Leucorrhoea
Definition
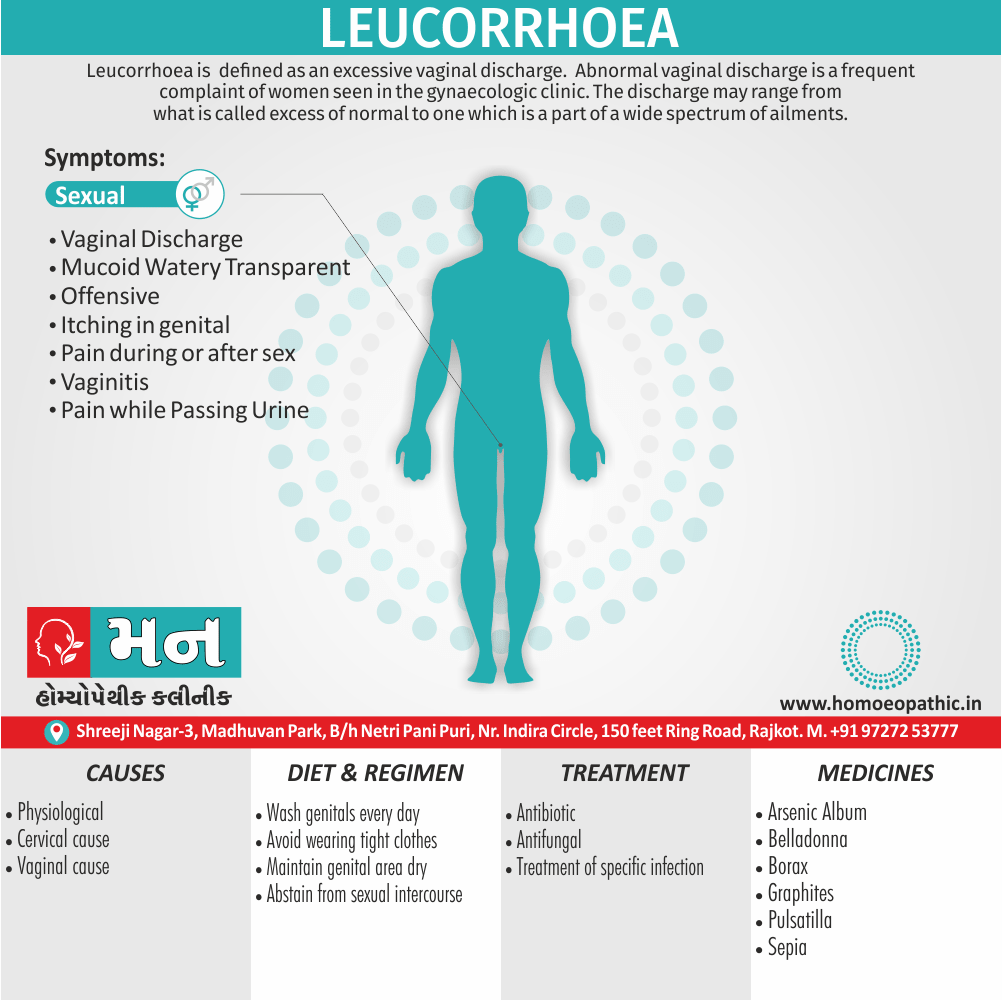
Leucorrhoea is strictly defined as an excessive vaginal discharge.[2]
Leucorrhoea is a medical term for a white or yellowish discharge of mucous material from the vagina. Here are some synonyms for leucorrhoea:
- Leukorrhea (American spelling)
- Fluor albus (Latin term)
- Whites (informal term)
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
Leucorrhoea/ Abnormal vaginal discharge is a frequent complaint of women seen in the gynaecologic clinic. The discharge may range from what is called excess of normal to one which is a part of wide spectrum of ailments. It may be blood-stained or contaminated with urine or stool, all of which are however excluded from the discussion made below.[2]
Epidemiology
Epidemiology:
Leucorrhea, or vaginal discharge, is a common gynecological complaint among Indian women. Several studies have explored its prevalence and associated factors in the Indian population.
A study of leucorrhoea in reproductive age group women of Nagpur City (2006):
- This study found leucorrhoea to be significantly more common in married women, pregnant women, and women of lower socioeconomic status. The study also found an association with high parity (number of pregnancies). [5]
Prevalence :
- This hospital-based study found a prevalence of 28.99% for vaginal discharge. It was found to be more common in younger women, illiterate women, women of lower socioeconomic status, and those married at a younger age. [6]
Socio demographic factors :
- This community-based study found a prevalence of 66.9% for leucorrhoea in an urban slum of Mumbai. The study found it to be more common in women aged 23-32 years, among the Muslim population, and those belonging to lower socioeconomic classes. [7]
These studies highlight the varying prevalence of leucorrhoea across different populations and the association with various sociodemographic factors such as marital status, age, socioeconomic status, and parity. However, it is important to note that these studies are based on specific populations and may not be generalizable to the entire Indian population. Further research is needed to understand the nationwide epidemiology of leucorrhoea in India.
Causes
Causes:
The excessive secretion is due to:
[a] Physiologic excess
[b] Cervical cause (cervical leucorrhoea)
[c] Vaginal cause (vaginal leucorrhoea)
[a] Physiologic excess:
The normal secretion is expected to increase in conditions when the oestrogen levels become high. Such conditions are:
- During pubertyIn general, Increased levels of endogenous oestrogen leads to marked overgrowth of the endocervical epithelium which may encroach onto the ectocervix producing congenital ectopy (in other words, erosion) →Increased secretion.
- During menstrual cycle
[1] Around ovulation—Peak rise of estrogen →
increase in secretory activity of the cervical glands.
[2]Premenstrual pelvic congestion also increased mucus secretion from the hypertrophied endometrial glands.
- Pregnancy—There is hyperestrinism with increased vascularity. This leads to increased vaginal transudate also cervical gland secretion.[2]
- During sexual excitement, when there is abundant secretion from the Bartholin’s glands.
[b]Cervical cause:
Non-infective cervical lesion may produce excessive secretion, which pours out at the vulva. Such lesions are—cervical ectopy, chronic cervicitis, mucous polyp also ectropion (cervical glands are exposed to the vagina).
[c] Vaginal cause:
Increased vaginal transudation occurs in conditions associated with increased pelvic congestion. Additionally, The conditions are uterine prolapse, acquired retroverted uterus, chronic pelvic inflammation, ‘pill’ use also vaginal adenosis. Ill health is one of the important causes of excessive discharge. It produces excess exfoliation of the superficial cells.[2]
Types
Types:
The Types of Leucorrhoea as per the book:
Physiological Leucorrhea:
- This is a normal vaginal discharge that varies in consistency and amount throughout the menstrual cycle. It is usually white or clear, odorless, and non-irritating.
Pathological Leucorrhea:
- This type of discharge is caused by an infection or inflammation of the reproductive tract. It may be yellow, green, or gray, have an unpleasant odor, and cause itching or burning.
Specific Types of Pathological Leucorrhoea:
- Trichomonal: Yellowish-green, frothy discharge with a foul odor.
- Candidal (Yeast Infection): Thick, white, curd-like discharge with itching.
- Bacterial Vaginosis: Thin, grayish-white discharge with a fishy odor.
Please note that this classification is based on the information provided in the referenced textbook. Other sources may offer different classifications or terminology. [8]
Risk Factors
Risk Factors
Poor Hygiene:
- Inadequate cleaning of the genital area can create a favorable environment for the growth of microorganisms, leading to infection and abnormal discharge.
Sexually Transmitted Infections (STIs):
- STIs like chlamydia, gonorrhea, and trichomoniasis are common causes of abnormal vaginal discharge.
Vaginal Douching:
- Douching disrupts the normal vaginal flora, increasing the risk of infection and abnormal discharge.
Use of Antibiotics:
- Antibiotics can disturb the balance of good and bad bacteria in the vagina, leading to yeast overgrowth and candidal vaginitis.
Contraceptive Use:
- Some contraceptives, such as intrauterine devices (IUDs), can increase the risk of infection and abnormal discharge.
Pregnancy:
- Hormonal changes during pregnancy can alter the vaginal environment, making it more susceptible to infection.
Diabetes:
- Uncontrolled diabetes can weaken the immune system, making it harder to fight off infections that can cause abnormal discharge.
Other Factors:
- Stress: Can suppress the immune system, increasing susceptibility to infections.
- Use of Irritants: Soaps, bubble baths, and scented products can irritate the vaginal lining, leading to inflammation and discharge. [9]
Please note that this list of risk factors is not exhaustive. Other factors, such as hormonal imbalances, foreign bodies in the vagina, and certain medical conditions, can also contribute to the development of leucorrhoea.
Pathogenesis
Pathogenesis
Leucorrhoea, or vaginal discharge, can be physiological (normal) or pathological (abnormal). The pathogenesis of leucorrhoea varies depending on the underlying cause.
Physiological Leucorrhoea:
Normal Vaginal Secretions: The vagina has a natural cleaning and lubricating system. This system involves the production of secretions from the cervix, vaginal walls, and Bartholin’s glands. These secretions typically contain:
- Cervical mucus
- Vaginal transudate
- Desquamated epithelial cells
- Normal vaginal flora (mainly Lactobacillus)
Hormonal Influences: The amount and consistency of these secretions vary throughout the menstrual cycle due to hormonal fluctuations. Estrogen, in particular, stimulates the production of cervical mucus.
Pathological Leucorrhoea:
Infectious Causes: The most common cause of pathological leucorrhoea is infection. The infection can be:
- Bacterial: Bacterial vaginosis (BV) is the most common cause of infectious vaginitis. It is characterized by an overgrowth of anaerobic bacteria and a decrease in Lactobacillus.
- Fungal: Candida albicans is the most common cause of fungal vaginitis (yeast infection). It is characterized by an overgrowth of Candida species.
- Protozoal: Trichomonas vaginalis is a protozoan parasite that causes trichomoniasis. It is a sexually transmitted infection (STI).
- Viral: Some viruses, such as herpes simplex virus (HSV) and human papillomavirus (HPV), can cause inflammation and abnormal discharge.
Inflammatory Causes: Non-infectious causes of pathological leucorrhoea can include:
- Chemical irritation: Soaps, douches, and spermicides can irritate the vaginal lining and cause inflammation.
- Foreign body: Retained tampons or other foreign objects can cause irritation and infection.
- Allergic reactions: Some women may be allergic to latex condoms or certain lubricants.
- Atrophic vaginitis: This occurs due to a decrease in estrogen levels after menopause, leading to thinning and inflammation of the vaginal walls.
Mechanisms of Leucorrhoea:
Changes in Vaginal pH: In normal conditions, the vagina has an acidic pH due to the presence of Lactobacillus. This acidic environment helps to prevent the overgrowth of harmful bacteria and yeast. Disruptions in the vaginal pH, such as those caused by douching or antibiotics, can increase the risk of infection.
Inflammation: Infection or irritation of the vaginal lining leads to inflammation, resulting in increased blood flow and the release of inflammatory mediators. This can cause the vaginal walls to become more permeable, leading to increased production of discharge.
Cellular Damage: In some cases, such as with trichomoniasis, the causative organism can directly damage the epithelial cells of the vaginal lining, leading to increased discharge. [10]
Understanding the pathogenesis of leucorrhoea is crucial for accurate diagnosis and appropriate treatment.
Pathophysiology
Pathophysiology of Leucorrhoea:
Normal Vaginal Secretion: The origin and nature of the normal vaginal secretion during the reproductive period.
The physiologic basis involved in normal vaginal secretion is dependent on the endogenous oestrogen level. In detail, With the rising oestrogen level, there is abundant secretory activity of the endocervical glands and the superficial vaginal epithelium becomes rich in glycogen.
The mucoid secretion from the cervical glands is normally small in amount. Besides this, The carbohydrate radicle of the glycoprotein mucin is split off and fermented into lactic acid. If, however, the mucus is secreted in excess, it pours out at the vulva.[2]
Clinical Features
Clinical Features
The clinical features of leucorrhoea can vary depending on the underlying cause. However, some common features include:
Change in Discharge:
- The most common symptom is an increase in the amount or a change in the consistency, color, or odor of the vaginal discharge.
- Physiological Leucorrhoea: Usually white or clear, odorless, and non-irritating. The amount may increase around ovulation or before menstruation.
- Pathological Leucorrhoea: Can be yellow, green, gray, or blood-tinged.
Associated Symptoms:
Depending on the cause, additional symptoms may be present:
- Itching: Common in candidal vaginitis and trichomoniasis.
- Burning: Can occur with infection or irritation.
- Pain: May be present with pelvic inflammatory disease (PID).
- Dyspareunia: Painful intercourse
- Dysuria: Painful urination
- Spotting or Bleeding: May occur with trichomoniasis or other infections.
Physical Examination Findings:
- Vaginal Erythema: Redness or inflammation of the vaginal walls.
- Discharge Characteristics: Examining the discharge for color, consistency, and odor.
- Vulvar Irritation: Excoriations or other signs of irritation.
- Cervical Friability: Bleeding or discharge from the cervix.
Laboratory Findings:
- Microscopic Examination: Wet mount or Gram stain of the discharge to identify causative organisms.
- Culture: To identify specific bacteria or fungi.
- pH Testing: To assess the acidity of the vaginal environment.
- Nucleic Acid Amplification Tests (NAATs): To detect STIs like chlamydia and gonorrhea. [11]
It’s important to note that not all women with leucorrhoea will experience all of these symptoms. The clinical presentation can vary depending on the underlying cause. A thorough history and physical examination, along with appropriate laboratory tests, are essential for accurate diagnosis and treatment.
Sign & Symptoms
Sign & Symptoms of Leucorrhoea:
- The leucorrhoea excess secretion is evident from persistent either vulval moistness or staining of the undergarments (brownish yellow on drying) or need to wear a vulval pad. [2]
- Intense itching of the vulva
- Vaginitis
- Pain while Passing Urine
- Pain during during or after sex
- Lower back pain[4]
Clinical Examination
Clinical Examination
The clinical examination of a patient with leucorrhoea involves a comprehensive assessment to determine the underlying cause of the abnormal discharge.
History Taking:
- Detailed history of the discharge:
- Duration of the discharge
- Changes in the amount, color, consistency, and odor
- Relation to the menstrual cycle
- Presence of associated symptoms (itching, burning, pain, etc.)
- Medical history:
- Previous episodes of vaginal infections
- History of sexually transmitted infections (STIs)
- Current medications (especially antibiotics or steroids)
- Presence of underlying medical conditions (diabetes, etc.)
- Sexual history:
- Number of sexual partners
- Use of barrier contraception
- History of STIs in partners
Physical Examination:
- General examination:
- Assess general health and well-being
- Look for signs of systemic illness
- Abdominal examination:
- Palpate for tenderness or masses in the lower abdomen
- Pelvic examination:
- Inspection:
- Examine the external genitalia for signs of inflammation, irritation, or discharge
- Note the color, consistency, and amount of discharge
- Speculum examination:
- Gently insert a speculum to visualize the vagina and cervix
- Observe the vaginal walls and cervix for any abnormalities
- Collect samples of the discharge for laboratory analysis
- Bimanual examination:
- Palpate the uterus and ovaries for tenderness, enlargement, or masses
- Inspection:
Laboratory Investigations:
- Microscopic examination of discharge:
- Wet mount: Examine the discharge for the presence of trichomonads, clue cells, or fungal hyphae
- Gram stain: Identify bacterial morphology and assess for inflammation
- Culture:
- Bacterial culture: Isolate and identify specific bacteria
- Fungal culture: Identify Candida species
- pH testing:
- Assess the vaginal pH (normal range is 3.8-4.5)
- Nucleic acid amplification tests (NAATs):
- Detect STIs like chlamydia and gonorrhea
Additional Investigations (if indicated):
- Colposcopy: Examine the cervix for abnormalities
- Biopsy: Obtain a tissue sample for further analysis
- Ultrasound: Assess the pelvic organs [12]
The clinical examination of leucorrhoea is essential for determining the underlying cause and guiding appropriate treatment. A thorough history and physical examination, along with relevant laboratory investigations, are key components of this evaluation.
Diagnosis
Diagnosis :
Evaluation of patient with vaginal discharge.
- History
- Physical examination
- Investigation
Pap smear
Urine for R/e, c/S
HIV serology
Blood tests when PID is suspected [2]
Differential Diagnosis
Differential Diagnosis
Leucorrhoea, or abnormal vaginal discharge, can be caused by a variety of conditions. The differential diagnosis includes:
Infectious Causes:
- Bacterial Vaginosis (BV): The most common cause of vaginal discharge in women of reproductive age. Characterized by a thin, gray-white discharge with a fishy odor.
- Vulvovaginal Candidiasis (VVC): Commonly known as a yeast infection. Characterized by a thick, white, curd-like discharge with itching and burning.
- Trichomoniasis: A sexually transmitted infection (STI) caused by a parasite. Characterized by a frothy, yellow-green discharge with a foul odor.
- Chlamydia and Gonorrhea: STIs that can cause cervicitis and abnormal discharge.
- Other Infections: Less common infections like herpes simplex virus (HSV), human papillomavirus (HPV), and group B streptococcus can also cause leucorrhoea.
Non-Infectious Causes:
- Atrophic Vaginitis: Occurs due to a decrease in estrogen levels after menopause. Characterized by a thin, watery discharge, vaginal dryness, and pain during intercourse.
- Irritant or Allergic Vaginitis: Caused by irritants like soaps, douches, or spermicides, or allergens like latex or lubricants. Characterized by inflammation and a watery discharge.
- Foreign Body: Retained tampons or other objects can cause irritation and a foul-smelling discharge.
- Cervical Polyps or Ectropion: These benign growths can cause increased mucus production and a clear or blood-tinged discharge.
- Vaginal or Cervical Cancer: Rare but serious causes of abnormal bleeding or discharge.
Other Causes:
- Physiologic Leucorrhoea: Normal vaginal discharge that varies in consistency and amount throughout the menstrual cycle. Usually clear or white and odorless.
- Pregnancy: Increased vaginal discharge is common during pregnancy due to hormonal changes. [13]
It’s important to consider all of these possibilities when evaluating a patient with leucorrhoea. A thorough history, physical examination, and appropriate laboratory tests are essential for accurate diagnosis and appropriate management.
Complications
Complications
While leucorrhoea itself is not a disease but a symptom of an underlying condition, it can lead to several complications if left untreated or if the underlying cause is not addressed. These complications can include:
Pelvic Inflammatory Disease (PID):
- Untreated sexually transmitted infections (STIs) like chlamydia or gonorrhea, which can cause leucorrhoea, can spread to the upper genital tract and cause PID. PID can lead to chronic pelvic pain, infertility, and ectopic pregnancy.
Infertility:
- Chronic inflammation of the reproductive organs due to untreated infections can damage the fallopian tubes, uterus, and ovaries, leading to difficulties in conception.
Pregnancy Complications:
- Some infections associated with leucorrhoea, such as bacterial vaginosis (BV) and trichomoniasis, have been linked to preterm birth, low birth weight, and other pregnancy complications.
Increased Risk of STIs:
- Disruptions in the normal vaginal flora, often seen with leucorrhoea, can increase susceptibility to other sexually transmitted infections.
Psychological Distress:
- Chronic or recurrent leucorrhoea can cause significant discomfort, embarrassment, and anxiety, leading to psychological distress.
Reduced Quality of Life:
- The physical discomfort and psychological impact of leucorrhoea can significantly affect a woman’s overall quality of life.
Complications Specific to the Underlying Cause:
- If leucorrhoea is caused by an underlying medical condition like diabetes or cervical cancer, the complications associated with those conditions may also arise. [14]
It is important to note that not everyone with leucorrhoea will experience these complications. However, prompt diagnosis and appropriate treatment of the underlying cause are essential to prevent these potential complications. Regular gynecological check-ups and safe sexual practices can also help reduce the risk of complications associated with leucorrhoea.
Investigations
Investigations:
The investigations for leucorrhoea aim to identify the underlying cause of the abnormal vaginal discharge. The following tests are commonly used:
Microscopic Examination of Vaginal Discharge:
- Wet Mount Preparation: A sample of the discharge is mixed with saline and examined under a microscope for the presence of trichomonads, clue cells (indicative of bacterial vaginosis), or fungal hyphae (indicative of candidiasis).
- Gram Stain: This staining technique helps identify the types of bacteria present in the discharge and can aid in the diagnosis of bacterial vaginosis.
Culture:
- Bacterial Culture: A sample of the discharge is cultured to isolate and identify specific bacteria, such as those causing gonorrhea or chlamydia.
- Fungal Culture: If a fungal infection is suspected, a sample of the discharge is cultured to identify the specific type of fungus, usually Candida species.
pH Testing:
- Vaginal pH: The acidity of the vaginal environment is measured. A pH above 4.5 may suggest bacterial vaginosis or trichomoniasis.
Nucleic Acid Amplification Tests (NAATs):
- Chlamydia and Gonorrhea Tests: These highly sensitive and specific tests are used to detect the genetic material of chlamydia and gonorrhea bacteria.
Other Tests (if indicated):
- Pap Smear: To screen for cervical cancer or precancerous changes.
- Colposcopy: If the Pap smear is abnormal, a colposcopy may be done to examine the cervix more closely.
- Biopsy: A tissue sample may be taken from the cervix or vagina for further analysis.
- Blood Tests: These may be done to rule out other conditions like diabetes or thyroid problems that can affect vaginal health. [15]
The specific investigations needed will depend on the patient’s clinical presentation and the suspected underlying cause of the leucorrhoea. A healthcare provider will select the appropriate tests to arrive at an accurate diagnosis and guide treatment decisions.
Treatment
Treatment:
- For Leucorrhoea, treatment may include antibiotics, such as metronidazole. Other antibiotics common for the treatment of STIs include clindamycin or tinidazole.[1]
- Improvement of general health.
- Cervical factors require surgical treatment for example, electrocautery, cryosurgery or trachelorrhaphy
- Pelvic lesions producing vaginal leucorrhoea require appropriate therapy for the pathology.
- Pill users may have to stop ‘pill’ temporarily, if the symptom is very much annoying.
- Above all, local hygiene has to be maintained meticulously.
- Treatment for specific infection.[2]
Prevention
Prevention:
Leucorrhea, a common vaginal discharge, is often a symptom of an underlying condition rather than a disease itself. Prevention focuses on addressing these potential causes and maintaining vaginal health:
Prevention Strategies:
Hygiene:
- Practice good genital hygiene by washing the external area with mild, unscented soap and water daily.
- Avoid douching, as it can disrupt the natural balance of vaginal flora.
- Wear breathable cotton underwear and change them regularly.
Diet:
- A balanced diet rich in fruits, vegetables, and whole grains can boost overall health and immunity.
- Include yogurt or probiotics in your diet to support a healthy vaginal microbiome.
Safe Sex:
- Practice safe sex by using condoms to prevent sexually transmitted infections (STIs), a potential cause of leucorrhea.
Regular Checkups:
- Schedule regular gynecological checkups for early detection and treatment of any underlying conditions. [16]
Homeopathic Treatment
Homeopathic Treatment
Homeopathy being an individualistic science tries to find an individual remedy for each case. Different females suffering from Leucorrhea (in other words, White Discharge) present with different symptoms regarding the character, localization, extension also severity. Also varying are the accompanying symptoms like backache, itching & burning in genital region etc.
Individualization
Some females will have complaints much before menses while others are worse only during it. The character of leucorrhea, its color, presence of blood, the underlying cause such as fibroids, cysts, endometriosis etc. differentiate one case from another.
From the treatment’s point of view, it is better to make it normal than to stop it because physiologically it is important. If it is stopped completely, vaginal dryness may result which may cause pain & distress during sexual activity.
Duration of treatment
Also, if it is not treated properly, it may often recur and sometimes it can be infected and become persistent. Always take treatment for 2-3 cycles of periods to analyze it.
In Homeopathy, we boost the immune system which plays a very important role in natural elimination of disease organism or the disease itself and also in prevention. Homeopathic prescriptions are based on the nature and time of the discharge and also depend upon the patient’s constitution.
The treatment can give permanent relief to recurrent leucorrhea.
Homeopathic Medicines for Leucorrhoea
Alumina. [Alum]
Leucorrhea in chlorotic girls which is transparent or of yellow mucus, which is very profuse and ropy, and greatly exhausting, as it is very rich in albumen. It occurs chiefly in the daytime; the great profuseness is its characteristic. It is apt to be acrid. Causticum. Leucorrhea occurring chiefly at night.
Arsenicum. [Ars]
Leucorrhea from exhausting diseases; cancer, etc. It best suit to weak persons, old women, especially the chronic form with much weakness; the discharge is acrid, corrosive and yellow. Dictamnus was one of Hahnemann’s remedies for leucorrhea. Secale. Brownish and offensive leucorrhea, with metrorrhagia, especially in thin scrawny women who suffer from excessive menstruation and prolapsus.[3]
Belladonna
corresponds to recent or acute attacks of leucorrhea dependent upon pelvic inflammation also congestion; oftentimes bearing down in pelvis. Thin, odorless, bland leucorrhea. Additionally, Sensitive cervix and bearing down pains. Stannum. Profuse bland leucorrhea, yellowish, with great debility, backache; patients weaken also sallow.
Borax [Bor]
suits a clear, copious and albuminous leucorrhea having an unnatural heat to it. Leucorrhea midway between menses with great nervousness, white as starch, perfectly bland without pain. Dr. Hughes recommends this remedy in the 2X trituration for a chronic vaginal catarrh, which sometimes mistaken for uterine leucorrhea. In detail, Graphites cures a leucorrhea associated with pains in the lower abdomen and weakness of back in pale young girls. Leucorrhea more profuse in morning when rising, especially indicates Graphites.[3]
Calcarea Carb
Indicated by its general symptoms, and these are always the more important in this affection. More prominent of these are morning hunger, acidity of the stomach, cold and damp feet. It corresponds especially to scrofulous persons with enlarged cervical glands. Sulphur is another remedy suitable to scrofulous subjects; it has a leucorrhea which makes the parts sore. It is rather indicated by the general than the local symptoms. Dr. Dyce Brown praises this remedy in leucorrhea, especially in nervous, neuralgic and hyper aesthetic patients.[3]
Kreasote. [Kreos]
Few medicines have the same power in leucorrhea as Kreasote. It cures a profuse watery, sometimes a yellowish leucorrhea. The acridity is marked; it causes excoriating of the parts which come in contact with it, causes soreness and smarting and red spots and itching on the vulva, always with great debility; leucorrhea preceding menses. It is so acrid that it causes the pudenda and thighs to swell and itch. Nitric acid.
Highly recommended by Jahr in a corrosive leucorrhea; it being one of our best remedies, and one too often neglected. Platinum.
Mercurius. [Merc]
Acrid excoriating leucorrhea smarting and burning, swelling of external genital organs. Purulent greenish yellow leucorrhea worse at night; heat, tenderness and pain involving Nabothian glands, form good indication for Mercurius. Scrofulous and syphilitic subjects with yellow and thick leucorrhea also indicate the remedy.[3]
Pulsatilla [Puls]
Basically, it produces a cures a milky leucorrhea which becomes watery, acrid also burning from being retained in the vagina. Additionally, It corresponds to a disposition to leucorrhea and suits leucorrhea in chlorotic subjects. Helonin. All in all, In anemic sallow patient with much prostration and general debility, worse from slight colds and exertion, it is a most useful remedy.[3]
Sepia
Cures a leucorrhea which is yellowish green color, somewhat offensive and often excoriating, due to pelvic congestion of a passive type. It is milky, worse before menses with bearing down; there are pains in the abdomen and pruritus. [3]
Diet & Regimen
Diet & Regimen
Diet:
- Gut health: Include probiotic-rich foods (yogurt, kefir) and prebiotic-rich foods (fruits, vegetables, whole grains) for a balanced gut microbiome.
- Immunity: Boost your immune system with vitamin C (citrus fruits, berries) and zinc (beans, nuts, seeds).
- Hydration: Drink plenty of water.
- Limit: Sugar and processed foods.
Regimen:
- Hygiene: Wash the genital area daily with mild soap, wipe front to back, wear breathable underwear, and change pads frequently.
- Safe sex: Use condoms to prevent STIs.
- Manage stress: Practice relaxation techniques.
- Avoid douching: It disrupts natural vaginal flora.
- Consider: Herbal remedies like neem, turmeric, and aloe vera (consult a healthcare professional first).
Do’s and Don'ts
Do’s & Don’ts
Leucorrhoea Do’s & Don’ts
Do’s:
- Maintain Good Hygiene: Wash the external genital area with mild, unscented soap and water daily. Pat dry thoroughly to avoid moisture buildup.
- Wear Breathable Underwear: Opt for cotton underwear and avoid tight-fitting clothes to allow for air circulation and prevent excessive sweating.
- Practice Safe Sex: Always use condoms to reduce the risk of sexually transmitted infections (STIs), a potential cause of leucorrhea.
- Eat a Balanced Diet: Consume a diet rich in fruits, vegetables, and whole grains to support overall health and vaginal health.
- Consider Probiotics: Include yogurt or probiotic supplements in your diet to maintain a healthy balance of vaginal bacteria.
- Consult a Doctor: Seek medical advice if you experience abnormal discharge, itching, burning, or foul odor.
Don’ts:
- Avoid Douching: Douching disrupts the natural balance of vaginal flora, increasing the risk of infections and worsening leucorrhea.
- Don’t Use Harsh Soaps or Perfumed Products: Avoid using harsh soaps, feminine hygiene sprays, or scented products in the genital area, as they can irritate the delicate skin and worsen symptoms.
- Don’t Ignore Symptoms: If you experience persistent or worsening symptoms, consult a doctor for diagnosis and appropriate treatment.
- Don’t Self-Medicate: Avoid using over-the-counter medications or home remedies without consulting a doctor, as they might not address the underlying cause.
- Don’t Wear Tight Clothing: Avoid tight pants, synthetic fabrics, and pantyhose, as they can trap moisture and create a breeding ground for bacteria.
Terminology
Terminology
Leucorrhea (or Leukorrhea):
- A whitish or yellowish vaginal discharge. It’s a common occurrence in women of all ages, but changes in its consistency, color, or odor can indicate underlying conditions.
Physiological Leucorrhea:
- Normal vaginal discharge that varies throughout the menstrual cycle. It’s usually clear, white, or slightly yellowish and odorless.
Pathological Leucorrhea:
- Abnormal vaginal discharge that can be caused by infections, hormonal imbalances, or other medical conditions. It may have an unusual color, odor, or consistency.
Vaginal Flora:
- The community of microorganisms (bacteria, fungi) that live in the vagina and help maintain its health.
pH Balance:
- The acidity or alkalinity of the vaginal environment, which plays a crucial role in maintaining a healthy vaginal flora.
Vulvovaginitis:
- Inflammation of the vulva and vagina, often accompanied by itching, burning, and abnormal discharge.
Candidiasis (Yeast Infection):
- A common fungal infection causing thick, white, curd-like discharge and itching.
Bacterial Vaginosis (BV):
- An imbalance of vaginal bacteria, causing a thin, grayish-white discharge with a fishy odor.
Trichomoniasis:
- A sexually transmitted infection caused by a parasite, leading to a frothy, yellow-green discharge with a foul odor.
Cervicitis:
- Inflammation of the cervix, often caused by infections, leading to an increase in vaginal discharge.
Pelvic Inflammatory Disease (PID):
- An infection of the female reproductive organs, often caused by untreated STIs, which can lead to abnormal discharge.
Hormonal Imbalance:
An imbalance in estrogen or progesterone levels, which can affect the amount and consistency of vaginal discharge.
These are just a few of the common terminologies used in articles about leucorrhea. Understanding these terms can help you better comprehend the information presented and make informed decisions about your health.
In homeopathic articles about leucorrhea, you’ll likely encounter these common terminologies:
Leucorrhoea:
- The central term, referring to a whitish or yellowish vaginal discharge. Homeopaths differentiate between physiological (normal) and pathological (abnormal) leucorrhoea.
Constitution:
- A person’s overall physical and mental makeup, including their tendencies towards certain ailments. Homeopathic treatment is often individualized based on the patient’s constitution.
Miasm:
- A predisposition to certain chronic diseases, believed to be inherited or acquired. Homeopaths may consider the miasm when selecting remedies for leucorrhoea.
Remedy:
- A homeopathic medicine, typically derived from natural substances, used to stimulate the body’s healing response.
Repertorization:
- The process of matching a patient’s symptoms to a list of remedies and their associated symptoms. This helps homeopaths choose the most appropriate remedy.
Materia Medica:
- A comprehensive reference book describing the properties and symptoms of homeopathic remedies.
Potency:
- The strength or dilution of a homeopathic remedy. Higher potencies are considered more dilute and are believed to act on a deeper level.
Aggravation:
- A temporary worsening of symptoms after taking a remedy, often seen as a positive sign that the body is responding to the treatment.
Modalities:
- Factors that make symptoms better or worse, such as time of day, temperature, or movement. These are important considerations in homeopathic case-taking.
Concomitant Symptoms:
- Additional symptoms experienced alongside leucorrhoea. These are crucial for differentiating between remedies.
Constitutional Remedy:
- A remedy that matches the patient’s overall constitution and is often used to treat chronic conditions.
Acute Remedy:
A remedy used to address specific, temporary symptoms, such as an acute flare-up of leucorrhoea.
Understanding these terms can help you navigate homeopathic articles and discussions about leucorrhoea. However, always consult with a qualified homeopathic practitioner for diagnosis and treatment, as they can guide you through the intricacies of homeopathic practice.
References
Reference
- https://en.wikipedia.org/wiki/Leukorrhea#:~:text=or%20yellow%20mucous.,Treatment,STIs%20include%20clindamycin%20or%20tinidazole.
- DC Dutta’s Gynaecology
- Therapeutics from zomeo ultimate LAN
- https://www.drbatras.com/all-about-leucorrhoea-and-homoeopathic-management#:~:text=Always%20wear%20cotton%20underwear%20to,cause%20dampness%20of%20genital%20organs.&text=Don’t%20Share%20towels%20and,zinc%2C%20to%20improve%20general%20health.
- A study of leucorrhoea in reproductive age group women of Nagpur City (2006)
- Prevalence and sociodemographic correlates of vaginal discharge among married women of reproductive age group at a teaching hospital (Date not specified)
- Socio demographic factors to assess leucorrhoea in married women of reproductive age group in an urban slum community (Date not specified)
- Book Title: Shaw’s Textbook of Gynaecology Edition: 16th Edition
Authors: Sheila Balakrishnan, Nikita Desai, Astha Gupta, Falguni Shah
Year of Publication: 2019, Publisher: Elsevier India - Book Title: Clinical Methods in Obstetrics and Gynaecology
Edition: 3rd Edition, Authors: Sarabatnam Arulkumaran, Sabaratnam Arulkumaran
Year of Publication: 2014
Publisher: JP Medical Ltd. - Book Title: Novak’s Gynecology
Edition: 16th Edition, Editors: Jonathan S. Berek, Evelyn Nicole
Year of Publication: 2020, Publisher: Wolters Kluwer - Book Title: Jeffcoate’s Principles of Gynaecology, Edition: 8th Edition
Authors: Sabaratnam Arulkumaran, Khalid S. Khan, Year of Publication: 2018, Publisher: JP Medical Ltd. - Book Title: Clinical Examination in Obstetrics and Gynaecology
Edition: 1st EditionAuthors: David M. Luesley, Philip Owen, Year of Publication: 2011, Publisher: JP Medical Ltd. - Book Title: Comprehensive Gynecology Edition: 7th Edition
Authors: William’s Gynecology
Year of Publication: 2017, Publisher: McGraw Hill Professional - Book Title: Te Linde’s Operative Gynecology, Edition: 12th Edition
Authors: John O. Schorge, Joseph I. Schaffer, Karen D. Bradshaw, Lisa M. Halvorson, Year of Publication: 2017, Publisher: Wolters Kluwer - Book Title: Practical Manual of Obstetrics & Gynecology
Edition: 1st Edition, Authors: Rekha Sachan, Shalini Rajaram, Neelima Singh, Savita Rani Singhal, Year of Publication: 2018, Publisher: JP Medical Ltd. - Title: Our Bodies, Ourselves
Edition: 40th Anniversary Edition
Authors: The Boston Women’s Health Book Collective
Year of Publication: 2011
Publisher: Touchstone
Also Search As
Also Search As
People can search for homeopathic articles on leucorrhoea using various online and offline resources:
Online Resources:
- Homeopathic Journals and Websites: Reputable homeopathic journals like the International Journal of Homeopathic Sciences or websites of homeopathic organizations often publish research articles and case studies on leucorrhoea.
- Search Engines: Use search engines like Google Scholar or PubMed with keywords like "homeopathy leucorrhoea" or "homeopathic treatment leucorrhoea" to find relevant articles.
- Homeopathic Databases: Online databases like Hompath or Complete Dynamics offer repertorization tools and materia medica references that can help identify homeopathic remedies for leucorrhoea.
- Homeopathic Forums and Communities: Online forums and communities dedicated to homeopathy can be a good source of discussions and shared experiences related to leucorrhoea treatment.
Offline Resources:
- Homeopathic Libraries: Visit libraries with homeopathic collections to access books, journals, and other publications on leucorrhoea.
- Homeopathic Clinics and Practitioners: Consult with experienced homeopathic practitioners who can provide insights and recommendations based on their clinical experience.
- Homeopathic Bookstores: Browse through homeopathic bookstores for books and publications on women’s health and specific conditions like leucorrhoea.
Tips for Effective Searching:
- Use specific keywords and search terms: Include relevant terms like "homeopathy," "leucorrhoea," "treatment," "remedies," and "case studies" to refine your search.
- Check the credibility of sources: Ensure that the articles or information you find come from reputable homeopathic journals, websites, or practitioners.
- Consider consulting a homeopath: If you have specific questions or concerns, consult with a qualified homeopathic practitioner for personalized advice and treatment.
By utilizing these resources and tips, individuals can effectively search for homeopathic articles on leucorrhoea and gain valuable insights into its treatment and management.
There are several ways to search for information about leucorrhoea, each offering different types of results:
Medical Websites and Databases:
- Reputable medical websites like Mayo Clinic, WebMD, or the National Institutes of Health (NIH) provide reliable information on leucorrhoea, its causes, symptoms, and treatment options. You can also search medical databases like PubMed for scientific articles and research studies on the topic.
Health Forums and Communities:
- Online forums and communities dedicated to women’s health can be a valuable resource for sharing experiences, asking questions, and learning from others who have dealt with leucorrhoea. However, always be cautious and verify any information you find on forums with reliable sources.
Books and Publications:
- Medical textbooks, encyclopedias, and books on women’s health often have sections dedicated to vaginal health and conditions like leucorrhoea. You can find these resources in libraries or bookstores.
Search Engines:
- General search engines like Google or Bing can be a starting point for your research. Use specific keywords like "leucorrhoea," "vaginal discharge," "causes of leucorrhoea," or "treatment for leucorrhoea" to refine your search.
Social Media:
- Some social media platforms have groups or communities focused on women’s health where you can find discussions and information about leucorrhoea. However, be critical of the information you find on social media and verify it with reliable sources.
Healthcare Professionals:
- If you have concerns about leucorrhoea, the best way to get accurate and personalized information is to consult a healthcare professional like a gynecologist or primary care physician. They can diagnose the cause of your leucorrhoea and recommend appropriate treatment options.
Remember to always evaluate the credibility of the sources you use and consult a healthcare professional for any medical concerns.
Frequently Asked Questions (FAQ)
What is leucorrhoea?
Definition:
Leucorrhoea refers to a whitish or yellowish vaginal discharge. It’s a common and often normal occurrence in women, but changes in color, odor, or consistency can sometimes indicate an underlying issue.
Is leucorrhoea always a cause for concern?
No, not always. Normal (physiological) leucorrhoea varies throughout your menstrual cycle and is generally clear, white, or slightly yellow. However, if you notice any unusual changes, it’s wise to consult a doctor.
What causes abnormal leucorrhoea?
Abnormal leucorrhoea can be caused by various factors, including:
- Infections (bacterial vaginosis, yeast infections, STIs)
- Hormonal imbalances
- Irritants (soaps, douches, fabrics)
- Certain medications
What are the symptoms of abnormal leucorrhoea?
Symptoms of abnormal leucorrhoea may include:
- Changes in color (greenish, grayish, brownish)
- Strong or foul odor
- Increased volume of discharge
- Itching, burning, or irritation
- Pain during intercourse or urination
How is leucorrhoea diagnosed?
A doctor will typically take a medical history, perform a pelvic exam, and may collect a sample of the discharge for testing to identify the underlying cause.
Can homeopathy help with leucorrhoea?
Yes,
homeopathy offers a holistic approach to managing leucorrhoea by addressing the root cause rather than just suppressing the symptoms. Homeopathic remedies are selected based on individual symptoms and constitutional factors.
How does a homeopath choose the right remedy for leucorrhoea?
Homeopaths conduct a detailed case-taking, considering the characteristics of the discharge (color, odor, consistency), accompanying symptoms, menstrual history, overall health, and emotional state to find the most suitable remedy.
How long does it take to see results with homeopathic treatment?
The response time varies depending on the individual, the cause of leucorrhoea, and the chosen remedy. Some may experience improvement within days or weeks, while others may require a longer course of treatment.
Where can I find a qualified homeopath for leucorrhoea?
You can search for qualified homeopathic practitioners through professional organizations like the Council for Homeopathic Certification (CHC) or the North American Society of Homeopaths (NASH).
Which homeopathic remedies are commonly used for leucorrhoea?
Homeopathic medicines for Leucorrhoea:
Several remedies are commonly used, including:
- Pulsatilla: For creamy, yellowish discharge, worse during ovulation.
- Sepia: For offensive, milky discharge with a bearing-down sensation.
- Kreosotum: For acrid, yellow-green discharge, worse before and after periods.
- Calcarea Carbonica: For thick, milky discharge, worse with exertion.
