Alcohol Use Disorder
Definition
Alcohol use disorder or Alcohol dependence was previously called as alcoholism. This term much like ‘addiction’ has been dropped due to its derogatory meaning. [2]
Here are some synonyms for Alcohol Use Disorder (AUD):
- Alcoholism: This is a widely recognized term for a severe form of AUD, characterized by a strong dependence on alcohol and difficulty controlling drinking.
- Alcohol dependence: Similar to alcoholism, this emphasizes the physical and psychological dependence on alcohol.
- Problem drinking: This is a broader term encompassing various levels of excessive or risky alcohol use, not necessarily dependence.
- Alcohol abuse: This term focuses on harmful patterns of alcohol use that lead to negative consequences but doesn’t necessarily imply dependence.
The best choice of synonym depends on the specific context and the severity of the condition you’re referring to.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Safe alcohol consumption
Acute intoxication
Withdrawal Syndrome
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do's & Don'ts
Terminology
References
Also Search As
Overview
Overview of Alcohol Use Disorder:
There are at least two billion users of alcohol worldwide, and alcohol is a major public health concern in most countries. Remembering to screen for alcohol misuse, recognizing the physical also psychological complications, and having the ability to offer basic advice and treatment are essential for all clinicians. [1]
Moving Ahead, Alcohol dependence is more common in males, and has an onset in late second or early third decade. The course is usually insidious. There is often an associated either abuse or dependence of other drugs. If the onset occurs late in life, especially after 40 years of age, an underlying mood disorder should be looked for. [2]
Epidemiology
Epidemiology
The epidemiology of Alcohol Use Disorder (AUD) in India is a complex and evolving landscape, with several studies highlighting its prevalence and patterns:
- The prevalence of alcohol use disorders using alcohol use disorders identification test (AUDIT) in the Indian setting: – a systematic review and meta-analysis (2022): This study found an overall prevalence of AUDs in India to be 12.5% (95% CI: 9 to 17.3%), with hazardous and harmful alcohol use (8.6%) being significantly higher than dependent alcohol use (2.3%).
- Epidemiological features of alcohol use in rural India: a population-based cross-sectional study | BMJ Open (2014): This research focused on rural areas and found that nearly one in four men (23.8%) had consumed alcohol in the past 12 months, with 33.2% of drinkers meeting criteria for hazardous drinking.
- (PDF) Prevalence of Alcohol use among the Indian Population and its Impact on Public Health – ResearchGate (Unknown year): This study highlights the significant impact of alcohol use on public health in India, contributing to road traffic accidents, violence, and various health conditions.
- (PDF) Epidemiology, pattern and prevalence of alcohol consumption in India: need for public health action – ResearchGate (2021): This study reports a wide range of alcohol consumption prevalence in India (10% to 60%), emphasizing the need for public health action to address this issue.
- ALCOHOL RELATED HARM – Implications for Public Health and Policy in India – NIMHANS (2019): This comprehensive report discusses the extensive implications of alcohol-related harm in India, including health, social, and economic consequences.
These studies collectively reveal a substantial burden of AUD in India, with varying patterns across different regions and populations. They underscore the urgent need for targeted public health interventions and policies to address this significant public health concern.
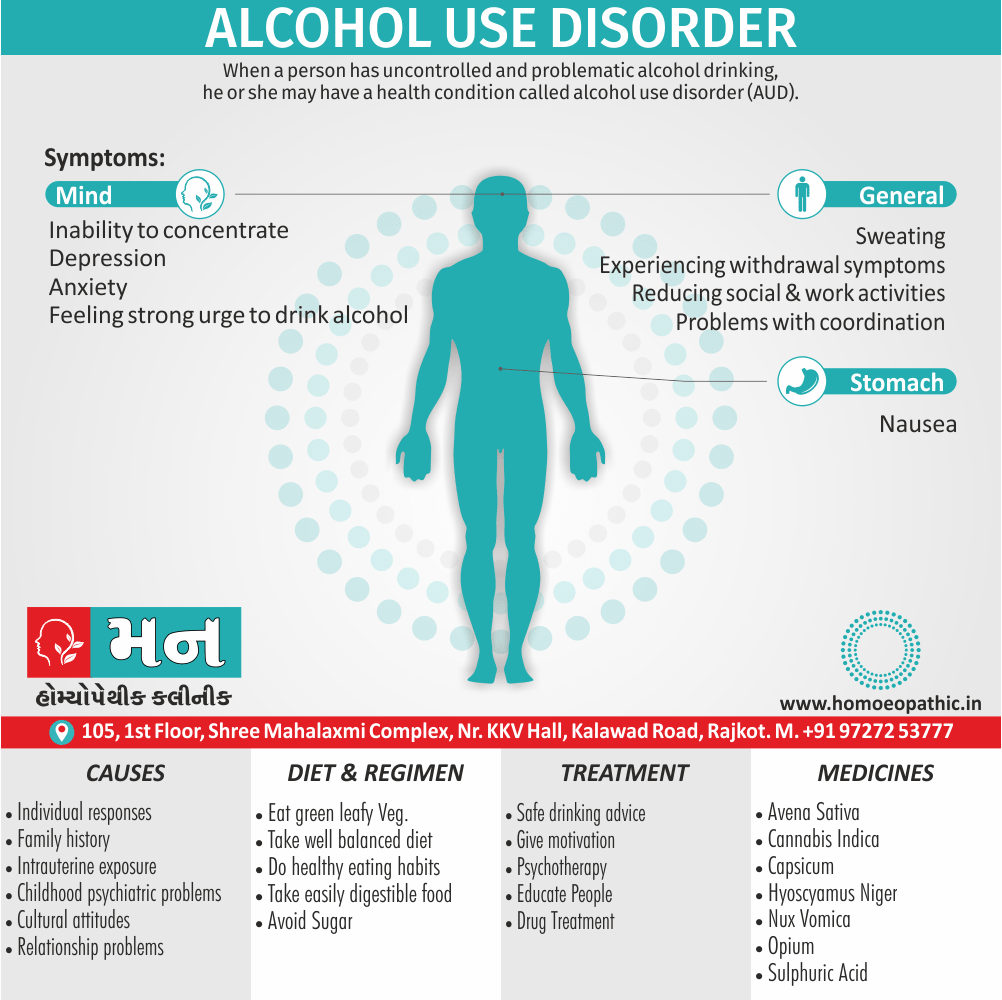
Causes
Causes of Alcohol Use Disorder
Biological:
- Heritable genetic factors
- Variations in alcohol metabolism
- Individual responses to alcohol
- Family history of substance abuse
- Intrauterine exposure to drugs or alcohol
Psychological:
- Risk taking and other personality traits
- Psychiatric problems in childhood (e.g. conduct disorder, abuse)
- Comorbid psychiatric disorders
Social:
- Laws affecting availability and price of alcohol
- Cultural attitudes and practices
- Peer pressure and/or role models Economic situation and employment
- Level of education
- Behavior within the family unit
- Divorce or relationship problems
Types
Types
According to Jellinek, there are five ‘species’ of alcohol dependence (alcoholism) on the basis of the patterns of use (also not on the basis of severity):
A. Alpha (α):
- Excessive but inappropriate drinking to relieve physical also emotional pain.
- No loss of control.
- Ability to abstain present.
B. Beta (β):
- Excessive and inappropriate drinking.
- Physical complications (e.g. cirrhosis, gastritis and neuritis) because of cultural drinking patterns and poor nutrition.
- No dependence.
C. Gamma (γ); also called as malignant alcoholism:
- Progressive course.
- Physical dependence with tolerance and withdrawal symptoms.
- Psychological dependence, also inability to control drinking.
D. Delta (δ):
- Inability to abstain.
- Tolerance.
- Withdrawal symptoms.
- The amount of alcohol consumed can be controlled.
- Social disruption is minimal.
E. Epsilon (ε):
- Dipsomania (compulsive-drinking).
- Spree-drinking.
Risk Factors
Risk factors
Genetic Factors:
- Family History: Individuals with a family history of alcoholism are at a higher risk of developing AUD. This is due to a combination of genetic and environmental factors.[4]
Environmental Factors:
- Early Exposure: Early exposure to alcohol, particularly during adolescence, increases the risk of developing AUD later in life.[5]
- Social and Cultural Influences: Cultural norms and social environments that promote heavy drinking can contribute to the development of AUD.[6]
- Stressful Life Events: Experiencing traumatic events or chronic stress can trigger or exacerbate alcohol use, leading to AUD.[7]
Psychological Factors:
- Mental Health Disorders: Co-occurring mental health disorders, such as depression, anxiety, or PTSD, can increase the risk of AUD.[4]
- Personality Traits: Certain personality traits, such as impulsivity and sensation-seeking, may be associated with a higher risk of AUD.[8]
Pathogenesis
Pathogenesis
Initial Exposure and Reinforcement:
- Reinforcement and Reward Pathways: Alcohol initially activates the brain’s reward system, particularly the mesolimbic dopamine pathway, leading to feelings of pleasure and euphoria. This positive reinforcement encourages repeated alcohol use.[10]
Neuroadaptation and Tolerance:
Neurotransmitter Changes: Chronic alcohol use leads to adaptations in neurotransmitter systems, including GABA, glutamate, dopamine, and serotonin. This results in tolerance, where higher amounts of alcohol are needed to achieve the same effects.[9]
Cellular Changes: Alcohol induces changes in the structure and function of neurons and brain circuits. This contributes to the development of dependence and withdrawal symptoms when alcohol use is reduced or stopped.[11]
Genetic and Environmental Interaction:
Genetic Predisposition: Genetic factors play a significant role in AUD pathogenesis. Certain genetic variations can increase an individual’s vulnerability to alcohol dependence and influence how their body processes alcohol.[12]
Environmental Factors: Environmental factors, such as stress, trauma, social environment, and cultural norms, can interact with genetic predisposition to trigger or exacerbate AUD.[14]
Progression to Dependence and Addiction:
- Negative Reinforcement: As alcohol use continues, it can become a way to cope with negative emotions and withdrawal symptoms, leading to a cycle of dependence and addiction.[10]
Pathophysiology
Pathophysiology
Neurotransmitter Imbalance:
GABA and Glutamate: Alcohol enhances the inhibitory neurotransmitter GABA and inhibits the excitatory neurotransmitter glutamate, leading to sedation and relaxation. Chronic alcohol use disrupts this balance, causing tolerance and withdrawal symptoms.[9]
Dopamine and Reward Pathway: Alcohol activates the brain’s reward pathway by increasing dopamine release. This reinforces alcohol-seeking behavior and contributes to the development of addiction.[10]
Brain Changes:
Neuroadaptation: Chronic alcohol use induces neuroadaptations in the brain, altering its structure and function. These changes can lead to impaired cognition, memory problems, and increased vulnerability to relapse.[11]
Brain Damage: Long-term heavy alcohol use can cause brain damage, including shrinkage of brain tissue and loss of neurons. This can lead to cognitive deficits, emotional dysregulation, and difficulty controlling impulses.[9]
Genetic and Epigenetic Factors:
Genetic Predisposition: Genetic variations can influence an individual’s susceptibility to AUD. Genes related to alcohol metabolism, neurotransmitter systems, and stress response may play a role.[12]
Epigenetic Modifications: Alcohol exposure can induce epigenetic changes, altering gene expression without changing the DNA sequence. These changes can contribute to the development and persistence of AUD.[13]
Clinical Features
Clinical Features of Alcohol use disorder
Behavioral and Psychological Symptoms:
- Craving: A strong desire or urge to drink alcohol, often accompanied by preoccupation with obtaining and consuming it.[15]
- Loss of Control: Difficulty controlling the amount or frequency of alcohol consumption, often drinking more or for longer periods than intended.[4]
- Tolerance: The need to drink increasing amounts of alcohol to achieve the desired effect or experiencing a diminished effect with continued use of the same amount.[9]
Withdrawal Symptoms:
Experiencing unpleasant physical and psychological symptoms when alcohol use is reduced or stopped, such as tremors, anxiety, nausea, and insomnia.[11]
Social and Occupational Impairment:
- Neglect of Responsibilities: Failing to fulfill major role obligations at work, school, or home due to alcohol use.[15]
- Social Problems: Continued alcohol use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by alcohol.[4]
Physical Health Problems:
- Physical Dependence: Experiencing withdrawal symptoms or using alcohol to relieve or avoid withdrawal symptoms.[9]
- Alcohol-Related Medical Conditions: Developing medical conditions related to alcohol use, such as liver disease, pancreatitis, or cardiovascular problems.[5]
Please note that the severity of AUD can vary, and individuals may not experience all of these clinical features. It’s important to consult with a healthcare professional for proper diagnosis and treatment.
Sign & Symptoms
Sign & Symptoms
Physical Effects of Alcohol Use Disorder
Gastrointestinal:
- Malnutrition and vitamin deficiencies (A, B, D, E, and folate)
- Carcinoma of the lip, tongue, pharynx, also larynx
- Gastritis also peptic ulcer
- Esophageal varices
- Esophageal carcinoma
- Either Acute or chronic pancreatitis
- Fatty liver, hepatitis, cirrhosis, also primary liver carcinoma.
Neurological:
- Peripheral neuropathy
- Dementia
- Wernicke’s encephalopathy
- Korsakoff’s syndrome
- Cerebellar degeneration
- Epilepsy
- Fetal alcohol syndrome
Other:
- Anemia, thrombocytopenia, also leukopenia
- Episodic hypoglycemia
- Haemochromatosis
- Hypertension
- Cardiomyopathy
- Myopathy
- Osteoporosis and osteomalacia
- Either Obesity or emaciation
- Facial erythema (plethora)
- Exacerbation of psoriasis
- Gout
Clinical Examination
Clinical Examination
From "The ASAM Criteria: Treatment Criteria for Addictive, Substance-Related, and Co-Occurring Conditions," Third Edition, by David Mee-Lee, MD, et al., Published in 2013 by the American Society of Addiction Medicine (ASAM).
"The clinical assessment is based on a careful history of alcohol use and related problems, coupled with a physical examination and laboratory tests. Standardized interviews and questionnaires can also be helpful. Screening tools like the Alcohol Use Disorders Identification Test (AUDIT) and the CAGE questionnaire can help identify patients who may have a problem with alcohol use." (p. 124)
The book also provides a detailed examination outline, including specific questions about:
- Quantity and frequency of alcohol use
- History of blackouts or withdrawal symptoms
- Social, occupational, or legal problems related to alcohol use
- Family history of alcohol use disorder
- Co-occurring medical or psychiatric conditions
It also recommends a physical examination to look for signs of alcohol-related organ damage, as well as laboratory tests to assess liver function, nutritional status, and other potential complications of alcohol use disorder.
Diagnosis
Diagnosis
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) is the authoritative reference for diagnosing alcohol use disorder (AUD).[16]
Key points from the DSM-5:
- AUD is defined as a problematic pattern of alcohol use leading to clinically significant impairment or distress.
- The diagnosis is based on the presence of at least two of eleven criteria within a 12-month period.
- The severity of AUD is classified as mild, moderate, or severe based on the number of criteria met.
Please note: that the DSM-5 does not provide specific wording for the diagnosis of AUD. Instead, it outlines the criteria that must be met for a diagnosis to be made. A qualified healthcare professional will use their clinical judgment to determine whether or not a diagnosis of AUD is appropriate.
Differential Diagnosis
Differential Diagnosis
1. Mood Disorders:
- Major Depressive Disorder (MDD): Individuals with MDD often self-medicate with alcohol, leading to a potential misdiagnosis of AUD.[16]
- Bipolar Disorder: Alcohol use can exacerbate mood swings in individuals with bipolar disorder or mask the underlying condition.[17]
2. Anxiety Disorders:
- Generalized Anxiety Disorder (GAD): Alcohol may temporarily relieve anxiety symptoms, leading to a cycle of dependence.[18]
- Social Anxiety Disorder (SAD): Individuals with SAD might use alcohol to cope with social situations, potentially masking the underlying disorder.[19]
3. Other Substance Use Disorders:
- Co-occurring substance use: Individuals with AUD may also misuse other substances, requiring comprehensive assessment and treatment.[20]
4. Medical Conditions:
- Medical conditions with similar symptoms: Certain medical conditions, such as liver disease or neurological disorders, can present with symptoms similar to AUD.[21]
5. Personality Disorders:
- Personality disorders with impulsive traits: Individuals with certain personality disorders, such as borderline personality disorder, may be prone to alcohol misuse due to impulsivity.[22]
Complications
Complications
Alcohol dependence is often associated with several complications; both medical and social.
Wernicke’s encephalopathy:
This is an acute reaction to a severe deficiency of thiamine, the commonest cause being chronic alcohol use. Characteristically, the onset occurs after a period of persistent vomiting.
The important clinical signs are:
- Ocular signs: Coarse nystagmus and ophthalmoplegia, with bilateral external rectus paralysis occurring early. In addition, pupillary irregularities, retinal hemorrhages and papilledema can occur, causing an impairment of vision.
- Higher mental function disturbance: Disorientation, confusion, recent memory disturbances, poor attention span also distractibility are quite common. Other early symptoms are apathy and ataxia.
Peripheral neuropathy and serious malnutrition are often co-existent. Neuropathologically, neuronal degeneration additionally hemorrhages are seen in thalamus, hypothalamus, mammillary bodies and midbrain.
Korsakoff’s psychosis:
As Korsakoff’s psychosis often follows Wernicke’s encephalopathy; these are together referred to as Wernicke-Korsakoff syndrome. Moreover, Clinically Korsakoff’s psychosis presents as an organic amnestic syndrome, characterized by gross memory disturbances, with confabulation. Insight is often impaired.
Marchiafava-Bignami disease:
This is a rare disorder characterized by disorientation, epilepsy, ataxia, dysarthria, hallucinations, spastic limb paralysis, also deterioration of personality also intellectual functioning. There is a widespread demyelination of corpus callosum, optic tracts also cerebellar peduncles. The cause is probably an alcohol-related nutritional deficiency.
Other Complications:
These include:
i. Alcoholic dementia.
ii. Cerebellar degeneration.
iii. Peripheral neuropathy.
iv. Central pontine myelinosis.
Social Complications:
- Accidents
- Marital disharmony
- Divorce
- Occupational problems, with loss of productive person-hours
- Increased incidence of drug dependence
- Criminality
- Financial difficulties.
Investigations
Investigations
Laboratory Markers of Alcohol Use Disorder
Certain laboratory markers of alcohol dependence have suggested.
These include:
i. GGT (γ-glutyl-transferase):
It raised to about 40 IU/L in about 80% of the alcohol dependent individuals. GGT returns to normal rapidly (i.e. within 48 hours) on abstinence from alcohol. An increase of GGT of more than 50% in an abstinent individual signifies a resumption of heavy drinking or an abnormality of liver function.
ii. MCV (mean corpuscular volume):
It is more than 92 fl (normal = 80-90 fl ) in about 60% of the alcohol dependent individuals. MCV takes several weeks to return to normal values after abstinence.
iii. Other lab markers:
It include alkaline phosphatase, AST, ALT, uric acid, blood triglycerides and CK. GGT and MCV together can usually identify three out of four problem drinkers. In addition, BAC (blood alcohol concentration) and breath analyzer can use for the purpose of identification.
For detection of the problem drinkers in the community, several screening instruments are available. MAST (Michigan Alcoholism Screening Test) frequently used for this purpose whilst CAGE questionnaire is the easiest to be administered (it takes only about 1-2 minutes).
Safe alcohol consumption
Safe Alcohol consumption
What is a safe level of alcohol consumption?
Low levels of alcohol consumption may protect older people against coronary heart disease. Very high levels clearly do harm, but where is the dividing line between safe and unsafe consumption? A widely accepted measure is in terms of units of alcohol; one unit is 8 g of ethanol, and corresponds to the following measures in which alcohol is usually consume:
- half a pint of beer (3–4 per cent);
- a wine glass of wine (125 ml);
- either a glass of sherry or other fortified wine (50 ml);
- a standard measure of spirits (25 ml).
It is generally agreed that the ‘safe level’ of alcohol consumption is:
- Men: up to 21 units per week;
- Women: up to 14 units per week (lower because of the lower average body weight of females).
These levels assume that the whole amount is not take on one occasion and that there are occasional drink-free days. This level is equivalent, for example, to an average of three half pints of beer a day for a man.
These limits should modified in some patients; for example, pregnant women should advise to abstain from alcohol. Dangerous levels of drinking (i.e. levels of consumption at which harm is likely) are:
- Men: over 50 units per week;
- Women: over 35 units per week.
Acute intoxication
Acute intoxication of Alcohol Use Disorder
Clinical symptoms of alcohol intoxication relate jointly to the level of alcohol in the blood and the tolerance of the individual.
Increasing blood alcohol levels lead to elated or unstable mood, impaired judgement, disinhibition, impaired social and occupational functioning, cognitive impairment, ataxia, slurred speech, incoordination, nystagmus, also eventually coma.
This state leads to an increased risk of accidents (especially road traffic accidents), violence, also public order offences.
After a brief period of excitation, there is a generalized central nervous system depression with alcohol use.
With increasing intoxication, there is increased reaction time, slowed thinking, distractibility also poor motor control. There is progressive loss of self-control with frank disinhibited behavior.
Duration of intoxication
The duration of intoxication depends on the amount and the rapidity of ingestion of alcohol. Usually the signs of intoxication are obvious with blood levels of 150-200 mg%. With blood alcohol levels of 300-450 mg%, increasing drowsiness followed by coma and respiratory depression develop.
Death occurs with blood alcohol levels between 400 to 800 mg%.
Occasionally a small dose of alcohol may produce acute intoxication in some persons. This is known as pathological intoxication.
Another feature, sometimes seen in acute intoxication, is the development of amnesia or blackouts.
Withdrawal Syndrome
Withdrawal Syndrome
Firstly, The most common withdrawal syndrome is a hangover on the next morning. Mild tremors, nausea, vomiting, weakness, irritability, insomnia also anxiety are the other common withdrawal symptoms.
Lastly, Sometimes the withdrawal syndrome may be more severe, characterized by one of the following three disturbances: delirium tremens, alcoholic seizures also alcoholic hallucinosis.
1. Delirium tremens:
Delirium tremens (DT) is the most severe alcohol withdrawal syndrome. It occurs usually within 2-4 days of complete or significant abstinence from heavy alcohol drinking in about 5% of patients, as compared to acute tremulousness which occurs in about 34% of patients.
The course is short, with recovery occurring within 3-7 days. This is an acute organic brain syndrome (delirium) with characteristic features of:
- Clouding of consciousness with disorientation in time and place.
- Poor attention span and distractibility.
- Visual (and also auditory) hallucinations and illusions, which are often vivid and very frightening. Tactile hallucinations of insects crawling over the body may occur.
- Marked autonomic disturbance with tachycardia, fever, hypertension, sweating also pupillary dilatation.
- Psychomotor agitation and ataxia.
- Insomnia, with a reversal of sleep-wake pattern.
- Dehydration with electrolyte imbalance.
- Death can occur in 5-10% of patients with delirium tremens and is often due to cardiovascular collapse, infection, hyperthermia or self-inflicted injury.
2. Alcoholic seizures (‘rum fits’):
Generalized tonic clonic seizures occur in about 10% of alcohol dependence patients, usually 12-48 hours after a heavy bout of drinking. Often these patients have been drinking alcohol in large amounts on a regular basis for many years.
Multiple seizures (2-6 at one time) are more common than single seizures. Sometimes, status epilepticus may be precipitated. In about 30% of the cases, delirium tremens follows.
3. Alcoholic hallucinosis:
Alcoholic hallucinosis is characterized by the presence of hallucinations (usually auditory) during partial or complete abstinence, following regular alcohol intake. It occurs in about 2% of patients.
These hallucinations persist after the withdrawal syndrome is over, also classically occur in clear consciousness. Usually recovery occurs within one month and the duration is very rarely more than six months.
Dehydration and electrolyte disturbance are characteristic. Blood testing shows leukocytosis, raised erythrocyte sedimentation rate (ESR), and impaired liver function.
Treatment
Treatment
Assessment:
- Extent of drinking, evidence for dependence, alcohol related disabilities, also co-morbidities.
- Arrange medical treatment for physical complications.
- Arrange psychiatric treatment for mental health problems.
Psychoeducation:
- Safe drinking advice.
- Education for either patient or family.
- Self-help materials.
Motivation for change:
- Brief interventions
- Motivational interviewing (extended brief interventions)
- Self-help materials
Safe withdrawal:
- Community based: benzodiazepines and oral thiamine.
- Inpatient based: benzodiazepines also parenteral thiamine, management of complications.
Relapse prevention and treatment of underlying issues:
- Outpatient follow-up or CBT
- Residential or day-patient programmes
- 12-step programmes (e.g. Alcoholics Anonymous)
- Marital or family therapy
- Medications: disulfiram, Acamprosate, also naltrexone
- Ongoing vitamin supplementation
- Antidepressants for depression or anxiety disorders
- Assistance with employment, accommodation, also legal issues
Pharmacological treatments:
Disulfiram:
- Disulfiram(Antabuse: 100–200 mg/day) is used, usually in specialist practice, as a deterrent to impulsive drinking. Furthermore, It interferes with the metabolism of alcohol by irreversibly blocking acetaldehyde dehydrogenase. After that, when alcohol is taken acetaldehyde accumulates with consequent flushing, headache, choking sensations, rapid pulse, and anxiety. At last, These unpleasant effects discourage the patient from drinking alcohol while taking the drug.
- Treatment with disulfiram carries the occasional risks of either cardiac irregularities or, rarely, cardiovascular collapse. So that, the drug should not be started until at least 12 hours after the last ingestion of alcohol.
- Disulfiram has unpleasant side effects, for example a persistent metallic taste in the mouth, gastrointestinal symptoms, dermatitis, urinary frequency, impotence, peripheral neuropathy, and toxic confusional states (extremely rare).
- It should not be used in patients with recent heart disease, severe liver disease, or significant suicidal ideation. The main use of disulfiram is to provide the patient with time to recover confidence that they can manage life without alcohol; also 6 months is the recommended prescription time.
Acamprosate:
- Acamprosate is a drug that enhances GABA transmission in the central nervous system. Particularly, In animals, acamprosate reduces drinking in dependent animals and reduces relapse in animals offered alcohol after a period of abstinence. RCTs have shown it to reduce cravings for alcohol in patients with alcohol dependence.
- The usual dose is 666 mg three times daily, and is started 2–7 days after cessation of drinking. Patients who benefit from it should continue for 6 months to a year.
Naltrexone:
- Naltrexone is an opiate antagonist, which inhibits the action of endogenous endorphins released when alcohol is drunk. It reduces the urge to drink, reduces the pleasurable ‘high’ produced by alcohol, also reduces the loss of control it causes.
- Short-term usage seems to reduce the risk of relapse, but is less effective than disulfiram. It is started once abstinence is achieved at 50 mg once daily.
- Patients recovering from an alcohol problem should be advised to continue taking vitamin supplements for at least 3 months after cessation of drinking.
Psychotherapy:
- The patient should be educated about the risks of continuing alcohol use, also asked to resume personal responsibility for change and be given a choice of options for change.
- Motivational enhancement therapy with or without cognitive behavior therapy and lifestyle modification is often useful, if available.
Group therapy:
- Of particular importance is the voluntary self-help group known as AA ( Alcoholics Anonymous), with branches all over the world and a membership in hundreds of thousands.
- Although the approach is partly religious in nature, many patients derive benefits from the group meetings which are non-professional in nature.
Prevention
Prevention of Alcohol use disorder
As described in the sections on epidemiology, the public health implications of alcohol use disorders are vast.
In most Western populations, approximately 90% of adults drink alcohol, and many occasionally get intoxicated.
There are seven main ways in which alcohol problems in society may be reduced.
Educate people,
- effectively persuading them not to misuse alcohol. Talking in schools, harnessing community groups, and television advertisements are all effective delivery methods. School-age education programmes are particularly important. Television and billboard adverts showing the harm alcohol may cause can deliver a striking message.
Integrated Strategies for Alcohol Prevention and Control
harmful drinking with penalties. Laws on driving whilst intoxicated have massively reduced the number of road traffic accidents due to alcohol.
Provide alternatives to drinking alcohol and engaging in drink-related activities.
Instigate harm-reduction strategies. For example, the mandatory use of seatbelts, airbags, and low speed limits has reduced driving-related morbidity and mortality.
Regulate the availability of alcohol and its price. Increasing taxation on alcohol, limiting the hours it may be sold, and having a minimum age for purchase are all effective methods.
Promote social, cultural, and religious movements to reduce alcohol consumption.
Treat individuals who have alcohol-related problems.
Homeopathic Treatment
Homoeopathic Treatment
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Alcohol Use Disorder
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Nux vomica:
Nux is the great anti.-alcoholic remedy. It corresponds to the tremor, to the nervous affection, to the headache, to the bad taste. It also corresponds to delirium tremens, where every little noise frightens and the victim finds no rest any place, springs up at night and has frightful visions. The tremor marked with ugliness and irritability and gastric disturbance. It is the remedy for the acute results of a spree; the morning big head is often large enough for the Nux cap, and the "rich brown" taste corresponds beautifully.
It is a remedy to give while the patient is still under the influence of liquor or any of the stages of alcoholism. Agaricus will sometimes control the characteristic tremor when Nux fails.
Hyoscyamus:
When delirium tremens occurs this is usually one of the first remedies indicated. The delirium is constant and loquacious, rarely inflammatory enough for Belladonna or maniacal enough for Stramonium; the pulse is small and quick and compressible, the skin is cold and clammy, the patient is tremulous and picks constantly at objects in the air. Marked sexual excitement, desire to expose person and fear of poison. The vision are those of persecution, are terrifying, and the patient makes efforts to escape. Constant insomnia is an excellent indication; outburst of laughter alerting with weeping may also occur. Dr Butler says that for the production of sleep no remedy compares with Hyoscyamus in the tincture, five or ten drops in a half glass of water, and teaspoonful doses given half-hourly.
Cannabis Indica:
A very reliable remedy in acute Alcohol Use Disorder. Some violence, talkativeness and active mind; subjects crowd upon it. Additionally, delusions and hallucination relate to exaggerated subjects time, space, etc.; face flushed, pupils dilated, perspires easily. Surprise is constantly express on the countenance.
Opium:
This is a remedy indicate in "old sinners" who have the delirium tremens over and over again. There is a constant expression of fright or terror, they have visions of animals springing up everywhere, they see ghosts, the sleep is uneasy, the breathing is stertorous. It is specifically indicate in those cases simulating apoplexy. Stramonium is suitable in habitual drunkards.
The prevailing mental characteristic is terror, all hallucinations and illusions are fright and terror producing. It has visions of animals coming at him from every corner and he tries to escape.
The face of Stramonium is bright red, not dark red as in Opium. Arsenic has visions of ghosts, also great weakness; diseases from overuse of alcohol; patients must have their accustomed drinks; great tremulousness and nervous weakness.
Suicidal tendency constantly annoyed by bugs and vermin that he sees upon his person and unceasingly tries to brush them off. Additionally, Belladonna too has delirium with visions of rats, mice, etc., and so has Calcarea Carbonica. Belladonna is easily distinguish from Opium, and Calcarea comes in as a last resort after Belladonna and Stramonium have ceased to do well.
Ranunculus bulbous
given in the tincture has found to be most calming in attacks of delirium tremens. It is undoubtedly one of our best remedies in the treatment of acute Alcohol Use Disorder. Specifically, The writer has prescribed this remedy with good results.
Cimicifuga
is useful in cases that are mentally depressed and tremor is a prominent symptom. On the other hand, The delirium is mild and the hallucinations of sight relate to small objects; there is persistent sleeplessness arid physical restlessness.
Avena sativa is a valuable remedy in alcoholism where the victim is nervous and sleepless almost to the point of delirium tremens. It is also a useful remedy in the either opium or cocaine habits. Whereas, Strophanthus has also successfully used.
Sulphuric acid :
This is the remedy for chronic alcoholism. It corresponds to inebriates on their last, who are pale and shrivelled and cold, whose stomach will not tolerate the slightest amount of food. They cannot drink water unless it is well whisked. They are quick and hasty in everything, and have a great and constant craving for brandy. It comes in long after Nux vomica, perhaps after Keely and other cures have failed over and over again. Particularly, It suits the sour breath and vomiting of alcoholic dyspepsia. "Should it produce a diarrhoea Pulsatilla is the proper antidote." ( Dr Luther Peck.) .
The constant craving for brandy reminds one of Sulphur, Nux vomica and Arsenicum, all of which have craving for spirituous liquors. Tartar emetic may useful when mucous gastric derangement predominates as after beer, with tendency to pneumonia, also accompanied by cool sweat.
Capsicum:
Capsicum in ten-drop doses of the tincture will stop the morning vomiting, sinking at the pit of the stomach and intense craving for alcohol in dipsomania, and promote the appetite. Additionally, It reduces the agitation and tremor and induces calm sleep.
Delirium tremens will often speedily relieve by Capsicum. Cantharis-continual attempts to bite; sexual excitement; face pale, yellow, dysuria. Spiritus glandium Quercus. Specifically, Burnett recommended this remedy as an antidote to the affects of alcohol, also Dr A. F. Schulz, of Fort Wayne Indiana, reported to the writer that in his opinion it would frequently cause disgust for alcoholic beverages. He has had success from its use.
Diet & Regimen
Diet and Regimen
Individuals with Alcohol Use Disorder (AUD) often experience nutritional deficiencies due to poor dietary habits and the impact of alcohol on nutrient absorption and metabolism. A well-balanced diet and healthy lifestyle can play a crucial role in their recovery and overall well-being.
Dietary Recommendations:
- Focus on nutrient-dense foods: Include plenty of fruits, vegetables, whole grains, lean protein sources, and healthy fats in the diet. These provide essential vitamins, minerals, and antioxidants that support overall health and aid in recovery.[23]
- Prioritize hydration: Drink plenty of water throughout the day to stay hydrated and support detoxification processes.[24]
- Limit processed foods, sugary drinks, and unhealthy fats: These can exacerbate nutritional deficiencies and contribute to other health problems.[25]
- Address specific nutrient deficiencies: Individuals with AUD are often deficient in thiamine (vitamin B1), folate, vitamin B12, and other nutrients. Supplementation may be necessary under medical supervision.[26]
Lifestyle Modifications:
- Regular exercise: Engaging in regular physical activity can improve mood, reduce stress, and support overall well-being.[27]
- Adequate sleep: Getting enough sleep is crucial for physical and mental health, and it can help manage cravings and improve mood.[28]
- Stress management: Practicing relaxation techniques, such as mindfulness meditation or yoga, can help reduce stress and prevent relapse.[29]
- Social support: Connecting with supportive friends, family, or support groups can provide encouragement and help individuals stay on track with their recovery.[30]
Important Note: This is a general guideline, and individual needs may vary. It is crucial to consult with a healthcare professional or registered dietitian for personalized recommendations and ongoing support.
Do's & Don'ts
Do’s & Don’ts
There isn’t a single book that provides a comprehensive list of "Do’s and Don’ts" for Alcohol Use Disorder (AUD) in the specific format you requested. However, many books offer guidance and information that can be distilled into such a list. Here are some recommendations and advice based on reputable sources:
Do’s:
- Do seek professional help: This could be through therapy, counseling, support groups, or a combination of approaches.[31]
- Do build a support system: Surround yourself with understanding and supportive people who can help you on your journey to recovery.[32]
- Do develop healthy coping mechanisms: Find alternative ways to manage stress and emotions without relying on alcohol.[33]
- Do prioritize self-care: Focus on your physical and mental health through exercise, proper nutrition, sleep, and relaxation techniques.[34]
Don’ts:
- Don’t isolate yourself: Staying connected with others is crucial for recovery.[35]
- Don’t give up: Recovery is a process, and setbacks may happen. Don’t lose hope and keep working towards your goals.[36]
- Don’t be afraid to ask for help: Reach out to professionals, support groups, or loved ones when you need it.[37]
- Don’t keep alcohol in your home: Remove temptations and triggers that could jeopardize your recovery.[38]
Important Note: It’s crucial to remember that AUD is a complex issue and what works for one person may not work for another. It’s essential to consult with healthcare professionals or addiction specialists for personalized guidance and treatment plans.
Terminology
Terminology
Although the term alcoholism is widely used in everyday speech, it has too broad a meaning to be clinically useful. It can refer to excessive consumption of alcohol, to dependence on alcohol, or to the damage caused by excessive use.
The following terms constitute more useful categories.
Hazardous:
Hazardous drinking is a level or pattern of drinking that will eventually cause harm. It applies to anyone drinking above the recommended limits, but without current alcohol-related problems.
It is not a diagnostic term in ICD-10/DSM-IV.
Harmful drinking:
Harmful drinking refers to a pattern of use that has already caused physical, mental, or social damage to the user. Additionally, It excludes those with dependence syndrome.
Damage may be acute or chronic. It is a term used in the ICD-10 but not the DSM-IV.
Alcohol abuse:
Alcohol abuse is the term used in the DSM-IV that is most similar to harmful drinking. It involves the continued drinking of alcohol despite significant employment, social, legal, or dangerous problems resulting from it.
Dependent drinking:
Dependent drinking (ICD-10) or alcohol dependency (DSM-IV). There are seven characteristics of dependence upon alcohol, three of which must have been present in the previous year to make a diagnosis:
1. Tolerance i.e.:Tolerance, as defined by either of the following i.e.:
- need for markedly increased amounts of alcohol to achieve intoxication or the desired effect;
- a markedly diminished effect with continued use of the same amount of alcohol.
2. Withdrawal i.e.:Withdrawal, as defined by either of the following:
- the characteristic withdrawal syndrome for alcohol;
- alcohol is take to relieve or avoid withdrawal symptoms.
3. Alcohol is often take in larger amounts or over a longer period than was intend.
4. There is a persistent desire for or there are unsuccessful efforts to cut down or control alcohol use.
5. A great deal of time is spend in activities necessary to obtain alcohol, use alcohol, or recover from its effects.
6. Important social, occupational, or recreational activities are give up or reduced because of alcohol use.
7. Alcohol use is continue despite knowledge of having a either persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the alcohol.
Collectively, all of these categories of disorder are best described as alcohol problems.
References
References
- Psychiatry, Fourth Edition- Oxford Medical Publications – SRG- by Geddes, Jonathan Price, Rebecca McKnight / Ch 29.
- A Short Textbook of Psychiatry by Niraj Ahuja / Ch 4.
- Homeopathy in treatment of Psychological Disorders by Shilpa Harwani / Ch 18.
- "Alcohol-Use Disorders" (2011) by The British Psychological Society & The Royal College of Psychiatrists.
- "Alcohol and Alcohol-related Diseases" (2023) edited by Helmut K. Seitz, et al.
- "ALCOHOL RELATED HARM – Implications for Public Health and Policy in India" (2019) by NIMHANS.
- "The Risk Factors of the Alcohol Use Disorders—Through Review of Its Comorbidities" (2018) by Frontiers in Neuroscience.
- "RISK FACTORS FOR ALCOHOL DEPENDENCE: A CASE-CONTROL STUDY" (2000) by Academic.oup.com (Oxford Academic).
- "Neurobiology of Alcohol Dependence" (2017) by Markus Heilig, et al. Published in Trends in Neurosciences.
"Neurobiology of Addiction" (2016) by George F. Koob and Michel Le Moal. Published in The Lancet Psychiatry.
- "The Neurobiology of Alcohol Dependence: Focus on Changes in the Brain" (2014) by Vijay A. Ramchandani, et al. Published in Alcohol Research: Current Reviews.
- "Genetics of Alcohol Use Disorder" (2019) by Howard J. Edenberg and Danielle M. Dick. Published in Annual Review of Genomics and Human Genetics.
- "Epigenetics of Alcohol Use Disorder" (2020) by Subhash C. Pandey. Published in Alcohol Research: Current Reviews.
- "Environmental Influences on Alcohol Use Disorder" (2018) by Kathleen K. Bucholz, et al. Published in Alcohol Research: Current Reviews.
- Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) (2013), American Psychiatric Association.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
- Sadock, B. J., Sadock, V. A., & Ruiz, P. (2015). Kaplan & Sadock’s synopsis of psychiatry: Behavioral sciences/clinical psychiatry (11th ed.). Wolters Kluwer.
- Stahl, S. M. (2013). Stahl’s essential psychopharmacology: Neuroscientific basis and practical applications (4th ed.). Cambridge University Press.
- Gabbard, G. O. (2014). Gabbard’s treatments of psychiatric disorders (5th ed.). American Psychiatric Publishing.
American Society of Addiction Medicine. (2016). The ASAM criteria: Treatment criteria for addictive, substance-related, and co-occurring conditions (3rd ed.).
- Kumar, V., Abbas, A. K., & Aster, J. C. (2015). Robbins and Cotran pathologic basis of disease (9th ed.). Elsevier Saunders.
- Millon, T., Krueger, R. F., & Simonsen, E. (2011). Millon clinical multiaxial inventory-IV (MCMI-IV). NCS Pearson, Inc.
- Krause’s Food & the Nutrition Care Process (14th ed., 2017) by L. Kathleen Mahan and Janice L. Raymond.
- Nutrition Therapy and Pathophysiology (3rd ed., 2016) by Marcia Nelms, Kathryn Sucher, and Sara Long.
- Advanced Nutrition and Human Metabolism (7th ed., 2016) by Sareen S. Gropper, Jack L. Smith, and James L. Groff.
- The Vitamins: Fundamental Aspects in Nutrition and Health (5th ed., 2012) by Gerald F. Combs, Jr.
- Exercise Physiology: Nutrition, Energy, and Human Performance (8th ed., 2015) by William D. McArdle, Frank I. Katch, and Victor L. Katch.
- Why We Sleep: Unlocking the Power of Sleep and Dreams (2017) by Matthew Walker.
- The Relaxation and Stress Reduction Workbook (6th ed., 2010) by Martha Davis, Elizabeth Robbins Eshelman, and Matthew McKay.
Substance Abuse Counseling: Theory and Practice (5th ed., 2014) by Patricia Stevens and Robert L. Smith.
- The Alcoholism and Drug Abuse Patient Workbook (6th Edition), by Albert Ellis and Emmett Velten (2007), Impact Publishers.
- Overcoming Alcoholism (2nd Edition), by Terence T. Gorski and Merlene Miller (2016), Independence Press.
- Sober for Good (1st Edition), by Anne M. Fletcher (2001), Houghton Mifflin Harcourt.
- The Mindfulness Workbook for Addiction (1st Edition), by Rebecca E. Williams and Patrick Fanning (2015), New Harbinger Publications.
- Staying Sober (1st Edition), by Terence T. Gorski (1987), Independence Press.
- The Big Book of Alcoholics Anonymous (4th Edition), by Alcoholics Anonymous World Services, Inc. (2001).
- Beyond Addiction (1st Edition), by Jeffrey Foote, Carrie Wilkens, and Nicole Kosanke (2009), Hazelden Publishing.
- Recovering from Alcoholism (1st Edition), by Kathleen W. FitzGerald (1996), The Rosen Publishing Group, Inc.
Also Search As
Also Search As
Online Resources:
- Reputable Websites: Organizations like the National Institute on Alcohol Abuse and Alcoholism (NIAAA) (https://www.niaaa.nih.gov/) and the Mayo Clinic (https://www.mayoclinic.org/diseases-conditions/alcohol-use-disorder/diagnosis-treatment/drc-20369250) provide comprehensive information on AUD, including symptoms, diagnosis, treatment options, and resources for seeking help.
- Search Engines: Using search engines like Google, Bing, or DuckDuckGo with keywords like "alcohol use disorder," "alcoholism," or "alcohol addiction" can yield a wealth of information, including articles, research studies, and support group listings.
Healthcare Professionals:
- Primary Care Physician: A primary care physician can assess for AUD, provide a diagnosis, and recommend appropriate treatment options or referrals to specialists.
- Addiction Specialists: Psychiatrists, psychologists, and licensed therapists specializing in addiction medicine can provide comprehensive assessment, diagnosis, and treatment for AUD.
Support Groups:
- Alcoholics Anonymous (AA): AA is a worldwide support group for individuals with AUD, offering a 12-step program for recovery.
- Al-Anon/Alateen: These groups provide support for family members and friends of individuals with AUD.
Helplines:
- The Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline: 1-800-662-HELP (4357) provides free, confidential, 24/7 support and referrals for individuals and families facing mental health and/or substance use disorders.
Libraries:
- Local libraries often have books, journals, and other resources on AUD that can be accessed by the public.
It’s important to remember that AUD is a complex medical condition requiring professional assessment and treatment. If you or someone you know is struggling with alcohol, seeking help is crucial for recovery.
Online Databases:
- PubMed: This is a free resource developed by the National Center for Biotechnology Information (NCBI) at the U.S. National Library of Medicine (NLM). It primarily focuses on biomedical literature, including research articles and reviews on AUD.
- Google Scholar: This is a free search engine that indexes scholarly literature across various disciplines, including medicine and psychology. It can be used to find research articles, theses, books, and other scholarly sources on AUD.
- ScienceDirect: This is a subscription-based database that provides access to a vast collection of scientific, technical, and medical research articles, including those on AUD.
Search Engines:
- Google, Bing, DuckDuckGo: These general search engines can be used to find a wide range of information on AUD, including news articles, blog posts, websites of organizations dedicated to AUD, and even scholarly articles. Using specific keywords like "alcohol use disorder," "alcoholism research," or "AUD treatment" can help refine your search results.
University Libraries:
- Many university libraries offer access to a variety of academic databases and journals that contain scholarly articles on AUD. If you are affiliated with a university, you may be able to access these resources through your library’s website.
Professional Organizations:
- Organizations like the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and the American Psychiatric Association (APA) often publish research articles, reports, and other resources on AUD on their websites.
Social Media:
- Platforms like Twitter and LinkedIn can be used to follow researchers, organizations, and experts in the field of AUD to stay updated on the latest research and news.
Tips for Effective Searching:
- Use specific keywords: Instead of just searching for "alcohol," use more specific terms like "alcohol use disorder," "alcohol dependence," or "alcoholism."
- Use Boolean operators: Words like "AND," "OR," and "NOT" can help you combine or exclude keywords to refine your search results.
- Use filters: Many databases and search engines allow you to filter results by date, publication type, or other criteria to narrow down your search.
- Check the credibility of sources: Ensure that the information you are accessing is from reputable sources, such as peer-reviewed journals, government agencies, or well-established organizations in the field of addiction medicine.
Frequently Asked Questions (FAQ)
What is Alcoholism?
Alcohol use disorder or Alcohol dependence was previously called as alcoholism. This term much like ‘addiction’ has been dropped due to its derogatory meaning.
What are the withdrawal symptoms of Alcohol use disorder ?
What are the causes of Alcoholism?
- Heritable genetic factors
- Variations in alcohol metabolism
- Individual responses to alcohol
- Family history of substance abuse
- Intrauterine exposure to drugs and alcohol
What are the signs and symptoms of AUD?
Sign&Symptoms
Common signs include drinking more or longer than intended, strong cravings, inability to cut down, neglecting responsibilities, and continuing to drink despite problems it causes.
How is AUD diagnosed?
Diagnosis involves a thorough assessment by a healthcare professional, including a physical exam, questions about drinking habits, and possibly questionnaires or lab tests.
What are the treatment options for AUD?
Treatment
Treatment may include counseling, medications, support groups (like Alcoholics Anonymous), and lifestyle changes. The best approach is tailored to individual needs and preferences.
Can homeopathy help with alcohol addiction?
Yes,
homeopathy offers a unique perspective on AUD, focusing on treating the individual’s specific symptoms and underlying imbalances. Homeopathic remedies aim to reduce cravings, ease withdrawal symptoms, and support overall well-being during recovery.
What homeopathic remedies are commonly used for alcohol addiction?
Homoeopathy For AUD
Several remedies may be considered, including Nux vomica (for hangover and irritability), Sulphur (for cravings and restlessness), Arsenicum album (for anxiety and weakness), and Avena sativa (for nervousness and sleep disturbances). A qualified homeopath will determine the most suitable remedy based on individual needs.
Is homeopathic treatment safe for alcohol addiction?
Homeopathic remedies are generally considered safe and non-addictive. However, it’s crucial to consult with a qualified homeopathic practitioner for proper assessment, diagnosis, and individualized treatment.
