgia/diagnosis-treatment/drc-20354785
- https://www.medicalnewstoday.com/articles/147083.php
- https://www.britishhomeopathic.org/charity/how-we-can-help/articles/conditions/f/fibromyalgia/
- Dhir V. AB0281 THE 2016 REVISED ACR FIBROMYALGIA CRITERIA IDENTIFY A HIGHER PREVALENCE OF FIBROMYALGIA IN RHEUMATOID ARTHRITIS PATIENTS: A CROSS-SECTIONAL STUDY FROM INDIA. | Annals of the Rheumatic Diseases (2017)
- Clinical Features, Socio-cultural Characteristics, Sleep Patterns, and Depression in Fibromyalgia Patients from India: A Cross-Sectional Study – The Open Rheumatology Journal (2023)
- Fibromyalgia in Indian patients with SLE – PubMed (1998)
- The Fibromyalgia Manual: A Complete Guide to Treatment (3rd Edition) by Devin J. Starlanyl, MD (2015) Published by, Johns Hopkins University Press
- The FibroManual: A User’s Guide to Fibromyalgia (2nd Edition) by Ginevra Liptan, MD (2018) , published by Ballantine Books
- Fibromyalgia (1st Edition), Editors: Daniel Clauw, M.D. and Muhammad Yunus, M.D. (2008) Published by Lippincott Williams & Wilkins
- Fibromyalgia: Up-to-Date (1st Edition), edited by Robert M. Bennett, M.D. (2011), Published by Oxford University Press
- The Trigger Point Therapy Workbook: Your Self-Treatment Guide for Pain Relief (3rd Edition), by Clair Davies, Amber Davies, and David G. Simons(2018), Published by New Harbinger Publications
- Fibromyalgia: A Practical Clinical Guide (1st Edition), by Dawn A. Marcus, MD, and Atul Deodhar, MD, MRCP (2010) Published by Springer Science+Business Media
- Fibromyalgia Syndrome: A Practitioner’s Guide to Treatment (1st Edition), by I. Jon Russell, MBChB, MRCP, FRCP (2009). Published By Humana Press
- The Fibromyalgia Advocate: Getting the Support You Need to Cope, Fight, and Heal (1st Edition). Author: Devin J. Starlanyl, MD (2010), Published by New Harbinger Publications
- Fibromyalgia and Chronic Fatigue Syndrome: The Complete Guide to Getting Well (1st Edition) by Martin L. Pall, PhD (2007), Published by Haworth Medical Press
Also Search As
Also Searched As
Online Search Engines:
- Use search terms like "homeopathy fibromyalgia," "homeopathic remedies fibromyalgia," or "homeopathic treatment fibromyalgia" in search engines like Google, DuckDuckGo, or Bing.
- Look for articles on reputable homeopathic websites, blogs, or online journals.
- Be sure to check the author’s credentials and the date of publication to ensure the information is current and reliable.
Homeopathic Databases and Journals:
- Search databases like the National Center for Homeopathy (NCH) or the Homeopathic Educational Services (HES) for articles on fibromyalgia.
- Look for peer-reviewed journals such as The American Journal of Homeopathic Medicine or Homeopathy.
Homeopathic Organizations and Clinics:
- Visit the websites of homeopathic organizations like the NCH or the Council for Homeopathic Certification (CHC). They often have resources and articles available.
- Contact local homeopathic clinics or practitioners to inquire about research or articles they recommend.
Social Media:
- Join online forums and groups dedicated to homeopathy or fibromyalgia. Members may share articles or discuss their experiences with homeopathic treatment.
- Follow homeopathic practitioners or organizations on social media platforms like Facebook, Twitter, or Instagram for updates and information.
Libraries:
- Visit your local library or university library and ask the librarian for assistance in finding relevant books or journals on homeopathy and fibromyalgia.
There are several ways to search for information on fibromyalgia, using various resources and platforms:
1. Online Search Engines:
- General Search: Use search engines like Google, Bing, or DuckDuckGo with keywords like "fibromyalgia," "fibromyalgia symptoms," "fibromyalgia treatment," or "fibromyalgia causes." This will yield a wide range of results, including websites, articles, news, and videos.
- Specific Websites: Search directly on reputable health websites like Mayo Clinic, Cleveland Clinic, National Institutes of Health (NIH), or dedicated fibromyalgia organizations like the National Fibromyalgia Association (NFA). These sites often provide reliable, comprehensive information on the condition.
2. Academic Databases:
- PubMed: This database provides access to a vast collection of biomedical literature, including research articles, reviews, and clinical trials on fibromyalgia.
- Google Scholar: This search engine specializes in academic literature and can help you find scholarly articles and studies related to fibromyalgia.
3. Social Media:
- Support Groups: Search for fibromyalgia support groups on platforms like Facebook or Reddit to connect with others who have the condition. These groups can be a valuable source of information, support, and personal experiences.
- Hashtags: Use relevant hashtags like #fibromyalgia, #fibrowarrior, or #fibromyalgiaawareness on platforms like Twitter or Instagram to find posts and discussions about fibromyalgia.
4. Books and Publications:
- Medical Libraries: Visit your local or university library for books and journals on fibromyalgia. Librarians can help you navigate the resources available.
- Online Bookstores: Search for books on fibromyalgia on platforms like Amazon or Barnes & Noble. Look for books written by medical professionals or experts in the field.
5. Medical Professionals:
- Consult Your Doctor: Your primary care physician or a rheumatologist can provide reliable information, diagnosis, and treatment options for fibromyalgia.
- Specialist Clinics: Seek out clinics or centers that specialize in fibromyalgia for comprehensive evaluation and management of the condition.
Frequently Asked Questions (FAQ)
What is Fibromyalgia?
Fibromyagia is a disorder characterized by widespread musculoskeletal pain accompanied by fatigue, sleep, memory also mood issues.
What causes Fibromyalgia?
- Prior illnesses
- Genetics
- physical or emotional trauma
- Stress
Is fibromyalgia a disability?
Fibromyalgia can be disabling for some individuals, significantly impacting their ability to work and perform daily activities. In such cases, it may be considered a disability and qualify individuals for certain benefits or accommodations.
Can fibromyalgia be cured?
Currently, there is no cure for fibromyalgia. However, with proper management, individuals can significantly improve their symptoms and quality of life.
Can homeopathy help with fibromyalgia?
Yes, many people with fibromyalgia find relief with homeopathy. It aims to address the root cause of the individual’s symptoms, promoting overall healing rather than just suppressing pain.
What are the symptoms of Fibromyalgia?
- Multiple regional pain
- Marked fatigability
- Marked disability
- Broken, also non-restorative sleep
- Low affect, irritability, weepiness
- Poor concentration, also forgetfulness
- Depression, Anxiety
Is homeopathic treatment safe for fibromyalgia?
Yes, homeopathic remedies are generally safe and have no known side effects when taken as directed by a qualified practitioner.
What are the treatment options for fibromyalgia?
Treatment typically involves a combination of medication (pain relievers, antidepressants, anticonvulsants), physical therapy, exercise, cognitive behavioral therapy (CBT), and lifestyle modifications like stress management and good sleep hygiene.
How does homeopathic treatment for fibromyalgia work?
Homeopathy works by stimulating the body’s innate healing abilities. Remedies are chosen based on the individual’s unique symptom pattern and constitutional type, aiming to restore balance and reduce pain.
Which homeopathic remedies are commonly used for fibromyalgia?
There are many remedies used depending on individual symptoms. Some common ones include Arnica (for muscle pain), Rhus Tox (for pain worse with rest), Bryonia (for pain worse with movement), and Kali Phos (for fatigue and mental exhaustion).
Homeopathic Medicines used by Homeopathic Doctors in treatment of Fibromyalgia?
Homeopathic Medicines
- Rhus Toxicodendron
- Ruta Graveolens
- Rhododendron
- Arnica
- Causticum
- Bryonia Alba
- Kalmia Latifolia
- Cimicifuga
