Systemic Sclerosis
Definition:
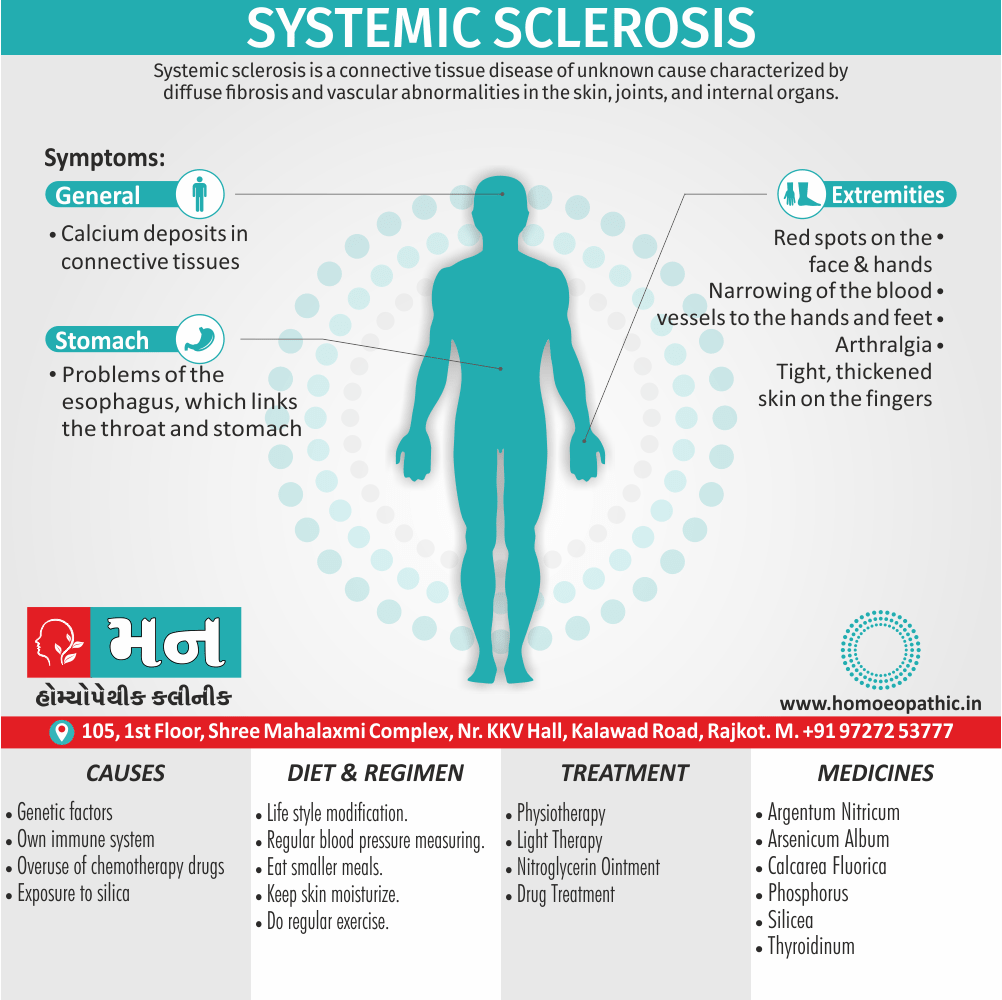
Systemic sclerosis is a connective tissue disease of unknown cause characterized by diffuse fibrosis and vascular abnormalities in the skin, joints, and internal organs. [3]
Systemic sclerosis, also known as scleroderma, is a chronic autoimmune disease characterized by the hardening and tightening of the skin and connective tissues.
There are two main types of systemic sclerosis:
- Limited cutaneous systemic sclerosis (lcSSc), previously known as CREST syndrome
- Diffuse cutaneous systemic sclerosis (dcSSc)
While there is no single synonym for systemic sclerosis, some alternative terms used to describe the condition include:
- Scleroderma
- Progressive systemic sclerosis
- CREST syndrome (limited cutaneous systemic sclerosis only)
Overview
Epidemiology
Causes of Systemic Sclerosis
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Systemic Sclerosis
- Basically, Scleroderma refers to a range of disorders in which the skin and connective tissues tighten and harden.
- That is a long-term, progressive disease also gradually gets worse.
- It is consider a rheumatic disease and a connective tissue disorder.
- This is also thought to be an autoimmune condition, in which the body’s own immune system attacks the body’s tissues.
- This results in an overproduction of collagen, the protein that forms the basis of connective tissue.
- The result is a thickening, or fibrosis, also scarring of tissue.
- Furthermore, Scleroderma is not contagious.
- And may run in families, but it often occurs in patients without any family history of the disease.
- It is thought to affect between 75,000 and 100,000 people in the United States, mostly women aged from 30 to 50 years. [2]
- Besides this, There is characterise by sclerodactyly in combination with Raynaud’s and digital ischaemia.
- The peak age of onset is in the fourth and fifth decades, and overall prevalence is 10–20 per 100 000, with a 4 : 1 female preponderance.
- All in all, That is subdivide into diffuse cutaneous systemic sclerosis & limited cutaneous systemic sclerosis. [1]
It is sometimes known as CREST syndrome, because the symptoms form the acronym, CREST i.e.:
- C: Calcinosis, or calcium deposits in tissues and under the skin
- R: Raynaud’s disease
- E:Esophageal problems, including GERD
- S: Sclerodactyly, or thick skin on the fingers
- T: Telangiectasias, or enlarged blood vessels, manifesting as red spots [2]
Epidemiology
Epidemiology:
- Female predominance: Several studies report a higher prevalence in females, with transgender man ratios ranging from 3.9:1 to 6.6:1. (Progressive systemic sclerosis in south India – 1997, Clinical and autoantibody profiles of systemic sclerosis patients: A cross-sectional study from North India – 2019)
- Peak age of onset: The peak age of onset is typically in the fourth decade of life. (Progressive systemic sclerosis in south India – 1997)
- Common presenting symptoms: The most frequent presenting symptoms include arthralgia (joint pain), skin thickening, and Raynaud’s phenomenon (less common than in Western populations). (Progressive systemic sclerosis in south India – 1997)
- High prevalence of skin involvement: Skin involvement is present in almost all patients, with skin biopsy confirming the diagnosis in a majority of cases. (Progressive systemic sclerosis in south India – 1997)
- Organ involvement: Internal organ involvement is frequent, with the lungs, gastrointestinal tract, heart, and kidneys being commonly affected. (Progressive systemic sclerosis in south India – 1997)
- Autoantibody positivity: A significant proportion of patients test positive for antinuclear antibodies (ANA), indicating autoimmune processes. (Progressive systemic sclerosis in south India – 1997)[6][7]
Causes of Systemic Sclerosis
Causes of Systemic Sclerosis:
- It is not known what causes scleroderma, but it is thought to an autoimmune condition that causes the body to produce too much connective tissue.
- This leads to a thickening, or fibrosis, and scarring of tissue.
- Connective tissue forms the fibers that make up the framework that supports the body.
- They are found under the skin and around the internal organs and blood vessels, and they help support muscles and bones.
- Genetic factors are thought to play a role, and possibly environmental factors, but this has not confirmed.
- People with scleroderma often come from families in which another autoimmune disease exists.
- It is not contagious. [2]
Risk Factors:
Risk factors that can increase your chances of developing the condition include i.e.:
- Being Native American / African American
- Being female
- Using certain chemotherapy drugs such as Bleomycin
- Exposed to silica dust also organic solvents
There’s no known way to prevent SS other than to reduce risk factors you can control. [4]
Types
Types of Systemic Sclerosis:
1. Limited Cutaneous Systemic Sclerosis (lcSSc)
- Previously known as CREST syndrome (Calcinosis, Raynaud’s phenomenon, Esophageal dysfunction, Sclerodactyly, Telangiectasias)
- Skin thickening is limited to the hands, face, feet, and forearms
- Slower progression of internal organ involvement
- Higher risk of pulmonary arterial hypertension
2. Diffuse Cutaneous Systemic Sclerosis (dcSSc)
- Skin thickening is widespread, affecting the trunk, arms, legs, and face
- Rapid progression of skin and internal organ involvement
- Higher risk of interstitial lung disease and renal crisis
It’s important to note that systemic sclerosis is a heterogeneous disease, and the severity and progression can vary significantly among individuals. Early diagnosis and treatment are crucial for managing symptoms and preventing complications.[8]
Risk Factors
Risk factors of Systemic Sclerosis:
- Genetic Predisposition: Family history and certain genetic markers have been linked to an increased risk of systemic sclerosis.
- Environmental Exposures: Exposure to certain environmental toxins, such as silica dust and organic solvents, has been associated with a higher incidence of the disease.
- Sex and Age: Women are more likely to be affected by systemic sclerosis than men, and the peak age of onset is between 30 and 50 years old.
- Ethnicity: Certain ethnic groups, such as African Americans and Native Americans, may have a higher risk of developing the condition.
- Autoimmune Diseases: Individuals with other autoimmune diseases, such as lupus or rheumatoid arthritis, may have an increased risk of developing systemic sclerosis.[4]
Pathogenesis
Pathogenesis of Systemic Sclerosis:
Systemic sclerosis (SSc) is a complex autoimmune disease characterized by fibrosis of the skin and internal organs, vasculopathy, and immune system dysregulation. Although the exact cause remains unknown, the pathogenesis involves a triad of:
Vascular Injury: Endothelial cell damage leads to microvascular dysfunction, resulting in tissue hypoxia and release of pro-fibrotic factors.
Immune Dysregulation: Autoreactive T and B cells, along with innate immune cells, drive inflammation and promote fibrosis through cytokine production and activation of fibroblasts.
Fibrosis: Excessive extracellular matrix deposition by activated fibroblasts leads to tissue scarring and organ dysfunction.[8]
Pathophysiology
Pathophysiology of Systemic Sclerosis:
The main pathophysiological processes involved in SSc include:
- Vascular Dysfunction: This is an early and prominent feature of SSc, characterized by endothelial cell damage, vasoconstriction, and microvascular obliteration. These changes lead to reduced blood flow to tissues, resulting in ischemia and tissue damage.
- Immune Dysregulation: SSc is associated with a dysregulated immune system, characterized by autoantibody production, T cell activation, and increased production of pro-inflammatory cytokines. This immune dysfunction contributes to inflammation and tissue damage.
- Fibrosis: This is the hallmark of SSc, characterized by excessive accumulation of extracellular matrix (ECM) proteins, primarily collagen, in the skin and internal organs. Fibrosis leads to tissue thickening, hardening, and loss of function.[9]
Clinical Features
Clinical Feature of Systemic Sclerosis:
- Skin: Thickening and hardening of the skin, typically starting on the fingers and hands (sclerodactyly), and progressing to involve other areas of the body. Raynaud’s phenomenon (cold-induced color changes in the fingers and toes) is often the first symptom.
- Musculoskeletal: Joint pain and stiffness, muscle weakness, and tendon friction rubs.
- Gastrointestinal: Esophageal dysmotility (difficulty swallowing), gastroesophageal reflux disease (GERD), small bowel bacterial overgrowth, and constipation.
- Pulmonary: Interstitial lung disease (ILD), pulmonary arterial hypertension (PAH), and aspiration pneumonia.
- Cardiovascular: Myocardial fibrosis, pericarditis, and Raynaud’s phenomenon.
- Renal: Scleroderma renal crisis (SRC), a rare but serious complication characterized by sudden onset of high blood pressure and kidney failure.[9]
Sign & Symptoms
Sign & Symptoms of Systemic Sclerosis
Scleroderma
Skin:
- Initially, there is non pitting oedema of fingers and flexor tendon sheaths.
- Subsequently, the skin becomes shiny and taut, and distal skin creases disappear.
- This is accompany by erythema and tortuous dilatation of capillary loops in the nailfold bed, readily visible with an ophthalmoscope or dissecting microscope (and oil placed on the skin).
- The face and neck are usually involve next, with thinning of the lips and radial furrowing.
- Moreover, In some patients, skin thickening stops at this stage.
- Skin involvement restricted to sites distal to the elbow or knee (apart from the face) is classifying as ‘limited disease’ or CREST syndrome.
- Involvement proximal to the knee and elbow and on the trunk is classified as ‘diffuse disease’.
Raynaud’s phenomenon:
- This is a universal feature also can precede other features by many years.
- Involvement of small blood vessels in the extremities may cause critical tissue ischaemia, leading to skin ulceration over pressure areas, localised areas of infarction and pulp atrophy at the fingertips.
Musculoskeletal features:
- Arthralgia, morning stiffness also flexor tenosynovitis are common.
- Restricted hand function is due to skin rather than joint disease also erosive arthropathy is uncommon.
- Muscle weakness and wasting can occur due to myositis.
Gastrointestinal Involvement:
- Smooth muscle atrophy and fibrosis in the lower two thirds of the oesophagus lead to reflux with erosive oesophagitis.
- Furthermore, Dysphagia and odynophagia may also occur.
- Involvement of the stomach causes early satiety and occasionally outlet obstruction.
- Recurrent occult upper gastrointestinal bleeding may indicate a ‘watermelon’ stomach (antral vascular ectasia), which occurs in up to 20% of patients.
- Besides this, Small intestine involvement may lead to malabsorption due to bacterial overgrowth and intermittent bloating, pain or constipation.
- Lastly, Dilatation of large or small bowel due to autonomic neuropathy may cause pseudo obstruction with nausea, vomiting, abdominal discomfort and distension, often worse after food.
Pulmonary Involvement:
- This is a major cause of morbidity also mortality.
- Pulmonary hypertension complicates long standing disease and is six times more prevalent in LCSS than in DCSS.
- It presents with rapidly progressive dyspnoea (more rapid than interstitial lung disease), right heart failure also angina, often in association with severe digital ischaemia.
- Fibrosing alveolitis mainly affects patients with DCSS who have topoisomerase 1 antibodies.
Renal involvement:
- In brief, One of the main causes of death is hypertensive renal crisis, characterised by rapidly developing malignant hypertension and renal failure. [1]
Clinical Examination
Clinical Examination:
Skin Examination
The skin examination is a critical component of the SSc clinical assessment. It involves a thorough evaluation of the skin’s texture, color, and thickness. The extent of skin involvement is typically assessed using the modified Rodnan skin score (mRSS), which ranges from 0 (no skin involvement) to 51 (severe skin involvement).
Musculoskeletal Examination
The musculoskeletal examination focuses on assessing joint mobility, muscle strength, and the presence of any deformities or contractures. The joints most commonly affected in SSc are the small joints of the hands and feet, although larger joints can also be involved.
Internal Organ Examination
The internal organ examination is an essential part of the SSc clinical assessment, as SSc can affect multiple organ systems, including the lungs, heart, kidneys, and gastrointestinal tract.
- Lungs: The lung examination involves assessing respiratory function and identifying any signs of pulmonary hypertension or interstitial lung disease.
- Heart: The heart examination focuses on identifying any signs of heart failure, pericarditis, or arrhythmias.
- Kidneys: The kidney examination involves assessing kidney function and identifying any signs of scleroderma renal crisis.
- Gastrointestinal Tract: The gastrointestinal examination focuses on identifying any signs of esophageal dysmotility, small bowel bacterial overgrowth, or colonic involvement.[10]
Diagnosis
Diagnosis of Systemic Sclerosis
Scleroderma is primarily a clinical diagnosis but various laboratory abnormalities are characteristic.
The ESR is usually elevate also raised levels of IgG are common, but CRP values tend to be normal unless there is severe organ involvement or coexisting infection.
ANA is positive in about 70%, and approximately 30% of patients with DCSS have antibodies to topoisomerase 1 (Scl70).
About 60% of patients with CREST syndrome have anticentromere antibodies. [1]
The following tests may be necessary:
- Looking at the skin under a microscope to check for changes either in the tiny blood vessels, or capillaries, around the fingernails
- Skin biopsy
- Blood tests to assess the levels of certain antibodies [2]
Differential Diagnosis
Diffrential Diagnosis:
Connective Tissue Diseases:
- Systemic lupus erythematosus (SLE)
- Dermatomyositis/polymyositis
- Mixed connective tissue disease (MCTD)
- Rheumatoid arthritis (RA)
Vasculitides:
- Eosinophilic fasciitis
- Scleroderma renal crisis
- Polyarteritis nodosa
Other Conditions:
- Raynaud’s phenomenon
- Fibromyalgia
- Carpal tunnel syndrome
- Edema
- Nephrogenic systemic fibrosis
- Graft-versus-host disease
- Drug-induced scleroderma-like reactions[8]
Complications
Complications :
Skin Complications:
- Raynaud’s Phenomenon: This is often the first symptom of systemic sclerosis, causing vasospasm of small blood vessels in the fingers and toes in response to cold or stress. Severe cases can lead to digital ulcers and tissue damage.
- Skin Tightening and Thickening: Fibrosis of the skin can lead to limited range of motion, difficulty swallowing, and facial disfigurement.
- Calcinosis: Calcium deposits can form under the skin, causing pain and discomfort.
- Digital Ulcers: These painful sores can develop on the fingertips or toes due to poor circulation and Raynaud’s phenomenon.
Musculoskeletal Complications:
- Joint Pain and Stiffness: Arthritis can affect joints, leading to pain, swelling, and limited mobility.
- Muscle Weakness and Atrophy: Muscle involvement can lead to weakness and decreased muscle mass.
- Tendinitis and Bursitis: Inflammation of tendons and bursae (fluid-filled sacs near joints) can cause pain and limited movement.
Gastrointestinal Complications:
- Esophageal Dysmotility: Difficulty swallowing and acid reflux can occur due to impaired esophageal function.
- Gastroparesis: Delayed stomach emptying can lead to nausea, vomiting, and bloating.
- Small Intestine Bacterial Overgrowth (SIBO): This condition can cause abdominal pain, bloating, and diarrhea.
- Malabsorption: Nutrient absorption can be impaired, leading to malnutrition and weight loss.
Pulmonary Complications:
- Interstitial Lung Disease (ILD): This is a serious complication where lung tissue becomes scarred and inflamed, leading to shortness of breath and decreased lung function.
- Pulmonary Arterial Hypertension (PAH): High blood pressure in the lungs can lead to heart failure and decreased exercise tolerance.
Cardiac Complications:
- Arrhythmias: Irregular heartbeats can occur, leading to palpitations and other symptoms.
- Heart Failure: The heart’s pumping ability can be compromised due to fibrosis and other complications.
- Pericarditis: Inflammation of the lining around the heart can cause chest pain and other symptoms.
Renal Complications:
- Scleroderma Renal Crisis: This rare but serious complication involves sudden onset of high blood pressure and kidney failure. It requires prompt medical attention.[8]
Investigations
Investigations:
Autoantibody Testing: Antinuclear antibodies (ANAs) are present in almost all patients with SSc. Specific autoantibodies, such as anti-centromere antibodies and anti-topoisomerase I antibodies, can help distinguish between limited and diffuse cutaneous SSc.
Blood Tests: These may include complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), renal function tests, and liver function tests.
Pulmonary Function Tests: Spirometry, lung volumes, and diffusing capacity measurements can assess lung involvement, particularly interstitial lung disease.
Imaging Studies: Chest X-ray, high-resolution computed tomography (HRCT) of the chest, echocardiogram, and barium swallow can assess organ involvement in the lungs, heart, and gastrointestinal tract.
Other Investigations: These might include nailfold capillaroscopy, skin biopsy, and electromyography (EMG) or nerve conduction studies, depending on the clinical presentation.[8]
Treatment
Treatment of Systemic Sclerosis
No treatments are available that either halt or reverse the fibrotic changes that underlie the disease.
The focus of management, therefore, is to ameliorate the effects of the disease on target organs.
Treatment for generalized symptoms may involve:
- Corticosteroids
- Immunosuppressants, such as methotrexate or Cytoxan
- Nonsteroidal anti-inflammatory drugs (in other words, NSAID)
Depending on your symptoms, treatment can also include:
- Blood pressure medication
- Medication to aid breathing
- Physical therapy
- Light therapy, such as ultraviolet A1 phototherapy
- Nitroglycerin ointment to treat localized areas of tightening of the skin [4]
Raynaud’s syndrome & Digital ulcers i.e.:
- Raynaud’s should treat by avoidance of cold exposure and use of mittens (heated mittens are available), supplemented if necessary with calcium antagonists.
- Intermittent infusions of prostacyclin may benefit severe digital ischaemia.
- The endothelin 1 antagonist bosentan can be of value in promoting healing of digital ulcers.
- If these become infected, antibiotics may required, but as these penetrate tissues poorly in scleroderma, they need to be given at higher doses for a longer duration than usual.
Oesophageal Reflux i.e.:
- It should treated with proton pump inhibitors and antireflux agents.
- Antibiotics may required for bacterial overgrowth syndromes, and metoclopramide or domperidone may help patients with symptoms of pseudo obstruction.
Hypertension i.e.:
- It should be treated aggressively with ACE inhibitors, even if renal impairment is present.
Joint involvement i.e.:
- This may be treated with analgesics and/or NSAID.
- If synovitis is present, immunosuppressants such as methotrexate can also be of value.
Pulmonary Hypertension i.e.:
- This may be treated with bosentan.
- In selected patients, heart–lung transplantation may be considered.
- Corticosteroids and cytotoxic drugs are indicated in patients who have coexisting myositis or fibrosing alveolitis. [1]
Prevention
Prevention:
- No Specific Preventive Measures: As the etiology of SSc remains unclear, there are no established strategies for primary prevention.
- Focus on Early Detection & Management: While we can’t prevent the onset of SSc, early diagnosis and prompt treatment can significantly improve outcomes and quality of life for those affected.
- Avoidance of Triggers (in susceptible individuals): Some environmental factors (like silica dust, certain chemicals) and possibly some medications might trigger SSc or worsen its symptoms in susceptible individuals. Avoiding these potential triggers might be helpful in some cases, but this needs to be discussed with a healthcare professional.[8]
Homeopathic Treatment
Homeopathic Treatment of Systemic Sclerosis
Argentum Nitricum:
- Pale face.
- Tight drawing of skin over bones.
- Skin becomes brown, tense, dry also hard.
- Drawing in skin as from a either spider web or dried albuminous substance.
- Irregular blotches.
- Worse by warmth in any form, at night, left side.
- Better especially in fresh air & cold.
Arsenicum Album:
- Face: Swollen, pale, sunken, cold.
- Throat: Swollen, oedematous, constricted, unable to swallow.
- Extremities: Swelling of feet.
- Skin: Swellings, oedema, gangrenous inflammations.
- Worse: Cold, wet weather.
- Better: Heat.
Calcarea Fluorica:
- Face: Hard swelling on cheek also jaw bone with pain.
- Extremities: Gouty enlargements of finger joints.
- Skin: Indurations of stony hardness.
- Worse: During rest, changes of weather.
- Better: Heat.
Phosphorus:
- Skin: Tightness on forehead.
- Face: Pale, sickly complexion, blue rings especially under eyes. Swelling also necrosis of lower jaw.
- Extremities: Ascending sensory also motor paralysis from ends of fingers also toes. In detail, Numbness in hands.
- Worse: Touch, physical or mental exertion, change of weather, from getting wet in hot weather.
- Better: specifically Cold, open air, washing with cold water.
Silicea:
- Skin: Delicate, pale, waxy. In detail, Dry fingertips.
- Worse: In morning, from washing, damp cold weather.
- Better: Warmth, summer, either in wet or humid weather.
Thyroidinum:
- Skin: Dry. Additionally, Swelling of glands of stony hardness.
- Worse: Night. [5]
Diet & Regimen
Diet And Regimen:
- Balanced and Nutritious: Focus on a diet rich in fruits, vegetables, whole grains, and lean protein. This provides essential nutrients and antioxidants that support immune function, tissue repair, and energy levels.
- Hydration: Staying well-hydrated is crucial, especially if you experience dry mouth or skin. Aim for at least 8 glasses of water daily.
- Small, Frequent Meals: This can aid digestion, particularly if you have gastrointestinal issues like reflux or bloating.
- Fiber: Adequate fiber intake supports gut health and regularity. Include sources like fruits, vegetables, legumes, and whole grains.
- Limit Salt: Reducing sodium can help manage blood pressure and swelling.
- Healthy Fats: Incorporate sources like avocados, nuts, seeds, and olive oil for heart health and inflammation control.
- Calcium and Vitamin D: These are important for bone health, especially if you’re at risk of osteoporosis.
- Mindful Eating: Pay attention to hunger and fullness cues. Avoid overeating, which can worsen reflux and discomfort.
Lifestyle Modifications
- Regular Exercise: Gentle exercise improves circulation, flexibility, and muscle strength. Consult your doctor for suitable options.
- Stress Management: Techniques like meditation, yoga, or deep breathing can help manage stress and its impact on symptoms.
- Sleep: Prioritize good sleep hygiene for optimal rest and recovery.
- Avoid Smoking and Alcohol: These can exacerbate SSc symptoms and complications.
- Skin Care: Use gentle, moisturizing products to protect and soothe dry skin.
- Oral Hygiene: Regular dental care is essential, especially if you have dry mouth.[11]
Do’s and Don'ts
Do’s :
Prioritize medical care:
- Establish a strong relationship with a rheumatologist specializing in SSc.
- Adhere to prescribed medications and treatment plans.
- Attend regular checkups for monitoring disease progression and addressing any complications promptly.
Adopt a healthy lifestyle:
- Eat a balanced diet rich in fruits, vegetables, whole grains, and lean protein.
- Stay hydrated by drinking plenty of water throughout the day.
- Engage in regular, gentle exercise to improve circulation, flexibility, and muscle strength.
- Prioritize good sleep hygiene for optimal rest and recovery.
- Practice stress management techniques like meditation, yoga, or deep breathing.
Protect your skin:
- Moisturize regularly to keep skin supple and prevent cracking.
- Use sunscreen with a high SPF when outdoors.
- Avoid harsh soaps and hot water.
- Wear protective clothing in cold weather to prevent Raynaud’s phenomenon.
Manage oral health:
- Brush and floss regularly, especially if you experience dry mouth.
- Visit your dentist for routine checkups and cleanings.
- Stay informed and connected:
- Learn about SSc and its management from reliable sources.
- Join support groups to connect with others facing similar challenges.
- Communicate openly with your healthcare team and loved ones about your needs and concerns.
Don’ts
- Smoke: Smoking can worsen SSc symptoms and increase the risk of complications.
- Consume excessive alcohol: Alcohol can interact with medications and exacerbate certain symptoms.
- Ignore symptoms:Report any new or worsening symptoms to your doctor promptly.
- Overexert yourself: Listen to your body and avoid strenuous activities that could lead to fatigue or injury.
- Isolate yourself: Seek support from friends, family, and healthcare professionals.
- Neglect mental health: Address any feelings of anxiety, depression, or stress with appropriate coping mechanisms or professional help.
Terminology
Terminology:
Systemic Sclerosis (SSc): This is the overarching term for the disease, signifying its impact on multiple body systems, not just the skin.
Scleroderma: Literally means "hard skin," reflecting a key symptom but not encompassing the full spectrum of the disease.
Autoimmune Disease: SSc falls into this category, implying that the body’s immune system mistakenly attacks its own healthy tissues.
Fibrosis: This refers to the excessive buildup of connective tissue, leading to hardening and thickening of skin and internal organs.
Vasculopathy: Denotes abnormalities in blood vessels, often manifesting as Raynaud’s phenomenon (cold sensitivity and color changes in fingers and toes).
Raynaud’s Phenomenon: This is a common early symptom, characterized by exaggerated blood vessel constriction in response to cold or stress.
other examples :
Telangiectasias: These are small, dilated blood vessels visible on the skin surface, often appearing as red spots.
Calcinosis: Refers to calcium deposits forming under the skin, causing hard lumps.
Esophageal Dysmotility: Indicates impaired movement of food through the esophagus, leading to difficulties with swallowing and reflux.
Interstitial Lung Disease (ILD): This involves inflammation and scarring of lung tissue, potentially impacting breathing function.
Pulmonary Arterial Hypertension (PAH): High blood pressure in the lung arteries can strain the heart and lead to shortness of breath.
Sclerodactyly: Describes thickening and tightening of the skin on fingers and toes, sometimes causing contractures (limited joint movement).
Digital Ulcers: These are painful sores on fingertips or toes, often associated with poor blood flow.
Renal Crisis: This is a serious complication involving sudden high blood pressure and kidney damage.
Antinuclear Antibodies (ANA): These are autoantibodies often present in SSc, helping in diagnosis.
Limited Cutaneous SSc (lcSSc): Previously known as CREST syndrome, this subtype involves skin thickening primarily on hands, feet, and face.
Diffuse Cutaneous SSc (dcSSc): This subtype features more widespread skin thickening and a higher risk of internal organ involvement.
Homeopathic Terminologies
- Similia Similibus Curentur: The fundamental principle of homeopathy, meaning "like cures like." It states that a substance that can cause symptoms in a healthy person can cure similar symptoms in a sick person.
- Repertory: A reference book listing symptoms and the homeopathic remedies associated with them.
- Materia Medica: A collection of detailed descriptions of the properties and effects of homeopathic remedies.
- Constitutional Remedy: A remedy chosen based on the patient’s overall physical, mental, and emotional characteristics.
- Miasm: A predisposition to certain types of diseases, believed to be inherited and treatable with specific homeopathic remedies.
- Potency: The degree of dilution and succussion (vigorous shaking) a homeopathic remedy undergoes. Higher potencies are believed to have deeper and longer-lasting effects.
- Aggravation: A temporary worsening of symptoms after taking a remedy, often seen as a positive sign of healing.
- Proving: A systematic process of testing a substance on healthy individuals to observe its effects and create a remedy picture.
References
Reference:
- Davidson’s Principles and Practice of Medicine (22nd edition) Ch. 25
- https://www.medicalnewstoday.com/articles/176357.php
- https://www.msdmanuals.com/professional/musculoskeletal-and-connective-tissue-disorders/autoimmune-rheumatic-disorders/systemic-sclerosis
- https://www.healthline.com/health/scleroderma#symptoms
- Zomeo Ultimate LAN 3.0
- Progressive systemic sclerosis in south India – 1997, Clinical and autoantibody profiles of systemic sclerosis patients: A cross-sectional study from North India – 2019
- Progressive systemic sclerosis in south India – 1997
- Kelly’s Textbook of Rheumatology
Edition ,11th - Varga, J., & Abraham, D. (2020). Systemic sclerosis. In Firestein, G. S., Budd, R. C., Gabriel, S. E., McInnes, I. B., & O’Dell, J. R. (Eds.), Kelley and Firestein’s Textbook of Rheumatology (11th ed., pp. 1342-1376). Elsevier.
- Systemic Sclerosis (Second Edition), Edited by Christopher P. Denton and Dinesh Khanna, 2017, Springer International Publishing AG
- Systemic Sclerosis: A Guide to Management. 3rd Edition. Clements PJ, Furst DE, editors. Springer; 2018.
Also Search As
Also Searched As :
Online search engines:
Use specific keywords:
"homeopathy systemic sclerosis"
"homeopathic treatment for scleroderma"
"natural remedies for systemic sclerosis"
"homeopathic articles on scleroderma"
Combine keywords with additional terms:
"case studies"
"research"
"clinical trials"
"patient testimonials"
Specify the type of information they need:
"remedies in homeopathy"
"homeopathic approach"
"doctors for systemic sclerosis"
Homeopathic websites and forums:
Visit websites of renowned homeopathic organizations and practitioners.
Search for articles and blogs on their websites related to systemic sclerosis.
Participate in online forums and discussions dedicated to homeopathy.
Ask questions and seek recommendations from experienced homeopaths.
Libraries and bookstores:
Browse the health and wellness sections for books on homeopathy.
Look for books specifically addressing autoimmune diseases or systemic sclerosis.
Consult librarians for assistance in finding relevant resources.
Recommendations from healthcare professionals:
Discuss homeopathy with their primary care physician or rheumatologist.
Ask for recommendations on reliable sources of information or homeopathic practitioners specializing in systemic sclerosis.
Using Different Terminology:
Systemic sclerosis: The official medical term, widely used in scientific literature and healthcare settings.
Scleroderma: A more common term, often used interchangeably with systemic sclerosis, but can also refer to localized scleroderma (a less severe skin condition).
CREST syndrome: An acronym for the five main features of limited cutaneous systemic sclerosis: Calcinosis, Raynaud’s phenomenon, Esophageal dysfunction, Sclerodactyly, and Telangiectasias.
Progressive systemic sclerosis: A term used to describe the more severe form of systemic sclerosis with widespread skin involvement and internal organ complications.
Specifying Search Intent:
General information: "What is systemic sclerosis?", "scleroderma symptoms", "scleroderma causes"
Specific aspects: "scleroderma diet", "scleroderma treatment options", "scleroderma and pregnancy"
Latest research: "scleroderma clinical trials", "new treatments for scleroderma", "scleroderma research breakthroughs"
Support and resources: "scleroderma support groups", "living with scleroderma", "scleroderma patient stories"
Using Search Engines and Databases:
General search engines: Google, Bing, DuckDuckGo, etc. Good for finding general information and patient resources.
Medical databases: PubMed, MedlinePlus, etc. Best for accessing scientific articles and clinical trial information.
Specialized websites: Scleroderma Foundation, National Institutes of Health (NIH), etc. Offer reliable, curated information and resources.
Frequently Asked Questions (FAQ)
What is Systemic Sclerosis?
Systemic sclerosis is a connective tissue disease of unknown cause characterized by diffuse fibrosis and vascular abnormalities in the skin, joints, and internal organs.
What causes Systemic Sclerosis?
- Autoimmune
- Genetic factors
- Using certain chemotherapy drugs
- Exposed to silica dust
- Come from families
Is there a cure for systemic sclerosis?
Currently, there’s no cure.Treatment focuses on managing symptoms, slowing progression, and preventing complications.
Can systemic sclerosis be prevented?
There’s no known way to prevent SSc, but early diagnosis and treatment can improve outcomes.
Can homeopathy cure systemic sclerosis?
Homeopathy aims to stimulate the body’s self-healing mechanisms to address the underlying imbalances contributing to systemic sclerosis. While it cannot guarantee a cure, it can offer significant relief from symptoms, improve quality of life, and potentially slow disease progression.
What are the symptoms of Systemic Sclerosis?
- Non pitting oedema of fingers and flexor tendon sheaths
- Shiny and taut
- Erythema and tortuous dilatation of capillary loops
How long does it take to see results with homeopathy?
The response to homeopathic treatment varies from person to person. Some individuals experience relief within weeks, while others may take longer. It’s essential to be patient and consistent with treatment for optimal results.
How does homeopathy differ from conventional treatment for systemic sclerosis?
Conventional treatment focuses on managing symptoms and preventing complications with medications and therapies. Homeopathy takes a holistic approach, considering the individual’s physical, mental, and emotional state to select remedies that address the root cause of the disease.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Systemic Sclerosis?
- Argentum Nitricum
- Arsenicum Album
- Calcarea Fluorica
- Phosphorus
- Silicea
- Thyroidinum
