Amenorrhea
Definition
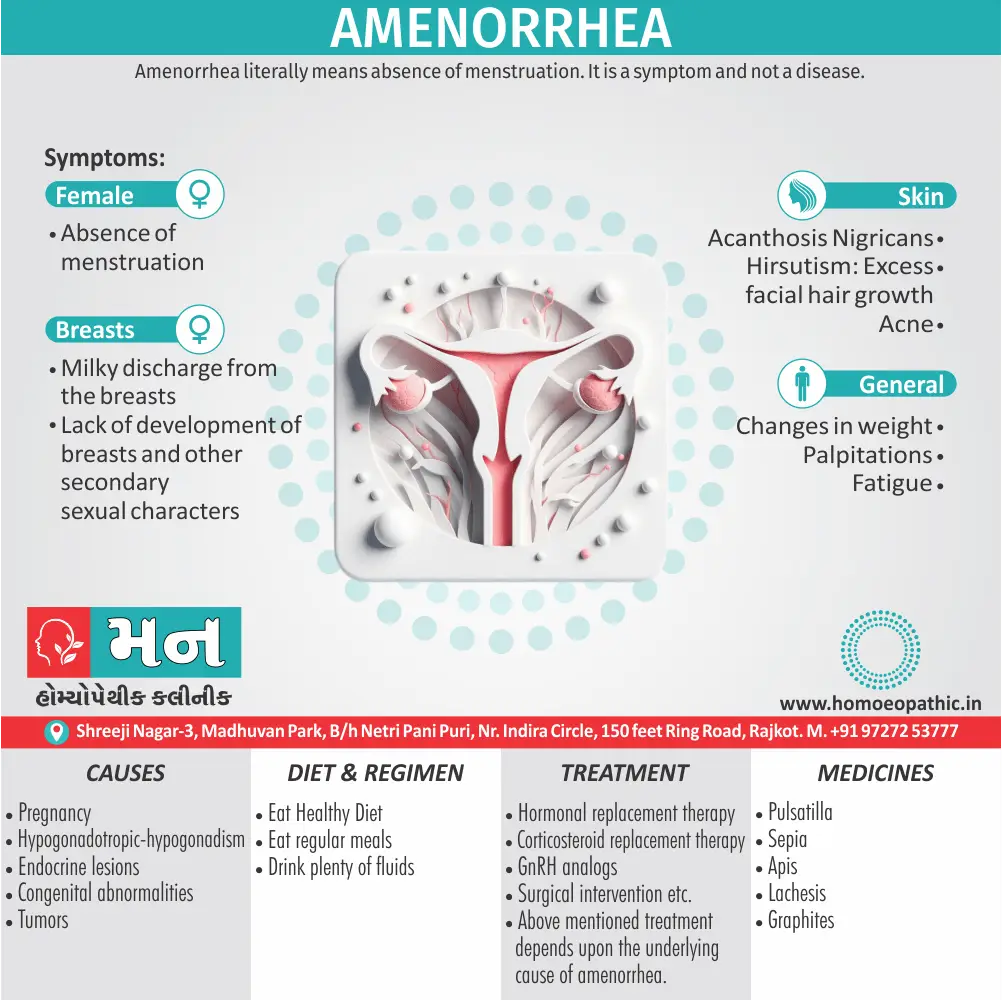
Amenorrhea literally means absence of menstruation. It is a symptom and not a disease.[2]
- Missing periods: This is a clear and understandable way to describe the condition in a general conversation.
- Absent menstruation: This is a more formal way to say "missing periods."
For medical contexts, some related terms can be used:
Primary Amenorrhea:
This refers to the absence of a first period by age 15.
Secondary Amenorrhea:
This refers to missing periods for three or more cycles in someone who previously had regular periods.
There aren’t many perfect synonyms for amenorrhea in everyday speech. However, depending on the context, some words or phrases that get close to the meaning include:
- Missed period(s) – This is a clear and common way to describe the absence of a period, but it’s not specific to amenorrhea (which can be longer than just missing one period).
- Absent period(s) – Similar to "missed period(s)", but emphasizes the lack of bleeding.
- Suppressed period(s) – This implies an underlying reason for the missing period, but doesn’t specify what that reason is.
For a more technical synonym, you could use:
- Acyclic menstruation – This is a medical term that specifically refers to the absence of menstrual cycles.
Overview
Epidemiology
Causes
Risk Factors
Types
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Terminology
References
Also Search As
Overview
Overview of Amenorrhoea
Any patient fulfilling the following criteria should be evaluated as having clinical problem of amenorrhea:
- Absence of menses by the age of 14 years with the absence of growth or development of secondary sexual characteristics.
- Absence of menses by the age of 16 years with normal development of secondary sexual characteristics (two years after complete sexual maturation).
- In a woman who has been normally menstruating, the absence of periods for a length of time equivalent to a total of at least three of the previous cycle intervals or 6 months of amenorrhea.[3]
Epidemiology
Epidemiology Of Amenorrhea:
The epidemiology of amenorrhea in India varies depending on the specific type (primary vs. secondary) and the population studied. However, some key findings include:
Primary Amenorrhea:
- A study conducted at AIIMS, New Delhi (2017) found that the most common causes of primary amenorrhea were Mullerian anomalies (47%), gonadal dysgenesis (20.5%), and hypogonadotropic hypogonadism (14.7%). [10]
Menstrual Disorders (Including Amenorrhea):
- A study on adolescent girls in Aligarh (2019) reported an overall prevalence of menstrual disorders of 76.9%, with amenorrhea specifically affecting 21.3% of participants. [11]
Postpartum Amenorrhea:
- Research in Manipur (2012) found the median duration of postpartum amenorrhea to be 5.7 months, with factors like place of residence, infant mortality, and breastfeeding duration significantly influencing its duration. [12]
It is important to note that these studies represent specific populations and regions within India, and the prevalence of amenorrhea may vary across the country. Additionally, there may be limited data available on certain aspects of amenorrhea epidemiology in India.
Causes
Causes of Amenorrhoea:
A) Primary Amenorrhea
- A young girl who has not yet menstruated by her 16 years of age is having primary amenorrhea rather than delayed menarche.
- The normal upper age limit for menarche is 15 years.
Causes:
Hypogonadotropic hypogonadism
- Delayed puberty: delayed GnRH pulse reactivation.
- Hypothalamic and pituitary dysfunction : Gonadotropin deficiency due to stress, weight loss, excessive exercise, anorexia nervosa, chronic disease (tuberculosis).
- Kallmann’s syndrome
- Central nervous system tumours
Hypergonadotropic hypogonadism
- Primary ovarian failure
- Resistant ovarian syndrome
- Galactosemia
- Enzyme deficiency (17 α hydroxylase deficiency)
- Others
Abnormal chromosomal pattern
- Turner’s syndrome (45 X)
- Pure gonadal dysgenesis (46 XX or 46 XY)
- Androgen insensitivity syndrome (Testicular feminization syndrome), (46 XY)
- Partial deletions of the X chromosome (46 XX).
Developmental defect of genital tract
- Imperforate hymen.
- Transverse vaginal septum.
- Atresia upper-third of vagina and cervix.
- Complete absence of vagina.
- Absence of uterus in MRKH syndrome
Dysfunction of thyroid and adrenal cortex
- Adrenogenital syndrome.
- Cretinism.
Metabolic disorders
- Juvenile diabetes.
Systemic illness
- Malnutrition, anaemia
- Weight loss
- Tuberculosis.
Unresponsive endometrium
- Congenital
- Uterine synechiae (tubercular)
B) Secondary Amenorrhoea
- It is the absence of menstruation for 6 months or more in a woman in whom normal menstruation has been established.
Causes:
Uterine factors:
- Tubercular endometritis
- Post radiation
- Synechiae: There is formation of adhesions following postabortal and puerperal curettage and following diagnostic curettage in dysfunctional uterine bleeding.
- Surgical removal
Ovarian factors:
- Polycystic ovarian syndrome
- Premature ovarian failure
- Resistant ovarian syndrome
- Hyper oestrogenic state
- Persistent follicles in metropathia
- Feminizing tumour of the ovary (Granulosa cell tumour)
- Masculinizing tumour of the ovary (Sertoli-leydig cell tumours)
- Hypo-estrogenic state
- Ablation of the ovaries
- Pelvic radiation
Pituitary factors:
- Adenoma (Prolactinoma)
- Cushing’s disease
- Acromegaly
- Sheehan’s syndrome
- Simmond’s disease (unrelated to pregnancy)
Hypothalamic factors
- Psychogenic shock, stress, anorexia nervosa, strenuous exercise, pseudocyesis, etc.
- Congenital malformation
- Trauma: Accidents, surgery or radiotherapy
- Infection: Tubercular or sarcoid granulomas
- Tumours: craniopharyngioma, meningioma
Adrenal factors
- Adrenal tumour or hyperplasia
- Cushing syndrome
Thyroid factors
- Hypothyroid state
General disease
- malnutrition, tuberculosis, chronic nephritis, diabetes, etc.
Iatrogenic
- Contraceptive pills (post pill amenorrhea)
- Psychotropic phenothiazine derivative drugs
- Antihypertensive drugs like reserpine ordopamine antagonists [2]
Risk Factors
Risk Factors of Amenorrhea:
For primary amenorrhea:
Chromosomal abnormalities:
- Turner syndrome (45,X), androgen insensitivity syndrome (46,XY)
Congenital anomalies:
- Müllerian agenesis (absence of uterus and upper vagina), imperforate hymen, transverse vaginal septum
Hypothalamic-pituitary disorders:
- Kallmann syndrome (anosmia and hypogonadotropic hypogonadism), functional hypothalamic amenorrhea
Gonadal dysgenesis:
- Swyer syndrome (46,XY gonadal dysgenesis)
Other:
- Craniopharyngioma (brain tumor), autoimmune polyglandular syndrome
For secondary amenorrhea:
Pregnancy:
- Most common cause
Hypothalamic-pituitary disorders:
- Functional hypothalamic amenorrhea (due to stress, weight loss, or excessive exercise), hyperprolactinemia
Ovarian disorders:
- Premature ovarian insufficiency (POI), polycystic ovary syndrome (PCOS)
Uterine disorders:
- Asherman syndrome (intrauterine adhesions)
Systemic disorders:
- Thyroid dysfunction, Cushing syndrome, chronic illness
Medications:
- Antipsychotics, antidepressants, chemotherapy, hormonal contraceptives
Note: This is not an exhaustive list, and other risk factors may exist. It is important to consult with a healthcare professional for proper evaluation and diagnosis [13]
Types
Clinical Types of Amenorrhoea
1. Physiological Amenorrhoea
Primary
- Before Puberty:
- The pituitary gonadotropins are not enough to stimulate the ovarian follicles for effective steroidogenesis → oestrogen levels are not sufficient to cause bleeding from the endometrium.
Secondry
During Pregnancy
- Large number of oestrogens and chorionic gonadotropins secreted from the trophoblasts suppress the pituitary gonadotropins → no maturation of the ovarian follicles.
During Lactation
- High level of prolactin → inhibits ovarian response to FSH → no follicular growth → hypoestrogenic state → no menstruation.
- If the patient does not breastfeed her baby, the menstruation returns by 6th week following delivery in about 40 percent and by 12th week in 80 percent of cases.
- If the patient breastfeeds her baby, the menstruation may be suspended in about 70 percent until the baby stops breast-feeding.
Following Menopause
- As women grow older, their ovarian follicles diminish in number due to atresia and ovulation.
- the leading producers of estradiol and inhibin B.
- As a result, a failure of endometrial development occurs, which may cause irregular menstrual cycles until menses eventually stop completely. [9]
2. Pathological Amenorrhoea
Concealed (Cryptomenorrhea)
- In cryptomenorrhea, there is periodic shedding of the endometrium and bleeding, but the menstrual blood fails to come out from the genital tract due to obstruction in the passage.
1. Congenital
- Imperforate hymen
- Transverse vaginal septum
- Atresia of upper-third of vagina and cervix.
2. Acquired
- Stenosis of the cervix following amputation, deep cauterization and conization.
- Secondary vaginal atresia following neglected and difficult vaginal delivery.
3. Real
A) Primary Amenorrhea
B) Secondary Amenorrhea
Pathophysiology
Pathophysiology of Amenorrhoea
The basic requirements for normal menstrual cycles include four anatomically and functionally distinct structural components:
- The hypothalamus, anterior pituitary gland, ovary, and the genital outflow tract composed of the uterus, endometrium, cervix, and vagina.
- If any of these components are nonfunctional or abnormal, menstrual bleeding may not occur; however, the precise pathophysiology associated with amenorrhea may vary based on the underlying aetiology and sometimes may be unclear.[6]
Clinical Features
Clinical Features of Amenorrheea:
Primary Amenorrhea:
Absence of menarche:
- By age 15 years in the presence of normal growth and secondary sexual development, or by age 13 years in the absence of secondary sexual characteristics
Hypogonadotropic hypogonadism:
- Short stature, anosmia (Kallmann syndrome)
Hypergonadotropic hypogonadism:
- Eunuchoidal proportions (long limbs relative to trunk), streak ovaries (Turner syndrome)
Androgen insensitivity syndrome:
- Breast development without pubic or axillary hair
Mullerian anomalies:
- Normal breast and pubic hair development, abdominal pain from hematocolpos (accumulation of blood in vagina due to obstruction)
Imperforate hymen or transverse vaginal septum:
- Normal breast and pubic hair development, abdominal pain, palpable vaginal mass
Constitutional delay of growth and puberty (CDGP):
- Delayed breast development, bone age less than chronologic age
Secondary Amenorrhea:
Absence of menses:
- For 3 or more consecutive months in women who have previously menstruated
Pregnancy:
- Nausea, breast tenderness, positive pregnancy test
Hypothalamic amenorrhea:
- Weight loss, excessive exercise, stress, eating disorders
Hyperprolactinemia:
- Galactorrhea (milky nipple discharge), headache, visual field changes
Premature ovarian insufficiency (POI):
- Hot flashes, vaginal dryness, decreased libido
Polycystic ovary syndrome (PCOS):
- Hirsutism (excess hair growth), acne, obesity, infertility
Asherman syndrome:
- Infertility, recurrent pregnancy loss, scant menses after dilation and curettage (D&C) [13]
Sign & Symptoms
Sign & symptoms of Amenorrhoea
- Absence of menstruation.
Primary Amenorrhea
- No history of menstruation with secondary sex characteristics present (eg, thelarche, pubic and axillary hair) by the age of 15 years or 3 years after thelarche
- No history of menstruation and no breast development or other secondary sex characteristics present in an adolescent girl aged 13 years [6]
- Other signs are evaluated based on underlying cause.[6]
secondary Amenorrhea
- History of infrequent and irregular periods (suggesting anovulation)
- Galactorrhoea to assess for hyperprolactinemia
- Thyroid symptoms should also be evaluated (fatigue, weight changes, skin/hair/nail changes, palpitations, tachycardia).
- Hirsutism and acne suggest PCOS [7]
Clinical Examination
Clinical Examination of Amenorrhea:
General Examination:
- Vital signs: Blood pressure, heart rate, respiratory rate, temperature
- Height and weight: Assess for underweight (BMI <18.5 kg/m²) or overweight/obesity (BMI ≥25 kg/m²)
- Body habitus: Note any signs of androgen excess (hirsutism, acne) or Turner syndrome (short stature, webbed neck, shield chest)
- Skin: Look for signs of hyperpigmentation (Addison’s disease) or striae (Cushing’s syndrome)
- Breast examination: Assess for Tanner stage (degree of breast development), galactorrhea (milky nipple discharge)
- Thyroid examination: Palpate for goiter (enlarged thyroid gland)
Pelvic Examination:
- External genitalia: Inspect for Tanner stage (degree of pubic hair development), clitoromegaly (enlarged clitoris), labial fusion
- Vaginal examination: Assess for vaginal patency, estrogen status (vaginal mucosa thickness), discharge, masses (hematocolpos)
- Bimanual examination: Palpate for uterine size and shape (normal, enlarged, absent), adnexal masses (ovarian cysts)
- Rectovaginal examination: Assess for rectovaginal septum, pelvic masses
Neurologic Examination:
- Visual fields: Assess for bitemporal hemianopsia (loss of outer half of visual field in both eyes) suggestive of pituitary tumor
- Cranial nerves: Test for anosmia (loss of smell) associated with Kallmann syndrome
- Deep tendon reflexes: Check for hyperreflexia associated with hypothyroidism
Additional Examinations (if indicated):
- Breast ultrasound: If galactorrhea is present
- Transvaginal ultrasound: To assess for uterine and ovarian abnormalities
- Brain MRI: If pituitary tumor is suspected
Note: The extent of the clinical examination will depend on the patient’s history, age, and presenting symptoms. A comprehensive evaluation is essential for determining the underlying cause of amenorrhea and guiding appropriate management. [13]
Diagnosis
Diagnosis of Amenorrhoea
Gonadal dysgenesis or POI
- Patent vagina and normal cervix and uterus noted on exam with signs of decreased estrogen (ie, no breast bud development, vaginal atrophy) or androgen (ie, no pubic hair)
- Elevated serum FSH and LH
- Decreased serum estrogen
- Ovaries may or may not be visible on ultrasound imaging
Müllerian agenesis
- Normal breast, sexual hair development, and external female genitalia; short vagina, ending in a blind pouch often noted
- Partial or complete absence of the müllerian structures (ie, upper vagina, cervix, uterus, and fallopian tubes) on clinical exam and ultrasound imaging
- Normal serum FSH and estrogen
- Other urogenital anomalies may also be noted on imaging
Transverse vaginal septum
- Similar findings to müllerian agenesis, except that müllerian structures are present on exam and ultrasound imaging
Imperforate hymen
- Normal breast, sexual hair development, and external female genitalia
- A bulging membrane (ie, the hymen) is visible when spreading the labia
- Normal serum FSH and estrogen
- Hematocolpos may be seen with transabdominal pelvic ultrasound
Constitutional delay of growth and puberty (CDGP)
- Little evidence of estrogen or androgens on an exam
- Normal anatomy on the pelvic exam and ultrasound
- Decreased FSH and estrogen levels
- Delayed bone age on radiography
- Family history is often consistent with CDGP
Functional hypothalamic amenorrhea (FHA)
- Similar presentation to CDGP, often with low BMI
- Typically associated with disordered eating, vigorous exercise, and systemic chronic disease
Polycystic ovary syndrome (PCOS)
- Normal thelarche and adrenarche on an exam, often with hirsutism and acne on an exam
- Serum FSH and estrogen within the normal range for reproductive-aged females
- Polycystic appearing ovaries on ultrasound imaging
- No clear consensus on diagnosing PCOS within 2 years of menarche exists; caution with diagnosis recommend in this age group
Complete androgen insensitivity syndrome (CAIS)
- Normal thelarche, often with very well-developed breasts but absent or sparse sexual hair
- Normal external female genitalia but no müllerian structures
- Testes within the pelvic cavity will be undescended and may be identified on ultrasound imaging
Ovarian Failure
- FSH is elevated and estradiol is low (The pituitary is yelling at the ovaries to make estrogen, but they are not responding.)
Hypothalamic Pituitary Dysfunction
- FSH is low and estradiol is low such as due to stress, exercise, or pituitary infarct (Sheehan’s syndrome).[6]
Differential Diagnosis
Differential Diagnosis of Amenorrhea:
The differential diagnosis of amenorrhea is broad and encompasses a wide range of conditions, categorized based on the primary or secondary nature of amenorrhea:
Primary Amenorrhea (Absence of menarche by age 15):
Chromosomal Abnormalities:
- Turner syndrome (45,X)
- Androgen insensitivity syndrome (46,XY)
- Swyer syndrome (46,XY gonadal dysgenesis)
Congenital Anomalies:
- Müllerian agenesis (absence of uterus and upper vagina)
- Imperforate hymen
- Transverse vaginal septum
Hypothalamic-Pituitary Disorders:
- Kallmann syndrome (anosmia and hypogonadotropic hypogonadism)
- Functional hypothalamic amenorrhea (due to stress, weight loss, or excessive exercise)
- Pituitary tumors (prolactinoma, craniopharyngioma)
Gonadal Disorders:
- Gonadal dysgenesis (46,XX or 46,XY)
Constitutional Delay of Growth and Puberty (CDGP)
Secondary Amenorrhea (Absence of menses for 3 or more months):
Pregnancy:
- Most common cause
Hypothalamic-Pituitary Disorders:
- Functional hypothalamic amenorrhea
- Hyperprolactinemia (due to prolactinoma or other causes)
Ovarian Disorders:
- Premature ovarian insufficiency (POI)
- Polycystic ovary syndrome (PCOS)
Uterine Disorders:
- Asherman syndrome (intrauterine adhesions)
Systemic Disorders:
- Thyroid dysfunction (hypothyroidism or hyperthyroidism)
- Cushing syndrome
- Chronic illness (e.g., diabetes, celiac disease)
Medication-Induced:
- Antipsychotics
- Antidepressants
- Chemotherapy
- Hormonal contraceptives [13]
Investigations
Investigation of Amenorrhoea
- Urine pregnancy test to exclude pregnancy
- Follicular stimulating hormone (FSH)/Luteinising hormone (LH)
- (FSH is elevated in ovarian failure,
- FSH is low in hypothalamic-pituitary dysfunction)
- Serum prolactin level (elevated)
- Thyroid function test (elevated or low)
- Progestogen challenge test
- Ultrasonography
- Transvaginal Ultrasonography
- Hysteroscopy
- Blood Sugar [4]
Treatment
Treatment of Amenorrhoea
Development Anomalies
- Complete agenesis of vagina:Vaginal reconstruction is the accepted form of treatment.
Chromosomal Abnormalities
- Hormone replacement therapy
Metabolic and Nutritional
- Underlying cause is treated
Hypothalamopituitary ovarian axis defect
- Oral oestrogen and progestin therapy
- GnRH Analogs
Thyroid and adrenal dysfunction
- Corticosteroid replacement therapy
Unresponsive Endometrium
- Uterine synechia (tubercular origin): Antitubercular drugs supplemented by adhesiolysis and intrauterine contraceptive device (IUCD) insertion.
- Congenital unresponsive endometrium: No known treatment is there.[2]
Prevention
Prevention of Amenorrhoea
- Promote healthy lifestyle
- Include nutritious diet
- Do appropriate levels of exercise and attention to one’s mental health should be stressed.[6]
- Eat Healthy Diet
- Eat regular meals
- Drink plenty of fluids
Homeopathic Treatment
Homeopathic Treatment of Amenorrhea
- Homeopathy treats the person as a whole.
- It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition.
- The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’? The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition. The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Amenorrhea:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity, but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor. So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines for Amenorrhoea:
PULSATILLA:
- Delayed menses after getting feet wet.
- Menses come too late.
- Flow is thick and changeable in character.
- Blood flows, stops and flows again.
- Sometimes there is intermittent flow, mixed with clots or fluid coagulable in character.
- Flow is more during the day and while walking.[5]
CALCAREA CARBONIC [CALC]
- This remedy is also, like Pulsatilla, indicated in amenorrhoea when the first menses are delayed, but with Calcarea there is apt to result congestion to the head or chest, giving rise to lung troubles.
- It is typically indicated in fleshy, scrofulous girls with fair complexion, perspiring easily about the head and subject to acidity of the stomach.
- Menstrual suppression in those decidedly scrofulous, or with lung affection, especially indicates Calcarea.
FERRUM METALLICUM [FERR]
- This is another useful remedy for delayed first menses where there is debility, languor, palpitation, sickly complexion and puffiness about the ankles.
- It corresponds to weakly, chlorotic women with flushed face, or pale and livid with blue margins about the eyes.
- It is especially useful in those who have been dosed with quinine and nervines.
SEPIA [SEP]
- Insufficient or tardy menstruation occurring in the feeble and debilitated, those of dark complexion, delicate skin and who are sensitive to all impressions.
- In delay of first menses where a leucorrhoea occurs in their stead with determination of blood to the chest and pale face, the remedy is well indicated.
CIMICIFUGA
- Cowperthwaite praises this remedy highly in amenorrhoea, giving it when no special indication are present, in nervous women subject to rheumatism or arthritic attacks, with aggravation of mental symptoms when the menses should appear.[8]
SENECIO
- Called "the female regulator".
- Menses delayed or absent.
- Wandering pains in back and shoulders.
- Nervous irritability.
ACONITE
- Suppression of menses after fright.
- In young girls of a full plethoric habit who lead a sedentary life.
Diet & Regimen
Diet & Regimen of Amenorrhoea
- Eat Healthy Diet
- Eat regular meals
- Drink plenty of fluids
Terminology
Terminologies and Meanings:
- Amenorrhea: The absence of menstrual periods. It can be primary (never having had a period) or secondary (cessation of periods after they have begun).
- Menarche: The first occurrence of menstruation in a female.
- Cryptomenorrhea (Concealed Menstruation): A condition where menstrual bleeding occurs but is not visible due to an obstruction in the genital tract.
- Hypogonadotropic Hypogonadism: A condition where the ovaries are not stimulated adequately due to low levels of hormones from the pituitary gland.
- Hypergonadotropic Hypogonadism: A condition where the ovaries are not functioning properly, leading to high levels of hormones from the pituitary gland trying to compensate.
- Mullerian Anomalies: Congenital abnormalities of the female reproductive tract.
- Kallmann Syndrome: A genetic condition characterized by delayed puberty and an impaired sense of smell.
- Turner Syndrome: A chromosomal condition in females where one X chromosome is missing or partially missing.
- Androgen Insensitivity Syndrome (AIS): A genetic condition where the body is unable to respond to male sex hormones (androgens).
- Polycystic Ovary Syndrome (PCOS): A hormonal disorder causing enlarged ovaries with small cysts on the outer edges.
- Premature Ovarian Insufficiency (POI): Also known as premature menopause, it’s the loss of normal ovarian function before age 40.
- Asherman Syndrome: A condition where scar tissue (adhesions) forms inside the uterus.
- Hyperprolactinemia: A condition where there are higher-than-normal levels of the hormone prolactin in the blood.
- GnRH Analogues: Medications that mimic the action of gonadotropin-releasing hormone (GnRH) to regulate the menstrual cycle.
References
References of Amenorrhoea
- Obestretics and Gynecology Sixth Edition
- DC Dutta’s Gynecology
- Sudha Salhan Textbook of Gynecology
- Practical Obstretics and Gynecology Handbook
- Textbook of Materia Medica by Dr. J.D.Patil
- Primary Amenorrhea – StatPearls – NCBI Bookshelf (nih.gov)
- Secondary Amenorrhea – StatPearls – NCBI Bookshelf (nih.gov)
- Practical Homoeopathic Therapeutics By Dewey W.A.
- https://www.ncbi.nlm.nih.gov/books/NBK507826/
- Etiology and management of primary amenorrhea: A study of 102 cases at tertiary centre(2017).https://pubmed.ncbi.nlm.nih.gov/29241916/
- Prevalence of Menstrual Disorders and Their Association with Physical Activity in Adolescent Girls of Aligarh City. (2019). International Journal of Health Sciences & Research (IJHSR). https://www.ijhsr.org/IJHSR_Vol.9_Issue.8_Aug2019/53.pdf
- Postpartum amenorrhoea among Manipuri women: a survival analysis. (2012). Journal of Health, Population, and Nutrition.https://pubmed.ncbi.nlm.nih.gov/22524125/
- Williams Gynecology, 4th Edition (2020)
Also Search As
Also Search As
Online Search Engines:
- Keywords: Using search engines like Google, Bing, or DuckDuckGo, people can search for terms like "amenorrhea," "absent periods," "missed periods," or "causes of amenorrhea."
- Specific Questions: They can also search for specific questions like "what are the symptoms of amenorrhea?" or "how is amenorrhea diagnosed?"
Medical Websites and Databases:
- Reputable Sources: Look for websites ending in .edu (educational institutions), .gov (government), or .org (non-profit organizations) for reliable information.
- Medical Journals: Search for articles in medical journals using databases like PubMed or Google Scholar.
- Online Encyclopedias: Websites like MedlinePlus or Mayo Clinic provide comprehensive information on medical conditions, including amenorrhea.
Libraries and Bookstores:
- Medical Textbooks: Books like "Williams Gynecology" offer in-depth information on amenorrhea and other gynecological conditions.
- Health and Wellness Books: Some books provide general information on women’s health and may have sections on amenorrhea.
Talking to Healthcare Professionals:
- Doctors and Nurses: The most reliable way to get information on amenorrhea is to consult a doctor or healthcare professional. They can provide personalized advice based on individual circumstances.
Additional Tips:
- Use Reliable Sources: Be sure to evaluate the credibility of the information you find online.
- Consult Multiple Sources: Get a well-rounded understanding by consulting multiple sources of information.
- Don’t Self-Diagnose: If you are concerned about amenorrhea, it is important to see a doctor for a proper diagnosis and treatment plan.
There are several ways to search for information on the topic of amenorrhea:
General Search:
Search Engines: Use search engines like Google, Bing, or DuckDuckGo and type in keywords such as:
- "amenorrhea"
- "absent menstruation"
- "missed periods"
Online Encyclopedias: Search for information on websites like:
- Wikipedia: While not always the most reliable, it can offer a starting point for basic information.
- MedlinePlus (National Institutes of Health): Offers trustworthy health information.
- Mayo Clinic: Provides comprehensive medical information.
Academic and Medical Search:
Medical Databases: Use specialized databases to access scholarly articles and research papers:
- PubMed: A free database of biomedical literature.
- Google Scholar: A wider search engine that includes scholarly articles.
Medical Journals: Look for articles in reputable medical journals like:
- The New England Journal of Medicine
- The Lancet
- JAMA (The Journal of the American Medical Association)
Specific Search:
Causes of Amenorrhea: You can specify your search by adding terms like:
- "causes of amenorrhea"
- "risk factors for amenorrhea"
- "primary amenorrhea" (if you never had a period)
- "secondary amenorrhea" (if your periods have stopped)
Symptoms and Treatment: Search for terms like:
- "symptoms of amenorrhea"
- "treatment of amenorrhea"
- "natural remedies for amenorrhea" (if you’re interested in alternative approaches)
Additional Resources:
- Healthcare Professionals: Consult with your doctor or a gynecologist for personalized information and guidance.
- Patient Support Groups: Online forums or support groups can provide a platform to connect with others who have experienced amenorrhea.
- Books: Look for books on women’s health or specific books on amenorrhea at your local library or bookstore.
By using these various search methods, you can find a wealth of information on amenorrhea to learn about its causes, symptoms, diagnosis, and treatment options.
Frequently Asked Questions (FAQ)
What is amenorrhea?
Amenorrhea is the absence of menstrual periods for three or more consecutive months in women who have previously menstruated, or the absence of menarche (first period) by age 15.
What causes amenorrhea?
Causes can vary and include natural factors like pregnancy and menopause, but also hormonal imbalances, stress, weight loss, medical conditions (like PCOS), and certain medications.
How is amenorrhea diagnosed?
Diagnosis involves a thorough medical history, physical exam, and often includes blood tests to check hormone levels, and sometimes imaging studies like ultrasound or MRI.
What are the symptoms of amenorrhea?
The primary symptom is the absence of menstrual bleeding. Other potential symptoms can include headaches, vision changes, hair loss, acne, or excessive hair growth.
How does homeopathy treat amenorrhea?
Homeopathic treatment aims to address the root cause of amenorrhea by selecting individualized remedies that match the unique physical, mental, and emotional symptoms of each person.
Is homeopathic treatment safe for amenorrhea?
Homeopathic remedies are generally considered safe when prescribed by a qualified practitioner. They are highly diluted substances that work on the principle of "like cures like."
What are the treatment options for amenorrhea?
Treatment
Treatment depends on the underlying cause. It may involve lifestyle changes, hormone therapy, medication to treat underlying conditions, or surgery in some cases.
Which homeopathic remedies are commonly used for amenorrhea?
Homoeopathic Medicine For Amenorrhea
Some frequently used remedies include Pulsatilla, Sepia, Natrum Muriaticum, and Lachesis. However, the most suitable remedy depends on the individual’s specific symptom profile.
How long does it take to see results with homeopathic treatment for amenorrhea?
The response time varies depending on the individual and the underlying cause. Some may experience improvement within weeks, while others may require longer-term treatment.
Should I consult a homeopath for amenorrhea even if I am undergoing conventional treatment?
Yes, homeopathy can be used alongside conventional treatments, and a homeopath can work in collaboration with other healthcare providers to create a comprehensive treatment plan.
