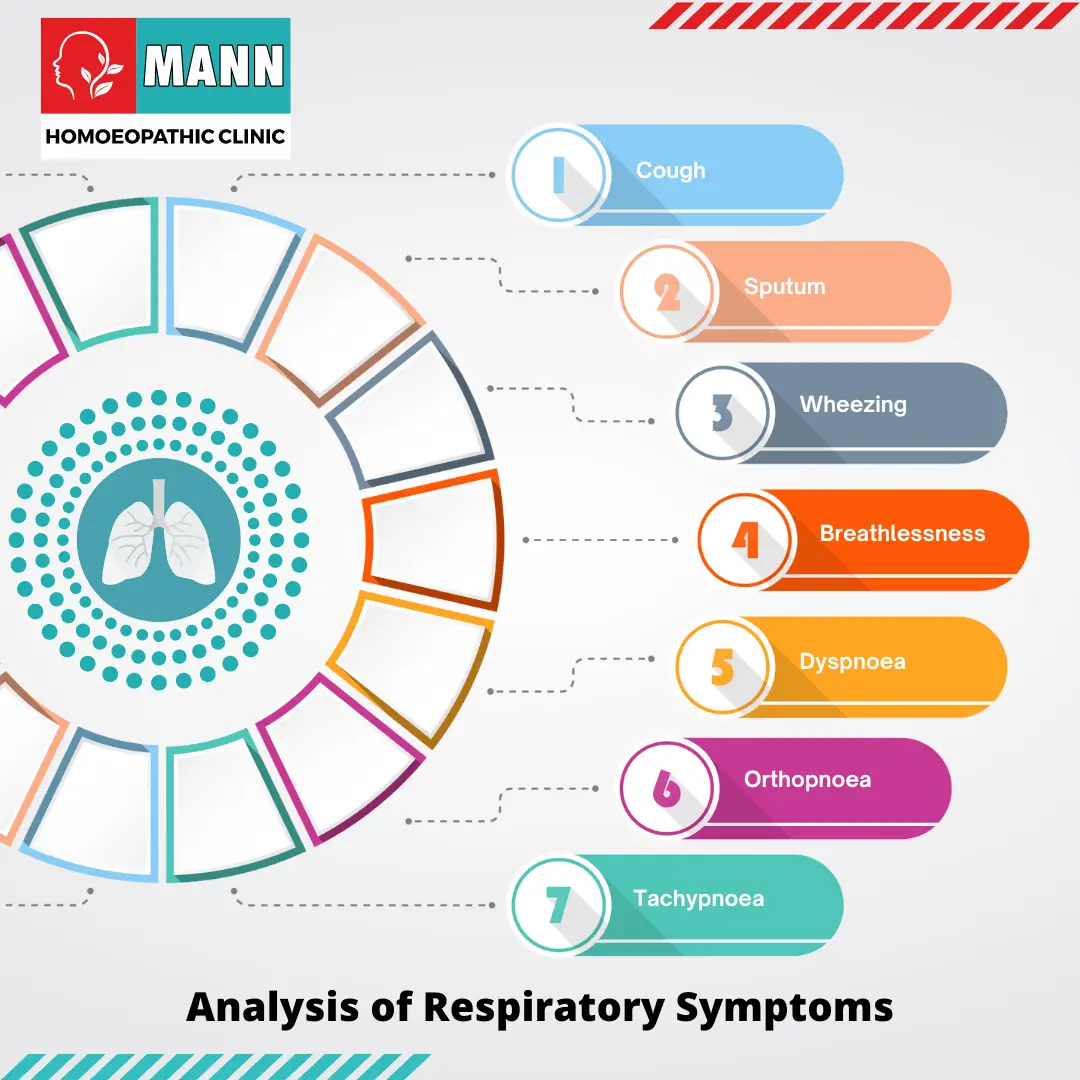
Analysis of Respiratory Symptoms
Definition:
Analysis of Respiratory Symptoms are indications of problems within the respiratory system, the network of organs responsible for breathing. This system includes the nose, throat, airways (windpipe and bronchi), lungs, and the muscles that help us breathe.
The Analyzing respiratory symptoms is a crucial step in diagnosing and managing respiratory conditions. Here’s a breakdown of the process, key symptoms, and their potential implications:
1. Core Respiratory Symptoms:
Cough:
A vital reflex to clear airways, it can be dry or produce phlegm (sputum).
Dyspnea (Shortness of Breath):
A feeling of breathlessness or difficulty breathing.
- Possible causes: Lung diseases, heart conditions, anxiety, or strenuous activity. Its severity and onset provide vital clues.
Wheezing:
A high-pitched whistling sound during breathing, often indicating narrowed airways.
- Possible causes: Asthma, COPD, allergies, or a foreign object obstructing the airway.
Chest Pain:
Can be sharp, dull, or pressure-like, and may worsen with breathing.
- Possible causes: Lung-related (pleurisy, pneumonia), heart-related (angina), or musculoskeletal problems.
Hemoptysis (Coughing up Blood):
A serious symptom warranting immediate medical attention.
- Possible causes: Infections, lung cancer, or blood clots in the lungs (pulmonary embolism).
2. Symptom Analysis:
Onset:
When did the symptoms start? Sudden or gradual?
Duration:
How long have the symptoms persisted? Acute or chronic?
Severity:
How bothersome are the symptoms? Mild, moderate, or severe?
Pattern:
Do symptoms follow a specific pattern (e.g., worse at night, with exertion, or in certain environments)?
Associated Symptoms:
Are there other symptoms like fever, chills, fatigue, or weight loss?
Aggravating/Relieving Factors:
What makes symptoms worse or better?
3. Diagnostic Tools:
Physical Examination:
Listening to the lungs with a stethoscope, checking oxygen levels.
Imaging:
Chest X-ray, CT scan to visualize lung structures.
Pulmonary Function Tests:
Measure lung capacity and airflow.
Sputum Analysis:
Identify pathogens or abnormal cells in coughed-up mucus.
Bronchoscopy:
Visual examination of the airways with a thin, flexible tube.
4. Importance of Analysis:
Early Diagnosis:
Identify respiratory problems early for better treatment outcomes.
Determine Severity:
Assess the severity of the condition to guide management.
Underlying Causes:
Uncover the root cause of the symptoms, be it infection, environmental factors, or chronic disease.
Treatment Planning:
Develop a targeted treatment plan based on the specific condition.
If you are experiencing respiratory symptoms, it’s essential to consult a healthcare professional for proper evaluation and diagnosis.
Important Note: The information provided here is for general knowledge and educational purposes only, and does not constitute medical advice. Always seek the guidance of a qualified healthcare provider for any questions you may have regarding a medical condition.
Overview
Sputum
Wheezing
Breathlessness
Decoding
Common Symptoms
When to See a Doctor
Self-Care Tips
Do’s and Don'ts
Terminology
References
Overview
Overview of Analysis of Respiratory Symptoms
Runny, blocked nose and sneezing in Analysis of Respiratory Symptoms
Analysis of Respiratory Symptoms– Nasal symptoms are extremely common and both common colds and allergic rhinitis cause ‘runny nose’ (rhinorrhoea), nasal blockage and attacks of sneezing. In allergic rhinitis, symptoms may be intermittent, following contact with pollens or animal danders, or persistent, especially when house-dust mite is the allergen. Colds are frequent during the winter but if the symptoms persist for weeks the patient probably has perennial rhinitis rather than persistent viral infection.
Nasal secretions are usually thin and runny in allergic rhinitis
but thicker and discoloured with viral infections. Nose bleeds and blood-stained nasal discharge are common and rarely indicate serious pathology. However, a blood-stained nasal discharge associated with nasal obstruction and pain may be the presenting feature of a nasal tumour. Nasal polyps typically present with nasal blockage and loss of smell.
Cough in Analysis of Respiratory Symptoms:
It is the commonest symptom of lower respiratory tract disease. Mechanical or chemical stimulation of cough receptors in the epithelium of the pharynx, larynx, trachea, bronchi, and diaphragm causes a cough.Afferent receptors transmit signals to the cough center in the medulla, which then generates efferent signals to the expiratory musculature.
Smokers often have a morning cough with a little sputum. A productive cough is the cardinal feature of chronic bronchitis, while dry coughing, particularly at night, can be a symptom of asthma. Cough also occurs in asthmatics after mild exertion or following forced expiration. Cough can also occur for psychological reasons without any definable pathology.
A worsening cough is the most common presenting symptom of lung cancer. Lung cancer, by infiltrating the left recurrent laryngeal nerve, paralyzes a vocal cord and thus eliminates the cough‘s normal explosive character (sometimes termed a bovine cough).". Cough can be accompanied by stridor in whooping cough or if there is laryngeal or tracheal obstruction.
Sputum
Sputum in Analysis of Respiratory Symptoms:
A healthy, non-smoking individual’s respiratory system produces approximately 100 mL of mucus daily. Cilia gradually move this mucus up the airways, through the larynx, where it is swallowed. The body expectorates any excess mucus as sputum. Excess mucus is expectorated as sputum. Cigarette smoking is the commonest cause of excess mucus production.
Mucoid sputum is clear and white but can contain black specks resulting from the inhalation of carbon. Yellow or green sputum is due to the presence of cellular material, including bronchial epithelial cells, or neutrophil or eosinophil granulocytes.
Yellow sputum is not necessarily due to infection, as eosinophils in the sputum, as seen in asthma, can give the same appearance. The production of large quantities of yellow or green sputum is characteristic of bronchiectasis.
Haemoptysis (blood-stained sputum) varies from small streaks of blood to massive bleeding.
Cause
- The commonest cause of mild haemoptysis is acute infection, particularly in exacerbations of chronic obstructive pulmonary disease (COPD) but it should not be attributed to this without investigation.
- Other common causes are pulmonary infarction, bronchial carcinoma and tuberculosis.
- In lobar pneumonia, the sputum is usually rusty in appearance rather than frankly blood-stained.
- Pink, frothy sputum is seen in pulmonary oedema.
- In bronchiectasis, the blood is often mixed with purulent sputum.
- Massive haemoptyses (>200 mL of blood in 24 hours) are usually due to bronchiectasis or tuberculosis.
- Uncommon causes of haemoptyses are idiopathic pulmonary haemosiderosis, Goodpasture’s syndrome, microscopic polyangiitis, trauma, blood disorders and benign tumours.
Haemoptysis should always be investigated. Although a diagnosis can often be made from a chest X-ray, a normal chest X-ray does not exclude disease. However, if the chest X-ray is normal, CT scanning and bronchoscopy are only diagnostic in about 5% of patients with haemoptysis.
Firm plugs of sputum may be coughed up by patients suffering from an exacerbation of allergic bronchopulmonary aspergillosis. Sometimes such sputum looks like casts of inflamed bronchi.
Wheezing
Wheezing in Analysis of Respiratory Symptoms:
It is a common complaint and results from airflow limitation due to any cause. The symptom of wheezing is not diagnostic of asthma; other causes include vocal chord dysfunction, bronchiolitis and chronic obstructive pulmonary disease (COPD). Conversely, wheeze may be absent in the early stages of asthma.
Chest pain in Analysis of Respiratory Symptoms:
The most common type of chest pain reported in respiratory disease is a localized sharp pain, often termed pleuritic. It is made worse by deep breathing or coughing and the patient can usually localize it. Localized anterior chest pain with tenderness of a costochondral junction is caused by costochondritis. Shoulder tip pain suggests irritation of the diaphragmatic pleura, while central chest pain radiating to the neck and arms is likely to be cardiac. Retrosternal soreness is associated with tracheitis, while malignant invasion of the chest wall causes a constant, severe, dull pain.
Breathlessness
Breathlessness of Analysis of Respiratory Symptoms
it should be assessed in relation to the
patient’s lifestyle. For example, a moderate degree of breathlessness will be totally disabling if the patient has to climb
many flights of stairs to reach home.
Dyspnoea
it is a sense of awareness of increased respiratory effort that is unpleasant and that is recognized by the patient as being inappropriate. Patients often complain of tightness in the chest; this must be differentiated from angina.
Orthopnoea
it is breathlessness on lying down. While it is classically linked to heart failure, it is partly due to the weight of the abdominal contents pushing the diaphragm up into the thorax. Such patients may also become breathless on bending over.
Tachypnoea and hyperpnoea
They are, respectively, an increased rate of breathing and an increased level of ventilation. These may be appropriate responses (e.g. during exercise).
Hyperventilation
it is inappropriate overbreathing. This may occur at rest or on exertion and results in a lowering of the alveolar and arterial PCO2.
Paroxysmal nocturnal dyspnoea
it is acute episodes of breathlessness at night, typically due to heart failure.
(Reference – Kumar and Clark’s Clinical Medicine 8th Ed.)
Decoding
Decoding Your Cough: A Guide to Analyzing Respiratory Symptoms
Feeling a tickle in your throat or struggling to catch your breath? Respiratory symptoms are incredibly common, affecting millions of people every year. While they can be disruptive, understanding them can help you determine the best course of action for getting back to feeling your best.
This guide will equip you to analyze your respiratory symptoms and navigate your path to feeling better.
Common Symptoms
Common Respiratory Symptoms:
Cough: Reflex that helps clear your airways of irritants and mucus. However, the type of cough can offer clues about the underlying cause.
Productive Cough: It brings up mucus or phlegm, often associated with a chest cold or sinus infection.
Dry Cough: Cough is hacking and unproductive, and may be caused by allergies, postnasal drip, or irritants like smoke.
Shortness of Breath: Feeling of breathlessness can be scary, but it doesn’t always indicate a serious problem. It can be caused by exertion, anxiety, asthma, or even heart conditions.
Chest Tightness: Uncomfortable feeling of pressure or tightness in your chest can be caused by conditions like costochondritis (inflammation of the cartilage in your ribs) or pleurisy (inflammation of the lining of your lungs).
When to See a Doctor
When to See a Doctor:
While many respiratory symptoms are mild and resolve on their own, certain signs indicate it’s time to seek medical attention:
- Fever above 100.4°F (38°C)
- Difficulty breathing at rest
- Wheezing (a high-pitched whistling sound when breathing)
- Coughing up blood
- Chest pain that worsens with breathing or movement
- Symptoms that don’t improve within a week.
Self-Care Tips
Self-Care Tips:
If your symptoms are mild, there are some simple things you can do at home to feel better:
- Rest: Allow your body to focus on healing.
- Hydration: Drinking plenty of fluids helps loosen mucus and soothe a sore throat.
- Humidifier: Adding moisture to the air can ease congestion and coughing.
- Over-the-counter Medications: Decongestants, cough suppressants, or pain relievers may provide temporary relief (consult the label and doctor if you have pre-existing health conditions).
Disclaimer:
This article provides information only and does not constitute medical advice.". Always consult a healthcare professional for diagnosis and treatment of any respiratory issue.
Bonus Tip:
By understanding your respiratory symptoms and taking appropriate steps, you can get back to feeling your best in no time. Remember, if your symptoms are severe or don’t improve within a reasonable timeframe, don’t hesitate to seek professional medical advice.
Do’s and Don'ts
Taking Charge of Your Respiratory Health: Additional Insights and Resources
Having explored common respiratory symptoms and self-care strategies, let’s delve deeper into taking charge of your respiratory health:
Preventive Measures:
- Frequent Handwashing: This simple act is the first line of defense against many respiratory illnesses.
- Maintain a Healthy Lifestyle: Getting enough sleep, eating a balanced diet rich in fruits and vegetables, and managing stress can all contribute to a strong immune system and lower your risk of infections.
- Avoid Smoking and Secondhand Smoke: Smoking is a major risk factor for lung cancer and chronic obstructive pulmonary disease (COPD).
- Vaccinations: Stay up-to-date on vaccinations like the flu shot and pneumonia vaccine, which can significantly reduce your risk of contracting these illnesses.
Terminology
Terminology
Understanding Common Respiratory Illnesses:
Knowing the most common respiratory conditions can help you manage your symptoms and navigate seeking help:
- The Common Cold: This viral infection usually causes a runny or stuffy nose, sore throat, and cough. It typically resolves on its own within a week.
- Flu: This more severe viral infection comes with fever, chills, muscle aches, fatigue, and respiratory symptoms. While most people recover within a few days to weeks, some individuals, especially young children and older adults, are at higher risk of complications.
- Sinusitis: Inflammation of the sinus cavities can cause facial pain, pressure, congestion, and a cough that worsens at night or when bending forward.
- Allergies: Seasonal allergies can trigger a runny or stuffy nose, itchy eyes, sneezing, and coughing.
- Asthma: This chronic condition causes inflammation and narrowing of the airways, leading to wheezing, coughing, chest tightness, and shortness of breath.
References
References
- National Institutes of Health (NIH): https://www.nhlbi.nih.gov/
- Centers for Disease Control and Prevention (CDC): https://www.cdc.gov/
- American Lung Association: https://www.lung.org/
Frequently Asked Questions (FAQ)
How long does it take to see improvement with homeopathic treatment for respiratory symptoms?
The response time varies depending on the individual, the nature of the symptoms, and their duration. Acute conditions may respond quickly, while chronic issues might require longer-term treatment.
Is homeopathic treatment safe for respiratory issues?
Yes,Homeopathic remedies are safe. However, it’s crucial to consult a qualified homeopath for proper assessment and treatment.
Can homeopathy help with chronic respiratory conditions like asthma or COPD?
While homeopathy cannot cure these conditions, it may offer supportive care by addressing symptom severity and frequency, potentially reducing reliance on conventional medications.
Can I use homeopathy with conventional medicine for my respiratory problems?
In many cases, homeopathy can be integrated with conventional treatments. Open communication with both your homeopath and conventional doctor is essential.
How does a homeopath choose the right remedy for respiratory symptoms?
Remedy selection involves a thorough case-taking process, where the homeopath gathers detailed information about the individual’s symptoms, medical history, and overall constitution.
What common respiratory symptoms does homeopathy address?
Symptoms
Homeopathy addresses a wide array of respiratory symptoms, including coughs (dry, productive, spasmodic), shortness of breath, wheezing, chest tightness, and nasal congestion.
How does homeopathy analyze respiratory symptoms?
Homeopathic analysis delves into the unique characteristics of each symptom, considering factors like timing, triggers, modalities (what makes it better or worse), and accompanying sensations.
Are there specific homeopathic remedies for respiratory symptoms?
Homoeopathic remedies for respiratory system
Yes, there are numerous remedies, each suited to particular symptom presentations. Common examples include Aconite for sudden onset with anxiety, Bryonia for dry coughs worsened by movement, and Antimonium Tartaricum for rattling coughs with difficulty expectorating.
