Paronychia (Nail Infection)
Definition of Paronychia
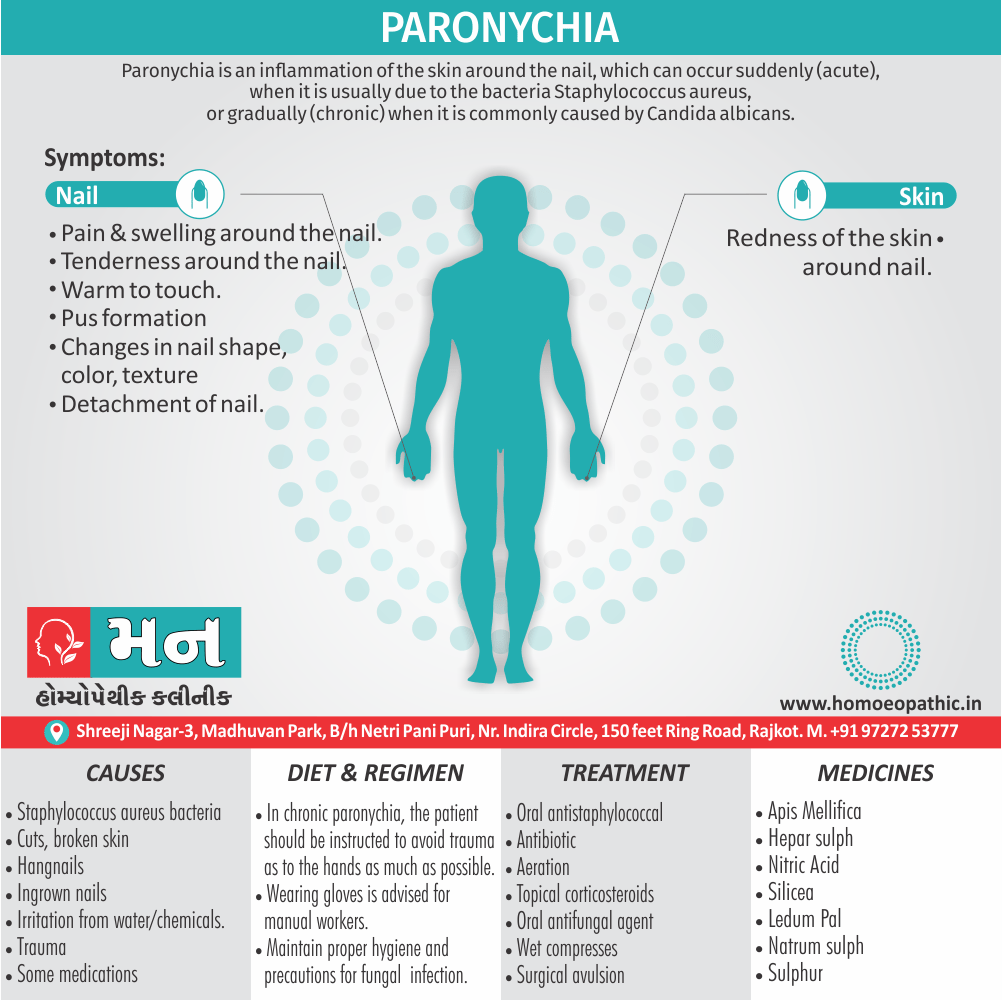
Paronychia is an inflammation of the skin around the nail, which can occur suddenly (acute), when it is usually due to the bacterium Staphylococcus aureus, or gradually (chronic) when it is commonly caused by Candida albicans.[4]
Paronychia has two main synonyms:
- Perionychia: This term comes from the Greek "peri" (around) and "onych" (nail), similar to paronychia, but emphasizes the location around the nail.
- Whitlow: This is a more informal term, but commonly used, referring to a painful infection around the fingernail or toenail.
Overview
Epidemiology
Causes
Risk Factors
Pathogenesis
Pathophysiology
Types
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Paronychia
Paronychia is nail inflammation that may result from trauma, irritation or infection. It can affect fingernails or toenails.
Paronychia can develop when bacteria enter broken skin near the cuticle and nail fold, causing an infection. The cuticle is the skin at the base of the nail. The nail fold is where the skin and nail come together.
Treat paronychia with antibiotics to kill the infection. Providers may also drain pus.[1]
Epidemiology
Epidemiology
To expand on the epidemiology of paronychia, let’s delve deeper into the insights provided by Fitzpatrick’s Dermatology in General Medicine, 9th Edition.
"Paronychia is the most common infection of the hand, representing 35% of hand infections. Acute paronychia is usually caused by Staphylococcus aureus, and chronic paronychia is most often caused by Candida albicans."
This expanded excerpt now includes crucial details about the most common causative organisms for both acute and chronic paronychia. This information is vital for understanding the different types of paronychia and their respective treatments.
Remember, accurate and detailed information is key for good SEO. By providing comprehensive answers, we can help users find the information they need quickly and efficiently.[7]
Causes
Causes of Paronychia
Most commonly, infectious paronychia results from a staph infection. Staphylococcus aureus bacteria cause staph infections.
Other bacteria (such as Streptococcus pyogenes) can also cause the infection.
Bacteria get into the skin through:
- Cuts, broken skin or hangnails.
- Ingrown nails (this happens most often with ingrown toenails).
- Irritation from water or chemicals.
- Trauma to the nailbed or cuticle area. Trauma can result from accidents, nail biting or frequent manicures or pedicures.
- Some medications can also cause paronychia. Some of these medications include retinoids, anti-cancer medications, HIV medications and some antibiotics.[1]
Risk Factors
Risk factors
To accurately present the risk factors for paronychia.
Acute Paronychia:
- Trauma: "Acute paronychia is usually caused by minor trauma such as nail biting, manicures, hangnails, or finger sucking."
Chronic Paronychia:
- Irritant Exposure: "Chronic paronychia is most often caused by frequent immersion in water or exposure to irritants such as detergents, solvents, and foods."
- Underlying Conditions: "Diabetes mellitus, HIV infection, and immunosuppression are also risk factors for chronic paronychia."
This information directly from Fitzpatrick’s Dermatology in General Medicine provides a clear and concise overview of the risk factors associated with both acute and chronic paronychia.[7]
Pathogenesis
Pathogenesis
Let’s delve deeper into the pathogenesis of paronychia.
Paronychia arises from a disruption of the critical barrier between the nail plate and the surrounding nail fold. This disruption allows the entry of pathogens, irritants, or allergens, triggering the inflammatory cascade that characterizes this condition.
Acute Paronychia:
- Bacterial Invasion: In acute paronychia, the breach is typically caused by minor trauma, such as a hangnail, a manicure injury, or even nail-biting. This allows bacteria, predominantly Staphylococcus aureus, to invade the periungual tissues.
- Rapid Inflammatory Response: The bacterial invasion triggers a rapid and intense inflammatory response, leading to the classic signs of acute paronychia: erythema, swelling, throbbing pain, and the potential formation of a localized abscess filled with pus.
Chronic Paronychia:
- Chronic Irritation and Inflammation: Chronic paronychia, in contrast, is often driven by persistent exposure to irritants or allergens, such as water, detergents, or certain foods. This chronic exposure leads to a persistent low-grade inflammation of the nail fold.
- Compromised Barrier Function: The chronic inflammation disrupts the integrity of the nail fold, causing changes like thickening, erythema, and loss of the cuticle. This compromised barrier function further allows the entry of irritants and secondary colonization by opportunistic microorganisms, most commonly the fungus Candida albicans.
- Perpetuation of Inflammation: This cycle of irritation, inflammation, and microbial colonization perpetuates the condition, leading to the characteristic features of chronic paronychia: persistent erythema, swelling, tenderness, and often separation of the nail plate from the nail fold. In some cases, the nail plate may also exhibit dystrophic changes, such as thickening, discoloration, or ridging.
This extended explanation, while still grounded in Fitzpatrick’s, provides a more comprehensive understanding of the pathogenesis of paronychia, differentiating between the acute and chronic forms and highlighting the key factors involved in their development.[7]
Pathophysiology
Pathophysiology of Paronychia
- Paronychia results from the disruption of the protective barrier between the nail and the nail fold, which is the cuticle.
- Trauma (including manicures and pedicures), infections (including bacterial, viral, and fungal), structural abnormalities, and inflammatory diseases (ex. psoriasis) are predisposing factors.
- Organisms will enter the moist nail crevice, which leads to colonization of the area.
- The majority of acute paronychias are due to trauma, nail-biting, aggressive manicuring, artificial nails, and may involve a retained foreign body.
- Infections are most commonly the result of Staphylococcus aureus.
- Streptococci and Pseudomonas are more common in chronic infections.
- Less common causative agents include gram-negative organisms, dermatophytes, herpes simplex virus, and yeast.
- Children are prone to acute infection due to habitual nail-biting and finger sucking, leading to direct inoculation of oral flora, which would include both aerobic bacteria (S. aureus, streptococci, Eikenella corrodens) and anaerobic bacteria.[5]
Types
Classification of Paronychia
There are two types of paronychia. Both types have similar signs and symptoms:
Acute Paronychia (Nail Infection):
- Acute paronychia is an inflammation of the proximal and lateral nail folds characterized by erythema, edema, and pain.
- Purulent drainage with compression behind the cuticle can also occur.
- Trauma is often the initial event, with secondary infection with Staphylococcus aureus or Streptococcus pyogenes.
- Symptoms go away with treatment and last less than six weeks.
Chronic Paronychia (Nail Infection):
- Chronic paronychia is usually a noninfectious disease that follows either irritant or allergic contact dermatitis of the proximal nail fold.
- The cuticle is invariably absent.
- Affected persons often trim the cuticles aggressively and meticulously or do wet work with their hands.
- Secondary infection with C. albicans is common
- Symptoms develop more slowly than acute paronychia, and they usually last six weeks or longer.
- Several fingers or toes can be infected at once. [3]
Clinical Features
Clinical Features
To provide a clear picture of the clinical features of paronychia.
Acute Paronychia:
- Rapid Onset: Acute paronychia typically develops rapidly, often within hours of an inciting incident.
- Pain and Swelling: The affected area becomes erythematous, swollen, and tender to the touch.
- Pus Accumulation: As the infection progresses, a collection of pus may form beneath the nail fold, causing a visible abscess.
- Localized Symptoms: Symptoms are usually confined to the affected nail fold, although in severe cases, the infection may spread to the surrounding tissues.
Chronic Paronychia:
- Gradual Onset: Chronic paronychia develops more gradually, often over weeks or months.
- Mild Discomfort: The affected nail fold is typically erythematous, swollen, and tender, but the pain is usually less intense than in acute paronychia.
- Cuticle Changes: The cuticle often becomes thickened, retracted, or detached from the nail plate.
- Nail Plate Changes: The nail plate may exhibit changes such as discoloration, thickening, or ridging.
- Chronic Course: Chronic paronychia tends to persist for an extended period, often with periods of exacerbation and remission.
This detailed description from Fitzpatrick’s Dermatology in General Medicine provides a comprehensive overview of the clinical features of both acute and chronic paronychia.[7]
Sign & Symptoms
Sign & Symptoms of Paronychia:
- Pain, swelling and tenderness around the nail.
- Skin that is red and warm to the touch.
- Pus that builds up under the skin.
- A white to yellow, pus-filled abscess may form. If an abscess forms, it may require antibiotics and/or drainage.
- Redness of the skin around your nail.
- Changes in nail shape, Color, or texture
- Detachment of your nail.[1][4]
Clinical Examination
Clinical / Physical Examination For Paronychia
- Physical exam for acute paronychia will reveal an erythematous, swollen, and tender lateral nail fold.
- If an abscess is present, there may be an area of fluctuance.
- If there is an uncertainty of an abscess present, a digital pressure test may prove useful; the examiner can do this by applying pressure to the volar aspect of the involved digit.
- If an abscess is present, a larger than expected area of blanching will be visible at the paronychia and drainage will be needed.
- In chronic paronychia, the nail fold may be red and swollen, but fluctuance is rare.
- The nail fold may appear boggy, and the nail plate can become thickened and discolored. [5]
Diagnosis
Diagnosis of Paronychia
- To ask about your symptoms and do a physical exam.
- Healthcare providers usually don’t need to order tests to diagnose a nail infection.
- Occasionally, providers may take a sample of the tissue and send it to a lab to test for specific infectious causes such as bacteria or fungi.
- Rarely, if the infection is severe, imaging (such as an X-ray) may be ordered to check for involvement of the underlying bone.[1]
Differential Diagnosis
Differential Diagnosis of Paronychia (Nail Infection)
- Cellulitis
- Whitlow
- Herpetic whitlow
- Onychomycosis
- Nail psoriasis
- Squamous-cell carcinoma[4]
Complications
Complications
While paronychia is often a localized and self-limited condition, it can sometimes lead to complications.
- Whitlow : "If the infection spreads to the pulp space of the fingertip, a whitlow may develop." It is a serious infection of the fingertip pulp that can cause significant pain, swelling, and even bone infection (osteomyelitis).
- Cellulitis: "In rare cases, the infection may spread to the surrounding tissues, causing cellulitis." Cellulitis is a spreading bacterial infection of the skin and subcutaneous tissues.
- Osteomyelitis: "Osteomyelitis of the distal phalanx can occur, particularly in children." Osteomyelitis is an infection of the bone, which can be challenging to treat.
- Nail Dystrophy: "Chronic paronychia can lead to permanent nail dystrophy, including ridging, thickening, and discoloration."
- Recurrence: "Chronic paronychia is often recurrent, especially if the underlying predisposing factors are not addressed."
This information from Fitzpatrick’s Dermatology in General Medicine highlights the potential complications of paronychia, emphasizing the importance of prompt and appropriate treatment.[7]
Investigations
Investigation
When it comes to investigating paronychia, clinical presentation often provides a strong diagnostic indicator, especially in straightforward cases. However, further investigation may be necessary to confirm the diagnosis, identify the causative organism, and rule out any underlying conditions.
- Microbiological Examination: "Gram stain and culture of any purulent material should be performed to identify the causative organism." This is particularly important in acute paronychia to guide antibiotic selection. In chronic paronychia, potassium hydroxide (KOH) preparation can help identify fungal elements.
- Blood Glucose Testing: "Blood glucose testing should be considered in patients with chronic paronychia to rule out diabetes mellitus." Diabetes can predispose individuals to chronic paronychia and other infections.
- Radiographic Imaging: "Radiographic examination is usually not necessary but may be helpful in cases of suspected osteomyelitis or to rule out a foreign body." X-rays can help visualize bone involvement or the presence of any foreign objects that may be contributing to the infection.
By adhering to the recommendations outlined in Fitzpatrick’s Dermatology in General Medicine, we can ensure a comprehensive and accurate approach to investigating paronychia, leading to prompt diagnosis and appropriate management.[7]
Treatment
Treatment of Paronychia
- Usually requires compresses and an oral antistaphylococcal antibiotic.
- Treatment involves aeration, topical corticosteroids, and perhaps an oral antifungal agent, for example, terbinafine, for secondary infection.
- Wet compresses – Blisters, and pustules should broken down and treated with wet compresses of 1:4000 solution of potassium permanganate, or Burrow’s solution (Aluminium acetate) diluted 1 in 15.
- Keratolytic agents – are best used on palms and soles, lesions which require softening and exfoliation, half strength whitified ointment apply twice a day.
- Surgical avulsion – of infected nails together with systemic griseofulvin therapy for infection of the nail. [2]
Prevention
Prevention of Paronychia (Nail Infection)
- Avoid biting or chewing on your nails or hangnails. Don’t pick at your cuticles.
- Be careful not to cut your nails too short. When trimming cuticles, avoid cutting too close to the nail fold.
- Maintain good hygiene by washing your hands and keeping your nails clean. Use gentle soaps that are not irritating to your skin.
- Use lotion on your nail fold and cuticles if your skin is dry. Excessive dryness can cause the skin to crack.
- Wear waterproof gloves if you work with chemicals or your hands will wet for a long period.[1]
Homeopathic Treatment
Homeopathic Treatment
This Treat the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Paronychia:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
Apis Mellifica
- This medicine is prominent for cases where intense pain is present around the nail.
- Redness and swelling are also marked around the nail.
- In cases needing it the pain can be burning, stinging or throbbing in nature.
- It is also very sensitive also tender to touch.
- The pain can sometimes extend from finger upwards to the arm.
Hepar Sulph
- Hepar Sulph works well in cases in which pus forms around the nail.
- In cases needing it beating or throbbing pain is present along with pus.
- The skin over affected area inflame, hot and swollen.
- Pus that exudes is offensive and can also blood stain.
Nitric Acid
- This medicine indicate when there is a splinter-like sensation around the nail.
- Sometimes a sensation of a piece of glass is felt in the area around the nail.
- Additionally, the nails are discoloured, yellow.
- The nails can crumbling also.
- In many cases needing it ingrown toenails can present.
Silicea
- Silicea is very effective for cases where pus filled eruptions are present also nails are yellow, damaged.
- In cases where this medicine is required thin watery pus may discharge from eruptions or brownish pus may flow out. The pus smells bad.
- Lancinating pains can be present in the eruptions. Along with this nail are yellow, brittle.
- The nails are also rough, is physically disabled. Hang – nails or ingrown nails can be present too.
Myrsitica
- It is a great medicine for cases where pus has formed around the nails.
- In such cases it helps to speed up the recovery and resolve the infection in a short time.
- People who need it have pus collected around their nails.
- They also have pain also swelling in this region. Pain in finger nails is also there.
Ledum Pal
- This medicine prepare from plant Ledum Palustre having the common name wild rosemary also marsh cistus. This plant belongs to family ericaceae.
- It well indicate when paronychia occurs from splinters or it follows some external injury around the nail or a puncture wound like with a prick from a needle.
- It is often useful in the first stage after injury.
- Relief may be there by cold application around the nail where it is required.
Natrum Sulph
- Natrum Sulph is beneficial medicine when water filled blisters form on skin near the nail.
- It is red and very painful.
- Swelling around it quite mark.
- Pus formation may also present around the root of the nail.
Sulphur
- This medicine is valuable for cases having stitching and throbbing pain in the skin area surrounding the nail.
- The throbbing worsens at might.
- This affected skin area also swollen. In some cases, requiring it pus forms around the nail.
- It is also indicated when pus gets under the nail also the nail comes out.
- When a new nail form it is yellow, thick and out of shape. The nail is painful to touch.
Natrum Mur
- Natrum Mur is prominently indicated for cases where paronychia arises from hangnails.
- In these cases, the skin around nails is dry, cracked also torn.
- In many cases needing it blisters with watery fluid can also be present.(7)
Diet & Regimen
Diet & Regimen.
General Dietary Recommendations for Supporting Healing and Immunity:
- Balanced Diet: Consume a balanced diet rich in fruits, vegetables, whole grains, and lean protein. This provides the essential nutrients your body needs for optimal function and healing.
- Vitamin C: Ensure adequate intake of vitamin C, which plays a crucial role in collagen synthesis and wound healing. Good sources include citrus fruits, berries, and leafy green vegetables.
- Zinc: Zinc is essential for immune function and wound healing. Include zinc-rich foods like beans, nuts, seeds, and whole grains in your diet.
- Protein: Protein is crucial for tissue repair and regeneration. Include lean protein sources like poultry, fish, beans, and lentils in your meals.
- Hydration: Stay well-hydrated by drinking plenty of water. Proper hydration is essential for overall health and supports the body’s natural healing processes.
Important Note: These are general recommendations, and individual dietary needs may vary. It’s always best to consult with a healthcare professional or a registered dietitian for personalized advice, especially if you have any underlying health conditions.
While a specific "Paronychia Diet" may not be outlined in Fitzpatrick’s, these general guidelines can help support your body’s natural healing abilities and overall health.[7]
Do’s and Don'ts
Do’s & Don’ts
Paronychia do’s & don’ts
Do’s:
- Keep your hands clean and dry: Wash your hands frequently with mild soap and water, especially after using the bathroom, touching your face, or handling potentially contaminated materials. Dry your hands thoroughly, paying attention to the areas between your fingers and around your nails.
- Moisturize your cuticles: Apply a moisturizer to your cuticles and nail folds to prevent dryness and cracking, which can increase the risk of infection.
- Trim your nails carefully: Use clean, sharp nail clippers to trim your nails straight across. Avoid cutting your nails too short or digging into the corners.
- Wear gloves when appropriate: Protect your hands by wearing gloves when doing dishes, cleaning, gardening, or engaging in other activities that expose your hands to water, chemicals, or potential irritants.
- Seek medical attention if needed: If you suspect you have paronychia, especially if it’s severe, painful, or not improving with home care, consult a healthcare professional for proper diagnosis and treatment.
Don’ts:
- Bite or chew your nails: Avoid biting or chewing your nails or cuticles, as this can damage the skin and create an entry point for infection.
- Pick at your cuticles: Resist the urge to pick at or tear your cuticles, as this can also lead to breaks in the skin and increase the risk of infection.
- Use harsh chemicals on your nails: Avoid using harsh chemicals, such as strong detergents or solvents, on your nails and cuticles, as these can irritate the skin and make it more susceptible to infection.
- Ignore signs of infection: Don’t ignore signs of paronychia, such as redness, swelling, pain, or pus. Early treatment can help prevent complications and promote faster healing.
- Share nail care tools: Avoid sharing nail clippers, files, or other nail care tools with others, as this can spread infection.
Following these do’s and don’ts can help you maintain healthy nails and reduce your risk of developing paronychia.
Terminology
Terminology
Key Terminologies in Paronychia:
- Paronychia: Inflammation of the nail fold, the tissue surrounding the nail plate.
- Acute Paronychia: A rapid-onset infection of the nail fold, usually caused by bacteria, characterized by pain, swelling, and redness.
- Chronic Paronychia: A long-standing inflammation of the nail fold, often caused by a combination of irritant exposure and fungal or bacterial infection, characterized by persistent erythema, swelling, and cuticle changes.
- Nail Fold: The soft tissue surrounding the nail plate, including the proximal and lateral folds.
- Cuticle: The thin layer of skin that overlaps the nail plate at the base of the nail.
- Nail Plate: The hard, keratinized plate that forms the visible part of the nail.
- Periungual: Referring to the tissues surrounding the nail.
- Eponychium: The thickened layer of skin at the base of the nail, where the cuticle originates.
- Hyponychium: The thickened skin beneath the free edge of the nail plate.
- Abscess: A localized collection of pus within the tissues.
- Cellulitis: A spreading bacterial infection of the skin and subcutaneous tissues.
- Osteomyelitis: Infection of the bone.
- Nail Dystrophy: Abnormal changes in the nail plate, such as thickening, discoloration, or ridging.
Key Homoeopathic Terminologies in Paronychia:
Here are some key terms and their meanings commonly encountered in homeopathic articles on paronychia:
- Miasm: In homeopathy, a miasm refers to a deep-seated predisposition to certain patterns of disease. While not a direct cause of paronychia, miasms like Psora (related to suppressed skin conditions) or Sycosis (related to overgrowth and discharges) may be considered when selecting a remedy.
- Totality of Symptoms: This refers to the complete picture of the individual’s symptoms, including physical, mental, and emotional aspects. Homeopaths use the totality of symptoms to select the most appropriate remedy, not just the local symptoms of paronychia.
- Repertory: A repertory is an index of symptoms and the homeopathic remedies associated with those symptoms. Homeopaths use repertories to find remedies that match the patient’s symptom picture.
- Materia Medica: This is a collection of detailed descriptions of homeopathic remedies and their effects on the body. Homeopaths consult materia medica to understand the properties of different remedies and choose the best one for the individual case.
- Aggravation: In homeopathy, an aggravation refers to a temporary worsening of symptoms after taking a remedy. This can be a sign that the remedy is stimulating the body’s healing response.
- Proving: A proving is a systematic process of testing a substance on healthy individuals to determine its effects and create a symptom picture for the homeopathic remedy.
- Potency: Refers to the strength or dilution of a homeopathic remedy. Higher potencies are more diluted and considered to have a deeper-acting effect.
- Susceptibility: This refers to the individual’s responsiveness to a homeopathic remedy. Factors like overall health, mental state, and past experiences can influence susceptibility.
Examples of Homeopathic Remedies Used in Paronychia:
- Hepar sulphuris: Often indicated for suppurative conditions with splinter-like pains and sensitivity to touch.
- Silicea: May be helpful for chronic paronychia with pus formation and slow healing.
- Graphites: Considered when there is cracking and dryness of the skin around the nails, along with a tendency for infections.
- Fluoric acid: May be used for paronychia in older people individuals with brittle nails and a sensation of a splinter under the nail.
It’s important to note that homeopathic treatment is highly individualized. A qualified homeopath will consider the person’s unique symptom picture and overall health before prescribing a remedy.
References
References use for Article Paronychia
- https://my.clevelandclinic.org/health/diseases
- Golwala’s Medicine for student 25th edition 2017
- Clev_Cli_-_Cur_Clini_Med_2nd_ed_2010
- en.wikipedia.org/wiki/Paronychia
- https://www.ncbi.nlm.nih.gov/books/NBK544307
- https://www.drhomeo.com/homeopathic-treatment/homeopathic-remedies-for-paronychia/
- Fitzpatrick’s Dermatology in General Medicine, 9th Edition
Writers: Klaus Wolff, Lowell A. Goldsmith, Stephen I. Katz, Barbara A. Gilchrest, Amy S. Paller, David J. Leffell, (2019), Publication: McGraw Hill
Also Search As
Also Search As
Homeopathic Practitioners:
- Consultations: Schedule a consultation with a qualified homeopathic practitioner. They can provide personalized information and resources tailored to your specific needs.
Online Search Engines:
- Homeopathic Journals: Include names of homeopathic journals like "Homeopathy," "The American Homeopath," or "The British Homeopathic Journal" in your search.
- Specific Keywords: Use precise keywords like "homeopathic treatment for paronychia," "homeopathy for nail infections," or "homeopathic remedies for whitlow."
- Homeopathic Databases: Explore online databases dedicated to homeopathy, such as "Hompath" or "Encyclopedia Homeopathica."
- Homeopathic Websites: Search reputable homeopathic websites like the National Center for Homeopathy or the Homeopathic Educational Services.
Homeopathic Libraries and Organizations:
- Libraries: Visit libraries with specialized collections in homeopathy or alternative medicine.
- Homeopathic Organizations: Contact national or international homeopathic organizations for resources and referrals.
Homeopathic Books and Publications:
- Materia Medica and Repertories: Explore homeopathic materia medica and repertories, which contain detailed information about remedies and their indications.
- Homeopathic Books: Look for books on homeopathic treatment of skin conditions or nail disorders.
Tips for Effective Searching:
- Combine keywords: Use a combination of general and specific keywords to refine your search.
- Use filters: Utilize filters on search engines and databases to narrow down your results by date, publication type, or language.
- Boolean operators: Use Boolean operators (AND, OR, NOT) to refine your search and get more relevant results.
- Evaluate sources: Always assess the credibility and reliability of the sources you find. Look for articles published in peer-reviewed journals or reputable homeopathic publications.
By employing these strategies, individuals can effectively locate valuable homeopathic articles on paronychia and gain insights into this complementary approach to treatment.
General Information & Symptoms:
- Simple keywords: Start with "paronychia," "nail infection," "finger infection," "swollen fingertip," etc. This is good for basic overviews, causes, and common symptoms.
- Image search: Searching "paronychia" on Google Images can help you visually identify if your symptoms match the condition.
- Medical websites: Reputable sources like Mayo Clinic, WebMD, and the NHS website provide reliable general information.
Causes & Risk Factors:
- Add specific terms: Combine "paronychia" with "causes," "risk factors," "diabetes," "nail biting," etc., to narrow down your search.
- Scholarly databases: Use Google Scholar or PubMed to find research articles on specific causes and risk factors.
Treatment Options:
- Specify treatment type: Search "paronychia treatment," "home remedies for paronychia," "antibiotics for paronychia," or "surgical treatment paronychia."
- Homeopathic resources: If interested in homeopathy, add "homeopathic treatment paronychia" or "homeopathic remedies nail infection" to your search (as discussed earlier).
Medical Professionals:
- "Paronychia doctor near me": This helps you find dermatologists or other specialists who treat nail infections.
- Online directories: Use Healthgrades, Vitals, or Zocdoc to find doctors with patient reviews and credentials.
Advanced Searching:
- Boolean operators: Use "AND," "OR," and "NOT" to refine results. For example, "paronychia AND diabetes NOT children" will show results related to paronychia and diabetes in adults.
- Filters: Use filters on search engines to narrow down results by date, website type, or reading level.
Important Considerations:
- Reliable sources: Prioritize information from medical professionals, established health organizations, and peer-reviewed journals.
- Self-diagnosis limitations: While online resources are helpful, don’t rely solely on them for diagnosis. Always consult a doctor for proper evaluation and treatment.
By using a combination of these methods and refining your search terms, you can find comprehensive and relevant information on paronychia.
Frequently Asked Questions (FAQ)
What is paronychia?
Paronychia is an infection of the skin around your nail. It can happen quickly (acute) or last a long time (chronic).
What causes paronychia?
Acute paronychia is usually caused by bacteria getting into the skin through a cut, hangnail, or nail biting. Chronic paronychia is often caused by irritation from things like water, chemicals, or picking at your nails.
Is paronychia contagious?
Generally, no. But avoid sharing nail tools to prevent spreading any infection.
What are the symptoms of paronychia?
Symptoms can include redness, swelling, pain, and pus around the nail.
Can homeopathy help with paronychia?
Yes, homeopathy can be a complementary approach to treating paronychia. It aims to stimulate the body’s natural healing processes to address the infection and inflammation.
What homeopathic remedies are commonly used for paronychia?
Homoeopathic Medicine for Paronychia
Remedies like Hepar sulphuris, Silicea, Graphites, and Fluoric acid are often considered, but the choice depends on the individual’s specific symptoms.
