Endometriosis
Definition
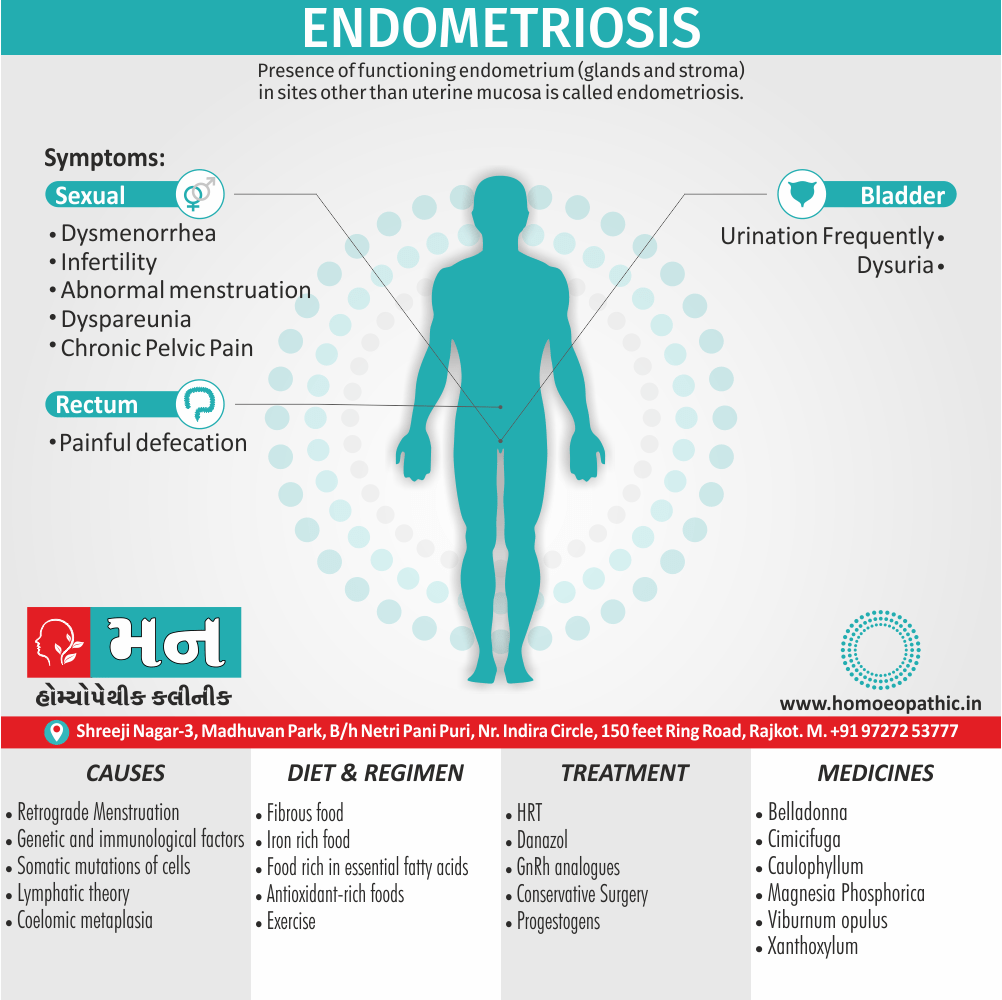
Presence of functioning endometrium (glands and stroma) in sites other than uterine mucosa is called endometriosis.[1]
There aren’t any true synonyms for endometriosis because it’s a specific medical condition. However, there are some related terms that you might encounter, such as:
- Endometriotic implants – These are the patches of endometrial tissue that grow outside of the uterus.
- Endometriomas – These are cysts that form in the ovaries and are filled with old blood and endometrial tissue. They are sometimes called "chocolate cysts" because of the brown, tar-like appearance of the fluid inside them.
- Pelvic endometriosis – This is the most common type of endometriosis, where the endometrial tissue grows on the organs in the pelvis, such as the ovaries, fallopian tubes, and the lining of the pelvis.
- Extra-pelvic endometriosis – This is a less common type of endometriosis, where the endometrial tissue grows outside of the pelvis, such as on the intestines, bladder, or diaphragm.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview Of Endometriosis
These ectopic endometrial tissues may be found in the myometrium when it is called endometriosis internal or adenomyosis. More commonly, however, these tissues are found at sites other than uterus and are called endometriosis externa or generally referred to as endometriosis. Endometriosis is a disease of contrast. It is a benign but it is locally invasive, disseminates widely. Cyclic hormones stimulate growth but continuous hormones suppress it.[1]
During the last couple of decades, the prevalence of endometriosis has been increasing both in terms of real and apparent. The real one is due to delayed marriage, postponement of first conception and adoption of small family norm. The apparent one is due to increased use of diagnostic laparoscopy as well as heightened awareness of this disease complex amongst the gynaecologists. The prevalence is about 10 percent. However, prevalence is high amongst the infertile women (30–40%) as based on diagnostic laparoscopy and laparotomy.[1]
Sites:
- Abdominal
- Extra-abdominal
- Remote
Abdominal:
It can occur at any site but is usually confined to the abdominal structures below the level of umbilicus.
Extra-abdominal:
The common sites are abdominal scar of hysterotomy, caesarean section, tubectomy and myomectomy, umbilicus, episiotomy scar, vagina and cervix.[1]
Epidemiology
Epidemiology of Endometriosis
The epidemiology of endometriosis in India demonstrates a significant prevalence, impacting a substantial number of women within the country.
A study published in 2023 in the PubMed journal, titled "Endometriosis and inflammatory immune responses: Indian experience," estimates that endometriosis affects approximately 42 million women in India. This figure represents a considerable portion of the global estimate of 247 million affected women. [9]
Another study published in the European Journal of Molecular & Clinical Medicine in 2019, titled "Prevalence, Surgical, and Medical Management of Patients with Endometriosis amongst Indian Women," found the prevalence of endometriosis to be 2.5% among 2400 Indian women who participated in the study. [10]
These figures highlight the widespread nature of endometriosis in India and underscore the need for increased awareness, early diagnosis, and effective management strategies to address this significant public health concern.
It is important to note that these are just two examples of studies on endometriosis in India. The prevalence of the condition may vary depending on the study population and methodology used. However, all studies point to the fact that endometriosis is a common and serious problem in India.
Causes
Causes of Endometriosis
- Retrograde menstruation: In retrograde menstruation, menstrual blood containing endometrial cells flows back through the fallopian tubes and into the pelvic cavity instead of out of the body. These endometrial cells stick to the pelvic walls and surfaces of pelvic organs, where they grow and continue to thicken and bleed over the course of each menstrual cycle.
- Transformation of peritoneal cells: In what’s known as the "induction theory," experts propose that hormones or immune factors promote transformation of peritoneal cells — cells that line the inner side of your abdomen — into endometrial-like cells.
- Embryonic cell transformation: Hormones such as estrogen may transform embryonic cells — cells in the earliest stages of development — into endometrial-like cell implants during puberty.
- Surgical scar implantation: After a surgery, such as a hysterectomy or C-section, endometrial cells may attach to a surgical incision.
- Endometrial cell transport: The blood vessels or tissue fluid (lymphatic) system may transport endometrial cells to other parts of the body.
- Immune system disorder.: A problem with the immune system may make the body unable to recognize and destroy endometrial-like tissue that’s growing outside the uterus.(4)
Types
Types of Endometriosis
Endometriosis is also grouped by what area of the pelvis or abdomen it affects. There are four main types:
- Superficial peritoneal endometriosis: The peritoneum is a thin membrane that lines your abdomen and pelvis. It also covers most of the organs in these cavities. In this type, the endometrial tissue attaches to the peritoneum. This is the least severe form.
- Endometriomas: These are dark, fluid-filled cysts. They’re also called chocolate cysts. They vary in size and can appear in different parts of your pelvis or abdomen, but they’re most common in the ovaries.
- Deeply infiltrating endometriosis (DIE): In this type, the endometrial tissue has invaded the organs either within or outside your pelvic cavity. This can include your ovaries, rectum, bladder, and bowels. It’s rare, but sometimes a lot of scar tissue can bond organs, so they become stuck in place. This condition is called frozen pelvis. But this only happens to 1%-5% of people with endometriosis.
- Abdominal wall endometriosis: In some cases, endometrial tissue can grow on the abdominal wall. The cells may attach to a surgical incision, like one from a C-section.(5)
Risk Factors
Risk factors of Endometriosis
Several factors place you at greater risk of developing endometriosis, such as:
- Never giving birth
- Starting your period at an early age
- Going through menopause at an older age
- Short menstrual cycles — for instance, less than 27 days
- Heavy menstrual periods that last longer than seven days
- Having higher levels of estrogen in your body or a greater lifetime exposure to estrogen your body produces
- Low body mass index
- One or more relatives (mother, aunt or sister) with endometriosis
- Any medical condition that prevents the passage of blood from the body during menstrual periods
- Disorders of the reproductive tract. (4)
Pathogenesis
Pathogenesis Of Eczema
The pathogenesis of endometriosis is complex and multifactorial, with several theories proposed to explain the development and progression of this condition.
Sampson’s Theory of Retrograde Menstruation
The most widely accepted theory is Sampson’s theory of retrograde menstruation, which suggests that endometrial tissue flows backward through the fallopian tubes during menstruation and implants on the pelvic organs and peritoneum. These implants then grow and respond to hormonal stimulation, causing pain, inflammation, and scarring.
Other Theories
- Coelomic Metaplasia: This theory proposes that cells lining the pelvic cavity can transform into endometrial-like tissue under the influence of certain factors.
- Vascular and Lymphatic Dissemination: Endometrial cells may spread through blood vessels or lymphatic channels to distant sites, leading to endometriosis in unusual locations.
- Genetic and Immunological Factors: Genetic predisposition and altered immune responses may contribute to the development and progression of endometriosis. [11]
Pathophysiology
Pathophysiology Of Eczema
still remains unclear and is full of theories. The principal ones are:
Retrograde Menstruation (Sampson’s theory)
There is retrograde flow of menstrual blood through the uterine tubes during menstruation. The endometrial fragments get implanted in the peritoneal surface of the pelvic organs (dependent sites, e.g., ovaries, uterosacral ligaments). Subsequently, cyclic growth and shedding of the endometrium at the ectopic sites occur under the influence of the endogenous ovarian hormones. Retrograde menstruation per se is unlikely to produce endometriosis. Probably, a genetic factor or favourable hormonal milieu is necessary for successful implantation and growth of the fragments of endometrium. While this theory can explain pelvic endometriosis, it fails to explain the endometriosis at distant sites.
Coelomic metaplasia (Meyer and ivanoff)
Chronic irritation of the pelvic peritoneum by the
menstrual blood may cause coelomic metaplasia which results in endometriosis. Alternatively, the Mullerian tissue remnants may be trapped within the peritoneum. They could undergo metaplasia and be transformed into endometrium. This theory can explain endometriosis of the abdominal viscera, the rectovaginal septum and the umbilicus.[1]
Direct implantation
According to the theory, the endometrial or decidual tissues start to grow in susceptible individual when implanted in the new sites. Such sites are abdominal scar following hysterotomy, caesarean section, tubectomy and myomectomy. Endometriosis at the episiotomy scar, vaginal or cervical site can also be explained with this theory. This theory however, fails to clarify endometriosis at sites other than mentioned.
Lymphatic theory (halban):
It may be possible for the normal endometrium to metastasize the pelvic lymph nodes through the draining lymphatic channels of the uterus. This could explain the lymph node involvement.
Vascular theory:
This is sound at least to explain endometriosis at distant sites such as lungs, arms or thighs. [1]
Genetic and immunological factors
Genetic basis of endometriosis probably accounts for less than 10 percent of the patients. There is 6–7 times increased incidence in first degree relatives. Multifactorial inheritance is thought of. However, a defect of local cellular immunity may be responsible for the ectopic tissue to grow in abnormal sites only in susceptible women. Peritoneal macrophages normally remove the menstrual debris by phagocytosis.
Pelvic endometriosis is associated with a subclinical peritoneal inflammation resulting in increase in peritoneal fluid. In patients with endometriosis, the activated macrophages secrete several factors like cytokines, interleukin–1, α TNF, integrins and angiogenic factors. These factors promote the growth of endometrial cells over the ectopic sites. Ectopic endometrium is more resistant to apoptosis. Furthermore, activated macrophages reduce sperm motility, increase sperm phagocytosis and interfere with fertilization.
Environment theory
suggests somatic mutations of cells due to environmental factors (pollutants, dioxins). Ovarian and deep infiltrating endometriotic lesions explain with this theory. Thus, it is certain that, not all cases of endometriosis at different sites can explain by a single theory.[1]
Pathology-
General Considerations
- The endometrium (glands and stroma) in the ectopic sites have got the potentiality to undergo changes under the action of ovarian hormones
- While proliferative changes constantly evidence, the secretory changes are conspicuously absent in many; may due to deficiency of steroid receptors in the ectopic endometrium
- Cyclic growth and shedding continue till menopause. The periodically shed blood may remain encysted or else, the cyst becomes tense and ruptures
- As the blood is irritant, there is dense tissue reaction surrounding the lesion with fibrosis. If it happens to occur on the pelvic peritoneum, it produces adhesions and puckering of the peritoneum
- If encysted, the cyst enlarges with cyclic bleeding.
chocolate cyst
The serum gets absorbed in between the periods and the content inside becomes chocolate coloured. Hence, the cyst call chocolate cyst which commonly locate in the ovary. Chocolate cyst may also due to haemorrhagic follicular or corpus luteum cyst or bleeding into a cystadenoma. For this reason, the term endometrial cyst or endometrioma prefer to chocolate cyst
- In spite of dense adhesions amongst the pelvic [1]
Clinical Features
Clinical Features of Endometriosis
The clinical features of endometriosis vary widely, ranging from asymptomatic to severe and debilitating symptoms. The most common symptoms include:
Pain:
- Dysmenorrhea: Painful periods, often described as more severe than normal menstrual cramps.
- Chronic pelvic pain: Pain in the lower abdomen or pelvis that may be constant or cyclical.
- Dyspareunia: Painful sexual intercourse.
- Dyschezia: Painful bowel movements, especially during menstruation.
- Dysuria: Painful urination, especially during menstruation.
Abnormal bleeding:
- Menorrhagia: Heavy menstrual bleeding.
- Intermenstrual bleeding: Bleeding between periods.
Infertility: Endometriosis is a common cause of infertility.
Other symptoms:
- Fatigue
- Nausea
- Bloating
- Constipation
- Diarrhea [12]
Sign & Symptoms
Sign & Symptoms Of Eczema
Patient Profile
The age is between 30–45. The patients are mostly nulliparous or have had one or two children long years prior to appearance of symptoms. Infertility, voluntary postponement of first conception until at a late age and higher social status are often related. Thus, it is more common in private than hospital patients. There is often family history of endometriosis. Outflow tract obstruction is an important cause when it is seen in teenagers (10%)
Symptoms
- About 25 percent of patients with endometriosis have no symptom, being accidentally discovered either during laparoscopy or laparotomy.
- Symptoms are not related with extent of lesion. Even when the endometriosis is widespread, there may not be any symptom; conversely, there may be intense symptoms with minimal endometriosis.
- Depth of penetration is more related to symptoms rather than the spread. Lesions penetrating more than 5 mm are responsible for pain, dysmenorrhea and dyspareunia.
- Non-pigmented endometriotic lesions compared to the classic pigmented “powder burns” lesions produce more prostaglandin F (PGF) and hence are more painful.
- The symptoms are mostly related to the site of lesion and its ability to respond to hormones. Midline lesions are more symptom producing. Degree of pain is not related to the severity of endometriosis.[1]
Dysmenorrhea (70%)
There is progressively increasing secondary dysmenorrhea. The pain starts a few days prior to menstruation; gets worsened during menstruation and takes time, even after cessation of period, to get relief of pain, (co-menstrual dysmenorrhea). Pain usually begins after few years pain-free menses. The site of pain is usually deep seated and, on the back, or rectum. Increased secretion of PGF 2α, thromboxane β2 from endometriotic tissue is the cause of pain.
Abnormal menstruation (20%):
Menorrhagia is the predominant abnormality. If the ovaries are also involved, polymenorrhagia or epimenorrhagia may be pronounced. There may be premenstrual spotting.
Infertility (40–60%):
Whether endometriosis causes infertility or infertility produces endometriosis is not clear. Endometriosis is found in 20–40 percent of infertile women, where as in about 40–50 percent patients with endometriosis suffer from infertility. The multiple factors involved in producing infertility [1]
Dyspareunia (20–40%)
The dyspareunia is usually deep. It may be due to stretching of the structures of the pouch of Douglas or direct contact tenderness. As such, it is mostly found in endometriosis of the rectovaginal septum or pouch of Douglas and with fixed retroverted uterus.
Chronic Pelvic Pain
The pain varies from pelvic discomfort, lower abdominal pain or backache. The cause may be multifactorial. These include—(i) Inflammation in the peritoneal implants and release of PGF, and also due to adhesions and ovarian cysts. (ii) Action of inflammatory cytokines released by the macrophages. (iii) Invasion of nerves or involvement of bladder and bowel. The pain aggravates during period.
Abdominal Pain
There may be variable degrees of abdominal pain
around the periods. Sometimes, the pain may be acute due to rupture of chocolate cyst.[1]
Other Symptoms
The symptoms are related to the organ involved.
- Urinary—frequency, dysuria, back pain or even
haematuria
- Sigmoid colon and rectum—painful defecation (dyschezia), diarrhea, constipation, rectal bleeding or even melena
- Chronic fatigue, perimenstrual symptoms (bowel, bladder)
- Hemoptysis (rarely), catamenial chest pain
- Surgical scars—cyclical pain and bleeding
Clinical Examination
Clinical examination of Endometriosis
Physical examination findings in a patient with endometriosis include:
HEENT
Patient may have:
- Pallor (due to anemia)
Respiratory
- Decreased breath sounds and tenderness, especially on the right side (commonly present in patients with thoracic endometriosis)
Abdominal examination
- Lower abdominal tenderness
- Fixed and tender retroverted uterus (on bi-manual examination)
Digital examination of the vagina
Common physical examination findings on digital examination include:
- Fixed retroverted uterus
- Nodularity of the uterosacral ligaments
- Narrowing of the posterior vaginal fornix in patients with stage 3 and stage 4 disease
- Lateral displacement of the cervix
Speculum examination of the vagina
Speculum examination may reveal:
- Lesions of endometriosis on the cervix or vagina
- Cervical displacement. (6)
Diagnosis
Diagnosis Of Eczema
Abdominal Examination:
Abdominal palpation may not reveal any abnormality. A mass may be felt in the lower abdomen arising from the pelvis— enlarged chocolate cyst or tubo-ovarian mass due to endometriotic adhesions. The mass is tender with restricted mobility.
Pelvic Examination
Bimanual examination may not reveal any pathology. The expected positive findings are—pelvic tenderness, nodules in the pouch of Douglas, nodular feel of the uterosacral ligaments, fixed retroverted uterus or unilateral or bilateral adnexal mass of varying sizes Speculum examination may reveal bluish spots in the posterior fornix. Rectal or rectovaginal examination is often helpful to confirm the findings.[1]
Clinical diagnosis
It is by the classic symptoms of progressively increasing secondary dysmenorrhea, dyspareunia and infertility. This corroborate by the pelvic findings of nodules in the pouch of Douglas, nodular feel of the uterosacral ligaments, fixed retroverted uterus and unilateral or bilateral adnexal mass. However, physical examination has poor sensitivity and specificity. Many patients have no abnormal findings on examination.
Serum marker CA 125—
A moderate elevation of serum CA 125 notice in patients with severe endometriosis. It is not specific for endometriosis, as it significantly raise in epithelial ovarian carcinoma. However, it is helpful to assess the therapeutic response and in follow up of cases and to detect any recurrence after therapy. Monocyte Chemotactic Protein (MCP-1) level is increased in the peritoneal fluid of women with endometriosis.
Imaging
- Ultrasonography is not much helpful to the diagnosis. TVS can detect ovarian endometriomas.
- Transvaginal (TVS) and Endorectal ultrasound are Found better for rectosigmoid endometriosis.
- Magnetic Resonance Imaging (MRI) Is a diagnostic tool. There is a characteristic hyperintensity on T1 weighted images and a hypo intensity on T2 Weighted images.
- CT better compare to ultrasonography in the diagnosis. MRI Is useful for deep infiltrating endometriosis. Colonoscopy, recto sigmoidoscopy and cystoscopy done when respective organs are involved.[1]
Laparoscopy is the gold standard. Confirmation done by double puncture laparoscopy or by laparotomy.
Other benefits are:
- Confirmation of the lesion with site, size and extent.
- Biopsy is take at the same time.
- Staging is do.
- Extent of adhesions is record.
Opportunity to do laparoscopic surgery if needed. The classic lesion of pelvic endometriosis describe as ‘powder burns’ or ‘match stick’ spots on the peritoneum of the pouch of Douglas. Findings may record on video or DVD (RCOG2006) Microscopically Some of these lesions contain endometrial glands, stroma and hemosiderin-laden macrophages. [1]
Biopsy confirmation of excised lesion is ideal but negative histology does not exclude it. None of the imaging techniques including ultrasound, can diagnose specifically the peritoneal endometriosis. Empiric medical treatment usually not recommend except for pain relief and to reduce menstrual flow.[1]
Differential Diagnosis
Differential diagnosis of Endometriosis
- Pelvic inflammatory disease (PID)
- Inflammatory bowel disease
- Adenomyosis
- Pelvic congestion syndrome
- Ovarian cysts
- Fibromyalgia
- Uterine fibroids
- Polycystic ovary syndrome (PCOS)
- Urinary tract infection (UTI) (7)
Complications
Complications of Endometriosis
Endometriosis can lead to a range of complications, some of which can significantly impact a woman’s quality of life and overall health. These complications include:
Infertility: One of the most common and devastating complications of endometriosis is infertility. The endometrial tissue growth and adhesions can disrupt the normal anatomy and function of the reproductive organs, making it difficult for an egg to be fertilized or for a fertilized egg to implant in the uterus.
Chronic Pelvic Pain: Endometriosis is a leading cause of chronic pelvic pain, which can range from mild discomfort to debilitating pain that interferes with daily activities and quality of life. The pain is often associated with menstrual cycles and may worsen over time.
Ovarian Cysts (Endometriomas): Endometriosis can cause the formation of fluid-filled cysts on the ovaries, known as endometriomas. These cysts can grow large and cause pain, as well as disrupt ovarian function.
Adhesions: Endometriosis can lead to the formation of scar tissue and adhesions, which are bands of fibrous tissue that can bind organs together. Adhesions can cause pain, organ dysfunction, and bowel obstruction.
Rare Complications: In rare cases, endometriosis can invade surrounding organs and tissues, leading to complications such as bowel perforation, bladder injury, and ureteral obstruction. [13]
Investigations
Investigation of Endometriosis
Laboratory findings associated with endometriosis include:
- Features of iron deficiency anemia may be present such as:
- Low MCV
- Low MCHC
- Elevated RBC distribution width
- Low ferritin levels
- Elevated levels of serum cancer antigen-125 may be present in patients with endometriosis
- Elevated levels of serum cancer antigen-125 may be used to differentiate between endometriosis and other adnexal masses
- Increased levels of interleukin 1, chemoattractant protein 1, and interferon gamma may be present in patients with endometriosis. These are useful markers to monitor disease activity and progression.(6)
Treatment
Treatment Of Eczema
Endometriosis needs to treat as it is a progressive disease (30–60%).
- Preventive
- Curative
Preventive:
The following guidelines may prescribe to prevent or minimize endometriosis:
- To avoid tubal patency test immediately after curettage or around the time of menstruation
- Forcible pelvic examination should not done during or shortly after menstruation.
- Married women with family history of endometriosis encourage not to delay the first conception but to complete the family.[1]
Curative:
The objectives are i.e.:
- To abolish or minimize the symptoms—pelvic pain and dyspareunia to improve the fertility
- approaching menopause
- To prevent recurrence.
But it is difficult to achieve the objectives because of obscure aetiology and unpredictable life history. The results of treatment are difficult to evaluate because of lack of uniform staging or grading. The following facts are to be borne in mind.
- Asymptomatic in good number of cases.
- Subjective symptoms are not proportionate to objective signs.
- Frequent association with infertility.
- Remission during pregnancy and menopause. Prerequisites prior to therapy are accurate diagnosis with the help of laparoscopy along with staging and pictorial documentation.[1]
Treatment options for Pelvic Endometriosis:
Expectant treatment
Endometriosis is a progressive disease in about 30–60 percent of women. It is not possible to predict in which woman it will progress. Some form of treatment often need regardless of the clinical profile and to arrest the progress of the disease. However, in women with minimal to mild endometriosis role of any treatment is controversial. Cumulative pregnancy rate is similar when expectant treatment compare with conservative surgery. Case selection is important.
Protocols for Expectant Management
Observation with administration of non-steroidal anti-inflammatory drugs or prostaglandin synthetase inhibiting drugs use to relieve pain. Ibuprofen 800–1200 mg or mefenamic acid 150–600 mg a day is quite effective. The married women encourage to have conception. Pregnancy usually cures the condition. This is due to absence of shedding and decidual changes in the ectopic endometrium causing its necrosis and absorption.[1]
Hormonal treatment
The aim of the hormonal treatment is to induce atrophy of the endometriotic implants. It should consider suppressive rather than curative because of high recurrence rate. The mechanism of endometrial atrophy is either by producing ‘pseudopregnancy’ (combined oral pills) or by ‘pseudo menopause’ (Danazol) or by ‘medical oophorectomy’ (GnRH agonists). The hormonal use is gratifying in superficial peritoneal implants and endometriomas of less than 1 cm. The drugs used combine estrogenic and progestogen (oral pill), progestogens, danazol and GnRH analogues. All the drugs use continuously to produce amenorrhea and as such individualization of the dose require.
Combined oestrogen and progestogen
The low dose contraceptive pills may prescribe either in a cyclic or continuous fashion with advantages in young patients with mild disease who want to defer pregnancy. It causes endometrial Decidualization and atrophy. Pills may induce amenorrhea. It relieves dysmenorrhea. Anastrozole an aromatase inhibitor is found to reduce the growth and pain of endometriosis.[1]
Progestogens:
It causes decidualization of endometrium and atrophy. High doses may suppress ovulation and induce amenorrhea.
Oral route commonly use. Injectable preparations as depot form should withheld in patients wishing to conceive. Ovulation may remain suspended for several months following withdrawal of the therapy. The side effects are well tolerated. The Drug is comparatively cheaper than danazol. Progesterone Antagonists (Mifepristone 50–100 mg/day) has also been found effective.
Levonorgestrel-releasing-IUCD when used, found to reduce dysmenorrhea, pelvic pain, dyspareunia and menorrhagia significantly. It is especially useful for rectovaginal endometriosis.[1]
Danazol
Danazol therapy is to start from the day 5 of the menstrual cycle. The dose (600–800 mg daily) is variable and depends upon the extent of the lesions but should be adequate enough to produce amenorrhea. The patient should use barrier methods of contraception to avoid virilization of a female fetus in accidental pregnancy. Resolution of endometriotic lesions has seen in about 80% of cases but the recurrence rate is high (40%). The side effects are at times intense and intolerable to the extent of discontinuation of the therapy. A few often persist even after the therapy. The drug is costlier than progestogen. Gestrinone has got the same mechanism of action like that of danazol. The side effects are less than danazol. Administration is simple, twice a week.[1]
GnRh analogues
When used continuously act as medical oophorectomy, a state of hypoestrinism and amenorrhea. The goal to maintain a reduce level of serum oestrogen (30–45 pg/mL) so that growth of endometriosis suppress. The side effects are more tolerable than danazol. The drugs have got limited availability and costliest of all the drugs used. Long-term therapy (more than 6 months) should avoid.
Results:
The efficacy of the hormone therapy judge by relief of symptoms, reduction of the volume of the lesions as revealed by second look laparoscopy, improvement of fertility and prevention of recurrence. For Quick relief of symptoms and reduction of the volume of the lesion, GnRH Analogues are the best. Progestogens take some Time to achieve these objectives. Danazol place midway between the two. Taking every aspect together (pain relief, pregnancy rates, recurrence rates, costs and side effects), no single medical treatment is superior to others. Following medical suppression or other conservative surgery, residual endometriotic lesions may regenerate once the ovarian function re-establish. Overall recurrence rate is about 40 percent after 5 years.[1]
Surgical Management
Indications
- Endometriosis with severe symptoms unresponsive to hormone therapy.
- Severe and deeply infiltrating endometriosis to correct the distortion of pelvic anatomy.
- Endometriomas of more than 1 cm. [1]
Surgery may conservative or definitive.
Conservative Surgery:
Conservative surgery plan to destroy the endometriotic lesions in an attempt to improve the symptoms (pain, subfertility) and at the same time to preserve the reproductive function.
Laparoscopy
It commonly done to destroy endometriotic lesions by excision or ablation by electro-diatherapy or by laser vaporization. Conservative surgical treatment in minimal to mild endometriosis (ablation plus adhesiolysis) improves the fertility outcome. Laparoscopi-cutero sacral nerve ablation (LUNA) is done when pain is very severe. The advantage of laser is to cut the tissues precisely with least chance of damage to the underlying vital structures. Great deal of technical expertise is essential to avoid injury to the ureters. Surgical treatment improves fertility and symptoms in women with moderate and severe endometriosis.[1]
Prevention
Prevention of Endometriosis
- Consider getting a 24-hour urine test to evaluate your: estradiol, estrone, estriol, DHEA, testosterone, and cortisol metabolites.
- Get your thyroid tested – Ask your doctor to check your TSH, free t3, free t4, reverse t3, and thyroid antibodies. Get treated if you are low.
- Check your basal body temperature – Right when you wake up check your temperature either under your arm or in your mouth and record it. Anything less than 97.8 is an issue that should be evaluated.
- Eat clean – Cut out sugar, refined grains, white flour, caffeine, alcohol, bread, pasta, artificial sugars, and hormone-filled foods like nonorganic dairy and non-grass-fed animal protein. Eat foods to help you detox your body (broccoli, cauliflower, kale, Brussels sprouts). Eat healthy fats like flax and wild-caught fish.
Exercise often –
- Focus on high-intensity interval training to boost fat metabolism. 15-20 minutes 1-2 times per week should do the trick. On days you don’t exercise stay active by walking or taking frequent breaks at work.
- Avoid environmental toxins and xenoestrogens – Eat organic foods, drink filtered water out of glass containers, avoid plastic drinking bottles and storing food in plastic containers, and stop touching receipts (have the cashier put it in the bag). Check out the clean fifteen and the dirty dozen to find out which foods you should buy as organic.
- Detoxify your body by sweating – Take a hot bath, go into an infrared sauna, or sweat during exercise. It doesn’t matter how you do it, just make sure you sweat frequently.
- Reduce stress and increase sleep – Make sure to get at least 7-8 hours of sleep every night to reduce inflammation and cortisol levels. Reduce stress by practicing daily yoga, meditation, or prayer for at least 20 minutes.
- Consider bioidentical progesterone therapy – Adding in bioidentical progesterone can help restore the balance of estrogen to progesterone.(8)
Homeopathic Treatment
Homeopathic Treatment
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Endometriosis:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
| Cimicifuga. [Cimic] |
| The characteristic indication for this remedy in dysmenorrhea is pain flying across the pelvic region from one side to the other. It is especially useful in rheumatic and neuralgic cases, and in congestive cases it may also be thought of along with Belladonna and Veratrum viride. Headache preceding menses; during menses sharp pains across abdomen, has to double up, labor-like pains, and during menstrual interval debility and perhaps a scanty flow. The resin Macrotin is preferred by many practitioners. The pains of Cimicifuga are not severe and intense nor felt with such acuteness as are those of Chamomilla. [2] |
Caulophyllum. [Caul]
The dysmenorrhea of Caulophyllum is essentially spasmodic in character; the pains are bearing down in character. It produces a continued spasm of the uterus simulating first stage of labor; the flow is mostly normal in quantity. The spasmodic intermittent pains which call for Caulophyllum are in the groins, a useful remedy in these spasmodic cases if given between the periods. to various part of the body.
Magnesia muriatic is also a remedy which may be studied in uterine spasm. Gelsemium is similar in many respects to Caulophyllum. It is very useful remedy in neuralgic and congestive dysmenorrhea when there is such bearing down. The pains are spasmodic and labor-like, with passages of large quantities of pale urine. It is one of the best given low in hot water. It will surely relieve the pains at the start.
Belladonna. [Bell]
The congestive forms of dysmenorrhea would call for Belladonna. There is pain preceding the flow and a sensation of heaviness as if everything would protrude from the vulva, relieved by sitting up straight. The pains come on suddenly and cease suddenly; the flow is offensive and clotted. The dysmenorrhea is intensely painful, the vagina is hot and dry and the pains are cutting through the pelvis in a horizontal direction, not around the body, as in Platinum and Sepia.
Veratrum viride is use with benefit in congestive dysmenorrhea, in plethoric women, accompany with strangury and preceded by intense cerebral congestion, also spasmodic dysmenorrhea at or near the climacteric. These are conditions in which the old school knows only Opium, yet these remedies are far superior to that drug, often curing permanently while Opium is only palliative.[2]
Viburnum opulus. [Vib]
This remedy produces a sudden pain in the region of the uterus before menstruation and much backache during menses. In neuralgic and spasmodic dysmenorrhea, it has achieved considerable reputation. Dr. Hale considers it specific in this form of painful menstruation. Its chief indications seem to be in the character of the pains, which are spasmodic.
Its keynotes, therefore, are bearing down, aching in sacral and pubic region, excruciating, cramp, colicky pains in hypogastrium, much nervousness, and occasional shooting pains in the ovaries. Like Sepia, Viburnum has pains going around the pelvis and also the empty, gone feeling in the stomach; but the bearing down is more violent, culminating in an intense uterine cramp. More indicated by clinical experience than by its pathogenesis.[2]
Xanthoxylum. [Xanth]
This remedy has about only one use in homoeopathic medicine, and that is in dysmenorrhea and uterine pains. It is useful where the pains are agonizing, burning, extending down thighs along the crural nerves with a feeling as if the limbs is paralyze, the menstruation is usually profuse and with it agonizing bearing down pains; chiefly left sided are the pains of Xanthoxylum, though it also affects the right ovary.
It corresponds closely to the neuralgic form of dysmenorrhea. Hale says that the neuralgic element must predominate to have the remedy efficacious. Some further symptoms may be headache over the left eye the day before the menses, and it seems to correspond to women of spare habits and of a delicate, nervous temperament.[2]
Magnesia Phosphorica. [Mag-p]
Perhaps no remedy has achieved a greater clinical reputation in dysmenorrhea than has Magnesia Phosphorica. The pains calling for it are neuralgic and crampy preceding the flow, and the great indication for the use of this remedy is the relief from warmth and the aggravation from motion. In neuralgia of the uterus Magnesia Phosphorica vies with Cimicifuga. Uterine engorgements with the characteristic crampy pains will indicate the remedy. It has also been used successfully in membranous dysmenorrhea. We have very few remedies for this affection.
Borax is one, but it is often unsuccessful, there seems to be no very special characteristic for it, unless it be the fear of downward motion which might exist in some cases. Hale mentions Viburnum, Guaiacum and Ustilago, besides Borax, for membranous dysmenorrhea. Their indications are chiefly empirical. Colocynth, a useful remedy in dysmenorrhea, may be compared with Magnesia Phosphorica. The symptoms of Colocynth are severe left-sided ovarian pains, causing patient to double up; pains extend from umbilicus to genitals.[2]
Pulsatilla. [Puls]
Dysmenorrhea calls for Pulsatilla when the menses are dark in color and delayed; the flow will be fitful and the more severe the pains are the chillier the patient will get. The pains gripe and double the patient up. It is perhaps more useful when give between the periods, and in congestive dysmenorrhea, from wetting of the feet, it is compared with Aconite, but in Aconite the discharge is bright red instead of dark.
Chamomilla and Cocculus are two remedies which run along side by side with Pulsatilla in dysmenorrhea, and all need careful individualization. Chamomilla has also a dark flow, but it has such characteristic mental symptoms of crossness and incivility that it cannot be mistaken. It will relieve many cases (12X). Cocculus also has dark flow. It has a pain as if sharp stones were rubbing against each other in the abdomen from accumulation of flatus; the pains are worse at night, awaken the the patient and make her irritable. Menses come too early, sometimes nausea is an accompaniment. It also is said to be more efficacious given between the periods. The mental condition of Pulsatilla, if present, will always indicate the remedy. Further, if the pains shift about the indications of Pulsatilla are still stronger.[2]
Cocculus. [Cocc]
A most useful remedy in dysmenorrhea and scanty, irregular menstruation. Uterine cramps. Profuse discharge of clotted blood and severe headache accompanied by nausea; a heaving up and down of the stomach as in seasickness. It suits cases on the borderland between the neuralgic and congestive types of dysmenorrhea. Uterine cramps with suppressed irregular menstruation and a sero-purulent bloody discharge were favorite indications of Dr. Conrad Wesselhoeft. Gelsemium IX has also proved useful in the spasmodic form. Ignatia has dysmenorrhea with menstrual colic or bearing-down in the hypogastric region, labor-like pains relieved by pressure.[2]
Diet & Regimen
Diet And Regimen Of Eczema
To fight inflammation and pain caused by endometriosis, it’s best to consume a nutrient-dense, well-balanced diet that’s primarily plant-based and full of vitamins and minerals. Add these to your diet:
- fibrous foods, such as fruits, vegetables, legumes, and whole grains
- iron-rich foods, such as dark leafy greens, broccoli, beans, fortified grains, nuts, and seeds
- foods rich in essential fatty acids, such as salmon, sardines, herring, trout, walnuts, chia, and flax seeds
- antioxidant-rich foods found in colorful fruits and vegetables, such as oranges, berries, dark chocolate, spinach, and beets
Make sure you pay attention to how your body acts when you eat certain foods. Keeping a journal of the foods you eat and any symptoms or triggers you have may be helpful.
Consider meeting with a registered dietitian. They can help you plan meals that work best with you and endometriosis, as there’s no one-size-fits-all approach.[3]
Exercise:
Exercise may help with the management of endometriosis, too. This is because exercise can reduce estrogen levels and release “feel-good” hormones.
In addition to conventional methods of treatment, alternative treatments may be very helpful for women with endometriosis. For example, relaxation techniques may be beneficial. These can include:
- Meditation
- Yoga
- Acupuncture
- Massage [3]
Do’s and Don'ts
Do’s and Don’ts
Of Eczema
Do’s:
- Do seek medical advice: If you suspect you have endometriosis, consult a healthcare professional for diagnosis and treatment options.
- Do track your symptoms: Keep a diary of your pain and other symptoms, noting any patterns or triggers. This information can help you and your doctor manage your condition.
- Do exercise regularly: Regular exercise can help reduce pain and improve overall well-being.
- Do eat a healthy diet: A balanced diet rich in fruits, vegetables, and whole grains can help reduce inflammation and improve symptoms.
- Do manage stress: Stress can worsen endometriosis symptoms, so find healthy ways to manage stress, such as yoga, meditation, or deep breathing exercises.
- Do consider alternative therapies: Some women find relief from acupuncture, massage therapy, or other alternative therapies. Talk to your doctor before trying any new treatment.
Don’ts:
- Don’t ignore your symptoms: Ignoring pain or other symptoms can lead to complications and delay diagnosis and treatment.
- Don’t self-medicate: Avoid taking over-the-counter pain relievers without consulting your doctor.
- Don’t smoke: Smoking can worsen endometriosis symptoms and increase the risk of complications.
- Don’t drink excessive alcohol: Alcohol can exacerbate pain and inflammation.
- Don’t isolate yourself: Talk to friends, family, or a support group for emotional support and coping strategies.
- Don’t give up hope: While endometriosis can be challenging, there are many treatment options available. Work with your doctor to find a plan that works for you.
Terminology
Terminology Of Eczema
Medical Terms:
Endometriosis: A chronic condition where tissue similar to the lining of the uterus (endometrium) grows outside of the uterus.
Endometrioma: A type of cyst formed by endometriosis on the ovaries, often filled with old blood (sometimes called a "chocolate cyst").
Laparoscopy: A minimally invasive surgical procedure used to diagnose and treat endometriosis.
Adhesions: Bands of scar tissue that can form between organs as a result of endometriosis.
Dysmenorrhea: Painful menstrual periods.
Dyspareunia: Pain during sexual intercourse.
Pelvic Inflammatory Disease (PID): An infection of the female reproductive organs, sometimes mistaken for endometriosis due to similar symptoms.
Treatments and Procedures:
Hormone Therapy: Medications that suppress ovulation and reduce estrogen levels, often used to manage endometriosis symptoms.
Excision Surgery: The surgical removal of endometriosis lesions, often considered the most effective treatment.
Ablation Surgery: The destruction of endometriosis lesions using heat or laser, less invasive than excision but with a higher risk of recurrence.
Pain Management: Various strategies to manage pain associated with endometriosis, including medication, physical therapy, and alternative therapies.
Other Relevant Terms:
Infertility: Difficulty conceiving, a common complication of endometriosis.
Chronic Pelvic Pain: Persistent pain in the pelvic area, often caused by endometriosis.
Quality of Life: A measure of overall well-being, often negatively impacted by endometriosis.
Support Groups: Organizations or online communities that provide support and information to individuals with endometriosis.
Homeopathic Principles:
Similia Similibus Curentur: The fundamental principle of homeopathy, meaning "like cures like." It suggests that a substance that can cause symptoms in a healthy person can treat similar symptoms in a sick person.
Potentization: The process of diluting and succussing (vigorously shaking) a homeopathic remedy to increase its potency.
Individualization: The practice of tailoring homeopathic treatment to the unique symptoms and characteristics of each individual patient.
Homeopathic Remedies for Endometriosis:
Specific Remedies: Homeopathic remedies are chosen based on the individual’s specific symptoms and overall constitution. Some commonly used remedies for endometriosis include:
Sepia: For pelvic pain, menstrual irregularities, and emotional symptoms like irritability and sadness.
Lachesis: For severe menstrual cramps, ovarian cysts, and pain that worsens with heat.
Belladonna: For sudden, intense pain and inflammation.
Thuja: For hormonal imbalances and growths.
Other Homeopathic Terms:
Repertory: A reference book that lists symptoms and the remedies associated with them.
Materia Medica: A collection of descriptions of the properties and effects of homeopathic remedies.
Aggravation: A temporary worsening of symptoms after taking a remedy, often considered a sign that the remedy is working.
Constitutional Remedy: A remedy that matches the overall constitution of the patient, addressing their underlying susceptibility to illness.
Important Considerations:
Research: Scientific research on homeopathy for endometriosis is limited and inconclusive.
Consultation: It’s crucial to consult a qualified homeopathic practitioner for individualised treatment recommendations.
Complementary Approach: Homeopathymay be used alongside conventional medical treatments, but it’s important to inform your healthcare providers of all the treatments you’re using.
References
Reference
- DC Dutta Text book of Gynaecology
- Therapeutics from zomeo Ultimte LAN
- https://www.healthline.com/health/endometriosis/endometriosis-diet#exercise-and-alternative-therapies
- Endometriosis – Symptoms and causes – Mayo Clinic
- Endometriosis: What Are the Types and Stages? (webmd.com)
- Endometriosis physical examination – wikidoc
- Differential Diagnosis for Endometriosis: Similar Conditions
- How to Treat Endometriosis Naturally without Drugs (restartmed.com)
- Williams Gynecology 4th edition, by Barbara L. Hoffman, John O. Schorge, Joseph I. Schaffer, Lisa M. Halvorson, Karen D. Bradshaw, and F. Gary Cunningham (2020), Published by McGraw Hill Professional
- Comprehensive Gynecology 8th edition, by Gretchen M Lentz, William Schlaff, Rogerio Lobo, Nicholas Spirtos, Jessica Illuzzi (2023), Published by Elsevier
- Te Linde’s Operative Gynecology 13th edition, by John A. Rock and Howard W. Jones III (2020), Published by Wolters Kluwer
Also Search As
Also Searched As
Online Resources:
Homeopathic Websites and Blogs: Many homeopathic organizations and practitioners have websites and blogs that publish articles on various conditions, including endometriosis. You can search their websites directly or use a search engine with keywords like "homeopathy endometriosis article." Some examples include:
- Homeopathy UK: https://homeopathy-uk.org/conditions-directory/endometriosis/
- Dr. Tathed’s Homeopathy: https://drtathed.com/treatments/female-disorder/endometriosis/
Online Journals and Databases: Some online journals and databases specialize in alternative medicine and homeopathy. You can search these databases using keywords like "endometriosis" and "homeopathy."
Social Media Groups and Forums: Many online groups and forums dedicated to homeopathy exist on platforms like Facebook and Reddit. You can search for these groups and ask for article recommendations or search their archives.
Libraries and Bookstores:
Homeopathic Libraries: Some homeopathic colleges and organizations have libraries with a collection of books and journals on homeopathy. You can visit these libraries to search for relevant articles.
Bookstores: Many bookstores have sections dedicated to alternative medicine and homeopathy. You can browse these sections to find books and potentially articles on endometriosis.
Homeopathic Practitioners:
- Consult a Homeopath: A qualified homeopathic practitioner can be a valuable resource for information on endometriosis. They may have access to articles or research studies that are not readily available to the public.
Tips for Searching:
- Use Specific Keywords: Use specific keywords like "homeopathy," "endometriosis," and "treatment" or "management" to refine your search results.
- Check the Credibility of Sources: Ensure that the articles you find are from reputable sources, such as established homeopathic organizations, practitioners, or peer-reviewed journals.
There are several ways to search for information about endometriosis:
Online Search Engines:
- General Search Engines: Using search engines like Google, Bing, or DuckDuckGo, you can search for general information about endometriosis, its symptoms, causes, and treatment options. You can also use specific keywords like "endometriosis diagnosis," "endometriosis treatment," or "endometriosis support groups."
- Specialized Search Engines: Some search engines are specifically designed for medical information, such as PubMed or Google Scholar. These can be helpful for finding scientific articles and research studies on endometriosis.
Medical Websites and Organizations:
- Reputable Medical Websites: Many reputable medical websites, such as Mayo Clinic, Cleveland Clinic, and Johns Hopkins Medicine, have comprehensive information about endometriosis, including its symptoms, diagnosis, and treatment options.
- Endometriosis Organizations: Organizations like the Endometriosis Foundation of America (EndoFound) and the National Institutes of Health (NIH) provide information and resources for individuals with endometriosis.
Social Media:
- Support Groups and Forums: Many online support groups and forums exist for people with endometriosis. These can be a great resource for connecting with others who have similar experiences, sharing information, and finding support.
Books and Libraries:
- Medical Libraries: If you have access to a medical library, you can find books and journals with in-depth information about endometriosis.
- Public Libraries: Many public libraries have health sections with books and resources on women’s health, including endometriosis.
Healthcare Professionals:
- Your Doctor or Gynecologist: Your doctor or gynecologist is the best source of information and guidance about endometriosis. They can answer your questions, provide a diagnosis, and discuss treatment options.
- Endometriosis Specialists: Some doctors specialize in endometriosis and have extensive experience in diagnosing and treating the condition.
Frequently Asked Questions (FAQ)
What is Endometriosis?
Presence of functioning endometrium (glands and stroma) in sites other than uterine mucosa is called endometriosis.
What causes Endometriosis?
- Retrograde Menstruation
- Coelomic metaplasia
- Direct implantation
- Lymphatic theory
- Genetic and immunological factors
- Environment theory
Can endometriosis affect fertility?
Yes, endometriosis can make it harder to get pregnant. However, many women with endometriosis can still conceive with the right treatment and support.
What are the symptoms of Endometriosis?
- Dysmenorrhea
- Abnormal menstruation
- Infertility
- Dyspareunia
- Chronic Pelvic Pain
- Abdominal Pain
- Dysuria
- Haematuria
What are the treatment options for endometriosis?
Treatment varies depending on symptoms and severity. Options include pain medication, hormone therapy, and surgery to remove or destroy endometriosis tissue.
Is homeopathic treatment safe for endometriosis?
Homeopathic remedies are generally safe when prescribed by a qualified practitioner. They are often used alongside conventional treatments.
Can homeopathy help with endometriosis-related infertility?
Yes, some women have reportedimproved fertility after homeopathic treatment. However, more research is needed to confirm its effectiveness.
How does homeopathic treatment for endometriosis work?
Yes, some women have reportedimproved fertility after homeopathic treatment. However, more research is needed to confirm its effectiveness.
Which homeopathic remedies are commonly used for endometriosis?
Common remedies include Sepia, Lachesis, Belladonna, and Thuja, but the best choice depends on your specific symptoms and overall health.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Endometriosis?
Homeopathic Medicines
- Cimicifuga
- Caulophyllum
- Belladonna
- Viburnum opulus
- Xanthoxylum
- Magnesia Phosphorica
- Pulsatilla
- Cocculus
