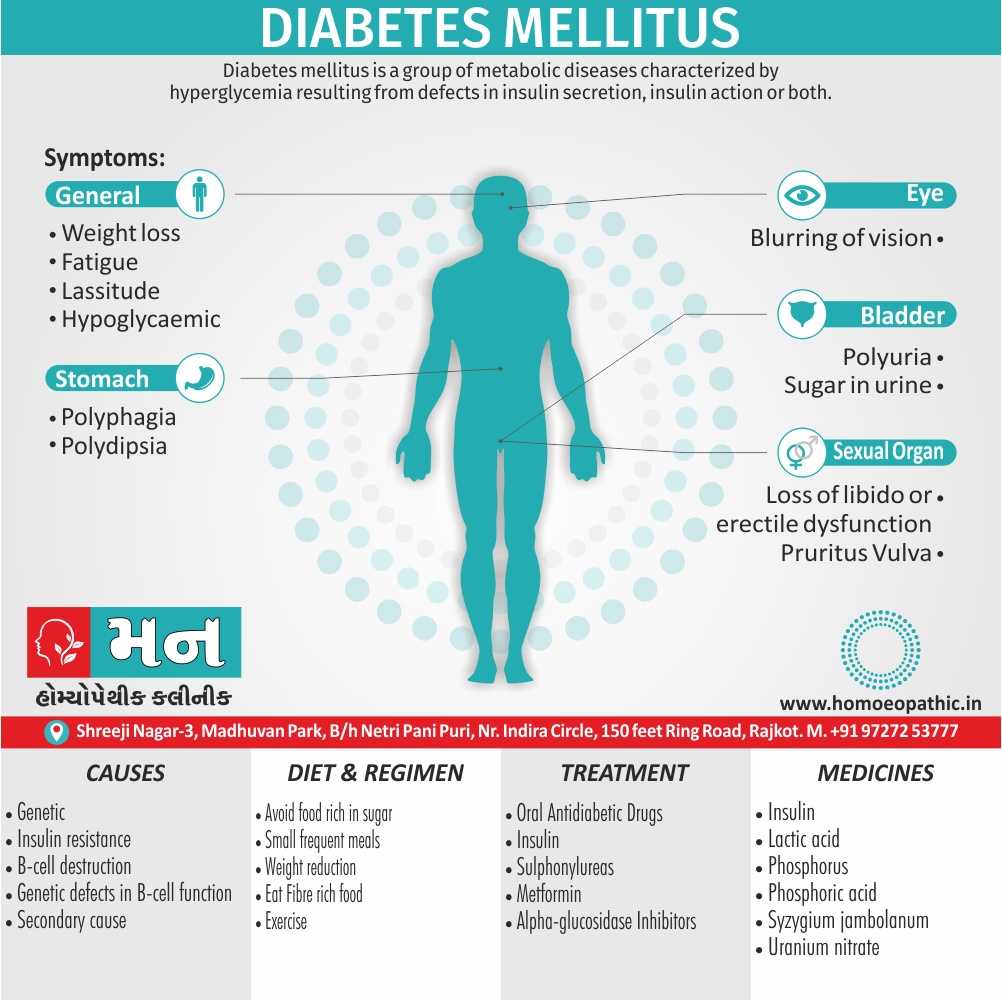
Diabetes Mellitus
Definition
Diabetes mellitus is a group of metabolic diseases characterized by hyperglycaemia resulting from defects in insulin secretion, insulin action or both.[1]
Absolutely! "Diabetes mellitus" is the precise medical term for the condition and remains the best choice for most situations. However, there are several ways to navigate communication depending on the context and desired level of specificity.
For specific types: When referring to specific subtypes, established terms like "type 1 diabetes" (often referred to as juvenile-onset diabetes in the past) or "type 2 diabetes" (adult-onset diabetes) are appropriate.
Informal terms: There are informal terms like "sugar disease" that reference the high blood sugar characteristic of diabetes. However, these can be vague and lack the clinical precision of "diabetes mellitus." Use them with caution, especially in medical contexts.
People-first language: Instead of focusing on the disease itself, consider people-first language that emphasizes the individual. "Someone with diabetes" or "a person living with diabetes" are respectful options that prioritize the person over the condition.
Historical terms: Be aware of outdated terms that are no longer appropriate. "Sugar sickness" is an older term for diabetes, while "diabetic coma" is a specific medical condition, not a synonym for diabetes itself.
Related conditions: Don’t confuse diabetes mellitus with other conditions that may have similar symptoms. "Gestational diabetes" is a temporary form of diabetes that develops during pregnancy, while "insipidus diabetes" is a completely different condition related to hormone imbalances.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
In Pregnancy
Special Categories
Diabetic Ketoacidosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
Diabetes mellitus is a disorder in which the amount of sugar in the blood is elevated. Doctors often use the full name diabetes mellitus, rather than diabetes alone, to distinguish this disorder from diabetes insipidus. Diabetes insipidus is a relatively rare disorder that does not affect blood glucose levels but, just like diabetes mellitus, also causes increased urination.[1]
Blood sugar
Generally, the three major nutrients that make up most food are carbohydrates, proteins, and fat. Sugars are one of three types of carbohydrates, along with starch also fiber.
Moreover, There are many types of sugar. Some sugars are simple, and others are complex. Table sugar (sucrose) is made of two simpler sugars called glucose and fructose. Additionally, Milk sugar (lactose) is made of glucose and a simple sugar called galactose. The carbohydrates in starches, such as bread, pasta, rice, and similar foods, are long chains of different simple sugar molecules. Sucrose, lactose, carbohydrates, also other complex sugars must be broken down into simple sugars by enzymes in the digestive tract before the body can absorb them.
Besides this, Once the body absorbs simple sugars, it usually converts them all into glucose, which is an important source of fuel for the body. Glucose is the sugar that is transported through the bloodstream and taken up by cells. All in all, The body can also make glucose from fats and proteins. Blood "sugar" really means blood glucose.[1]
Insulin
Basically, Insulin, a hormone released from the pancreas (an organ behind the stomach that also produces digestive enzymes), controls the amount of glucose in the blood. In detail, Glucose in the bloodstream stimulates the pancreas to produce insulin. Insulin helps glucose to move from the blood into the cells. Besides this, Once inside the cells, glucose is converted to energy, which is used immediately, or the glucose is stored as fat or the starch glycogen until it is needed. Lastly, The levels of glucose in the blood vary normally throughout the day.
Level of Glucose
They rise after a meal and return to pre-meal levels within about 2 hours after eating. In detail, Once the levels of glucose in the blood return to pre-meal levels, insulin production decreases. The variation in blood glucose levels is usually within a narrow range, about 70 to 110 milligrams per decilitre (mg/dL), or 3.9 to 6.1 millimoles per liter (mmol/L) of blood in healthy people. If people eat a large amount of carbohydrates, the levels may increase more. People older than 65 years tend to have slightly higher levels, especially after eating.
If the body does not produce enough insulin to move the glucose into the cells, or if the cells stop responding normally to insulin (called insulin resistance), the resulting high levels of glucose in the blood also the inadequate amount of glucose in the cells together produce the symptoms and complications of diabetes.[1]
Epidemiology
Epidemiology
Indian Epidemiology of Diabetes Mellitus
The India Diabetes (ICMR-INDIAB) study: prevalence of diabetes and prediabetes in 15 states of India in 2021 (The Lancet, 2023) found that India has a national diabetes prevalence of 101 million (10.1 crores), with an additional 136 million (13.6 crores) having prediabetes. This study provides the most recent and comprehensive data on the diabetes burden in India.[7]
Socioeconomic inequality in awareness, treatment and control of diabetes among adults in India: Evidence from National Family Health Survey of India (NFHS), 2019–2021 (Scientific Reports, 2023) highlights the significant disparities in diabetes awareness, treatment, and control across socioeconomic groups in India, emphasizing the need for targeted interventions to address these inequities.[8]
Epidemiology of type 2 diabetes in India (PubMed, 2021) offers a comprehensive review of the epidemiology of type 2 diabetes in India, covering prevalence, risk factors, and complications. It provides valuable insights into the trends and challenges associated with this chronic condition.[9]
These references, along with other sources such as the World Health Organization and the Indian government’s National Programme for Prevention and Control of Non Communicable Diseases (NP-NCD), collectively paint a picture of a growing diabetes epidemic in India. The increasing prevalence of diabetes, coupled with significant disparities in care, underscores the urgent need for comprehensive and equitable approaches to diabetes prevention, early detection, and management in the country.
Causes
Causes
- Insulin resistance
- Central obesity
- Predispose individuals to insulin resistance
- Abdominal fat is especially active hormonally, secreting a group of hormones called adipokines that may possibly impair glucose tolerance
- Obesity is found in approximately 55% of patients diagnosed with type 2 diabetes
- In the last decade, type 2 diabetes has increasingly begun to affect children and adolescents, likely in connection with the increased prevalence of childhood obesity
- Positive family history
Types
Classification of Diabetes Mellitus:
Etiological Classification of Diabetes mellitus and Impaired glucose tolerance
1.Type I DM (in other words; β-cell destruction, absolute insulin deficiency).
Insulin dependent diabetes mellitus (IDDM)
(a) Autoimmune
(b) Idiopathic
2.Type II DM – Non-insulin dependent (in other words; NIDDM)
3. Maturity onset diabetes in young (in other words; MODY 1-6)
Genetic defects in β-cell function have the following
mutations:
- MODY 1 – Hepatocyte Nuclear Transcription factor (HNF) 4α
- MODY 2 – Glucokinase
- MODY 3 – HNF – 1α
- MODY 4 – Insulin promotor factor-1 (IPF1)
- MODY 5 – INF – 1β
- MODY 6 – Neurogenic differentiation1, (Neuro D1)
4.Secondary causes
a. Pancreatic disease i.e.
- Cystic fibrosis
- Trauma / pancreatopathy
- Hemochromatosis
- Pancreatitis
- Fibrocalcific pancreatic diabetes (in other words; FCPD)
- Carcinoma of pancreas
b. Endocrine disorder i.e.
- Acromegaly
- Cushing syndrome
- Glucagonoma
- Conn’s syndrome
- Pheochromocytoma
- Hyperthyroidism
c. Drug induced i.e.
- Glucocorticoids
- Diazoxide
- Thiazides
- Phenytoin
- Pentamidine
- Alpha Interferon
- Thyroid hormone
- Beta adrenergic
d. Infection i.e.
- Congenital Rubella
- Coxsackie B virus
- Cytomegalovirus
e. Insulin Receptor Defect i.e.
- Anti-insulin Receptor Antibodies [in other words; Stiffman syndrome]
- Lipoatrophic Diabetes
f. Other Genetic syndrome associated with DM i.e.
- Down’s Syndrome
- Turner’s Syndrome
- Wolframe’s syndrome
- Prader willi syndrome
- Kline filters syndrome
- Porphyria
- Myotonic Dystrophy
- Laurence-Moon-Biedl syndrome
- Friedreich’s ataxia
5.Gestational diabetes
6.Impaired glucose tolerance (Borderline diabetes)
a. Primary: Higher weight, non-higher weight
b. Secondary: All conditions mentioned under secondary DM, cirrhosis of liver, kidney failure, chronic undernutrition, hypokalaemia, stress, e. g. myocardial infarction.[1]
Risk Factors
Risk Factors
type 1 diabetes
- Family history: Having a parent, brother, or sister with type 1 diabetes.
- Age: You can get type 1 diabetes at any age, but it usually develops in children, teens, or young adults.(3)
type 2 diabetes
- Age ± 45 years
- Higher weight (BMI ≥ 25 kg/m2)
- Family history of diabetes (parents or siblings with diabetes)
- Habitual physical inactivity
- Previously identified IFG or IGT
- History of GDM or deliver of a baby >9 lbs
- Hypertension (≥ 140/90 mm Hg in adults)
- HDL cholesterol ≥35 mg/dL (0.9 mmol/L) and/or triglyceride level ≥250 mg/dL (2.82 mmol/L)
- Polycystic ovary syndrome
- History of vascular disease
Pathogenesis
Pathogenesis of Diabetes Mellitus:
Type 1 diabetes i.e. –
Due to a combination of genetic, autoimmune and environmental factors, there is destruction of pancreatic β cells.
Genetic factors i.e.–
(a) Twin studies: Among monozygotic twins, the concordance rate is 30–70%, i.e., if one twin gets DM, the chances of second twin getting are 30–70%. (b) Major Histocompatibility Complex (MHC). Genes on the short arm of chromosome 6 Encodes for Human Leucocyte Antigens (in other words; HLA). There Is a strong association with Type I DM and HLA-DRD and HLA-DR4.
Autoimmunity
leads to lymphocytic infiltration of the islets of Langerhans called insulinitis. β cells are more susceptible to destruction by cytokines like TNF-α, TNF-γ IL-1.
Autoimmune basis is also suggested by association with other autoimmune diseases like Graves’ disease, Coeliac disease, pernicious anaemia. Addison’s disease, polyglandular autoimmune syndrome I and II.
Environmental Factor
(a) Viruses: Congenital rubella, Rota virus, mumps
(b) Chemical: Nitrosourea compounds, Rodenticide,
Pentamidine are associated with increased risk.
(c) Diet: (i) Cow’s milk (bovine milk proteins) may
stimulate immune response against β cells. (ii)
Type 2 Diabetes (NIDDM)
Etiopathogeneses
Type 2 DM is disorder characterized by insulin resistance and impaired insulin secretion. Hyperglycemia develops due to (i) Peripheral resistance to action of insulin. (ii) Increased hepatic glucose output. (iii) Impaired pancreatic β- cell secretion of insulin.[1]
1.Genetic factors:
Type 2 DM has very strong genetic predisposition.
(a) Firstly, Twin studies – Concordance in monozygotic twins is 70–90%. If both parents are diabetic, their off spring has 90% chance of developing type 2 DM.
(b) Secondly, Polygenic factors – Type 2 DM is a polygenic multifactorial disease, in majority of cases. No consistent major genetic genes have yet been implicated.
(c) Thirdly, Monogenic forms are rare, e.g., Wolfram syndrome, MODY types 1-6, MELAS (e.g. mitochondrial myopathy, encephalopathy, lactic acidosis, stroke).
2.Obesity lipotoxicity, nutrition i.e.
(a) Obesity and central fat distribution. The cut offs for BMI are 23 kg/m2 and waist circumference for men at 90 cm and for women 80 cm.
(b) Lipotoxicity. Adipose tissue can secrete a large number of ‘adipokines’ which can impair insulin secretion and action by an endocrine effect, e.g. leptin or increase in insulin resistance, e.g., TNFα,
Resist in, Adiponectin (low levels contribute to Insulin resistance). Free fatty acids inhibit glucose uptake and increase hepatic glucose output
3.Nutrition i.e.:
Generous dietary intake Physical inactivity Vitamins and trace elements – Low levels of Vitamin D, zinc, copper, chromium.
4.Insulin resistance i.e.
It is a state in which a given concentration of insulin gives a subnormal biological response on patients target tissue e.g., skeletal muscle, adipose tissue and liver. There is resistance to exogenous and endogenous insulin. There are overt diabetics who do not respond to conventional and supraphysiological levels of insulin, but at the end are commonly seen in individuals with mild glucose intolerance. It is also called metabolic syndrome. Deadly quartet-CHAOS (CAD, HT, Obesity, Adult-Onset diabetes and Stroke).
5.The ‘thrifty phenotype’ hypothesis i.e.
Individuals with low birth weight appear to have higher risk of NIDDM, particularly if they become higher weight in later life. This hypothesis suggests that intra uterine malnutrition leads to defective pancreatic development. Such individuals may become susceptible to diabetes, hypertension and heart disease in later life.[1]
Pathophysiology
Pathophysiology
Diabetes mellitus is a group of metabolic disorders characterized by chronic hyperglycemia resulting from defects in insulin secretion, insulin action, or both. The two main types of diabetes mellitus are:
Type 1 Diabetes Mellitus (T1DM): Caused by autoimmune destruction of pancreatic beta cells, leading to absolute insulin deficiency. The resulting hyperglycemia is due to impaired glucose uptake by peripheral tissues and unrestrained hepatic glucose production.
Type 2 Diabetes Mellitus (T2DM): Characterized by insulin resistance in peripheral tissues and relative insulin deficiency. Initially, the pancreas compensates by increasing insulin secretion, but eventually, beta-cell function declines, exacerbating hyperglycemia.
Key Pathophysiological Mechanisms:
- Insulin Resistance: Decreased responsiveness of target tissues (muscle, liver, adipose tissue) to insulin, resulting in impaired glucose uptake and utilization.
- Beta-Cell Dysfunction: Progressive decline in the ability of pancreatic beta cells to secrete insulin in response to glucose.
- Increased Hepatic Glucose Production: Unregulated glucose production by the liver, contributing to hyperglycemia.
- Glucagon Dysregulation: Inappropriate glucagon secretion, further promoting hepatic glucose production.
- Incretin Deficiency: Reduced levels of incretin hormones (GLP-1 and GIP), which normally enhance insulin secretion and suppress glucagon release.
- Inflammation and Oxidative Stress: Chronic low-grade inflammation and oxidative stress contribute to the development and progression of both T1DM and T2DM.
Complications:
Chronic hyperglycemia can lead to microvascular complications (retinopathy, nephropathy, neuropathy) and macrovascular complications (cardiovascular disease, stroke, peripheral arterial disease).[10]
Clinical Features
Clinical Features
The clinical presentation of diabetes mellitus can vary depending on the type and severity of the disease. However, some common features include:
Type 1 Diabetes:
- Cardinal symptoms: Polyuria (excessive urination), polydipsia (excessive thirst), polyphagia (excessive hunger), and weight loss.
- Other symptoms: Fatigue, blurred vision, and recurrent infections.
- Acute complications: Diabetic ketoacidosis (DKA), a life-threatening condition characterized by severe hyperglycemia, dehydration, and metabolic acidosis.
Type 2 Diabetes:
- Asymptomatic: Many individuals with type 2 diabetes are asymptomatic initially.
- Non-specific symptoms: Fatigue, blurred vision, and recurrent infections.
- Chronic complications: Microvascular (retinopathy, nephropathy, neuropathy) and macrovascular (cardiovascular disease, stroke, peripheral arterial disease).
Gestational Diabetes:
- Usually asymptomatic: Most women with gestational diabetes do not experience symptoms.
- Screening: Routine screening is recommended for pregnant women at 24-28 weeks of gestation.
Other Clinical Features:
- Hyperglycemia: Elevated blood glucose levels.
- Glycosuria: Glucose in the urine.
- Ketonuria: Ketone bodies in the urine (more common in T1DM).
- Skin manifestations: Acanthosis nigricans (darkening of skin folds), diabetic dermopathy (skin lesions), and necrobiosis lipoidica (skin plaques).
- Foot problems: Ulcers, infections, and neuropathy.[11]
Sign & Symptoms
Sign & symptoms of Dibetes Mellitus
Onset –
Usually gradual in adults, but acute in children.
Modes of presentation –
Presence of osmotic symptoms (i.e. polyuria, polyphagia, polydipsia)
- Weight loss, fatigue and lassitude
- Pruritus vulvae in females or balanitis in males
- Loss of libido or erectile dysfunction
- Blurring of vision
- Symptoms due to diabetes – related complications e.g., abdominal pain in ketoacidosis [1]
Convulsions – Fits should be considered hypoglycaemic until proved otherwise, especially in children. EEG abnormalities are common in insulin-treated patients, especially those with recurrent hypoglycaemia. Day Time attacks suggest epilepsy, while nocturnal attacks are often hypoglycaemic.
Clinical Examination
Clinical Examination of Diabetes Mellitus
- Patients with diabetes mellitus type 2 usually have normal physical examination findings unless complications develop in these patients.
Appearance of the patient
Patients are usually well-appearing.
Vital signs
- High blood pressure with normal pulse pressure may be seen.
Skin
- Acanthosis nigricans is suggestive of insulin resistance.
- Diabetic dermopathy (DD), one of the skin findings of diabetes mellitus, appears as dull red papules which cause bilateral involvements on bony prominences. Nevertheless, involvement of pretibial region is the most common presentation, described as pigmented pretibial patches.
- The following skin disorders are reported more frequently in diabetic patients:
- Onychomycosis
- Tinea pedis
- Candidiasis
- Non-candidal intertrigo
- Eczema
- Psoriasis
HEENT
- Periorbital edema is a finding in patients with diabetic nephropathy.
Neck
- Carotid bruits may be auscultated unilaterally using the bell of the stethoscope, it is a sign suggestive of atherosclerosis.
Lungs
- Pulmonary examination of patients with Diabetes mellitus type 2 is usually normal.
Heart
- Normal findings unless complications occur which may lead to heart failure with preserved EF (HFpEF).
Abdomen
- Abdominal examination of patients with Diabetes Mellitus is usually normal.
Back
- Back examination of patients with Diabetes Mellitus is usually normal.
Genitourinary
- Genitourinary examination of patients with Diabetes Mellitus is usually normal.
Neuromuscular
- The patient is usually oriented in person, place, and time.
- Bilateral sensory loss in the upper and lower extremities may develop as neuropathy progresses.
Extremities
- Signs of pretibial myxedema or ankle edema are findings in late diabetes. (4)
Diagnosis
Criteria for diagnosis of IR (WHO)
- Central obesity (BML, WHR)
- Low Tg (>150 mg/L, high LDL)
- Low HDL (< 40-50 mg/dL)
- High BP (>130/85 mm Hg)
- FBS >100 mg/dL
Differential Diagnosis
Differential Diagnosis of Diabetes Mellitus
- Hypothyroidism
- Cushing Syndrome
- Metabolic Syndrome
- Anemia
- Type 2 Diabetes Mellitus (5)
In Pregnancy
Pregnancy and diabetes
Pregnancy predisposes to diabetes by three mechanisms.
- Antagonization of peripheral actions of insulin due
to raised levels of oestrogens, progesterone, corticosteroids, human chorionic somatomammotropin and human placental lactogen.
- Rapid insulin destruction due to high insulins activity of placenta.
- Depletion of β cell insulin reserve. Increased utilization of stored nutrients and glucose to feed the foetus leads to fasting hypoglycaemia, ketonemia and elevated free acids which leads to insulin release and ultimately depletion of beta cell insulin reserve.
Management of diabetes in pregnancy
- Diet high protein intake. Restriction of salt if oedema.
- Exercise
- Insulin therapy is essential. In first half of pregnancy requirement may be reduced due to morning sickness. Constant glucose utilization through the placenta and absence of antagonists to maternal glucose utilization. Post-partum insulin dosage must be readjusted as insulin requirements fall due to removal of placental lactogen.
- Oral hypoglycaemic agents should be avoided except metformin which is effective in women with PCOD to aid conception.[1]
Foetal monitoring in GDM for foetal anomalies
(a) USG at 18–22 weeks for malformations.
(b) Foetal echo at 20–24 wks.
(c) Serum α-fetoproteins.
(d) Chromosomal studies if required.
For foetal well-being
(a) Maternal records of foetal movements. (b) Foetal heart rate patterns (cardiotocography). (c) USG. Non-stress test, contraction. (d) Lecithin: Sphingomyelin ratio (for lungs). Renal glycosuria is a rare condition in which sugar is eliminated in urine despite a normal or low blood sugar.
This is due to improper functioning of renal tubules. When glucose in blood increases beyond 180 mg/dL, it is excreted in urine. This point is known as renal threshold for glucose (RTG).
Adverse effects of diabetes on pregnancy
- Polyhydramnios
- Pre-eclampsia, eclampsia
- Recurrent abortions
- Premature labour
- Prolonged labour
- Abnormal presentations
- UTI
- Monilial vaginitis
- Hypoglycaemia (first trimester)
- Hyperglycaemia (third trimester)
- Postpartum haemorrhage
- Puerperal sepsis
- Retinopathy
- Nephropathy
- Gastropathy
Adverse effect on foetus
- Macrosomia (large babies) because of foetus/hyper-insulinemic causing excessive fat deposition and visceromegaly.
- Prematurity.
- Post-partum hypoglycaemia from persisting insulin secretion after birth in absence of glucose supplied via placenta.
• Intra-uterine death more common after 37th week, hence early termination of pregnancy is advisable especially if she has vascular complications.[1]
Special Categories
Special Categories
- Late-onset Autoimmune Diabetes of Adults (LADA) –A variation of type 2 DM, patients have autoanti bodies such as anti-islet cell and anti-glutamic acid (GAD) antibodies. Insulin levels are low. However, they progress gradually and present in non- higher weight young adults and may respond to OHAs. Eventually they became insulin dependent.
- Maturity onset Diabetes of the Young (MODY2) is
- inherited genetic defect in β-cell glucokinase function inherited genetic defect in β-cell glucokinase function defect. Patients are detected during routine screening or during pregnancy. The hyperglycaemia is minimal. MODY 1,3,4,5,6 present in early adulthood, are symptomatic, have severe hyperglycaemia and are prone to develop complications.
- Fibro Calculous Pancreatic Diabetes (FCPD). See later.
- Brittle diabetes – Here patients have wide fluctuations in blood sugar and recurrent episodes of ketoacidosis in spite of adequate doses of insulin. It usually occurs in young females with psychiatric problems and menstrual irregularities.[1]
Diabetic Ketoacidosis
Diabetic Ketoacidosis
Is a state of acidaemia induced by excess production of ketoacids, Dehydration and hyperglycaemia are the rule, lactic acidosis may also be present.[1]
Pathophysiology –
Diabetic ketoacidosis is caused by severe insulin deficiency and is accentuated by excessive glucagon secretion. This leads to major clinical and laboratory abnormalities seen in diabetic ketoacidosis, which includes excess mobilization of free acids from adipose tissue, increased glucose production from the liver and impaired glucose uptake and utilization by muscle.
The two major effects of uncontrolled diabetes are:
- Increased glucose production which causes hyperglycaemia, osmotic diuresis, electrolyte depletion and dehydration
- Increased ketogenesis, resulting in metabolic acidosis.
Diagnosis –
The cardinal features are:
- Acidosis (arterial pH ≤ 7.3)
- Plasma anion gap (≥ 16 mmol/liter)
- Serum ketone is positive
- Serum bicarbonate ≥ 15 mmol/liter
- Hyperglycaemia (plasma glucose ≥ 11.1 mmol/liter)
Investigations:
Blood glucose, urea and electrolytes (especially potassium), full blood count and blood gases. ECG should be monitored continuously for signs of hypokalaemia.[1]
Management:
Admission
- Diagnosis suspected and confirmed immediately by blood glucose and ketone measurements
- Initial assessment of magnitude of dehydration, hyperosmolality, and acidosis
- Fluid loss measured by subtracting admission weight from last recently known stable weight
- Effective serum osmolality = 2 × [serum Na+ (mmol/liter) + serum K + (mmol/liter)] + serum glucose (mmol/liter) + urea
- Evaluate patient for sepsis and/or precipitating illness [1]
Hour 1
- Fluid administration
– If strikingly hypovolaemic with low blood pressure and relative or absolute anuria, fluid administration should be normal saline and, if necessary, colloids; rate of administration should be that necessary to restore circulatory function
– When blood pressure is normal and urine output adequate: fluid administration should be normal saline; rate of (mmol/liter)] administration 1000 mL/hour
- Initial assessment of serum potassium and kidney function.
- Insulin
– Continuous intravenous infusion of regular insulin 5–10 units/ hour or intramuscular regular insulin (20 units loading dose and 5 units/hour) Potassium
– Start intravenous potassium at 10–40 mmol/hour at initiation of insulin therapy if serum potassium is not > 5 mmol/litter and renal output is good. If patient is hyperkaliaemic, temporary delay intravenous potassium Alkali
– Sodium bicarbonate intravenously is seldom indicated, except in severe acidosis (pH < 7.0) with incipient circulatory collapse Dose, if given, is 50–100 mmol/litter sodium bicarbonate given in 0.45% saline over 30–60 minutes. Additional K + must be given with bicarbonate therapy
Hour 2
- Fluid administration
- Continue normal saline at 500 mL/hour. Maintain calculated plasma osmolality > 285 mOsmol/liter throughout the first 12 hours. If serum Na + >150 mmol/liter switch to 0.45% saline
- Insulin
- Check blood glucose and adjust insulin dose to maintain a fall of about 5 mmol/litre/hour. Do not allow blood glucose to fall below 11.1–14.0 mmol/litre. Anion gap should be decreasing and blood pH increasing
- Potassium
- Maintain serum potassium at 4.0–5.0 mmol/litre by continued addition of potassium to intravenous fluids[1]
Hours 3-4
Continue as for hour 2
Observe for cognitive or neurological symptoms and continue to do so for 12 hours
Hours 5-8
- Fluid administration
– Normal saline 250 mL/hour. When blood glucose reaches 11.1–14.0 mmol/liter, change intravenous fluid to 500 mL/ hour normal saline with 5% glucose
- Insulin
– Continue insulin at maintenance dose until ketoacidosis has cleared (blood pH > 7.35, serum ketones negative)
- Potassium
– Continue at 10–40 mmol/hour until ketoacidosis has cleared
- Phosphate
– Consider phosphate replacement at 6 hours if serum phosphate is < 2.0 mg/dL
Hours 8-24
- Fluid administration
– Continue intravenous repletion with 0.45% saline with or without 2.5% or 5.0% glucose as needed
- Insulin
– After ketoacidosis has cleared (blood pH > 7.35, serum ketones negative) switch to subcutaneous insulin and then stop intravenous or intramuscular insulin.
Complications of DKA
Iatrogenic complications
Osmotic and volume disturbances–
Administration of insulin without sufficient fluids causes shift of water from extracellular space; further shrinking of extracellular fluid volume impairs blood flow to critical vascular beds, or precipitates vascular collapse. Similarly, insufficient saline administration may also result in hypotension.
Potassium disturbances –
Premature (before insulin has begun to act) and inappropriate potassium administration may cause fatal hyperkalaemia (cardiotoxicity) in early course of management. Glucose, insulin, and volume expansion with normal saline are potential modalities for lowering serum potassium; hence failure to administer potassium in latter stages may cause fatal hypokalaemia in potassium depleted patient.[1]
Hypoglycaemia and reappearance of ketosis –
During therapy of DKA, normalization of blood glucose usually achieve sooner than reversal of ketoacidosis state. Because insulin therapy must continue, hypoglycaemia develops unless glucose is given.
Fingerstick glucose measurements should done hourly for 4h, 2 hourlies for next 4h, and 4 hourlies till pt. improves. Glucose generally falls at rate of 50–100 mg/ dL/h. Failure to maintain glucose and insulin treatment until ketones have clear and depleted glycogen stores restored, results in recurrence of ketosis
Cerebral oedema –
It may rarely occur in children but is even rarer in adults. The condition should suspect when a pt. with ketoacidosis begins to deteriorate 3 to 10 hours into treatment with increasing stupor or coma coupled with signs of raised intracranial pressure; an unexpected fever may also an early sign. Osmotic disequilibrium between intracellular and extracellular fluids probably plays a role. Tr. – Mannitol 20% iv 1.5–2 mL/kg body wt. over 15 minutes and dexamethasone 10 mg iv followed by 4mg in q6h. Clinical response will seen in 12–24 h.
Hypocalcaemia –
It may develop during phosphate replacement.[1]
Non-iatrogenic complications
Infection –
Although leucocytosis may occur in DKA in absence of infection, fever generally indicates infection and demands careful search for pneumonia, pyelonephritis and septicaemia. A Rare ketoacidosis-associated infection is mucormycosis of paranasal sinuses with facial pain, bloody nasal discharge, orbital swelling, blurred vision and impaired consciousness. Tr. – Broad spectrum antibiotics. Blood, Urine and throat cultures should be taken prior to giving antibiotic.
Vascular thrombosis –
Combination of volume contraction, low cardiac output, increased blood viscosity, underlying atherosclerosis, direct endothelial damage due to hyperosmolar milieu, and changes in clotting factors and platelet function predispose to thrombosis.
Respiratory distress syndrome i.e.–
Hypoxia and ARDS may develop in course of therapy of DKA hyperosmolar coma. Additionally, Clinical picture is characterized by unexplained hypoxaemia and dyspnoea in absence of any underlying pulmonary/cardiac disease.
Pancreatitis i.e.–
Acute abdominal pain is a common presentation of DKA, and resolves rapidly on therapy. specific aetiologies can be gastroparesis, ischaemic bowel, and cholecystitis. Raised serum amylase is observed in 80% of cases. It may represent pancreatic damage (in other words; hypertonicity and hyper perfusion); in some instances, it is subclinical.
Myocardial infarction i.e.–
can precipitate or complicate DKA, it is a major cause of morbidity.
Hyperlipidaemia –
Severe hypertriglyceridemia (triglycerides > 1000 mg/dl) is seen in about 10% which on follow-up resolve in 70% of cases. The abnormality is related to acute metabolic changes in DKA.[1]
Complications
Complications of Diabetes Mellitus
- Metabolic Complications
- Diabetic Ketoacidosis.
- Hyperosmolar Hyperglycaemic State
- Hypoglycaemic Coma
- Diabetic Retinopathy
- Diabetic Nephropathy
- Pregnancy also Proteinuria in Diabetes
- Diabetic Foot
Investigations
Investigation of Diabetes Mellitus
Blood glucose estimation
In non-diabetes, blood glucose levels are 70-100 mg/dl.
(a) Firstly, Random blood glucose is done at any time in the day, irrespective of meals. If <140 mg normal, >200 mg indicates DM and between 140–200 mg, GTT is required.
(b) Secondly, Fasting blood glucose is measured after 12 hr fast. Normal <100 mg, diabetes if >126 mg and impaired fasting glucose 101–125 mg (pre-diabetics).
(c) Thirdly, Post-prandial blood glucose is measured 2 hr after a meal. Normal <140 mg, Diabetes >200 mg Impaired glucose tolerance 140–199 mg.
Oral Glucose tolerance test (in other words; OGTT)
Pre diabetes also known as impaired glucose tolerance is a condition with no symptoms. But this patient develops more serious DM. Hence individuals with family history DM 2, Women with gestational diabetes or had a baby weighing >9 pounds, the higher weight with much belly fat and older people should go under the test. In OGTT the first sample taken overnight fast of 8 hrs following which patient is given glucose 1 g/kg body wt. Blood is then collected at 30, 60, 120, 180 minutes. In diminished Glucose tolerance, a level of blood glucose is raised at 180 minutes.
Factor affecting GTT i.e.
- Age – GTT decreases in patient > 60 years of age
- Obesity
- Surgery – Due to stress of surgery, there is increase in cortisol and catecholamine secretion.
- Drugs – For example; Thiazides, phenytoin, oral contraceptives, thyroxine, corticosteroids.
Urine glucose –
In brief, Normally about 100 mg/d is excreted and can be estimated by tests for reducing sugar e.g. Benedict’s tests or clinistix method. Those measurements are now not recommended.
3.Glycosylated haemoglobin (GHb)
In general, It is used to measure long-term glycaemic control. Hb in the blood is glycated by sugar. In detail, Glucose combined with protein residues on Hb chain by slow ‘Non-enzymatic’ Glycation. This results in formation of Haemoglobin A1c proportionate to amount of blood glucose. Since life span of RBCs is 21 days, HbA1c will reflects blood glucose level over past 2-3 months.
Advantages – No relation to meals, physical activity, crash diets or modes of therapy.
Disadvantages –
(a) Firstly; Cannot be used to change daily diseases of drugs or insulin.
(b) Secondly; Values are unreliable in haemolytic anaemia and haemoglobinopathies because of reduced life span of RBCs.
(c) Thirdly; In iron deficiency anaemia, values are higher, lower values in pregnancy, Vitamin C, E deficiency.
Self-monitoring of Blood Glucose
- Type I diabetes 4–6 times a day depending on the insulin regimens.
- Type II diabetics on oral hypoglycaemic drugs need to monitor 1-2 times/d
- During pregnancy more frequent monitoring.
- During acute complications or illness 2-hourly.
Microalbumin. Pts with microalbuminuria have a greater risk of developing kidney failure, also cardiovascular damage. Furthermore; Reference is 0-1.7 mg/dl in spot random sample, up to 20 mg/L in 24 hr urine volume.
Urine protein/creatinine ratio gives information about proteinuria in pts with diabetic nephropathy.
Higher the ratio, greater the damage.
Serum creatinine.
In diabetics with nephropathy a doubling of creatinine suggests a 50% reduction in GFR. Presence of the antibody – (a) Is a strong predictive marker for onset of type 1 DM. (b) Helps differentiate between Type 1 and Type 2 diabetes. (c) Aids in prediction, diagnosis also management of DM. (d) Indicates need for progression to insulin therapy in Type 2DM. (e) To determine the cause of hypoglycaemia. (f) To monitor recovery after removal of an insulin producing tumour of the pancreas. Early detection of IDDM – Some of the markers that we can predict the development are given in.
Insulin levels.
Elevated blood glucose levels with low insulin levels indicate insufficient insulin for adequate control of blood glucose. Similarly, high insulin levels with low blood glucose indicate a change in dosage of drugs.
C-peptide
It is used to monitor beta cell activity and capability over time and help in deciding when to start insulin therapy. C-peptide in conjunction with insulin and glucose levels can be used to diagnose cause of hypoglycaemia and monitor its treatment.
Insulin antibody test–
Quantitative determination of antibodies against insulin in serum.
GAD-65 antibody
It is an enzyme produced primarily by pancreatic islet cells. GAD-65 antibodies are common in newly diagnosed diabetic patients also often appear years before clinical onset of the disease.
Presence of the antibody – (a) Is a strong predictive marker for onset of type 1 DM. (b) Helps differentiate between Type 1 and Type 2 diabetes. (c) Aids in prediction, diagnosis and management of DM. (d) Indicates need for progression to insulin therapy in Type 2 DM. (e) To determine the cause of hypoglycaemia. (f) To monitor recovery after removal of an insulin producing tumour of the pancreas.
Treatment
Treatment of Diabetes Mellitus
Total calories requirements are determined by the patient’s activity
Higher weight person NIDDM should ne encourage to establish within their weight within a desirable range. A reduction of approximately 500 kcal/day can result in loss of 1–2 kg/month.
Carbohydrates i.e.–
should comprise 55–60% of the calories, With the form and amount to determine by individual eating habits also blood glucose and lipid responses. Unrefined carbohydrates should substitute by refined carbohydrates to the extent possible
Proteins i.e. –
In brief, Recommended dietary allowance of 0.85 g/kg body weight for adult is an appropriate guide. If kidney dysfunction, reduce intake to 0.6 g/kg.
Fat i.e.–
should comprise ≤ 30% of total calories and all components should reduce proportionately. Replacement of saturated with polyunsaturated fat is desirable to reduce cardiovascular risk. Cholesterol intake should < 300 mg/day.
Fibre i.e.–
Increased consumption of dietary fibre especially soluble fibre associate with lower levels of blood glucose and serum lipids. The Water insoluble fibres such as cellulose, lignin and most hemicelluloses found in whole grain breads, cereals and wheat bran affect gastrointestinal transit time and faecal bulk with little impact on plasma glucose. However highly viscous water-soluble fibres such as pectins, gums and storage polysaccharide found in fruits, legumes, lentils roots, tubers, oat and oatbran, when eaten in purified form, reduce serum levels of glucose and insulin. Ideal recommended amount of fibre in patient’s diet is 35–40 g/day.
Alternative sweeteners i.e. –
Both nutritive and non-nutritive sweeteners are acceptable in diabetes management.[1]
Sodium –
Should restrict to 1000 mg/1000 kcal, not to exceed 3000 mg/d to minimize symptoms of hypertension.
Alcohol –
in moderation and may need to restrict entirely by person with diabetes and insulin-induced hypoglycaemia, neuropathy, poor control of glucose and lipids, or obesity. Vitamins, minerals and antioxidants – intake should encourage.
- Forbidden foods – e.g. Sugar, jam, jellies, honey, jaggery, tinned fruits and juices, sweets, chocolate, ice creams, pastries, glucose drinks, foods made with sugar, pudding, sauces.
(b) Foods allowed in moderation – e.g. Bread of all kinds and chapattis made from wheat or millets, plain biscuits, all fresh fruits, baked beans, breakfast cereals.
(c) Free foods – e.g. All meat, fish, eggs (not fried), clear soup or meat extracts; tea or coffee; vegetables such as cabbage, cauliflower, spinach, pumpkin, brinjal, lady’s finger, turnip, French beans, cucumber, lettuce, tomato, spring onions, radish, asparagus. Spices, salt, pepper and mustard; butter and margarine. Sugar Substitutes For sweetening.
Exercise
Medical evaluation prior to formulating exercise programme, History and physical examination i.e.
- Review of diet and medication
- Fundoscopy
- Foot evaluation
Neurological evaluation –
(a) Firstly, Sensory/motor.
(b) Secondly, Autonomic
- Cardiovascular risk-factor profile
- Stress test assessment of glucose control
Exercise prescription
Type must adjust to patient’s preference and existing medical condition. Aerobic exercise is preferred (e.g. swimming, cycling, walking, running). Addition of moderate resistance should be considered.
Duration – 20–45 mins. per session
Frequency 3-4 sessions per week is required to observe beneficial metabolic effect. 4-5 session per week for weight reduction.
Potential benefits of exercises i.e.
- Maintenance of desirable body weight
- Improved sense of wellbeing also enhanced social interactions
- Enhanced insulin sensitivity
- Improved glucose control
- Decreases triglycerides also increases HDL-cholesterol levels
- Improved fibrinolysis
- Improved cardiac performance
Potential risks of exercises
- Cardiovascular – Either, Myocardial ischaemia or infarction, dysrhythmias. Hypertensive response to exercise.
- Microvascular – For Example; Retinal haemorrhage, proteinuria, accelerated microvascular disease.
- Metabolic – For Example; Hypoglycaemia, hyperglycaemia, ketosis.
- General – For Example; Muscle strains/sprains, foot injury, joint injury, degenerative arthritis, poor dietary compliance.
ADA recommends 150 min/week (distributed over at least 3 days) of moderate aerobic physical activity with no gaps longer than 2 days.
Intensity – Patient’s maximal pulse rate estimate by subtracting patient’s age from 220. Patient can start at 40 to 50% of their maximal pulse rate with gradual increments to 60–70% over 6–8 weeks.
Programme
- Stretching (5–10 mins)
- Warm up (5–10 mins)
- Exercise (20–45 mins)
- Warm down (10 mins at 30% of full exercise intensity) Exercise should be avoided when plasma glucose concentration is > 250 to 300 mg/dL and/or presence of ketones in urine.[1]
Oral Antidiabetic Drugs (OADs)
[1] Insulin Secretagogues.
Sulphonylureas
[2] Insulin Sensitizers
Biguanides: Metformin
[3] Thiazolidinediones
[4] Alpha-glucosidase Inhibitors
[5] Sodium-Glucose Co-Transporter 2 Inhibitors (in other words; SLGT2)
[6] Insulin
Prevention
Prevention of Diabetes Mellitus
- Losing weight and keeping it off: Weight control is an important part of diabetes prevention. You may be able to prevent or delay diabetes by losing 5 to 10% of your current weight. For example, if you weigh 200 pounds, your goal would be to lose between 10 to 20 pounds. And once you lose the weight, it is important that you don’t gain it back.
- Following a healthy eating plan: It is important to reduce the amount of calories you eat and drink each day, so you can lose weight and keep it off. To do that, your diet should include smaller portions and less fat and sugar. You should also eat a variety of foods from each food group, including plenty of whole grains, fruits, and vegetables. It’s also a good idea to limit red meat and avoid processed meats.
- Get regular exercise: Exercise has many health benefits, including helping you to lose weight and lower your blood sugar levels. These both lower your risk of type 2 diabetes. Try to get at least 30 minutes of physical activity 5 days a week. If you have not been active, talk with your health care professional to figure out which types of exercise are best for you. You can start slowly and work up to your goal.
- Don’t smoke: Smoking can contribute to insulin resistance, which can lead to type 2 diabetes. If you already smoke, try to quit.(6)
Homeopathic Treatment
Homeopathic Treatment of Diabetes Mellitus
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Diabetes Mellitus:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
Uranium nitrate. [Uran] |
This remedy is praised highly by Hughes also others in diabetes originating in dyspepsia. It has polyuria, polydypsia, dryness of the mouth and skin. Additionally, It causes sugar in the urine. Dr. Laning said that no remedy gives such universally good results; it lessens the sugar and quantity of the urine; he recommended the 3X trituration. Besides this; It is when the disease is due to assimilative derangements that Uranium is the remedy, and symptoms e.g. defective digestion, languor, debility and much sugar in the urine, enormous appetite and thirst, yet the patient continues to emaciate.[2] Syzygium jambolanumIt is a remedy capable of diminishing the amount of sugar in the urine, especially when used in the tincture also lower trituration, and some cases have reported cured, but it cannot consider a reliable drug, and its use seems entirely palliative. [2] |
Phosphoric acid [Phos]
corresponds to diabetes of nervous origin; the urine is increased, perhaps milky in color and containing much sugar. In detail; It suits cases due to grief, worriment and anxiety, those who are indifferent and apathetic, poor in mental and physical force. It is unquestionably curative of diabetes mellitus in the early stages, great debility and bruised feeling in the muscles. Moreover, There will be loss of appetite, sometimes unquenchable thirst and perhaps the patient will be troubled with boils.
Besides this, When patients pass large quantities of pale colorless urine or where there is much phosphatic deposit in the urine it is the remedy. It thus may be a remedy in the form known as diabetes insipidus. Hering considered Plumbum one of the most important remedies in diabetes mellitus. Causticum, Scilla also Strophanthus may be of use in diabetes insipidus. All in all, Lycopodium cured a case in a weary, wretched patient; emaciated, increased appetite also great thirst; pale, profuse urine. Eight quarts in 24 hours.
Phosphorus. [Phos]
Useful in diabetes also pancreatic diseases, especially in those of a either tuberculous or gouty diathesis. The pancreatic involvement will call attention to Phosphorus. Natrum sulphuricum corresponds to the hydrogenoid constitution, with dry mouth also throat, and Arsenicum should be studied in diabetic gangrene, thirst and emaciation. Besides this; Sudden and extreme dryness of the mouth and marked physical restlessness are also guiding symptoms to this remedy, especially with a dark watery stool. Dr. P.Jousset reports positive success where the mouth is dry; frequent, abundant urination and tendency to skin eruption.[2]
Lactic acid. [Lact]
Generally, An exceedingly good remedy in the gastrohepatic variety of diabetes and good results often follow its use. It has a fine clinical record. Furthermore, The symptoms are: urinates copiously and freely, urine light yellow also saccharine, thirst, nausea, debility, voracious appetite also costive bowels. Dry skin, dry tongue, gastralgia. Acetic acid also a valuable diabetic remedy, and it has passing of large quantities of pale urine, intense thirst, hot, dry skin and marked debility Carbolic acid may also found useful.[2]
Bryonia. [Bry]
Should not neglected in this disease. In brief, No remedy has dryness of the lips as a symptom of hepatic disorder more marked than Bryonia, also this is often one of the first symptom of diabetes. There is a persistent bitter taste, the patient is languid, morose also dispirited, thirst may not extreme nor the appetite voracious, the patient may lose strength through inability to eat. Podophyllum has a bitter taste, but the tongue is flabby. It may of use in the disease.
Chionanthus a remedy use by the Eclectic School upon the indications of thirst, frequent also copious urine; constipation with stools light colored, devoid of bile. Functional liver disorders. Argentum metallicum. Hahnemann suggests the use of this remedy especially, in diuresis, it decide use in diabetes insipidus. The urine is profuse, turbid also of sweet odor. Micturition is frequent and copious. Natrum sulphuricum. Hinsdale reports good results with this remedy. It has polyuria, intense itching of the skin, especially upon the upper surface of the thighs. Lastly, It is the Tissue Remedy of diabetes.
Insulin. [Insulin]
Long before the discovery of Insulin Dr.Pierre Jousset of Paris prepared a pancreatic juice on a glycerine basis which he administered to diabetic patients in doses of 10 or 20 drops a day in water also had results sufficiently good to consider pancreatic juice, orally administered, as a remedy of great value in diabetes. Dr. Cartier, his practical successor, praised it insisted on smaller doses given by mouth as larger doses and hypodermic injections of it had no effect in ordinary diabetes.
Baker advises the homoeopathic strengths of Insulin 3d to 30th and reports happy results therefrom. Additionally, Great care must be taken not to overdose. Boericke says that it maintains the blood sugar at a normal level and the urine remains free of sugar. Lastly, Epileptic convulsions also mental derangements have been produced by hypodermic use of this hormone.[2]
Diet & Regimen
Diet & Regimen
- Restoration of normal blood glucose and optimal lipid levels.
- Maintenance of blood glucose level as near to physiologic levels to prevent onset or progression of complications.
- Maintenance of normal growth rate in children and adolescents as well as attainment and maintenance of reasonable body weight in adolescents and adults.
- Provision of adequate nutrition for pregnant women, the fetus and during lactation.
- Moreover, Consistency in timing of meals and snacks to prevent inordinate swings in blood glucose levels.
- Motivation to have small frequent meals.
- Determination of a meal plan appropriate for individual’s lifestyle and based on dietary history to have good compliance.
- Besides this, Management of weight reduction for higher weight person individuals with NIDDM.
- Improvement in the overall health of patients with diabetes through optimal nutrition carbohydrates to the extent possible.[1]
Do’s and Don'ts
The Do’s & Don’ts
Diabetes Mellitus Do’s & Don’ts
Do’s:
- Do monitor your blood glucose levels regularly as advised by your healthcare provider.
- Do follow a healthy, balanced eating plan with regular meals and snacks.
- Do engage in regular physical activity, aiming for at least 150 minutes of moderate-intensity exercise per week.
- Do take your prescribed medications as directed by your healthcare provider.
- Do maintain a healthy weight.
- Do get regular checkups and screenings for diabetes-related complications.
- Do educate yourself about diabetes and its management.
- Do seek support from healthcare professionals, diabetes educators, and support groups.
Don’ts:
- Don’t skip meals or snacks, as this can lead to hypoglycemia (low blood sugar).
- Don’t overeat or consume excessive amounts of sugary drinks or foods high in saturated and trans fats.
- Don’t smoke or use tobacco products, as these increase the risk of diabetes complications.
- Don’t drink alcohol excessively. If you choose to drink, do so in moderation and with meals.
- Don’t ignore signs or symptoms of hypoglycemia or hyperglycemia (high blood sugar).
- Don’t neglect foot care. Inspect your feet daily and wear comfortable, well-fitting shoes.
- Don’t hesitate to ask for help or support if you’re struggling with managing your diabetes.
Please refer to Diabetes For Dummies (3rd Edition) for detailed information and guidance on managing diabetes.[12]
Terminology
Terminology
Hyperglycemia
High blood glucose levels, a key feature of diabetes.
Insulin Resistance Reduced responsiveness of body cells to insulin, leading to impaired glucose uptake and utilization.
Polyuria
Excessive urination, a common symptom of diabetes due to high blood sugar levels.
Polydipsia
Excessive thirst, another common symptom of diabetes caused by dehydration resulting from increased urination.
Acanthosis nigricans
Darkening and thickening of the skin in areas like the neck, armpits, and groin, often associated with insulin resistance.
Polyphagia
Excessive hunger, often experienced by people with diabetes due to the body’s inability to use glucose for energy effectively.
Diabetic Neuropathy
Nerve damage caused by diabetes, leading to numbness, tingling, pain, and weakness in the hands, feet, and other parts of the body.
DKA
A serious complication of diabetes, mainly type 1, characterized by the buildup of ketones in the blood due to a lack of insulin.
Diabetic Retinopathy
Damage to the blood vessels in the retina (the light-sensitive tissue at the back of the eye) caused by diabetes, which can lead to blindness.
Diabetic Nephropathy
Kidney damage caused by diabetes, which can lead to kidney failure.
References
References
- Text book of medicine by Golwala
- Therapeutics from Zomeo ultimate LAN
- Diabetes Risk Factors | CDC
- Diabetes mellitus type 2 physical examination – wikidoc
- Differential Diagnosis | Type 1 Diabetes Mellitus (osu.edu)
- How to Prevent Diabetes: MedlinePlus
- The India Diabetes (ICMR-INDIAB) study: prevalence of diabetes and prediabetes in 15 states of India in 2021 (The Lancet, 2023).
- Socioeconomic inequality in awareness, treatment and control of diabetes among adults in India: Evidence from National Family Health Survey of India (NFHS), 2019–2021 (Scientific Reports, 2023).
- Epidemiology of type 2 diabetes in India (PubMed, 2021).
- Harrison’s Principles of Internal Medicine (21st edition, 2022) by Dennis L. Kasper, Anthony S. Fauci, Stephen L. Hauser, Dan L. Longo, J. Larry Jameson, and Joseph Loscalzo, published by McGraw Hill.
- Davidson’s Principles and Practice of Medicine (24th edition, 2022) by Brian R Walker, Nicki R Colledge, Stuart H Ralston, Ian D Penman, published by Elsevier.
- Diabetes For Dummies (3rd Edition, 2021) by Alan L. Rubin, M.D., published by Wiley.
Also Search As
Also Search As
People can search for this article on homeopathy and diabetes mellitus using the following search terms and phrases:
General Search Terms:
- homeopathy for diabetes
- homeopathic treatment for diabetes
- natural remedies for diabetes
- complementary medicine for diabetes
- holistic approach to diabetes
Specific Search Terms:
- homeopathic remedies for diabetes
- Syzygium jambolanum for diabetes
- Uranium nitricum for diabetes
- Cephalandra indica for diabetes
- homeopathic treatment for high blood sugar
- homeopathy for diabetes complications
Long-Tail Keywords:
- can homeopathy cure diabetes?
- is homeopathy safe for diabetes?
- how does homeopathy help with diabetes?
- best homeopathic remedies for diabetes
- homeopathic doctor for diabetes
Additional Tips:
- Include these keywords in the title, meta description, and throughout the article content.
- Use relevant hashtags on social media when sharing the article.
- Submit the article to homeopathic directories and websites.
- Engage in online forums and discussions about homeopathy and diabetes.
By incorporating these search terms and strategies, you can increase the visibility of your article and make it easier for people to find information on homeopathy for diabetes mellitus.
People can find information about the homeopathic treatment of diabetes mellitus through several search methods:
Search Engines:
- Use specific keywords and phrases related to homeopathy and diabetes (e.g., "homeopathy for diabetes," "homeopathic remedies for diabetes," "homeopathic treatment for high blood sugar").
- Try using long-tail keywords that are more specific (e.g., "best homeopathic remedies for diabetes," "homeopathic doctor for diabetes").
- Consider using different search engines like Google, DuckDuckGo, or Bing to get a variety of results.
Online Forums and Communities:
- Participate in online forums and discussions about homeopathy and diabetes.
- Ask questions and share experiences with other people who are interested in or using homeopathic treatments for diabetes.
- Look for recommendations from other users about reputable homeopathic practitioners or resources.
Homeopathic Websites and Directories:
- Explore websites of homeopathic organizations and clinics that specialize in treating diabetes.
- Search online directories of homeopathic practitioners to find qualified professionals in your area.
- Look for articles and resources on homeopathic websites that discuss the treatment of diabetes.
Social Media:
- Follow homeopathic organizations, practitioners, and groups on social media platforms like Facebook, Twitter, or Instagram.
- Search for relevant hashtags like #homeopathy, #diabetes, #naturalremedies, and #holistichealth.
- Engage with others in discussions about homeopathy and diabetes.
Academic Research Databases:
- If you are interested in scientific research on homeopathy and diabetes, you can search academic databases like PubMed, ResearchGate, or Google Scholar.
- Look for clinical trials, case studies, and review articles on the use of homeopathy for diabetes management.
By utilizing these different search methods, you can find a wealth of information on the homeopathic approach to diabetes mellitus, including articles, research studies, practitioner recommendations, and personal experiences from other people with diabetes.
Frequently Asked Questions (FAQ)
What is Diabetes Mellitus?
Definitions
Diabetes mellitus is a group of metabolic diseases characterized by hyperglycaemia resulting from defects in insulin secretion, insulin action or both.
What causes Diabetes Mellitus?
- β-cell destruction, absolute insulin deficiency
- Mutations: Glucokinase, HNF – 1α, Insulin promotor factor-1
- Pancreatic disease
- Endocrine disorder
- Drug induced
- Infection
- Insulin Receptor Defect
- Down’s Syndrome
- Turner’s Syndrome
What are the types of Diabetes Mellitus?
Types
- Type I DM
- Type II DM
- Maturity onset diabetes in young
- Secondary causes
- Gestational diabetes
- Impaired glucose tolerance
Can homeopathy cure diabetes mellitus?
Homeopathy aims to stimulate the body’s self-healing abilities and address the underlying imbalances that contribute to diabetes. While it does not claim to cure diabetes, it can be a complementary approach to conventional treatment, potentially helping manage symptoms and improve overall well-being.
What are the symptoms of Diabetes Mellitus?
- Polyuria, Polyphagia, also Polydipsia
- Weight loss, fatigue and lassitude
- Pruritus vulvae in females
- Balanitis in males
- Either Loss of libido or erectile dysfunction
- Blurring of vision
- Abdominal pain in ketoacidosis
How does homeopathy help in managing diabetes?
It focuses on addressing the underlying imbalances and improving the body’s ability to regulate blood sugar levels, potentially reducing complications and improving quality of life.
Is it safe to use homeopathy alongside conventional diabetes treatment?
Generally, yes. However, it is crucial to inform your doctor about any homeopathic remedies you are taking to avoid potential interactions.
Can homeopathy help prevent diabetes complications?
By improving overall health and blood sugar control, homeopathy may contribute to reducing the risk of diabetes-related complications.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Diabetes Mellitus?
Homeopathic Medicines for Diabetes Mellitus
- Uranium nitrate
- Syzygium jambolanum
- Phosphoric acid
- Phosphorus
- Lactic acid
- Bryonia