Rabies
Definition
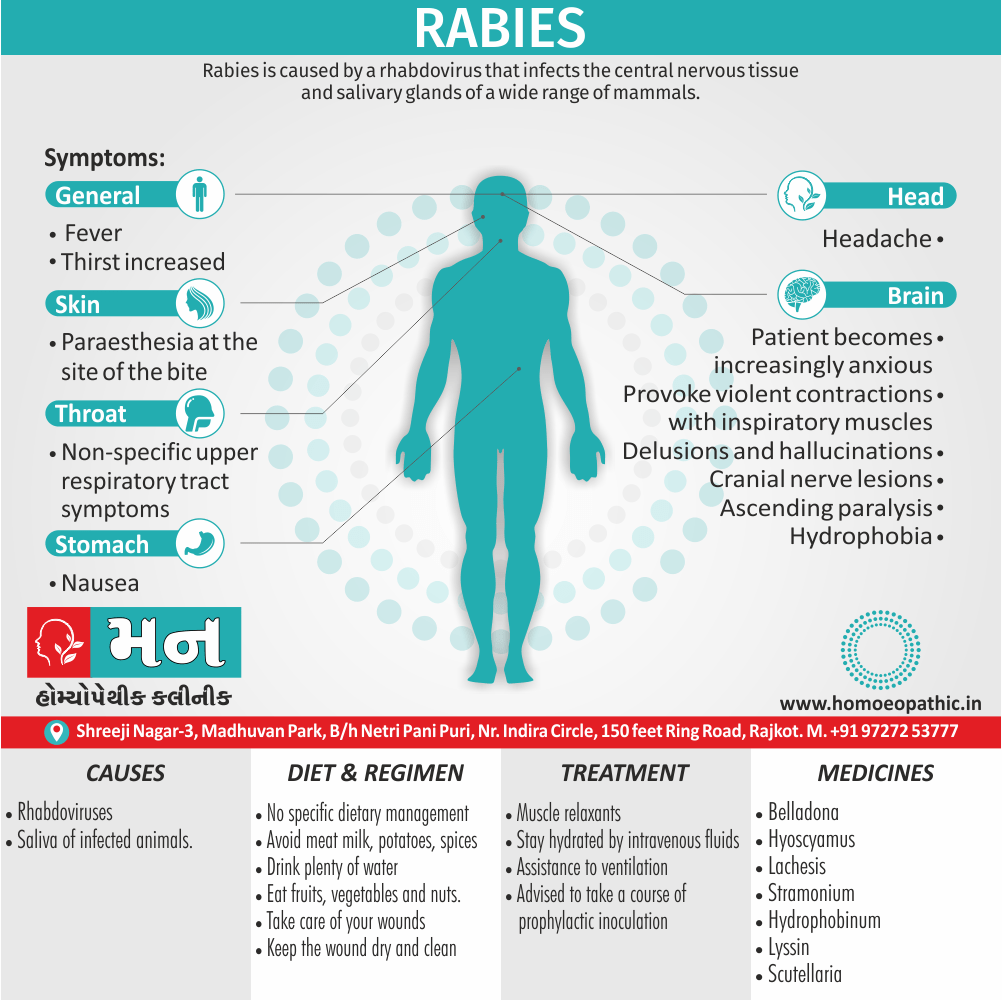
Rabies is caused by a rhabdovirus that infects the central nervous tissue and salivary glands of a wide range of mammals, clinically characterized by rapidly progressive and fatal encephalitis, acquired by man through the bites or licks of infected animals. [1][2]
There isn’t a perfect synonym for "rabies" itself, but depending on the context, here are some options:
Medical context:
- Acute viral encephalitis (inflammation of the brain caused by the rabies virus)
- Lyssa (historical term for rabies)
Informal contexts (referring to the disease):
- Hydrophobia (fear of water, a symptom of rabies)
- Madness (though a less specific term)
Remember, these options might not be appropriate for all situations. "Rabies" itself is a clear and accurate term.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
- Humans are most frequently infected from dogs and bats.
- In Europe, the maintenance host is the fox. The incubation period varies in humans from a minimum of 9 days to many months but is usually between 4 and 8 weeks
- Severe bites, especially if on the head or neck, are associated with shorter incubation periods. Human rabies is a rare disease, even in endemic areas.
- However, because it is usually fatal, major efforts are directed at limiting its spread and preventing its importation into uninfected countries, such as the UK. [1][2]
Epidemiology
Epidemiology
India bears a disproportionately high burden of rabies, accounting for approximately 36% of global rabies deaths. A study published in 2020 in the journal PLOS Neglected Tropical Diseases estimates that there are approximately 20,800 human rabies deaths in India each year. This translates to a rabies incidence of 1.5 deaths per 100,000 population.[9]
Causes
Causes
- The etiological agent is an RNA virus belonging to the group of rhabdo viruses
- It is a rod-shaped virus approximately 180 by 75 nm. When isolated first from animals, it was called “street virus”.
- Saliva of infected animals. [1][2]
Types
Types
Furious Rabies: This is the most common form, characterized by hyperactivity, aggression, and hydrophobia (fear of water). Animals with furious rabies may also exhibit excessive salivation, hallucinations, and seizures.
Paralytic Rabies: This form is less common and is characterized by paralysis, weakness, and coma. Animals with paralytic rabies may appear calm and docile, but they are still infectious.[10]
Risk Factors
Risk factor
- The bite takes place in a geographic area where rabies is still present
- The animal looks ill or displays unusual behavior
- The animal’s saliva comes in contact with a wound or mucous membrane. [3]
Pathogenesis
Pathogenesis of Rabies
The pathogenesis of rabies involves several key stages:
- Inoculation: The virus enters the body through a bite or scratch from an infected animal, typically depositing itself in muscle tissue.
- Replication: The virus replicates in the muscle cells at the site of inoculation.
- Neural Invasion: The virus enters peripheral nerves and travels towards the central nervous system (CNS).
- CNS Infection: The virus reaches the brain and spinal cord, where it replicates extensively, causing inflammation and neuronal damage.
- Centrifugal Spread: The virus spreads from the CNS to other organs, particularly the salivary glands, where it is shed in saliva, making the animal infectious.[10]
Pathophysiology
Pathophysiology of Rabies
- Disease is caused by one of three polioviruses, which constitutes a subgroup of the enteroviruses.
- Infection usually occurs through the nasopharynx
- The virus causes a lymphocytic meningitis and infects the grey matter of the spinal cord, brainstem and cortex
- There is a particular propensity to damage anterior horn cells, especially in the lumbar segments.[1]
Clinical Features
Clinical Features of Rabies
Rabies presents with a variety of clinical features, often categorized into two main forms: furious and paralytic.
- Furious Rabies: This form is characterized by hyperactivity, agitation, anxiety, confusion, hallucinations, hydrophobia (fear of water), and aerophobia (fear of drafts or air currents). It typically progresses rapidly and results in death within a few days.
- Paralytic Rabies: This form presents with progressive muscle weakness and paralysis, often starting at the site of the bite. It is typically less dramatic than furious rabies but can also be fatal.
Other common clinical features of rabies include:
Sign & Symptoms
Sign & Symptoms of Rabies
- Fever
- Paraesthesia at the site of the bite
- Nausea and headache and nonspecific upper respiratory tract symptoms.
- A prodromal period of 1–10 days, during which the patient becomes increasingly anxious, leads to the characteristic ‘hydrophobia’.
- Although the patient is thirsty, attempts at drinking provoke violent contractions of the diaphragm and other inspiratory muscles.
- Delusions and hallucinations may develop, accompanied by spitting, biting and mania, with lucid intervals in which the patient is markedly anxious.[1][2]
- Cranial nerve lesions develop and terminal hyperpyrexia is common.
- Death ensues, usually within a week of the onset of symptoms.
Neurological involvement may present in rabies as i.e.:
The spastic (furious) form i.e.:
- The lesions are more marked in the brain stem, cranial nerves, limbic system and higher centres. painful spasms. These are most marked and characteristic in the oropharynx.
- Swallowing liquid and later on a spray of water, its sight or even thought of it produces painful oropharyngeal spasms with respiratory distress. Hydrophobia.
- Though not pathognomonic, this is almost confirmatory of the diagnosis.[2]
The paralytic form of rabies i.e.:
- This is characterized by ascending paralysis.
- It may start as monoplegia or paraplegia.
- Paralytic form is known to occur more often after vampire bat bites.
- Hydrophobia is rare.
- Patients may survive for a month even without intensive care [2]
Clinical Examination
Clinical / Physical Examination For Rabies
- Hyperpyrexia alternating with hypothermia
- Tachycardia
- Respiratory and vascular collapse
- Bradycardia
- Percussion myoedema (mounding of the muscle at the percussion site)
- Bite marks
- Bruises
- Hypersalivation
- Lacrimation
- Sweating
- Dilatation of the pupils. [4]
Diagnosis
Diagnosis of Rabies
- Immunofluorescent testing: of skin biopsies or corneal impressions can establish diagnosis ante-mortem
- Viral detection: in saliva, throat swabs also tracheal aspirates is possible in 100% on days 0-4, 50% on days 5-8 and 9-12, and 14% on days 13-16. Virus isolation may take several weeks
- Antibody detection: is the most successful method for confirming diagnosis; however, its success depends on maintaining life until antibody can be detected.
- Post-mortem diagnosis: can be achieved by observation of Negri bodies in the brain, virus isolation, immunofluorescence of viral antigen in the brain, PCR and electron microscopy of brain.[2]
Differential Diagnosis
Differential Diagnosis of Rabies
- Encephalitis and other neurological disorders leading to paralysis.
- The spasms of tetanus may resemble hydrophobia especially if they involve the pharyngeal muscles
- Psychiatric conditions, such as maniac excitement and hysteria and drug reactions such as akathisia have to be differentiated at times.
- chaotic subjects adopt hydrophobic manifestations, but absence of aerophobia excludes this condition. [2]
Complications
Complications of Rabies
Once rabies symptoms develop, the disease is almost always fatal. However, even before reaching that stage, rabies can lead to several severe complications:
- Respiratory Failure: Difficulty breathing and respiratory arrest are common complications in the later stages of rabies.
- Cardiac Complications: Arrhythmias and cardiac arrest can also occur.
- Neurological Complications: Rabies can cause encephalitis (inflammation of the brain), seizures, coma, and ultimately, brain death.
- Hydrophobia and Aerophobia: These phobias can make it difficult for individuals to drink or even tolerate the feeling of air on their skin, leading to dehydration and further complications.
- Aspiration Pneumonia: Difficulty swallowing and excessive salivation can increase the risk of aspiration pneumonia, a serious lung infection.[12]
Investigations
Investigation of Rabies
- The CSF shows a lymphocytic pleocytosis
- Rise in protein also a normal sugar content.
- Poliomyelitis virus may be cultured from CSF and stool [1]
Treatment
Treatment
- Once the disease is manifested treatment is only symptomatic
- There is no specific treatment. Treatment aims at controlling spasms with muscle relaxants, maintenance of hydration by intravenous fluids, and assistance to ventilation
- Those who attend on the patients should use gloves, masks, and protective goggles.
- Though the virus eliminated in human saliva is not very virulent, as a matter of abundant caution, attendants who have been inadvertently exposed to very close contact with rabies may be advised to take a course of prophylactic inoculation.[2]
Prevention
Prevention of Rabies
- Vaccinate dogs and cats against rabies as required by law. All dogs and cats more than four months of age must be vaccinated against rabies. Keep vaccinations current at all times.
- Keep dogs and cats under control. Animal control laws prohibit allowing animals to roam unsupervised. Roaming pets are more likely to have been exposed to rabies than those supervised by their owners.
- Leave stray or unknown dogs and cats alone. Loose animals are more likely to have been exposed to rabies and to attack others. Keep pets away from strays, too.
- Do not keep wild animals as pets. Even a raccoon or skunk born in captivity may be a rabies carrier. Local laws prohibit acquiring of keeping such animals as pets. There are no approved vaccines or known quarantine for wild animals.[6]
Homeopathic Treatment
Homeopathic Treatment of Rabies
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Rabies:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
Belladona:
- Throbbing headaches from within outward, especially stabbings in the brain.
- Moreover, Pain externally over whole head, as after violently pulling the hair; distracted features.
- Paleness of face, or bright-red face with throbbing carotids, with thirst; sweat only on the face; additionally increased sensitiveness of the meatus auditorious.
- Spasmodic distortion of the mouth; the head drawn backward, burying the head in the pillow.
- Besides this, Great trouble in swallowing water; violent, small, frequent, anxious respiration; convulsive movements of the limbs.
- With lassitude and anxiousness; extreme sensibility to cold aid; delirious prattle about dogs, which swarm around him; in detail desirous of drying when free from rage.
- All in all, He wants to bite those around him, bites and spits.
Hyoscyamus:
- Posterior part of throat affected; hawking up of mucus; thirst also dryness in throat.
- Constriction of throat with inability to swallow; additionally unquenchable thirst
- Furthermore, Violent sweat after thirst; mental derangement with occasional muttering; horrid anguish, fits of anxiety.
- Moves about from one place to another; concussive starting, alternating with trembling also convulsions; strange fear that he will bit by animals; excessive sweat.
Lachesis:
- Deep stinging throughout the whole head; tearing lancinations in forehead, above eyebrows; distortion of face.
- Hurried talking, with headache, redness of face, mental derangement also constrictive sensation in throat.
- Difficulty of swallowing food, or drink, or saliva; dryness of pharynx also oesophagus, preventing deglutition; convulsions and other spasms, with violent shrieks.
- Lastly, Sopor after cessation of pain.
Stramonium:
- Afraid to be alone; great desire to bite and tear himself with his teeth
- Wants to bite those around him, with a terrible cry and rage; aditionally fancies full of fright and terror, staring eyes, and pupils dilated.
- Turgid swollen face, bloody froth at mouth, excessive restlessness.
- Aversion specifically to watery liquids; frequent spitting, saliva hanging out of the mouth; stiffness of the whole body.
- Any bright object causes furious delirium, spasms of throat also horrible convulsions.
Hydrophobinum:
- Slight dizziness and nausea; intolerable, snappish; irritable headache, with stiffness of the jaws and numb hands; twitching of face and hands: hyperaesthesia of all the senses.
- A breath of air blowing on him causes chronic convulsions; face pale, yellow, and nearly brown.
- Mouth Full or Saliva and total disinclination to drinks; saliva more viscid, constant spitting; sensation of inability to swallow, but can do so when trying.
- Violent spasm of throat with sense of suffocation; constrictive sensation in throat, much worse when swallowing liquids; all reflex symptoms increased.
Lyssin:
- Slight dizziness and nausea; severe headache with stiffness of jaws and numb hands; twitching of face and hands; face pale, yellow, nearly brown.
- Mouth full of saliva and total disinclination to drink.
- Saliva viscid with constant spitting; sensation of inability to swallow but can do so when trying; violent spasm of throat with sense of suffocation; constrictive sensation in throat, much worse when swallowing liquids
Scutellaria:
- Depression of the nervous and vital powers; spasmodic or constricting closing of the jaws, tightness of the muscles of face.
- Nervous agitation from pain; sleeplessness, frightful dreams; tremulousness and twitching of muscles.[8]
Diet & Regimen
Diet & Regimen
- There is no specific dietary management after dog bite.
- You are free to eat anything. But some of the studies in India says it’s not good to have meat milk, potatoes, spices.
- Drink plenty of water and have fruits and vegetables and nuts.
- Take care of your wounds. keep it dry and clean. [7]
Do’s and Don'ts
Do’s and Don’ts
Rabies Do’s and Don’ts
Rabies is a deadly viral disease that affects the nervous system of mammals, including humans. While rare in many developed countries, it’s still a significant public health concern in certain regions. Here’s a breakdown of essential do’s and don’ts to safeguard yourself and your community:
Do’s:
- Vaccinate Your Pets:
- Ensure your dogs, cats, and ferrets receive regular rabies vaccinations, as required by law in many areas. This is the most effective way to protect them and yourself from rabies.
- Report Animal Bites or Scratches:
- Immediately report any animal bites or scratches to your local health department or animal control agency. They can assess the risk of rabies and advise on necessary precautions, including post-exposure prophylaxis (PEP).
- Seek Immediate Medical Attention:
- If you’ve been bitten or scratched by a potentially rabid animal, seek medical care immediately. Early intervention with PEP is crucial in preventing rabies from developing.
- Educate Yourself and Others:
- Learn about rabies prevention, symptoms, and transmission to protect yourself and others. Share this information with your family, friends, and community.
- Secure Garbage and Pet Food:
- Store garbage and pet food in tightly sealed containers to avoid attracting wild animals.
Don’ts:
- Approach Wild Animals:
- Never approach or attempt to handle wild animals, even if they appear friendly or injured. Contact animal control professionals for assistance.
- Leave Pets Unattended Outdoors:
- Supervise your pets when outdoors, especially at night. Keep them on a leash or in a fenced yard to prevent encounters with wild animals.
- Attempt to Capture Wild Animals:
- Do not try to capture or handle wild animals yourself. Contact animal control professionals for assistance.
- Keep Wild Animals as Pets:
- Keeping wild animals as pets is illegal and dangerous. They can carry rabies and other diseases, posing a risk to you and your family.
Remember: Rabies is a preventable disease. By following these do’s and don’ts, you can protect yourself, your loved ones, and your community from this deadly virus.
Terminology
Terminology
1. Zoonosis
- Meaning: A disease that can be transmitted from animals to humans. Rabies is a classic example of a zoonotic disease, primarily transmitted through the bite of an infected animal.
2. Viral Encephalitis
- Meaning: Inflammation of the brain caused by a viral infection. Rabies virus specifically targets the nervous system, leading to encephalitis and ultimately, if untreated, death.
3. Incubation Period
- Meaning: The time between exposure to an infectious agent (like the rabies virus) and the appearance of the first symptoms. The incubation period for rabies can vary widely, from weeks to months, depending on factors like the location of the bite and the amount of virus transmitted.
4. Hydrophobia
- Meaning: Fear of water. This is a classic symptom of rabies, caused by painful spasms in the throat muscles when attempting to swallow.
5. Aerophobia
- Meaning: Fear of drafts or air currents. This is another symptom associated with rabies, often triggered by the same throat spasms that cause hydrophobia.
6. Post-Exposure Prophylaxis (PEP)
- Meaning: A series of vaccinations and sometimes rabies immune globulin given to people who have been exposed to rabies. PEP is highly effective in preventing the development of rabies if administered promptly after exposure.
7. Reservoir Host
- Meaning: An animal species in which a pathogen (like the rabies virus) naturally lives and multiplies. Different animals serve as reservoir hosts for rabies in different regions, such as dogs, bats, raccoons, and foxes.
8. Vector
- Meaning: An organism that transmits a pathogen from one host to another. In the case of rabies, the vector is typically the infected animal that bites and transmits the virus through its saliva.
9. Negri Bodies
- Meaning: Microscopic inclusions found in the nerve cells of animals infected with rabies. These are a hallmark diagnostic sign of rabies infection.
10. Furious Rabies
- Meaning: One of the two main clinical forms of rabies, characterized by hyperactivity, aggression, and agitation.
11. Paralytic Rabies
- Meaning: The other main clinical form of rabies, characterized by progressive paralysis and weakness.
Note: These are just some of the common terminologies you may encounter in articles about rabies. The specific terms used may vary depending on the focus and context of the article.
References
References use for Rabies
- Davidsons Principles and Practice of Medicine (PDFDrive.com)
- KV Krishna Das (Textbook of Medicine)
- http://poshukach.com/redir? user_type=2f&type=sr&redir=eJzLKCkpKLbS1y8 vL9crSy2qLE_NyclITcwpydBLzs_VL0pMykwt1k1 OLC0GUol5KbpFmcXZummJySX5RcW6JoZmxq ZGZgwMhmamxiYWBgbm5gzL9hxZKKUZs7RY7 pr89n2F_gDkIiLe&src=86144a&via_page=1
- http://poshukach.com/redir? user_type=43&type=sr&redir=eJzLKCkpKLbS1y8 vL9crz8zOTMlP1ssvStfPzEtJrdAryCjQD0pMykwtj i_IqCzOTE7MiU tSMzNzEssyczPY2AwN DM1NrEwtbC0ZJgypbKi9XzNdO3PPkuKdNu2Aw D3YyI9&src=882cea&via_page=1
- Golwala’s Medicine for student 25th edition 2017
- http://poshukach.com/redir? user_type=32&type=sr&redir=eJzLKCkpKLbS109 JzkhNzCnJ0EtJ1kvPL9MvTi0qy0xO1S9KTMpM LdYtKEotS80ryczPY2AwNDM1NrEwNzY2Y3DZdE LJTyl1v7bJav5s3hVuAErpGrU&src=5f5b9a&via_page=1
- http://poshukach.com/redir? user_type=42&type=sr&redir=eJwtzLsNwkAQRV GntGBqeF4h_ggyMqoYr8d4JOM1u2NWlqiFjEYIo AcyOuEj0qOrW6m2YWVMjDFrPVl1mXUHY10Tul pNIazke3gO6sWqfBxUKnsQCrdHLsqQEoKKToyc ufka8v4fxMohUkDZ1XWPri1IuUAUrSAa4CkXDjiR tdLQ72-OSTKaTceTxXw5XSbrx3 VzO-8Gr_Q-vGyf6RsiDkEV&src=ff9b4&via_page=1
- Homoeopathic Therpeutics by Lilienthal
- Hampson K, Coudeville L, Lembo T, Sambo M, Kieffer A, Attlan M, et al. (2020). "Estimating the global burden of endemic canine rabies." PLOS Neglected Tropical Diseases 14(4): e0008210.
- Rabies: Scientific Basis of the Disease and Its Management, 3rd Edition, Alan C. Jackson, 2007, Academic Press.
- Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases, 9th Edition, Edited by John E. Bennett, Raphael Dolin, and Martin J. Blaser, Published in 2020 by Elsevier.
- Harrison’s Principles of Internal Medicine, 21st Edition, Edited by Dennis L. Kasper, Anthony S. Fauci, Stephen L. Hauser, Dan L. Longo, J. Larry Jameson, and Joseph Loscalzo, Published in 2022 by McGraw Hill.
Also Search As
Also Search As
Online Search Engines:
- Utilize search engines like Google, DuckDuckGo, or Bing.
- Use specific search terms such as:
Homeopathic Journals and Publications:
- Access online databases or libraries that specialize in homeopathic literature.
- Look for reputable homeopathic journals like "The American Journal of Homeopathic Medicine" or "Homeopathy."
- Search within these publications using rabies-related keywords.
Homeopathic Organizations and Websites:
- Visit websites of national or international homeopathic organizations.
- Many of these organizations provide resources and articles on various health topics, including rabies.
Consulting Homeopathic Practitioners:
- Ask a qualified homeopathic practitioner for recommendations on relevant articles or research papers.
- They can often provide insights and guidance on homeopathic approaches to rabies prevention and treatment.
Important Considerations:
- While searching for homeopathic information on rabies, it is crucial to prioritize reliable sources and evidence-based research.
- Be critical of the information you encounter and consult with qualified healthcare professionals before making any decisions regarding rabies prevention or treatment.
- Remember that conventional post-exposure prophylaxis (PEP) is the only scientifically proven and recommended method for preventing rabies after a potential exposure.
Frequently Asked Questions (FAQ)
What is rabies?
Rabies is a viral disease that affects the central nervous system of mammals, including humans. It is transmitted through the saliva of infected animals, usually through bites or scratches.
What are the symptoms of rabies?
How is rabies diagnosed?
There is no definitive test for rabies in living humans. Diagnosis is typically based on a combination of factors, including exposure history, symptoms, and laboratory tests on the animal that inflicted the bite
How is rabies treated?
How can I prevent rabies?
Prevention measures include:
- Vaccinating pets: Make sure your pets are up-to-date on their rabies vaccinations.
- Avoiding contact with wild animals: Do not approach or feed wild animals.
- Seeking medical attention immediately after a bite: If you are bitten by an animal, wash the wound thoroughly with soap and water and seek medical attention immediately.
Can homeopathy cure rabies?
No. Rabies is a serious viral infection with a near 100% fatality rate once symptoms appear. Conventional post-exposure prophylaxis (PEP) with vaccination and immunoglobulin is the only proven effective treatment. Homeopathy should not be considered a substitute for PEP
Can homeopathy be used alongside conventional treatment for rabies exposure?
While homeopathy may be used alongside conventional treatment, it’s crucial to prioritize PEP as the primary intervention. Consult your doctor immediately if you suspect rabies exposure.
Is it safe to use homeopathy for rabies prevention?
Are there any homeopathic remedies that can help with the symptoms of rabies?
Homoeopathic Medicines For Rabies
Some homeopathic remedies like Belladonna, Hyoscyamus, and Stramonium have been traditionally used to address symptoms like anxiety, agitation, hydrophobia (fear of water), and spasms. However, their effectiveness in treating rabies itself is unproven. Some homeopathic remedies like Belladonna, Hyoscyamus, and Stramonium have been traditionally used to address symptoms like anxiety, agitation, hydrophobia (fear of water), and spasms. However, their effectiveness in treating rabies itself is unproven.
