Breastfeeding
Definition
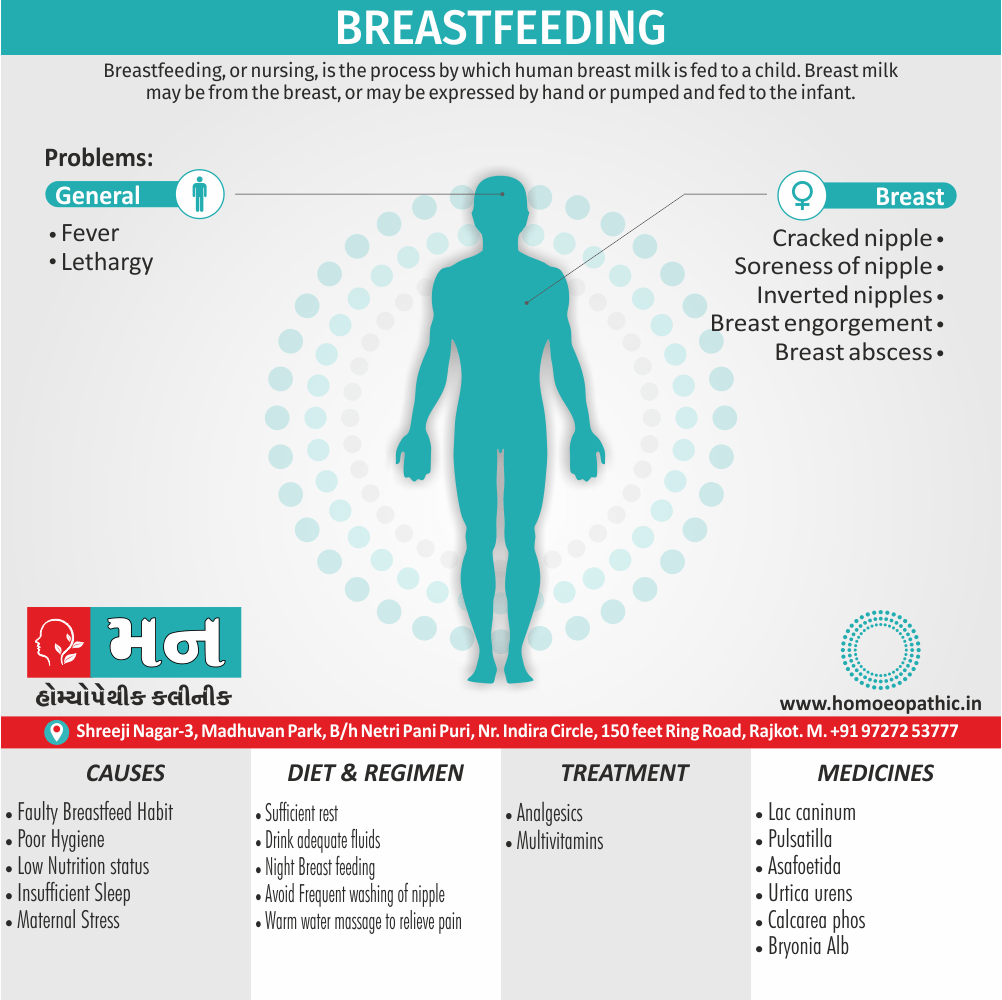
Breastfeeding, or nursing, is the process by which human breast milk is fed to a child. Breast milk may be from the breast, or may be expressed by hand or pumped and fed to the infant.[3]
Here are some synonyms for "breastfeeding" depending on the context:
Formal Synonyms:
- Lactation: This is the biological term for milk production in mammals, including breastfeeding.
- Nursing: This term emphasizes the act of a baby feeding from the breast.
- Direct breastfeeding: This clarifies that the baby is feeding directly from the breast, as opposed to expressed milk.
Informal Synonyms:
- Nursing on the breast: This is a more descriptive version of "nursing."
- Feeding at the breast: Similar to "nursing on the breast," but emphasizes the feeding aspect.
- Breastfeeding a baby: This explicitly mentions both the mother and the baby.
Neutral terms (avoiding "breast"):
- Chestfeeding: This is a more inclusive term for people who may not identify with the term "breastfeeding."
- Milk feeding: This is a general term that doesn’t specify the source of the milk.
Important Considerations:
- In a medical setting, "breastfeeding" is the most widely used and understood term.
- "Lactation" is appropriate for formal discussions or scientific contexts.
- When aiming for inclusivity, "chestfeeding" or "milk feeding" can be used.
- Consider your audience and the level of formality when choosing a synonym.
Additionally:
- Some cultures have specific terms for breastfeeding. If you’re referring to breastfeeding in a particular cultural context, research the appropriate term.
Overview
Anatomy
Physiology
Benefits
Composition
Affecting Factors
Reflexes
Technique
Problems with Breastfeeding
Breastfeeding Breast Care
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
Breastfeeding is one of the most effective ways to ensure child health and survival. However, nearly 2 out of 3 infants are not exclusively breastfed for the recommended 6 months—a rate that has not improved in 2 decades.
Breastmilk is the ideal food for infants. It is safe, clean and contains antibodies which help protect against many common childhood illnesses. Breastmilk provides all the energy and nutrients that the infant needs for the first months of life, and it continues to provide up to half or more of a child’s nutritional needs during the second half of the first year, and up to one third during the second year of life.
Breastfed children perform better on intelligence tests, are less likely to be higher-weight person and less prone to diabetes later in life. Women who breastfeed also have a reduced risk of breast and ovarian cancers.
Inappropriate marketing of breast-milk substitutes continues to undermine efforts to improve breastfeeding rates and duration worldwide.[3]
Anatomy
Anatomy
- The breast is made up of glandular tissue, supporting tissue and fat.
- The glandular tissue consists of small clusters of sac-like spaces which produce milk.
- Each sac is lined by network of myoepithelial cells that propel the milk into lactiferous ducts towards nipple.
- Before reaching the nipple, the ducts widen to form lactiferous sinuses which store milk.
- The lactiferous sinuses lie beneath the junction of areola and rest of breast.
- The areola and nipples are extremely sensitive as they are supplied by a rich network of nerve endings.
- On the areola there are small swellings of glands which produce an oily fluid to keep the nipple skin soft.
- Since the lactiferous sinuses lie beneath the areola, a baby must suck at the nipple and areola.
- The gum line of the baby should rest at the junction of areola and rest of breast tissue in order to express milk stored in lactiferous sinuses.[1]
Physiology
Physiology
- Lactogenesis is a complex phenomenon involving many hormones and reflexes. Two hormones are most important, prolactin and oxytocin Prolactin reflex (milk secretion reflex).
- Prolactin produced by the anterior pituitary gland is responsible for milk secretion by the alveolar epithelial cells.
- When the baby sucks, the nerve ending in the nipple carry impulse to the anterior pituitary which in turn release prolactin and that acts on the alveolar glands in the breast to stimulate milk secretion.
- This cycle from stimulation to secretion is called the prolactin reflex or the milk secretion reflex.
- The more the baby sucks at the breast, the greater is the milk production. The earlier the baby is put to the breast, the sooner this reflex is initiated.
- The greater the demand more is the production. It is, therefore, important for mothers to feed early, frequently and empty out the breasts completely at each feeding session.
Other factors
- Since prolactin is produced during night time, breastfeeding during night is very important for maintenance of this reflex.
- This cycle from stimulation to secretion is called the prolactin reflex or the milk secretion reflex. The more the baby sucks at the breast, the greater is the milk production.
- The earlier the baby is put to the breast, the sooner this reflex is initiated. The greater the demand more is the production.
- It is, therefore, important for mothers to feed early, frequently and empty out the breasts completely at each feeding session.
- Since prolactin is produced during night time, breastfeeding during night is very important for maintenance of this reflex.
Oxytocin reflex
- Oxytocin is a hormone produced by the posterior pituitary.
- It is responsible for ejection of the milk from the glands into the lactiferous sinuses.
- This hormone is produced in response to stimulation to the nerve endings in the nipple by suckling as well as by the thought, sight, or sound of the baby.
- Since this reflex is affected by the mother’s emotions, a relaxed, confident attitude helps the milk ejection reflex. On the other hand, tension and lack of confidence hinder the milk flow.[1]
Benefits
Benefits
Breast milk is the best source of nutrition for most babies-
- As the baby grows, the mother’s breast milk will change to meet her baby’s nutritional needs.
Breastfeeding can help protect babies against some short- and long-term illnesses and diseases-
- Breastfed babies have a lower risk of asthma, obesity, type 1 diabetes, and sudden infant death syndrome (SIDS). Breastfed babies are also less likely to have ear infections and stomach bugs.
Breast milk shares antibodies from the mother with her baby-
- These antibodies help babies develop a strong immune system and protect them from illnesses.
Mothers can breastfeed anytime and anywhere-
- Mothers can feed their babies on the go without worrying about having to mix formula or prepare bottles. When traveling, breastfeeding can also provide a source of comfort for babies whose normal routine is disrupted.
Breast feeding can reduce the mother’s risk of breast and ovarian cancer, type 2 diabetes, and high blood pressure-
- Breastfeeding has health benefits for the mother too! Some cancers, type 2 diabetes, and high blood pressure are less common among women who breastfeed.[4]
Composition
Composition
The composition of breast milk varies at different time points of lactation to suit the needs of the baby.
Milk of a mother who has delivered a preterm baby is different from milk of a mother delivered a term baby.
Colostrum
Colostrum is the milk secreted during the initial 3—4 days after delivery. It is small in quantity, yellow and thick and contains large number of antibodies and immune-competent cells and vitamins A, D, E and K.
Transitional milk
Transitional milk is the milk secreted after 3-4 days until two weeks. The immunoglobulin and protein content decreases while the fat and sugar content increases.
Mature milk
Mature milk follows transitional milk. It is thinner and watery but contains all the nutrients essential for optimal growth of the baby.
Preterm milk
Preterm milk is the milk of a mother who delivers before 37 weeks. It contains more proteins, sodium, iron, immunoglobulins and calories as per the requirement of preterm baby.
Foremilk
Foremilk is the milk secreted at the start of a feed. It is watery and is rich in proteins, sugar, vitamins, minerals and water that quenches the baby’s thirst.
Hindmilk
Hindmilk comes later towards the end of feed and is richer in fat that provides more energy and gives a sense of satiety. Thus, the composition of milk also varies during the phase of feeding. For optimum growth, the baby needs both fore as well as hind milk. Therefore, the baby should be allowed to empty out one breast completely before switching over to the other.[5]
- Human breast milk is recognized by health organizations around the world as an ideal source of nutrition to support early life.
- A diet of exclusively breast milk is recommended for the first 6 months of life followed by the addition of solid foods plus breastmilk for up to 2 years of age.
- Breast milk is produced by a woman’s body specifically to meet her child’s nutritional needs.
- It provides everything a baby’s body requires for proper growth and development, changing in response to the baby’s needs.
- Not only is breast milk a complete source of nutrition and hydration, but it also helps protect babies from getting sick through antibodies that pass from mother to baby through the milk.
- Breast milk is composed of hundreds of distinct bioactive molecules, some of which are not yet fully understood by scientists.
- Although infant formula also provides complete nutrition, it doesn’t fully replicate the immune benefits of breast milk.
Macronutrient Composition
Breast milk is primarily composed of water, carbohydrates, lipids, and proteins. Each of these nutrients plays a role in contributing to infant growth and development.
Water
- Human breast milk is made up of about 90% water.
- The human body depends on water to function.
- Water maintains hydration, helps regulate body temperature, lubricates joints, and protects organs.
- Luckily, breast milk alone provides all of the water required by young babies for survival.
Carbohydrates
- Carbohydrates are a preferred energy source for the brain.
- The main carbohydrate in breast milk is milk sugar, known as lactose.
- Human milk contains more lactose than cow’s milk.
- Other carbohydrates found in breast milk (such as oligosaccharides) promote healthy bacteria in your baby’s intestines. These bacteria protect your baby’s gut and can help fight off diseases like infant diarrhea.
Lipids (Fats)
- Lipids may only make up about 4% of breast milk, but they provide over half of the calories that your baby receives from it.
- Lipids are a major source of energy, cholesterol, and essential fatty acids such as DHA.
- These nutrients are necessary for the development of your baby’s brain, nervous system, and vision.
- The high-calorie content of lipids in breast milk is also responsible for the baby’s healthy weight gain. Breast milk should naturally contain all the lipids your baby needs to grow for the first 6 months of life.
Proteins
- Proteins build, strengthen, and repair the body’s tissue. They are also needed to make hormones, enzymes, and antibodies.
- The protein in breast milk is easy for babies to digest and these proteins are essential throughout every stage of the lifecycle for humans to survive.
- Lactoferrin is a form of protein in breast milk that moves iron through your baby’s body. It also helps protect your newborn’s intestines from infections.10
Bioactive Components
There are several elements of breast milk that cannot be found in formula. These unique substances are passed from the mother.
Immunoglobulins (Antibodies)
- Immunoglobulins are antibodies that fight off illness and disease. Because of these natural immune substances, breast milk can almost be thought of as a baby’s first vaccine.
- The properties of breast milk help protect against the common cold, ear infections, vomiting, diarrhea, and other potentially dangerous infections.
- The primary antibody in breast milk is Secretory Immunoglobulin A (IgA). IgA coats the baby’s lungs and intestines, sealing them to prevent germs from entering the body and bloodstream.
Hormones
- Hormones have many jobs in the human body. They influence growth and development, metabolism, stress and pain responses, and blood pressure regulation.
- Hormones involved in milk production include prolactin, thyroid hormones, and growth factors.
Enzymes
- Several key enzymes are found in human breast milk. Some aid digestion by breaking down fats or proteins, while others provide immune support.
- Many of the enzymes in human breast milk have unknown functions. While we may not fully understand what all of these enzymes do, there’s a good chance they play beneficial roles in infant development.
Micronutrients
Breast milk contains the vitamins and minerals needed to support young babies. Formulas also contain many of these vital micronutrients.
Vitamins
- Vitamins support healthy bones, eyes, and skin. They are necessary to prevent diseases of malnutrition, such as scurvy and rickets.
- Breast milk typically contains all the vitamins needed to support your baby’s health as they grow. However, the amount of vitamin D, folate, or vitamin B6 in your body may be lower if you follow certain dietary restrictions.
Minerals
- Like vitamins, breast milk is also full of minerals that your baby’s body needs to grow healthy and strong.
- These include iron, zinc, calcium, sodium, chloride, magnesium, and selenium.
- Minerals are used to build strong bones, produce red blood cells, and promote proper muscle and nerve function.[3]
Affecting Factors
Affecting Factors which reduce milk production
- Dummies, pacifiers and bottles not only interfere with breastfeeding but also predispose the baby to diarrhea.
- Giving supplements such as sugar water, gripe water, honey, breast milk substitutes or formula, either as prolateral (before initiation of breastfeeding) or supplemental (concurrent to breastfeeding) feeds. Studies have reported that even 1 or 2 supplemental feeds reduce the chances of successful breastfeeding.
- Painful breast conditions like sore or cracked nipples and engorged breast.
- Lack of night feeding, as the prolactin reflex is not adequately stimulated.
- Inadequate emptying of breast such as when baby is sick or small and the mother does not manually express breast milk or when baby is fed less frequently.[1]
Reflexes
Reflexes in the Baby
A baby is born with certain reflexes which help the baby to feed. These include rooting, sucking and swallowing reflexes.
The Rooting reflex
- When cheek or the side of the mouth is touched, the baby opens her mouth and searches for the nipple.
- This is called rooting reflex. This reflex helps the baby to find the nipple and in proper attachment to the breast.
The Suckling reflex
- When baby’s palate is touched with nipple, the baby starts sucking movements.
- This reflex is very strong immediately after birth.
The sucking reflex consists of:
- Drawing in the nipple and areola to form an elongated teat inside the mouth.
- Pressing the stretched nipple and areola with the jaw and tongue against the palate.
- Drawing milk from the lactiferous sinuses by wave
like peristaltic movement of the tongue underneath the areola and the nipple and compressing them against the palate above.
suckle effectively, the baby has to attach (latch) well.
Obtaining good attachment at breast is a skill, which both the mother and the baby have to learn.
Technique
Technique of Breastfeeding
Mothers require substantial assistance to learn the technique of breastfeeding. With correct technique, breastfeeding is natural and a pleasurable experience for the mother.
However, a variety of breastfeeding problems do occur in large proportion of mothers that require counseling and support from the health providers for their prevention and appropriate treatment.
Provision of lactation support services by lactational counsellor or trained health providers greatly increase the success of breastfeeding.
Positioning
- Position of the mother. The mother can assume any position that is comfortable to her and the baby.
- She can sit or lie down, her back should well support and she should not leaning on her baby Position of baby.
- Make sure that baby wrap properly in a cloth.
- Firstly, Baby’s whole body supported not just neck or shoulders
- Secondly, Baby’s head and body are in one line without any twist in the neck
iii. Baby’s body turned towards the mother (abdomens of the baby and the mother touching each other)
- Baby’s nose is at the level of the nipple.[1]
Attachment (Latching)
- After proper positioning, the baby’s cheek touch and that initiates rooting reflex.
- Allow the baby to open his mouth widely and at that point, the baby should latch on to the breast ensuring that the nipple and most of the areola are within baby’s mouth.
- It important that the baby brought on the mother’s breast and mother should not lean on to baby.
Signs of good attachment
- The baby’s mouth is wide open
- Most of the nipple and areola in the mouth, only upper areola visible, not the lower one
iii. The baby’s chin touches the breast
- The baby’s lower lip everted
Effective Suckling
- Baby suckles slowly and pauses in between to swallow (suck, suck, suck. and swallow). One may see throat cartilage and muscles moving and hear the gulping sounds of milk being swallowed.
- Baby’s cheeks are full and not hollow or retracting during sucking. [1]
Problems with Breastfeeding
Problems with Breastfeeding
Inverted nipples
- Flat or short nipples which become prominent easily on pulling out do not pose difficulty in breastfeeding.
- However, truly inverted or retracted nipples make latching difficult.
- As the baby is not able to take nipple and areola in the mouth properly, sucking on the nipples makes them sore and excoriated.
- Treatment start after birth of the baby. The nipple manually everted, stretched and rolled out several times a day. A plastic syringe use to draw out to correct the problem
Sore nipple
- Nipples become sore when baby suckles on the nipple rather than areola because of incorrect attachment.
- As the baby is unable to express milk, he sucks vigorously in frustration and bites the nipple causing soreness.
- Frequent washing with soap and water and pulling the baby off the breast while he is still sucking may also result in sore nipple.
- Treatment consists of correct positioning and latching of the baby to the breast.
- A mother would able to feed the baby despite sore nipple if the baby attach properly.
- Hind milk should apply to the nipple after a feed and the nipple should air and allowed to heal in between feeds.
- She should advise not to wash nipple each time before/ after feeding.
- She can clean breast and nipple once daily at time of bathing.
- There is no need to apply any cream or ointment to the sore nipples.[1]
Breast engorgement
- The milk production increases by the second and third day after delivery. Additionally, If feeding delay or infrequent, or the baby is not well positioning at the breast, the milk accumulates in the alveoli. In detail, As milk production increases, the amount of milk in the breast exceeds the capacity of the alveoli to store it comfortably. Such a breast becomes swollen, hard, warm and painful also term as an ‘engorged breast’.
- Breast engorgement can prevent by early and frequent feeds also correct attachment of the baby to the breast. Treatment consists of local warm water packs, breast massage also analgesics to relieve the pain. Milk should gently express to soften the breast.
Breast abscess
- If a congested engorged breast, cracked nipple, blocked duct or mastitis are not treated in the early stages, breast abscess formation can occur.
- The mother has high grade fever and a raised blood count. She must treat with analgesics also antibiotics.
- The abscess may require incision and drainage. Breastfeeding must be continued. [1]
Not enough milk
- First make sure that the perception of “not enough milk” is correct.
- If baby satisfy and sleeping for 2-3 hr after breastfeeding, passing urine at least 6-8 times in 24 hr and gaining weight, the mother is producing enough milk.
- There could a number of reasons for insufficient milk such as incorrect method of breastfeeding, supplementary or bottle feeding, no night breastfeeding, engorgement of breast, any illness, painful condition, maternal stress or insufficient sleep. Try to identify the possible reason and take appropriate actions.
- Advise mother to take sufficient rest and drink adequate fluids. Feed the baby on demand. Let the baby feed as long as possible on each breast. Advise the mother to keep the baby with her.
Expressed Breast Milk (EBM)
- If a mother is not in a position to feed her baby (e.g., ill mother, preterm baby, working mother, etc.), she should express her milk in a clean wide-mouthed container and this milk should be fed to her baby.
- EBM can store at room temperature for 6-8 hr, in a refrigerator for 24 hr and a freezer at -20 C for 3 months.[1]
Breastfeeding Breast Care
Breastfeeding Breast Care
- There really isn’t anything special you need to do for your breasts when you’re breastfeeding, beyond basic cleanliness, monitoring the moisture balance of your skin (too dry can cause cracking and too wet can breed germs), and noticing any changes that might need attention.
- As your breasts fill up with breast milk, you may experience breast engorgement, tenderness, tingling, and the leaking of breast milk.
- These are all normal experiences that can help by diligent breast care, which will also minimize other types of discomfort and help prevent infection.
Practice Good Hygiene
- Wash your hands before touching your breasts.
- Keep your breasts and nipples clean by washing them daily with warm water in the shower or bath.
- Also, avoid using soap on your breasts.
- Soap can cause dry, cracked, and irritated skin.
- It can also remove the natural oils produced by the Montgomery glands located on the dark area surrounding your nipples.
- These oils help to keep the nipples and areolas clean and moisturized.
Change Breast Pads Often
- If you are using breast pads or cotton squares inside your bra to soak up the breast milk from leaking breasts, be sure to change them when they become wet, as dampness can prompt germs to grow.
- Clean, dry nursing pads can help to prevent sore nipples, thrush, or mastitis.
Wear a Supportive Bra
- Choose a supportive nursing bra or a regular bra that fits well, but is not too tight.
- Cotton is an excellent choice of fabric since it allows your skin to breathe.
Make Sure Your Baby Is Latching On Correctly
- Getting your baby to latch on well from the first breastfeeding, and nursing very often—at least every 2 to 3 hours—can help prevent the development of painful breast problems such as sore nipples, breast engorgement, plugged milk ducts, and mastitis.
Remove Your Baby From Your Breast Correctly
- When you’re ready to take your baby off of the breast, do not pull them off. Instead, place your finger in the corner of their mouth to gently break the suction between their mouth and your breast.
Treat Sore Nipples
- After nursing your baby, to treat (and prevent) sore nipples, rub a safe nipple cream or some of your breast milk on your nipples and areola, and then let them air dry.
- If you have sore nipples, talk to your doctor or a lactation consultant about using purified lanolin or hydrogel pads to help soothe your breasts.
- Stay away from any lotions, creams, or sprays without first discussing them with your healthcare provider, as some products can harm your baby, clog your milk ducts, or irritate your skin even more.
Treat Engorgement
- If your breasts become painfully overfull, hard, and swollen, you can use cold cabbage leaves or cold compresses to reduce inflammation and relieve pain.
- Pumping or nursing often to relieve the pressure can also help.[5]
Homeopathic Treatment
Homeopathic Treatment of Breastfeeding
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Breastfeeding
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicine
Lac caninum
- It suits for people who experience irregular pains on the alternating sides of body and extreme weakness.
- It helps to reduce difficulties in lactation by treating galactorrhea and helping dry up milk when women cannot feed the baby.
- Swelling in breasts.
- Pain in breast before menstruation which becomes better after menstruation.
- Severe mastitis with even a little bit of jarring.
- Symptoms become worse in the morning time of one day and evening of next day.
- Better after drinking cold drinks and in cold weather.
Pulsatilla
- It is also an excellent remedy in scanty flow or absence of milk, the patient being gloomy or tearful.
- It is useful where mechanical irritation excites the flow of milk in young girls.
Asafoetida:
- It best suit for people with bone caries, pain during the night time and deep ulcer formations.
- It helps reduce lactation issues treating the low milk supply.
- Non pregnant women with breasts filled with milk.
- Oversensitivity of the breasts.
- Deficient milk production.
- Symptoms worsen at night, while taking rest, with warm application and lying on left side.
- Better in open air and after applying pressure or moving.
Urtica Urens
- In brief, Non-appearance of milk, with no special symptoms, may correct by this remedy.[2]
Calcarea phos
- It suit for children who are anemic and are flabby, weak and irritable.
- It helps reduce lactation problem by treating the problem of faulty and sour tasting milk.
- Pain and pressure in the uterine area after nursing specifically for a long time.
- Salty taste of milk so the child tends to refuse.
- Getting sexually excited during lactation.
- The infants want to nurse often also vomits easily.
- Symptoms become worse in cold weather, in damp places and presence of melting snow.
- Better especially in warm and dry weather and during summer seasons.
Bryonia Alb
- It is best especially for those who are irritable and experience tearing and stitching type of pain that worsen after moving.
- Brest pain along with a sensation of heat in breasts.
- Hardening of the breast.
- Pain in the breasts during periods
- Abscess in the breast
- Milk fever.
- Symptoms become worse specifically in morning, hot weather and after eating.
- Better after resting, on lying down on painful side, and with application of pressure.
Silicea terra
- It suit especially for people who experience pus formation.
- They are extremely sensitive to cold, which worsen in winter season.
- It helps reduce lactating issues by healing sore nipples and insufficient milk production.
- Nipples drawn inwards
- Ulcers on nipples
- Fistulous ulcers on breast
- Blood containing discharge from the vagina every time the child nurse.
- Hard lumps in breast.
- Symptoms become worse in morning, during menstruation, after lying on the left side, in presence of cold weather. On the other hand, Better in the presence of in warm and wet weather, after wrapping one’s head.
Thyroidinum:
- It suit for people with pale skin tone.
- It helps reduce problem during lactation by treating inadequate milk production.
- Fibroid and other tumours in the breast.
- Vomiting during pregnancy
- Fibroids in the uterus
- Increased weakness
- Fatigue with a tendency to faint.[2][6]
Diet & Regimen
Diet & Regimen
- Satisfy the urges of drinking and eating foods of your desire without any hesitation.
- Set the room temperature and select your clothing as pr your comfort.
- Do not over exert your mind.
- Do not get emotionally excited.[6]
Do’s and Don'ts
The Do’s and Don’ts
Do:
Nurse frequently:
- Let your baby set the feeding schedule. Frequent nursing helps establish your milk supply.
Offer both breasts at each feeding:
- This ensures your baby gets both foremilk (thinner, thirst-quenching milk) and hindmilk (richer, fattier milk).
Seek support:
- Attend La Leche League meetings or consult with a lactation consultant if you have any questions or concerns.
Trust your instincts:
- You know your baby best. Listen to your intuition when it comes to feeding and caring for your little one. [7]
Ensure a good latch:
- A proper latch is crucial for comfortable and effective breastfeeding.
Pay attention to your baby’s cues:
- Learn to recognize your baby’s hunger signs and offer the breast promptly.
Take care of yourself:
- Eat a healthy diet, get enough rest, and manage stress to support milk production.[8]
Don’ts:
Introduce bottles or pacifiers too early:
- These can interfere with breastfeeding and may lead to nipple confusion.
Limit feeding time:
- Let your baby nurse until they are satisfied. Restricting feeding time can negatively impact milk supply.
Give up easily:
- Breastfeeding can have challenges, but with support and perseverance, most mothers can successfully breastfeed. [7]
Supplement with formula unnecessarily:
Unless medically necessary, avoid supplementing with formula, as it can decrease your milk supply.
Compare yourself to other mothers:
- Every breastfeeding journey is unique. Focus on your and your baby’s needs.
Ignore pain:
- If you experience nipple pain, seek help from a lactation consultant to correct any latch issues. [8]
Terminology
Terminology:
General Homeopathic Terms:
- Vital Force: The innate healing energy within each individual, which homeopathy aims to strengthen and balance.
- Law of Similars (Similia Similibus Curentur): The principle that "like cures like." This means a substance that causes symptoms in a healthy person can cure similar symptoms in a sick person when given in a highly diluted form.
- Provings: Controlled experiments where healthy volunteers take a substance and record their physical, mental, and emotional symptoms to understand its potential therapeutic effects.
- Repertory: An extensive index of symptoms cross-referenced with homeopathic remedies that could potentially treat those symptoms.
- Materia Medica: Detailed descriptions of the therapeutic properties and effects of various homeopathic remedies.
- Potency: The level of dilution and succussion (vigorous shaking) a remedy undergoes. Higher potencies are considered more dilute and potent.
- Aggravation: A temporary worsening of symptoms after taking a remedy, often seen as a positive sign that the remedy is working to stimulate healing.
- Constitutional Remedy: A remedy chosen based on the individual’s overall physical and mental makeup, aiming to address the root cause of their health concerns.
Breastfeeding-Specific Homeopathic Terms:
- Galactagogue: A substance used to increase breast milk production. In homeopathy, several remedies are considered galactagogues.
- Mastitis: Inflammation of the breast tissue, often accompanied by pain, redness, and swelling.
- Engorgement: Overfullness of the breasts with milk, which can cause discomfort and pain.
- Sore Nipples: A common issue for breastfeeding mothers, often caused by incorrect latch or positioning.
- Thrush: A fungal infection that can affect the nipples and baby’s mouth, causing pain and discomfort.
- Low Milk Supply: Insufficient milk production.
Additional Terms Relevant to Homeopathic Breastfeeding Support:
- Letdown Reflex: The release of milk from the breast during breastfeeding.
- Nipple Blebs: Small white spots or blisters on the nipple, which can be painful.
- Cracked Nipples: Fissures or cracks in the nipple skin, often caused by dryness or poor latch.
- Inverted Nipples: Nipples that retract inward instead of protruding.
Important Considerations:
- Homeopathic remedies are highly individualized, and the specific remedy chosen will depend on the mother’s unique symptoms and overall constitution.
- It is always best to consult with a qualified homeopathic practitioner for proper assessment and personalized treatment recommendations.
- Homeopathy can be used alongside conventional medical care to support breastfeeding and address any challenges that may arise.
References
References
- Paediatrics (8th Edition) -O.P. Ghai-
- Therapeutics from Zomeo Ultimate LAN
- https://www.who.int/health-topics/breastfeeding#tab=tab_1
- https://www.cdc.gov/nccdphp/dnpao/features/breastfeeding-benefits/index.html
- https://www.verywellfamily.com/whats-in-breast-milk-4047820
- https://www.myupchar.com/en/motherhood/common-breastfeeding-problems-and-solutions-in-hindi/homeopathy
- The Womanly Art of Breastfeeding by La Leche League International (8th Edition, 2010)
- Breastfeeding Made Simple by Nancy Mohrbacher and Kathleen Kendall-Tackett (3rd Edition, 2010).
Also Search As
Breastfeeding Also Search As
There are many ways people can search for information on breastfeeding:
Online Search Engines:
Google: The most common way to search. Typing "breastfeeding" will bring up numerous articles, websites, and resources.
Bing, DuckDuckGo, etc.: Other search engines can also provide relevant results.
Health Websites:
World Health Organization (WHO): A reliable source for evidence-based information on breastfeeding recommendations and benefits.
HealthyChildren.org (American Academy of Pediatrics): Provides comprehensive information on breastfeeding for parents.
La Leche League International: A global organization dedicated to supporting breastfeeding mothers.
Medical Databases:
PubMed: A database of scientific articles, including research on breastfeeding.
Google Scholar: Another source for scientific articles on breastfeeding.
Libraries:
Public libraries: May have books and resources on breastfeeding.
University libraries: Often have more in-depth research and journal articles available.
Support Groups:
La Leche League meetings: Offer support and information for breastfeeding mothers.
Online forums and communities: Connect with other breastfeeding mothers and share experiences.
Healthcare Professionals:
Doctors and midwives: Can provide medical advice and answer questions about breastfeeding.
Lactation consultants: Specialists who can help with breastfeeding challenges and provide support.
Tips for Searching:
Use specific keywords: Instead of just "breastfeeding," try searching for specific topics like "breastfeeding positions," "breastfeeding diet," or "breastfeeding and medication."
Check the source’s credibility: Look for information from reputable organizations, healthcare professionals, and peer-reviewed research articles.
Consider the date of publication: Ensure the information is up-to-date and reflects current recommendations.
There are several ways to search for an article on any topic, depending on where the article might be located and what type of information you’re looking for:
General Web Search:
Search Engines (Google, Bing, etc.): The most common method, simply enter keywords related to the article’s topic (e.g., "breastfeeding benefits," "breastfeeding challenges," "breastfeeding history") in the search bar.
Specialized Websites:
Health and Parenting Websites: Many organizations and websites focus on health and parenting topics. Examples include:
- World Health Organization (WHO)
- La Leche League International
- KellyMom
- BabyCenter
- National Institutes of Health (NIH)
Government Websites: Many government health departments and agencies have resources on breastfeeding. Look for websites like the Centers for Disease Control and Prevention (CDC) or your country’s health ministry website.
Academic Databases:
PubMed: A database of scientific articles on health and medicine, including many research papers on breastfeeding.
Google Scholar: Another source for academic articles and research on breastfeeding.
Libraries:
Physical Libraries: Local or university libraries may have books, journals, and other resources on breastfeeding.
Online Libraries: Many libraries offer access to online databases and articles that you can search remotely.
Social Media:
Facebook Groups: Many breastfeeding support groups exist on Facebook where you can ask questions and find articles shared by other members.
Twitter: Follow organizations and experts who share information on breastfeeding.
Tips for Effective Searching:
Use specific keywords: Instead of just searching for "breastfeeding," use more specific terms to narrow down your results.
Combine keywords: Use Boolean operators like AND, OR, and NOT to refine your search. For example, "breastfeeding AND nutrition" will find articles that discuss both topics.
Use quotation marks: Enclosing phrases in quotation marks will search for the exact phrase, rather than individual words.
Check the source: Always evaluate the credibility and reliability of the source before using the information.
Frequently Asked Questions (FAQ)
What is Breastfeeding?
Definition:
Breastfeeding, or nursing, is the process by which human breast milk is fed to a child. Breast milk may from the breast, or may express by hand or pumped and fed to the infant.
How often should I breastfeed my newborn?
Newborns typically need to breastfeed 8-12 times in a 24-hour period. This helps establish your milk supply and ensures your baby gets enough nourishment.
What is the importance of Breastfeeding?
Breastmilk is the ideal food for infants. It is safe, clean and contains antibodies which help protect against many common childhood illnesses. Breastmilk provides all the energy and nutrients that the infant needs for the first months of life, and it continues to provide up to half or more of a child’s nutritional needs during the second half of the first year, and up to one third during the second year of life.
What are 5 advantages of Breastfeeding?
5 Advantages of Breastfeeding:
- Breast milk is the best source of nutrition for most babies
- Breast feeding can help protect babies against some short- and long-term illnesses and diseases
- Breast milk shares antibodies from the mother with her baby
- Mothers can breastfeed anytime and anywhere
- Breast feeding can reduce the mother’s risk of breast and ovarian cancer, type 2 diabetes, and high blood pressure
Is it normal to experience some discomfort while breastfeeding?
Some initial tenderness is common as you and your baby adjust to breastfeeding. However, severe or persistent pain could indicate a latch issue. A lactation consultant can help you get a comfortable and effective latch.
Can homeopathy help with breastfeeding problems?
Yes,
homeopathy can offer gentle and effective support for various breastfeeding challenges like low milk supply, engorgement, mastitis, sore nipples, and difficulties with latching.
Which homeopathic remedies are commonly used for breastfeeding issues?
Some frequently recommended remedies include:
- Pulsatilla: For emotional ups and downs, fluctuating milk supply, and nipple soreness.
- Phytolacca: For mastitis, engorgement, and pain in the breasts.
- Urtica urens: For increasing milk supply.
- Chamomilla: For fussy babies and colicky symptoms.
Always consult with a qualified homeopath for proper remedy selection and dosage.
Is homeopathy safe for breastfeeding mothers and babies?
Yes,
When prescribed by a qualified homeopath, homeopathic remedies are generally considered safe for both mother and baby. The remedies are highly diluted and have no known side effects.
How long does it take to see results with homeopathy for breastfeeding?
The response time varies depending on the individual and the specific issue. Some mothers may experience improvement within a few days, while others may take longer.
How does homeopathy work for breastfeeding?
Homeopathy works by stimulating the body’s natural healing abilities. Remedies are chosen based on the specific symptoms and individual characteristics of the mother and baby.
