Appendicitis
Definition:
Appendicitis is an inflammation of the appendix. The appendix is a finger-shaped pouch that sticks out from the colon on the lower right side of the belly, also called the abdomen [1]
There aren’t any true synonyms for appendicitis since it’s a specific medical condition. However, depending on the context, you could use descriptive phrases that highlight the key features:
Inflamed appendix:
- This directly describes the condition, mentioning the inflamed organ.
Appendix inflammation:
Similar to the above, but uses a more technical term "inflammation."
Acute appendicitis:
- "Acute" refers to the sudden onset of symptoms, which is characteristic of appendicitis.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
- Appendix is a vestigial organ which serves no useful purpose in human beings but instead becomes the site of trouble at times.
- It is like a diverticulum of the caecum, usually lying behind the caecum and varies in length from 4 to 20 cm (average 7 cm).
- The condition is seen more commonly in older children and young adults and is uncommon at the extremes of age.
- The disease is seen more frequently in the West and in affluent societies which may be due to variation in diet— a diet with low bulk or cellulose and high protein intake more often causes appendicitis [2]
Epidemiology
Epidemiology
In India varies across studies, with the following references highlighting key findings:
- IJCMAAS, May 2018: In a rural tertiary care hospital in Tamil Nadu, the highest occurrence of appendicitis was in the 11-20 years age group (30.92%), followed by 21-30 years (29.21%).[9]
- IJARS, September 2023: Citing Singh A et al., the prevalence of acute appendicitis in the Indian population is approximately 8%, especially among individuals aged 10 to 30 years.[10]
- IJCMR: This study in a tertiary care hospital in North India found the least number of patients in the >50 years age group (4%). The mean age reported in various Indian studies ranges from 20.9 to 30.8 years[11].
- ResearchGate: This study from a peripheral hospital in Maharashtra found the occurrence of acute appendicitis to be more common in males, with the highest rate in the 20-30 years age group.[12]
- International Journal of Medicine and Medical Research: A study from North-East India found acute appendicitis affected both sexes equally, with a slightly higher incidence in males and a peak during the second and third decades of life.[13]
Please note that the prevalence and demographics of appendicitis can vary depending on the region, healthcare setting, and study population. For a comprehensive understanding, it is recommended to consult multiple sources and consider the specific context of each study.
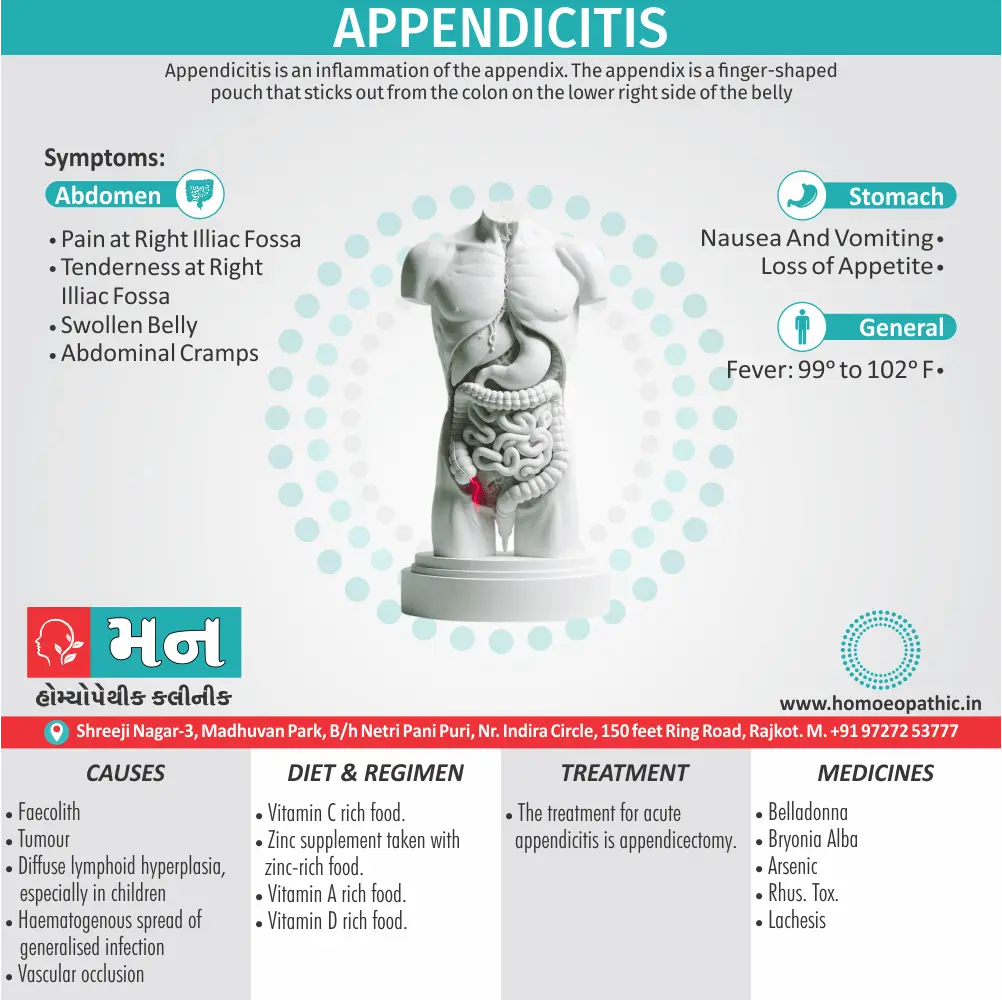
Causes
Causes
Obstructive:
- Faecolith – A Mass of An Accumulation of Hardened Fecal Matter
- Calculi
- Foreign body
- Tumour
- Worms (especially Enterobius vermicularis)
- Diffuse lymphoid hyperplasia, especially in children.
Non-obstructive:
- Haematogenous spread of generalised infection
- Vascular occlusion
- Inappropriate diet lacking roughage. [2]
Types
Types of Appendicitis
Acute non-obstructive appendicitis:
- Inflammation of mucous membrane with redness, oedema and haemorrhages which may go for following courses: Resolution; Ulceration; Fibrosis; Suppuration; Recurrent appendicitis; Gangrene; Peritonitis.
Acute obstructive appendicitis:
- Here pus collects in the blocked lumen of the appendix which has become blackish, gangrenous, oedematous and rapidly progresses leading to perforation either at the tip or at the base of the appendix.
- This will lead to peritonitis, formation of appendicular abscess or pelvic abscess.
- Most often there will be thrombosis of the appendicular artery.
Recurrent appendicitis:
- Repeated attacks of non-obstructive appendicitis leads to fibrosis, adhesions causing recurrent appendicitis.
Subacute appendicitis:
- it is milder form of acute appendicitis [4]
Risk Factors
Risk Factors of Appendicitis
Age:
- Appendicitis most often affects teens and people in their 20’s but it can occur at any age.
Sex :
- Appendicitis is more common in males than females.
Family history :
- People who have a family history of appendicitis are at heightened risk of developing it.[3]
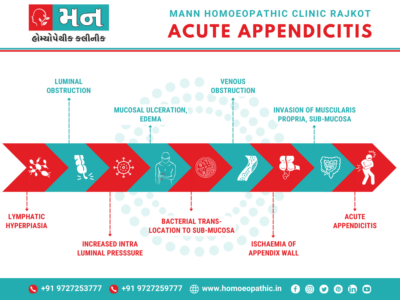
Pathogenesis
Pathogenesis
Several books elaborate on the pathogenesis of appendicitis, including:
The pathogenesis as starting with luminal obstruction, usually by a faecolith, leading to increased intraluminal pressure, impaired venous drainage, and bacterial overgrowth. This results in mucosal ulceration, inflammatory exudate, and eventually, perforation.[14]
Appendicitis is explained as a sequence of events initiated by luminal obstruction, which causes mucosal ischemia and bacterial invasion. This leads to inflammation, edema, and eventually, gangrene and perforation if not treated.[15]
The pathogenesis as a cascade involving luminal obstruction (often by a fecalith), followed by distension, bacterial overgrowth, vascular compromise, and transmural inflammation. This can culminate in necrosis, perforation, and peritonitis.[16]
Please note that the exact wording in these books might vary slightly. It’s recommended to refer to the specific edition for detailed information.
Pathophysiology
Pathophysiology
Clinical Features
Clinical Features
The clinical features of appendicitis, including:
- The classic presentation as central abdominal pain migrating to the right iliac fossa, associated with anorexia, nausea, and low-grade fever. It emphasizes the importance of localized tenderness at McBurney’s point and rebound tenderness.[14]
- The clinical features are highlighted as periumbilical pain shifting to the right lower quadrant, accompanied by anorexia, nausea, vomiting, and low-grade fever. Physical examination findings include tenderness at McBurney’s point, guarding, and rebound tenderness.[15]
- The typical clinical picture as starting with dull periumbilical pain progressing to sharp right lower quadrant pain, along with anorexia, nausea, vomiting, and fever. It mentions additional signs like Rovsing’s sign, psoas sign, and obturator sign.[16]
- Please note that the exact wording in these books might vary slightly. It’s recommended to refer to the specific edition for detailed information.
Sign & Symptoms
Sign & Symptoms of Appendicitis
- Pain in your lower right belly or pain near your navel that moves lower. This is usually the first sign.
- Loss of appetite
- Nausea and vomiting soon after belly pain begins
- Swollen belly
- Fever of 99-102 F
- Can’t pass gas
- Other less common symptoms of appendicitis include:
- Dull or sharp pain anywhere in your upper or lower belly, back, or rear end
- Painful or difficult peeing
- Vomiting before your belly pain starts
- Severe cramps
- Constipation or diarrhoea with gas [6]
Clinical Examination
Clinical Examination of Appendicitis
1. Rebound Tenderness, pain, rigidity, and guarding at the McBurney point. McBurney Point is that lie one-third of the distance laterally on a line drawn from the umbilicus to the right anterior superior iliac spine
2. Release sign—Blumberg’s sign: Tenderness and rebound tenderness in right iliac fossa are typical.
3. Rovsing’s sign: On pressing left iliac fossa, pain occurs in right iliac fossa which is due to shift of bowel loops which irritates the parietal peritoneum
4.Hyperextension (in case of retrocecal appendix— Cope’s psoas test) or internal rotation (in case of pelvic appendix—obturator test) of right hip causes pain in right iliac fossa due to irritation of psoas muscle and obturator internus muscle respectively.
5. Baldwing’s test is positive in retrocecal appendix– when legs lifted off the bed with knee extended, the patient complains of pain while pressing over the
6. P/R examination shows tenderness in the right side of the rectum. Often infection gets localized by omentum, dilated ileum and parietal peritoneum leading to appendicular mass. Most often suppurations occur in the localized area resulting in appendicular abscess. [4]
Diagnosis
Diagnosis
To diagnose appendicitis, your health care team will likely take a history of your symptoms and examine your abdomen. Tests used to diagnose appendicitis include:
1. Physical examination.
- Physician may apply gentle pressure on the painful area. When the pressure is suddenly released, appendicitis pain will often feel worse. This is because of inflammation of the lining of the abdominal cavity, called the peritoneum. Physician also may look for abdominal stiffness and a tendency for you to flex your abdominal muscles in response to pressure over the inflamed appendix. This is called guarding.
- Doctor also may use a lubricated, gloved finger to examine your lower rectum. This is called a digital rectal examination. People of childbearing age may be given a pelvic examination to check for other problems that could be causing the pain.
2. Blood test.
- This test checks for a high white blood cell count.
- A high white blood cell count may indicate an infection.
3. Urine test.
- You may have to take a urine test, also called a urinalysis.
- A urinalysis makes sure that a urinary tract infection or a kidney stone isn’t causing your pain.
4. Imaging tests.
- You also may have imaging tests to help confirm appendicitis or find other causes for your pain.
- These tests may include an abdominal X-ray, an abdominal ultrasound, a CT scan or an [1]
Differential Diagnosis
Differential Diagnosis of Appendicitis
- Gastroenteritis – a stomach bug that causes diarrhoea and vomiting.
- Severe irritable bowel syndrome (IBS).
- Constipation.
- Bladder or urinary tract infections.
- Crohn`s Disease
- Pelvic infection.
Complications
Complications
The complications of appendicitis, including:
- A complications such as perforation leading to peritonitis, abscess formation, and septicemia. It also mentions complications of surgery, such as wound infection, intra-abdominal abscess, and adhesive small bowel obstruction.[14]
- A complications are outlined as perforation with peritonitis, abscess formation (localized or pelvic), and sepsis. It also mentions rare complications like pylephlebitis (septic thrombosis of the portal vein) and post-operative complications like wound infection and bowel obstruction.[15]
- A complications as perforation with peritonitis, abscess formation (periappendiceal, pelvic, or subphrenic), and bacteremia. It also discusses post-operative complications like wound infection, intra-abdominal abscess, and intestinal obstruction.[16]
Please note that the exact wording in these books might vary slightly. It’s recommended to refer to the specific edition for detailed information.
Investigations
Investigations of Appendicitis
- The diagnosis of acute appendicitis is essentially clinical; however, a decision to operate based on clinical suspicion alone can lead to the removal of a normal appendix in 15–30% of cases.
- The premise that it is better to remove a normal appendix than to delay diagnosis does not stand up to scrutiny, particularly in the older people.
- Several clinical and laboratory-based scoring systems have been devised to assist diagnosis.
- The most widely used is the Alvarado score. A score of 7 or more is strongly predictive of acute appendicitis. In patients with an equivocal score (5–6), abdominal ultrasound or contrast-enhanced CT examination further reduces the rate of negative appendicectomy.
- Abdominal ultrasound examination is more useful in children and thin adults, particularly if gynaecological pathology is suspected, with a diagnostic accuracy more than 90%.
- Contrast-enhanced CT scan is most useful in patients in whom there is diagnostic uncertainty, particularly older patients, in whom acute diverticulitis, intestinal obstruction and neoplasm are likely differential diagnoses.
- Selective use of CT scanning may be cost-effective by reducing both the negative appendicectomy rate and the length of hospital stay.[5]
ALVERADO SCORE
| Symptoms | Score |
| Migratory RIF Pain | 1 |
| Anorexia | 1 |
| Nausea And Vomiting | 1 |
| Signs | |
| Tenderness (RIF) | 2 |
| Rebound Tenderness | 1 |
| Elevated Temperature | 1 |
| Laboratory | |
| Leucocytosis | 2 |
| Shift To Left | 1 |
| Total | 10 |
Treatment
Treatment of Appendicitis
- The treatment for acute appendicitis is appendicectomy.
- There is a perception that urgent operation is essential to prevent the increased morbidity and mortality of peritonitis.
- While there should be no unnecessary delay, all patients, particularly those most at risk of serious morbidity, benefit by a short period of intensive preoperative preparation.
- Intravenous fluids, sufficient to establish adequate urine output (catheterisation is needed only in the very ill), and appropriate antibiotics should be given.
- There is ample evidence that a single peroperative dose of antibiotics reduces the incidence of postoperative wound infection.
- When peritonitis is suspected, therapeutic intravenous antibiotics to cover Gram-negative bacilli as well as anaerobic cocci should be given.
- Hyperpyrexia in children should be treated with salicylates in addition to antibiotics and intravenous fluids. With appropriate use of intravenous fluids and parenteral antibiotics, a policy of deferring appendicectomy after midnight to the first case on the following morning does not increase morbidity.
- However, when acute obstructive appendicitis is recognised, operation should not be deferred longer than it takes to optimise the patient’s condition.[5]
Prevention
Prevention of Appendicitis
There’s no way to prevent appendicitis. But it may be less common in people who eat foods high in fiber, such as fresh fruits and vegetables.[6]
Homeopathic Treatment
Homeopathic Treatment of Appendicitis
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’? The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition. The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Appendicitis:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity, but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also considered for selecting a remedy, potency and repetition of dose by Homeopathic doctor. So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
Belladonna
- In the early stages of this affection where there is severe pain in the ileo-caecal region, where the slightest touch cannot be borne, worse from jar, motion of bed or turning of body and patient lies on back, this remedy will be found most useful. Worse from jar, motion of bed or turning of body.
- It corresponds to the pain, the vomiting the paralysis of the intestine.
- It comes in after the chill of the Aconite stage has passed off and the inflammation has localized itself. Much pain contraindicates Aconite.
- Ferrum phosphoricum and Kali muriaticum have proved themselves clinically in inflammation about the ileo-caecal region and their indications rest on clinical grounds only.
- Belladonna is especially useful in catarrhal and recurring cases.
Bryonia Alba
- As in all inflammations about serous membranes, Bryonia will here find a place.
- It has throbbing and sharp stitching pains confined to a limited spot and the patient is constipated. The ileo-caecal region is very sore and sensitive to touch.
- Any movement is painful, and the patient lies perfectly still and on the painful side.
- The febrile disturbance of the drug will be present.
- Mercurius being Homoeopathic inflammation of the mucous membranes deserves consideration, especially has it hard swelling, fever, flushed face, red, dry tongue, etc.
Arsenicum Album
- When the condition points to sepsis Arsenicum may be the remedy. There are chills, hectic symptoms, diarrhoea and restlessness, and sudden sinking of strength.
- It relieves vomiting in these conditions more quickly than any other remedy.
- Dr.Mitchell finds it more often indicated in appendicitis than Mercurius corrosivus, which may also be a useful remedy.
- Arnica is a remedy suiting septic cases and it should be employed after operations.
Rhus Toxicodendron
- This remedy, with its great correspondence to septic troubles may be required and may be indicated by its peculiar symptoms; locally, took it has extensive swelling over the ileo-caecal region and great pain, causing an incessant restlessness.
- Dr.Cartier, of Paris, recommends Rhus radicans 6x. in appendicitis of influenzal origin at the onset.
- Hepar has a deep-seated induration and Dioscorea has proved a valuable, remedy when the pain is constant, the patient never being entirely free from pain. One observer claims Dioscorea to be as important a remedy in appendicitis as is Bryonia in hepatitis.
- Its indications are bowels filled with gas and griping, twisting pains. It may be given in hot water. It is a far more inflammatory remedy than Colocynth, deeper acting, and its paroxysmal pains are an indication. Echinacea, it is claimed, has acted brilliantly in septic appendicitis; the tincture, 1x and 3x are the strengths used. No indications except septic condition; tiredness is characteristic.
Lachesis
- This is also a valuable remedy; its great characteristics of sensitiveness all over the abdomen and stitching from the seat of the inflammation backward and downward to the thighs, will indicate it in this disease.
- The patient lies on the back with knees drawn up, and other general Lachesis symptoms present.
- Plumbum has a tense swelling in the ileo-caecal region, painful to touch and on movement; the abdominal walls are retracted, there are eructations of gas and vomiting and both have a faecal odor. [8]
Diet & Regimen
Diet & Regimen
- The appendicitis diet plan should primarily include Vitamin A, Vitamin C, Zinc, Omega-3 fatty acids, glutamine, etc.
- Vitamin C rich food such as orange, guava, lemon, etc. can be very useful in this condition.
- An extra zinc supplement can also be taken with zinc-rich food.
- Carrots and sweet potatoes which are good sources of Vitamin A should be consumed along with the other food.
- Vitamin D is important to have a healthy body, high-quality supplements of which include eggs, fish, cheese, ginger, etc. [7]
Do’s and Don'ts
Do’s & Don’ts
While medical textbooks do not explicitly list "Do’s and Don’ts" for appendicitis, we can infer recommendations based on their content regarding diagnosis, management, and complications:
Do’s:
- Emphasizes early diagnosis and prompt surgical intervention to prevent complications.
- Recommends thorough history and physical examination, including assessing for signs of peritonitis.
- Advocates the use of imaging studies (ultrasound, CT scan) to confirm the diagnosis, especially in atypical cases.[14]
- Stresses the importance of considering appendicitis in the differential diagnosis of abdominal pain.
- Recommends initiating antibiotic therapy preoperatively and continuing postoperatively.
- Advises close monitoring for complications like abscess formation and sepsis.[15]
- Encourages early surgical consultation for suspected appendicitis.
- Suggests laparoscopic appendectomy as the preferred surgical approach.
- Recommends adequate pain control and early ambulation postoperatively.[16]
Don’ts:
- Caution against delaying diagnosis and treatment, as it increases the risk of perforation and peritonitis.
- Discourage the use of laxatives or enemas, which can worsen inflammation and increase the risk of perforation.
- Advise against administering analgesics before diagnosis, as they can mask symptoms and delay treatment.[14][15][16]
Remember, these are general recommendations based on textbook content. The specific management of appendicitis may vary depending on individual circumstances and should be determined by a qualified healthcare professional.
Terminology
Terminology
- Acute Appendicitis: A sudden and severe inflammation of the appendix.
- Faecolith: A hard mass of fecal matter that can obstruct the appendix.
- Pathogenesis: The development or origin of a disease (in this case, appendicitis).
- Peritonitis: Inflammation of the peritoneum, the membrane lining the abdominal cavity.
- Rebound Tenderness: Pain felt upon the release of pressure on the abdomen, a sign of peritoneal irritation.
- McBurney’s Point: A specific area on the lower right abdomen where tenderness is often a sign of appendicitis.
- Rovsing’s Sign: Pain in the right lower quadrant when pressure is applied to the left lower quadrant.
- Alvarado Score: A scoring system used to assess the likelihood of appendicitis.
- Appendicectomy: Surgical removal of the appendix.
Homeopathic Terminology:
- Miasmatic Tendency: A predisposition to certain types of diseases, a key concept in homeopathic philosophy.
- Therapeutic Affinity: The tendency of a homeopathic remedy to address certain symptoms or conditions.
- Catarrhal: Relating to inflammation of mucous membranes.
- Sepsis: A life-threatening condition caused by the body’s response to an infection.
- Ileo-caecal region: The area where the small intestine (ileum) joins the large intestine (cecum), where the appendix is located.
Additional Terms in the Article:
- Epidemiology: The study of the distribution and determinants of health-related states or events (like appendicitis) in populations.
- Pathophysiology: The disordered physiological processes associated with disease or injury.
- Differential Diagnosis: The process of distinguishing a particular disease or condition from others that present with similar clinical features.
Important Note:
- The homeopathic treatment section emphasizes the importance of consulting a registered homeopathic practitioner for personalized treatment. Self-treatment based on the information in this article is not advisable.
References
References
- Appendicitis – Symptoms and cause MayoClinic
- Harsh Mohan Textbook Chepter20
- Appendicitis: Symptoms, Causes, Treatment, and (healthline.com)
- SRB`s Clinical Method
- Bailey and Loves Short Practice of Surgery chep.67
- Appendicitis: Early Symptoms, Causes, Pain Location, Surgery, Recovery (webmd.com)
- Diet Chart For appendicitis Patient, Appendicitis Diet chart | Lybrate.
- Practical Homoeopathic Therapeutics By Dewey W.A.
- IJCMAAS, May 2018
- IJARS, September 2023
- IJCMR
- ResearchGate
- International Journal of Medicine and Medical Research.
Bailey & Love’s Short Practice of Surgery, 27th Edition (2018),Authors:Norman S. Williams, Christopher J.K. Bulstrode, P Ronan O’Connell,Publisher:CRC Press.
Schwartz’s Principles of Surgery, 11th Edition (2019),Authors:F. Charles Brunicardi et al,Publisher:McGraw Hill Professional.
Sabiston Textbook of Surgery, 21st Edition (2022),Authors:Courtney M. Townsend Jr. et al.,Publisher:Elsevier
Also Search As
Also Search As
People can search for the article "Appendicitis" using several different search terms and phrases, depending on their specific interests and needs:
General Search Terms:
- Appendicitis
- Symptoms of appendicitis
- Appendicitis treatment
- Appendicitis causes
- Appendicitis surgery
- Appendix inflammation
- What is appendicitis?
For Homeopathic Information:
- Homeopathic treatment for appendicitis
- Homeopathy for appendix pain
- Homeopathic remedies for appendicitis
- Natural remedies for appendicitis
- Alternative medicine for appendicitis
Long-Tail Keywords & Phrases:
- Can appendicitis be cured without surgery?
- How to relieve appendicitis pain at home
- Is appendicitis an emergency?
- What are the risks of untreated appendicitis?
- Appendicitis in children/adults/elderly
Additional Tips:
- Include relevant keywords in the title and meta description of your article to improve its visibility in search results.
- Consider using structured data (schema markup) to help search engines understand the content of your article and display it in rich results.
- Promote your article on social media and other online platforms to attract more readers.
There are several ways people might search for an article on appendicitis, depending on their specific needs and interests:
General Searches:
- Simple keywords:
- Appendicitis
- Appendix
- Appendicitis symptoms
- Appendicitis treatment
- Appendicitis causes
- Question format:
- What is appendicitis?
- What are the signs of appendicitis?
- How is appendicitis treated?
- Can appendicitis be prevented?
Specific Searches:
- Focused on symptoms:
- Appendicitis pain
- Abdominal pain right side
- Nausea and vomiting with abdominal pain
- Focused on diagnosis:
- Appendicitis tests
- How to know if I have appendicitis
- Appendicitis vs. other conditions (e.g., gastroenteritis)
- Focused on treatment:
- Appendicitis surgery recovery
- Antibiotics for appendicitis
- Appendicitis diet
Alternative Medicine Searches:
- Homeopathic focus:
- Homeopathic remedies for appendicitis
- Homeopathy for appendicitis pain
- Natural treatment for appendicitis
- Other alternative medicine:
- Herbal remedies for appendicitis
- Acupuncture for appendicitis
Essential oils for appendicitis
Additional Tips:
- Consider long-tail keywords: These are longer, more specific phrases that people might use when searching, such as "appendicitis pain in pregnancy" or "appendicitis in children."
- Use synonyms: Search engines understand synonyms, so use different words with similar meanings (e.g., "appendix inflammation" instead of "appendicitis").
- Local searches: If your article is specific to a certain location, include the location in your search terms (e.g., "appendicitis treatment in [your city]").
Frequently Asked Questions (FAQ)
What is appendicitis?
Definition
Appendicitis is the inflammation of the appendix, a small finger-shaped pouch that extends from the colon. It often causes sudden pain in the lower right abdomen
What are the symptoms of appendicitis?
How is appendicitis diagnosed?
Diagnosis
- Physical examination to check for tenderness in the abdomen
- Blood tests to look for signs of infection
- Urine tests to rule out other causes of pain
- Imaging tests like ultrasound or CT scans to confirm appendicitis
What is the treatment for appendicitis?
Treatment
The standard treatment for appendicitis is surgery (appendicectomy) to remove the inflamed appendix. In some cases, antibiotics may be used before or after surgery.
What are the complications of appendicitis?
Complications
- If left untreated, appendicitis can lead to serious complications, including:
- Rupture of the appendix, which can cause peritonitis (a dangerous infection of the abdominal lining)
- Abscess formation (a pocket of pus)
- Sepsis (a life-threatening response to infection)
Can homeopathy cure appendicitis?
Homeopathy may offer supportive care for some individuals experiencing early symptoms of appendicitis. However, it’s crucial to understand that homeopathic remedies are not a replacement for conventional medical diagnosis and treatment, which typically involves surgery (appendicectomy).
Which homeopathic remedies are commonly used for appendicitis?
Homoeopathic remedy for Appendicitis
- Belladonna: For severe pain and sensitivity in the lower right abdomen.
- Bryonia Alba: For sharp, stitching pains and constipation.
- Arsenicum Album: For symptoms suggesting infection, such as chills, fever, and diarrhea.
It’s essential to consult a qualified homeopathic practitioner to determine the most appropriate remedy and dosage.
Is it safe to use homeopathy for appendicitis?
Homoeopathic for Appendicitis
While homeopathic remedies are generally considered safe, delaying conventional medical treatment for appendicitis can lead to serious complications. If you suspect appendicitis, seek immediate medical attention.
Are there any risks or side effects associated with using homeopathy for appendicitis?
Homeopathic remedies are generally considered safe when used correctly. However, it’s important to be aware that delaying or avoiding conventional medical treatment for appendicitis can have serious consequences.


