Gout
Definition
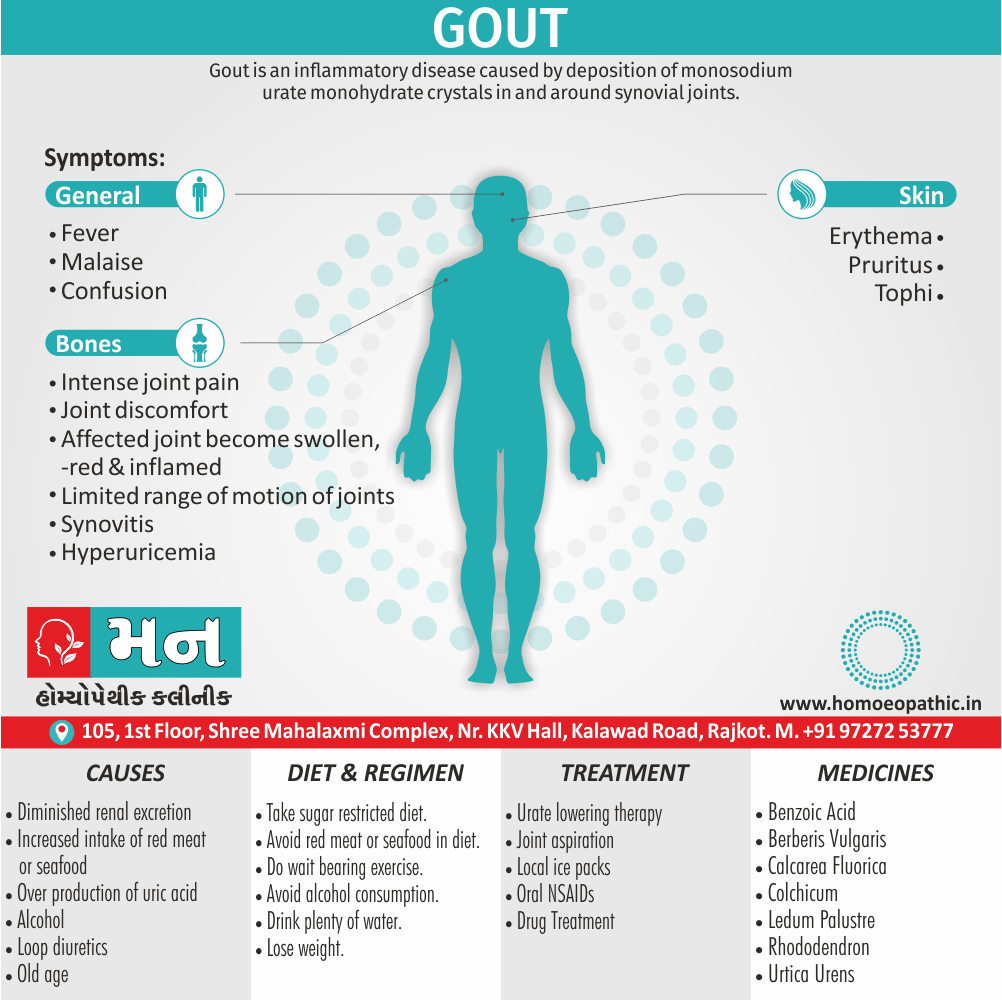
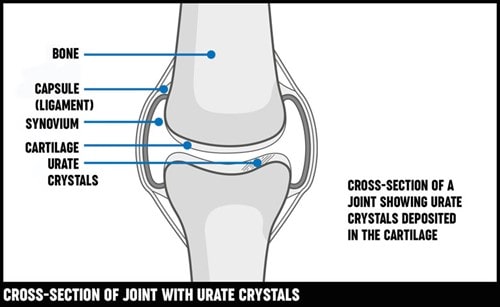
Gout is an inflammatory disease caused by deposition of monosodium urate monohydrate crystals in and around synovial joints. [1]
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigationss
Treatment
Homeopathic Treatment
Prevention
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
It is the most common inflammatory arthritis in men also in older women.
Moreover, The risk of developing gout increases with age and with serum uric acid (SUA) levels, which are normally distributed in the general population.
Levels are higher in men, increase with age and are associated with body weight.
Hyperuricemia is defined as an SUA level greater than 2 standard deviations above the mean for the population.
Additionally, Gout has become more common over recent years in parallel with increased longevity and the higher prevalence of metabolic syndrome, of which hyperuricemia is an integral component.
Although hyperuricemia is an independent risk factor for hypertension, vascular disease, renal disease and cardiovascular events, only a minority of hyperuricemic people develop gout.
Besides this, There is currently no evidence to support the use of urate lowering therapy in patients with asymptomatic hyperuricemia. [1]
Gout is a form of arthritis which can be intensely painful; and it’s caused by having sodium urate crystals in your joints.
Lastly, It’s characterized by sudden, severe attacks of pain, swelling, redness and tenderness in the joints, often the joint at the base of the big toe.
Onset of pain
An attack of gout can occur suddenly, often waking you up in the middle of the night with the sensation that your big toe is on fire.
The affected joint is hot, swollen also so tender that even the weight of the sheet on it may seem intolerable. [2]
In detail, Gout attacks can come on quickly and keep returning over time, slowly harming tissues in the region of the inflammation.
It has also been related to an increased incidence of cardiovascular also metabolic disease and can be extremely painful.
Women become more susceptible to it after the menopause. [3]
Epidemiology
Epidemiology of Gout
Indian Epidemiology of Gout
Several studies have shed light on the epidemiology of gout in India:
Hyperuricemia prevalence in Indian subjects with underlying comorbidities of hypertension and/or type 2 diabetes (2020):
This study found an overall hyperuricemia (HU) prevalence of 24.66% among individuals attending HU camps. The prevalence was higher in those with type 2 diabetes (T2DM) and hypertension (HTN) (7.36%) compared to T2DM (5.63%) or HTN (4.25%) alone. Prevalence increased with age and was higher in males. [6]
Global, regional and national burdens of gout in the young population from 1990 to 2019: a population-based study (2023):
While this study provides a global perspective, it includes data on India, indicating a rise in years lived with disability (YLD) due to gout between 1990 and 2019. [7]
Epidemiology, Comorbidities and Clinical Features of Gout in Southern Part of India (Year not explicitly mentioned):
This study found that 80% of gout patients had comorbidities, with hyperlipidemia (40%), obesity (34%), and hypertension (30%) being the most common. [8]
Epidemiology and risk factors associated with gout control among adult Asians: a real-world retrospective cohort study (2023):
While focused on Asia, this study includes data from Singapore, showing 28.2% of gout patients had poorly controlled disease, with male gender, Malay ethnicity, and congestive heart failure being associated risk factors. [9]
Key Points:
Gout prevalence appears to be increasing in India.
Comorbidities like hypertension, diabetes, obesity, and hyperlipidemia are common among gout patients.
There are regional variations in prevalence and clinical presentation.
More research is needed to fully understand the burden of gout in India and to develop effective prevention and management strategies.
Please note that this is a summary of the available information. The epidemiology of gout is a complex and evolving field, and more research is needed to fully understand the situation in India.
Causes
Causes
Diminished renal excretion:
Increased renal tubular reabsorption
Renal failure
Lead toxicity
Lactic acidosis
Alcohol
Drugs: Thiazide, loop diuretics, low-dose aspirin, ciclosporin, pyrazinamide
Increased intake:
Red meat
Seafood
Offal
Shellfish
Organ meat
Sweet juices
Salt
Over production of uric acid:
Myeloproliferative and lymphoproliferative disease
High fructose intake
Glycogen storage disease
Inherited disorders
Lesch–Nyhan syndrome (HPRT mutations) [1]
Types
Types
While gout itself is a single disease, it can be categorized into different stages or types based on its progression and clinical presentation:
1. Asymptomatic Hyperuricemia:
Elevated uric acid levels in the blood without any symptoms of gout. [10]
2. Acute Gouty Arthritis:
Sudden onset of severe joint pain, swelling, redness, and warmth, typically affecting a single joint (often the big toe). [11]
3. Intercritical Gout:
The period between acute gout attacks, where there are no symptoms. [12]
4. Chronic Tophaceous Gout:
Advanced stage of gout characterized by the formation of tophi (deposits of uric acid crystals) in joints, tendons, and other tissues. [13]
Risk Factors
Risk Factor
You’re more likely to develop gout if you have high levels of uric acid in your body.
Factors that increase the uric acid level in your body include:
Diet:
Eating a diet rich in meat and seafood and drinking beverages sweetened with fruit sugar (fructose) increase levels of uric acid, which increase your risk of gout.
Alcohol consumption, especially of beer, also increases the risk of gout.
Obesity:
If you’re higher weight body, your body produces more uric acid and your kidneys have a more difficult time eliminating uric acid.
Medical conditions:
Certain diseases and conditions increase your risk of gout.
These include untreated high blood pressure and chronic conditions such as diabetes, metabolic syndrome, and heart and kidney diseases.
Certain medications:
The use of thiazide diuretics commonly used to treat hypertension and low-dose aspirin also can increase uric acid levels.
So can the use of anti-rejection drugs prescribed for people who have undergone an organ transplant.
Family history of gout:
If other members of your family have had gout, you’re more likely to develop the disease.
Age and sex:
Gout occurs more often in men, primarily because women tend to have lower uric acid levels.
After menopause, however, women’s uric acid levels approach those of men.
Men are also more likely to develop gout earlier usually between the ages of 30 and 50 whereas women generally develop signs and symptoms after menopause.
Recent surgery or trauma:
Experiencing recent surgery or trauma has been associated with an increased risk of developing a gout attack. [2]
Pathogenesis
Pathogenesis of Gout
Hyperuricemia:
The fundamental cause of gout is hyperuricemia, an elevated level of uric acid in the blood.
Uric acid is a waste product formed from the breakdown of purines, which are found in certain foods and also produced by the body.
Hyperuricemia can result from either increased production of uric acid, decreased excretion of uric acid by the kidneys, or a combination of both.
Urate Crystal Formation:
When uric acid levels exceed the saturation point in the blood, it can form monosodium urate (MSU) crystals.
These crystals can deposit in joints, tissues, and organs.
Acute Inflammation:
MSU crystals trigger an inflammatory response when they are released into the joint space.
This inflammatory response is characterized by the activation of immune cells, the release of inflammatory mediators (such as cytokines and chemokines), and the recruitment of white blood cells (neutrophils).
The resulting inflammation causes the characteristic pain, swelling, redness, and warmth of an acute gout attack.
Chronic Tophaceous Gout:
If hyperuricemia persists, MSU crystals can continue to accumulate and form tophi.
Tophi are large, visible deposits of urate crystals that can cause joint damage, deformity, and disability. [10]
Pathophysiology
Pathophysiology of Gout
Hyperuricemia:
Mechanism: Elevated levels of uric acid in the blood (serum urate > 6.8 mg/dL). This can occur due to:
Increased production: Overactive purine metabolism or increased intake of purine-rich foods (organ meats, seafood, alcohol).
Decreased excretion: Impaired kidney function or certain medications.
Consequence: Uric acid becomes supersaturated, leading to the formation of monosodium urate (MSU) crystals.
MSU Crystal Deposition:
Mechanism: MSU crystals precipitate in joints, tendons, and surrounding tissues.
Consequence: Crystals trigger a local inflammatory response.
Acute Inflammation:
Mechanism: MSU crystals activate the innate immune system, leading to:
Neutrophil recruitment and activation
Release of pro-inflammatory cytokines (IL-1β, TNF-α)
Activation of the NLRP3 inflammasome
Consequence: Intense joint inflammation, pain, swelling, redness, and warmth.
Chronic Tophaceous Gout:
Mechanism: Repeated acute attacks and persistent hyperuricemia lead to:
Accumulation of MSU crystals in tophi (urate deposits)
Chronic inflammation and joint damage
Potential for extra-articular manifestations (kidney stones, renal impairment) [14]
Clinical Features
Clinical Features of Gout
Acute Gouty Arthritis:
Onset: Sudden, often nocturnal
Pain: Severe, excruciating, often described as "throbbing" or "crushing"
Joints Affected: Primarily the first metatarsophalangeal joint (big toe), but can affect other joints (ankles, knees, wrists, fingers)
Signs of Inflammation: Swelling, redness, warmth, tenderness
Systemic Symptoms: Fever, chills, malaise (in some cases)
Intercritical Gout:
Asymptomatic period: Between acute attacks, patients are usually symptom-free.
Variable Duration: Can last months or years.
Chronic Tophaceous Gout:
Tophi: Visible, firm nodules under the skin, composed of uric acid crystals
Location: Typically occur in joints, tendons, bursae, and cartilage
Other Manifestations:
Chronic joint pain and stiffness
Joint deformity and limited range of motion
Uric acid kidney stones
Chronic kidney disease [11]
Sign & Symptoms
Sign & Symptoms
The signs and symptoms of gout almost always occur suddenly, and often at night. They include:
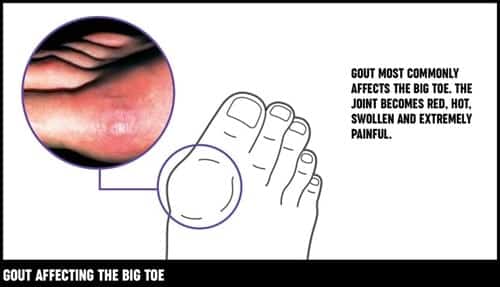
Gout Affecting The Big Toe
Intense joint pain:
Gout usually affects the large joint of your big toe, but it can occur in any joint.
Other commonly affected joints include the ankles, knees, elbows, wrists also fingers.
The pain is likely to be most severe within the first four to 12 hours after it begins.
Lingering discomfort:
After the most severe pain subsides, some joint discomfort may last from a few days to a few weeks.
Later attacks are likely to last longer and affect more joints.
Inflammation and redness:
The affected joint or joints become swollen, tender, warm also red.
Limited range of motion:
As gout progresses, you may not be able to move your joints normally. [2]
The classical presentation is with an acute monoarthritis, which in over 50% of cases affects the first MTP joint.
Other common sites are;
Ankle
Midfoot
Knee
Small joints of hands
Wrist
Elbow
The axial skeleton and large proximal joints are rarely involved.
Typical features include:
Rapid onset
Reaching maximum severity in 2–6 hours,
Often waking the patient in the early morning
Severe pain
Often described as the ‘worst pain ever’
Extreme tenderness, such that the patient is unable to wear a sock or to let bedding rest on the joint
Marked swelling with overlying red, shiny skin
Self limiting over 5–14 days, with complete resolution
During the attack, the joint shows signs of;
Marked synovitis
Swelling
Erythema
There may be accompanying;
Malaise and even confusion
Especially if a large joint such as the knee is involved.
As the attack subsides;
Pruritus and desquamation of overlying skin are common.
The main differential diagnosis is septic arthritis, infective cellulitis or reactive arthritis.
Acute attacks may also manifest as bursitis, tenosynovitis or cellulitis, which have the same clinical characteristics.
Many patients describe milder episodes lasting just a few days.
Some have attacks in more than one joint.
Others have further attacks in other joints a few days later (cluster attacks), the first possibly acting as a trigger.
Simultaneous polyarticular attacks are unusual.
In others, several years may elapse before the next attack.
In many, however, a second attack occurs within 1 year and may progress to chronic gout, with chronic pain and joint damage, and occasionally severe deformity and functional impairment.
Patients with uncontrolled hyperuricemia who suffer multiple attacks of acute gout may also progress to chronic gout.
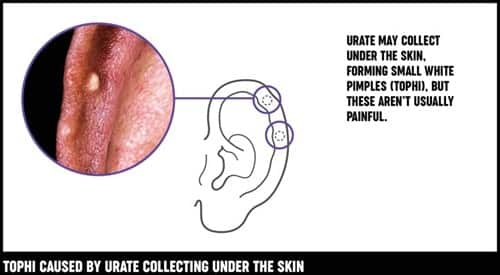
Tophi On Ear
Urate Crystals
Crystals may be deposited in the joints and soft tissues to produce irregular firm nodules called tophi.
These have a predilection for the extensor surfaces of fingers, hands, forearm, elbows, Achilles tendons and sometimes the helix of the ear.
Characteristics of Tophi
Tophi have a white colour, differentiating them from rheumatoid nodules.
Tophi can ulcerate, discharging white gritty material, become infected or induce a local inflammatory response, with erythema and pus in the absence of secondary infection.
They are usually a feature of longstanding gout but can sometimes develop within 12 months in patients with chronic renal failure.
Occasionally, tophi may develop in the absence of previous acute attacks, especially in patients on thiazide therapy who have coexisting OA.
In addition to causing musculoskeletal disease, chronic hyperuricemia may be complicated by renal stone formation and, if severe, renal impairment due to the development of interstitial nephritis as the result of urate deposition in the kidney.
This is particularly common in patients with chronic tophaceous gout who are on diuretic therapy. [1]
Clinical Examination
Clinical Examination of Gout
1. Acute Gouty Arthritis:
Inspection:
Affected joint: Red, swollen, warm, and shiny.
Most commonly involved joint: First metatarsophalangeal joint (big toe).
Other possible joints: Ankles, knees, wrists, fingers.
Palpation:
Exquisite tenderness: Even light touch can provoke severe pain.
Joint effusion: Swelling due to fluid accumulation within the joint.
Warmth: Increased temperature compared to the surrounding skin.
2. Intercritical Gout:
Usually asymptomatic: No specific findings on examination.
May have:
Residual joint swelling or tenderness
Tophi (if present)
3. Chronic Tophaceous Gout:
Tophi:
Palpable, firm nodules under the skin.
Common locations: Ears, fingers, elbows, Achilles tendon.
May be ulcerated and drain chalky white material.
Joint Deformity:
Chronic inflammation can lead to joint damage and deformities.
Limited range of motion and decreased function. [12]
Diagnosis
Diagnosis
Tests to help diagnose gout may include:
Joint fluid test:
Your doctor may use a needle to draw fluid from your affected joint.
Urate crystals may be visible when the fluid is examined under a microscope.
Blood test:
Your doctor may recommend a blood test to measure the levels of uric acid and creatinine in your blood.
Blood test results can be misleading, though.
Some people have high uric acid levels, but never experience gout.
And some people have signs and symptoms of gout, but don’t have unusual levels of uric acid in their blood.
X-ray imaging:
Joint X-rays can be helpful to rule out other causes of joint inflammation.
Ultrasound:
Musculoskeletal ultrasound can detect urate crystals in a joint or in a tophus.
Dual energy CT scan:
This type of imaging can detect the presence of urate crystals in a joint, even when it is not acutely inflamed.
This test is not used routinely in clinical practice due to the expense and is not widely available. [2]
Differential Diagnosis
Differential Diagnosis of Gout
Conditions that can mimic gout clinically can be broadly categorized as:
Crystalline Arthropathies:
Calcium Pyrophosphate Deposition Disease (CPPD) (Pseudogout): Similar presentation to gout, but caused by calcium pyrophosphate crystals.
Basic Calcium Phosphate (BCP) Crystal Deposition Disease: Can cause acute or chronic arthritis, often affecting multiple joints.
Hydroxyapatite Deposition Disease (HADD): Usually causes periarticular inflammation (tendinitis, bursitis).
Infectious Arthritis:
Septic Arthritis: Bacterial infection of the joint, causing severe pain, swelling, and fever. Crucial to rule out due to potential for joint destruction.
Reactive Arthritis: Triggered by infection elsewhere in the body, often associated with genitourinary or gastrointestinal symptoms.
Other Inflammatory Arthritides:
Rheumatoid Arthritis: Chronic autoimmune disease, typically affecting multiple joints symmetrically.
Psoriatic Arthritis: Associated with psoriasis, can affect any joint and may have a "sausage digit" appearance.
Non-Inflammatory Conditions:
Osteoarthritis: Degenerative joint disease, usually affecting weight-bearing joints with gradual onset.
Trauma: Joint injury can mimic acute gout attack.
Cellulitis: Bacterial skin infection, can cause localized redness, swelling, and pain. [11]
Complications
Complications of Gout
Recurrent Gout Attacks:
Description: Untreated or undertreated gout can lead to more frequent and severe attacks, often affecting multiple joints.
Impact: Increased pain, disability, and reduced quality of life.
Tophi Formation and Joint Damage:
Description: Chronic hyperuricemia can lead to the formation of tophi (urate crystal deposits) in joints, tendons, and soft tissues.
Impact: Joint damage, deformity, limited range of motion, and disability.
Kidney Stones:
Description: Uric acid can crystallize in the urinary tract, forming kidney stones.
Impact: Severe pain, hematuria (blood in the urine), and potential for kidney damage.
Chronic Kidney Disease (CKD):
Description: Long-term hyperuricemia and urate crystal deposition can damage the kidneys, leading to chronic kidney disease.
Impact: Reduced kidney function, potentially progressing to kidney failure requiring dialysis.
Cardiovascular Disease (CVD):
Description: Gout is associated with an increased risk of cardiovascular events (heart attack, stroke) due to shared risk factors like hypertension, obesity, and dyslipidemia.
Impact: Increased morbidity and mortality. [15]
Investigationss
Investigations of Gout
Synovial Fluid Analysis:
Gold Standard: Definitive diagnosis of gout requires identifying monosodium urate (MSU) crystals in the synovial fluid.
Procedure: Arthrocentesis (joint aspiration) is performed to obtain synovial fluid.
Microscopy: Polarized light microscopy reveals needle-shaped MSU crystals with negative birefringence.
Serum Uric Acid Level:
Utility: Elevated serum uric acid levels (>6.8 mg/dL) are suggestive of gout but not diagnostic.
Limitations: Uric acid levels may be normal during an acute attack. Some individuals with hyperuricemia never develop gout.
Monitoring: Useful for monitoring treatment response and assessing the risk of future attacks.
Imaging Studies:
X-rays:
Early stages: May be normal or show soft tissue swelling.
Chronic gout: Erosions, joint space narrowing, and tophi may be seen.
Ultrasound: Detects MSU crystals in joints and soft tissues.More sensitive than X-rays in early stages.
Dual-Energy CT (DECT): Most sensitive and specific imaging modality for detecting MSU crystals. [14]
Treatment
Treatment
Oral NSAIDs:
They are effective for pain relief in the acute attack and are the standard treatment, but have to be prescribed with caution in old age.
Patients with recurrent episodes can keep a supply of an NSAID also take it as soon as the first symptoms occur, continuing until the attack resolves.
Oral colchicine:
It works by inhibiting microtubule assembly in neutrophils, is also very effective.
It is usually given in doses of 0.5 mg twice or 3 times daily.
The most common adverse effects are nausea, vomiting also diarrhoea.
Joint aspiration:
It can give pain relief, and may be combined with an intra articular steroid injection if the diagnosis is clear also infection can be excluded.
Urate Lowering Therapy:
Patients who have more than one acute attack within 12 months and those with complications should be offered urate lowering therapy.
Acute flares of gout often occur following initiation of urate lowering therapy.
The patient should be warned about this and told to continue therapy, even if an attack occurs.
The risk of flares can be reduced by administration of oral colchicine (0.5 mg twice daily) or NSAID therapy for the first few months.
In the longer term, annual monitoring of uric acid levels is recommended.
In most patients, urate lowering therapy needs to be continued indefinitely.
Allopurinol:
This is the drug of first choice.
It is a xanthine oxidase inhibitor, which reduces the conversion of hypoxanthine and xanthine to uric acid.
The recommended starting dose is 100 mg daily, or 50 mg in older patients and in renal impairment.
The dose of allopurinol should be increased by 100 mg every 4 weeks (50 mg in the older people and those with renal impairment) until the target uric acid level is achieved, side effects occur or the maximum recommended dose is reached (900 mg/day).
Febuxostat:
It is a xanthine oxidase inhibitor that is useful in patients who fail to respond adequately to allopurinol, and those in whom it is contraindicated or has been poorly tolerated.
It undergoes hepatic metabolism and so no dose adjustment is required for renal impairment.
This is more effective than allopurinol at reducing uric acid levels and, as a result, commonly provokes attacks at the recommended starting dose (80 mg daily).
In view of this, treatment with colchicine or NSAID should be considered for the initial 6 months.
Uricosuric drugs:
Such as probenecid or sulfinpyrazone, can be effective but require several doses each day and maintenance of a high urine flow to avoid uric acid crystallisation in renal tubules.
Salicylates antagonise the uricosuric action of these drugs also should be avoided.
Uricosurics are contraindicated in overproducers, those with renal impairment and in urolithiasis (they increase stone formation).
The uricosuric benzbromarone can be very effective and safe in mild to moderate renal impairment, but can cause hepatotoxicity.
A short course of oral or intramuscular corticosteroids can also be highly effective in treating acute attacks.
Local ice packs can also be used for symptomatic relief.
The long term therapeutic aim is to prevent attacks occurring by bringing uric acid levels below the level at which monosodium urate monohydrate crystals form. [1]
Homeopathic Treatment
Homeopathic Treatment of Gout
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Benzoic acid:
- This is use for gout, especially of the knee or big toe.
- Tearing and stitching pain in the affected joint, for acute rheumatism and gout with stiffness, swelling and lameness.
- Also, symptoms of gout associated with highly colored and offensive urine.
- Symptoms are worse in open air and from uncovering the affected parts.
Berberis vulgaris:
- This remedy is indicate when there are sudden twinges of pain stitching pains in gouty joints, which are worse from motion.
- Furthermore, the pains often radiate out from the affect part or move to a different area all together.
- All in all, the person has a tendency towards kidney stones and may ache all over.
Urtica urens:
- This remedy helps specifically in the elimination of uric acid from the body.
- The patient has a tendency to gout also uric acid formations.
- Additionally; the joint symptoms are associate with hive-like eruptions.
- There is pain in the shoulders (especially deltoid region), wrists also ankles.
- The patient is worse especially from exposure to cool moist air, snow-air, water and touch.
- Lastly, Select the remedy that most closely matches the symptoms.
Colchicum:
- Gout in the big toe or heel so painful that the person cannot bear to have it touched or moved.
- Joints are red, hot and swollen.
- The pain is often worse in the evening and at night.
- Pains are worse in cold, damp weather and flare-ups may occur with weather changes or in the spring.
- The person often has a feeling of internal coldness
Ledum:
- This remedy is indicate when the gouty pains shoot through the foot, limb and joints especially the small joints.
- The foot and ankle are extremely swollen.
- Cold or ice cold applications relieve the pain and swelling.
Lycopodium:
- This remedy is for chronic gout, with chalky deposits in the joints.
- There is a pain in the heels on treading, as from a pebble.
- One foot feels hot and the other cold.
- The urine is slow to produce and has heavy, red sediment.
- There may a backache, which relieve by passing urine.
- The right side of the body is particularly affect and all the complaints seem to be worse, especially between 4pm and 8pm.
Rhododendron:
- This remedy can useful for gouty swelling of the big toe joint that flares up before a storm.
- Other joints may ache and swell, especially on the right side of the body.
- Pain usually is worse toward early morning and after staying still too long.
- The person may feel better from warmth and after eating.
Calcarea fluorica:
- When this remedy is indicate, the finger joints may become enlarge because of gout, and the knees and toes may involve.
- Stabbing pain is experience, and the joints may make a cracking sound on movement.
- Discomfort is worse during weather changes, and warmth may bring relief.
Belladonna:
- Symptoms that suggest this remedy are sudden onset.
- Joints are swelling, red, throbbing also extremely sensitive.
- It’s worse especially from touch and jarring.
- The person may feel restless, flushed also hot.
Arnica:
- This remedy is use when the pain is sore and bruise, such as it hurts to walk.
- The person may afraid to touched or approached because of pain. [5]
Prevention
Prevention
During symptom-free periods, these dietary guidelines may help protect against future gout attacks:
Drink plenty of fluids:
- Stay well-hydrated, including plenty of water.
- Limit how many sweetened beverages you drink, especially those sweetened with high-fructose corn syrup.
Limit or avoid alcohol:
- In general, Talk with your doctor about whether any amount or type of alcohol is safe for you.
- Furthermore, recent evidence suggests that beer may be particularly likely to increase the risk of gout symptoms, especially in men.
Get your protein from low-fat dairy products:
- Low-fat dairy products may actually have a protective effect against gout, hence these are your best-bet protein sources.
Limit your intake of meat, fish also poultry:
- Basically, a small amount may be tolerable, but pay close attention to what types and how much seem to cause problems for you.
Maintain a desirable body weight:
- Choose portions that allow you to maintain a healthy weight.
- Losing weight may decrease uric acid levels in your body.
- But avoid fasting or rapid weight loss, since doing so may temporarily raise uric acid levels. [2]
Diet & Regimen
Diet & Regimen for Gout:
Gout Diet & Regimen
Diet
Limit Purine-Rich Foods:
- High-Purine Foods: Organ meats (liver, kidney), red meat, certain seafood (anchovies, sardines, mussels, scallops), yeast extracts.
- Moderate-Purine Foods: Other meats, poultry, fish, beans, lentils, spinach, asparagus.
Increase Low-Purine Foods:
- Fruits and Vegetables: Cherries, berries, citrus fruits, leafy greens, other non-starchy vegetables.
- Whole Grains: Brown rice, quinoa, oats, whole wheat bread.
- Low-Fat Dairy Products: Milk, yogurt, cheese.
Hydration:
- Drink Plenty of Fluids: Water, herbal tea, unsweetened coffee.
- Limit Sugar-Sweetened Beverages: Soda, juice, sports drinks.
Alcohol:
- Limit or Avoid Alcohol: Especially beer, which is high in purines.
- Moderate Wine Consumption: May be acceptable, but discuss with your doctor.
Regimen for Gout:
Weight Management:
- Maintain a Healthy Weight: Losing weight if over-weight can help lower uric acid levels.
- Regular Exercise: Aim for at least 150 minutes of moderate-intensity exercise per week.
Medication:
Regular Monitoring:
- Check Uric Acid Levels: Monitor your uric acid levels regularly as advised by your doctor. [16]
Do’s and Don'ts
Do’s & Don’ts
Gout do’s and don’ts
Do’s:
Maintain a Healthy Weight: Losing weight if you’re over-weight can significantly lower uric acid levels and reduce the risk of gout attacks.
Stay Hydrated: Drink plenty of water (8-16 cups per day) to help flush out uric acid from your body.
Follow a Low-Purine Diet:
Limit or avoid high-purine foods (organ meats, red meats, certain seafood, sugary drinks, high-fructose corn syrup).
Increase intake of low-purine foods (fruits, vegetables, whole grains, low-fat dairy).
Eat Cherries: Cherries contain compounds that may help lower uric acid levels and reduce inflammation.
Consider Vitamin C: Some studies suggest that vitamin C supplementation may help lower uric acid levels. Talk to your doctor about the appropriate dosage for you.
Drink Coffee (in Moderation): Moderate coffee consumption has been associated with a lower risk of gout.
Exercise Regularly: Engage in moderate-intensity exercise for at least 150 minutes per week.
Manage Other Medical Conditions:
Control conditions like high blood pressure, diabetes, and high cholesterol, as they can increase the risk of gout.
Take Medications as Prescribed: If your doctor has prescribed medications for gout, take them as directed.
Attend Regular Checkups: See your doctor for regular checkups to monitor your uric acid levels and adjust your treatment plan as needed.
Don’ts:
Don’t Overindulge in High-Purine Foods: Limit your intake of red meat, organ meats, certain seafood, and other high-purine foods.
Don’t Drink Excessive Alcohol: Alcohol, especially beer, can increase uric acid levels and trigger gout attacks. Limit your intake or avoid alcohol altogether.
Don’t Consume Sugary Drinks: Sugary drinks, like soda and sweetened fruit juices, can raise uric acid levels. Choose water or unsweetened beverages instead.
Don’t Skip Medications: Don’t stop taking your gout medications without consulting your doctor, even if you feel better.
Don’t Ignore Symptoms: If you experience a gout attack, seek medical attention promptly. Early treatment can help reduce pain and prevent complications.
Terminology
Terminology
Gout:
A type of inflammatory arthritis caused by the deposition of monosodium urate (MSU) crystals in joints and other tissues.
Hyperuricemia:
Elevated levels of uric acid in the blood, a key risk factor for developing gout.
Uric Acid:
A waste product produced by the body from the breakdown of purines, which are found in certain foods and also produced naturally by the body.
Purines:
Chemical compounds found in some foods and drinks that can be broken down into uric acid.
Monosodium Urate (MSU) Crystals:
Needle-shaped crystals that form when uric acid levels in the blood become too high.
Tophi:
Deposits of MSU crystals that can form under the skin or in other tissues, often seen in chronic gout.
Acute Gout Attack/Flare:
A sudden onset of intense joint pain, swelling, redness, and warmth, typically affecting one joint (often the big toe).
Intercritical Gout:
The period between acute gout attacks, when symptoms are absent.
Chronic Tophaceous Gout:
A more advanced stage of gout characterized by the formation of tophi and chronic joint damage.
Arthrocentesis:
A procedure in which a needle is used to remove fluid from a joint for analysis, often done to diagnose gout by looking for MSU crystals.
Urate-Lowering Therapy (ULT):
Medications that reduce uric acid levels in the blood, used to prevent gout attacks and complications.
Anti-Inflammatory Drugs:
Medications used to treat the pain and inflammation associated with acute gout attacks.
Colchicine:
A medication used to treat acute gout attacks and prevent recurrent attacks.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
A class of medications used to reduce pain and inflammation, often used in gout treatment.
Allopurinol/Febuxostat:
Urate-lowering drugs that reduce uric acid production in the body.
Probenecid/Lesinurad:
Urate-lowering drugs that increase the excretion of uric acid by the kidneys.
General Homeopathic Terms:
Similia Similibus Curentur: The fundamental principle of homeopathy, meaning "like cures like." This suggests that a substance that can cause symptoms in a healthy person can cure similar symptoms in a sick person.
Potentization/Dilution: The process of repeatedly diluting and succussing (shaking) a homeopathic remedy to increase its potency.
Proving: A systematic study in which healthy volunteers take a homeopathic remedy and record their symptoms, helping to determine the remedy’s therapeutic properties.
Materia Medica: A comprehensive reference book that lists homeopathic remedies and their associated symptoms.
Repertory: An index of symptoms and the remedies associated with them, used to select the most appropriate remedy for a patient.
Gout-Specific Terms:
Podagra: A specific term for gout affecting the big toe joint.
Arthritic Diathesis: A predisposition to developing arthritis, including gout.
Constitutional Remedy: A homeopathic remedy chosen based on the patient’s overall physical and mental characteristics, not just their gout symptoms.
Aggravation: A temporary worsening of symptoms after taking a homeopathic remedy, often considered a positive sign of healing.
Miasm: In homeopathy, a miasm is a predisposing factor or inherited weakness that makes a person susceptible to certain diseases, including gout. The three main miasms are psora, sycosis, and syphilis.
Common Homeopathic Remedies for Gout:
Colchicum: Often used for acute gout attacks with intense pain and inflammation.
Ledum: May be indicated when gout affects the feet and is worse with warmth.
Benzoic Acid: Usefulwhen gout is associated with strong-smelling urine and kidney problems.
Lycopodium: Considered for right-sided gout or when symptoms are worse on the right side.
References
References
- Davidson’s Principles and Practice of Medicine (22nd edition)
- https://www.mayoclinic.org/diseases-conditions/gout/diagnosis-treatment/drc-20372903
- https://www.healthline.com/health/gout
- https://www.versusarthritis.org/about-arthritis/conditions/gout/
- http://homeopathyclinic.co.in/10-best-homeopathic-medicines-treatment-gout/
- Hyperuricemia prevalence in Indian subjects with underlying comorbidities of hypertension and/or type 2 diabetes (2020): Patel, H., et al. (2020). Hyperuricemia prevalence in Indian subjects with underlying comorbidities of hypertension and/or type 2 diabetes. International Journal of Research in Medical Sciences, 8(3), 794-800. https://www.msjonline.org/index.php/ ijrms/article/download/7690/5464/30116
- Global, regional and national burdens of gout in the young population from 1990 to 2019: a population-based study (2023): Zhao, J., et al. (2023). Global, regional and national burdens of gout in the young population from 1990 to 2019: a population-based study. RMD Open, 9(2), e003025. https://rmdopen.bmj.com/content/ 9/2/e003025
- Epidemiology, Comorbidities and Clinical Features of Gout in Southern Part of India (Year not explicitly mentioned): Dasari, B., et al. Epidemiology, Comorbidities and Clinical Features of Gout in Southern Part of India. SAS Publishers. https://saspublishers.com/media/articles/ SJAMS_39B_3284-3288.pdf
- Epidemiology and risk factors associated with gout control among adult Asians: a real-world retrospective cohort study (2023): Harrold, L. R., et al. (2023). Epidemiology and risk factors associated with gout control among adult Asians: a real-world retrospective cohort study. Rheumatology, 62(7), 2844-2853.
- Kelley’s Textbook of Rheumatology (11th edition, 2023) by Firestein, G.S. et al.
- Harrison’s Principles of Internal Medicine (21st edition, 2022) by Jameson, J.L. et al.
- Rheumatology Secrets (5th edition, 2015) by Imboden, J.B. et al.
- Oxford Textbook of Rheumatology (4th edition, 2018) by Maddison, P. et al.
- Rheumatology (6th Edition, 2015) by Marc C. Hochberg, Alan J. Silman, Josef S. Smolen, Michael E. Weinblatt, Michael H. Weisman, Elsevier
- Goldman-Cecil Medicine (26th Edition, 2020) by Lee Goldman, Andrew I. Schafer, Elsevier
- The Gout Diet: The Ultimate Nutritional Plan for Relief in 7 Days, by Dr. Scott Brady 2021
Also Search As
Also Search As
There are several ways people can search for homeopathic articles on gout:
Online Databases:
PubMed: While primarily focused on conventional medicine, PubMed may index some homeopathic journals or articles related to complementary and alternative medicine (CAM). Use keywords like "gout" AND "homeopathy" or "homeopathic treatment" to narrow down your search.
The Homœopathic Journal: This online journal publishes original research articles, case reports, and reviews on homeopathic practice.
National Center for Homeopathy (NCH): The NCH website has a searchable database of articles and resources related to homeopathy.
Search Engines:
Google Scholar: This search engine can be used to find scholarly articles and publications on homeopathy and gout.
Google: A general search using terms like "homeopathic articles on gout" or "homeopathic treatment for gout" can yield relevant results from websites, blogs, and online journals.
Homeopathic Organizations and Libraries:
National Center for Homeopathy (NCH): The NCH website offers a variety of resources, including articles, research summaries, and links to other relevant organizations.
North American Society of Homeopaths (NASH): The NASH website may have articles and resources for members.
Local Homeopathic Libraries: Many cities have homeopathic libraries or clinics that may have a collection of books and articles on homeopathy.
Social Media:
Homeopathic Groups and Forums: Online forums and social media groups dedicated to homeopathy can be a good source of information and discussion on the topic of gout.
Consult a Homeopathic Practitioner:
Ask for Recommendations: Homeopathic practitioners may be able to suggest specific articles or resources based on your individual needs and interests.
There are several ways to search for information about gout, depending on your specific needs and interests:
Online Search Engines:
Google: The most straightforward way is to search on Google using keywords like "gout," "gout symptoms," "gout treatment," "gout diet," or specific questions you may have.
Google Scholar: If you’re looking for scholarly articles and research studies, Google Scholar is a valuable resource. You can find in-depth information on gout epidemiology, pathophysiology, diagnosis, and treatment.
Health Websites:
Reputable Health Organizations: Websites like the Mayo Clinic (mayoclinic.org), the National Institutes of Health (NIH) (nih.gov), and the Arthritis Foundation (arthritis.org) provide reliable information on gout, including symptoms, causes, risk factors, diagnosis, and treatment options.
Medical Databases:
PubMed: This is a free database of biomedical literature that includes articles from medical journals. You can search for specific topics related to gout, such as recent research findings or clinical trials.
Books:
Medical Textbooks: Standard medical textbooks like Harrison’s Principles of Internal Medicine and Kelley’s Textbook of Rheumatology provide comprehensive information on gout, covering all aspects of the disease.
Patient Education Books: Books written for patients, such as "The Gout Diet" by Dr. Scott Brady, offer practical advice on managing gout through diet and lifestyle changes.
Social Media Groups and Forums:
Online Communities: Many online forums and social media groups are dedicated to gout, where you can connect with other patients, share experiences, and ask questions. However, it’s important to be cautious and consult with a healthcare professional before making any decisions based on information found online.
Consult a Doctor:
Expert Advice: If you have concerns about gout or are experiencing symptoms, the best way to get accurate and personalized information is to consult with a doctor or rheumatologist. They can diagnose your condition, recommend treatment options, and answer any questions you may have.
Frequently Asked Questions (FAQ)
What is Gout?
Gout is a form of inflammatory arthritis caused by the buildup of uric acid crystals in the joints. This leads to sudden, severe episodes of pain, redness, and swelling, often starting in the big toe.
What causes Gout?
High levels of uric acid in the blood (hyperuricemia) are the primary cause of gout. This can occur due to increased production of uric acid, decreased excretion by the kidneys, or a combination of both. Dietary factors, genetics, certain medical conditions, and medications can also contribute.
How is gout diagnosed?
Gout is typically diagnosed based on the characteristic symptoms and a medical history. Doctors may also perform tests like:
- Synovial fluid analysis (to identify uric acid crystals)
- Blood tests (to measure uric acid levels)
- Imaging studies (X-rays, ultrasound)
Can homeopathy cure gout?
What are the symptoms of Gout?
Symptoms
- Intense joint pain
- Lingering discomfort
- Inflammation also redness
- Limited range of motion
- Rapid onset
- Severe pain
- ‘Worst pain ever’
- Extreme tenderness
- Marked swelling
How does homeopathy treat gout?
Homeopathic treatment for gout involves selecting individualized remedies based on the person’s unique symptoms, constitution, and overall health.These remedies are highly diluted substances that work by stimulating the body’s self-healing response.
What are the treatment options for gout?
- Medications: Anti-inflammatory drugs (NSAIDs, colchicine) to reduce pain and swelling during attacks, and urate-lowering therapies (ULTs) to lower uric acid levels.
- Lifestyle changes: Dietary modifications (low-purine diet), weight loss, limiting alcohol intake, and staying hydrated.
What are some common homeopathic remedies for gout?
Some commonly used homeopathic remedies for gout include:
Are there any side effects of homeopathic remedies for gout?
Homeopathic remedies are generally considered safe when used correctly. However, some people may experience a temporary worsening of symptoms (aggravation) before they start to improve. It’s important to consult with a qualified homeopathic practitioner for proper diagnosis and treatment.
