Retained Placenta
Definition
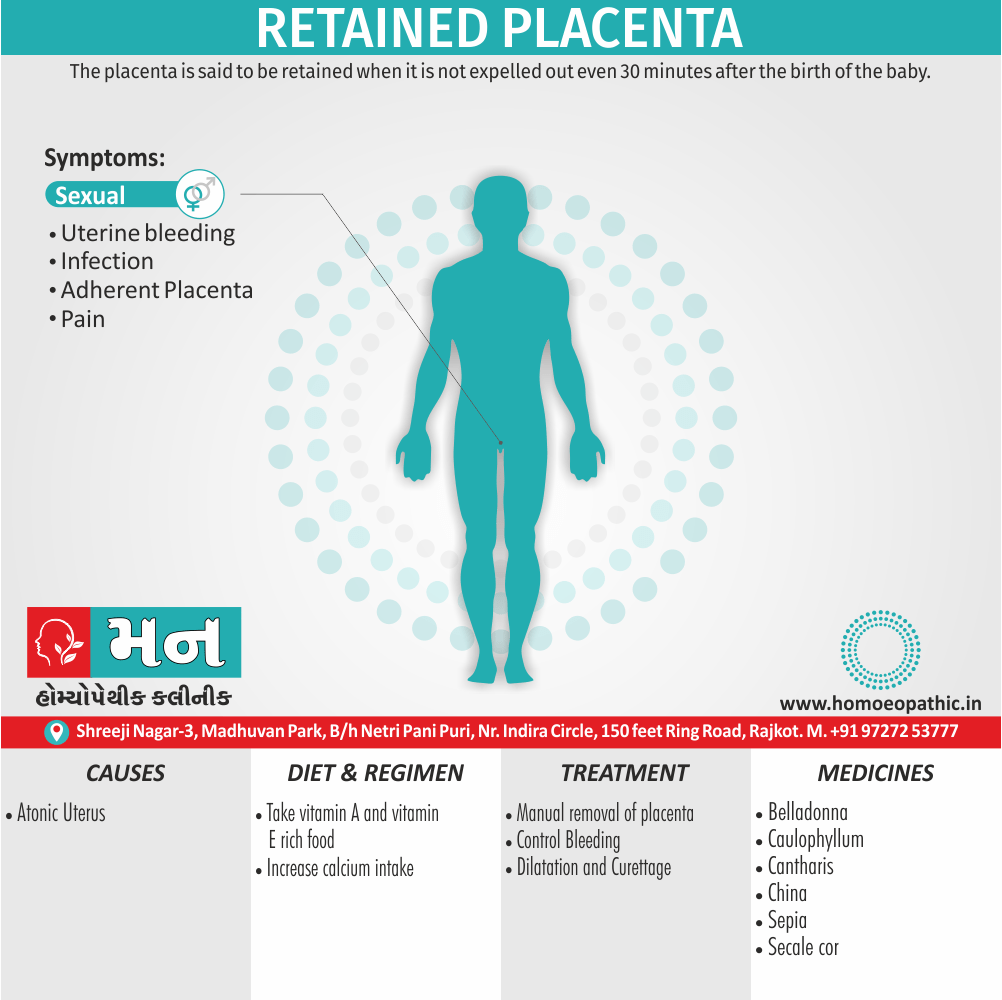
Retained placenta is a complication that occurs after childbirth when all or part of the placenta remains in the uterus instead of being expelled naturally. Typically, the placenta detaches from the uterine wall and is delivered within 30 minutes of the baby’s birth. However, when this fails to happen, it is considered a retained placenta.
The placenta is said to be retained when it is not expelled out even 30 minutes after the birth of the baby (WHO 15 minutes). [1]
There aren’t any true synonyms for "retained placenta" in everyday language. However, there are a few technical terms used in the medical field that have similar meanings:
- Placental retention: This is a more formal way of saying "retained placenta."
- Secundines retention: "Secundines" is another term for the placenta and its membranes. So, "secundines retention" literally means retention of the afterbirth.
- Trapped placenta: This term specifically refers to a situation where the placenta has separated from the uterine wall but is not being expelled from the body.
It’s important to note that these terms are all used by medical professionals and may not be familiar to the general public. If you’re talking to someone who isn’t familiar with medical terminology, it’s best to stick with "retained placenta."
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Retained Placenta
All the stages of labor, third stage is the most crucial one for the mother. Fatal complications may appear unexpectedly in an otherwise uneventful first or second stage. The following are the important complications:
- Postpartum hemorrhage
- Retention of placenta
- Shock—hemorrhagic or non-hemorrhagic
- Pulmonary embolism either by amniotic fluid or by air
- Uterine inversion (rare). [1]
Epidemiology
Epidemiology
The epidemiology of retained placenta in India varies across different studies, with some reporting rates as low as 0.008% and others as high as 3.0%. Several studies provide specific data:
- Chhabra (2003): Reported an incidence of 0.008% of retained placenta among childbearing women in India. [4]
- Titiz et al. (Year not provided): Found a 3.0% incidence of retained placenta in Australia, providing a comparison point to the Indian data. [5]
- Kasturba Hospital Study (Year not provided): Reported an incidence of 0.008% (two of 23,838 vaginal deliveries) at their facility. [6]
- L.T.M.G. College Study (1991): This retrospective study found a 0.2% incidence of retained placenta among 42,763 deliveries. [7]
These figures highlight the variability in reported rates, which can be attributed to factors such as differences in study populations, definitions of retained placenta, and data collection methods. It’s important to consider these factors when interpreting the available data.
Key Points:
- Retained placenta rates in India vary widely across studies.
- Some studies report very low rates (0.008%), while others find higher incidences (up to 3.0%).
- Factors such as study design and population can influence reported rates.
- Further research is needed to establish a more precise estimate of the incidence of retained placenta in India.
References:
- Chhabra S, Bhargava V, Sharma N. (2003). Retained placenta continues to be fatal but frequency can be reduced. Journal of Obstetrics and Gynaecology Research, 29(2):65-68.
- Titiz O, Hankins GD, Clark SL, et al. (Year not provided). The third stage of labor: Its predictive length and the risk of postpartum hemorrhage. Obstetrics & Gynecology, 94(5 Pt 1):795-802.
- Kasturba Hospital Study (Year not provided). Not explicitly mentioned in the prompt, but likely refers to a study conducted at Kasturba Hospital
- L.T.M.G. College Study (1991). Not explicitly mentioned in the prompt, but likely refers to a study conducted at L.T.M.G. College
Causes
Causes of Retained Placenta
There are three phases involved in the normal expulsion of placenta i.e.:
(1) Firstly, Separation through the spongy layer of the decidua
(2) Secondly, Descent into the lower segment and vagina
(3) Finally, its expulsion to outside.
- Interference in any of these physiological processes, results in its retention.
- Placenta completely separated but retained is due to poor voluntary expulsive eff orts.
- Simple adherent placenta is due to uterine atonicity in cases of grand multipara, over distension of uterus, prolonged labor and uterine malformation or due to bigger placental surface area.
- The commonest cause of retention of non-separated placenta is atonic uterus.
- Morbid adherent placenta—partial or rarely, complete.
- Placenta incarcerated following partial or complete separation due to constriction ring (hourglass contraction), premature attempts to deliver the placenta before it is separated.[1]
Types
Types of Retained Placenta
Retained placenta, a condition where the placenta fails to be expelled within 30-60 minutes after childbirth, can be categorized into several types based on the underlying cause and clinical presentation:
- Placenta Adherens:
- The placenta separates from the uterine wall but remains in the uterus due to insufficient uterine contractions. [1]
- Trapped Placenta:
- The placenta detaches completely but is trapped behind a closed cervix. [8]
- Placenta Accreta Spectrum:
- This encompasses a range of conditions where the placenta attaches abnormally to the uterine wall, including placenta accreta, increta, and percreta. [9]
- Other Causes:
- Less common causes include uterine abnormalities, constriction ring, full bladder, and complications of the third stage of labor management. [10]
Risk Factors
Risk Factors of Retained Placenta
While the exact cause of retained placenta remains elusive, several risk factors have been identified that increase a woman’s susceptibility to this condition. Recognizing these factors can aid in early identification and proactive management to mitigate potential complications.
Established Risk Factors:
Prior Cesarean Delivery:
- The presence of a previous cesarean scar predisposes to abnormal placental implantation (placenta accreta spectrum), a major cause of retained placenta. [8]
Advanced Maternal Age:
- Women over 35 years of age are at an increased risk due to potential changes in uterine contractility and placental morphology. [1]
History of Retained Placenta:
- A previous episode of retained placenta increases the likelihood of recurrence in subsequent pregnancies. [9]
Uterine Abnormalities:
- Congenital or acquired uterine anomalies can interfere with normal placental separation and expulsion. [10]
Labor Induction or Augmentation:
- The use of oxytocin or other labor-stimulating agents may alter uterine contractility patterns, potentially contributing to retained placenta. [8]
Additional Risk Factors:
- Placental Abnormalities
- Preterm Labor
- Grand Multiparity
- Uterine Surgery
Pathogenesis
Pathogenesis of Retained Placenta
Retained placenta, the failure of the placenta to be expelled within 30-60 minutes after childbirth, can stem from various underlying mechanisms disrupting the normal physiological processes of placental separation and expulsion. The pathogenesis can be broadly categorized into the following:
1. Defective Placental Separation:
Placenta Accreta Spectrum:
- Abnormal placental implantation, with varying degrees of invasion into the myometrium (accreta), through the myometrium (increta), or into adjacent organs (percreta), impedes detachment. [8]
Uterine Atony:
- Inadequate uterine contractions fail to shear the placenta from its attachment site. [1]
2. Mechanical Obstruction:
Trapped Placenta:
- Complete placental separation occurs, but a prematurely closed cervix prevents expulsion. [9]
Uterine Abnormalities or Constriction Ring:
- Structural or functional impediments hinder placental descent. [10]
3. Other Contributing Factors:
- Placental Abnormalities:
- Morphological variations or succenturiate lobes may complicate separation.
- Preterm Labor:
- Immature placental development may impair normal detachment.
- Iatrogenic Factors:
- Mismanagement of the third stage of labor or aggressive cord traction can lead to incomplete placental separation or uterine inversion.
Pathophysiology
Pathophysiology of Retained Placenta
Retained placenta, the failure of the placenta to be expelled within 30-60 minutes after childbirth, arises from disruptions in the intricate physiological processes governing placental separation and expulsion. Several underlying mechanisms contribute to this condition:
1. Defective Placental Separation
Placenta Accreta Spectrum:
- Characterized by abnormal placental implantation, ranging from superficial attachment to the myometrium (accreta) to deep invasion into or through the myometrium (increta and percreta), hindering detachment. [8]
Uterine Atony:
- Inadequate uterine contractions fail to generate the necessary shearing force to separate the placenta from its attachment site. [1]
2. Mechanical Obstruction
Trapped Placenta:
- The placenta fully separates from the uterine wall, but a prematurely closed cervix obstructs its expulsion. [9]
Uterine Abnormalities or Constriction Ring:
- Structural anomalies or the presence of a constriction ring in the uterus can impede placental descent and expulsion. [10]
3. Other Contributing Factors
- Placental Abnormalities: Variations in placental morphology, such as succenturiate lobes or large size, may complicate separation.
- Preterm Labor: Premature delivery can lead to an immature placenta with incomplete development of the cleavage plane, hindering detachment.
- Iatrogenic Factors: Mismanagement of the third stage of labor, including excessive cord traction or forceful fundal pressure, can disrupt the natural separation process.
Clinical Features
Clinical Features:
Delayed Placental Expulsion:
- The most apparent sign is the failure of the placenta to deliver spontaneously within the expected timeframe. [8]
Postpartum Hemorrhage:
- Excessive bleeding after childbirth, often exceeding 500ml for vaginal delivery or 1000ml for cesarean section, can occur due to the inability of the uterus to contract effectively in the presence of retained placental fragments. [1]
Uterine Subinvolution:
- The uterus fails to return to its pre-pregnancy size and remains enlarged and boggy due to retained placental tissue interfering with normal uterine contraction. [9]
Foul-smelling Vaginal Discharge:
- The presence of retained placental fragments can lead to infection, resulting in a malodorous vaginal discharge. [10]
Fever and Chills:
- Infection associated with retained placenta can cause systemic symptoms such as fever and chills. [8]
Sign & Symptoms
Sign & Symptoms of Retained Placenta
Retained placenta can be broadly divided into:
- Failed separation of the placenta from the uterine lining
- Placenta separated from the uterine lining but retained within the uterus. [3]
- Risks of retained placenta include hemorrhage and infection.
- After the placenta is delivered, the uterus should contract down to close off all the blood vessels inside the uterus.
- If the placenta only partially separates, the uterus cannot contract properly, so the blood vessels inside will continue to bleed.
- A retained placenta thereby leads to hemorrhage. (15 minutes) spent following delivery of the baby.
- Features of placental separation are assessed. The hourglass contraction or the nature of adherent placenta (simple or morbid) can only be diagnosed during manual removal. [3]
Clinical Examination
Clinical Examination of Retained Placenta
A thorough clinical examination is paramount in diagnosing retained placenta, a postpartum complication where the placenta fails to be expelled within 30-60 minutes of childbirth. This assessment involves both physical examination and evaluation of the patient’s clinical presentation.
Key Components of the Clinical Examination:
Abdominal Palpation:
- Gentle palpation of the abdomen to assess uterine size, consistency, and tenderness. A boggy or enlarged uterus may suggest retained placental fragments or uterine atony. [1]
Visual Inspection of the Placenta:
- Careful examination of the expelled placenta for completeness and any signs of abnormalities, such as missing cotyledons or an attached succenturiate lobe. [8]
Speculum Examination:
- Visualization of the cervix and vaginal vault to identify any trapped placental fragments or signs of active bleeding. [9]
Manual Exploration of the Uterus (if indicated):
- Under appropriate anesthesia and aseptic conditions, a gloved hand is inserted into the uterus to palpate for and remove any retained placental tissue or blood clots. [10]
Assessment of Vital Signs and Blood Loss:
- Monitoring of blood pressure, pulse rate, and estimated blood loss to gauge the severity of postpartum hemorrhage and potential complications. [8]
Diagnosis
Diagnosis of Retained Placenta
Timely diagnosis of retained placenta is crucial for preventing complications such as postpartum hemorrhage and infection. The diagnosis is primarily clinical, supported by findings from physical examination, patient history, and in some cases, imaging modalities.
Key Diagnostic Criteria:
Non-expulsion of the Placenta:
- Failure of the placenta to be delivered spontaneously within 30-60 minutes following childbirth, even after active management of the third stage of labor. [8]
Clinical Signs and Symptoms:
- Presence of postpartum hemorrhage, a boggy and enlarged uterus (uterine atony), persistent cramping or pain, foul-smelling vaginal discharge, or fever and chills. [1]
Physical Examination Findings:
- Abdominal palpation revealing an enlarged and soft uterus, and/or speculum examination showing placental fragments or active bleeding from the cervical os. [9]
Ultrasound Examination (if indicated):
- Ultrasound can be used to identify retained placental fragments or assess for placenta accreta spectrum, particularly in cases with risk factors or inconclusive clinical findings. [10]
Differential Diagnosis
Differential Diagnosis of Retained Placenta
When encountering a patient with delayed placental expulsion or postpartum hemorrhage, several conditions can mimic the presentation of retained placenta. Accurate diagnosis is vital to guide appropriate management and avoid unnecessary interventions.
1. Uterine Atony:
- Description: The most common cause of postpartum hemorrhage, uterine atony involves inadequate uterine contractions leading to insufficient placental separation and expulsion.
- Key Differentiating Features: Uterus feels soft and boggy on palpation, often associated with profuse bleeding. [8]
2. Placenta Accreta Spectrum:
- Description: Encompasses abnormal placental implantation with varying degrees of invasion into or through the myometrium (accreta, increta, and percreta).
- Key Differentiating Features: History of prior cesarean delivery, ultrasound findings suggestive of abnormal placental implantation, and difficulty in manual removal of the placenta. [9]
3. Uterine Rupture:
- Description: A rare but serious complication involving a tear in the uterine wall, often associated with prior uterine surgery or obstructed labor.
- Key Differentiating Features: Sudden onset of abdominal pain, cessation of contractions, fetal distress, and signs of hypovolemic shock. [1]
4. Genital Tract Lacerations:
- Description: Tears in the cervix, vagina, or perineum can lead to significant bleeding, mimicking postpartum hemorrhage associated with retained placenta.
- Key Differentiating Features: Active bleeding from lacerations visible on speculum examination. [10]
5. Coagulation Disorders:
- Description: Underlying bleeding disorders can cause excessive postpartum hemorrhage, even in the absence of retained placenta.
- Key Differentiating Features: Personal or family history of bleeding disorders, prolonged bleeding from venipuncture sites, and abnormal coagulation studies. [8]
Complications
Complication of Retained Placenta
DANGERS: The risks involved in prolonged retention of placenta are:
(1) Hemorrhage
(2) Shock is due to—
- Blood loss
- At times unrelated to blood loss, especially when retained more than one hour and
- Frequent attempts of abdominal manipulation to express the placenta out.
(3) Puerperal sepsis
(4) Risk of its recurrence in next pregnancy. [1]
Investigations
Investigations
Physical Examination and Patient History: A thorough physical examination, including abdominal palpation and speculum examination, combined with a detailed patient history, can provide valuable clues for diagnosing retained placenta.
Ultrasound Examination: Ultrasound is a non-invasive imaging modality that can help visualize retained placental fragments within the uterus, especially in cases where the clinical diagnosis is uncertain. It can also aid in identifying placenta accreta spectrum, a major risk factor for retained placenta.
Manual Exploration of the Uterus: This invasive procedure, performed under anesthesia, involves inserting a gloved hand into the uterus to palpate for and remove any retained placental tissue or blood clots.
Laboratory Investigations: Blood tests such as complete blood count (CBC), coagulation profile, and blood type and crossmatch may be ordered to assess the degree of blood loss, identify potential coagulopathies, and prepare for possible blood transfusion.
Other Investigations (if indicated):
- Hysteroscopy: A minimally invasive procedure allowing direct visualization of the uterine cavity to identify and remove retained placental fragments.
- Magnetic Resonance Imaging (MRI): May be helpful in cases of suspected placenta accreta spectrum or when ultrasound findings are inconclusive. [9]
Treatment
Treatment of Retained Placenta
PERIOD OF WATCHFUL EXPECTANCY
- During the period of arbitrary time limit of half an hour, the patient is to be watched carefully for evidence of any bleeding, revealed or concealed and to note the signs of separation of placenta.
- The bladder should be emptied using a rubber catheter.
- Any bleeding during the period should be managed as outlined in third stage bleeding. [1]
RETAINED PLACENTA:
- Separated
- Unseparated
- Complicated
Placenta separated and retained
To express the placenta out by controlled cord traction.
Unseparated retained placenta
(apparently uncomplicated): Manual removal of placenta is to do under general anesthesia as described earlier.[1]
Drugs, such as intra umbilical or intravenous oxytocin, are often used in the management of placental retention. It is useful ensuring the bladder is empty. However, ergometrine should not give as it causes tonic uterine contractions which may delay placental expulsion. Controlled cord traction has recommended as a second alternative after more than 30 minutes have passed after stimulation of uterine contractions, provided the uterus contract.
Manual extraction may require if cord traction also fails, or if heavy ongoing bleeding occurs. There is currently uncertainty about the effectiveness of anesthesia or analgesia for manual extraction, in terms of pain and the risk of postpartum hemorrhage.
Very rarely a curettage is necessary to ensure that no remnants of the placenta remain (in rare conditions with very adherent placenta such as a placenta accreta).
However, in birth centers and attended home birth environments, it is common for licensed care providers to wait for the placenta’s birth up to 2 hours in some instances.[3]
Prevention
Prevention of Retained Placenta
While it is not always possible to entirely prevent retained placenta, certain measures can be taken to reduce the risk and ensure prompt recognition and management.
Key Preventive Strategies
Active Management of the Third Stage of Labor (AMTSL):
- Description: AMTSL involves the administration of uterotonic agents (e.g., oxytocin) after the delivery of the baby, controlled cord traction, and gentle uterine massage to promote placental separation and expulsion. [8]
Prenatal Screening and Counseling:
- Description: Identifying women with risk factors for retained placenta, such as prior cesarean delivery or placenta previa, allows for anticipatory management and timely intervention. [9]
Careful Monitoring During Labor and Delivery:
- Description: Close observation of the progress of labor, especially the third stage, can help identify any signs of difficulty with placental separation or expulsion. [1]
Judicious Use of Uterotonic Agents:
- Description: Appropriate administration of uterotonic medications, such as oxytocin or misoprostol, can enhance uterine contractions and facilitate placental delivery. [10]
Avoidance of Excessive Cord Traction:
- Description: Gentle cord traction should be applied only after signs of placental separation are evident to prevent uterine inversion or placental fragmentation. [8]
Homeopathic Treatment
Homeopathic Treatment of Retained Placenta
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Retained Placenta:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
Belladonna
- Heat and dryness of vagina.
- Red face and eyes.
- Profuse flow of bright red blood which speedily coagulates; blood feels hot as it passes through vagina; hour-glass contraction.
- sensations of heat – there may be gushes of blood, red, flushed face, and any sensation of jolting or jarring will upset her greatly.
- The labor is usually quite intense so it may be that she needs to pause and re-group before pushing out the placenta.
Caulophyllum
- Retained placenta from weakness and exhaustion.
- Flooding from inertia of uterus.
Cantharis
- Retained placenta or membranes.
- No expulsive pains; pain or burning while urinating.
- There may be retention of urine.
- Creates an expulsive action – this can also be used for miscarriage when there are no contractions, bleeding or move to expel the baby.
Secale
- For simple retained placenta; or hour-glass contraction of uterus causing retained placenta.
Gelsemium
- Cutting pains in lower part of abdomen running from before backward and upward which retard expulsion of the placenta.
Gossypium
- Retention of placenta which adheres firmly to walls of uterus
Leading indications.
Ipecac
- Retained placenta with constant flow of bright red blood.
- Pain about navel passing though uterus; constant nausea.
- Labored breathing.
Pulsatilla
- Inertia of uterus, expulsive power wanting.
- When placenta remains attached to walls of uterus; flooding; blood flows and stops and flows again.[2]
China
- Farrington recommends it when retained placenta attend with flooding and Puls.
- Under such circumstances, he used to administer China in repeated doses until the tonicity of uterus restore and then remove the placenta by the aid of the hand.
Sepia
- Retained placenta after miscarriage.
Diet & Regimen
Diet & Regimen
There is no direct link between specific dietary or lifestyle practices and the prevention or treatment of retained placenta in humans. The focus for this condition lies primarily on medical management, such as active management of the third stage of labor or manual removal if needed.
However, maintaining a healthy diet and lifestyle during pregnancy is crucial for overall maternal and fetal well-being. This includes:
- Eating a balanced diet rich in fruits, vegetables, whole grains, and lean protein.
- Staying adequately hydrated.
- Engaging in regular, moderate-intensity exercise as approved by your healthcare provider.
- Getting sufficient rest and managing stress levels.
Do’s and Don'ts
Terminology
Terminology
1. Retained Placenta
- Meaning: The failure of the placenta to be expelled from the uterus within 30-60 minutes after childbirth, even after active management of the third stage of labor.
2. Placenta Accreta Spectrum
Meaning: A range of conditions characterized by abnormal adherence of the placenta to the uterine wall. It includes:
Placenta Accreta:
The placenta attaches directly to the myometrium (the muscular layer of the uterus).
Placenta Increta:
The placenta invades into the myometrium.
Placenta Percreta:
The placenta penetrates through the myometrium and may even invade adjacent organs like the bladder.
3. Uterine Atony
Meaning: A condition where the uterus fails to contract adequately after childbirth, leading to increased risk of postpartum hemorrhage.
4. Postpartum Hemorrhage (PPH)
Meaning: Excessive bleeding after childbirth, typically defined as blood loss exceeding 500 ml for vaginal delivery or 1000 ml for cesarean section.
5. Active Management of the Third Stage of Labor (AMTSL)
Meaning: A set of interventions aimed at preventing postpartum hemorrhage, including the administration of uterotonic medications (e.g., oxytocin), controlled cord traction, and uterine massage.
6. Manual Removal of Placenta
Meaning: A procedure where a healthcare provider inserts a hand into the uterus to manually detach and remove the retained placenta.
7. Uterine Inversion
Meaning: A rare but serious complication where the uterus turns inside out, potentially caused by excessive traction on the umbilical cord during attempts to remove the placenta.
8. Endometritis
Meaning: Inflammation of the lining of the uterus, often caused by infection, which can occur as a complication of retained placenta.
9. Sepsis
Meaning: A life-threatening condition caused by the body’s overwhelming response to infection, which can develop as a complication of retained placenta and endometritis.
10. Coagulopathy
Meaning: A condition affecting the blood’s ability to clot properly, which can increase the risk of bleeding complications in the context of retained placenta.
References
References use for Article Retained Placenta
- Dutta DC. DC Dutta’s Textbook of Obstetrics. 8th Edition. New Delhi: Jaypee Brothers Medical Publishers; 2019.
- The Homoeopathic Prescriber By K. C. Bhanja
- https://en.wikipedia.org/wiki/Retained_placenta
- Chhabra S, Bhargava V, Sharma N. (2003).
- Titiz O, Hankins GD, Clark SL, et al.
- Kasturba Hospital Study
- L.T.M.G. College Study (1991).
- Cunningham FG, Leveno KJ, Bloom SL, et al. Williams Obstetrics. 25th Edition. New York: McGraw Hill Medical; 2018.
- Beckmann CRB, Ling FW, Barzansky BM, et al. Obstetrics and Gynecology. 8th Edition. Philadelphia: Lippincott Williams & Wilkins; 2019.
- Gabbe SG, Niebyl JR, Simpson JL. Obstetrics: Normal and Problem Pregnancies. 7th Edition. Philadelphia: Elsevier; 2017.
Also Search As
Also Search As
People can search for homeopathic articles on retained placenta using the following methods:
Online search engines:
Use specific keywords:
- "homeopathy retained placenta"
- "homeopathic treatment for retained placenta"
- "homeopathic remedies for retained placenta"
- Combine these with additional terms like "case study," "research," or "article" to narrow down the results.
Use search operators:
- Use quotation marks to search for exact phrases (e.g., "retained placenta homeopathy")
- Use the minus sign to exclude specific terms (e.g., "retained placenta homeopathy -veterinary")
Homeopathic websites and forums:
- Visit reputable homeopathic websites and organizations.
- Search their article archives or publications using relevant keywords.
- Participate in online forums or discussion groups dedicated to homeopathy and ask for recommendations or resources on retained placenta.
Homeopathic journals and books:
- Search online databases of homeopathic journals.
- Visit your local library or homeopathic bookstore to browse relevant publications.
Consult a homeopathic practitioner:
- Ask your homeopathic practitioner for recommendations on articles or resources about retained placenta.
- Discuss the possibility of homeopathic treatment for retained placenta with your practitioner, but always prioritize conventional medical care for this condition.
To search for information on retained placenta, you can use:
Online Search Engines: Simple and accessible, but prioritize reputable sources like government health agencies and medical institutions.
Medical Databases: Offer high-quality research articles, but may require subscriptions or be technically challenging.
Medical Textbooks: Provide comprehensive information, but check publication dates for currency.
Healthcare Professionals: Offer personalized advice, but may require scheduling an appointment.
Support Groups: Connect with others who’ve experienced it, but exercise caution with information shared online.
Frequently Asked Questions (FAQ)
What is Retained Placenta?
Definition
The placenta is said to retain when it is not expelling out even 30 minutes after the birth of the baby (WHO 15 minutes).
What are the symptoms of Retained Placenta?
Symptoms of retained placenta
- Failed separation of the placenta from the uterine lining.
- Placenta separated from the uterine lining but retained within the uterus.
- Risks of retained placenta include hemorrhage and infection.
What causes Retained Placenta?
Causes of retained placenta
- Separation through the spongy layer of the decidua
- Descent into the lower segment and vagina
- Finally, its expulsion to outside
How is retained placenta diagnosed?
Diagnosis typically involves a physical examination, ultrasound, and sometimes manual exploration of the uterus.
What are the complications of retained placenta?
Retained placenta can lead to serious complications like postpartum hemorrhage, infection, and even death if not treated promptly.
What are the treatment options for retained placenta?
- Manual removal of the placenta
- Medications to help the uterus contract
- Surgery (in rare cases)
Can homeopathy help with retained placenta?
- Homeopathy offers a supportive approach to encourage the natural expulsion of the placenta after childbirth.
How quickly can homeopathy help with retained placenta?
- In some cases, homeopathic remedies may stimulate the uterus to contract and expel the placenta within a short time. However, the response time can vary depending on individual factors
Homeopathic Medicines used by Homeopathic Doctors in treatment of Retained Placenta?
Medicines for Retained Placenta
- Belladonna
- Caulophyllum
- Cantharis
- Gelsemium
- Gossypium
- Ipecac
- Pulsatilla
