Uterine Fibroid
Definition
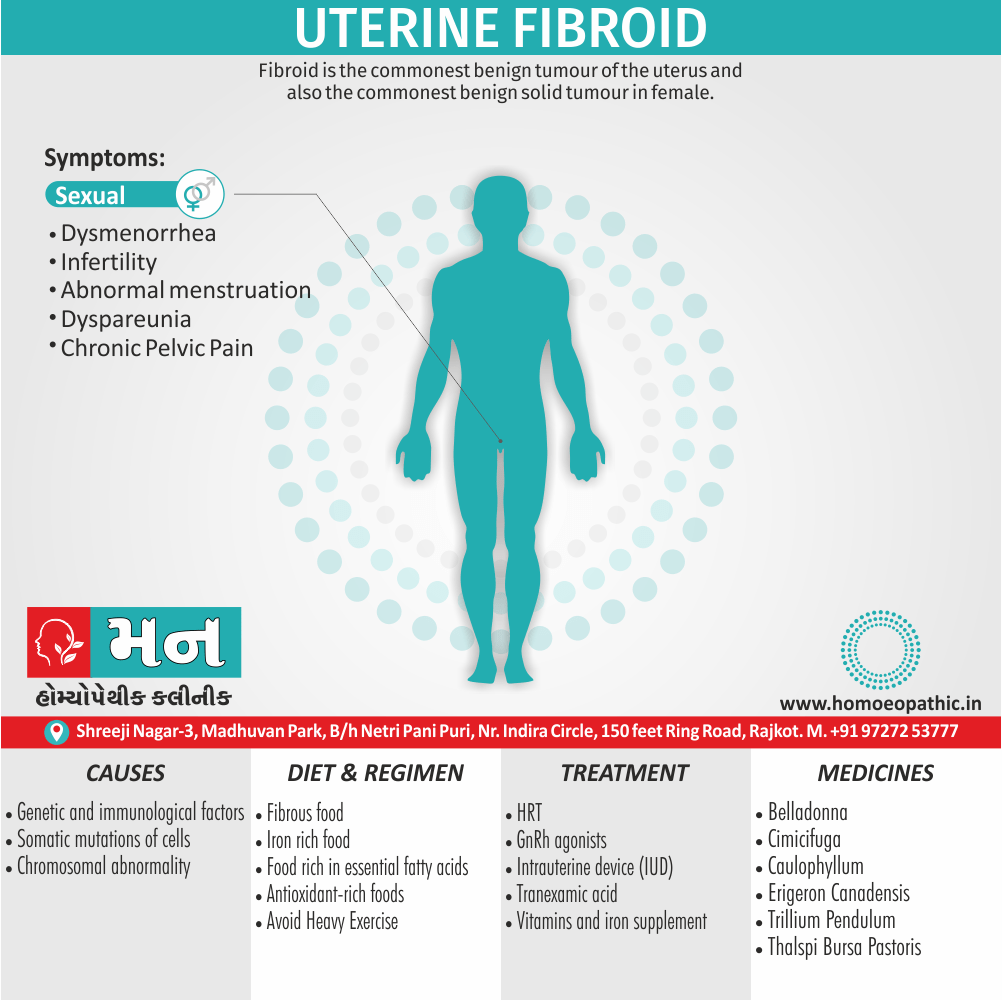
Uterine Fibroid is the commonest benign tumour of the uterus and also the commonest benign solid tumour in female. Histologically, this tumour is composed of smooth muscle and fibrous connective tissue, so named as uterine leiomyoma, myoma or fibromyoma.[1]
Uterine fibroids, also known as leiomyomas or myomas, are benign growths that develop in the muscular wall of the uterus.
There are a few synonyms for uterine fibroids, including:
- Fibroids: This is a shortened version of the term and is often used interchangeably with uterine fibroids.
- Leiomyomas: This is the medical term for fibroids, referring to their smooth muscle origin.
- Myomas: This is another medical term for fibroids, often used in clinical settings.
- Fibromyoma: This term is less common but still refers to the same type of growth.
It’s important to note that all of these terms refer to the same condition, which is non-cancerous growths in the uterus.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Uterine Fibroid
- Histologically, this tumor is composed of smooth muscle and fibrous connective tissue, so named as uterine leiomyoma, myoma or fibromyoma.
- It has been estimated that at least 20 percent of women at the age of 30 have got fibroid in their wombs.
- A high incidence of 10 percent prevails in England. Additionally, In colored races (black women), the incidence is even higher. [1]
Epidemiology
Epidemiology of Uterine Fibroid
The epidemiology of uterine fibroids in India varies depending on the population studied and the diagnostic methods used. Here’s what some recent studies have shown:
- Munusamy et al. (2017) reported a prevalence of 37.65% in rural South Indian women over a 3-year period.
- Gavli et al. (2017) found a prevalence of 24% in an urban population in Maharashtra.
These studies suggest that fibroids are quite common in India, affecting a significant proportion of women, especially in rural areas. However, it’s important to interpret these findings with caution, as they might not represent the entire Indian population due to regional variations and potential study limitations. [6] [7]
Please let me know if you have other questions or requests.
Causes
Causes of Uterine Fibroid
- Chromosomal abnormality
- Epidermal growth factor, Insulin-like growth factor-1, Transforming growth factor, Stimulate the growth of leiomyoma either directly or via estrogen
- positive family history
- Estrogen and progesterone are incriminated as the cause [1]
Types
Types of Uterine Fibroid
Body
- Interstitial or intramural (75%)
- Sub peritoneal or subserous (15%)- Subserous fibroid, Broad ligament, Wandering
- Submucous (5%)- Pedunculated, Sessile
Cervical e.g.–
- Anterior
- Posterior
- Lateral
- Central
Pseudo cervical fibroid [1]
Risk Factors
Risk Factors of Uterine Fibroid
Increased risk i.e.
- Nulliparity
- Obesity
- Hyper estrogenic state
- Black women
Reduced risk i.e.
- Multiparity
- Smoking [1]
Pathogenesis
Pathogenesis of Uterine Fibroid:
Cellular Origin
Uterine fibroids, also known as leiomyomas, are benign monoclonal tumors arising from the smooth muscle cells of the myometrium. The exact cellular origin remains uncertain, but evidence suggests they may arise from progenitor cells within the myometrium or from circulating stem cells that home to the uterus.
Genetic and Epigenetic Factors
- MED12 Mutations: Mutations in the mediator complex subunit 12 (MED12) gene are found in approximately 70% of uterine leiomyomas. These mutations are thought to disrupt gene transcription and cell signaling pathways, contributing to tumor development.
- Other Genetic Alterations: Additional genetic alterations have been identified in uterine fibroids, including mutations in HMGA2, FH, and COL4A5-COL4A6 genes, as well as chromosomal rearrangements.
- Epigenetic Changes: Epigenetic modifications, such as DNA methylation and histone modifications, also play a role in the pathogenesis of uterine fibroids by altering gene expression without changing the DNA sequence.
Hormonal Factors
- Estrogen and Progesterone: Estrogen and progesterone are key drivers of uterine fibroid growth. These hormones stimulate the proliferation of smooth muscle cells and promote the synthesis of extracellular matrix components within the tumor.
- Growth Factors: Various growth factors, including transforming growth factor-beta (TGF-β), insulin-like growth factors (IGFs), and fibroblast growth factors (FGFs), contribute to the development and growth of uterine fibroids.
Extracellular Matrix Remodeling
Uterine fibroids are characterized by an excessive accumulation of extracellular matrix (ECM) components, such as collagen, fibronectin, and proteoglycans. The balance between ECM synthesis and degradation is disrupted in these tumors, leading to their characteristic firm, rubbery consistency.
Additional Factors
- Inflammation: Chronic inflammation within the uterus may contribute to the development and growth of uterine fibroids.
- Stem Cells: The presence of stem cells within uterine fibroids may contribute to their growth and recurrence after treatment.
- Environmental Factors: Exposure to environmental toxins, such as endocrine-disrupting chemicals, may increase the risk of developing uterine fibroids.
Conclusion
The pathogenesis of uterine fibroids is complex and involves a combination of genetic, epigenetic, hormonal, and environmental factors. Further research is needed to fully elucidate the mechanisms underlying the development and growth of these tumors, which will aid in the development of more effective prevention and treatment strategies. [8]
Pathophysiology
Pathophysiology of Uterine Fibroid
- Genetic predisposition
- Menstrual cycle–related mitotic dysregulation
- Myometrial cell phenotype transformation in response to ischemia
- An inherent myometrial predisposition to fibroid formation. [4]
Clinical Features
Clinical Features of Uterine Fibroid:
Uterine fibroids, also known as leiomyomas, can present with a variety of clinical manifestations, depending on their size, number, location, and the individual patient’s characteristics. Some women with uterine fibroids may remain asymptomatic, while others experience significant symptoms that impact their quality of life.
Common Clinical Features:
- Abnormal Uterine Bleeding: This is the most common presenting symptom of uterine fibroids, affecting up to 30% of women. It can manifest as heavy menstrual bleeding (menorrhagia), prolonged menstrual bleeding, or irregular bleeding between periods (metrorrhagia).
- Pelvic Pressure and Pain: Large fibroids or those located in certain positions can cause a feeling of pelvic pressure or fullness. Pain may also occur, particularly during menstruation or sexual intercourse.
- Reproductive Dysfunction: Uterine fibroids can interfere with fertility and pregnancy outcomes. They may cause infertility, miscarriage, preterm labor, or abnormal fetal presentation.
- Urinary Symptoms: Fibroids that press on the bladder can cause urinary frequency, urgency, or difficulty emptying the bladder completely.
- Bowel Symptoms: Fibroids that press on the rectum can cause constipation or difficulty passing stool.
- Other Symptoms: Less common symptoms associated with uterine fibroids include fatigue, anemia (due to heavy menstrual bleeding), leg pain, and back pain.
Clinical Presentation Based on Fibroid Location:
- Submucosal Fibroids: These fibroids protrude into the uterine cavity and are most likely to cause heavy or prolonged menstrual bleeding.
- Intramural Fibroids: These fibroids are located within the myometrium (the muscular wall of the uterus) and can cause a variety of symptoms, including heavy menstrual bleeding, pelvic pain, and pressure.
- Subserosal Fibroids: These fibroids grow on the outer surface of the uterus and may cause pelvic pressure or pain, or they may be asymptomatic.
- Pedunculated Fibroids: These fibroids are attached to the uterus by a stalk and can sometimes twist, causing severe pain.
Asymptomatic Fibroids:
Many women with uterine fibroids have no symptoms. These fibroids are often discovered incidentally during a routine pelvic examination or imaging study.
Diagnosis:
The diagnosis of uterine fibroids is typically made based on a combination of clinical symptoms, pelvic examination findings, and imaging studies, such as ultrasound or magnetic resonance imaging (MRI).
Conclusion:
Uterine fibroids are common benign tumors that can cause a variety of clinical manifestations. The specific symptoms experienced by a woman depend on the size, number, and location of the fibroids, as well as individual patient factors. If you are experiencing any symptoms suggestive of uterine fibroids, it is important to consult with your healthcare provider for evaluation and appropriate management. [8]
Sign & Symptoms
Sign & Symptoms of Uterine Fibroid
Menstrual problems
- Menorrhagia
- Dysmenorrhea
Abdominal discomfort
- Feelings of pressure
Abdominal distension
Urinary problems
- Frequency of micturition
- Urinary retention
Bowel problems
Subfertility i.e.
- Difficulty in conceiving
- Pregnancy loss
- Intrapartum bleeding (particularly Caesarian section) [3]
Clinical Examination
Clinical Examination of Uterine Fibroid:
The clinical examination of a patient with suspected uterine fibroids typically involves a comprehensive assessment to identify any physical signs or symptoms associated with the condition. The examination may include the following components:
Abdominal Examination:
- Inspection: The clinician will visually inspect the abdomen for any signs of distension or asymmetry, which may suggest the presence of a large fibroid or multiple fibroids.
- Palpation: The clinician will gently palpate the abdomen to assess for any masses or tenderness. In some cases, a large fibroid may be palpable as a firm, irregular mass arising from the pelvis.
Pelvic Examination:
- Speculum Examination: A speculum is inserted into the vagina to visualize the cervix and vaginal walls. The clinician will look for any signs of abnormal bleeding or discharge.
- Bimanual Examination: The clinician will insert two fingers into the vagina and gently palpate the uterus and ovaries with the other hand placed on the abdomen. This allows for assessment of the size, shape, and consistency of the uterus, as well as the presence of any palpable masses or tenderness. Uterine fibroids may be felt as firm, irregular nodules within the uterine wall or projecting from its surface.
Additional Considerations:
- Rectovaginal Examination: In some cases, a rectovaginal examination may be performed to assess the posterior aspect of the uterus and the uterosacral ligaments.
- Assessment of Associated Symptoms: The clinician will also inquire about and assess for any associated symptoms, such as abnormal uterine bleeding, pelvic pain or pressure, urinary or bowel symptoms, or any impact on sexual function or fertility.
Findings on Examination:
The findings on clinical examination can vary depending on the size, number, and location of the fibroids. In some cases, the examination may be entirely normal, particularly if the fibroids are small or intramural (located within the uterine wall). However, the following findings may be suggestive of uterine fibroids:
- Enlarged Uterus: The uterus may be enlarged and irregularly shaped due to the presence of fibroids.
- Palpable Masses: Firm, irregular nodules may be palpable within the uterine wall or projecting from its surface.
- Pelvic Tenderness: Tenderness may be present in the lower abdomen or pelvis, particularly if the fibroids are large or degenerating.
Conclusion:
The clinical examination plays an important role in the evaluation of patients with suspected uterine fibroids. While the examination findings may not be specific for fibroids, they can help guide further investigation and management. Imaging studies, such as ultrasound or magnetic resonance imaging (MRI), are typically used to confirm the diagnosis and assess the size, number, and location of the fibroids. [8]
Diagnosis
Diagnosis of Uterine Fibroid
- Ultrasonography is very useful as a first line, unless the uterus is either very large or distorted leading to difficulty in visualizing the ovaries.
- Under these circumstances an MRI scan can give excellent visualization of the uterus and ovaries.
- In addition, enhancement with gadolinium gives an indication of the vascularity of the uterus.
- Biopsy of the fibroid is not commonly undertaken. [3]
Differential Diagnosis
Differential Diagnosis of Uterine Fibroid i.e.:
- Pregnancy
- Full bladder
- Adenomyosis
- Myohyperplasia
- Ovarian tumor
- TO mass [1]
Complications
Complications of Uterine Fibroid:
While uterine fibroids are generally benign tumors, they can lead to various complications that impact a woman’s health and well-being. The severity and type of complications often depend on the size, number, location, and growth pattern of the fibroids.
Abnormal Uterine Bleeding:
- Heavy Menstrual Bleeding (Menorrhagia): Excessive blood loss during menstruation can lead to anemia, fatigue, and a reduced quality of life.
- Prolonged Menstrual Bleeding: Extended periods of menstrual flow can disrupt daily activities and lead to iron deficiency.
- Irregular Bleeding: Bleeding between periods (metrorrhagia) can be unpredictable and distressing.
Pain and Pressure:
- Pelvic Pain and Pressure: Large fibroids or those located in certain positions can cause chronic pelvic discomfort, pain during intercourse (dyspareunia), and a feeling of heaviness or fullness in the lower abdomen.
- Acute Pain: Torsion (twisting) of a pedunculated fibroid can cause severe, sudden pain requiring emergency intervention.
- Degenerative Changes: Fibroid degeneration (such as necrosis or infarction) can lead to acute pain and inflammation.
Reproductive Complications:
- Infertility: While rare, fibroids can interfere with fertility by distorting the uterine cavity, blocking fallopian tubes, or impairing implantation.
- Pregnancy Complications: Fibroids can increase the risk of miscarriage, preterm labor, placental abruption, malpresentation, and cesarean delivery.
Urinary and Bowel Complications:
- Urinary Symptoms: Large fibroids pressing on the bladder can cause urinary frequency, urgency, and incomplete emptying, increasing the risk of urinary tract infections.
- Bowel Symptoms: Fibroids pressing on the rectum can cause constipation, straining, and difficulty with bowel movements.
Rare Complications:
- Ureteral Obstruction: Rarely, fibroids can compress the ureters (tubes connecting the kidneys to the bladder), leading to hydronephrosis (swelling of the kidney).
- Malignant Transformation: While extremely rare, leiomyosarcoma (a malignant tumor arising from smooth muscle) can occur within a fibroid.
Conclusion:
Although most women with uterine fibroids experience no complications, it is essential to be aware of potential risks and seek medical attention if any concerning symptoms arise. Early diagnosis and appropriate management can help prevent or mitigate complications and improve quality of life. [8]
Investigations
Investigations of Uterine Fibroid
A hemoglobin concentration i.e.:
- In brief, It will help to indicate anaemia if there is clinically significant menorrhagia.
Ultrasonography i.e.:
- Generally, It is the mainstay of diagnosis to distinguish between a fibroid and an ovarian mass.
- Furthermore, In the presence of large fibroids, ultrasonography is helpful to exclude hydronephrosis from pressure on the ureters. [2]
Saline Infusion Sonography (SIS)
Magnetic resonance imaging (MRI)
Laparoscopy
Hysteroscopy
HSG
Uterine curettage [1]
Treatment
Treatment of Uterine Fibroid
Drugs used to minimise blood loss i.e.:
- Antiprogesterones (Mifepristone)
- Danazol
- GnRH analogs: e.g.Agonists, Antagonists
- LNG–IUS
- Prostaglandin synthetase inhibitors
Surgical Treatment i.e.:
- Myomectomy
- Embolotherapy [1]
Prevention
Prevention of Uterine Fibroid:
Currently, there is no definitive way to prevent uterine fibroids. The exact cause of these tumors remains unknown, and their development is likely influenced by a complex interplay of genetic, hormonal, and environmental factors. However, some strategies may help reduce the risk or slow the growth of fibroids.
Lifestyle Modifications:
- Maintaining a Healthy Weight: Obesity is associated with an increased risk of developing fibroids. Maintaining a healthy weight through diet and exercise may help reduce this risk.
- Dietary Factors: Some studies suggest that a diet rich in fruits, vegetables, and whole grains may be associated with a lower risk of fibroids. Limiting red meat and alcohol consumption may also be beneficial.
- Stress Management: Chronic stress can impact hormone levels and potentially contribute to fibroid growth. Stress reduction techniques, such as meditation, yoga, or exercise, may be helpful.
Hormonal Contraception:
- Combined Oral Contraceptive Pills (COCPs): COCPs containing both estrogen and progestin may help reduce menstrual blood loss and alleviate some symptoms associated with fibroids.
- Progestin-Only Contraceptives: Progestin-only pills, injections, or implants may also help reduce menstrual bleeding and potentially slow fibroid growth.
- Levonorgestrel-Releasing Intrauterine System (LNG-IUS): The LNG-IUS can significantly reduce menstrual bleeding and may be a suitable option for women with fibroids who desire long-term contraception.
Other Potential Strategies:
- Early Pregnancy: Some studies suggest that having children at a younger age may be associated with a lower risk of developing fibroids.
- Vitamin D Supplementation: There is some evidence that vitamin D deficiency may be linked to an increased risk of fibroids. Maintaining adequate vitamin D levels through sun exposure or supplementation may be beneficial.
- Avoiding Exposure to Environmental Toxins: Limiting exposure to endocrine-disrupting chemicals, such as bisphenol A (BPA) and phthalates, may help reduce the risk of developing fibroids.
Important Considerations:
- Limited Evidence: The evidence supporting these preventive strategies is limited, and more research is needed to confirm their effectiveness.
- Individualized Approach: The best approach to preventing or managing fibroids will vary depending on individual circumstances and preferences. Discussing the risks and benefits of different options with a healthcare provider is essential.
- Early Detection and Management: While prevention is ideal, early detection and appropriate management of fibroids can help minimize complications and improve quality of life. Regular pelvic examinations and seeking medical attention for any concerning symptoms are crucial. [8]
Remember: While complete prevention of uterine fibroids may not be possible, adopting a healthy lifestyle and discussing potential preventive strategies with a healthcare provider can help reduce the risk and improve overall well-being.
Homeopathic Treatment
Homeopathic Treatment of Uterine Fibroid:
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Uterine Fibroid
Thalspi Bursa Pastoris – For Uterine Fibroids with Prolonged Menses
Thalspi Bursa is one of the top-grade medicines for treating uterine fibroids with prolonged menses. The menses continue for 10-15 days. Menses appear very frequently as well. The next menstrual cycle appears even before recovery from the periods has occurred. Menstrual bleeding is profuse, with the presence of large clots. Violent uterine colic during menses may also arise. Cramping pain in the uterus during menstruation in uterine fibroids cases is also suggestive of use of Thalspi Bursa Pastoris.[2]
Calcarea Carb – For Heavy Periods from Uterine Fibroids
Calcarea Carb is a very useful medicine for treating heavy periods from uterine fibroids. Menses continue for long and may even appear early. Vertigo during menses may arise. Leucorrhea of thick, milky or yellow color is another complaint that may attend.
Belladonna and Sepia Officinalis – For Uterine Fibroids where Menses are Painful
When the menses are painful Belladonna and Sepia Officinalis are well-indicate medicines for uterine fibroids. When there is cramping pain in the uterus during menses, the menses are bright red in colour and profuse at that time belladonna is use. While in case of griping, burning or bearing down pains during menses use Sepia Officinalis. Menses start early and are quite copious. Fainting and chilliness during menses may attend. Sepia Officinalis is also indicate when there is painful intercourse in uterine fibroids.[2]
Ustilago Maydis – For Uterine Fibroids with Dark Menstrual Bleeding
Ustilago Maydis is a highly suitable medicine for uterine fibroids where menstrual bleeding is dark. Clots may also be present in menstrual blood. Uterine bleeding may be stringy in nature.[2]
Sabina Officinalis – For Uterine Fibroids where Clots Pass with Menstrual Blood
In the case of menstrual bleeding with clots in uterine fibroid cases, Sabina Officinalis is a significant medicine. The slightest motion increases menstrual bleeding. Pain from sacrum to pubis is another attending feature. During menses, pain in the uterus may be present that gets better by lying on the back. Uterine pain may extend to the thighs. Other symptoms include foul, acrid, corrosive, yellow leucorrhea.[2]
Fraxinus Americana – Excellent Homeopathic medicine for uterine fibroids with bearing down sensation
Fraxinus Americana is a top-grade medicine for uterine fibroids where indicating feature is a bearing down sensation in the pelvis from uterine fibroid.[2]
Trillium Pendulum and Kali Carbonicum – For Uterine Fibroids with Back Pain during Menses
In uterine fibroid cases with back pain during the menstrual cycle, Trillium Pendulum comes highly recommended. The pain may radiate to the hips from the back during menses. Tight binding of the back and hips provides relief. Menstrual bleeding is bright red and gushing. The slightest movement worsens uterine bleeding. Trillium Pendulum is also use for inter-menstrual bleeding every two weeks. Another attending feature is faintness from uterine bleeding. Kali Carbonicum is select when there is violent back pain during menses. The pain gets better from sitting and pressure. The menstrual flow is also copious.[2]
Erigeron Canadensis – For Frequent Urination in case of Uterine Fibroids
Erigeron Canadensis is a beneficial medicine for treating frequent urination in case of uterine fibroids. In some cases, painful urination may also arise. The attending features are excessive menstrual bleeding which is bright red in colour. Erigeron Canadensis is also indicate for inter-menstrual bleeding from slight exertion.[2]
China Officinalis and Ferrum Met – For Uterine Fibroids with Heavy Bleeding and Anemia
Both China Officinalis and Ferrum Met are effective medicines for treating uterine fibroids with heavy bleeding and anemia.
Among them, China Officinalis works best when there is profuse, dark menstrual bleeding, clots in menstrual blood, exhaustion and anemia. Fainting spells may also arise.
Ferrum Met is best use where the symptoms include pale, watery, heavy and prolonged menses leading to anemia. Menstrual flow get worse by the slightest movement. Lower back pain or abdomen pain during menses may be present.[5]
Diet & Regimen
Diet & Regimen
Regimen
Engage in Regular Physical Activity:
- Rationale: Exercise helps maintain a healthy weight, reduce stress, and improve blood circulation.
- Suggestion: Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Manage Stress Effectively:
- Rationale: Chronic stress can disrupt hormone balance and potentially contribute to fibroid growth.
- Techniques: Explore stress-reduction techniques like yoga, meditation, or deep breathing exercises.
Limit Alcohol Consumption:
- Rationale: Excessive alcohol intake may increase fibroid risk.
- Recommendation: Consume alcohol in moderation, if at all.
Avoid Smoking:
- Rationale: Smoking is detrimental to overall health and may also contribute to fibroid development.
- Recommendation: If you smoke, seek support to quit.[4]
Diet:
Embrace Fiber-Rich Foods:
- Rationale: Fiber aids in estrogen detoxification, helping to regulate hormone levels and potentially reduce fibroid growth.
- Sources: Incorporate whole grains, legumes, fruits, and vegetables into your daily diet.
Prioritize Fruits and Vegetables:
- Rationale: These nutritional powerhouses are rich in antioxidants and phytochemicals, which may combat inflammation and oxidative stress associated with fibroid development.
- Emphasis: Include a variety of colorful fruits and vegetables to maximize nutrient intake.
Limit Red Meat and Processed Foods:
- Rationale: High consumption of red meat and processed foods has been linked to an increased risk of fibroids.
- Recommendation: Opt for lean protein sources like poultry, fish, and plant-based options.
Moderate Dairy Consumption:
- Rationale: Some studies suggest that high dairy intake may be associated with a higher risk of fibroids.
- Suggestion: Choose low-fat or fat-free dairy products in moderation.
Maintain a Healthy Weight:
- Rationale: Obesity is a risk factor for fibroids, as excess fat tissue can produce estrogen.
- Recommendation: Strive for a healthy weight through a balanced diet and regular exercise
Do’s and Don'ts
Do’s & Don’ts
Uterine Fibroid Do’s & Don’ts
Do’s
Load up on fresh fruits and vegetables.
Basically, A recent study found that eating plenty of fruits like apples and tomatoes, and cruciferous vegetables like broccoli and cabbage, could lower the risk of developing fibroids. Additionally, eating healthier choices like organic fruits and vegetables and whole-grain foods could help improve your symptoms.[4]
Keep an eye on your blood pressure.
Researchers have shown a strong link between fibroids also high blood pressure. In detail, Talk to your doctor about how to manage your blood pressure, either with diet, lifestyle, or medication.
Manage your stress level.
While researchers are still examining the impact of stress on fibroids, some studies suggest the two may link. Try relaxation techniques like yoga, massage, also tai chi to help manage your stress. Some women find that alternative therapies like acupuncture can help relieve their period pain, too.[4]
Make yourself comfortable.
If you’re having painful periods because of your fibroids, try lying down and elevating your legs with a pillow. Or lie on your side and bring your knees into your chest to take the pressure off your back.
Talk to your doctor before trying any supplements.
There is some research that suggests supplements like vitamin D could be helpful in lowering your risk for fibroids.
While some alternative medicine practitioners recommend supplements like raspberry leaf tea to support pregnancy and treat issues like PMS but not for fibroids. That’s because the tea can have an estrogen-like effect on the body and make your problem worse. That’s why it’s always important to discuss all medications and supplements — even if they’re natural — with your doctor. They could have side effects you’re not aware of.[4]
Don’ts of Uterine Fibroid
Don’t eat a diet full of processed foods, red meats, and high-fat dairy.
Studies show that eating these foods can make your fibroids worse. The same goes for alcohol and caffeine.
Don’t skip your workouts.
One study found that women who exercised the most (about 7 hours per week of activities like running, dancing, or walking) had the lowest chance of developing fibroids. Exercise can also help keep your blood pressure down.
Don’t overdo it on the sugar.
A study found that a higher risk of fibroids can link to eating a high-sugar diet .
Don’t smoke.
Experts believe that smoking can increase your period pain because it reduces the amount of oxygen that gets to your pelvic region.[4]
Terminology
Terminology of Uterine Fibroid
Certainly, here are some terminologies and their meanings commonly used in the context of uterine fibroids:
Uterine Fibroids:
- Meaning: Benign (non-cancerous) tumors that grow from the muscle layers of the uterus. They are also called leiomyomas or myomas.
Myometrium:
- Meaning: The muscular wall of the uterus.
Submucosal Fibroids:
- Meaning: Fibroids that grow into the inner cavity of the uterus.
Intramural Fibroids:
- Meaning: Fibroids that grow within the muscular wall of the uterus.
Subserosal Fibroids:
- Meaning: Fibroids that grow on the outside of the uterus.
Pedunculated Fibroids:
- Meaning: Fibroids that grow on a stalk or pedicle, extending from the uterus.
Menorrhagia:
- Meaning: Heavy or prolonged menstrual bleeding.
Metrorrhagia:
- Meaning: Bleeding between periods.
Dyspareunia:
- Meaning: Painful sexual intercourse.
Anemia:
- Meaning: A condition where the blood doesn’t have enough healthy red blood cells.
Pelvic Pressure:
- Meaning: A feeling of fullness or heaviness in the lower abdomen or pelvis.
Urinary Frequency:
- Meaning: The need to urinate more often than usual.
Constipation:
- Meaning: Difficulty passing stools or infrequent bowel movements.
Infertility:
- Meaning: The inability to conceive after one year of trying.
Miscarriage:
- Meaning: The spontaneous loss of a pregnancy before 20 weeks of gestation.
Preterm Labor:
- Meaning: Labor that starts before 37 weeks of pregnancy.
Ultrasound:
- Meaning: An imaging technique that uses sound waves to create pictures of internal organs.
Magnetic Resonance Imaging (MRI):
- Meaning: An imaging technique that uses a magnetic field and radio waves to create detailed images of organs and tissues.
Hysterectomy:
- Meaning: Surgical removal of the uterus.
Myomectomy:
- Meaning: Surgical removal of fibroids while preserving the uterus.
These are just a few of the common terminologies encountered when discussing uterine fibroids. Understanding these terms is essential for com
Certainly, let’s explore some terminologies and their meanings that are commonly used in homeopathic articles discussing uterine fibroids:
Homeopathic Terms:
Similia Similibus Curentur: This Latin phrase translates to "like cures like," and it is the fundamental principle of homeopathy. It suggests that a substance that can cause symptoms in a healthy person can also cure similar symptoms in a sick person.
Potentization: This refers to the process of diluting and succussing (vigorously shaking) a homeopathic remedy to increase its therapeutic effect while reducing any potential toxicity.
Repertory: A repertory is a reference book used by homeopaths to find remedies based on the patient’s specific symptoms.
Materia Medica: A materia medica is a collection of detailed information about the therapeutic properties of homeopathic remedies.
Constitutional Remedy: A constitutional remedy is chosen based on the patient’s overall physical, mental, and emotional characteristics, and it aims to address the root cause of the disease.
Uterine Fibroid Specific Terms:
Menorrhagia: Excessive menstrual bleeding.
Metrorrhagia: Bleeding between periods.
Dysmenorrhea: Painful menstruation.
Prolapse: Downward displacement of the uterus.
Bearing-down Sensation: A feeling of pressure or heaviness in the pelvis.
Leucorrhoea: Whitish or yellowish vaginal discharge.
Common Homeopathic Remedies for Uterine Fibroids:
Calcarea carbonica: Indicated for heavy menstrual bleeding, fatigue, and a tendency to be chilly.
Thuja occidentalis: Often used for multiple fibroids, especially if they are hard and painful.
Pulsatilla: Suitable for women with changeable moods, weepiness, and a tendency to feel better in open air.
Lachesis: Indicated for fibroids with premenstrual aggravation, a sense of constriction, and left-sided symptoms.
Sepia: Helpful for women with a sense of indifference, bearing-down sensation, and hormonal imbalances.
Remember, homeopathic treatment is individualized, and the selection of the appropriate remedy depends on the unique symptom picture of each patient. It is crucial to consult with a qualified homeopath for personalized treatment and management of uterine fibroids.
References
References of Uterine Fibroid
- DC Dutta’s Textbook of Gynecology (PDF Drive)
- Gynecology by Ten Teachers
- Dewhurst_s_Textbook_of_Obstetrics_and_Gynaecology_7th_ed
- Women’s Encyclopedia of Natural Medicine 2nd Edition
- https://www.drhomeo.com/uterine-fibroids/homeopathic-remedies-for-uterine-fibroids-treatment/
- Munusamy et al. (2017)
- Gavli et al. (2017)
- Williams Gynecology", 4th Edition, by Barbara L. Hoffman, John O. Schorge, Joseph I. Schaffer, Lisa M. Halvorson, Karen M. Brader, and Vanessa L. Jacoby, published in 2020 by McGraw Hill Medical.
Also Search As
Also Search As
People can search for homeopathic articles on uterine fibroids in several ways:
Online Search Engines:
- Specific search terms: Use keywords like "homeopathy uterine fibroids," "homeopathic remedies for fibroids," or "homeopathic treatment for uterine fibroids" on popular search engines like Google, DuckDuckGo, or Bing.
- Include specific remedies: If you’re interested in a specific remedy, include it in your search, e.g., "Calcarea carbonica for fibroids."
- Use quotation marks: Enclose phrases in quotation marks to search for the exact phrase, ensuring more relevant results.
Websites and Blogs:
- Reputable homeopathic organizations: Visit the websites of well-known homeopathic organizations or associations. They often have articles or resources on various health conditions, including uterine fibroids.
- Homeopathic practitioners’ blogs: Many homeopathic practitioners maintain blogs where they share information and case studies related to their practice. Search for blogs that specialize in women’s health or gynecology.
Forums and Communities:
- Online forums: Engage in discussions on homeopathic forums or communities where individuals share their experiences and knowledge about different remedies and approaches for various health issues.
- Social media groups: Join relevant social media groups or pages dedicated to homeopathy. These platforms often facilitate the exchange of information and allow you to ask questions or seek recommendations.
Libraries and Bookstores:
- Local libraries: Check your local library for books or journals on homeopathy. They may have resources dedicated to specific conditions like uterine fibroids.
- Online bookstores: Explore online bookstores that offer a wide range of homeopathic literature. Look for books written by experienced homeopaths specializing in women’s health or gynecology.
Additional Tips:
- Be specific in your search: The more specific your search terms, the more likely you are to find relevant articles.
- Use reliable sources: Choose websites and publications from reputable homeopathic organizations or practitioners to ensure accuracy and credibility.
- Consult with a qualified homeopath: If you are considering homeopathic treatment for uterine fibroids, it is essential to consult with a qualified homeopath for personalized advice and guidance.
By following these strategies, individuals interested in learning about homeopathic approaches to uterine fibroids can access a wealth of information and resources.
There are numerous ways to search for information about Uterine Fibroids, each catering to different needs and preferences:
Online Search Engines:
- General search terms: Use broad keywords such as "uterine fibroids," "fibroids," or "leiomyomas" on major search engines like Google, Bing, or DuckDuckGo.
- Specific queries: Refine your search by including specific aspects like "uterine fibroids symptoms," "fibroids treatment options," or "fibroids causes."
- Image search: Explore images related to uterine fibroids to better understand their appearance and location within the uterus.
Medical Websites and Databases:
- Reputable health organizations: Consult websites of well-known medical institutions like the Mayo Clinic, Cleveland Clinic, or the National Institutes of Health (NIH). They provide reliable information on various health conditions, including uterine fibroids.
- Medical journals and databases: Access academic articles and research papers on uterine fibroids through medical databases like PubMed or Google Scholar.
- Patient support groups and forums: Connect with others dealing with uterine fibroids through online communities and forums to share experiences and gain insights.
Health Professionals and Organizations:
- Consult your doctor: Schedule an appointment with your gynecologist or primary care physician to discuss your concerns about uterine fibroids and seek personalized advice.
- Specialized clinics: Visit clinics or hospitals that specialize in women’s health or gynecology for expert opinions and treatment options.
- Non-profit organizations: Reach out to organizations dedicated to women’s health or specific conditions like uterine fibroids for educational resources and support services.
Books and Libraries:
- Medical textbooks: Consult medical textbooks specializing in gynecology or women’s health for detailed information on uterine fibroids.
- Patient education books: Look for books specifically written for patients to understand uterine fibroids in a simplified and accessible manner.
- Local libraries: Utilize your local library’s resources to find books and articles on uterine fibroids.
Other Resources:
- Health magazines and blogs: Explore reputable health magazines and blogs that publish articles on women’s health and related topics.
- Documentaries and videos: Watch informative documentaries or videos on uterine fibroids available on platforms like YouTube or streaming services.
- Podcasts: Listen to podcasts featuring healthcare professionals discussing various aspects of uterine fibroids.
Remember, when searching for information on uterine fibroids, focus on reliable sources like reputable medical institutions, healthcare professionals, and peer-reviewed journals. Always prioritize information that is current, evidence-based, and relevant to your specific situation. If in doubt, consult with your doctor for personalized advice and guidance.
Frequently Asked Questions (FAQ)
What is uterine prolapse?
Uterine prolapse occurs when the uterus descends from its normal position in the pelvis and protrudes into the vagina.
This happens due to weakening or damage to the pelvic floor muscles and ligaments that support the uterus.
What are the symptoms of uterine prolapse?
Common symptoms include:
- A sensation of heaviness or pressure in the pelvis
- Feeling like something is falling out of the vagina
- Tissue protruding from the vagina
- Difficulty with bowel movements or urinationLower back painDiscomfort during sexual intercourse
What causes uterine prolapse?
Several factors can contribute to uterine prolapse, including:
- Childbirth: Vaginal deliveries can weaken the pelvic floor muscles and ligaments.
- Aging: The natural aging process can lead to decreased muscle tone and support.
- Menopause: Reduced estrogen levels after menopause can affect the strength of pelvic tissues.
- Chronic conditions: Conditions that increase intra-abdominal pressure, like obesity or chronic constipation, can put stress on the pelvic floor.
- Genetics: Some women may have a genetic predisposition to weaker connective tissue.
How is uterine prolapse diagnosed?
A healthcare provider can usually diagnose uterine prolapse during a pelvic exam.
They will assess the position of the uterus and the extent of prolapse. Additional tests, like imaging studies, may be done to rule out other conditions.
What are the treatment options for uterine prolapse?
Treatment They include:
- Observation and lifestyle changes: For mild cases, observation and lifestyle changes like weight management, pelvic floor exercises, and avoiding heavy lifting may be sufficient.
- Pessary: A pessary is a removable device inserted into the vagina to support the uterus.
- Surgery: Surgical options include repairing or reconstructing the pelvic floor muscles and ligaments or removing the uterus (hysterectomy).
Can homeopathy help with uterine fibroids?
Yes,
homeopathy offers a potential approach to managing uterine fibroids by addressing the underlying imbalances and stimulating the body’s self-healing abilities.
Which homeopathic remedies are commonly used for uterine fibroids?
Some Homeopathic frequently used remedies include:
Calcarea carbonica, Thuja occidentalis, Pulsatilla, Lachesis, and Sepia. The choice of remedy depends on the individual’s specific symptoms and constitution.
How does homeopathy work for fibroids?
Homeopathy aims to stimulate the body’s vital force to restore balance and promote healing.
Remedies are chosen based on the principle of "like cures like," addressing the unique symptom picture of each individual.
Is homeopathic treatment safe for fibroids?
Homeopathic remedies are generally considered safe and non-toxic when prescribed by a qualified practitioner.
They are often used alongside conventional treatments or as a complementary approach.
How long does it take to see results with homeopathy for fibroids?
The response time varies depending on the individual, the severity of the condition, and other factors. Some individuals may experience improvement in symptoms within a few weeks, while others may require longer-term treatment.
