Obsessive Compulsive Disorder
Definition
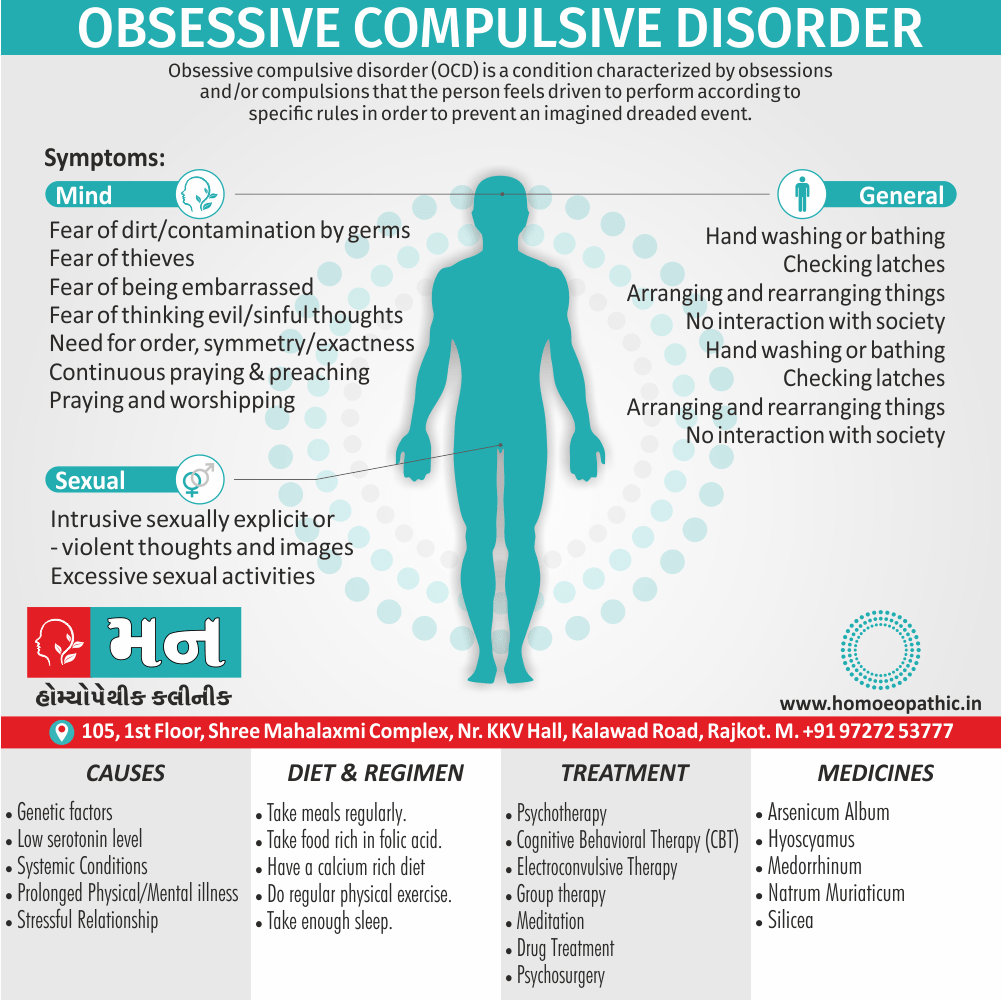
Obsessive compulsive disorder (OCD) is a condition characterized by obsessions and/or compulsions that the person feels driven to perform according to specific rules in order to prevent an imagined dreaded event.
OCD is the fourth most common psychiatric disorder and is usually a chronic condition—it therefore represents a high burden of morbidity within the population. Effective treatment is available, so prompt diagnosis and referral are essential. [1]
While there aren’t perfect synonyms for Obsessive Compulsive Disorder (OCD) that capture the full clinical picture, here are some options depending on the aspect you want to emphasize:
Focusing on obsessions:
- Rumination disorder: This emphasizes the dwelling on intrusive thoughts.
Focusing on compulsions:
- Intrusive thoughts disorder: This highlights the unwanted and repetitive thoughts.
- Repetitive behavior disorder: This focuses on the repetitive actions.
Informal terms:
- Obsessive-compulsive personality disorder (OCPD): This is a different condition, but the term is sometimes misused for OCD. It describes a personality pattern of perfectionism and orderliness, not intrusive thoughts and compulsions.
It’s important to note that these are not official diagnoses and shouldn’t be used for self-diagnosis. "OCD spectrum disorder" is also used sometimes, but it’s not a recognized diagnosis either.
For accuracy, it’s best to use Obsessive-Compulsive Disorder (OCD) or refer to the specific obsessions or compulsions someone experiences.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Obsessive Compulsive Disorder
Obsessions are recurrent persistent thoughts, impulses, or images that enter the mind despite efforts to exclude them. The feeling of compelled to undergo the intrusion of a thought, impulse, or image and the resistances produced against them are key characteristics of an obsession. [1]
In India, obsessive compulsive disorder (OCD) is more common in unmarried males, while in other countries, no gender differences are reported.
This disorder is commoner in persons from upper social strata and with high intelligence. The average age of onset is late third decade (i.e. late 20s) in India, while in the Western countries the onset is usually earlier in life.
A summary of long-term follow-up studies shows that about 25% remained unimproved over time, 50% had moderate to marked improvement while 25% had recovered completely. [2]
An obsession is define as:
- An idea, impulse or image which intrudes into the conscious awareness repeatedly.
- It is recognise as one’s own idea, impulse or image but is perceive as ego-alien (foreign to one’s personality).
- It is recognise as irrational and absurd (insight is present).
- Patient tries to resist against it but is unable to.
- Failure to resist, leads to mark distress.
- An obsession is usually associate with compulsion.
A compulsion is define as:
- A form of behaviour which usually follows obsessions.
- It is aim at either preventing or neutralising the distress or fear arising out of obsession.
- The behaviour is not realistic and is either irrational or excessive.
- Insight is present, so the patient realises the irrationality of compulsion.
- The behaviour is perform with a sense of subjective compulsion (urge or impulse to act).
- Compulsions may diminish the anxiety associate with obsessions. [2]
Epidemiology
Epidemiology of Obsessive Compulsive Disorder
The epidemiology of Obsessive-Compulsive Disorder (OCD) in India has been studied in various research publications.
One study, "An epidemiological study of obsessive compulsive disorder in adolescents from India" (2015), found that the prevalence of OCD among adolescents in India was 0.8%, with a male predominance. The study also revealed that OCD was more prevalent among Muslims and increased with age.[5]
Another source, "Clinical practice guidelines for Obsessive-Compulsive Disorder" (2017), reported that the lifetime prevalence of OCD in India is estimated to be between 1-3%, similar to global estimates. However, it highlights that Indian patients tend to have higher remission rates compared to those in Western countries.[6]
Additional information from "An overview of Indian research in obsessive compulsive disorder" (2011) mentions a lifetime prevalence of 0.6% based on a study by Reddy et al. (2010). It also emphasizes the chronic course of OCD, with symptoms often waxing and waning over time.[7]
These studies collectively provide insights into the prevalence, demographics, and clinical course of OCD in the Indian population. It is important to note that prevalence rates may vary across different studies due to methodological differences and the populations sampled.
Causes
Causes of Obsessive Compulsive Disorder
Genetics:
The lifetime risk for Obsessive compulsive disorder increase tenfold in first-degree relatives of patients diagnosed with OCD.
It is not certain whether this familial pattern indicates genetic causes rather than family environment, because the necessary large-scale twin and adoption studies have not carried out.
Neurobiological mechanisms:
Structural organic abnormalities i.e.:
Parents with OCD have an increase rate of minor, non-localizing neurological signs but no specific neurological lesion has identified.
Positron emission tomography (in other words; PET) and functional MRI have shown increased activity in the frontal lobes, caudate nucleus, and cingulum in OCD patients.
Neurotransmitters i.e.:
Generally, The clinical benefits of SSRIs in OCD suggest that a dysregulation of the 5HT pathways may play a role in its aetiology.
Furthermore, A variety of randomized controlled challenge studies have undertaken and have shown that giving a 5HT antagonist increased anxiety levels in OCD.
Lastly, Evidence for the involvement of dopaminergic pathways in OCD comes from the fact that disorders of the basal ganglia (for example; Tourette’s, post-encephalitic parkinsonism) show a high level of obsessive symptoms.
Autoimmune factors i.e.:
For many years it has known that Sydenham’s chorea—an autoimmune disease of the basal ganglia—is associated with OCD in two-thirds of cases.
Besides this, These patients have autoantibodies to the caudate nucleus. Additionally, More recently, an association has made between Group A streptococcal infections and OCD/tic disorders.
Early experience:
In brief, Obsessional mothers might expected to transmit a tendency to obsessional symptoms to their children through social learning.
Psychological causes:
Obsessions can thought of as a conditioned response to an anxiety-provoking event.
The patient develops avoidant behaviours (of which compulsions are part) to try also avoid experiencing the anxiety provoking event.
Sigmund Freud’s psychoanalytic approach suggests that the symptoms of OCD reflect unsolved conflicts or impulses of either a violent or sexual nature.
All in all, These impulses create anxiety, which avoid by the use of defence mechanisms. [1]
Types
Types of Obsessive Compulsive Disorder
Obsessive-Compulsive Disorder (OCD) encompasses various subtypes, each characterized by distinct obsessions and compulsions.
This book Obsessive-Compulsive Disorder: The Ultimate Teen Guide (2nd Edition) provides a detailed exploration of different OCD themes, including:
Contamination OCD:
Obsessions with germs, dirt, or illness leading to excessive cleaning or avoidance behaviors.
Harm OCD:
Fear of causing harm to oneself or others, often accompanied by checking compulsions.
Symmetry/Orderliness OCD:
Obsessions with things being "just right," leading to arranging, counting, or repeating behaviors.
Religious/Scrupulosity OCD:
Obsessive thoughts and compulsions related to religious beliefs, morality, or fear of sinning.
Relationship OCD (ROCD):
Obsessive doubts and anxieties about romantic relationships.
Sexual Orientation OCD (SO-OCD):
Obsessive doubts about one’s sexual orientation.
Pedophilia OCD (POCD):
Unwanted intrusive thoughts about harming children, leading to significant distress and compulsions.[8]
Risk Factors
Risk factors
A comprehensive resource discussing risk factors for OCD is:
This book Obsessive-Compulsive Disorder Demystified delves into various factors that can increase the likelihood of developing OCD, including:
- Genetics: Having a family history of OCD or related disorders
- Brain Structure and Function: Abnormalities in certain brain regions and neurotransmitter systems
- Environmental Factors: Stressful life events, trauma, or infections
- Personality Traits: Certain personality traits, such as perfectionism or high anxiety
- Comorbid Conditions: Co-occurring mental health disorders, such as depression or anxiety disorders[9]
Pathogenesis
Pathogenesis of Obsessive Compulsive Disorder
A comprehensive resource discussing the pathogenesis of OCD is:
This book Neuroscientific Foundations of Cognitive Behaviour Therapy: Theory and Practice explores the underlying neurobiological mechanisms involved in OCD, including:
Cortico-Striato-Thalamo-Cortical (CSTC) Circuits:
Dysfunction in these brain circuits, which are involved in regulating thoughts and behaviors, plays a key role in OCD.
Neurotransmitters:
Imbalances in neurotransmitters like serotonin, dopamine, and glutamate contribute to the development and maintenance of OCD symptoms.
Genetic Predisposition:
Certain genes increase the susceptibility to OCD, although the exact genetic mechanisms are still being investigated.
Environmental Factors:
Stressful life events, trauma, or infections can trigger or exacerbate OCD symptoms in individuals with a genetic predisposition.[10]
Pathophysiology
Pathophysiology
This book Obsessive-Compulsive Disorder: Phenomenology, Pathophysiology, and Treatment provides a comprehensive overview of the current understanding of the pathophysiology of Obsessive-Compulsive Disorder (OCD), including:
Neurocircuitry:
Dysfunction in specific brain circuits, primarily the cortico-striato-thalamo-cortical (CSTC) loops, is implicated in OCD. These circuits are involved in regulating thoughts, emotions, and behaviors.
Neurotransmitters:
Imbalances in neurotransmitters, particularly serotonin, dopamine, and glutamate, are believed to play a crucial role in OCD. Serotonin reuptake inhibitors (SRIs) are often effective in treating OCD, supporting the involvement of serotonin dysregulation.
Genetics:
OCD has a heritable component, with studies suggesting a complex interplay of multiple genes contributing to susceptibility. However, the exact genetic mechanisms are still under investigation.
Environmental Factors:
Stressful life events, trauma, and infections can trigger or exacerbate OCD symptoms in individuals with a genetic predisposition. [11]
Clinical Features
Clinical Features of Obsessive Compulsive Disorder
Washers:
- Basically; This is the commonest type.
- Here the obsession is of contamination with dirt, germs, body excretions and the like.
- Additionally; The compulsion is washing of hands or the whole body, repeatedly many times a day.
- It usually spreads on to washing of clothes, washing of bathroom, bedroom, door knobs also personal articles, gradually.
- The person tries to avoid contamination but is unable to, so that washing becomes a ritual.
Checkers:
- In this type, the person has multiple doubts, e.g. the door has not been locked, kitchen gas has been left open, counting of money was not exact, etc.
- The compulsion, of course, is checking repeatedly to ‘remove’ the doubt.
- Any attempt to stop the checking leads to mounting anxiety.
- Before one doubt has cleared, other doubts may creep in.
Pure Obsessions:
- Generally, This syndrome is characterize by repetitive intrusive thoughts, either impulses or images which are not associated with compulsive acts.
- The content is usually sexual or aggressive in nature.
- The distress associated with these obsessions is dealt usually by counter-thoughts (for example counting) and not by behavioural rituals.
- A variant is obsessive rumination, which is a preoccupation with thoughts.
- Here, the person repetitively ruminates in his mind about the pros and cons of the thought concerned.
Primary Obsessive Slowness:
Obsessive compulsive disorder A relatively rare syndrome, additionally it is characterize by severe obsessive ideas and/or extensive compulsive rituals, in the relative absence of manifested anxiety.
This leads to mark slowness in daily activities. This sub type is quite difficult to diagnose in the routine clinical practice, unless the possibility of this subtype is keep in mind.
In clinical practice, one of the most useful scales is the Y-BOCS (Yale-Brown Obsessive compulsive disorder Scale). It can use to elicit the symptomatology and rate the severity of OCD.
The Y-BOCS classifies the symptoms and signs of OCD as follows:
- Aggressive obsessions
- Contamination obsessions
- Sexual obsessions
- Hoarding/Saving obsessions
- Religious/Scrupulous obsessions
- Obsession with need for symmetry or exactness
- Somatic obsessions
- Miscellaneous obsessions
- Cleaning/washing compulsions
- Checking compulsions
- Repeating rituals
- Counting compulsions
- Ordering/arranging compulsions
- Hoarding/collecting compulsions
- Miscellaneous compulsions. [2]
Sign & Symptoms
Sign & Symptoms
Obsessive compulsive disorder is characterize by obsessional thinking, compulsive behaviour, and varying degrees of other psychiatric symptomatology.
The feeling of being compell to undergo the intrusion of a thought, impulse, or image and the resistances produced against them are key characteristics of an obsession.
They may come in the form of any of the following:
Obsessions:
Obsessional thoughts i.e.:
These intrude forcibly into the patient’s mind and the patient attempts to exclude them. Obsessional thoughts may be single words, phrases, or rhymes; they are usually unpleasant or shocking to the patient, obscene, or blasphemous.
Obsessional images i.e.:
They typically appear as vividly imagine scenes, often of violence or of a kind that disgusts the patient, such as abnormal sexual practices.
Obsessional ruminations i.e.:
They are internal debates in which continuous arguments reviewed endlessly.
Obsessional doubts i.e.:
They thoughts about actions that may have completed inadequately, such as failing to turn off a gas tap completely, or about actions that may have harmed other people.
Obsessional impulses i.e.:
These are urges to perform acts, usually of a violent or embarrassing kind; for example, leaping in front of a car or shouting blasphemies in church. The urges are resist strongly, and are not carried out, but the internal struggle may very distressing.
Obsessional rituals:
- These are repeat but senseless activities.
- They may mental activities, such as counting repeatedly in a special way or repeating a certain form of words, or behaviours, such as excessive hand washing or lock checking.
- Rituals are usually follow by temporary release of distress. The ritual may follow by doubts whether it has completed in the right way, and the sequence may be repeated over and over again.
- Patients are aware that their rituals are illogical, and usually try to hide them.
Anxiety and depressive symptoms:
- Symptoms are often present in patients with Obsessive compulsive disorder. In some patients these are an understandable reaction to the obsessional symptoms, but in others there are recurring depressive moods that arise independently of the other symptoms.
- Depersonalization occurs sometimes, adding to the patient’s disability. Although they share the same name, obsessional personality and Obsessive compulsive disorders do not have a simple one-to-one relationship.
Obsessional personality:
- It is over-represent among patients who develop Obsessive compulsive disorder, but about a third of obsessional patients have other types of personality.
- Moreover, although people with obsessional personality may develop OCDs, they are more likely to develop depressive disorders.
Clinical Examination
Clinical Examination of Obsessive Compulsive Disorder
A comprehensive resource detailing the clinical examination of Obsessive-Compulsive Disorder (OCD) is:
This book "Obsessive-Compulsive Disorder: Practical Management" (Fourth Edition) provides a detailed guide for clinicians on assessing OCD, including:
Clinical Interview:
Thoroughly exploring the patient’s history, including the nature and severity of obsessions and compulsions, their impact on daily life, and any associated distress or impairment.
Mental Status Examination:
Evaluating the patient’s cognitive functioning, emotional state, and presence of any other psychiatric symptoms.
Rating Scales:
Utilizing standardized rating scales, such as the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS), to assess the severity of OCD symptoms and monitor treatment response.
Physical Examination:
Ruling out any underlying medical conditions that may contribute to or mimic OCD symptoms.[12]
Diagnosis
Diagnosis
The diagnosis of Obsessive-Compulsive Disorder (OCD) is primarily based on the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM).
The DSM-5 provides specific criteria for diagnosing OCD, including:
Presence of Obsessions and/or Compulsions:
- Obsessions: Recurrent and persistent thoughts, urges, or images that are experienced as intrusive and unwanted, causing marked anxiety or distress.
- Compulsions: Repetitive behaviors or mental acts that an individual feels driven to perform in response to an obsession or according to rules that must be applied rigidly.
Time-Consuming or Clinically Significant Distress/Impairment:
The obsessions and/or compulsions are time-consuming (e.g., take more than 1 hour per day) or cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
Not Attributable to Substance Use or Another Medical Condition:
The symptoms are not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition.
Not Better Explained by Another Mental Disorder:
The disturbance is not better explained by the symptoms of another mental disorder (e.g., excessive worries in generalized anxiety disorder, preoccupation with appearance in body dysmorphic disorder).[13]
Differential Diagnosis
Differential Diagnosis
While this book Obsessive-Compulsive Disorder: The Ultimate Teen Guide (2nd Edition) primarily targets teenagers, it offers valuable insights into the differential diagnosis of Obsessive-Compulsive Disorder (OCD), which involves distinguishing it from other conditions with similar symptoms. These include:
- Anxiety Disorders: Generalized Anxiety Disorder (GAD), Panic Disorder, and Specific Phobias can share some features with OCD, such as excessive worry and avoidance behaviors.
- Tic Disorders: Tourette’s Syndrome and other tic disorders can co-occur with OCD or present with repetitive behaviors that may resemble compulsions.
- Eating Disorders: Anorexia Nervosa and Bulimia Nervosa can involve ritualistic behaviors around food and body image that may appear similar to OCD compulsions.
- Body Dysmorphic Disorder (BDD): Individuals with BDD have excessive preoccupation with perceived flaws in their appearance, leading to repetitive behaviors like mirror checking or grooming rituals.
- Obsessive-Compulsive Personality Disorder (OCPD): While sharing some features with OCD, OCPD is a personality disorder characterized by a pervasive pattern of preoccupation with orderliness, perfectionism, and control. [14]
Complications
Complications of Obsessive Compulsive Disorder
This book Obsessive-Compulsive Disorder Demystified discusses several complications that can arise from untreated or poorly managed Obsessive-Compulsive Disorder (OCD), including:
- Social Isolation: The time-consuming nature of OCD rituals and the fear of judgment can lead to social withdrawal and isolation.
- Relationship Problems: OCD can strain relationships due to the impact on daily routines, intimacy, and communication.
- Occupational Impairment: The time and energy devoted to OCD rituals can interfere with work or school performance.
- Physical Health Problems: Skin problems from excessive washing, musculoskeletal issues from repetitive movements, and sleep disturbances are common physical complications.
- Comorbid Mental Health Disorders: OCD frequently co-occurs with other mental health conditions, such as depression, anxiety disorders, and eating disorders, exacerbating the overall burden.[9]
Investigations
Investigation
There is no specific investigation for diagnosing Obsessive-Compulsive Disorder (OCD). The diagnosis is primarily based on clinical assessment, including a detailed interview and observation of the patient’s symptoms and behaviors. However, some investigations may be done to rule out other medical conditions that could mimic OCD or contribute to its symptoms.
This book Obsessive-Compulsive Disorder: Practical Management (Fourth Edition) mentions the following investigations that may be relevant in the context of OCD:
Physical Examination and Medical History: A thorough physical examination and review of the patient’s medical history can help identify any underlying medical conditions that may be contributing to the symptoms or that need to be considered in the differential diagnosis.
Laboratory Tests: Blood tests or other laboratory investigations may be conducted to rule out medical conditions that can mimic OCD symptoms, such as thyroid disorders or autoimmune diseases.
Neuroimaging: In some cases, brain imaging studies like MRI or PET scans may be used to investigate brain structure and function in individuals with OCD, although these are not routinely used for diagnosis.
Psychological Assessments: Standardized rating scales like the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) can be used to assess the severity of OCD symptoms and monitor treatment response.[12]
Treatment
Treatment
General measures for all patients:
Psychoeducation
Problem-solving techniques and relaxation
Self-help books
Psychotherapy:
Psychoanalytic psychotherapy is use in certain selected patients, who are psychologically oriented.
Supportive psychotherapy is an important adjunct to other modes of treatment. Supportive psychotherapy is also need by the family members.
Behavior Therapy and Cognitive Behavior Therapy (in other words; CBT):
Behavior modification is an effective mode of therapy, with a success rate as high as 80%, especially for the compulsive acts. It is customary these days to combine CBT with BT at most centers.
The techniques used are listed below:
- Thought-stopping (and its modifications)
- Response prevention
- Systematic sensitization
- Modelling
Electroconvulsive Therapy (ECT):
In presence of severe depression with OCD, ECT may be needed.
ECT is particularly indicated when there is a risk of suicide and/or when there is a poor response to the other modes of treatment. However, ECT is not the treatment of first choice in OCD.
Drug Treatment:
1. Benzodiazepines (e.g. alprazolam, clonazepam) have a limited role in controlling anxiety as adjuncts and should be used very sparingly.
2. Antidepressants: Some patients may improve dramatically with specifi c serotonin reuptake inhibitors (SSRIs).
- Clomipramine (75-300 mg/day), a nonspecifi c serotonin reuptake inhibitor (SRI), was the first drug used effectively in the treatment of OCD. The response is better in the presence of depressive symptoms, but many patients with pure OCD also improve substantially.
- Fluoxetine (20-80 mg/day) is a good alternative to clomipramine and often preferred these days for its better side-effect profi le. Fluvoxamine (50-200 mg/day) market as a specific anti-obsessional SSRI drug, whilst paroxetine (20-40 mg/day) and sertraline (50-200 mg/day) are also effective in some patients.
3. Antipsychotics: These occasionally use in low doses (e.g. haloperidol, risperidone, olanzapine, aripiprazole, pimozide) in the treatment of severe, disabling anxiety.
4. Buspirone has also used beneficially as an adjunct for augmentation of SSRIs, in some patients.
5. Anxiolytic drugs are not recommending to use routinely in OCD, although they may be used in the short term whilst waiting for an SSRI to take effect.
Psychosurgery:
Psychosurgery can use in treatment of OCD that has become intractable, and is not responding to other methods of treatment. It is worth mentioning that psychosurgery is only available as a treatment choice at a very few centres throughout the world.
The best responders are usually those who have significant associate depression, although pure obsessives also do respond.
The main benefit is the mark reduction in associated distress and severe anxiety.
The procedures which can be employed are:
i. Stereotactic limbic leucotomy.
ii. Stereotactic subcaudate tractotomy.
Psychosurgery is usually followed by intensive behaviour therapy aimed at rehabilitation. [2]
Prevention
Prevention
While this book Is Fred in the Refrigerator? Taming OCD and Reclaiming My Life primarily focuses on the author’s personal experience with OCD and recovery journey, it indirectly touches upon prevention strategies by highlighting the importance of:
- Early Identification and Intervention: Recognizing early signs and symptoms of OCD can lead to timely intervention and prevent the disorder from worsening.
- Stress Management: Developing healthy coping mechanisms for stress can reduce the likelihood of OCD symptoms emerging or escalating.
- Building Resilience: Cultivating resilience and emotional well-being can protect against the development of OCD in response to life challenges.
- Seeking Support: Reaching out to mental health professionals and support groups can provide guidance and resources for managing stress and preventing OCD from taking hold.
While there is no guaranteed way to prevent OCD, these strategies can contribute to reducing the risk and promoting mental well-being.[15]
Homeopathic Treatment
Homoeopathic Treatment of Obsessive Compulsive Disorder
Few of our amazing remedies in Homeopathic treatment of OCD include:
Arsenicum Album:
For persistent thoughts of death.
Indicated in people with fear of solitude, of spectres, and of robbers, with desire to hide oneself. Indecision and Changeable humour, which demands this at one time, that at another, and rejects everything after having obtained it.
Hyoscyamus Niger:
For persistent thoughts of sex.
Indicated in people who are obsessed with thoughts of sex. They constantly pick at clothes and resort to obscene gesturing.
Medorrhinum:
For persistent thoughts of washing hands.
Indicated when there is obsession to wash hands repeatedly. There is also an intense fear of going incomprehensible and the dark.
Natrum Muriaticum:
For compulsion to check locked doors repeatedly. When there is such intense fear of being robbed that they keep checking locks. Obsessed about being in control of a situation.
Silicea:
For persistent thoughts of pins.Obsessive fear of pins and needles. Keep collecting and counting them. These people are mentally very alert and oversensitive to sounds. [3]
Homeopathic treatment for OCD offers a minimum of 100 remedies effective against the disease.
THOUGHTS: Persistent: Disease, of: 1Alum, 1Aral, 3Ars, 1Aur, 1Chel, 1Cygn-c, 1Harp, 1Hura, 1Kali-p, 1Lepi, 1Loxo-r, 1Merc, 1Murx, 1Nat-m, 1Nat-p, 3Ph-ac, 1Phos, 1Sabal, 1Sep, 1Sulph, 1Tax-br, 1Zinc
WASHING, GENERAL: Hands, always, washes the: 1Allox, 1Ars, 2Carc, 1Coca, 1Cur, 2Lac-c, 2Med, 2Nat-m, 1Nat-sil, 1Plat, 2Psor, 1Sep, 1Sil, 2Sulph, 3Syph, 1Thuj
HOUSEKEEPING, GENERAL: Obsessed, with house cleaning: 3Ars, 2Calc, 3Carc, 1Lac-f, 2Nux-v,1Rhus-g, 1Sep, 1Sil, 1Sulph, 1Syph, 1Thuj
FEARS, PHOBIAS, GENERAL: Contamination, germs, of: 3Ars, 1Bor, 1Bov, 3Calc, 2Carc, 1Cur, 1Lac-c, 2Lach, 1Med, 1Nat-m, 1Psor, 1Sil, 3Sulph, 1Syph, 3Thuj
The remedy abbreviations with
- 4 marks- most effective,
- 3 marks- quite effective,
- 2 marks- less effective,
- 1 mark- least effective. [4]
Diet & Regimen
Diet & Regimen
While there isn’t a specific "OCD diet" that cures the disorder, certain dietary and lifestyle modifications may help manage symptoms and improve overall well-being for individuals with Obsessive-Compulsive Disorder (OCD).
A helpful resource in this regard is:
The Mindfulness Workbook for OCD: A Guide to Overcoming Obsessions and Compulsions Using Mindfulness and Cognitive Behavioral Therapy by Jon Hershfield, MFT
This book doesn’t explicitly focus on diet, but it emphasizes the importance of a healthy lifestyle for managing OCD.
Diet
- Balanced Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean protein can provide essential nutrients for brain health and overall well-being.
- Regular Meals: Eating regular meals and avoiding skipping meals can help stabilize blood sugar levels and reduce anxiety, which can trigger OCD symptoms.
- Limit Caffeine and Alcohol: Caffeine and alcohol can exacerbate anxiety and interfere with sleep, potentially worsening OCD symptoms.
- Omega-3 Fatty Acids: Some studies suggest that omega-3 fatty acids found in fish oil may have a positive impact on OCD symptoms. However, more research is needed.
Regimen:
In addition to diet, a healthy regimen can play a crucial role in managing OCD:
- Regular Exercise: Regular physical activity can reduce stress, improve mood, and promote better sleep, all of which can benefit individuals with OCD.
- Adequate Sleep: Sleep deprivation can worsen OCD symptoms, so it’s important to prioritize good sleep hygiene.
- Stress Management Techniques: Mindfulness, meditation, yoga, and other relaxation techniques can help manage stress and reduce the intensity of OCD symptoms.
- Cognitive Behavioral Therapy (CBT): CBT is an effective treatment for OCD that focuses on identifying and changing unhelpful thought patterns and behaviors.
Disclaimer:
It’s important to note that dietary and lifestyle changes alone are not a substitute for professional treatment for OCD. It’s crucial to consult with a healthcare provider or a registered dietitian for personalized advice and guidance.[16]
Do’s and Don'ts
Do’s & Don’ts
Obsessive Compulsive Disorder (OCD) Do’s and Don’ts:
Do’s:
Do seek professional help:
OCD is a treatable condition, and early intervention can lead to better outcomes. Consult a mental health professional specializing in OCD for accurate diagnosis and treatment.
Do educate yourself about OCD:
Learn about the symptoms, causes, and treatment options for OCD. This knowledge can empower you and help you manage the disorder effectively.
Do practice relaxation techniques:
Mindfulness, meditation, deep breathing exercises, and yoga can help reduce stress and anxiety, which can trigger OCD symptoms.
Do engage in regular physical activity:
Exercise can improve mood, reduce stress, and promote overall well-being, which can be beneficial for individuals with OCD.
Do maintain a healthy lifestyle:
Eating a balanced diet, getting enough sleep, and avoiding substance abuse can support overall mental health and potentially reduce the severity of OCD symptoms.
Do join a support group:
Connecting with others who understand what you’re going through can provide invaluable support, encouragement, and coping strategies.
Do be patient and persistent with treatment:
Recovery from OCD takes time and effort. Be patient with yourself and the process, and don’t give up on treatment even if you experience setbacks.
Don’ts:
Don’t try to control your thoughts or compulsions directly:
Trying to suppress obsessions or resist compulsions can often backfire and make them stronger. Instead, focus on accepting them as intrusive thoughts and gradually reducing their impact on your life.
Don’t isolate yourself:
Social withdrawal can worsen OCD symptoms. Stay connected with loved ones and engage in activities you enjoy.
Don’t be ashamed or embarrassed to seek help:
OCD is a common and treatable mental health condition. There is no shame in seeking professional help or sharing your experiences with others.
Don’t self-medicate with drugs or alcohol:
Substance abuse can worsen OCD symptoms and interfere with treatment.
Don’t engage in excessive reassurance seeking:
Constantly seeking reassurance from others can reinforce OCD rituals and prevent you from learning to cope with uncertainty.
Don’t give up hope:
OCD can be effectively managed with the right treatment and support. Don’t lose hope and continue to work towards recovery.
Remember, OCD is a complex disorder, and what works for one person may not work for another. It’s essential to work with a qualified mental health professional to develop an individualized treatment plan that addresses your specific needs and challenges.
Terminology
Terminology
Common Terminologies Used in Articles about Obsessive Compulsive Disorder (OCD):
Obsessions:
Recurrent and persistent thoughts, urges, or images that are experienced as intrusive and unwanted, causing marked anxiety or distress. Common themes of obsessions include contamination, harm, symmetry, religion, and sexuality.
Compulsions:
Repetitive behaviors or mental acts that an individual feels driven to perform in response to an obsession or according to rules that must be applied rigidly. Compulsions are aimed at reducing anxiety or preventing a dreaded event, but they are excessive and not realistically connected to what they are intended to neutralize or prevent. Common compulsions include washing, checking, ordering, counting, and repeating words silently.
Ego-dystonic:
Refers to thoughts, feelings, or behaviors that are inconsistent with one’s self-concept or values. In OCD, obsessions and compulsions are often experienced as ego-dystonic, meaning they are unwanted and distressing to the individual.
Insight:
The degree to which an individual recognizes that their OCD beliefs are not true or that their behaviors are excessive or unreasonable. Individuals with OCD can have good, fair, poor, or absent/delusional insight.
Comorbidity:
The presence of one or more additional mental health disorders alongside OCD. Common comorbidities include anxiety disorders, depression, and tic disorders.
Yale-Brown Obsessive-Compulsive Scale (Y-BOCS):
A widely used clinician-administered rating scale to assess the severity of OCD symptoms.
Exposure and Response Prevention (ERP):
A type of cognitive-behavioral therapy (CBT) that is considered the gold standard treatment for OCD. It involves gradually exposing individuals to their feared stimuli (obsessions) and preventing them from engaging in their usual compulsive responses.
Serotonin Reuptake Inhibitors (SRIs):
A class of medications that are commonly used to treat OCD by increasing the availability of serotonin in the brain.
Terminologies and Their Meaning in Homeopathic Articles on Obsessive Compulsive Disorder (OCD):
Miasm:
In homeopathy, miasm refers to a predisposing factor or underlying susceptibility to disease that is inherited and passed down through generations. In the context of OCD, homeopaths may assess the miasmatic background to understand the root cause of the disorder and select appropriate remedies.
Constitutional Remedy:
A homeopathic remedy chosen based on the individual’s overall physical, mental, and emotional characteristics, rather than just the specific symptoms of OCD. This remedy aims to address the underlying susceptibility and strengthen the person’s vital force to promote healing.
Repertory:
A comprehensive index of homeopathic symptoms and the corresponding remedies associated with them. Homeopaths use repertories to find remedies that match the patient’s unique symptom picture, including those related to OCD.
Materia Medica:
A collection of detailed descriptions of homeopathic remedies and their therapeutic properties. Homeopaths refer to materia medica to understand the specific indications and actions of each remedy and choose the most appropriate one for the patient.
Proving:
A systematic process in homeopathy where healthy individuals are given a specific remedy and their physical, mental, and emotional reactions are recorded. These provings help to establish the symptom picture of each remedy.
Aggravation:
A temporary worsening of symptoms after taking a homeopathic remedy. This is considered a positive sign in homeopathy, indicating that the remedy is stimulating the body’s healing response.
Potency:
The strength or dilution of a homeopathic remedy. Homeopathic remedies are prepared through a process of serial dilution and succussion (vigorous shaking), and the potency indicates the level of dilution.
Nosode:
A homeopathic remedy prepared from diseased tissue or pathological product. Nosodes are sometimes used in the treatment of OCD to address underlying miasmatic influences or specific disease patterns.
References
Reference
- Psychiatry, Fourth Edition- Oxford Medical Publications – SRG- by Geddes, Jonathan Price, Rebecca McKnight / Ch 24.
- A Short Textbook of Psychiatry by Niraj Ahuja / Ch 8.
- https://www.drhomeo.com/obsessive-compulsive-disorder/homeopathic-remedies-for-obsessive-compulsive-disorder/
- https://www.welcomecure.com/diseases/obsessive-compulsive-disorder-ocd/homeopathic-treatment
- "An epidemiological study of obsessive compulsive disorder in adolescents from India" (2015).
- "Clinical practice guidelines for Obsessive-Compulsive Disorder" (2017).
- "An overview of Indian research in obsessive compulsive disorder" (2011).
Obsessive-Compulsive Disorder: The Ultimate Teen Guide (2nd Edition),Author: Shala Nicely,(2021),Publisher: Instant Help Books.
Obsessive-Compulsive Disorder Demystified,Author: Cheryl Carmin,(2008),Publisher: McGraw Hill,Edition: 1st Edition
Neuroscientific Foundations of Cognitive Behaviour Therapy: Theory and Practice,Authors: Stefan G. Hofmann, Steven C. Hayes, and Eilenna Denis,(2012),Publisher: Wiley-Blackwell,Edition: 1st Edition.
Obsessive-Compulsive Disorder: Phenomenology, Pathophysiology, and Treatment,Editor: Christopher Pittenger ,(2014),Publisher: Oxford University Press,Edition: 1st Edition
"Obsessive-Compulsive Disorder: Practical Management" (Fourth Edition),Authors: Dan J. Stein, Eric Hollander, Michael A. Jenike, and Lee Baer,(2019),Publisher: Oxford University Press.
Diagnostic and Statistical Manual of Mental Disorders (DSM-5),Author: American Psychiatric Association (APA),(2013),Publisher: American Psychiatric Association Publishing
Obsessive-Compulsive Disorder: The Ultimate Teen Guide (2nd Edition),Author: Shala Nicely,(2021),Publisher: Instant Help Books
Is Fred in the Refrigerator? Taming OCD and Reclaiming My Life,Author: Shala Nicely,(2012),Publisher: New Harbinger Publications,Edition: First Edition
The Mindfulness Workbook for OCD: A Guide to Overcoming Obsessions and Compulsions Using Mindfulness and Cognitive Behavioral Therapy by Jon Hershfield, MFT ,(2011)
Publisher: New Harbinger Publications
Edition: 1st Edition
Also Search As
Also Search As
People can search for homeopathic articles on Obsessive Compulsive Disorder (OCD) through various methods:
Online Databases and Journals:
- The International Journal of Research in Homeopathy (IJRH): This peer-reviewed journal often publishes case reports and studies on homeopathic treatment for OCD. You can search their website or use academic databases like PubMed to access articles.
- The National Center for Homeopathy (NCH): The NCH website has a searchable database of articles and resources related to homeopathy, including OCD.
Homeopathic Organizations and Websites:
- National Center for Homeopathy (NCH): As mentioned above, their website is a valuable resource.
- Council for Homeopathic Certification (CHC): This organization certifies homeopathic practitioners and may have resources or links to articles on their website.
- Homeopathic Educational Services (HES): This organization offers online courses and resources, which may include articles on OCD.
Online Search Engines:
- Use specific keywords: Try searching for terms like "homeopathy OCD," "homeopathic treatment OCD," or "homeopathic remedies OCD" on Google Scholar or other search engines.
- Look for reputable sources: Stick to websites of recognized homeopathic organizations, journals, or practitioners to ensure the information is reliable and accurate.
Social Media:
- Homeopathic forums and groups: Join online forums or social media groups dedicated to homeopathy, where you can ask questions and find relevant articles shared by other members.
Libraries:
- Medical libraries: Many medical libraries have access to journals and databases that may contain homeopathic research on OCD.
Word of Mouth:
- Ask a homeopathic practitioner: If you are already seeing a homeopath, ask them for recommendations for articles or research on OCD.
Important Considerations:
- Quality of information: It’s important to critically evaluate the quality of information you find. Look for articles published in reputable journals or websites, and be wary of anecdotal evidence or unverified claims.
- Consult a homeopathic practitioner: Always consult a qualified homeopathic practitioner for personalized advice and treatment for OCD. The information found online should not be a substitute for professional consultation.
I hope this helps!
There are numerous ways to search for information on Obsessive Compulsive Disorder (OCD), catering to different needs and preferences:
Online Search Engines:
- Use search terms like "OCD," "Obsessive Compulsive Disorder," "OCD symptoms," "OCD treatment," or specific questions you have.
- Utilize reputable sources like the National Institute of Mental Health (NIMH), Mayo Clinic, or other trusted medical websites.
Academic Databases:
- If you’re looking for scholarly articles or research papers, databases like PubMed, Google Scholar, or PsycINFO can be invaluable.
- Use keywords like "OCD," "obsessive-compulsive disorder," or specific topics like "OCD neurobiology," "OCD treatment efficacy," etc.
Books:
- Many books delve into OCD’s complexities. Search online bookstores or libraries for titles like "Obsessive-Compulsive Disorder Demystified" by Cheryl Carmin or "Is Fred in the Refrigerator? Taming OCD and Reclaiming My Life" by Shala Nicely.
Mental Health Organizations:
- Organizations like the International OCD Foundation (IOCDF) offer extensive information, resources, and support for individuals with OCD and their families.
Social Media:
- Online communities and forums dedicated to OCD can provide personal stories, support, and information. Look for groups on platforms like Facebook, Reddit, or specialized mental health forums.
Medical Professionals:
- Consult a mental health professional specializing in OCD. They can provide personalized guidance, diagnosis, and treatment options.
Support Groups:
- Local or online support groups can offer a safe space to share experiences, learn coping mechanisms, and gain emotional support from others with OCD.
Additional Tips:
- Be specific in your search terms: Instead of just searching for "OCD," try using more specific terms like "OCD exposure therapy" or "OCD medication."
- Consider your needs: Are you looking for basic information, treatment options, personal stories, or research data? This will help you narrow down your search.
- Evaluate the source: Ensure the information comes from reputable sources like established medical institutions, mental health organizations, or peer-reviewed journals.
By utilizing these various methods, you can access a wealth of information on OCD, tailored to your specific interests and needs.
Frequently Asked Questions (FAQ)
What is Obsessive Compulsive Disorder?
Obsessive compulsive disorder (OCD) is a condition characterized by obsessions and/or compulsions that the person feels driven to perform according to specific rules in order to prevent an imagined dreaded event.
What causes Obsessive Compulsive Disorder?
- Genetics
- Structural organic abnormalities
- Neurotransmitters
- Autoimmune factors
- Early experience
How is Obsessive Compulsive Disorder diagnosed?
It is typically diagnosed by a mental health professional based on a clinical evaluation, including a detailed interview and assessment of symptoms.
Describe - What are the treatment options for OCD?
Treatment options for OCD include therapy (such as Cognitive Behavioral Therapy (CBT) and Exposure and Response Prevention (ERP)), medication, or a combination of both.
What are the symptoms of Obsessive Compulsive Disorder?
- Obsessional thoughts
- Obsessional images
- Obsessional ruminations
- Obsessional doubts
- Obsessional impulses
- Anxiety and depressive symptoms
- Obsessional personality
Is homeopathic treatment for OCD safe?
Homeopathic remedies are generally considered safe due to their high dilution. However, it’s essential to consult a qualified homeopath for proper assessment and treatment.
How does homeopathic treatment for OCD work?
Homeopathy seeks to stimulate the body’s self-healing abilities by using highly diluted substances that, in their undiluted form, produce symptoms similar to those of the illness.
Can homeopathy help with Obsessive-Compulsive Disorder (OCD)?
Homeopathy aims to address the individual’s unique symptoms and underlying imbalances, which may offer support for managing OCD.
How long does it take to see results with homeopathic treatment for OCD?
The response to homeopathic treatment varies depending on the individual and the severity of their condition. Some may experience improvement within weeks, while others may require longer-term treatment.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Obsessive Compulsive Disorder?
Homeopathic Medicine for Obsessive Compulsive Disorder
- Arsenicum Album
- Hyoscyamus Niger
- Medorrhinum
- Natrum Muriaticum
- Silicea
