Varicose vein
Definition
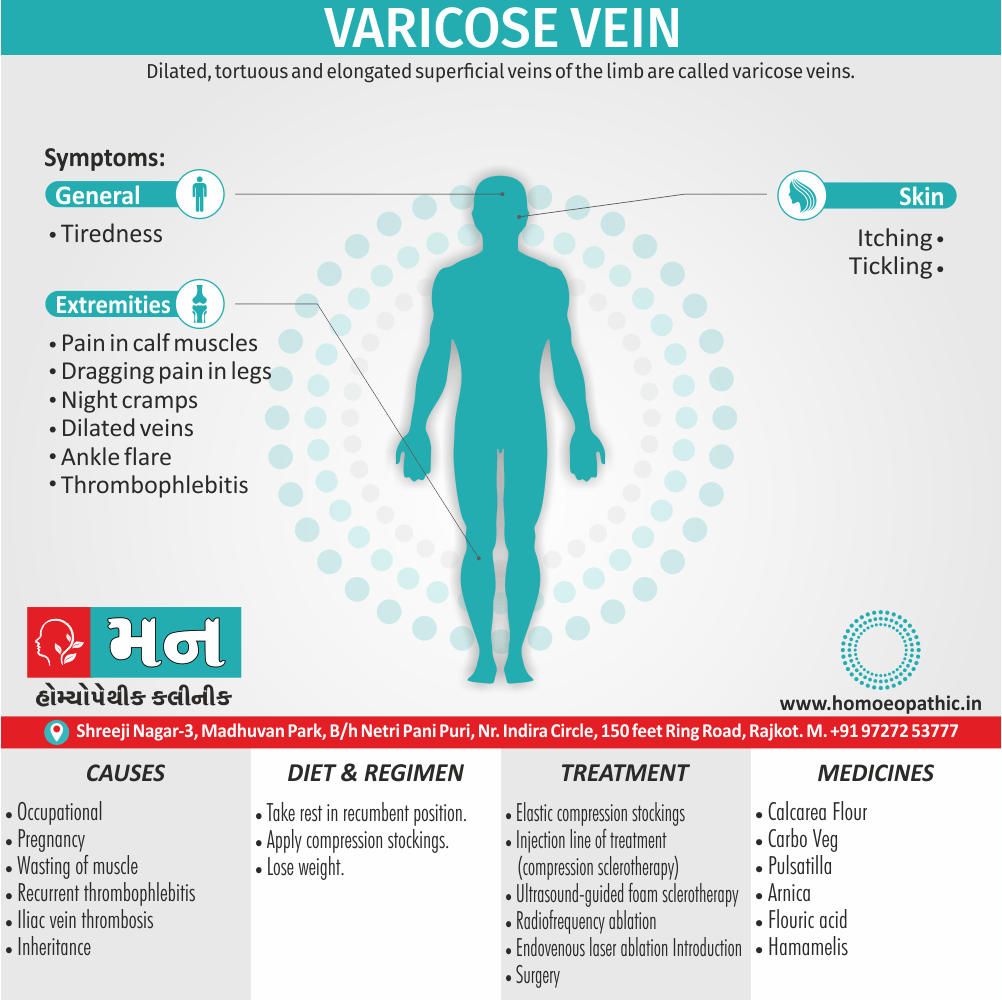
Varicose vein are dilated, tortuous and elongated superficial veins of the limb. [2]
Varicose veins are swollen, twisted veins that often appear blue or dark purple. They happen when faulty valves in the veins allow blood to flow in the wrong direction or to pool.
While there’s no exact synonym for varicose veins, they are sometimes referred to as:
- Varicosities: A medical term for varicose veins.
- Varicose veins disease: This term emphasizes the chronic nature of the condition.
- Venous insufficiency: This refers to the underlying problem of improper blood flow in the veins that causes varicose veins.
- Spider veins: These are smaller, red, purple, or blue blood vessels that can appear near varicose veins.
- Thread veins: Another term for spider veins.
Please note that "varicose veins" is the most commonly used and understood term for this condition.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Varicose vein
- Varicosity is the penalty for verticality against gravity.
- The blood has to flow from the lower limbs into the heart against gravity because of the upright posture of human beings.
- In many cases, varicose veins are asymptomatic.
- Raised intra-abdominal pressure also precipitates varicose veins, more commonly in females due to repeated pregnancy.
- The complications of varicose veins are responsible for hospitalization of the patient. [2]
Epidemiology
Indian epidemiology of Varicose vein
Prevalence:
- A study on Indian railroad workers in 1972 found a prevalence of 25% in southern India and 6.8% in northern India.[6]
- A more recent study in northern India found 46.7% of females and 27.8% of males had varicose veins.[7]
Gender:
- In contrast to Western studies, varicose veins are more common in men in India.
- Studies from Pune and Rohtak found 70% and 64% of patients were men, respectively.[6]
Age:
- A study from Mangalore found the majority of cases (31.2%) were in the age group of 41 to 50 years.[6]
- Another study found age to be a significant risk factor for varicose veins in both sexes.[7]
Occupation:
- A study from Mangalore found the majority of patients (59.4%) were unskilled workers.[6]
Other findings:
- Superficial veins were involved in the majority of cases (72.4%) in a study from Mangalore.[6]
- A study from Banaras Hindu University investigated the role of bacterial infection in varicose veins. [6]
Causes
Causes of Varicose vein
Varicosities are more common in lower limb because of erect posture and long column of blood has to be supported which can lead to weakness and incompetency of valves.
1.Primary varicosities due to i.e.:
- Congenital either incompetence or absence of valves.
- Weakness or wasting of muscles: defective connective tissue also smooth muscle in the venous wall.
- Stretching of deep fascia.
- Inheritance (family history) with FOXC2 gene.
- Klippel – Trenaunay syndrome.
2. Secondary varicosities i.e.:
- Recurrent thrombophlebitis,
- Occupational – standing for long hours (e.g. traffic police, guards).
- Obstruction to venous return like abdominal tumours, retroperitoneal fibrosis, lymphadenopathy.
- Pregnancy (due to progesterone hormone).
- AV malformations: Either Congenital or acquired.
- Iliac vein thrombosis. [1]
Types
Classification of Varicose vein
- Long saphenous vein varicosity.
- Short saphenous vein varicosity.
- Varicose veins due to perforator incompetence.
- Thread veins (or dermal flares/telangiectasias/spider
- veins are 0.5 – 1 mm in size): Are small varices in the skin usually around ankle which look like dilated,
- Red or purple network of veins.
- Reticular varices (1-3 mm in size): Are slightly larger
- Varices than thread veins located in subcutaneous region.
- Combinations of any of above.
Small varicose vein is < 3 mm in diameter.
Large varicose vein is > 3 mm in diameter. [1]
Risk Factors
Risk factor of Varicose vein
- Height: Tall individuals suffer more
- Weight: Obesity may weaken vein wall
- Occupation: e.g. Hotel workers, police officers, shopkeepers, tailors
- Side: Left is comparatively affected more than the right
- Age and sex: Not very clear. [2]
Pathogenesis
Pathogenesis of Varicose Veins:
"The primary pathophysiologic event in the development of primary varicose veins is venous valvular insufficiency, which allows for retrograde (reversed) venous flow and subsequent venous hypertension. Elevated ambulatory venous pressures cause progressive venous dilatation." (Rutherford’s Vascular Surgery, 9th Edition, 2014)
Explanation:
- Valvular Insufficiency: The valves in the veins are designed to ensure one-way blood flow back to the heart. In varicose veins, these valves become weak or damaged, allowing blood to flow backward (retrograde flow).
- Venous Hypertension: This retrograde flow causes blood to pool in the veins, increasing pressure within them (venous hypertension).
- Venous Dilatation: The sustained increased pressure causes the vein walls to stretch and become dilated, leading to the characteristic bulging appearance of varicose veins.
Additional Factors (not directly from the reference):
- Genetic Predisposition: Family history is a strong risk factor.
- Hormonal Factors: Pregnancy and hormonal changes can contribute.
- Lifestyle Factors: Prolonged standing, obesity, and lack of exercise can increase risk.
- Age: Vein walls weaken with age.[8]
Pathophysiology
Pathophysiology of Varicose vein
- Generally, Incompetence of venous valves causes stasis of blood.
- Furthermore, Chronic ambulatory venous hypertension causes defective microcirculation.
- So, RBC diffuses into tissue planes also lysis of RBC’s start.
- This leads to release of haemosiderin.
- It leads to Pigmentation, Dermatitis also Capillary endothelial
- Results in to Prevention of diffusion also exchange of nutrients causes severe
- Lastly, It leads to chronic venous ulceration.
Clinical Features
Clinical Features
"The clinical manifestations of chronic venous insufficiency and varicose veins vary depending on the severity of the venous reflux and hypertension.
The most common symptoms include aching, heaviness, fatigue, and swelling, which typically worsen with prolonged standing and improve with leg elevation.
Other symptoms include throbbing, burning, muscle cramps, and restless legs.
Patients may also present with telangiectasias, reticular veins, varicose veins, edema, skin changes, and ulceration.
The physical examination should include inspection of the skin for the presence of telangiectasias, reticular veins, and varicose veins; palpation of the legs for the presence of edema, tenderness, and pulses; and assessment for the presence of venous reflux by the Brodie-Trendelenburg test or duplex ultrasonography." (Rutherford’s Vascular Surgery, 9th Edition, 2014)
Explanation of Clinical Features:
Symptoms:
- Aching, heaviness, fatigue, swelling
- Throbbing, burning, muscle cramps, restless legs
Signs:
- Telangiectasias (spider veins)
- Reticular veins (small, bluish veins)
- Varicose veins (enlarged, twisted veins)
- Edema (swelling)
- Skin changes (pigmentation, eczema, lipodermatosclerosis)
- Ulceration (in advanced cases)[8].
Sign & Symptoms
Sign & Symptoms of Varicose vein
Symptoms:
- Majority of the patients present with dilated veins in the leg.
- They are minimal to start with and at the end of the day they are sufficiently large because of the venous engorgement.
- Dragging pain in the leg or dull ache is due to heaviness.
- Night cramps occur due to change in the diameter of veins.
- Aching pain is relieved at night on taking rest or elevation of limbs.
- Sudden pain in the calf region with fever and Oedema on the ankle region suggests deep vein thrombosis.
- Patients can present with ulceration, eczema, dermatitis and bleeding.
- Symptoms of pruritus/itching and skin thickening. [2]
Signs:
Inspection (should be done in standing position)
- Dilated veins are present in the medial aspect of leg and the knee. Sometimes they are visible in the thigh also.
- Single dilated varix at SF junction is called saphenous varix. It is due to saccular dilatation of the upper end of long saphenous vein at the saphenous opening.
- Veins are tortuous and dilated.
- A localized, dilated segment of the vein, if present, is an indication of a blowout. It signifies underlying perforator.
- Ankle flare is a group of veins near the medial malleolus.
- Complications such as ulceration, bleeding, eczema and dermatitis may be present.
- Healed scar indicates previous ulceration.
- Look at the popliteal fossa region also.
Palpation
- First palpate along the whole length of vein. Look for tenderness. If present, it indicates thrombophlebitis.
- Vein which is thrombosed will feel as a firm/hard nodule. [2]
Clinical Examination
Clinical / Physical Examination For Varicose vein
Cough impulse test (Morrissey’s test):
- This test should be done in the standing position.
- The examiner keeps the finger at SF junction and asks the patient to cough.
- Fluid thrill, an impulse felt by the fingers, is indicative of ‘saphenofemoral incompetence’.
Trendelenburg test:
- This test is done in 2 parts.
Method:
- The patient is asked to lie on the couch in the supine position.
- The leg is elevated above the level of heart and the vein emptied.
- SF junction is occluded with the help of the thumb (or a tourniquet) and the patient is asked to stand.
Trendelenburg I i.e.:
- Release the thumb or tourniquet immediately.
- Rapid gush of blood from above downwards indicates saphenofemoral incompetence.
Trendelenburg II i.e.:
- The pressure at the SF junction is maintained without releasing the thumb or tourniquet.
- The patient is then asked to stand.
- Slow filling of the long saphenous is seen. It is due to per/orator incompetence (retrograde flow of blood).
Multiple Tourniquet test:
- It is done to find out exact site of perforators
Method i.e.:
- The patient is asked to lie supine on the couch.
- The vein is emptied by elevation.
- As the name suggest 3-5 tourniquets (multiple) can be applied.
- However, more tourniquets are applied, the exact localization c the perforators can be made out but it is not practical.
- There are mainly ankle, knee and thigh perforatons.
- Hence, four tourniquets can be applied at various level as mentioned below.
- 1st Tourniquet: At the level of saphenofemoral junction (SF junction).
- 2nd Tourniquet: At the level of middle of the thigh, t, occlude perforator in the Hunter’s canal.
- 3rd Tourniquet: Just below the knee.
- 4th Tourniquet: Palm breadth (lower third of the leg above medial malleolus/ankle.
- Ask the patient to stand and observe appearance of veins
Inference i.e.:
- Appearance of veins between first and second tourniquets indicates incompetence of thigh perforators between second and third indicates incompetence of knee, perforators and below the fourth tourniquet indicates incompetence of ankle perforators.
- Most commonly, below knee and ankle perforators are incompetent.
- On releasing the tourniquets one by one from be upwards, sudden retrograde filling of the veins occurs.
Schwartz test:
- It is done with the patient in the standing position.
- Place the fingers of the left hand over a dilated segment of the vein and with the right index finger tap the vein below.
- A palpable impulse suggests a superficial column of blood in the vein and it also suggests incompetence of the valves in between the segment of the vein.
Modified Perthes’ test:
- It done to rule out deep vein thrombosis.
- The patient ask to stand, the tourniquet is applied at SF junction and he ask to have a brisk walk.
Inference i.e.:
- If the patient complains of severe pain in calf region or if superficial veins become more prominent, it is an indication of deep vein thrombosis and is a contraindication for surgery.
Fegan’s method (test):
- It done to detect the site of perforators.
- The patient ask to stand. The varicosity is marked with methylene blue and he is asked to lie down.
- The leg elevate to empty the vein and the vein palpate throughout its course.
- The defects in the deep fascia have a circular, buttonhole consistency. [2]
Diagnosis
Diagnosis
"The diagnosis of varicose veins is primarily clinical and is based on the patient’s history and physical examination findings. Duplex ultrasonography is the most commonly used imaging modality to confirm the diagnosis of varicose veins and to assess the severity of venous reflux." (Rutherford’s Vascular Surgery, 9th Edition, 2014)
Explanation of Diagnostic Process:
Clinical Assessment:
- History: Detailed patient history focusing on symptoms like aching, heaviness, swelling, etc., and any risk factors.
- Physical Examination: Visual inspection for the presence of telangiectasias, reticular veins, and varicose veins. Palpation to assess for edema and tenderness.
Duplex Ultrasonography:
- Confirms Diagnosis: Visualizes the veins and assesses blood flow direction to confirm the presence of venous reflux (backward blood flow), which is the hallmark of varicose veins.
- Assesses Severity: Determines the extent of reflux and helps identify the source of the problem (e.g., saphenofemoral junction incompetence).
- Guides Treatment: Helps in planning appropriate treatment options.
Additional Points (not directly from the reference):
Other Imaging Modalities:
- Venography: May be used in complex cases or when duplex ultrasonography is inconclusive.
- Magnetic Resonance Venography (MRV): Can provide detailed images of the venous system, but is less commonly used for initial diagnosis.[8]
Differential Diagnosis
Differential Diagnosis of Varicose vein
- Lymphoedema
- A-V malformation
- Orthostatic Oedema
- Renal and cardiac disease
- Hepatic causes
- Vasculitis
- Metabolic diseases like gout, myxedema, and morbid obesity
- Chronic infections like tuberculosis, syphilis. [1]
Complications
Complications
"Although varicose veins are often considered a cosmetic problem, they can be associated with a number of significant complications, including superficial thrombophlebitis, hemorrhage, skin changes, and venous ulceration. (Rutherford’s Vascular Surgery, 9th Edition, 2014)
Superficial Thrombophlebitis:
- Inflammation of a superficial vein due to blood clot formation.
- Presents with pain, redness, and tenderness along the affected vein.
- Usually self-limiting, but can occasionally extend into deeper veins (deep vein thrombosis), which is a serious condition.
Hemorrhage:
- Bleeding from a varicose vein, usually due to minor trauma.
- Can be significant and alarming, but is usually easily controlled with direct pressure.
Skin Changes:
- Chronic venous insufficiency can lead to various skin changes, including:
- Pigmentation (brownish discoloration)
- Eczema (itchy, inflamed skin)
- Lipodermatosclerosis (hardening and thickening of the skin)
- Atrophie blanche (white, scarred patches)
Venous Ulceration:
- The most serious complication of varicose veins.
- Open sores that develop on the lower leg, usually near the ankle.
- Can be painful, slow to heal, and prone to infection.
Additional Points (not directly from the reference):
Deep Vein Thrombosis (DVT): Although less common, DVT can occur in association with varicose veins. It’s a serious condition that requires prompt medical attention.
Pulmonary Embolism (PE): A potentially life-threatening complication of DVT, where a blood clot travels to the lungs.[8]
Investigations
Investigation
Hand held Doppler i.e.:
- It is the first, mm1mum level investigation to do before treating a patient with venous disease.
- When the blood flows, the wave emits a signal – the Doppler signal.
- If there is SF incompetence, fo1ward and backward flow can detect.
- Biphasic signal: Gently squeeze calf muscles and the flow can assess by Doppler probe in the SF junction.
- It can also pick up accessory long saphenous vein in the groin.
- It is not an investigation to identify the perforators.
Duplex ultrasound imaging i.e.:
- In this investigation high resolution B-mode ultrasound imaging and Doppler ultrasound use.
- It helps in getting images of veins, measure flow in all lower limb veins.
- Origin of venous ulcers and varicose veins can also assess.
Venography i.e.:
- Both ascending and descending venography can done in a case of deep vein thrombosis.
- It is an invasive procedure and risk of spreading infection and septicemia is present.
- Duplex ultrasonography has largely replaced this investigation (rarely done now).
- Varicography refers to injecting contrast into surface veins (indicated in recurrent varicose veins).
- It can follow by sclerosant injections.
Plethysmography i.e.:
- They base on measurement of volume changes in the leg.
- By placing a light-emitting diode above medial malleolus and patient performing tiptoe movements, venous recovery time can measure.
- This call phot plethysmography (PPT). [2]
Treatment
Treatment
Elastic compression stockings:
- Elastic compression bandage and elevation of leg.
- It forming the fundamental steps in treating varicose veins.
- This can advise in asymptomatic cases of varicose veins and 1r secondary varicose veins.
- Usually, 20-30 mmHg stockings are sufficient.
- It should worn from ankle to below knee.
- It should worn during working hours (entire day).
- Should remove while lying down but legs should be kept elevated.
- Unna boot i.e.: It is a three-layered dressing.
- Inner layer i.e.: It contains roller gauze bandage impregnated with calamine, zinc, glycerine, etc. with graded compression.
- Middle layer i.e.: 4" wide continuous gauze dressing
- Outer layer i.e.: Elastic wrap with graded compression.
- Pneumatic compression devices not commonly used.
Injection line of treatment (compression sclerotherapy)
Indications
- Basically, Below knee varicosity.
- Moreover, Recurrent varicosity after surgery.
- Varicose veins mark in the standing position.
- The veins puncture with a needle attached to a syringe containing sclerosant agent also the patient ask to lie down.
- 3% sodium tetradecyl sulphate or 1-2 ml of ethanolamine oleate or hypertonic saline inject into the column of vein.
- Aseptic thrombosis occurs also when fibrosis occurs, the vein shrinks.
- Tight elastic compression bandage apply.
- Success of sclerotherapy depends upon effective sclerosant, injection into an empty vein and compression followed especially by exercise.
Ultrasound-guided foam sclerotherapy.
- It is popular in a few centers in the UK only.
- Foam sclerosant C (Polidocanol) use. It prepare specifically by air mixing technique with sclerosant.
- It inject into veins (superficial) under ultrasound guidance.
- LSV should compress in the upper thigh to prevent foam from entering into femoral vein.
- Elevate the leg to prevent foam from entering into calf veins.
Endovenous laser ablation (EVLA) Introduction:
- It is a minimally invasive, outpatient procedure using laser fibre to ablate varicose veins.
- This gives excellent cosmetic and functional results.
Radiofrequency ablation (RFA):
- It is also a minimally invasive technique of ablation of the veins by using a two minds catheter at a temperature of 85- 1200C, using a power of2-4 W.
- The position of the patient, accurate marking of the veins, tumescent anaesthesia, are similar to that of EVLA.
- However, the vein cannulate with a 7F sheath and catheter is not positioning within 2 cm of the SF junction.
- Segment of the vein over 7 cm long can ablate.
- Complications include thrombophlebitis, pain, skin bums
Surgery:
- Trendelenburg’s operation:
- An inguinal incision made, long saphenous vein identified and the 3 tributaries ligate.
- Long saphenous vein ligate close to the femoral vein juxta femoral flush ligation.
- Sub fascial ligation of Cockett and Dodd
- In this operation, the perforators identify deep to deep fascia and ligate subfascially.
- This indicate in cases of perforator incompetence with saphenofemoral competence.
- This can also done using an endoscope.
- Sub fascial endoscopic perforator surgery (SEPS) :
- Small port incisions make in the skin of calf region, deepened through the fascia.
- Carbon dioxide insufflation done.
- A balloon expander may also use to distend the sub fascial plane.
- 2-6 perforators identify and ligate.
- The procedure is simple, quick with least morbidity and is becoming popular.
- Indicated for below knee perforators. [2]
Prevention
Prevention
- Patients with normal deep veins should offer treatment to obliterate any sites of saphenous or perforator reflux.
- Elastic stockings should prescribe for all patients with evidence of post-thrombotic deep vein damage and these remain an alternative treatment for patients with superficial venous disease who decline intervention. [3]
Homeopathic Treatment
Homeopathic Treatment
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Varicose vein:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
Calcarea Flouricum
- This tissue salt relaxes the Elastic Fibers, especially of veins and glands.
- Glands enlarge also Become Stony Hard.
- Veins dilated also become varicose, inflamed.
- Weakness, in the morning.
- Besides this, Feeling of fatigue all day.
- Aggravation at beginning of motion, whereas Amelioration by continue motion. [4]
Hamamelis Verginica:
- Venous congestion.
- Varicose veins with bruised soreness of affected parts.
- Furthermore, Acts upon the coats of veins causing relaxation with consequent engorgement.
- Tired feeling especially in legs.
- Chilliness in back also hips, extending down legs.
- Bleeding veins. [5]
Pulsatilla:
- Drawing, tensive pains in thighs also legs, with restlessness, sleeplessness and chilliness.
- Pain in limbs, shifting rapidly.
- Tensive pain, letting up with a snap.
- Suffering worse specifically from letting the affected limb hang down.
- Legs feel heavy also weary.
- Lastly, Feet red, inflamed, swollen. [5]
Carbo vegetablis:
- Disintegration also imperfect oxidation.
- Body becomes blue, icy-cold.
- Venous congestions. Heavy, stiff, feel paralyzed; limbs go to sleep; additionally want of muscular energy, joints weak.
- Cold from knees down.
- Toes red, swollen, burning pains in bones also limbs.
- Cramps in soles, feet numb also sweaty. [5]
Flouricum Acidum:
- Varicose veins.
- Distended blood vessels.
- Complaint of old age, feel weak.
- Ulcers; additionally red edges and vesicles. [5]
- Generally, Limbs and body ache as if beaten; joints as if sprained.
- Relaxed blood vessels, black also blue spots.
- Tendency to tissue degeneration. sore, unimpressive, bruised feeling. Pain in back also limbs.
- Soreness after overexertion. Great fear of being either touched or approached. [5]
- Tingling and itching which moves from place to place; In detail, after scratching,
- Besides this, Itching begins somewhere else.
- All in all, Blood vessels are relaxed, causing ecchymosis, blue-black spots; with tendency to hemorrhage; epistaxis.[4]
Diet & Regimen
Diet & Regimen
for Varicose Veins
Diet
The goal is to promote healthy circulation and reduce inflammation:
Fiber Power: Fiber helps prevent constipation, which can strain veins in the legs. Excellent sources include:
- Oats
- Beans and lentils
- Whole grains (brown rice, quinoa)
- Fruits and vegetables (especially berries, apples, and broccoli)
Flavonoid Boost: These compounds strengthen vein walls and improve blood flow. Find them in:
- Berries (blueberries, strawberries, raspberries)
- Cherries
- Citrus fruits
- Onions
- Garlic
Vitamin C: Essential for collagen production, which keeps veins strong and elastic. Good sources are:
- Citrus fruits (oranges, grapefruits, lemons)
- Bell peppers
- Strawberries
- Kale and spinach
Water, Water, Water: Hydration is key for healthy blood flow. Drink plenty of:
- Water
- Herbal teas
Foods to Limit:
- Processed foods: High in sodium and unhealthy fats, which can worsen inflammation.
- Sugary drinks and snacks: Contribute to poor vein health.
- Excessive alcohol: Can dehydrate you and weaken veins.
- Excess salt: Can cause water retention and increase pressure on veins.
Regimen for Varicose Veins
- Move Your Body: Regular exercise, like walking, swimming, or cycling, improves circulation and strengthens calf muscles, which act as pumps for your veins.
- Elevate Your Legs: When resting, elevate your legs above your heart to encourage blood flow back towards your heart.
- Compression Therapy: Wearing compression stockings provides support to your veins and helps prevent blood from pooling.
- Maintain a Healthy Weight: Excess weight puts extra pressure on your veins.
- Avoid Prolonged Standing or Sitting: If your job requires it, take breaks to move around and stretch your legs.
- Hydrotherapy: Alternating between warm and cool water in the shower can stimulate blood circulation
Do’s and Don'ts
Do’s and Don’ts
Varicose Veins do’s & don’ts
Do’s:
- Exercise Regularly: Engage in activities that promote leg muscle activity, like walking, swimming, and cycling. This helps improve blood circulation and reduce venous pressure.
- Maintain a Healthy Weight: Excess weight puts additional pressure on your veins. Aim for a healthy weight through a balanced diet and regular exercise.
- Elevate Your Legs: Whenever possible, elevate your legs above heart level to encourage blood flow back to the heart and reduce swelling.
- Wear Compression Stockings: These specialized stockings provide graduated compression, helping to improve blood flow and reduce symptoms.
- Eat a Healthy Diet: Focus on foods rich in fiber and antioxidants, which can help improve circulation and vein health.
- Stay Hydrated: Adequate fluid intake helps maintain blood volume and prevents blood from becoming too thick, which can worsen circulation.
- See a Doctor: If you notice any signs of varicose veins or experience discomfort, consult a doctor for proper diagnosis and treatment options.
Don’ts:
- Sit or Stand for Long Periods: Prolonged periods of inactivity can worsen blood flow and increase pressure on your veins. Take breaks and move around frequently.
- Cross Your Legs: Crossing your legs can restrict blood flow and increase pressure on your veins. Try to avoid this position, especially for extended periods.
- Wear Tight Clothing: Tight clothing, especially around the waist or legs, can impede blood flow and contribute to venous problems.
- Wear High Heels: High heels can shorten calf muscles and impair blood circulation. Opt for comfortable shoes with low heels.
- Ignore Signs of Vein-Related Problems: If you experience symptoms like leg pain, swelling, or skin changes, seek medical evaluation. Early detection and treatment can prevent complications.
- Smoke: Smoking damages blood vessels and increases the risk of circulatory problems, including varicose veins.
Additional Tips:
- Consider Dietary Changes: Some studies suggest that certain foods, like flavonoids and vitamin C-rich foods, may help improve vein health.
- Avoid Hot Baths and Saunas: Excessive heat can dilate blood vessels and worsen varicose veins.
- Practice Good Posture: Maintaining good posture helps optimize blood flow and reduces strain on your veins.
Terminology
Terminology
1. Varicose Veins:
- Meaning: Enlarged, twisted veins that usually appear blue or dark purple. They most commonly occur in the legs and feet.
2. Chronic Venous Insufficiency (CVI):
- Meaning: A condition where the veins are unable to pump blood back to the heart efficiently, leading to blood pooling in the legs. Varicose veins are a common manifestation of CVI.
3. Venous Reflux:
- Meaning: The backward flow of blood in the veins, caused by weakened or damaged valves. This is a key factor in the development of varicose veins.
4. Venous Hypertension:
- Meaning: Increased pressure within the veins, often caused by venous reflux. This can lead to various symptoms and complications.
5. Telangiectasias (Spider Veins):
- Meaning: Tiny, red or blue blood vessels that appear close to the skin’s surface. They are often associated with varicose veins.
6. Reticular Veins:
- Meaning: Small, bluish veins that are larger than telangiectasias but smaller than varicose veins.
7. Edema:
- Meaning: Swelling caused by fluid retention in the tissues. It is a common symptom of varicose veins and CVI.
8. Lipodermatosclerosis:
- Meaning: Hardening and thickening of the skin, often associated with advanced CVI.
9. Venous Ulceration:
- Meaning: Open sores that develop on the lower leg, usually near the ankle, due to poor circulation.
10. Duplex Ultrasonography:
- Meaning: An imaging technique used to visualize the veins and assess blood flow. It is crucial for diagnosing varicose veins and evaluating the severity of venous reflux.
11. Sclerotherapy:
- Meaning: A treatment that involves injecting a solution into the vein to close it off.
12. Endovenous Ablation:
- Meaning: A minimally invasive procedure that uses heat or radiofrequency energy to close off the affected vein.
13. Vein Stripping:
- Meaning: A surgical procedure to remove the affected vein.
References
References
- SRB’S manual of surgery 3rd edition
- Manipal manual of surgery 4th edition
- Bailey and Love short practice of surgery 25th edition
- Materia medica of homoeopathic medicine by DR. S.R.Phatak.
- Homoeopathic Body-System Prescribing – A Practical Workbook of Sector Remedies by Isaac Golden.
- Venous Scenario in India | Indian Journal of Surgery – SpringerLink, 2021.
- Prevalence and risk factors of varicose veins, skin trophic changes, and venous symptoms among northern Indian population.
- Rutherford’s Vascular Surgery, 9th Edition, Jack L. Cronenwett, K. Wayne Johnston, 2014, Elsevier Saunders.
Also Search As
Also search as
Using Search Engines:
Specific Search Terms:
- "homeopathy for varicose veins"
- "homeopathic treatment for varicose veins"
- "homeopathic remedies for varicose veins"
- "varicose veins homeopathic medicine"
- Include additional terms like "symptoms," "causes," "relief," or "cure" for more targeted results.
General Search Terms:
- "varicose veins natural treatment"
- "alternative treatments for varicose veins"
- These broader terms may also surface homeopathic articles alongside other natural or alternative approaches.
Advanced Search Techniques:
- Use quotation marks to search for an exact phrase (e.g., "homeopathic treatment for varicose veins")
- Use the minus sign to exclude certain terms (e.g., varicose veins -surgery)
- Use the site: operator to search within a specific website (e.g., varicose veins site:homoeopathy.dpu.edu.in)
Exploring Homeopathic Websites and Resources:
Homeopathic Organizations and Clinics: Many homeopathic organizations and clinics have websites with articles and resources. Search their websites or blogs using the search bar or browsing through relevant categories.
Homeopathic Journals and Publications: Search online databases for homeopathic journals and publications that may contain articles on varicose veins.
Online Homeopathic Forums and Communities: Participate in online discussions and forums related to homeopathy, and ask for recommendations for articles or resources on varicose veins.
Additional Tips:
Specify the Language: If you’re looking for articles in a specific language (e.g., Hindi or English), include the language in your search query.
Check the Credibility of the Source: Look for articles published by reputable homeopathic organizations, practitioners, or journals. Be wary of information from unverified sources or websites promoting specific products.
Consult a Homeopathic Practitioner: If you have varicose veins and are considering homeopathic treatment, consult a qualified homeopathic practitioner for personalized advice and guidance.
Frequently Asked Questions (FAQ)
What is Varicose vein?
Definition
Varicose vein are dilated, tortuous and elongated superficial veins of the limb.
What causes Varicose vein?
- Congenital incompetence or absence of valves.
- Weakness or wasting of muscles
- Stretching of deep fascia.
- Inheritance (family history)
- Klippel – Trenaunay syndrome
- Recurrent thrombophlebitis,
- Occupational
How are varicose veins treated?
Treatment
- Lifestyle changes: Exercise, weight management, elevation of the legs, and compression stockings.
- Minimally invasive procedures: Sclerotherapy, endovenous laser therapy (EVLT), and radiofrequency ablation (RFA) to close or remove the affected veins.
- Surgery: Vein stripping or ligation to remove larger varicose veins.
What are the symptoms of Varicose vein?
Symptoms
- Dilated veins in the leg
- Dragging pain in the leg or dull ache is due to heaviness.
- Night cramps occur due to change in the diameter of veins
- Aching pain is relieved at night on taking rest or elevation of limbs
Who is at risk of developing varicose veins?
Risk Factors
Age: The risk increases as you get older.
Gender: Women are more likely to develop varicose veins than men.
Can varicose veins be prevented?
- Maintain a healthy weight.
- Exercise regularly to improve circulation.
- Avoid prolonged standing or sitting.
- Elevate your legs when resting.
- Wear compression stockings, especially if you’re at high risk.
What are varicose veins, and how does homeopathy approach their treatment?
- Varicose veins are enlarged, twisted veins commonly appearing in the legs. Homeopathy views them as a manifestation of an underlying imbalance within the body, aiming to treat not only the visible veins but also the root cause for long-term relief.
Can homeopathy cure varicose veins completely?
Homeopathy offers a holistic approach to varicose veins, aiming to stimulate the body’s self-healing mechanisms. While complete cure depends on individual cases, homeopathy can significantly improve symptoms, reduce the appearance of veins, and prevent complications.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Varicose vein?
Homoeopathic medicines for varicose vein
- Calcarea Flouricum
- Hamamelis Verginica
- Pulsatilla
- Carbo vegetablis
- Flouricum Acidum
- Arnica
