Conjunctivitis
Definition
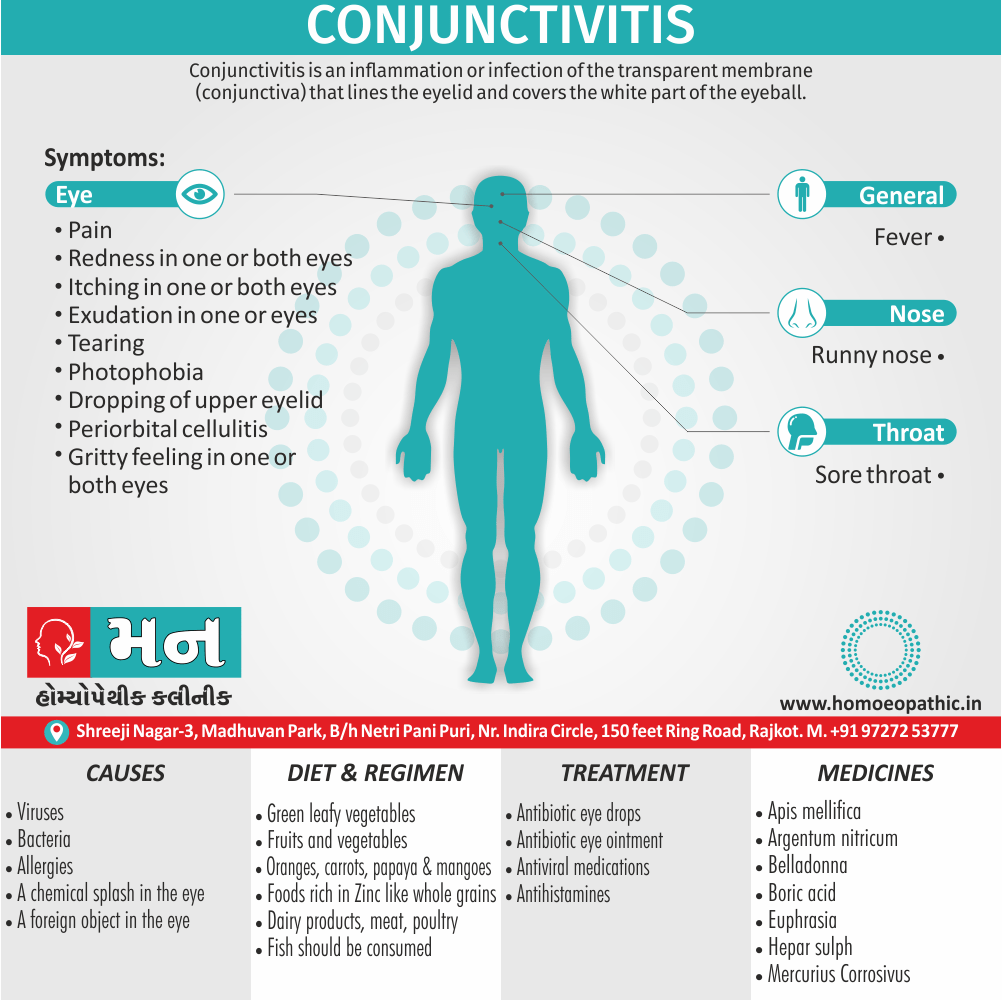
Conjunctivitis is an inflammation or infection of the transparent membrane (in other words, conjunctiva) that lines the eyelid and covers the white part of the eyeball. [1]
The most common synonym for conjunctivitis is pink eye.
Here are other, less common synonyms for conjunctivitis:
- Madras eye (archaic)
- Acute catarrhal conjunctivitis (referring specifically to viral conjunctivitis)
- Egyptian ophthalmia (archaic, refers to a specific type of bacterial conjunctivitis)
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications XXX
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
When small blood vessels in the conjunctiva become inflamed, they are more visible. Additionally, This is what causes the white of the eyes to appear reddish or pink. Also known as “pink eye”.
Moreover, Conjunctivitis resulting from irritation
Irritation from a either chemical splash or foreign object in the eye is also associated with conjunctivitis.
Lastly, Sometimes flushing and cleaning the eye is done to get rid of the chemical or object causing redness and irritation. [1]
Epidemiology
Epidemiology
Key Points:- Describes the outbreaks of enteroviral conjunctivitis (causing acute hemorrhagic conjunctivitis) in India since it was first documented in 1971.
- Details the cyclical nature of these epidemics, occurring initially every four years and then more frequently every 2-3 years.
- Discusses the lack of systematic epidemiological investigations despite the widespread impact of the disease.
- Mentions the identification of two enteroviruses, EV70 and CA24v, as causative agents of the outbreaks.[6]
Conjunctivitis cases continue to surge in India; Here’s what you need to know
Key Points:- Reports a significant surge in conjunctivitis cases across India, particularly in Maharashtra, with over 87,000 cases in July 2024.
- Highlights the spread of Adenovirus conjunctivitis as the primary cause of the current outbreak.
- Mentions the most affected regions, including Buldhana in Maharashtra, Vijayanagar district in Karnataka, and Patna in Bihar.[7]
Case report: An outbreak of viral conjunctivitis among the students and staff of visually impaired school, Tamil Nadu, India, 2020
Key Points:- Describes an outbreak of viral conjunctivitis in a school for the visually impaired in Tamil Nadu in early 2020.
- Reports an overall attack rate of 76% among students and staff.
- Identifies potential risk factors, including male gender, hostel residence, and close contact with a confirmed case.[8]
Prevalence of Conjunctivitis among the Population of Kanyakumari District
Key Points:- Reports a prevalence of bacterial conjunctivitis of 68.1% in the Kanyakumari district.
- Highlights the higher prevalence of conjunctivitis in rural residents (59%) compared to urban residents (34.66%).
- Finds that males are more affected (59.4%) than females (40.6%).[9]
Additional Notes:
- These references provide snapshots of conjunctivitis outbreaks and prevalence studies at different times in India.
- The epidemiology of conjunctivitis in India is dynamic and influenced by various factors, including seasonality, causative agents, and population demographics.
- Please note that this is not an exhaustive list, and further research may reveal additional epidemiological studies and outbreaks in India.
Causes
Causes
- Viruses
- Bacteria
- Allergies
- A chemical splash especially, in the eye
- A foreign object in the eye
- In new-borns, a blocked tear duct [1]
Types
Types
Viral:
May affect one or both eyes. Furthermore, Viral conjunctivitis usually produces a watery discharge. It can associate with colds or with symptoms of a respiratory infection, such as sore throat. Generally, It can spread through direct or indirect contact with the eye secretions of someone who’s infected. Lastly, Adults and children alike can develop both of these types of pink eye secretions of someone who’s infected.
Bacterial:
It may affect one or both eyes. Specifically, Bacterial conjunctivitis produces a thick, yellow-green discharge. It can spread through either direct or indirect contact with the eye secretions of someone who’s infected. Adults also children alike can develop both of these type of pink eye secretions of someone who’s infected.
Allergic conjunctivitis:
Allergic conjunctivitis affects both eyes and a response to allergens, the body produces an antibody call immunoglobulin E (in other words, Ig.E). Most allergic conjunctivitis can control with allergy eye drops. [1]
Risk Factors
Risk factors
- Explore to something for which the person has an allergy (in other words, allergic conjunctivitis).
- Explore to someone infected with either viral or bacterial form of conjunctivitis.
- Using contact lenses.
Pathogenesis
Pathogenesis
Conjunctivitis is an inflammation of the conjunctiva. The specific pathogenesis depends on the underlying cause:
Infectious Conjunctivitis:
- Bacterial: Bacteria adhere to the conjunctival epithelium, multiply, and release toxins, leading to inflammation and tissue damage.
- Viral: Viruses invade conjunctival cells, replicate, and cause cell death, leading to inflammation.
- Chlamydial: Chlamydia infects conjunctival epithelial cells, causing inflammation and chronic infection.
Allergic Conjunctivitis:
- Allergens bind to IgE on mast cells, triggering the release of histamine and other mediators, leading to vasodilation, edema, and itching.
Irritant Conjunctivitis:
- Chemicals or irritants directly damage the conjunctival epithelium, leading to inflammation.[10]
Pathophysiology
Pathophysiology
Microbes enter the eye on contact with infected objects that produce Inflammation of the eye also Dilation of blood vessels of eye that leads to Swelling, redness, exudates also discharge of eyes.[1]
Clinical Features
Clinical Features
The clinical features of conjunctivitis vary depending on the underlying cause:
Bacterial Conjunctivitis:
- Mucopurulent discharge (yellow or green)
- Matting of eyelashes, especially upon waking
- Conjunctival hyperemia (redness)
- Conjunctival papillae (small bumps on the inner surface of the eyelid)
- Mild discomfort or foreign body sensation
Viral Conjunctivitis:
- Watery discharge
- Conjunctival hyperemia
- Conjunctival follicles (small, clear bumps on the conjunctiva)
- Preauricular lymphadenopathy (swollen lymph node in front of the ear)
- Itching and burning sensation
Allergic Conjunctivitis:
- Itching (hallmark symptom)
- Watery discharge
- Conjunctival hyperemia
- Conjunctival edema (swelling)
- Chemosis (swelling of the conjunctiva that makes it look like it is overlapping the cornea)
- Papillary hypertrophy (enlarged papillae on the inner surface of the eyelid)
Irritant Conjunctivitis:
- Foreign body sensation
- Burning and stinging
- Tearing
- Conjunctival hyperemia
- Mild discharge[10]
Sign & Symptoms
Sign & Symptoms
- Pain
- Redness in one or both eyes
- Itching in one or both eyes
- A discharge in one or both eyes that forms the crust during the night that may prevent your eye or eyes from opening in the morning i.e., exudation.
- Tearing
- Photophobia
- Dropping of upper eyelid
- Periorbital cellulitis
- Fever
- Sore throat
- Runny nose
- A gritty feeling in one or both eyes. [1]
Clinical Examination
Clinical examination of Conjunctivitis
Physical examination of patients with conjunctivitis is usually remarkable for conjunctival injections, epiphora, hyperemia, chemosis, and muco-purulent or watery discharge. However, ophthalmologic examination may be varies based on conjunctivitis subtypes.
Viral Conjunctivitis
Patients with viral conjunctivitis usually appear febrile, and they have preauricular adenopathy. Ophthalmologic examination of patients with viral conjunctivitis is usually remarkable for:
- Epiphora
- Hyperemia
- Chemosis
- Lymphoid follicle on the under-surface of the eyelid
- Follicular conjunctival reaction
- Pseudomembrane formation (occasionally)
- Cicatricial conjunctival reaction
- Eyelids ecchymosis
- Corneal epithelial defect (in severe cases)
Acute Hemorrhagic Conjunctivitis
Ophthalmologic examination of patients with acute hemorrhagic conjunctivitis is usually remarkable for:
- Eyelid edema
- Eye pain in palpation
- Bulbar conjunctival hemorrhage
Bacterial Conjunctivitis
Ophthalmologic examination of patients with bacterial conjunctivitis is usually remarkable for:
- Bulbar conjunctival injection
- Palpebral conjunctival papillary reaction
- Watery or mucopurulent discharge
- Chemosis
- Lid erythema
- Corneal involvement
Neonatal Conjunctivitis
Ophthalmologic examination of patients with neonatal conjunctivitis or ophthalmia neonatorum is usually remarkable for:
- Neisseria gonorrhea
- Chemosis
- Severe lid edema
- Mucopurulent discharge
- Corneal involvement (diffuse epithelial edema, ulceration, corneal perforation, and endophthalmitis
- Chlamydia trachomatis
- Mild hyperemia
- Mucoid discharge
- Chemosis
- Pseudomembrane formation
- Chemical
- Mild conjunctival injection
- Epiphora
Allergic Conjunctivitis
Ophthalmologic examination of patients with allergic conjunctivitis is usually remarkable for:
- Bilateral conjunctival injection
- Chemosis
- Watery discharge or mild mucous discharge
- Large cobblestone papillae under upper eyelid
Keratoconjunctivitis Sicaa
Examination should include evaluation of the face, eyelids, blinking patterns, eyelid margins, eyelashes, conjunctiva, cornea, and tear film. Examination of patients with keratoconjunctivitis sicaa is usually remarkable for:
- Conjunctival redness
- Damage to the ocular surface with punctate epithelial
- Thickened eyelid margins and telangiectasia (signs of meibomian gland dysfunction)
- Meibomian gland orifices are obstructed with a cloudy or granular secretion (expressed by exerting considerable pressure on the lower lid)
- Blepharitis (associated with meibomian gland dysfunction)
- Meibomitis (inflammation of the meibomian glands)
Superior Limbic Keratoconjunctivitis
Ophthalmologic examination of patients with superior limbic keratoconjunctivitis (SLK) is usually remarkable for
- Hyperemia
- Micro-papillary reaction in the upper tarsal conjunctiva
- Thickening of the superior bulbar conjunctiva
- Ciliary injection in the upper bulbar conjunctiva
- Corneal erosion in the upper quadrants
- Diffuse superficial corneal erosions
- Eyelid edema (4)
Diagnosis
Diagnosis of Conjunctivitis
To determine whether the patient have pink eye, the doctor will examine the eyes.
Take a sample of eye secretions from the conjunctiva for laboratory analysis if the patient has a very severe case of conjunctivitis, if the corneas are affected or if the person had repeated infections that are not responding to treatment.
Differential Diagnosis
Differential diagnosis of Conjunctivitis
- Acute viral conjunctivitis.
- Blepharitis.
- Allergic conjunctivitis.
- Toxic and chemical conjunctivitis.
- Anterior uveitis
- Episcleritis
- Scleritis. (5)
Complications XXX
Complications
Bacterial Conjunctivitis:
- Corneal involvement: In severe cases or with certain bacteria (e.g., Neisseria gonorrhoeae), the infection can spread to the cornea, causing keratitis (inflammation of the cornea) or even corneal ulceration. This can lead to permanent vision loss if not treated promptly.
- Membranous or pseudomembranous conjunctivitis: Some bacteria (e.g., Corynebacterium diphtheriae) can cause a severe form of conjunctivitis with the formation of membranes or pseudomembranes on the conjunctival surface. These can lead to scarring and vision impairment.
Viral Conjunctivitis:
- Subconjunctival hemorrhage: In some cases, viral conjunctivitis can cause bleeding under the conjunctiva, leading to a red patch on the white of the eye. This is usually harmless and resolves on its own.
- Keratitis: Certain viruses (e.g., adenovirus) can also cause keratitis, which can lead to vision loss if not treated.
Allergic Conjunctivitis:
- Chronic conjunctivitis: If left untreated or if exposure to allergens continues, allergic conjunctivitis can become chronic, leading to persistent discomfort and potentially long-term damage to the eye.
- Keratoconus: In rare cases, chronic allergic conjunctivitis has been associated with the development of keratoconus, a condition where the cornea becomes thin and cone-shaped, leading to vision distortion.
Other Complications (All Types):
- Dry eye syndrome: Conjunctivitis can disrupt the tear film, leading to dry eyes, which can cause discomfort and increase the risk of eye infections.
- Secondary infections: In some cases, conjunctivitis can predispose to secondary bacterial infections, especially if the eye is repeatedly rubbed or if the immune system is compromised.[10]
Investigations
Investigations
Clinical History:
- A detailed history is crucial to assess the onset, duration, and characteristics of symptoms (e.g., discharge, itching, pain).
- Questions about recent illness, contact with others with conjunctivitis, allergies, and use of contact lenses can provide valuable clues.
Physical Examination:
- Slit-lamp examination allows for a detailed assessment of the conjunctiva, cornea, and eyelids.
- It helps identify specific features like papillae, follicles, membranes, discharge characteristics, and corneal involvement.
- Preauricular lymph nodes are also examined.
Laboratory Investigations:
- Conjunctival swab and culture: This is the most important test for identifying the causative organism in bacterial or fungal conjunctivitis.
- Viral studies: Polymerase chain reaction (PCR) or viral culture may be performed in suspected viral conjunctivitis, particularly if adenovirus is considered.
- Allergy testing: Skin prick tests or serum IgE levels may be considered in suspected allergic conjunctivitis.[10]
Treatment
Treatment of Conjunctivitis
For bacterial conjunctivitis–
In detail, If the infection is bacterial, the doctor may prescribe antibiotic eye drops as pink eye treatment, and the infection should go away within several days. Additionally, Antibiotic eye ointment, in place of eye drops, is sometimes prescribed for treating bacterial pink eye in children.
With either form of medication, expect signs also symptoms to start getting better in a few days.
Treatment for viral conjunctivitis–
There is no treatment for most cases of viral conjunctivitis. Instead, the virus needs time to run its course- up to two or three weeks. Viral conjunctivitis often begins in one eye and then infects the other eye within a few days. Moreover, The signs and symptoms should gradually clear on their own.
In brief, Antiviral medications may be an option if the doctor determines that the viral conjunctivitis is caused by the herpes simplex virus.
Treatment for allergic conjunctivitis–
These may include medications that help control allergic reactions, such as antihistamines or drugs that help control inflammation, such as steroids and anti-inflammatory drops. [1]
Prevention
Prevention of Conjunctivitis
- Wash your hands often with soap and warm water for at least 20 seconds. Wash them especially well before and after cleaning, or applying eye drops or ointment to, your infected eye. If soap and water are not available, use an alcohol-based hand sanitizer that contains at least 60% alcohol to clean hands.
- Avoid touching or rubbing your eyes. This can worsen the condition or spread it to your other eye.
- With clean hands, wash any discharge from around your eye(s) several times a day using a clean, wet washcloth or fresh cotton ball. Throw away cotton balls after use, and wash used washcloths with hot water and detergent, then wash your hands again with soap and warm water.
- Do not use the same eye drop dispenser/bottle for your infected and non-infected eyes.
- Wash pillowcases, sheets, washcloths, and towels often in hot water and detergent; wash your hands after handling such items.
- Stop wearing contact lenses until your eye doctor says it’s okay to start wearing them again.
- Clean eyeglasses, being careful not to contaminate items (like hand towels) that might be shared by other people.
- Clean, store, and replace your contact lenses as instructed by your eye doctor.
- Do not share personal items, such as pillows, washcloths, towels, eye drops, eye or face makeup, makeup brushes, contact lenses, contact lens storage cases, or eyeglasses.
- Do not use swimming pools. (5)
Homeopathic Treatment
Homeopathic Treatment of Conjunctivitis
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Conjunctivitis:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicine:
Argentum nitricum:
- Especially, Purulent, protargol more useful.
Belladonna:
- Bright redness, photophobia.
Boric acid:
- Specifically, for Saturated solution, with cocaine two to three grains to the ounce.
Rhus tox:
- it is indicated especially in much swelling of lids.
Hepar sulfurious:
- Purulent conjunctivitis, with marked chemosis, profuse discharge, great sensitiveness to touch and air. Moreover, Eyes and lids red also inflamed. Pains in the eyes as if pulled back into the head. Vision obscured by reading; field reduced one-half. Worse – from dry, cold winds; cool air; slightest draught, touch. On the other hand, Better – in damp weather; from wrapping head up; warmth; after eating.
Mercurius Corrosivus:
- Excessive photophobia and acrid lachrymation. Little tendency to pus formation. Pain severe at night; burning, shooting, tearing. Lids oedematous, red, excoriated. Especially, Soreness of the eyes.
Apis mellifica:
- For acute conditions, lids swollen, red, oedematous, everted, inflamed, burn also sting. Conjunctiva bright red, puffy. Lachrymation hot. Photophobia. Sudden piercing pains. Suppurative inflammation of eyes. Keratitis with intense chemosis of ocular conjunctiva.
Euphrasia:
- Catarrhal conjunctivitis.; discharge acrid, thick, also excoriating. Eyes water all the time. Additionally, Burning and swelling of the lids. Lastly, Frequent inclination to blink. Pressure in eyes.
Diet & Regimen
Diet & Regimen of Conjunctivitis
- Apply a compress to the eyes
- Try eye drops
- Stop wearing contact lenses
- Refuse exposure to light
- Prevent rubbing of the eye
- Clean the eyes using sterile water and cotton swabs, from inner canthus to outer canthus
- Use of dark sunglasses is advised, in presence of photophobia [2]
Do’s and Don'ts
The Do’s & Don’ts :
Do’s:
- Practice good hygiene: Wash hands frequently with soap and water, especially before and after touching the eyes.
- Avoid touching or rubbing eyes: This can worsen the irritation and spread the infection.
- Clean eyes regularly: Use clean cotton balls and warm water or saline solution to gently wipe away discharge.
- Apply warm compresses: Soak a clean cloth in warm water and apply it to closed eyes for 5-10 minutes several times a day. This can help soothe the inflammation and loosen any crusting.
- Use lubricating eye drops: Artificial tears can help relieve dryness and irritation.
- Follow treatment instructions: If prescribed antibiotics or other medications, use them as directed.
- See an ophthalmologist: If symptoms persist or worsen, seek professional evaluation and treatment.
- Stay home if contagious: To prevent spreading the infection, avoid close contact with others and stay home from work or school if possible.
Don’ts:
- Don’t share personal items: Avoid sharing towels, washcloths, cosmetics, or eye drops with others.
- Don’t wear contact lenses: If you wear contact lenses, discontinue use until the infection clears.
- Don’t use expired or contaminated eye drops: Discard any eye drops that are past their expiration date or appear cloudy or discolored.
- Don’t self-medicate: Avoid using over-the-counter medications or remedies without consulting an ophthalmologist.
- Don’t ignore symptoms: If you experience vision changes, severe pain, or other concerning symptoms, seek immediate medical attention.[11]
Terminology
Terminology
Medical Terminology:
- Conjunctiva: The transparent membrane lining the eyelid and covering the white part of the eyeball.
- Inflammation: A response to injury or infection, characterized by redness, swelling, and pain.
- Infection: The invasion and multiplication of microorganisms (like bacteria or viruses) in body tissues.
- Pink eye: A common synonym for conjunctivitis, referring to the redness of the eye.
- Madras eye: An archaic term for conjunctivitis.
- Acute catarrhal conjunctivitis: Specifically refers to viral conjunctivitis.
- Egyptian ophthalmia: An archaic term for a specific type of bacterial conjunctivitis.
- Enteroviral conjunctivitis: Conjunctivitis caused by enteroviruses, often leading to acute hemorrhagic conjunctivitis.
- Adenovirus conjunctivitis: Conjunctivitis caused by adenoviruses.
- Prevalence: The proportion of a population found to have a condition at a specific time.
- Attack rate: The proportion of individuals in a population who develop a disease during an outbreak.
- Pathogenesis: The biological mechanism that leads to a disease.
- Pathophysiology: The functional changes associated with or resulting from disease or injury.
- Epiphora: Excessive tearing or watering of the eyes.
- Hyperemia: Increased blood flow to a part of the body, causing redness.
- Chemosis: Swelling of the conjunctiva.
- Lymphadenopathy: Swelling of lymph nodes.
- Mucopurulent discharge: Discharge from the eyes containing mucus and pus.
- Photophobia: Sensitivity to light.
- Periorbital cellulitis: Infection of the tissues around the eye.
Homeopathic Terminology:
- Homeopathy: A system of alternative medicine based on the principle of "like cures like."
- Remedies: Substances used in homeopathy to treat specific symptoms or conditions.
- Potency: The strength or dilution of a homeopathic remedy.
- Repetition: The frequency with which a homeopathic remedy is taken.
- Therapeutic affinity: The tendency of a homeopathic remedy to act on specific organs or systems.
- Miasmatic tendency: A predisposition or susceptibility to certain types of diseases in homeopathy.
- Constitutional indications: The overall health and temperament of the patient, considered in homeopathic prescribing.
References
Reference
- The concise textbook of surgery by S.das.
- https://www.mtatva.com/en/disease/conjunctivitis-treatment-diet-and-home-remedies/
- Homoeopathic Body-System Prescribing – A Practical Workbook of Sector Remedies
- https://www.wikidoc.org/index.php/Conjunctivitis_physical_examination
- Preventing Pink Eye (Conjunctivitis) | CDC
- J. Baba, T. Jacob John, Chapter 9: Epidemiology of Acute Enteroviral Conjunctivitis in India, 1987.
- Financial Express, July 2024.
- Frontiers in Public Health, 2022.
- International Journal of Contemporary Medical Research (IJCMR), August 2018.
- Vaughan & Asbury’s General Ophthalmology,19th Edition
- Kanski’s Clinical Ophthalmology,9th Edition
Also Search As
Also Search As
1. Search Engines:
- Use keywords related to conjunctivitis and its synonyms like "pink eye," "eye infection," or "conjunctival inflammation."
- Include additional terms like "homeopathic treatment," "causes," "symptoms," or "prevention" to narrow down the search results.
- Use quotation marks around specific phrases like "homeopathic remedies for conjunctivitis" to get more relevant results.
2. Online Health Platforms and Websites:
- Look for articles on reputable health websites and platforms like WebMD, Mayo Clinic, or specialized homeopathic websites.
- Search their article databases or blogs using relevant keywords.
3. Social Media:
- Follow homeopathic organizations or practitioners on social media platforms like Facebook, Twitter, or Instagram. They often share articles and information about various health conditions, including conjunctivitis.
- Use hashtags like #conjunctivitis, #pinkeye, or #homeopathy to find relevant posts and discussions.
4. Homeopathic Forums and Communities:
- Participate in online forums and communities dedicated to homeopathy.
- Ask questions or search for discussions about conjunctivitis and its treatment options.
5. Direct Website Search:
- If you know the name of the website or organization that published the article, you can directly search for it on their website using their search bar or browsing through their articles section.
The article on Conjunctivitis can be searched in the following ways:
On the Website Itself:
- Search Bar: Look for a search bar on the website and type in keywords like "conjunctivitis," "pink eye," or "eye infection."
- Browse by Category: If the website has categories or sections, look for one related to eye health or homeopathic remedies.
On External Search Engines:
- Keywords: Use search engines like Google, Bing, or DuckDuckGo and enter keywords like "conjunctivitis homeopathic treatment," "conjunctivitis symptoms," or "conjunctivitis prevention."
- Specific Website: If you know the website’s name, include it in your search query, like "conjunctivitis [website name]."
- Advanced Search: Use advanced search options to filter results by date, language, or region.
Other Methods:
- Social Media: Look for the website’s social media pages (Facebook, Twitter, etc.) and check if they have shared the article.
- Homeopathic Forums: Search on homeopathic forums or online communities for discussions about conjunctivitis and the article.
Tips:
- Synonyms: Use different words or phrases that mean the same thing, like "pink eye" instead of "conjunctivitis."
- Quotation Marks: Use quotation marks around specific phrases to get more precise results.
- Boolean Operators: Use words like "AND," "OR," and "NOT" to combine keywords and narrow down your search.
Frequently Asked Questions (FAQ)
What is Conjunctivitis?
Conjunctivitis is an inflammation or infection of the transparent membrane (in other words, conjunctiva) that lines the eyelid and covers the white part of the eyeball.
What are the symptoms of Conjunctivitis?
Symptoms
- Pain
- Redness in one or both eyes
- Itching in one or both eyes
- A discharge in one or both eyes
- Tearing
- Photophobia
- Dropping of upper eyelid
- Periorbital cellulitis
- Fever
- Sore throat
- Runny nose
- A gritty feeling in one or both eyes
How is conjunctivitis diagnosed?
Diagnosis
Diagnosis usually involves a physical examination of the eyes and a review of the patient’s medical history. In severe cases, a sample of eye secretions may be taken for laboratory analysis.
What are the causes of Conjunctivitis?
- Viruses
- Bacteria
- Allergies
- A chemical splash in the eye
- A foreign object in the eye
- In new-born, a blocked tear duct
What are the treatment options for conjunctivitis?
Treatment
Treatment depends on the cause. Bacterial conjunctivitis may be treated with antibiotic eye drops or ointments. Viral conjunctivitis usually resolves on its own, but antiviral medication may be prescribed in some cases. Allergic conjunctivitis is often treated with antihistamines or anti-inflammatory eye drops.
Can conjunctivitis be prevented?
Prevention
Yes, practicing good hygiene, avoiding contact with infected individuals, and not sharing personal items can help prevent the spread of conjunctivitis.
When should I consult a homeopathic doctor for conjunctivitis?
If symptoms are severe, persistent, recurrent, or do not improve with self-care measures, it is recommended to consult a qualified homeopathic doctor for proper evaluation and treatment.
Can homeopathic remedies prevent conjunctivitis?
Homoeopathy For Conjuctivitis
While homeopathy focuses on treating existing conditions, certain remedies may help boost immunity and reduce susceptibility to infections, including conjunctivitis.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Conjunctivitis?
Homoeopathic medicines for Comjunctivitis
- Argentum nitricum
- Belladonna
- Boric acid
- Rhus tox
- Hepar sulph
- Mercurius Cor
- Apis mell
- Euphrasia
