Vitiligo
Definition
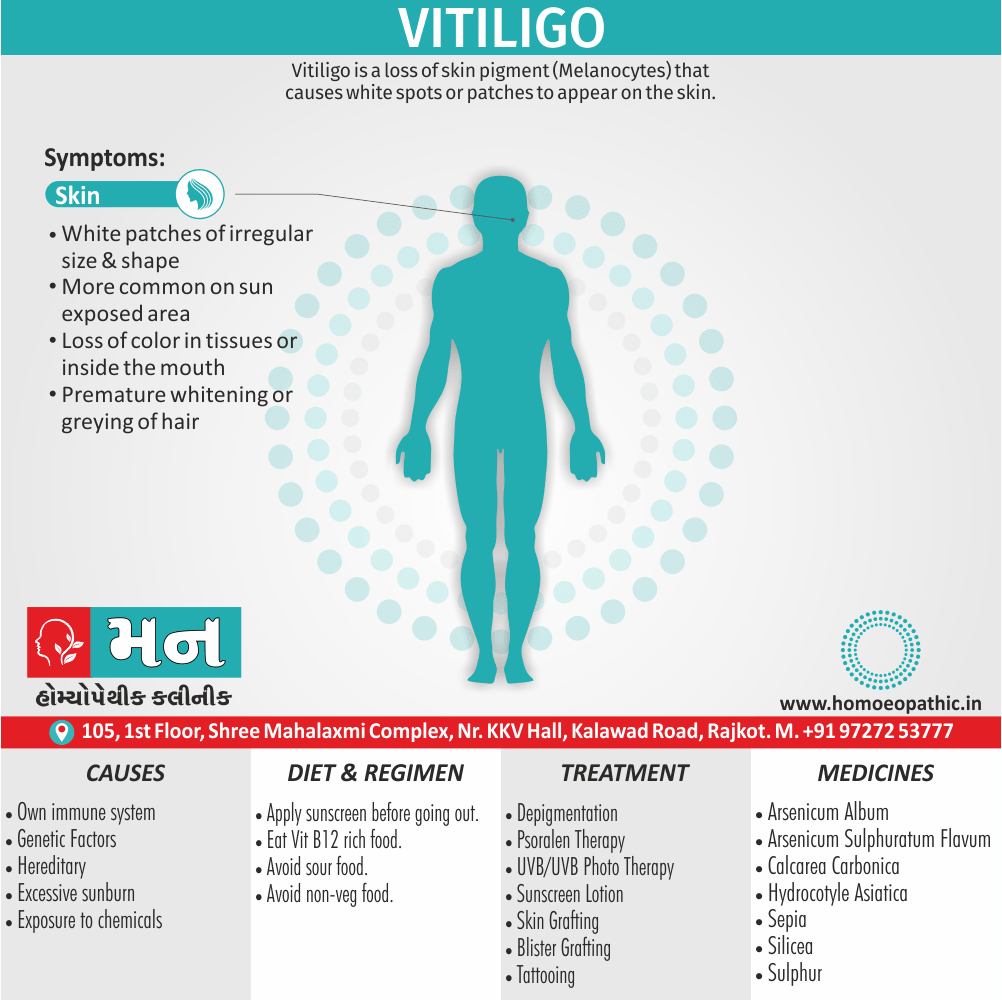
Vitiligo is a loss of skin pigment (Melanocytes) that causes white spots or patches to appear on the skin. [3]
Vitiligo is a specific medical term for a skin condition. It does not have exact synonyms, but you could refer to it as:
- Leukoderma: This is a broader term referring to any condition causing loss of skin pigmentation.
- Piebaldism: This is a rare genetic disorder causing patches of white skin, often from birth. While related, it’s distinct from vitiligo.
- Depigmentation disorder: This is a general term encompassing various conditions leading to skin pigment loss, including vitiligo.
Please note that these are not perfect synonyms, as each term has slightly different meanings and uses.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Vitiligo:
- Vitiligo is an acquire condition affecting 1% of the population worldwide.
- Focal loss of melanocytes results in the development of patches of hypopigmentation.
- A positive family history of vitiligo is relatively common in those with extensive disease, and this type is also associate with other autoimmune diseases.
- Trauma and sunburn may precipitate the appearance of vitiligo.
- The pathogenesis is unclear and, whilst melanocytes may be the target of a cell-mediated autoimmune attack, it is not known why only focal areas are affected. [1]
- The extent and rate of color loss from vitiligo is unpredictable.
- It can affect the skin on any part of your body & may also affect hair and the inside of the mouth.
- Normally, the color of hair and skin is determine by melanin.
- Vitiligo occurs when the cells that produce melanin die or stop functioning.
- Vitiligo affects people of all skin types, but it may more noticeable in people with darker skin.
- The condition is not life-threatening or contagious.
- It can stressful or make you feel bad about yourself.
- Treatment for vitiligo may restore color to the affected skin.
- But it does not prevent continued loss of skin color or a recurrence. [2]
Epidemiology
Epidemiology of Vitiligo:
The epidemiology of vitiligo in India is characterized by a high prevalence, with estimates ranging from 0.46% to 8.8% (Clinical and sociodemographic study of vitiligo, 2009). Some studies have reported even higher incidence rates, such as 8.8% in Delhi (Epidemiological profile of vitiligo in Northern India – Journal of Applied Pharmaceutical Science). The wide variation in prevalence may be attributed to factors such as differing ethnic backgrounds, geographical locations, and environmental conditions across the country.
Additionally, certain regions in India, like Gujarat and Rajasthan, exhibit notably high prevalence rates, sometimes described as epidemic proportions (Clinical and sociodemographic study of vitiligo, 2009).[7][8]
Causes
Causes of Vitiligo:
These include:
- An autoimmune disorder, in which the immune system becomes overactive and destroys the melanocytes
- Genetic oxidative stress imbalance
- A stressful event
- Harm to the skin due to a critical sunburn or cut
- Exposure to some chemicals
- Heredity, as it may run in families
- Virus
Vitiligo is not contagious. One person cannot catch it from another.
It can appear at any age, but studies suggest that it is more likely to start around the age of 20 years. [4]
Types
Types of Vitiligo:
Non-segmental vitiligo:
If the first white patches are symmetrical, this suggests a type of vitiligo known as non-segmental vitiligo.
The development will be slower than if the patches are in only one area of the body.
Non-segmental vitiligo is the most common type, accounting for up to 90 percent of cases.
The patches often appear equally on both sides of the body, with some measure of symmetry.
They often appear on skin that is commonly exposed to the sun, such as the face, neck, and hands.
Common areas include i.e.:
- Backs of the hands
- Arms
- Eyes
- Knees
- Elbows
- Feet
- Mouth
- Armpit and groin
- Nose
- Navel
- Genitals and rectal area
Non-segmental vitiligo is further broken down into subcategories i.e.:
- Generalized: There is no specific area or size of patches. This is the most common type.
- Acrofacial: This occurs mostly on the fingers or toes.
- Mucosal: This appears mostly around the mucous membranes and lips.
- Universal: Depigmentation covers most of the body. This is very rare.
- Focal: One, or a few, scattered white patches develop in a discrete area. It most often occurs in young children.
Segmental vitiligo:
- Segmental vitiligo spreads more rapidly but is consider more constant and stable and less erratic than the non-segmental type.
- It is much less common and affects only about 10 percent of people with vitiligo.
- It is non-symmetrical.
- And more noticeable in early age groups, affecting about 30 percent of children diagnosed with vitiligo.
- Segmental vitiligo usually affects areas of skin attached to nerves arising in the dorsal roots of the spine.
- Responds well to topical treatments. [4]
Risk Factors
Risk Factors Vitiligo:
- Family History: Having a close relative with vitiligo increases the likelihood of developing the condition.
- Autoimmune Diseases: People with other autoimmune disorders, such as Hashimoto’s thyroiditis, type 1 diabetes, or pernicious anemia, are at a higher risk.
- Stressful Events: Significant emotional or physical stress can trigger or worsen vitiligo.
- Sunburn or Skin Trauma: Severe sunburn or injury to the skin can sometimes lead to the development of vitiligo patches.
- Exposure to Certain Chemicals: Contact with specific industrial chemicals may increase the risk.[9]
Pathogenesis
Pathogenesis of Vitiligo:
- Autoimmune: The predominant hypothesis posits that vitiligo is primarily an autoimmune disorder. Cytotoxic T lymphocytes target and destroy melanocytes, leading to the characteristic depigmented patches. Evidence supporting this includes the presence of autoantibodies against melanocyte antigens, the association of vitiligo with other autoimmune diseases, and the responsiveness of some patients to immunomodulatory therapies.
- Oxidative Stress: Increased oxidative stress within melanocytes is another key factor in vitiligo pathogenesis. This imbalance between reactive oxygen species (ROS) and antioxidant defenses can damage melanocyte cellular components, including DNA and mitochondria, ultimately leading to cell death.
- Genetic Predisposition: Genetic susceptibility plays a role in vitiligo development. Several genes associated with immune regulation and melanocyte function have been identified as risk factors. These genes may influence an individual’s susceptibility to autoimmune responses or the ability of melanocytes to withstand oxidative stress.
- Environmental Triggers: While the primary cause is likely autoimmune, environmental factors can trigger or exacerbate vitiligo in susceptible individuals. These triggers may include physical trauma, chemical exposure, emotional stress, or even certain medications.[10]
Pathophysiology
Pathophysiology of Vitiligo:
- Association with other autoimmune diseases: Vitiligo frequently coexists with conditions like autoimmune thyroid disease, pernicious anemia, and type 1 diabetes, suggesting a shared autoimmune predisposition.
- Presence of autoantibodies: Circulating antibodies against melanocyte antigens, such as tyrosinase and melan-A, have been detected in patients with vitiligo.
- Inflammatory infiltrate: Histological examination of vitiliginous skin often reveals a lymphocytic infiltrate surrounding and destroying melanocytes.
- Response to immunosuppressive therapy: Some patients experience repigmentation with treatments that modulate the immune system, such as corticosteroids and topical calcineurin inhibitors.[11]
Clinical Features
Clinical Features of Vitiligo:
Depigmented Macules and Patches:
- The hallmark of vitiligo is the appearance of well-demarcated, depigmented macules and patches on the skin. These areas lack melanin pigment, resulting in a stark contrast with the surrounding normal skin.
Distribution:
- The distribution of vitiligo lesions can vary widely. Common patterns include:
Generalized:
- Widespread involvement of the body surface.
Acrofacial:
- Primarily affecting the face and extremities.
Segmental:
- Limited to one side of the body or a specific dermatome.
Focal:
- A few isolated lesions.
Mucosal:
- Involvement of mucous membranes, such as the lips or genitals.
Progression:
- The course of vitiligo is unpredictable. Lesions may remain stable for years, spread slowly, or rapidly enlarge. New lesions may appear over time.
Associated Features:
- Vitiligo may be associated with other autoimmune or inflammatory conditions, such as thyroid disease, pernicious anemia, or alopecia areata.
Koebner Phenomenon:
- In some individuals, new vitiligo lesions may develop at sites of injury or trauma, a phenomenon known as the Koebner phenomenon.
Trichrome Vitiligo:
- A less common presentation where a zone of partially depigmented skin surrounds the completely depigmented areas.
Quadrichrome Vitiligo:
- An even rarer variant with four distinct shades of pigmentation: normal, partially depigmented, completely depigmented, and hyperpigmented.
Inflammation:
- In some cases, vitiligo lesions may exhibit signs of inflammation, such as redness or itching.
Hair Depigmentation:
- Hair within vitiligo patches may also lose pigment, turning white or gray.[12]
Sign & Symptoms
Sign And Symptoms of Vitiligo:
Usually, the discoloration first shows on sun-exposed areas, such as the hands, feet, arms, face and lips.
- Generalised vitiligo is often symmetrical and involves hands, wrists, knees also neck, as well as areas around body orifices.
- The hair of the scalp, beard, eyebrows and lashes may also depigment.
- Segmental vitiligo is restrict to one part of the body but not necessarily a dermatome.
- The patches of depigmentation are sharply define, and in Caucasians may surrounded by hyperpigmentation.
- Spotty perifollicular pigment may seen within the depigmentation and is often the first sign of repigmentation.
- Sensation in the depigmented patches is normal.
- Wood’s light examination enhances the contrast between pigmented and non-pigmented skin.
- The course is unpredictable but most patches remain static or enlarge; a few repigment spontaneously.[1]
Clinical Examination
Clinical Examination:
- Distribution: Note the pattern of vitiligo, whether it is focal, segmental, generalized, or universal.
- Morphology: Observe the size, shape, and borders of the lesions. Vitiligo typically presents with well-demarcated, chalk-white macules or patches.
- Associated findings: Look for signs of other autoimmune diseases, such as thyroid disorders or alopecia areata. Also, check for evidence of Koebner phenomenon (new lesions appearing at sites of trauma).
- Wood’s lamp examination: Using a Wood’s lamp can help to better visualize the extent of depigmentation, especially in individuals with lighter skin tones.[13]
Diagnosis
Diagnosis:
Medical history and examination:
If your doctor suspects you have vitiligo, he will ask about your medical history, examine you and try to rule out other medical problems, such as dermatitis or psoriasis.
He may use a special lamp to shine ultraviolet light onto the skin to determine whether you have vitiligo.
Skin biopsy and blood draw:
In addition to gathering your personal and family medical history and examining your skin, your doctor may:
- Take a small sample (biopsy) of the affected skin.
- Draw blood for lab tests to look for underlying autoimmune conditions, such as anemia or diabetes. [2]
Differential Diagnosis
Differential Diagnosis:
Postinflammatory Hypopigmentation:
- This occurs after skin inflammation or injury, such as eczema or psoriasis. The hypopigmented patches often have irregular borders and may gradually repigment over time.
Pityriasis Alba:
- This common condition in children and young adults presents with hypopigmented patches on the face and upper arms. The patches are often scaly and have indistinct borders.
Tinea Versicolor:
- This fungal infection causes hypopigmented or hyperpigmented patches on the trunk and upper arms. The patches may be scaly and have a fine, powdery appearance.
Nevus Depigmentosus:
- This congenital birthmark presents as a hypopigmented patch with well-defined borders. The patch usually remains stable in size and does not change over time.
Leprosy:
- This infectious disease can cause hypopigmented patches with sensory loss. The patches may have raised borders and be associated with nerve thickening.
Chemical Leukoderma:
- Exposure to certain chemicals can cause hypopigmentation. The patches often have well-defined borders and may be associated with a history of chemical exposure.
Tuberous Sclerosis:
- This genetic disorder can cause hypopigmented patches known as ash-leaf macules. The patches are often oval-shaped and have well-defined borders.[11]
Complications
Complications :
Physical Complications:
Sunburn and Skin Cancer: The loss of melanin in vitiligo-affected areas leaves the skin vulnerable to sunburn and increases the risk of developing skin cancer. It’s crucial to use sunscreen with a high SPF and seek shade whenever possible.
Eye Problems: Vitiligo can also affect the eyes, leading to inflammation of the uvea (uveitis) and an increased risk of cataracts and glaucoma. Regular eye exams are essential for early detection and treatment of any eye-related complications.
Hearing Loss: Studies suggest a potential link between vitiligo and hearing loss, although more research is needed to fully understand this connection. If you experience any changes in your hearing, consult an audiologist.
Psychological Complications:
Social Stigma and Low Self-Esteem: The visible nature of vitiligo can lead to social stigma, discrimination, and low self-esteem. This can impact social interactions, relationships, and overall quality of life.
Anxiety and Depression: The emotional challenges associated with vitiligo can contribute to anxiety and depression. Seeking support from mental health professionals or support groups can be beneficial in managing these psychological complications.[13]
Investigations
Investigations :
Wood’s Lamp Examination:
- Helps to accentuate subtle hypopigmentation and identify areas of subclinical involvement.
- Lesions appear brighter under the Wood’s lamp due to the absence of melanin.
Skin Biopsy:
- Confirms the diagnosis, especially in atypical presentations or when other conditions are suspected.
- Reveals an absence of melanocytes in the epidermis.
Blood Tests:
- May be performed to rule out associated autoimmune conditions such as thyroid disease, pernicious anemia, or Addison’s disease.
- Thyroid function tests (TSH, T3, T4) and complete blood count (CBC) are commonly ordered.[11]
Treatment
Treatment :
Many treatments are available to help restore skin color or even out skin tone.
Results vary and are unpredictable.
Some treatments have serious side effects. So your doctor may suggest that you first try improving the appearance of your skin by applying self-tanning products or makeup.
Medications:
No drug can stop the process of vitiligo – the loss of pigment cells (melanocytes). But some drugs, used alone or with light therapy, can help restore some skin tone.
Creams that control inflammation i.e.:
- Applying a corticosteroid cream to affected skin may help return color, particularly if you start using it early in the disease.
- You may not see a change in your skin’s color for several months.
- This type of cream is effective and easy to use.
- But it can cause side effects, such as skin thinning or the appearance of streaks or lines on your skin.
- Milder forms of the drug may prescribed for children and for people who have large areas of discolored skin.
Medications that affect the immune system i.e.:
- Ointments containing tacrolimus or pimecrolimus (calcineurin inhibitors) may effective for people with small areas of depigmentation, especially on the face and neck.
- This treatment may have fewer side effects than corticosteroids and can be used with ultraviolet B (UVB) light.
- However, the Food and Drug Administration has warned about a possible link between these drugs and lymphoma and skin cancer.
Therapies:
Combining psoralen and light therapy i.e.:
- This treatment combines a plant-derived substance called psoralen with light therapy (photochemotherapy) to return color to the light patches.
- After you take psoralen by mouth or apply it to the affected skin, you’re exposed to ultraviolet A (UVA), UVB light or excimer light.
- These approaches tend to have better results than just medication or just light.
- You may need to repeat treatments up to three times a week for six to 12 months.
Removing the remaining color (depigmentation) i.e.:
- This therapy may be an option if your vitiligo is widespread and other treatments haven’t worked.
- A depigmenting agent is applied to unaffected areas of skin.
- This gradually lightens it so that it blends with the discolored areas.
- The therapy is done once or twice a day for nine months or longer.
- Side effects can include redness, swelling, itching and dry skin.
- Depigmentation is permanent, and you’ll always be extremely sensitive to sunlight.
Surgery:
It may be an option for you if light therapy doesn’t work. Surgery can also be used with those therapies. The goal of the following techniques is to even out your skin tone by restoring color.
Skin grafting i.e.:
- In this procedure, your doctor removes very small sections of your normal, pigmented skin also attaches them to areas that have lost pigment.
- This procedure is sometimes used if you have small patches of vitiligo.
- Possible risks include infection, scarring, a cobblestone appearance, spotty color also failure of the area to recolor.
Blister grafting i.e.:
- In this procedure, your doctor creates blisters on your pigmented skin, usually with suction.
- They then removes the tops of the blisters and transplants them to an area of discolored skin.
- Possible risks include scarring, a cobblestone appearance and failure of the area to recolor. And the skin damage caused by suctioning may trigger another patch of vitiligo.
Tattooing (micropigmentation) i.e.:
- In this technique, your doctor uses a special surgical instrument to implant pigment into your skin.
- It’s most effective in and around the lips in people with darker complexions.
- Drawbacks include difficulty matching the skin color and potential for the tattooing to trigger another patch of vitiligo.
Potential future treatments:
A drug to stimulate color-producing cells (melanocytes) i.e.:
- In brief, Called afamelanotide, this potential treatment is implanted under the skin to promote the growth of melanocytes.
A drug that helps control melanocytes i.e.:
- Prostaglandin E2 is being tested as a way to restore skin color in people with localized vitiligo that isn’t spreading.
- Besides this, It’s applied to the skin as a gel.
drug that reverses loss of color i.e.:
- Tofacitinib, an oral drug typically used to treat rheumatoid arthritis, has shown some potential as a treatment for vitiligo. [2]
Prevention
Prevention :
Sun Protection:
- Diligent sun protection is paramount. Using broad-spectrum sunscreen with a high SPF, wearing protective clothing, and seeking shade during peak sun hours can significantly reduce the risk of new patches and protect existing pigment.
Stress Management:
- While the exact link between stress and vitiligo remains an area of research, stress management techniques such as meditation, yoga, and exercise can contribute to overall well-being and potentially reduce disease activity.
Skin Trauma Avoidance:
- Minimizing skin injuries, including cuts, burns, and friction, is crucial. These injuries can trigger the Koebner phenomenon, where new vitiligo patches develop at the site of trauma.
Dietary Considerations:
- While no specific diet has been proven to prevent vitiligo, a balanced diet rich in antioxidants and vitamins may support skin health. Avoiding potential triggers like certain foods or additives can be helpful for some individuals.
Early Intervention:
- If you notice any early signs of vitiligo, such as small white patches or loss of pigment, seeking prompt medical attention can allow for early intervention and potential management options.[9]
Homeopathic Treatment
Homeopathic treatment :
For Vitiligo is natural, safe and without any side-effects, and one can enjoy immense relief from these frustrating symptoms.
It is a patient-oriented science and medicines are prescribed on the characteristics of the individual rather than just the symptoms of the disease.
Arsenicum Sulphuratum Flavum:
- This is one of the specific remedies used for the treatment of vitiligo in homeopathy.
- It has discoloration of the skin in blotches that are pale or white in color.
- It is also a good remedy for eczematous lesions which are moist and have intense itching with corrosive discharge.
- Pyoderma and urticaria also find a solution to this drug.
- Its sphere of action also extends to catarrhal affections and asthmatic states.
- A deep acting drug which has been known to give good results in vitiligo.
Hydrocotyle Asiatica:
- This is a remedy that is prepared from the tincture of plant called Indian Pennywort.
- After undergoing the process of Potentization, the curative powers of this remedy are brought forth.
- This is one of the very good remedies for vitiligo.
- It is supposed to stimulate the process of pigmentation.
- It is also beneficial for other skin problems such as psoriasis, lupus, leprosy, acne and other disorders of the skin in which there is much exfoliation of the skin.
- This medicine is often prescribed in combination with a constitutional medicine or other deeper acting medicine to get the best effect. [6]
Calcarea Carbonica – For Milky White Spots on the Skin:
- Calcarea Carb is a top grade constitutional medicine specifically for Vitiligo.
- Moreover, It is prescribed to patients of Vitiligo with milky white spots on skin.
- These white spots can appear anywhere on the body.
- The first among these is tendency to free perspiration over the head, neck also chest.
- Besides this, Next is intolerance to cold weather.
- Certain peculiar cravings may be present are eggs, lime, pencils.
- Person needing calcarea carb may show tendency to catch cold easily.
- Weakness of bone & easily fatigued especially by exertion.
- The tendency to chronic constipation and obesity also guides the selection of calcarea carb in vitiligo.
- On the mental sphere, the person may show a number of fears.
- The prominent fears among them are fear of misfortune, of contagious disease, of losing reason and of insanity.
Arsenic Album – For Vitiligo in Anxious Personalities:
- Arsenic Album is yet another useful remedy for vitiligo in persons prone to dry, rough skin.
- The skin shows whitish spots and skin is dry, dirty and rough.
- And skin complaint alternating with respiratory complaints like asthma is a strong pointer for using arsenic.
- In general sphere warmth is a relieving factor for persons needing Arsenic album.
- Warm applications over skin and warm drinks are highly desirable.
- Burning sensations in varying body parts may also be noticed.
- Extreme exhaustion may also be present.
- The most prominent out of these are fears and anxieties.
- This remedy is often indicated in persons who have fears including that of death, disease, germs and of catching infection.
- Patients requiring arsenic are highly anxious personalities.
- They may show anxieties about health, trifles and anxiety about others.
- Marked restlessness is often seen on both mental and physical planes in persons needing Arsenic Album.
- Next distinctive feature for selecting arsenic album in vitiligo is fastidiousness.
- Person demanding extreme neatness and order in everything are yet another suitable subjects requiring Arsenic Album.
Sepia – For Vitiligo in People with Indifferent Attitude:
- Sepia is another important remedy in the list that is selected constitutionally in vitiligo treatment.
- If the constitutional picture of Sepia matches with that of a person suffering with vitiligo, it possess a great ability to completely eradicate the disease.
- Constitutional symptoms that indicate the use of sepia are; in detail having an indifferent approach towards life and family.
- They show aversion towards family members and friends who were once loved with great affection.
- They lack interest in doing any work.
- Tendency to avoid both physical or mental labor is present .
- They are constantly depressed with marked irritability, weeping tendency, desire to be alone also an aversion to consolation or sympathy.
- The use of sepia must also be thought in women with menstrual irregularities or those around menopausal age with tendency to hot flushes.
Silicea – Constitutional Medicine for Vitiligo:
- Silicea carries a good scope to treat vitiligo when selected as per the constitutional makeup of the person.
- The set of symptoms that indicate the use of Silicea are; pale and waxy skin; additionally tendency to excessive perspiration on hands and feet; tendency to eruptions with pus formation in various body parts, and to catch cold on frequent basis; lean, thin physical makeup.
- The main mind symptom are timidity also an under-confident nature.
- Besides this, Silicea may be thought of in people who seem under-confident, fear public speaking, are timid and bashful.
- Obstinate behavior and stubbornness may also indicate its use .
Sulphur – One of the best Medicines for Vitiligo:
- Although Sulphur mention quite low down in the list for treating vitiligo but its worth equivalent to above narrated medicines.
- Furthermore, Sulphur is a deep acting medicine used frequently in treatment of varying skin diseases including vitiligo.
- Additionally, It goes deep inside the basic root cause to annihilate the disease in its complete extent.
- Besides this, The persons requiring Sulphur usually show a philosophical mindset.
- They popularly refer as ‘ragged philosophers’.
- Their mind constantly occupy with various theories also plans.
- As a result they suffer from mental fatigue and absent mindedness.
- They take little or no care for their physical appearance and even show aversion to bathing.
- Persons who have suffered a lot from skin troubles, itchy skin with long term use of ointments are also likely to be benefited from use of Sulphur.
- Apart from all above said symptoms burning sensations in various body parts may present along with white spots on skin.
- An extraordinary craving for sweets may also show as a constitutional symptom. [5]
Diet & Regimen
Diet & Regimen:
Dietary Considerations
- Antioxidant-Rich Foods: Emphasize fruits, vegetables, and whole grains, which are rich in antioxidants. These compounds may help protect melanocytes from oxidative damage.
- Vitamin and Mineral Intake: Ensure adequate intake of vitamins and minerals, particularly vitamin D, vitamin B12, folic acid, and zinc. These nutrients play a role in melanin production and immune function.
- Probiotics: Consider incorporating probiotic-rich foods or supplements into your diet. Probiotics may help modulate the immune system and potentially benefit individuals with vitiligo.
- Avoid Potential Triggers: Some individuals with vitiligo report that certain foods or food additives may trigger or worsen their condition. If you suspect any food sensitivities, consider keeping a food diary and eliminating potential triggers.
Lifestyle Recommendations
- Sun Protection: Protect your skin from excessive sun exposure. Use sunscreen with a high SPF, wear protective clothing, and seek shade when necessary. Sun protection is crucial for preventing sunburn and further pigment loss.
- Stress Management: Practice stress reduction techniques such as meditation, yoga, or deep breathing exercises. Stress may contribute to vitiligo flares, so managing stress is important for overall well-being.
- Regular Exercise: Engage in regular physical activity. Exercise can improve blood circulation, reduce stress, and boost overall health, potentially benefiting individuals with vitiligo.
- Adequate Sleep: Prioritize getting enough quality sleep. Sleep is essential for immune function and overall health, which may indirectly impact vitiligo.[9]
Do’s and Don'ts
The Do’s & Don’ts
Do’s
- Protect your skin from the sun: The white patches are more susceptible to sunburn, so it’s crucial to use sunscreen with a high SPF (at least 30) and reapply it frequently. Wear protective clothing like hats and long sleeves when outdoors.
- Consult a dermatologist: They can diagnose the condition, rule out other possibilities, and suggest suitable treatment options based on the severity and extent of the patches.
- Consider treatment options: Several treatments can help improve the appearance of the patches, including topical medications, light therapy, and surgical procedures.
- Boost your self-confidence: Vitiligo can impact self-esteem, so it’s important to focus on self-acceptance and embrace your unique beauty. Connect with support groups or seek counseling if needed.
- Maintain a healthy lifestyle: Eating a balanced diet, exercising regularly, and managing stress can contribute to overall well-being and potentiallybenefit skin health.
Don’ts
- Not use harsh soaps or chemicals: These can irritate the skin and worsen the condition. Opt for mild, fragrance-free cleansers.
- Don’t scratch or pick at the patches: This can lead to further damage and increase the risk of infection.
- Never get tattoos or piercings on affected areas: These can trigger the development of new patches.
- Must Not compare yourself to others: Everyone’s vitiligo journey is unique. Focus on self-acceptance and celebrate your individuality.
- Don’t give up hope: While there’s no cure for vitiligo, many treatments can help improve the appearance of the patches and enhance quality of life.
Terminology
Terminology:
Vitiligo: A skin condition characterized by the loss of pigment, leading to white patches on the skin. It occurs due to the destruction or malfunction of melanocytes, the cells responsible for producing melanin, the pigment that gives skin its color.
Melanocytes: Specialized cells located in the epidermis (the outermost layer of skin) that produce melanin.
Melanin: The pigment that gives skin, hair, and eyes their color. It also helps protect the skin from the harmful effects of ultraviolet (UV) radiation from the sun.
Depigmentation: The loss of pigment or color from the skin, resulting in white patches.
Autoimmune: Relating to a condition where the body’s immune system mistakenly attacks its own healthy tissues. Vitiligo is often considered an autoimmune disorder.
Other Examples:
Genetic Predisposition: An increased likelihood of developing a condition due to inherited genes. People with a family history of vitiligo or other autoimmune diseases may have a higher risk.
Oxidative Stress: An imbalance between the production of free radicals (unstable molecules) and the body’s ability to neutralize them. This imbalance can damage cells, including melanocytes.
Trigger: An event or factor that initiates or exacerbates the development of vitiligo. Triggers can include stress, sunburn, injury, or exposure to certain chemicals.
Segmental Vitiligo: A type of vitiligo where the white patches are localized to one area of the body and often follow a nerve pathway.
Non-segmental Vitiligo: A more common type of vitiligo where the white patches are widespread and symmetrical, often affecting both sides of the body.
Phototherapy: A treatment using UV light to stimulate repigmentation of the skin.
Topical Corticosteroids: Creams or ointments containing corticosteroids that can help reduce inflammation and promote repigmentation in some cases.
Depigmentation Therapy: A treatment option for people with extensive vitiligo where the remaining pigmented skin is lightened to match the white patches.
- Camouflage: The use of makeup or self-tanners to cover the white patches and blend them with the surrounding skin.
Homoeopathic Terminology:
- Miasm: In homeopathy, a miasm is a theoretical underlying predisposition to chronic disease.
- Constitutional Remedy: A homeopathic remedy chosen based on the individual’s overall physical, mental, and emotional characteristics.
- Totality of Symptoms: The complete picture of a person’s symptoms, including physical, mental, and emotional, used in homeopathy to select the most appropriate remedy.
- Individualized Treatment: A homeopathic approach where treatment is tailored to the unique characteristics and symptoms of each person.
Other Examples:
- Potency: The strength or dilution of a homeopathic remedy.
- Repertory: A reference book used in homeopathy to identify remedies based on specific symptoms.
- Materia Medica: A reference book containing detailed descriptions of the properties and effects of homeopathic remedies.
- Aggravation: A temporary worsening of symptoms after taking a homeopathic remedy, often considered a positive sign of healing.
- Proving: A process in homeopathy where healthy volunteers take a remedy to observe its effects and create a symptom picture.
References
References:
- Davidson’s Principles and Practice of Medicine (22nd edition) Ch. 28
- https://www.mayoclinic.org/diseases-conditions/vitiligo/diagnosis-treatment/drc-20355916
- https://kidshealth.org/en/teens/vitiligo.html
- https://www.medicalnewstoday.com/articles/245081.php
- https://www.drhomeo.com/homeopathy-for-skin/vitiligo-its-homeopathic-treatment/
- https://www.askdrshah.com/app/vitiligo/vitiligo-medicines.aspx
- Clinical and sociodemographic study of vitiligo, 2009
- Epidemiological profile of vitiligo in Northern India – Journal of Applied Pharmaceutical Science
- Vitiligo: A Comprehensive Overview" (2nd Edition)
- Rook’s Textbook of Dermatology (10th Edition)
- Dermatology, 4th Edition. Bolognia, Jorizzo, Schaffer. 2018. Elsevier.
- A Monograph on the Basic and Clinical Science. 2nd Edition
- Fitzpatrick’s Dermatology in General Medicine, 9th Edition (2019)
Also Search As
Also Search As:
Online:
- Search engines: Use search terms like "homeopathy for vitiligo," "homeopathic treatment for white patches," or "best homeopathic doctor for vitiligo near me."
- Homeopathy websites: Reputable homeopathy organizations and clinics often have dedicated sections or articles on vitiligo treatment.
- Social media: Look for groups or pages related to homeopathy and vitiligo, or follow homeopathic practitioners who specialize in skin conditions.
- Video platforms: Search for videos on homeopathic vitiligo treatments, testimonials, and expert interviews.
Offline:
- Homeopathic practitioners: Consult a qualified homeopath directly for personalized advice and treatment plans.
- Homeopathy clinics: Visit specialized clinics that offer homeopathy for various skin conditions, including vitiligo.
- Word-of-mouth: Ask friends, family, or other people with vitiligo for recommendations based on their experiences.
- Local directories: Check local directories or listings for homeopathic practitioners in your area.
Additional tips for searching:
- Specify your location: Include your city or region in your search to find relevant local practitioners and clinics.
- Check credentials: Ensure the homeopath you consider is qualified and registered with a recognized homeopathic body.
- Read reviews and testimonials: Look for feedback from other patients about their experiences with specific practitioners or clinics.
- Ask questions: During consultations, ask about the practitioner’s experience with vitiligo, their treatment approach, and expected outcomes.
Online search engines:
- General search: Use broad keywords like "vitiligo", "white patches on skin", or "loss of skin pigment".
- Specific searches: Narrow down your search with terms like "vitiligo causes", "vitiligo treatment", "vitiligo support groups", or "vitiligo images".
Medical websites and databases:
- Reputable health organizations: Consult websites like Mayo Clinic, Cleveland Clinic, American Academy of Dermatology, or National Institutes of Health.
- Medical journals: Search databases like PubMed or Google Scholar for scientific research on vitiligo.
Social media and online communities:
Frequently Asked Questions (FAQ)
What is Vitiligo?
Definition:
Vitiligo is a loss of skin pigment (Melanocytes) that causes white spots or patches to appear on the skin.
Can vitiligo be cured?
Currently, there is no cure for vitiligo. However, several treatment options are available to help improve the appearance of the skin and slow down the progression of the condition. These include topical medications, light therapy, surgical treatments, and camouflage techniques.
Is vitiligo contagious?
No,
Vitiligo is not contagious. It cannot be spread from person to person through touch or any other means.
Can homeopathy cure Vitiligo?
While there’s no guarantee of a cure, homeopathy aims to stimulate the body’s self-healing mechanisms to potentially repigment the affected areas.
The effectiveness varies depending on individual cases, the extent of the condition, and other factors.
What is the main cause of Vitiligo?
Causes:
- Autoimmune disorder
- Genetic
- A stressful event
- critical sunburn or cut
- Exposure to some chemicals
- Heredity, as it may run in families
- Virus
What are the symptoms of Vitiligo?
Symptoms:
- Patchy loss of skin color
- Discoloration on sun-exposed areas
- Hair of the scalp, beard, eyebrows and lashes may also depigment
- Segmental vitiligo is restrict to one part
- Spotty perifollicular pigment
How long does homeopathic treatment for Vitiligo take?
- The duration of treatment can vary widely, from months to years.
- It depends on factors like the severity of the condition, the individual’s response to treatment, and overall health.

