Psoriasis
Definition
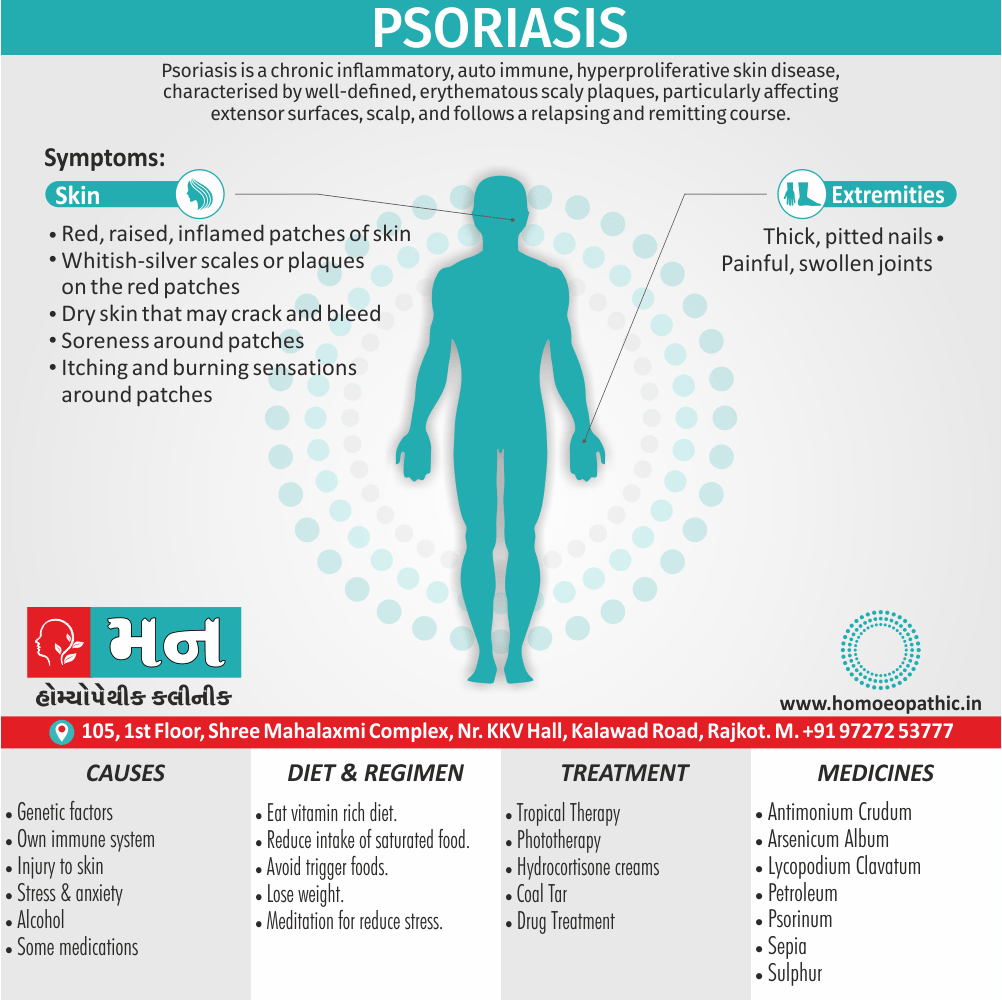
Psoriasis is a chronic inflammatory, auto immune, hyperproliferative skin disease, characterised by well-defined, erythematous scaly plaques, particularly affecting extensor surfaces and scalp, and usually follows a relapsing and remitting course. [1]
It is a chronic skin condition and there aren’t many direct synonyms for it. However, there are some related terms you might encounter depending on the context:
Types
- Plaque psoriasis (most common type characterized by red, scaly patches)
- Guttate psoriasis (small, teardrop-shaped lesions)
- Inverse psoriasis (smooth, red patches in skin folds)
- Pustular psoriasis (white pustules on red, inflamed skin)
- Erythrodermic psoriasis (widespread redness, scaling, and inflammation)
- Psoriatic arthritis (joint pain and inflammation that can occur with psoriasis)
- Dermatosis (technical term for any skin condition. Dermatosis is a disease of the skin, especially one that does not cause inflammation.)
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
It is a chronic autoimmune disease that causes skin cells to grow too quickly, resulting in thick, scaly patches on the skin’s surface. These patches can be itchy, painful, and sometimes even embarrassing. While there’s no cure, various treatments can help manage symptoms and improve quality of life.[1]
Epidemiology
Epidemiology
According to the study "Psoriasis in India: Prevalence and pattern" published in the Indian Journal of Dermatology, Venereology and Leprology in 2010, the prevalence of psoriasis in India varies from 0.44% to 2.8%. It is twice more common in males compared to females, and most of the patients are in their third or fourth decade at the time of presentation.[2]
Causes
Causes
It is a complex condition with multiple contributing factors. While the exact cause remains unknown, it is widely believed to be an autoimmune disease triggered by a combination of genetic and environmental factors.
Key Factors:
- Genetics: A family history of significantly increases the risk of developing the condition. Certain genes have been linked to psoriasis, suggesting a strong hereditary component.
- Immune System: In psoriasis, the immune system mistakenly attacks healthy skin cells, leading to their rapid overgrowth. T cells, a type of white blood cell, play a crucial role in this process.
- Environmental Triggers: Various environmental factors can trigger or worsen psoriasis flare-ups. These include stress, infections, skin injuries, certain medications, and smoking.[3]
Types
Types
Plaque Psoriasis
- Description: This is the most common type of psoriasis, affecting about 80% of people with the condition.It is characterized by raised, red patches of skin covered with silvery scales. These patches are often itchy and painful, and they can occur anywhere on the body, but are most commonly found on the elbows, knees, scalp, and lower back.
Guttate Psoriasis
- Description: This type of psoriasis typically appears as small, drop-shaped, red spots on the skin. It often develops after a strep throat infection and is more common in children and young adults.
Pustular Psoriasis
- Description: This type of psoriasis is characterized by white pustules (blisters of noninfectious pus) surrounded by red skin. It can occur on any part of the body but is most common on the palms of the hands and soles of the feet.
Inverse Psoriasis
- Description: This type of psoriasis occurs in the folds of the skin, such as the armpits, groin, and under the breasts. It is characterized by smooth, red lesions that are often uncomfortable and may be worsened by friction and sweating.
Erythrodermic Psoriasis
- Description: This is a rare but very serious type of psoriasis that affects most of the body’s surface. It causes widespread redness, scaling, and shedding of the skin. Erythrodermic psoriasis can be life-threatening and requires immediate medical attention.
Other Types
- Nail Psoriasis: Affects the fingernails and toenails, causing pitting, discoloration, and thickening of the nails.
- Psoriatic Arthritis: A type of arthritis that can develop in people with psoriasis, causing pain, stiffness, and swelling in the joints.
- Scalp Psoriasis: This affects the scalp, causing red, itchy, and scaly patches.
Risk Factors
Risk Factors of Psoriasis
Several factors can increase the likelihood of developing psoriasis or experiencing flare-ups. Recognizing these risk factors can aid in prevention and management strategies.
Key Risk Factors:
- Family History: A strong genetic predisposition exists for psoriasis, with individuals having a parent or sibling with the condition being at a significantly higher risk.
- Infections: Certain infections, particularly strep throat, can trigger the onset of guttate psoriasis, especially in children and young adults.
- Skin Injury: Trauma to the skin, like cuts, scrapes, burns, or even tattoos, can provoke the Koebner phenomenon, where psoriasis develops at the site of injury.
- Stress: Emotional stress can trigger or worsen psoriasis symptoms, highlighting the importance of stress management techniques.
Other Risk factors
- Smoking & Alcohol: Smoking and heavy alcohol consumption are associated with an increased risk of developing psoriasis and more severe disease.
- Obesity: Excess weight can contribute to psoriasis severity and may hinder treatment effectiveness.
- Medications: Certain medications, including lithium, beta-blockers, and antimalarials, can trigger or exacerbate psoriasis in some individuals.[5]
Pathogenesis
Pathogenesis
It is a complex interplay of genetic predisposition, immune dysregulation, and environmental triggers leading to characteristic skin changes. Understanding its pathogenesis is crucial for developing targeted therapies.
Key Elements in Pathogenesis:
- Genetic Susceptibility: Specific genes associated with immune function and skin barrier regulation increase an individual’s risk of developing psoriasis.
- Immune Dysregulation: The immune system becomes overactive, with T cells (a type of white blood cell) mistakenly attacking healthy skin cells. This triggers inflammation and excessive skin cell growth.
- Keratinocyte Hyperproliferation: The abnormal immune response leads to rapid proliferation of keratinocytes (skin cells), causing thickening and scaling of the skin.
- Angiogenesis: New blood vessels form in the affected skin, contributing to redness and inflammation.
- Environmental Triggers: Factors like stress, infections, injury, and certain medications can initiate or exacerbate the inflammatory process in genetically predisposed individuals.[5]
Pathophysiology
Pathophysiology
It is a chronic inflammatory skin disease characterized by accelerated keratinocyte proliferation, immune cell infiltration, and vascular changes. Understanding its pathophysiology aids in comprehending the clinical manifestations and developing targeted treatments.
Key Processes in Pathophysiology:
- Hyperproliferation of Keratinocytes: In psoriasis, keratinocytes (skin cells) divide and mature at an abnormally rapid rate, leading to the accumulation of thick, scaly plaques on the skin’s surface.
- Immune Cell Infiltration: The skin becomes infiltrated with various immune cells, including T cells, dendritic cells, and macrophages, which release inflammatory cytokines and perpetuate the inflammatory process.
- Inflammation: The release of inflammatory mediators leads to vasodilation, increased blood flow, and the recruitment of more immune cells to the affected skin, further amplifying the inflammatory response.
- Angiogenesis: New blood vessels form in the inflamed skin, contributing to redness and providing nutrients for the rapidly dividing keratinocytes.
- Altered Skin Barrier Function: The disrupted skin barrier allows for increased water loss and penetration of irritants, exacerbating inflammation and itching.[6]
Clinical Features
Clinical features of Psoriasis
It is presents with various clinical features, depending on the type and severity of the condition. Recognizing these manifestations is crucial for accurate diagnosis and appropriate management.
Common Clinical Features:
- Plaques: The hallmark of psoriasis, these are well-demarcated, red patches covered in silvery scales. They commonly appear on the elbows, knees, scalp, and lower back.
- Itching & Burning: It plaques can be itchy and sometimes painful, significantly impacting quality of life.
- Nail Changes: It can affect nails, leading to pitting, thickening, discoloration, and even separation from the nail bed (onycholysis).
- Joint Pain: It arthritis affects up to 30% of individuals with psoriasis, causing joint pain, stiffness, and swelling.
- Scalp Involvement: It manifests as thick, scaly patches on the scalp, often extending beyond the hairline.
- Other Manifestations: It can also affect the palms and soles (palmoplantar psoriasis), skin folds (inverse psoriasis), or cause widespread redness and inflammation (erythrodermic psoriasis).[7]
Sign & Symptoms
Sign & Symptoms of Psoriasis
It is manifests with a variety of signs and symptoms, which can vary in severity and presentation depending on the type and extent of the condition. Recognizing these manifestations is crucial for early diagnosis and timely management.
Common Signs & Symptoms:
- Red, Scaly Patches: These are the hallmark of psoriasis, appearing as raised, inflamed patches covered in silvery-white scales. They often occur on the elbows, knees, scalp, and lower back.
- Itching & Burning: It lesions can be itchy, and in some cases, may also cause a burning or stinging sensation.
- Dry, Cracked Skin: The affected skin may become dry and cracked, sometimes even bleeding.
- Thickened Nails:It can affect the nails, leading to pitting, discoloration, thickening, and separation from the nail bed.
- Joint Pain & Stiffness: Psoriatic arthritis, a form of inflammatory arthritis, can develop in some individuals with psoriasis, causing joint pain, swelling, and stiffness.[8]
Clinical Examination
Clinical Examination
A thorough clinical examination is essential for diagnosing psoriasis and assessing its severity and impact on the patient. Dermatologists employ various techniques to evaluate the characteristic skin lesions and identify any associated complications.
Key Components of the Examination:
- Visual Inspection: The dermatologist carefully examines the skin, noting the distribution, size, shape, and color of the psoriatic plaques. They also assess the scalp, nails, and joints for signs of involvement.
- Palpation: The dermatologist gently palpates the plaques to assess their thickness, texture, and tenderness. They may also check for signs of inflammation, such as warmth or swelling.
- Auscultation: If joint involvement is suspected, the dermatologist may use a stethoscope to listen for any signs of inflammation or fluid accumulation in the affected joints.
- Dermoscopy: This technique involves using a handheld magnifying device to examine the skin lesions in greater detail, aiding in differentiating psoriasis from other skin conditions.
- Assessment of Severity: The dermatologist evaluates the extent of skin involvement, using tools like the Psoriasis Area and Severity Index (PASI) to quantify the severity of the disease.
- Assessment of Impact: The dermatologist inquires about the patient’s quality of life, including the impact of psoriasis on their physical, emotional, and social well-being.[9]
Diagnosis
Diagnosis
It is typically involves a combination of clinical assessment, patient history, and sometimes additional tests to rule out other skin conditions. Accurate diagnosis is crucial for tailoring appropriate treatment plans and managing the disease effectively.
Key Elements of Diagnosis:
- Clinical Presentation: The dermatologist carefully examines the patient’s skin, looking for characteristic psoriatic lesions, such as red, scaly plaques on typical locations like the elbows, knees, scalp, and lower back.
- Patient History: The dermatologist inquires about the patient’s medical history, family history of psoriasis, any triggers or exacerbating factors, and the impact of the condition on their quality of life.
- Dermoscopy: A handheld magnifying device may be used to examine the skin lesions in greater detail, helping to differentiate psoriasis from other conditions like eczema or fungal infections.
- Biopsy: In some cases, a small skin sample (biopsy) may be taken for microscopic examination to confirm the diagnosis, especially if the presentation is atypical or other conditions are suspected.
- Blood Tests: Blood tests may be ordered to rule out psoriatic arthritis or other autoimmune conditions that can sometimes coexist with psoriasis.
- Imaging Studies: If joint involvement is suspected, X-rays or other imaging studies may be performed to assess the extent of joint damage.[10]
Differential Diagnosis
Differential Diagnosis
It can sometimes mimic other skin conditions, necessitating a careful differential diagnosis to ensure accurate treatment. Consideration of various possibilities is crucial for effective management.
Common Differential Diagnoses:
- Eczema: Eczema often presents with red, itchy patches, but it typically lacks the thick, silvery scales characteristic of psoriasis. Eczema tends to affect flexural areas (skin folds) more commonly than psoriasis.
- Lichen Planus: This inflammatory skin condition causes purplish, flat-topped bumps that may be itchy. Unlike psoriasis, lichen planus often affects the wrists, ankles, and mucous membranes.
- Tinea Corporis (Ringworm): This fungal infection causes circular or oval patches with raised borders and central clearing. It can be distinguished from psoriasis by its characteristic appearance and positive fungal culture.
- Seborrheic Dermatitis: This condition causes greasy, yellow scales on the scalp, face, and chest. It can be differentiated from psoriasis by its location and lack of thick, silvery scales.
- Pityriasis Rosea: This self-limiting condition causes a "herald patch" followed by a widespread rash of smaller, scaly lesions. It typically resolves on its own within a few weeks.[11]
Complications
Complications
While primarily a skin condition, psoriasis can lead to various complications affecting physical and mental health. Recognizing and addressing these potential issues is crucial for comprehensive patient care.
Common Complications:
- Psoriatic Arthritis: This inflammatory arthritis affects joints, causing pain, stiffness, and swelling. It can lead to joint damage and disability if left untreated.
- Cardiovascular Disease: It is associated with an increased risk of heart disease, stroke, and other cardiovascular conditions. Managing cardiovascular risk factors is essential for people with psoriasis.
- Metabolic Syndrome: This cluster of conditions, including obesity, high blood pressure, high blood sugar, and abnormal cholesterol levels, is more prevalent in people with psoriasis and can increase the risk of heart disease and diabetes.
- Depression & Anxiety: The visible nature of psoriasis and its impact on quality of life can contribute to mental health issues like depression and anxiety.
- Other Complications: It can also lead to eye problems, sleep disturbances, and social isolation.[12]
Investigations
Investigations
While a diagnosis of psoriasis is often made clinically based on the characteristic appearance of the skin lesions, certain investigations can help confirm the diagnosis, assess disease severity, rule out other conditions, and monitor treatment response.
Common Investigations:
- Dermoscopy: A handheld magnifying device allows for detailed examination of the skin lesions, revealing characteristic features like pinpoint bleeding points (Auspitz sign) that support a psoriasis diagnosis.
- Biopsy: A small skin sample is taken and examined under a microscope to confirm the diagnosis, particularly in atypical presentations or when other conditions are suspected.
- Blood Tests: Blood tests may be ordered to assess for signs of inflammation (e.g., C-reactive protein, erythrocyte sedimentation rate) or to rule out psoriatic arthritis (e.g., rheumatoid factor, anti-cyclic citrullinated peptide antibodies).
- Imaging Studies: X-rays, ultrasounds, or MRIs may be used to evaluate joint involvement in cases of suspected psoriatic arthritis.
- Severity Assessment Tools: Standardized tools like the Psoriasis Area and Severity Index (PASI) and the Dermatology Life Quality Index (DLQI) help quantify the extent and impact of the disease.[4]
Treatment
Treatment
It is treatment aims to control symptoms, improve quality of life, and prevent complications. The choice of treatment depends on factors like disease severity, location of lesions, patient preferences, and potential side effects.
Common Treatment Options:
Topical Therapies: These are applied directly to the skin and include:
- Corticosteroids: Reduce inflammation and slow skin cell growth.
- Vitamin D Analogs: Slow skin cell growth and reduce inflammation.
- Coal Tar: Decreases scaling and itching.
- Retinoids: Normalize skin cell growth.
Phototherapy: Exposure to ultraviolet (UV) light can slow skin cell growth and reduce inflammation. Types include:
- Narrowband UVB: Targets specific wavelengths of UVB light.
- PUVA: Combines UVA light with a medication called psoralen.
Systemic Medications: These oral or injected medications are used for moderate to severe psoriasis:
- Methotrexate: Suppresses the immune system.
- Cyclosporine: Suppresses the immune system.
- Biologics: Target specific parts of the immune system involved in psoriasis.
Lifestyle Modifications: These can complement medical treatments and improve overall health:
- Stress Management: Techniques like meditation and yoga can help reduce stress and flare-ups.
- Moisturizing: Keeping skin well-moisturized can help reduce itching and scaling.
- Avoiding Triggers: Identifying and avoiding triggers like infections, skin injuries, and certain medications can help prevent flare-ups.[13]
Prevention
Prevention
1. Minimize Triggers:
- Skin Injuries: Avoid cuts, scrapes, and harsh scrubbing, as skin trauma can trigger the Koebner phenomenon, where psoriasis develops at the injury site.
- Infections: Promptly treat infections, especially strep throat, which can trigger guttate psoriasis.
- Stress: Practice stress management techniques like exercise, yoga, meditation, or deep breathing to reduce flare-ups.
- Certain Medications: Some medications, like lithium, antimalarials, and beta-blockers, may worsen psoriasis. Discuss potential side effects with your doctor.
- Smoking: Smoking increases your risk of developing psoriasis and can make symptoms worse.
- Excessive Alcohol: Limit alcohol consumption as it can trigger flare-ups.
2. Maintain a Healthy Lifestyle:
- Healthy Weight: Obesity can increase the risk of psoriasis and make symptoms worse. Maintain a healthy weight through diet and exercise.
- Balanced Diet: Eat a nutritious diet rich in fruits, vegetables, and whole grains. Some people find that limiting nightshade vegetables (tomatoes, potatoes, peppers, eggplant), gluten, or dairy may help.
- Sunlight: Moderate sun exposure can be beneficial, but avoid sunburn. Always use sunscreen with an SPF of 30 or higher.
- Hydration: Drink plenty of water to keep your skin hydrated.
3. Skincare:
- Moisturize: Use a thick, oil-based moisturizer regularly, especially after showering or bathing, to prevent dry skin.
- Gentle Cleansing: Use mild, fragrance-free soaps and cleansers. Avoid harsh scrubbing.
- Lukewarm Water: Bathe or shower in lukewarm water, not hot water.
- Humidifier: Use a humidifier to add moisture to the air, especially during dry months.
4. Early Intervention:
- Family History: If you have a family history of psoriasis, be aware of the early signs and symptoms.
- Dermatologist: See a dermatologist for early diagnosis and treatment to help manage the condition and prevent it from becoming severe.
Homeopathic Treatment
Homoeopathic Treatment
Homeopathy offers a holistic approach to managing psoriasis, focusing on individualizing treatment based on the patient’s unique symptoms and constitutional makeup. While research on homeopathy for psoriasis is limited, anecdotal evidence and some clinical studies suggest potential benefits in reducing symptom severity and improving quality of life.
Commonly Used Homeopathic Remedies:
- Sulphur: Often indicated for dry, itchy, and burning skin with a tendency for scratching and aggravation from warmth.
- Arsenicum Album: Considered for dry, scaly, and inflamed skin with restlessness and anxiety.
- Graphites: May be helpful for thick, cracked skin with a tendency for bleeding and oozing.
- Petroleum: Often used for dry, rough, and cracked skin aggravated by cold weather.
- Psorinum: Considered a "nosode" prepared from psoriatic scales and may be used in cases where other remedies fail to provide significant relief.
Important Considerations:
- Individualization: Homeopathic treatment is highly individualized, and the choice of remedy depends on the patient’s specific symptoms and overall constitution.
- Consultation with a Qualified Practitioner: It’s essential to consult a qualified homeopathic practitioner for proper assessment and prescription of the most suitable remedies.
- Complementary Approach: Homeopathy can be used as a complementary therapy alongside conventional medical treatment for psoriasis.[13]
Diet & Regimen
Diet & Regimen of Psoriasis
While there’s no specific certain dietary and lifestyle choices can help manage symptoms, reduce inflammation, and promote overall well-being. Adopting a healthy regimen complements medical treatment and empowers individuals to take an active role in managing their condition.
Dietary Recommendations:
- Anti-Inflammatory Foods: Emphasize fruits, vegetables, whole grains, and healthy fats (omega-3 fatty acids from fish, nuts, and seeds). These foods contain antioxidants and anti-inflammatory compounds that may help reduce psoriasis flare-ups.
- Limit Trigger Foods: Some individuals may find that certain foods trigger or worsen their symptoms. Common culprits include alcohol, red meat, processed foods, and sugary drinks. Keeping a food diary can help identify personal triggers.
- Weight Management: Maintaining a healthy weight is crucial, as obesity can worsen psoriasis symptoms. A balanced diet and regular exercise are key components of weight management.
- Vitamins and Supplements: While research is ongoing, some studies suggest that vitamin D and fish oil supplements may benefit people with psoriasis. Consult your doctor before starting any new supplements.
Lifestyle Recommendations:
- Stress Management: Stress is a known trigger for psoriasis flare-ups. Incorporate stress-reducing activities like meditation, yoga, or spending time in nature into your routine.
- Regular Exercise: Exercise promotes overall health and may help reduce psoriasis severity. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Adequate Sleep: Sleep deprivation can worsen psoriasis symptoms. Strive for 7-8 hours of quality sleep each night.
- Skin Care: Gentle skin care is essential. Avoid harsh soaps and hot water, and moisturize regularly to keep skin hydrated.[14]
Do’s and Don'ts
Do’s & Don’ts
Psoriasis Do’s and Don’ts
Do’s:
- Moisturize Regularly: Keep your skin well-hydrated with thick creams or ointments to reduce dryness, cracking, and itching. Apply moisturizer immediately after bathing to lock in moisture.
- Take Lukewarm Baths/Showers: Avoid hot water, which can irritate and dry out your skin. Opt for lukewarm water and gentle, fragrance-free soaps.
- Follow Your Treatment Plan: Adhere to your prescribed medications and therapies as directed by your dermatologist. Consistency is key to managing psoriasis effectively.
- Manage Stress: Stress can trigger flare-ups, so practice stress-reducing techniques like meditation, yoga, or spending time in nature.
- Get Regular Exercise: Exercise promotes overall health and may help reduce psoriasis severity. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Other Do’s
- Protect Your Skin: Avoid skin injuries, as they can trigger psoriasis in susceptible individuals (Koebner phenomenon).
- Eat a Healthy Diet: Focus on fruits, vegetables, whole grains, and lean protein. Some people find that avoiding trigger foods like alcohol, red meat, and processed foods helps reduce flare-ups.
- Get Adequate Sleep: Aim for 7-8 hours of quality sleep each night, as sleep deprivation can worsen psoriasis symptoms.
- Join a Support Group: Connecting with others who have psoriasis can provide emotional support and valuable information about managing the condition.
Don’ts:
- Scratch or Pick at Lesions: This can worsen inflammation, increase the risk of infection, and lead to scarring.
- Use Harsh Soaps or Cleansers: Avoid harsh soaps, fragrances, and other irritants that can dry out and aggravate your skin.
- Smoke or Drink Excessively: Smoking and heavy alcohol consumption can worsen psoriasis and increase the risk of complications.
- Skip Doctor’s Appointments: Regular follow-ups with your dermatologist are crucial for monitoring your condition and adjusting treatment as needed.
- Let Psoriasis Control Your Life: While It can be challenging, don’t let it dictate your life. Stay positive, focus on self-care, and seek support when needed.
Terminology
Terminology
Psoriasis:
A chronic autoimmune disease that causes skin cells to grow too quickly, leading to the buildup of thick, scaly patches on the skin’s surface.
Plaques:
The raised, red, scaly patches characteristic of psoriasis.
Keratinocytes:
The predominant cell type in the epidermis (outer layer of skin). In psoriasis, these cells multiply too rapidly, leading to plaque formation.
Inflammation:
A localized physical condition in which part of the body becomes reddened, swollen, hot, and often painful, especially as a reaction to injury or infection. In psoriasis, the immune system triggers inflammation in the skin.
Autoimmune Disease:
A condition in which the body’s immune system mistakenly attacks its own healthy tissues. Psoriasis is considered an autoimmune disease.
T cells:
A type of white blood cell that plays a central role in the immune response. In psoriasis, T cells become overactive and trigger inflammation in the skin.
Cytokines:
Small proteins released by cells that have a specific effect on the interactions and communications between cells. In psoriasis, certain cytokines promote inflammation.
Comorbidities:
The presence of one or more additional diseases or conditions co-occurring with a primary disease or condition. It is associated with several comorbidities, such as psoriatic arthritis, cardiovascular disease, and metabolic syndrome.
Psoriatic Arthritis:
An inflammatory arthritis that affects some people with psoriasis, causing joint pain, stiffness, and swelling.
Topical Treatments:
Medications applied directly to the skin to treat psoriasis, such as corticosteroids, vitamin D analogs, and coal tar.
Systemic Treatments:
Medications taken orally or by injection that work throughout the body to treat psoriasis, such as methotrexate, cyclosporine, and biologics.
Phototherapy:
A treatment for psoriasis that involves exposing the skin to ultraviolet light.
Flare-ups:
Periods when symptoms worsen.
Remission:
A period when symptoms improve or disappear.
Quality of Life:
The general well-being of individuals and societies. Psoriasis can significantly impact a person’s quality of life due to physical discomfort, emotional distress, and social stigma.
Miasm:
In homeopathy, a miasm refers to a predisposing constitutional weakness or taint that underlies chronic disease. Understanding the patient’s miasm is crucial for selecting appropriate remedies. Psoriasis is often associated with the psoric and sycotic miasms.
Totality of Symptoms:
This refers to the complete picture of the patient’s physical, mental, and emotional symptoms, as well as their modalities (factors that make symptoms better or worse). Homeopathic treatment aims to address the totality of symptoms rather than just the physical manifestations of psoriasis.
Repertory:
A reference book used by homeopaths to find remedies based on specific symptoms and their modalities. The repertory lists remedies associated with various symptoms, helping to narrow down the choices for a particular patient.
Materia Medica:
A comprehensive collection of information about homeopathic remedies, including their sources, preparation, and symptom picture. The materia medica helps homeopaths understand the characteristic effects of each remedy and choose the most suitable one for a given patient.
Potency:
The strength or dilution of a homeopathic remedy. Homeopathic remedies are prepared through a process of serial dilution and succussion (vigorous shaking), and higher potencies are believed to have deeper and longer-lasting effects.
Aggravation:
A temporary worsening of symptoms after taking a homeopathic remedy, often considered a positive sign indicating the remedy is working.
Amelioration:
An improvement or relief of symptoms after taking a homeopathic remedy.
Constitutional Remedy:
A remedy that matches the patient’s overall constitution, including their physical, mental, and emotional characteristics. A well-chosen constitutional remedy can address the underlying susceptibility to psoriasis and promote long-term healing.
Nosode:
A homeopathic remedy prepared from diseased tissue or secretions. Psorinum, a nosode prepared from psoriatic scales, is sometimes used in the treatment of psoriasis.
Suppression:
In homeopathy, suppression refers to the suppression of symptoms without addressing the underlying cause of disease. It’s believed that suppressing symptoms can lead to deeper health issues in the long run. Homeopathy aims to stimulate the body’s healing response rather than suppressing symptoms.
References
References
- Fitzpatrick’s Dermatology in General Medicine (9th Edition)
Authors: Klaus Wolff, Lowell A. Goldsmith, Stephen I. Katz, Barbara A. Gilchrest, Amy S. Paller, David J. Leffell, 2019
Publisher: McGraw-Hill Education / Medical - "Psoriasis in India: Prevalence and pattern" published in the Indian Journal of Dermatology, Venereology and Leprology in 2010
- Andrews’ Diseases of the Skin: Clinical Dermatology (13th Edition)
Authors: William D. James, Timothy G. Berger, Dirk M. Elston
,2020, Publisher: Elsevier - Bolognia JL, Schaffer JV, Cerroni L. Dermatology (4th Edition)
Authors: Jean L. Bolognia, Joseph L. Jorizzo, Julie V. Schaffer
,2018, Publisher: Elsevier - Rook’s Textbook of Dermatology (10th Edition)
Authors: Christopher Griffiths, Jonathan Barker, Tanya Bleiker, Richard Chalmers, Fiona Creamer, Neil Cox, Sarah Hogan, Daniel Lackenby, Hywel Williams
,2020, Publisher: Wiley-Blackwell - Lever’s Histopathology of the Skin (11th Edition)
Authors: David Weedon
,2016, Publisher: Lippincott Williams & Wilkins - Clinical Dermatology: A Color Guide to Diagnosis and Therapy (6th Edition)
Authors: Thomas P. Habif
,2016, Publisher: Elsevier - Dermatology: 2-Volume Set (4th Edition)
Authors: Jean L. Bolognia, Joseph L. Jorizzo, Julie V. Schaffer
,2018, Publisher: Elsevier - Dermatology: An Illustrated Colour Text (6th Edition)
Authors: David J. Gawkrodger, Fiona J. Curley, Mark R. Richards, Peter J. Milligan
,2016, Publisher: Churchill Livingstone - Clinical Dermatology (6th Edition)
Authors: Thomas P. Habif, Michael J. Dinulos, James G. H. Dinulos
,2021, Publisher: Elsevier - Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology (8th Edition)
Authors: Klaus Wolff, Richard Allen Johnson, Dick Suurmond
,2017, Publisher: McGraw-Hill Education / Medical. - Kelley and Firestein’s Textbook of Rheumatology (11th Edition)
Editors: Gary S. Firestein, Ralph C. Budd, Sherine E. Gabriel, Iain B. McInnes, James R. O’Dell
,2021, Publisher: Elsevier - Homoeopathic Therapeutics (8th Edition)
Author: Samuel Lilienthal
,2010 (Reprint)
Publisher: B. Jain Publishers - The Psoriasis and Psoriatic Arthritis Pocket Guide (5th Edition)
Authors: The National Psoriasis Foundation, 2019,Publisher: National Psoriasis Foundation
Also Search As
Also Search As
People can search for homeopathic articles on psoriasis using a variety of online resources and strategies. Here are some effective ways:
Search Engines:
Use Specific Keywords:
Homeopathic Websites and Databases:
National Center for Homeopathy (NCH):
- The NCH website has a resources section with articles, research summaries, and links to other relevant organizations.
British Homeopathic Association (BHA):
- The BHA website has a library of articles and research related to homeopathy.
Homeopathy Research Institute (HRI):
- The HRI website provides access to a database of research studies on homeopathy.
Social Media and Online Forums:
Homeopathy Groups and Pages:
- Search for homeopathy groups and pages on platforms like Facebook and LinkedIn. These platforms often share articles and discuss homeopathic approaches to various health conditions.
Online Forums:
- Participate in online health forums specifically dedicated to homeopathy.
Tips for Effective Searching:
Be specific:
- The more specific your search terms, the more relevant the results will be.
Use a variety of sources:
- Consult multiple sources to get a well-rounded understanding of homeopathic approaches to psoriasis.
Be critical:
- Evaluate the quality and credibility of the information you find. Look for articles from reputable sources and be wary of anecdotal evidence.
Additional Points to Consider:
Consult a Homeopath:
- For personalized advice and treatment for psoriasis, it’s recommended to consult a qualified homeopathic practitioner.
By utilizing these strategies and resources, individuals interested in learning more about homeopathy for psoriasis can access a wealth of valuable information.
There are numerous ways to search for information on psoriasis, catering to various needs and preferences. Here’s a breakdown of the different avenues for exploration:
Online Search Engines:
General Search Engines: Using popular search engines like Google, Bing, or DuckDuckGo, you can simply type in "psoriasis" or more specific queries like "psoriasis symptoms", "psoriasis treatment", "psoriasis causes" etc. This will yield a wide array of websites, articles, images, and videos related to psoriasis.
Medical Websites & Databases: Explore reliable medical websites such as Mayo Clinic, Cleveland Clinic, WebMD, National Psoriasis Foundation, etc. These platforms provide comprehensive and evidence-based information on psoriasis, including its types, causes, symptoms, diagnosis, and treatment options. You can often filter your searches by specific topics or keywords within these sites.
Academic & Research Resources:
Medical Journals & Databases: If you are seeking in-depth, scientific information on psoriasis, delve into medical journals and databases like PubMed, Google Scholar, or Cochrane Library. These resources offer access to research articles, clinical trials, and expert reviews on psoriasis.
Books & E-books: Libraries and online bookstores offer a wide selection of medical textbooks and e-books dedicated to dermatology or specifically psoriasis. These resources can provide a comprehensive overview of the condition, its management, and latest advancements in research.
Social Media & Online Communities:
Support Groups & Forums: Online communities and forums offer a space to connect with other individuals living with psoriasis. You can share experiences, seek advice, and learn about coping strategies. Look for groups on platforms like Facebook, Reddit, or dedicated psoriasis support websites.
Social Media Hashtags: Follow relevant hashtags like #psoriasis, #psoriasisawareness, #psoriasiscommunity on platforms like Instagram and Twitter to discover posts, articles, and discussions related to psoriasis.
Healthcare Professionals:
Consult Your Dermatologist: Your dermatologist is the primary source of reliable and personalized information about your condition. They can answer your specific questions, offer guidance on treatment options, and provide support in managing your psoriasis.
Seek Second Opinions: If you seek further insights or alternative perspectives, consider consulting another dermatologist or specialist in psoriasis.
Remember:
Evaluate Sources Critically: Always evaluate the credibility and reliability of the sources you find. Look for information from reputable medical organizations, research institutions, and healthcare professionals. Be cautious of anecdotal evidence or unverified claims.
Prioritize Your Needs: Choose the search methods that align best with your information needs and preferences. If you prefer visual content, videos and images may be helpful. For in-depth research, academic resources may be more suitable.
Stay Updated: Psoriasis research and treatment options are constantly evolving. Stay informed about the latest developments by following reliable sources and engaging with online communities.
Frequently Asked Questions (FAQ)
What is psoriasis?
Definition
Psoriasis is a chronic autoimmune disease that accelerates skin cell growth, causing red, scaly patches on the skin’s surface. These patches can be itchy, painful, and even affect joints in some cases (psoriatic arthritis).
Is psoriasis contagious?
No, psoriasis is not contagious. It cannot be spread from person to person through touch or any other form of contact.
What causes psoriasis?
Causes
The exact cause of psoriasis is unknown, but it is believed to be an autoimmune disorder triggered by a combination of genetic and environmental factors.
Can homeopathy cure psoriasis?
While some individuals experience significant improvement or even complete remission with homeopathic treatment, the concept of a "cure" in homeopathy is different from conventional medicine. Homeopathy focuses on restoring balance and promoting overall health, which can lead to long-term symptom management and reduced flare-ups.
