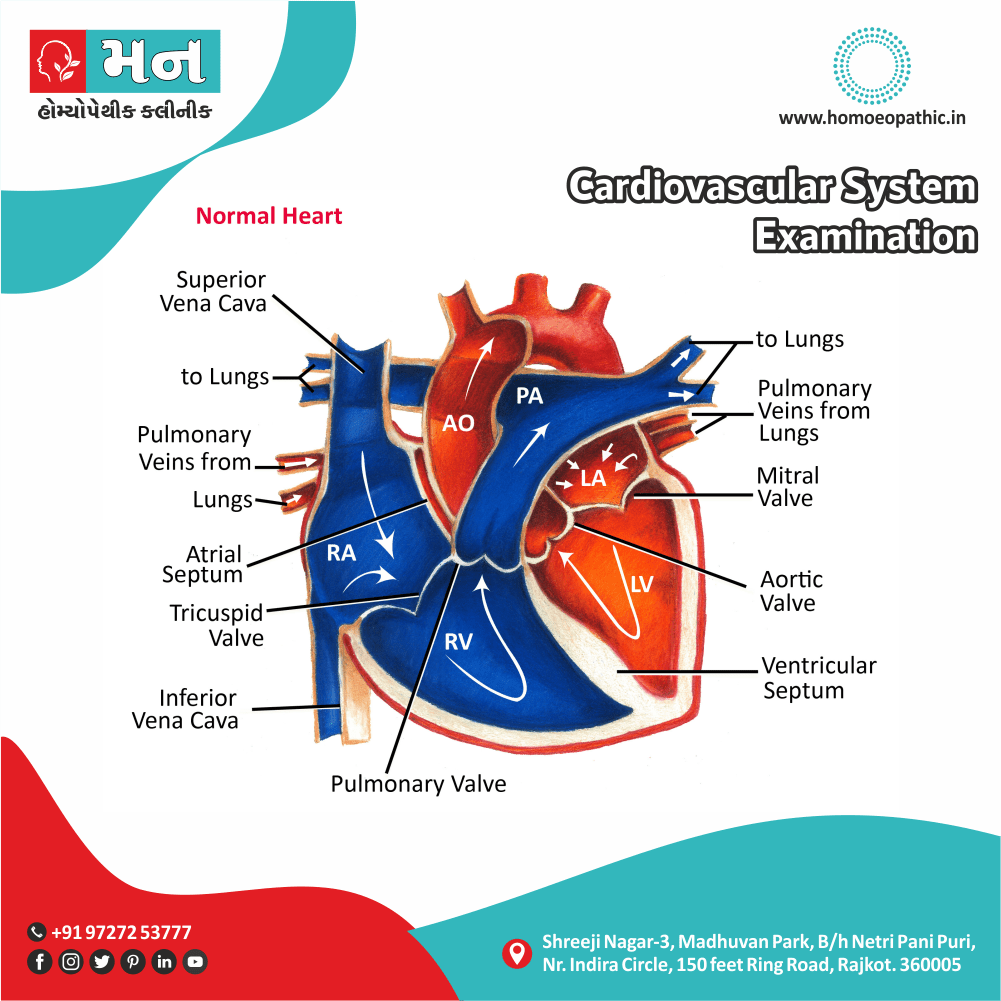
Cardiovascular System Examination
Definition
Before a detail Cardiovascular System Examination is begun, it is always helpful to ask the patient’s background history as to his age, occupation, hobbies, family history and past history of cardiac, metabolic, connective tissue or neoplastic disease, as well as whether the patient is experiencing any symptoms currently.
Also, the blood pressure, heart rate and Jugular Venous Pressure (JVP) need to review before beginning the physical examination.
Formal Synonyms:
- Cardiovascular assessment: This is a general term for evaluating the health of the cardiovascular system.
- Cardiac evaluation: This focuses specifically on the heart, but can be part of a broader cardiovascular exam.
- Circulatory examination: This emphasizes the blood circulation aspect of the cardiovascular system.
Informal Synonyms (use with caution in some contexts):
- Heart check: This is a simple and understandable term for a general audience.
- Cardio check-up: Similar to "heart check," but emphasizes a planned examination.
More Specific Examinations (within Cardiovascular System Examination):
- Echocardiogram exam: This refers to an ultrasound examination of the heart.
- Electrocardiogram (ECG) test: This measures the electrical activity of the heart.
- Chest X-ray: While not specific to the heart, it can be used to assess the heart size and lungs (which can be affected by heart issues).
Choosing the Right Term:
- Medical Setting: Use "cardiovascular system examination" or a more specific term like "cardiac evaluation" for clarity.
- Patient Education: "Heart check" or "cardiovascular assessment" might be easier for patients to understand.
- Informal Settings: "Heart check-up" is acceptable for casual conversation.
Additionally:
- You could describe the purpose of the examination, such as "an examination to assess the health of your heart and blood vessels."
Remember:
- The most appropriate term depends on the context and audience.
- In a medical setting, prioritize accuracy and use established medical terms.
INSPECTION
PALPATION
PERCUSSION
AUSCULTATION
INSPECTION
Inspection Of Cardiovascular System Examination :
ANAEMIA
Look for pallor of mucous membranes; however a haemoglobin measurement is necessary to confirm anaemia.
CYANOSIS
Look for any bluish discoloration of the skin and mucosae. Peripheral cyanosis occurs due to a sluggish blood flow which seen in cases of cardiac failure. Central cyanosis, or bluish mucosae, may observe in cases of pulmonary oedema and congenital heart diseases like Fallot’s tetralogy and Eisenmenger’s syndrome.
Cyanosis of the malar area call mitral facies and typically seen in cases of mitral stenosis complicated by pulmonary hypertension.
CLUBBING
Clubbing of the fingers and, in some cases, toes can seen in cardiac conditions like Congenital Cyanotic Heart Disease and Infective Endocarditis.
OEDEMA
Examine the ankles, sacrum and torso for pitting type of oedema, which may suggest a case of Congestive Cardiac Failure.
DEFORMITIES
Look for deformities of the chest wall as a funnel chest or pectus excavatum may displace the apex, and give a false positive impression of enlargement of the heart.
PRECORDIUM
The anterior part of the chest overlying the heart, called the precordium, has a smooth and faintly convex form. The precordium abnormally appears bulging if there is cardiac enlargement, pericardial effusion, pleural effusion, etc. It may flattened in cases of a congenital deformity or old pleural/pericardial effusion.
APEX IMPULSE
The apex impulse, also called the left ventricular thrust, is the point of maximum outward movement of the left ventricle of the heart during systole, normally localized in the fifth left intercostal space in the mid-clavicular line. It usually seen when the patient is in the supine position, but if not, then turning the patient in the left lateral position makes the impulse visible in the anterior axillary line. Apex impulse gets obliterated when the patient has a pericardial effusion, or even in cases of emphysema.
VENOUS COLLATERALS
Prominent venous collaterals over the chest wall may seen in cases of superior and inferior venacaval obstruction. I am text block. Click edit button to change this text. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
PALPATION
PALPATION:
APEX BEAT-
AREA OF LEFT VENTRICLE:
It is the furthermost point laterally and inferiorly where the cardiac impulse is felt. Normally, it can palpated at the point of intersection of the left 5th intercostal space and the left mid-clavicular line. In those patients where the apex beat cannot felt in the supine position, examine the patient in left lateral decubitus. If the beat can still not palpate, ask the patient to exhale completely and hold his breath for a few seconds.
The apex beat is assessed as per its:
LOCATION–
The typical location is the point of intersection of the left 5th intercostal space and the left mid-clavicular line in the supine decubitus. A laterally displaced apex beat suggests ischemic heart disease, congestive cardiac failure and cardiomyopathy. If the apex beat is absent, it suggests dextrocardia, pericardial effusion, pleural effusion and emphysema. Obesity or a highly muscular chest wall may also make the apex beat undetectable.
DIAMETER–
The diameter of the apex beat in the supine position is usually less than 2.5 cm. In cases of left ventricular enlargement, the diameter is greater than 3 cm.
DURATION–
The duration of the apex beat can assessed by auscultating for heart sounds while feeling the beat. Usually the duration lasts for the first two-thirds of systole. When the impulse sustained throughout the period of systole, it called heaving apex, which seen in left ventricular hypertrophy. In aortic stenosis, where there primarily systolic overload, the heave well-sustained. In aortic or mitral regurgitation, where there primarily diastolic overload, the heave is ill-sustained.
AMPLITUDE–
The amplitude of the apex beat is brisk and small. Increased or hyperkinetic amplitude may seen in normal conditions like post-exercise or during any excitement, or in pathological conditions like aortic stenosis, mitral regurgitation, left ventricular hypertrophy, severe anaemia and hyperthyroidism. Dilated cardiomyopathy will manifest as a hypokinetic apex beat.
AREA OF RIGHT VENTRICLE:
The right ventricle of the heart can be palpated as a systolic impulse by placing the tips of the fingers in the 3rd, 4th and 5th intercostal spaces to the left of the sternum. Here again the location, duration and amplitude is assessed. An exaggerated systolic impulse (in other words parasternal heave) seen in right ventricular enlargement or if an enlarged left atrium pushes the right ventricle up.
AREA OF PULMONARY ARTERY (PULMONARY AREA)
The left 2nd intercostal space is the area overlying the pulmonary artery. Moreover, In cases of pulmonary hypertension, a loud pulmonary component of the second heart sound can felt in this area.
AREA OF AORTA
The right 2nd intercostal space is the area overlying the outflow tract of the aorta. Additionally, In cases of systemic hypertension or aortic aneurysm, the second heart sound becomes palpable in this area and has a loud aortic component.
THRILLS
Palpable vibrations of the chest wall occurring due to a cardiac murmur. A thrill is usually a sign of stenotic lesion in the heart, depending on its location.
PERCUSSION
Percussion Of Cardiovascular System Examination:
In CVS examination, Percussion enables to determine the boundaries of the heart except the lower border, since it cannot differentiate from hepatic dullness.
UPPER BOUNDARY
The upper border of the heart percuss in the 2nd and 3rd intercostal spaces in the parasternal line. A resonant note felt in the 2nd space while a dull note percussed in the 3rd space. In cases of pericardial effusion, left atrial enlargement, aortic aneurysm and pulmonary hypertension, a dull note percuss in the 2nd space also.
LEFT BOUNDARY
The left border of the heart percuss, beginning from the 4th and 5th intercostal spaces in the mid-axillary region and then moving medially. The left border locate along the apex beat. In cases of pericardial effusion, it locate outside the apex beat.
RIGHT BOUNDARY
For the right border of the heart, percussion first begun in the right mid-clavicular line until liver dullness is encountered. Thereafter, the percussion done one space higher from mid-clavicular line to the sternal border. The right border typically retrosternal, hence cannot felt. However, if parasternal dullness observed, then it suggests aortic aneurysm, pericardial effusion, right atrial enlargement or even dextrocardia.
AUSCULTATION
AUSCULTATION :
HEART SOUNDS IN CARDIOVASCULAR SYSTEM EXAMINATION:
Normally, there are 4 heart sounds. However, clinically, only two heart sounds can be auscultated in a majority of people. The 1st heart sound best heard in the mitral area and the 2nd sound is best auscultated in the aortic and pulmonary areas.
1ST HEART SOUND
This heart sound cause by the closure of the mitral and tricuspid valves. Splitting may heard during inspiration and is normal.
A loud S1(tapping apex) can hear in cases of mitral stenosis, because the stenotic valves open maximally at the end of diastole and then shut rapidly, tachycardia and high cardiac output states like anaemia and hyperthyroidism.
A soft S1 hear if the diastolic time prolong, i.e. in cases of mitral incompetence, because the mitral leaflets fail to close properly, calcified mitral valves and first degree heart block.
A variable S1 can hear in complete heart block and atrial fibrillation.
2ND HEART SOUND
This heart sound cause by the closure of aortic (A2) and pulmonary (P2) valves.
A soft A2 hear in aortic stenosis whereas a loud A2 is heard in hypertension and transposition.
A soft P2 hear in pulmonary stenosis whereas a loud P2 can be heard in pulmonary hypertension.
Splitting a normal phenomenon occurring during respiration. It best hear in the pulmonary area.
Wide splitting may indicate pulmonary stenosis, mitral regurgitation, right bundle branch block or ventricular septal defect. Wide fixed splitting seen in cases of atrial septal defect.
Reverse splitting seen in cases of aortic stenosis, patent ductus arteriosus and left bundle branch block.
Single 2nd heart sound heard in severe aortic or pulmonary stenosis, Eisenmenger’s syndrome and Fallot’s tetralogy.
3RD HEART SOUND
This is a low-pitched heart sound, which may hear with the bell of the stethoscope. It occurs immediately after the second sound.
A loud S3 occurs when rapid ventricular filling occurs in a dilated left ventricle, as in mitral regurgitation and ventricular septal defect or when the left ventricular function is poor, as seen in dilated cardiomyopathy and post- Myocardial infarction. It more high-pitched and occurs early in restrictive cardiomyopathy and constrictive pericarditis (pericardial knock).
4TH HEART SOUND
This heart sound occurs just before the first heart sound. It dull and low-pitch and is best heard with the bell of the stethoscope. An audible 4th heart sound observe in cases of aortic stenosis and hypertensive heart disease.
When the 3rd or 4th sound occur with tachycardia (heart rate > 100/min), it may give the effect of galloping hooves. In such cases (e.g. pulmonary embolism), discrimination between the 3rd and 4th sounds is not possible and they may summate and seem like a single sound. This call a summation gallop.
MURMURS IN CARDIOVASCULAR SYSTEM EXAMINATION:
Murmurs abnormal heart sounds caused by turbulence of blood flow within the heart and great blood vessels, usually caused by valve disease, or sometimes by increased flow through a normal valve.
They characterized on the basis of 4 parameters- Location, Loudness, Timing and Quality.
LOCATION denotes the site of origin of the murmur.
LOCATION AND TYPE OF MURMUR:
- Near cardiac apex -Near cardiac apex
- Left sternal edge -Tricuspid
- Right 2nd intercostal space -Aortic
- Left 2nd intercostal space -Pulmonary
LOUDNESS signifies the degree of turbulence, which determie by the volume and velocity of blood flow, but not the severity of the cardiac pathology. Murmurs have graded based on their loudness as follows:
GRADE AND NATURE OF MURMUR:
- I (1/6): Very soft, heard with effort and after listening for a while
- II (2/6): Soft, but audibly detectable immediately
- III (3/6): Clearly audible and moderately loud, but no palpable thrill
- IV (4/6): Clearly audible, with palpable thrill
- V (5/6): Audible, with thrill, and can hear with stethoscope only partially touching chest, or away from involved site
- VI (6/6): Audible without placing stethoscope on chest
QUALITY
signifies the frequency of the murmur and is described as low-, medium-, or high-pitch.
TIMING denotes the phase of systole (mid-systolic, pansystolic or late systolic) or diastole (early diastolic, mid-diastolic or pre-systolic) during which the murmur is audible. Continuous murmurs are audible throughout the cardiac cycle.
Mid Systolic (Ejection) Phase:
- NATURE:
1.AORTIC: Turbulence in the left ventricular outflow tract during ejection. Follows opening of aortic valve, loudening in mid-systole.
- HEARD IN: Aortic area with radiation to neck
- CONDITIONS SEEN IN: Aortic stenosis, PDA, Coarctation of aorta hypertrophic cardiomyopathy
2.PULMONARY: Turbulence in the right ventricular outflow tract during ejection. Follows opening of pulmonary valve, loudening in mid-systole.
- HEARD IN: Pulmonary area
- CONDITIONS SEEN IN: Pulmonary stenosis, Fallot’s tetralogy, pulmonary hypertension, ASD, High output states.
Pansystolic Phase:
- NATURE: Murmur is audible throughout systole. Caused by incompetent atrioventricular valves or VSDs
- HEARD IN:
1.Firstly, Cardiac apex radiating to left axilla :CONDITIONS SEEN IN: Mitral incompetence
2. Secondly, Lower left edge of sternum: CONDITIONS SEEN IN: Tricuspid incompetence, VSD
Late Systolic Phase:
- HEARD IN:
1.Firstly, Cardiac apex (Mitral valve prolapse) :CONDITIONS SEEN IN: Tricuspid incompetence, VSD
2. Secondly, Lower left sternal border (Tricuspid valve prolapse): CONDITIONS SEEN IN: Mitral valve prolapse, tricuspid valve prolapse, papillary muscle dysfunction
Early Diastolic Phase:
- NATURE: Begin after 2ndheart sound and decline in sound; they are high-pitched. Occur due to incompetent aortic and pulmonary valves.
- HEARD IN:
1.Firstly, AORTIC: Aortic area radiating to left sternal edge: CONDITIONS SEEN IN: Aortic incompetence
2.Secondly, PULMONARY: Pulmonary area :CONDITIONS SEEN IN: Pulmonary incompetence
Mid Diastolic Phase:
- NATURE: Begin late after 2nd heart sound and occur due to turbulent flow through the valves.
- HEARD IN:
1.Firstly, Cardiac apex :CONDITIONS SEEN IN: Mitral stenosis, Austin Flint murmur of Aortic incompetence, VSD, Mitral incompetence
2.Secondly, Lower left edge of sternum :CONDITIONS SEEN IN: Tricuspid stenosis, ASD, Tricuspid imcompetence
Pre-systolic Phase:
- NATURE:
1.Firstly, Cardiac apex :CONDITIONS SEEN IN: Mitral stenosis
2.Secondly, Lower left edge of sternum: CONDITIONS SEEN IN: Tricuspid stenosis
Continuous Phase:
CONDITIONS SEEN IN: PDA, Ruptured sinus of Valsalva
VENOUS HUM
This a soft, continuous and low-pitch murmur occurring due to hyperkinetic jugular venous flow, audible at the base of the heart. It emphasize in early diastole and commonly hear in infants.
MAMMARY SOUFFLE
This a soft, continuous murmur, emphasize during systole, occurring in the third month of pregnancy. It is audible over the mammary area and second intercostal spaces.
SYSTOLIC CLICKS
They high-pitch sounds coming in early systole due to excessive ejection of blood into the vessels from the ventricles.
Clicks are of 2 types:
- AORTIC: It transmit to the cardiac apex and is heard in cases of Aortic stenosis, aortic aneurysm, aortic incompetence and aortic coarctation.
- PULMONARY: It is audible best during the phase of inspiration and hear in cases of pulmonary stenosis, pulmonary hypertension and pulmonary arterial dilatation.
OPENING SNAP
It a loud, sharp, high-pitch sound occurring due to sudden tensing of the mitral/tricuspid valves heard between the 2nd and 3rd heart sounds, during early diastole. It hear in cases of mitral/tricuspid stenosis and indicates a non-calcified valve.
PERICARDIAL FRICTION RUB
It a scratching type of high-pitched sound heard during systole and diastole over the left precordium. This occurs in pericardial effusion due to the movement of the exudate in the pericardial cavity as a result of the beating of the heart. It best hear in maintained expiration, in the sitting position with the patient leaning slightly forward.
Frequently Asked Questions (FAQ)
What is a cardiovascular system examination?
It’s a comprehensive physical assessment of the heart and blood vessels to evaluate their function and detect potential abnormalities. This involves inspecting, palpating, and auscultating various areas of the body.
Why is a cardiovascular system examination important?
It helps identify signs and symptoms of heart disease, such as abnormal heart rhythms, murmurs, or fluid buildup. Early detection allows for timely intervention and management, potentially preventing serious complications.
What are the key components of a cardiovascular system examination?
The exam typically includes:
Vital signs: Measuring heart rate, blood pressure, and respiratory rate.
Inspection: Observing the patient for any visible signs like chest deformities, abnormal pulsations, or skin discoloration.
Palpation: Feeling for pulses in different areas (e.g., carotid, radial, femoral) and checking for any abnormal vibrations or thrills.
Auscultation: Listening to heart sounds using a stethoscope to assess rate, rhythm, and identify any murmurs or extra sounds.
Peripheral vascular assessment: Examining the extremities for signs of decreased blood flow, such as swelling, coldness, or abnormal capillary refill.
What are some common abnormalities detected during a cardiovascular examination?
Some common findings include:
Abnormal heart rhythms: Irregular heartbeats, such as atrial fibrillation or tachycardia.
Heart murmurs: Abnormal sounds caused by turbulent blood flow through the heart valves.
Fluid buildup: Signs of heart failure, like swelling in the legs or crackles in the lungs.
Peripheral artery disease: Reduced blood flow to the limbs, leading to pain, numbness, or skin changes.
How often should I have a cardiovascular system examination?
The frequency depends on your age, risk factors, and overall health. Generally, adults should have their cardiovascular system checked during routine physical exams, at least every few years. However, more frequent assessments may be necessary for individuals with existing heart conditions or multiple risk factors.
How can I prepare for a cardiovascular system examination?
No specific preparation is usually needed. However, wearing comfortable clothing that allows easy access to your chest and arms can be helpful. It’s also a good idea to inform your doctor about any medications you’re taking and any symptoms you’ve been experiencing.
What are some lifestyle factors that can improve cardiovascular health?
Maintaining a healthy lifestyle is crucial for optimal cardiovascular health. This includes:
Regular exercise: Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Healthy diet: Choose a balanced diet rich in fruits, vegetables, whole grains, and lean protein.
Maintaining a healthy weight: Losing even a small amount of weight can significantly improve heart health.
Quitting smoking: Smoking is a major risk factor for heart disease.
Limiting alcohol consumption: Excessive alcohol intake can damage the heart.
What are some additional resources for learning more about cardiovascular health?
Reputable organizations like the American Heart Association (AHA) and the Centers for Disease Control and Prevention (CDC) offer valuable information and resources on heart health. You can also consult your healthcare provider for personalized advice and guidance.
