Lipoma
Definition
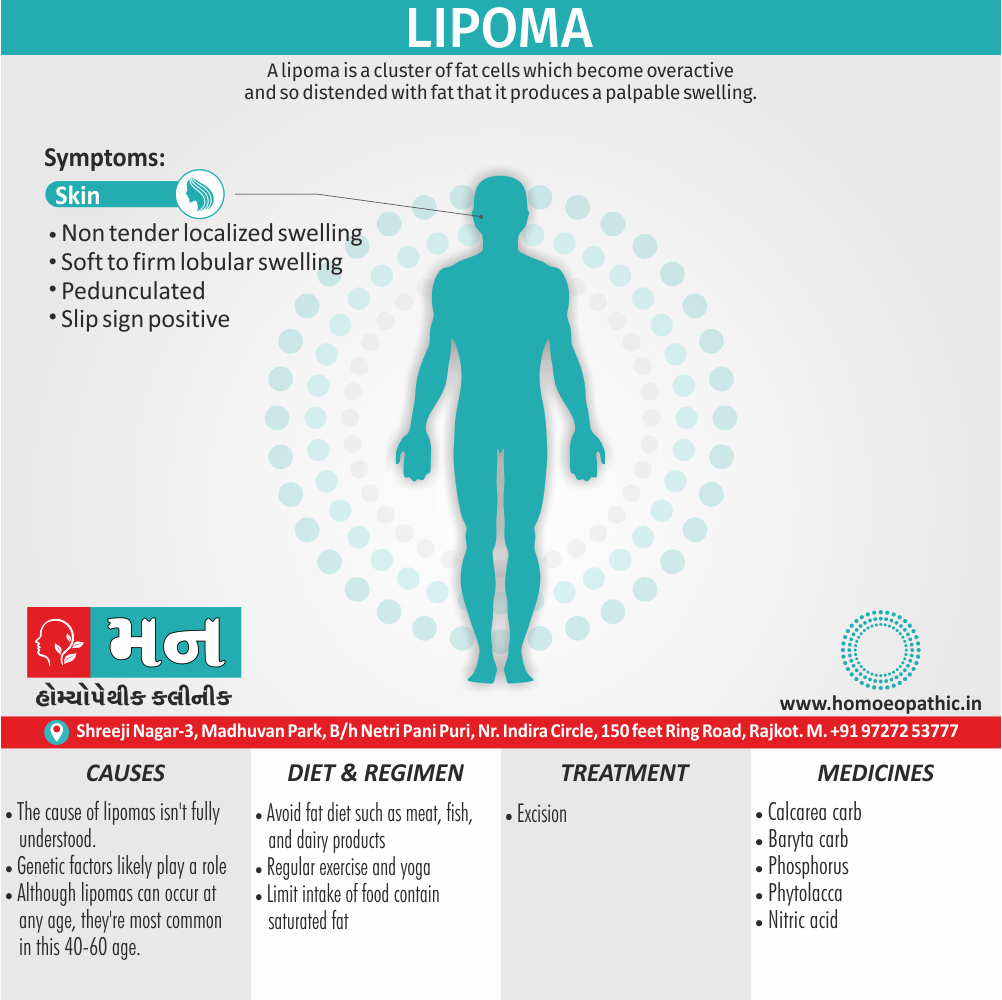
A lipoma is a cluster of fat cells which become overactive and so distended with fat that it produces a palpable swelling. [3]
There aren’t any true synonyms for lipoma in the sense of another word that medically means exactly the same thing. However, there are a couple of related terms you might encounter:
- Lipomatosis: This is a condition where there are multiple lipomas throughout the body.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
- Generally, Lipoma is a benign tumour arising from fat cells of adult type. [3]
- Tumour arising from brown fat call as hibernoma (specifically reddish brown).
- It call as universal tumour (especially ubiquitous tumour) as it can occur anywhere in the body (except in brain).
- It is the commonest benign tumour.
- It can either diffuse or localize.
- Furthermore, Diffuse lipomas are not encapsulated, not well localized.
- Common in palm, sole, head also neck region, difficult to remove.
- It seen in subcutaneous also intermuscular tissues.
- It can either single or multiple (5%). Multiple lipomas often associated with many syndromes like MEN syndrome (in other words, Multiple endocrine neoplasia syndrome) [2]
- Besides this, It may occur at any age, but it rarely seen in children.
- It is a painless.
- It is usually small but it may attain very big size.
- All in all, It is a freely mobile swelling over the deeper structures.[1]
Epidemiology
Epidemiology of Lipoma
The prevalence of lipomas has been cited as affecting 1% of the population, while its incidence, which is possibly underreported, is 2.1 per 1000 individuals per year. (Lipoma Pathology – StatPearls – NCBI Bookshelf, 2023)
Regarding studies specifically focused on the Indian population, one study found:
- 23 cases of oral lipomas (14 males and 9 females) over 12 years (2005-2017) at a dental college in Jaipur.
- Only 49 published cases of oral lipoma in the Indian population from 1976-2017. (Prevalence of oral lipomas in Indian population: An institutional retrospective study of 12 years and analysis of 49 published cases from 1976 – 2017 reported in Indian patients – Electronic Journal of General Medicine, 2018)[6].
It’s important to note that this study focused on oral lipomas, which are rarer than lipomas in general. More comprehensive epidemiological studies on lipomas across the entire Indian population are needed to provide a more accurate picture.
Causes
Causes
- The cause of lipomas isn’t fully understood.
- They tend to run in families, so genetic factors likely play a role in their development. [4]
Types
Classification of Lipoma
Single encapsulated:
- This is a single, soft, slow-growing, painless and semi fluctuant swelling.
- The swelling is soft, may feel cystic with fluctuation.
- This is also called pseudo fluctuation.
- Commonly present as a subcutaneous swelling.
- It is freely mobile.
- The flank is the commonest site.
- Dimpling sign: Fibrous bands connect a lipoma to the skin.
- When the skin moved, a dimple appears on the skin
Multiple lipomatosis
- Such lipomas are multiple and very often tender because of nerve elements mixed with them.
- Hence, they are called multiple neurolipomatosis.
- Dercum s disease is one example of this variety (Adiposis dolorosa) wherein tender, lipomatous swellings are present in the body, mainly the trunk.
Uncapsulated (diffuse)
- Diffuse variety is a rare type of lipoma.
- It is called pseudo lipoma.
- It is an overgrowth of fat without a capsule.
- Histological types:
Risk Factors
Risk factor:
- Being between 40 and 60 years old: Although lipomas can occur at any age, they’re most common in this age group.
- Genetics: Lipomas tend to run in families. [4]
.
Pathogenesis
Pathogenesis
The exact pathogenesis of lipomas is still unclear. However, several factors and mechanisms have been proposed:
- Genetic Predisposition:
- Chromosomal abnormalities: Rearrangements involving chromosome 12q13-15 (HMGA2 gene) are frequently observed in lipomas.
- Familial cases: Some individuals have a genetic predisposition to developing multiple lipomas (familial multiple lipomatosis).[7]
- Adipocyte Differentiation and Proliferation:
- Increased expression of adipogenic transcription factors (PPARγ, C/EBPα): These factors promote the differentiation of mesenchymal stem cells into adipocytes.
- Dysregulation of signaling pathways (Wnt/β-catenin, Hedgehog): These pathways play a crucial role in adipocyte proliferation and differentiation.[8]
- Other Factors:
It is important to note that the pathogenesis of lipomas is likely multifactorial, with a combination of genetic, molecular, and environmental factors contributing to their development. Further research is needed to fully elucidate the underlying mechanisms.
Pathophysiology
Pathophysiology
The exact pathophysiology of lipomas remains unclear. However, several theories and observations have been proposed:
Monoclonal Origin: Research suggests that lipomas arise from a single precursor cell (monoclonal), meaning all the cells within a lipoma are genetically identical. This is supported by studies showing consistent chromosomal abnormalities in lipoma cells.
Chromosomal Abnormalities: Specific chromosomal translocations, particularly involving chromosome 12, have been frequently observed in lipomas. These translocations can disrupt genes involved in regulating cell growth and differentiation, potentially leading to the uncontrolled growth of fat cells.
HMGA2 Gene: The High Mobility Group AT-hook 2 (HMGA2) gene, often affected by chromosomal translocations in lipomas, plays a crucial role in adipogenesis (fat cell formation). Overexpression of HMGA2 due to these translocations may contribute to the development of lipomas.
Other Genetic Factors: Inherited genetic syndromes like familial multiple lipomatosis indicate a genetic predisposition to lipoma formation. Additionally, mutations in other genes like PTEN and p53, known to be involved in tumor suppression, have also been implicated in some cases.
Inflammation and Trauma: While not definitively proven, chronic inflammation and trauma have been suggested as potential triggers for lipoma formation. However, more research is needed to establish a causal link.[10]
This comprehensive textbook provides a detailed discussion of the pathophysiology, clinical features, and management of various soft tissue tumors, including lipomas.
Clinical Features
Clinical Features
- Presentation: Lipomas typically present as soft, mobile, painless subcutaneous masses. They are most commonly found on the trunk, neck, and extremities, but can occur anywhere in the body where fat is present.
- Size: Lipomas can vary in size from small nodules less than a centimeter to large masses several centimeters in diameter.
- Growth: Lipomas generally grow slowly and rarely cause symptoms unless they compress nearby nerves or blood vessels.
- Consistency: Lipomas are usually well-circumscribed and have a rubbery or doughy consistency.
- Skin Changes: The overlying skin is usually normal, but in some cases, it may appear slightly yellowish or have a dimpled appearance.[10]
Please note that while Enzinger and Weiss’s Soft Tissue Tumors is a comprehensive textbook on soft tissue tumors, it may not provide an exhaustive description of the clinical features of lipomas. However, it is a valuable resource for understanding the pathology and diagnosis of lipomas.
Sign & Symptoms
Sign & Symptoms:
- Localized swelling, which is lobular, nontender.
- Semi fluctuant (because fat in body temperature remains in semi liquid condition).
- Mobile, with edges slipping between the palpating fingers (‘slip sign’).
- Skin is free.
- Lipomas may be pedunculated at times.[2]
Clinical Examination
Clinical Examination of Lipoma
Lipomas are typically diagnosed based on their characteristic clinical features, which include:
Appearance:
- Soft, mobile, non-tender subcutaneous masses.
- Round or oval in shape.
- Skin overlying the lipoma is normal in color.
- Size can range from a few millimeters to several centimeters.
Location:
- Can occur anywhere in the body but are most common on the trunk, neck, shoulders, and proximal extremities.
Palpation:
- Doughy or rubbery consistency.
- Slips easily under the fingers.
- Usually well-circumscribed.[11]
The textbook provides detailed information on the clinical presentation, diagnosis, and management of lipomas, including various surgical techniques for their removal.
Diagnosis
Diagnosis:
- Subcutaneous-commonest type.
- Soft to firm lobular swelling.
- ‘Slip’ sign positive-a pathognomonic sign.
- Semi fluctuant swelling.
- ‘Smart’ dimple sign on movement of the skin.[3]
Differential Diagnosis
Differential Diagnosis:
- Neurofibroma
- Cystic swellings.[2]
Complications
Complications
While most lipomas are benign and asymptomatic, they can occasionally cause complications:
- Pain and Discomfort: Larger lipomas or those located near nerves or joints can cause pain or discomfort.
- Cosmetic Concerns: Lipomas can be a cosmetic concern, especially if they are large or located in visible areas.
- Infection: Rarely, lipomas can become infected, leading to pain, redness, and swelling.
- Malignant Transformation: While extremely rare, lipomas can transform into liposarcomas, a type of cancer.
- Compression of Surrounding Structures: Large lipomas can compress surrounding structures, such as nerves, blood vessels, or organs, leading to various symptoms depending on the location.
- Functional Impairment: Lipomas in specific locations, such as the hand or foot, can impair function due to their size or location.
- Psychological Distress: Lipomas can cause psychological distress due to their appearance or associated symptoms.
It’s important to consult with a healthcare professional if you experience any concerning symptoms or have a lipoma that is causing pain, discomfort, or functional impairment.[12]
Investigations
Investigation:
- A physical exam
- A tissue sample removal (biopsy) for lab examination
- An X-ray or other imaging test, such as an MRI or CT scan, if the lipoma is large, has unusual features or appears to be deeper than the fatty.
Treatment
Treatment:
- Excision
- Small lipoma is excised under local anesthesia and larger one under general anesthesia.
- If it is lipo sarcoma, CT chest should be done to see secondary in lungs. Later wide excision is done along with adjuvant chemotherapy and radiotherapy.[2]
Prevention
Prevention of Lipoma
There are no definitive preventive measures for lipomas mentioned in standard medical texts. Lipomas are benign tumors of fat cells, and their exact cause is unknown. Although some genetic conditions can predispose individuals to developing multiple lipomas, most cases occur sporadically without a clear underlying cause.
However, maintaining a healthy weight and lifestyle may potentially reduce the risk of developing lipomas. This includes a balanced diet, regular exercise, and avoiding excessive alcohol consumption.
It’s important to note that this is based on general health recommendations, and there is no specific research linking these practices directly to lipoma prevention.
This comprehensive textbook provides a detailed overview of lipoma pathology, clinical presentation, diagnosis, and treatment options.[13]
Homeopathic Treatment
Homeopathic Treatment of Lipoma
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Lipoma:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
Baryta Carb:
- Glandular and atheromatous tumors, especially in old persons where pus is scanty and growth slow.
- Lipoma especially of drunkards; sarcoma in neck, with burning.
- Worse at night, when lying on affected side.
- Better when walking in open air.
- Steatoma; small fibroid tumours. [5]
Calcarea Carb:
- Leucophlegmasia and malnutrition, polypi, nasal and uterine, fibroid tumors.
- Lipoma encephaloma, tendency to boils, deficient animal heat, cold feet, perspiration on head also feet;
- Pus copious, putrid, yellowish or white, like milk.
- Worse either in cold air or wet weather.
- Better from having the garments loose.
- Pedunculated fibroids.[5]
Phosphorus:
- Open cancers, bleeding profusely, polypi bleeding readily on slight provocation.
- Lipoma, encephaloma, colloid cancer, condyloma of large size, rough and dry, following the vagina painfulness of stomach to touch, and when walking.
- Worse especially after eating anything warm; pus thick, ichorous, hectic, desires to be magnetized.
- Lymphoma on neck with hectic fever. [5]
Phytolaca:
- Swelling and induration of a glands.
- Carcinoma mammae.
- Lipoma; shooting lancinating pains,
- worse after sleeping;
- Great exhaustion and prostration. [5]
Nitric Acid:
- Pain and swelling of gland, ultimately becoming scirrhus;
- Ulceration following tumor, with a sticking pain as from a painter upon touching them or on notion;
- Bone tumours following mercury or syphilis;
- Condylomata, with sticking pain and much moisture on anus also perineum;
- Pus bloody and corroding. [5]
Diet & Regimen
Diet & Regimen
While there is no specific diet proven to cure lipomas, some dietary and lifestyle modifications may help manage their size and prevent new ones from forming.
Dietary Recommendations:
- Increase fiber intake: Consume plenty of fruits, vegetables, whole grains, and legumes to promote healthy digestion and elimination.
- Choose lean protein: Opt for lean meats, fish, poultry, beans, lentils, and tofu.
- Limit saturated and trans fats: Avoid fried foods, processed foods, red meat, and full-fat dairy products.
- Reduce sugar intake: Limit sugary drinks, desserts, and processed foods.
- Stay hydrated: Drink plenty of water throughout the day.
- Limit alcohol consumption: Excessive alcohol intake can contribute to fat accumulation.
Lifestyle Modifications:
- Maintain a healthy weight: Obesity is a risk factor for lipomas.
- Exercise regularly: Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Manage stress: Chronic stress can contribute to hormonal imbalances that may affect fat metabolism.
The above recommendations are based on general principles of healthy eating and lifestyle. For more specific guidance on managing lipomas through diet and lifestyle, consult a healthcare professional or a registered dietitian.
Do’s and Don'ts
Do’s & Don’ts
Lipoma Do’s & Don’ts
Do’s:
- Consult a doctor: If you notice a new lump or bump under your skin, it’s important to have it evaluated by a doctor to rule out any serious conditions.
- Monitor the lipoma: Keep track of any changes in size, shape, or texture of the lipoma. If it grows rapidly, becomes painful, or feels hard, consult your doctor.
- Maintain a healthy lifestyle: Eat a balanced diet, exercise regularly, and maintain a healthy weight. Although not directly linked to lipoma treatment, a healthy lifestyle can improve overall well-being and potentially reduce the risk of developing new lipomas.
- Manage stress: Chronic stress can contribute to hormonal imbalances that may affect fat metabolism. Practice stress-reducing techniques like yoga, meditation, or deep breathing exercises.
- Consider removal options: If the lipoma is causing pain, discomfort, or affecting your self-esteem, discuss removal options with your doctor. Surgical excision or liposuction are common procedures for lipoma removal.
Don’ts:
- Don’t attempt to self-diagnose: While lipomas are generally harmless, it’s crucial to have a doctor confirm the diagnosis to rule out any other conditions.
- Not remove the lipoma yourself: Attempting to squeeze, puncture, or remove the lipoma at home can lead to infection, scarring, and other complications.
- Don’t ignore changes in the lipoma: If you notice any sudden changes in size, shape, or texture, consult your doctor promptly.
- Don’t rely on unproven remedies: There’s no scientific evidence to support the effectiveness of home remedies for lipomas. Stick to doctor-recommended treatments.
Remember, lipomas are usually benign and don’t require treatment unless they cause discomfort or cosmetic concerns. However, it’s always best to consult a doctor for proper diagnosis and treatment recommendations.
Terminology
Terminology
Lipoma: A benign (non-cancerous) tumor composed of mature fat cells. It typically presents as a soft, movable lump under the skin.
Benign: Not cancerous; does not invade surrounding tissues or spread to other parts of the body.
Tumor: An abnormal growth of tissue. Tumors can be benign or malignant (cancerous).
Subcutaneous: Located beneath the skin.
Adipose Tissue: Fat tissue; the main component of lipomas.
Encapsulated: Enclosed in a fibrous capsule, which separates the lipoma from surrounding tissues.
Lobulated: Having a lobed or segmented appearance.
Mesenchymal: Originating from embryonic connective tissue.
Angiolipoma: A variant of lipoma containing numerous blood vessels.
Fibrolipoma: A lipoma with a significant amount of fibrous tissue.
Liposarcoma: A rare, malignant tumor of fat cells. Liposarcomas are distinct from lipomas and require different treatment approaches.
Excision: Surgical removal of a lipoma.
Liposuction: A procedure that uses suction to remove fat, including lipomas, from the body.
Recurrence: The return of a lipoma after it has been removed. Lipomas rarely recur.
Spontaneous Regression: The disappearance of a lipoma without treatment. This is uncommon but can occur.
Understanding these terminologies can help you better comprehend articles and discussions about lipomas.
Terminology Related To Homoeopathy
Lipoma: A benign, slow-growing tumor composed of fatty tissue.
Benign: Non-cancerous, not spreading to other parts of the body.
Tumor: An abnormal growth of tissue.
Constitutional Remedy: A homeopathic medicine chosen based on the individual’s overall physical and mental characteristics, not just the symptoms of the lipoma.
Miasm: In homeopathy, a miasm is a predisposition to certain types of diseases, including lipomas. The three main miasms are psora, sycosis, and syphilis.
Repertory: A book that lists symptoms and the homeopathic remedies associated with them. Homeopaths use repertories to help select the most appropriate remedy for a patient.
Materia Medica: A collection of descriptions of the properties and effects of homeopathic remedies.
Potency: The strength or dilution of a homeopathic remedy.
Aggravation: A temporary worsening of symptoms after taking a homeopathic remedy. This is considered a positive sign that the remedy is working.
Proving: A process in which healthy volunteers take a homeopathic remedy and record their symptoms. This helps determine the remedy’s therapeutic properties.
Nosode: A homeopathic remedy prepared from diseased tissue or secretions.
Sarcode: A homeopathic remedy prepared from healthy tissue or secretions.
Similimum: The most similar remedy to the patient’s symptoms. This is the ideal remedy for treating the patient.
Vital Force: In homeopathy, the vital force is the life energy that animates the body and maintains health. Homeopathic remedies are believed to stimulate the vital force to heal the body.
Law of Similars: The fundamental principle of homeopathy, which states that a substance that can cause symptoms in a healthy person can cure similar symptoms in a sick person.
These terms are commonly used in homeopathic articles on lipoma and understanding them can help you navigate and interpret the information presented.
References
References
- Clinical surgery S. Das
- SRB’S manual of surgery 3rd edition
- Manipal manual of surgery 4th edition
- www.mayoclinic.org
- Homeopathic Theraputics by Lilienthal.
- Electronic Journal of General Medicine, 2018.
- Weiss SW, Goldblum JR. Enzinger and Weiss’s Soft Tissue Tumors. 6th ed. Philadelphia, PA: Elsevier Saunders; 2014.
- Fletcher CDM, Bridge JA, Hogendoorn PCW, Mertens F. WHO Classification of Tumours of Soft Tissue and Bone. 4th ed. Lyon: IARC Press; 2013.
- Kransdorf MJ, Murphey MD. Imaging of Soft Tissue Tumors. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.
- Enzinger and Weiss’s Soft Tissue Tumors, 7th Edition, Sharon W. Weiss, John R. Goldblum, 2018, Elsevier.
- MacDonald’s Atlas of Procedures in Surgery, 6th Edition, James A. Nunley, J. Lawrence Marsh,2019, Elsevier.
- Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice, 21st Edition, Courtney M. Townsend Jr., et al., 2022, Elsevier.
- Fitzpatrick’s Dermatology in General Medicine, Ninth Edition, Klaus Wolff, Lowell A. Goldsmith, Stephen I. Katz, Barbara A. Gilchrest, Amy S. Paller, David J. Leffell, 2019, McGraw-Hill Education.
- General principles of healthy eating and lifestyle.
Also Search As
Also Search As
- Online search engines: Using general search engines like Google, DuckDuckGo, or Bing, people can enter search queries such as:
- "homeopathic treatment for lipomas"
- "homeopathy and lipomas"
- "homeopathic remedies for lipomas" on lipomas"
- Specialized homeopathic websites: Several websites focus on homeopathy and may have dedicated sections or search functions for specific conditions like lipomas.
- Homeopathic journals and publications: Many peer-reviewed journals and publications within the field of homeopathy exist. Searching their archives or online databases could reveal relevant articles.
- Consulting a homeopathic practitioner: Homeopaths often have access to professional resources and literature, and they might be able to provide or recommend specific articles.
There are several ways to search for information about lipomas:
Online Search Engines:
Medical Websites & Databases:
- Consult reputable medical websites like:
- Mayo Clinic
- Cleveland Clinic
- WebMD
- MedlinePlus
- National Institutes of Health (NIH)
- Search medical databases like PubMed for research articles and studies.
- Consult reputable medical websites like:
Image Search:
- Use image search on search engines or specialized medical image websites to see visual examples of lipomas.
- Be cautious and ensure the images are from reliable sources.
Books & Libraries:
- Consult medical textbooks or books on dermatology or general surgery at libraries.
- Ask librarians for assistance in finding relevant resources.
Consult a Healthcare Professional:
- If you have any concerns about a lump or suspect you have a lipoma, consult a doctor or dermatologist.
- They can provide accurate diagnosis, information, and treatment options.
Additional Tips for Searching:
- Use specific keywords: Be specific in your search terms to get more relevant results.
- Check the source: Always ensure the information you find is from a reputable and reliable source.
- Consult multiple sources: Gather information from various sources to get a comprehensive understanding.
- Be aware of potential misinformation: Be critical of information found online and verify it with trusted medical sources.
- Seek professional advice: If you have any health concerns, always consult a qualified healthcare professional.
Remember, the internet is a valuable resource, but it is essential to be discerning and prioritize information from trusted medical sources.
Frequently Asked Questions (FAQ)
What is Lipoma ?
A lipoma is a cluster of fat cells which become overactive and so distended with fat that it produces a palpable swelling.
What causes lipomas?
The exact cause of lipomas is unknown, but they may be linked to genetics, injury, or certain medical conditions.
How are lipomas diagnosed?
Lipomas are typically diagnosed through a physical examination and may be confirmed with imaging tests like ultrasound or MRI.
What are the types of Lipoma ?
What are the 5 symptoms of Lipoma?
- Localized swelling, which is lobular, nontender.
- Semi fluctuant
- Mobile, with edges slipping between the palpating fingers (‘slip sign’).
- Skin is free.
- Lipomas may be pedunculated at times.
Can homeopathy effectively treat lipomas?
Homeopathy offers a holistic approach to managing lipomas by addressing the underlying imbalances that contribute to their formation. While individual results may vary, many people have reported positive outcomes with homeopathic treatment.
What are the treatment options for lipomas?
If a lipoma is causing problems, it can be removed through surgical excision or liposuction.
Is homeopathy suitable for all types of lipomas?
Homeopathy may be considered for various types of lipomas, but a thorough evaluation by a homeopath is essential to determine its suitability in each case.
Can homeopathy prevent the recurrence of lipomas?
By addressing the underlying constitutional factors and improving overall health, homeopathy may help reduce the likelihood of lipoma recurrence.
How long does it take to see results with homeopathic treatment for lipomas?
The response time varies depending on the individual, the size and duration of the lipoma, and the overall health condition. It may take weeks or months to observe significant changes.
Homeopathic medicines use by Homeopathic Doctors in treatment of Lipoma ?
Homoeopathic Medicines For Lipoma
- Baryta Carb
- Calcarea Carb
- Phosphorus
- Phytolaca
- Nitric Acid
