Chronic obstructive pulmonary disease
Definition
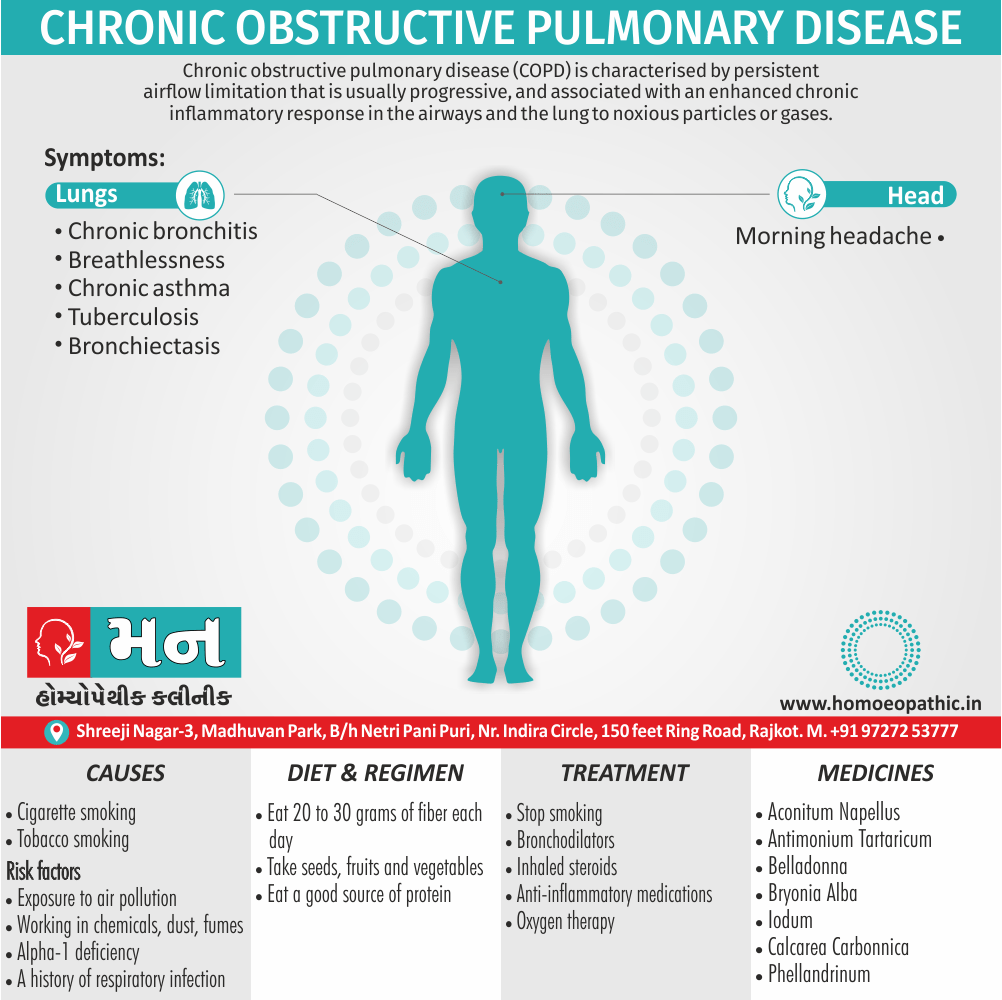
Chronic obstructive pulmonary disease (COPD) is a preventable and treatable disease characterized by persistent airflow limitation that is usually progressive, and associated with an enhanced chronic inflammatory response in the airways and the lung to noxious particles or gases. [1]
Chronic obstructive pulmonary disease (COPD) is a lung disease that obstructs the airflow from the lungs. This makes it difficult to breathe. Symptoms include shortness of breath, coughing, and wheezing. COPD can be caused by smoking, air pollution, and occupational exposures. There is no cure for COPD, but there are treatments that can help manage the symptoms and slow the progression of the disease.
Chronic obstructive pulmonary disease (COPD) doesn’t have many true synonyms in the medical field, as it’s a specific lung condition. However, here are some related terms you might encounter:
- Chronic obstructive airway disease (COAD): This term emphasizes the airway obstruction aspect of COPD.
- Emphysema and chronic bronchitis: These are the two main conditions that contribute to COPD.
- Emphysema: This is a condition where the air sacs in the lungs are damaged, leading to shortness of breath.
- Chronic bronchitis: This is a long-term inflammation of the lining of the bronchial tubes, causing coughing and mucus production.
Important Considerations:
- In a medical setting, "chronic obstructive pulmonary disease (COPD)" is the most precise term.
- "Chronic obstructive airway disease (COAD)" or mentioning "emphysema and chronic bronchitis" might be used in specific contexts, but prioritize clarity for a general audience.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Chronic obstructive pulmonary disease
- Exacerbations and comorbidities contribute to the overall severity in individual patients.
- Extra-pulmonary effects include weight loss and skeletal muscle dysfunction commonly associated comorbid conditions include cardiovascular disease, cerebrovascular disease, the metabolic syndrome, osteoporosis, depression and lung cancer. [1]
- The prevalence of COPD is directly related to the prevalence of tobacco smoking and, in low- and middle-income countries, the use of biomass fuels.
- Current estimates suggest that 80 million people worldwide suffer from moderate to severe disease. [1]
Epidemiology
Epidemiology
Lancet Respiratory Medicine (2018):
Estimated 55.3 million COPD cases in India in 2016. Crude prevalence high in Himachal Pradesh, Uttarakhand, Haryana, and Jammu & Kashmir. [9]
Annals of the National Academy of Medical Sciences (India) (2022):
In a study conducted in Delhi, the overall prevalence rate of COPD was 9.8/1,000 population, and among the population over 30 years of age, the prevalence rate was 21.2/1,000. [10]
Global Burden of Disease Study (2017):
Chronic Respiratory Diseases, which includes COPD, accounted for 10.9% of total deaths and 6.4% of total Disability Adjusted Life Years (DALY) in India. [11]
World Health Organization (WHO):
COPD is the third leading cause of death worldwide, and while the majority of COPD deaths occur in low- and middle-income countries, India faces a significant burden. [12]
It’s important to note that these are just a few examples, and the epidemiology of COPD in India may vary depending on the specific population studied and the methodology used.
Causes
Causes
- Cigarette smoking represents the most significant risk factor, and the risk of developing COPD relates to both the amount and the duration of smoking.
- It is unusual to develop COPD with less than 10 pack years and not all smokers develop the condition, suggesting that individual susceptibility factors are important. [1]
Types
Types
The two most common conditions of COPD are chronic bronchitis and emphysema. Some physicians agree that asthma should be classified as a chronic obstructive pulmonary disease, while others do not.
1.Chronic bronchitis
Chronic bronchitis is a long-term inflammation of the bronchi (breathing passages in the lungs), which results in increased production of mucus, as well as other changes.
- These changes may result in breathing problems, frequent infections, cough, and disability.
2. Pulmonary emphysema
Emphysema is a chronic lung condition in which alveoli (air sacs in the lungs) may be:
- Destroyed
- Narrowed
- Collapsed
- Stretched
- Over-inflated
This can cause a decrease in respiratory function and breathlessness. Damage to the air sacs is irreversible and results in permanent "holes" in the lung tissue.
3. Asthma
Asthma is a chronic, inflammatory lung disease involving recurrent breathing problems. The characteristics of asthma include the following:
- The lining of the airways become swollen and inflamed.
- The muscles that surround the airways tighten.
- The production of mucus is increased, leading to mucus plugs. (5)
Risk Factors
Risk factors
- Exposure to air pollution
- Breathing second hand smoke
- Working with chemicals, dust and fumes
- A genetic condition called Alpha-1 deficiency
- A history of childhood respiratory infection [4]
Pathogenesis
Pathogenesis
- Chronic Inflammation: COPD is characterized by chronic inflammation of the airways and lung parenchyma. Inhaled noxious particles and gases, primarily cigarette smoke, trigger an abnormal inflammatory response involving neutrophils, macrophages, and lymphocytes.
- Protease-Antiprotease Imbalance: An imbalance between proteases (enzymes that break down proteins) and antiproteases (enzymes that inhibit proteases) is thought to play a crucial role in the development of emphysema, a component of COPD. Increased protease activity, particularly from neutrophils, can lead to the destruction of alveolar walls and loss of lung elasticity.
- Oxidative Stress: Oxidative stress, caused by an imbalance between reactive oxygen species (ROS) and antioxidants, contributes to lung damage in COPD. Inhaled toxins and inflammatory cells generate ROS, which can damage lung tissue and impair its repair mechanisms.
- Small Airway Remodeling: Chronic inflammation and repeated injury lead to structural changes in the small airways, including fibrosis, increased mucus production, and smooth muscle hypertrophy. These changes contribute to airflow obstruction and impaired gas exchange.
- Systemic Effects: COPD is not just a lung disease. It can have systemic effects on other organs and systems, leading to comorbidities such as cardiovascular disease, skeletal muscle dysfunction, and metabolic abnormalities. [13]
Pathophysiology
Pathophysiology of Chronic obstructive pulmonary disease
- COPD has both pulmonary and systemic components The presence of airflow limitation combined with premature airway closure, leads to gas trapping and hyperinflation, reducing pulmonary and chest wall compliance.
- Pulmonary hyperinflation also flattens the diaphragmatic muscles and leads to an increasingly horizontal alignment of the intercostals muscles, placing the respiratory muscles at a mechanical.
- The work of breathing is therefore markedly increased, first on exercise, when the time for expiration is further shortened, but then, as the disease advances, at rest Emphysema may be classified by the pattern of the enlarged airspaces as centri acinar, pan acinar or Para septal.
- Bullae form in some individuals. This results in impaired gas exchange and respiratory Failure.[1]
Clinical Features
Clinical Features
Key Clinical Features from Harrison’s:
Dyspnea (Shortness of Breath):
- The most common and disabling symptom of COPD.
- Progressive and persistent, worsening with exertion.
- May be accompanied by chest tightness.
Chronic Cough:
- Persistent cough, often worse in the morning.
- May produce sputum (mucus) that can be clear, white, yellow, or green.
Sputum Production:
- Increased production of mucus, especially during exacerbations.
- Can be a sign of airway inflammation and infection.
Wheezing:
- A high-pitched whistling sound when breathing, particularly during exhalation.
- Indicates airflow obstruction in the airways.
Chest Tightness:
- A feeling of pressure or discomfort in the chest.
- May be associated with dyspnea and wheezing.
Fatigue and Exercise Intolerance:
- Reduced ability to perform physical activities due to shortness of breath and fatigue.
Recurrent Respiratory Infections:
- Increased susceptibility to respiratory infections like bronchitis and pneumonia.
- Exacerbations often triggered by infections.
Weight Loss (in Later Stages):
- Unintentional weight loss due to increased energy expenditure for breathing and reduced appetite.
Peripheral Edema (in Severe Cases):
- Swelling in the ankles, feet, or legs due to right-sided heart failure (cor pulmonale).
Additional Clinical Features:
- Barrel Chest: An increased anteroposterior diameter of the chest due to air trapping in the lungs.
- Decreased Breath Sounds: Reduced intensity of breath sounds on auscultation.
- Prolonged Expiratory Phase: Longer time taken to exhale compared to inhale.
- Cyanosis (in Severe Cases): A bluish discoloration of the skin and mucous membranes due to low oxygen levels in the blood. [14]
Sign & Symptoms
Sign & Symptoms of Chronic obstructive pulmonary disease
- COPD should be suspected in any patient over the age of 40 years who presents with symptoms of chronic bronchitis and/or breathlessness.
- Cough and associated sputum production ‘smoker’s cough’.
- Breathlessness
- Physical signs are non-specific, correlate poorly with lung function, and are seldom obvious until the disease is advanced. Breath sounds are typically quiet.
- Crackles may accompany infection but, if persistent, raise the possibility of bronchiectasis.
- Tuberculosis [1]
Clinical Examination
Clinical examination of Chronic obstructive pulmonary disease
Appearance of the Patient
- Cyanosis
- Tachypnea
- Respiratory distress indicated by use of accessory respiratory muscles. Hoover sign presenting as paradoxical indrawing of lower intercostal spaces is evident (known as the Hoover sign)
- Elevated jugular venous pulse (JVP)
- Peripheral edema can be observed.
Lungs
Inspection
- Hyperinflation (barrel chest)
Percussion
- Hyper resonance
Auscultation
- Prolonged expiration; wheezing
- Diffusely decreased breath sound
- Additional sounds – coarse crackles with inspiration. (6)
Diagnosis
Diagnosis of Chronic obstructive pulmonary disease
- The best test for COPD is a lung function test called spirometry. This involves blowing out as hard as possible into a small machine that tests lung capacity.
- Using a stethoscope to listen to the lungs can also be helpful. Pictures of the lungs (such as x-rays and CT scans) can be helpful
- Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood. [2]
Differential Diagnosis
Differential diagnosis of Chronic obstructive pulmonary disease
- Asthma
- Congestive heart failure
- Bronchiectasis
- Tuberculosis
- Obliterative bronchiolitis (7)
Complications
Complications
Acute Exacerbations:
- Episodes of worsening respiratory symptoms (increased dyspnea, cough, sputum production).
- Often triggered by respiratory infections or environmental pollutants.
- Can lead to hospitalization and increased mortality risk.
Respiratory Failure:
- Inability of the lungs to maintain adequate gas exchange (oxygenation and carbon dioxide removal).
- May require supplemental oxygen therapy or mechanical ventilation.
Pulmonary Hypertension:
- Elevated blood pressure in the pulmonary arteries.
- Can lead to right-sided heart failure (cor pulmonale).
Cor Pulmonale (Right-Sided Heart Failure):
- Enlargement and weakening of the right ventricle due to increased workload from pulmonary hypertension.
- Symptoms include peripheral edema, jugular venous distention, and hepatic congestion.
Pneumothorax:
- Air leakage into the pleural space, causing lung collapse.
- More common in patients with emphysema.
- May require chest tube insertion or surgery.
Depression and Anxiety:
- COPD can significantly impact quality of life, leading to psychological distress.
- Depression and anxiety are common comorbidities.
Nutritional Depletion and Weight Loss:
- Increased energy expenditure for breathing and decreased appetite can lead to malnutrition and weight loss.
- Contributes to muscle weakness and decreased exercise tolerance.
Osteoporosis:
- Chronic inflammation and corticosteroid use (a common treatment for COPD) can increase the risk of osteoporosis.
- Leads to increased fracture risk.
Lung Cancer:
- COPD is a significant risk factor for lung cancer.
- Screening for lung cancer is recommended for individuals with a history of smoking and COPD.
Additional Complications:
- Infections: Increased susceptibility to respiratory infections (pneumonia, bronchitis).
- Polycythemia: Increased red blood cell mass due to chronic hypoxemia.
- Sleep Apnea: Obstructive sleep apnea is more common in people with COPD. [15]
Investigations
Investigation of Chronic obstructive pulmonary disease
- A chest X- ray is essential to identify alternative diagnoses, such as cardiac failure, other complications of smoking such as lung cancer, and the presence of bullae.
- A blood count is useful to exclude anaemia or polycythemia, and in younger patients with predominantly basal emphysema, α1-antiproteinase should be assayed.
- Measurement of lung volumes provides an assessment of hyperinflation.
- Emphysema is suggested by a low gas transfer value (p. 653). Exercise tests provide an objective assessment of exercise tolerance and a baseline for judging response to bronchodilator therapy or rehabilitation programmed; they may also be valuable when assessing prognosis.
- Pulse oximetry of less than 93% may indicate the need for referral for a domiciliary oxygen assessment.
- The assessment of health status provides valuable clinical information.
- HRCT is likely to play an increasing role in the assessment of COPD, as it allows the detection, characterization and quantification of emphysema and is more sensitive than a chest X-ray for detecting bullae. [1]
Treatment
Treatment of Chronic obstructive pulmonary disease
- There is no cure for COPD. However, there are many things you can do to relieve symptoms and keep the disease from getting worse.
- Persons with COPD must stop smoking. This is the best way to slow down the lung damage.
- Medications used to treat COPD include:
- Inhalers (bronchodilators) to open the airways, such as ipratropium (Atrovent), tiotropium (Spiriva), salmeterol (Serevent), formoterol (Foradil), or
- Inhaled steroids to reduce lung inflammation.
- Anti-inflammatory medications such as Montelukast(Singulair) and roflimulast are sometimes used.
- In severe cases or during flare-ups, you may need to receive:
- Steroids by mouth or through a vein (intravenously)
- Bronchodilators through a nebulizer
- Oxygen therapy
- Assistance during breathing from a machine (through a mask, BiPAP, or endotracheal tube)
- Antibiotics are prescribed during symptom flare-ups, because infections can make COPD
- You may need oxygen therapy at home if you have a low level of oxygen in your blood.
- Walk to build up strength.
- Use pursed lip breathing when breathing out (to empty your lungs before the next breath)
- Things you can do to make it easier for yourself around the home include:
- Avoiding very cold air
- Making sure no one smokes in your home
- Reducing air pollution by getting rid of fireplace smoke and other irritants
10.Surgery may be used, but only a few patients benefit from these surgical treatments:
- Surgery to remove parts of the diseased lung can help other areas (not as diseased) work better in some patients with emphysema
- Lung transplant for severe cases [2]
Prevention
Prevention of Chronic obstructive pulmonary disease
- Don’t rub your eyes, as this can transmit germs to your nasal passages via the tear ducts.
- Quitting smoking and avoiding secondhand smoke (the smoke from a burning cigarette or cigar and the smoke exhaled by a smoker) are important steps you can take to protect your lungs from infection.
- Follow your doctor’s medication guidelines.
- Get enough sleep and rest.
- Manage your stress.
- Talk to your doctor or healthcare provider about getting a flu shot every year and get the pneumonia vaccine if you haven’t had one.
- Be careful to avoid infection when traveling. In areas where the water might be unsafe, drink bottled water or other beverages (order beverages without ice). Swim only in chlorinated pools.(8)
Homeopathic Treatment
Homeopathic Treatment of Chronic obstructive pulmonary disease
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Chronic obstructive pulmonary disease
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
Aconitum Napellus:
- The first remedy that is often indicated at the onset of the infection. It is effective only within the first twenty-four hours.
- Useful when there is a short, dry cough, a temperature and an irritation of the throat, chest and trachea.
- There is a chilly restlessness, anxiety and a full, bounding pulse, with general weakness.
Antimonium Tartaricum:
- Useful when there is a accumulation of considerable loose, rattling, moist mucus in the chest.
- For children breathing and a loose cough, but little phlegm is expectorated.
- There may be vomiting and labored breathing. Pronounced physical and mental exhaustion.
Belladona:
- A high temperature, dry cough, a pounding, pulsating headache and a flushed face with a dry, hot skin.
- The cough is worse at night and when lying down.
Bryonia Alba:
- A painful, violent, dry, stitching cough with a headache and pain in the chest wall.
- Worse with coughing and better when supporting the area with both hands.
- The expectoration is yellow and often blood streaked. The cough is worse after meals.
- Patient drinks large quantities of fluids at long intervals.
Iodum:
- Difficult expansion of chest, blood-streaked sputum; internal dry heat, external coldness.
- Inspiration difficult. Croupy cough with difficult respiration; wheezy.
- Cold extends downwards from head to throat and bronchi. Great weakness about chest.
- Palpitation from the least exertion. Iodum cough.
Calcarea carbonica:
- Extreme Dyspnoea. Suffocating spells, tightness, burning and soreness in chest.
- Chest very sensitive to touch, percussion or pressure. Longing for fresh air.
- Bloody expectoration.
Phellandrinum:
- Respiratory remedy. Good remedy for offensive expectoration and cough phthisis.
- Tuberculosis, affecting generally the middle lobes. Everything tastes sweet.
- Dyspnoea and continuous cough early in morning.
- Cough, with profuse and fetid expectoration; compels him to sit up. Hoarseness.[3]
Diet & Regimen
Diet & Regimen of Chronic obstructive pulmonary disease
- Eat 20 to 30 grams of fiber each day, from items such as bread, pasta, nuts, seeds, fruits and vegetables.
- Eat a good source of proteinase least twice a day to help maintain strong respiratory muscles.
- Good choices include milk, eggs, cheese, meat, fish, poultry, nuts and dried beans or peas. [2]
- Eat a healthy diet with fish, poultry, or lean meat, as well as fruits and vegetables.
Do’s and Don'ts
Do’s & Don’ts
Chronic obstructive pulmonary disease do’s and don’ts
Do’s:
- Do quit smoking: This is the single most important thing you can do to slow down the progression of COPD and improve your quality of life.
- Do follow your doctor’s treatment plan: Take your medications as prescribed, attend regular checkups, and participate in pulmonary rehabilitation if recommended.
- Do get vaccinated: Get an annual flu shot and pneumococcal vaccine to protect yourself from respiratory infections that can worsen COPD.
- Do stay active: Regular exercise can improve your lung function and overall well-being. Talk to your doctor about an exercise program that’s right for you.
- Do eat a healthy diet: A balanced diet rich in fruits, vegetables, and whole grains can help you maintain your strength and energy levels.
- Do manage stress: Stress can worsen COPD symptoms. Find healthy ways to manage stress, such as relaxation techniques or meditation.
- Do get enough sleep: Aim for 7-8 hours of sleep each night to help your body repair and recharge.
- Do join a support group: Connecting with others who have COPD can provide emotional support and helpful tips for managing the condition.
Don’ts:
- Don’t smoke: Avoid smoking and exposure to secondhand smoke.
- Don’t ignore your symptoms: If you experience any worsening of your symptoms, contact your doctor right away.
- Don’t skip your medications: Take your medications as prescribed, even if you’re feeling better.
- Don’t overexert yourself: Pace yourself during physical activity and rest when you need to.
- Don’t expose yourself to respiratory irritants: Avoid air pollution, dust, fumes, and other irritants that can trigger COPD symptoms.
- Don’t isolate yourself: Stay connected with friends and family and seek support when you need it.
Remember, COPD is a chronic condition that requires ongoing management. By following these do’s and don’ts, you can improve your quality of life and slow down the progression of the disease.
Terminology
Terminology
The article utilizes several medical terms specific to COPD and its homeopathic management:
- Chronic Obstructive Pulmonary Disease (COPD): A progressive lung disease characterized by airflow limitation, making it difficult to breathe.
- Emphysema: A component of COPD where the air sacs (alveoli) in the lungs are damaged, leading to shortness of breath.
- Chronic Bronchitis: A persistent inflammation of the bronchial tubes, causing cough and mucus production. Often coexists with emphysema in COPD.
- Exacerbations: Flare-ups or episodes of worsening COPD symptoms, often triggered by infections or environmental pollutants.
- Comorbidities: Additional medical conditions that occur alongside COPD, such as cardiovascular disease or osteoporosis.
- Pathogenesis: The biological mechanisms that lead to the development of a disease. In COPD, this includes inflammation, protease imbalance, oxidative stress, and airway remodeling.
- Pathophysiology: The functional changes in the body that result from a disease. In COPD, this includes gas trapping, hyperinflation, and reduced lung compliance.
- Dyspnea: Shortness of breath, the most common and disabling symptom of COPD.
- Wheezing: A high-pitched whistling sound heard during breathing, indicating airflow obstruction.
- Miasmatic Tendency: A homeopathic concept referring to an individual’s predisposition to certain types of illnesses, often used to guide treatment selection.
- Homeopathic Remedies: Substances used in homeopathy to treat disease based on the principle of "like cures like." Examples include Aconitum Napellus, Antimonium Tartaricum, and Bryonia Alba.
- Potency: A measure of the dilution of a homeopathic remedy. Higher potencies are thought to have a deeper-acting effect.
- Repetition: The frequency with which a homeopathic remedy is administered.
References
References
- Davidsons Principles and Practice of Medicine
- Chronic obstructive pulmonary disease – PubMed Health
- Homoeopathic Therapeutics By Lilienthal
- https://www.lung.org/lung-health-diseases/lung-disease-lookup/copd/what-causes-copd
- https://stanfordhealthcare.org/medical-conditions/chest-lungs-and-airways/chronic-obstructive-pulmonary-disease/types.html
- https://www.wikidoc.org/index.php/Chronic_obstructive_pulmonary_disease_physical_examination
- https://my.clevelandclinic.org/health/diseases/8709-chronic-obstructive-pulmonary-disease-copd#prevention
- Lancet Respiratory Medicine (2018)
- Annals of the National Academy of Medical Sciences (India) (2022)
- Global Burden of Disease Study (2017)
- World Health Organization (WHO)
- Fishman’s Pulmonary Diseases and Disorders (5th Edition) by, Michael Grippi, Robert Mason, John Murray, Jay Nadel (2015)
- Harrison’s Principles of Internal Medicine (20th Edition) by, Dennis Kasper, Anthony Fauci, Stephen Hauser, Dan Longo, J. Larry Jameson, Joseph Loscalzo (2018) published by McGraw Hill Education
- Goldman-Cecil Medicine (26th Edition) by, Lee Goldman, Andrew Schafern (2020) Published by, Elsevier.
Also Search As
Also Search As
People can search for this article using various keywords and phrases related to its content:
- Chronic Obstructive Airway Disease (COAD)
- Chronic Bronchitis
- Emphysema
- Homeopathy for COPD
- Homeopathic Remedies for COPD
- Natural Treatment for COPD
- Alternative Treatment for COPD
- COPD Symptoms and Treatment
- COPD Prevention and Management
- Breathing difficulties
- Wheezing and Coughing
- Smoking and Lung Disease
- Air Pollution and Lung Health
Broad search terms:
- Chronic Obstructive Pulmonary Disease (COPD)
- COPD homeopathic treatment
- Homeopathy for COPD
- Lung disease treatment
- Emphysema and chronic bronchitis
- Breathing difficulties
- Wheezing and coughing
Specific search terms:
- COPD symptoms and causes
- COPD complications
- COPD Diet and Regimen
- COPD do’s and don’ts
- Homeopathic remedies for lung diseases
- Natural remedies for COPD
Additional search terms based on the article’s content:
- Aconitum Napellus for COPD
- Antimonium Tartaricum for COPD
- Bryonia Alba for COPD
- Iodum for COPD
Searches can also be conducted using a combination of keywords:
- COPD homeopathic medicine
- Homeopathic treatment for bronchitis
- Natural remedies for emphysema
- Alternative medicine for COPD
- Lung disease homeopathic remedies
Additionally, users can search for the specific titles of referenced books or publications mentioned in the article for further information.
There are several ways to search for this article, depending on the platform or search engine you are using:
Using search engines:
- Keyword search: Type relevant keywords or phrases into the search bar of your preferred search engine (e.g., Google, Bing, DuckDuckGo). You can use combinations of terms like "chronic obstructive pulmonary disease," "COPD," "homeopathic treatment," "natural remedies," "emphysema," "chronic bronchitis," etc.
- Specific terms: If you remember specific phrases from the article, try searching for those exact phrases. This could include the names of homeopathic remedies mentioned in the article or specific sections of the article (e.g., "COPD diet and regimen").
Within websites or databases:
- Site-specific search: If you know the website where this article is published, use their internal search bar to look for it.
- Homeopathic resource websites: Search on websites dedicated to homeopathic information and remedies, as they may have indexed this article in their database.
Using academic databases:
- If you are looking for scholarly articles on homeopathy and COPD, search in academic databases like PubMed, Google Scholar, or ScienceDirect. These databases often index articles from journals and other publications.
Using social media:
- If the article was shared on social media platforms like Twitter or Facebook, you might be able to find it by searching for relevant hashtags or the author’s name.
Asking for help:
- If you are struggling to find the article, consider asking for help from a librarian or a homeopathic practitioner. They might have access to resources that can help you locate the article.
Remember to use a variety of search terms and strategies to increase your chances of finding the article you are looking for.
Frequently Asked Questions (FAQ)
What is Chronic obstructive pulmonary disease?
Chronic obstructive pulmonary disease (COPD) is a preventable and treatable disease characterized by persistent airflow limitation that is usually progressive, and associated with an enhanced chronic inflammatory response in the airways and the lung to noxious particles or gases.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Chronic obstructive pulmonary disease?
Homoeopathic medicine for Chronic Obstructive pulmonary disease
- Aconitum Napellus
- Antimonium Tartaricum
- Belladona
- Bryonia Alba
- Iodum
- Calcarea carbonica
- Phellandrinum
What are the causes of Chronic obstructive pulmonary disease?
- Cigarette smoking
- Exposure to air pollution
- Breathing second hand smoke
- Working with chemicals, dust and fumes
- A genetic condition called Alpha-1 deficiency
What are the symptoms of Chronic obstructive pulmonary disease?
- Chronic bronchitis and/or breathlessness
- Cough and associated sputum production ‘smoker’s cough’
- Breath sounds are typically quiet
Can homeopathy help with COPD?
Homeopathy offers a holistic approach to COPD management, focusing on the individual and their unique symptoms. Some homeopathic remedies like Aconitum Napellus, Antimonium Tartaricum, and Bryonia Alba may help alleviate symptoms, but it’s crucial to consult a qualified homeopathic practitioner for personalized treatment.
What are the treatment options for COPD?
Treatment options include quitting smoking, medications (bronchodilators, inhaled steroids, etc.), pulmonary rehabilitation, oxygen therapy, and in severe cases, surgery or lung transplant.
What lifestyle changes can help manage COPD?
Making lifestyle changes like quitting smoking, eating a healthy diet, exercising regularly, and managing stress can significantly improve COPD symptoms and slow disease progression.
Can COPD be prevented?
Prevention of COPD
While some risk factors are unavoidable, the most effective way to prevent COPD is to never smoke or quit if you are a smoker. Avoiding exposure to secondhand smoke, air pollution, and occupational hazards can also help reduce the risk of developing COPD.
Which homeopathic remedies are commonly used for COPD?
Some commonly used homeopathic remedies for COPD include Aconitum Napellus, Antimonium Tartaricum, Bryonia Alba, Iodum, Calcarea Carbonica, and Phellandrinum. The choice of remedy depends on the individual’s specific symptoms and constitution.
Can homeopathy be used alongside conventional COPD treatments?
Yes, homeopathy can be used as a complementary therapy alongside conventional treatments. It is essential to discuss with both your conventional doctor and homeopathic practitioner to ensure a safe and integrated approach.
