Idiopathic Thrombocytopenic Purpura
Definition
Idiopathic thrombocytopenic purpura or immune thrombocytopenia also known as Immune thrombocytopenic purpura (ITP), is a type of thrombocytopenic purpura defined as an isolated low platelet count with a normal bone marrow in the absence of other causes of low platelets. Additionally, It causes a characteristic red or purple bruise-like rash and an increased tendency to bleed.[1]
Idiopathic thrombocytopenic purpura (ITP) actually has a preferred synonym that is more widely used in the medical community:
- Immune thrombocytopenic purpura (ITP): This term reflects the current understanding of the condition as an autoimmune disorder affecting platelets.
While "idiopathic thrombocytopenic purpura" is still technically correct, it means "unknown cause" for the low platelet count. Since the cause is now understood to be immune-related, "immune thrombocytopenic purpura" is the more accurate and up-to-date term.
Here’s a quick breakdown:
- Best choice: Immune thrombocytopenic purpura (ITP)
- Technically correct but outdated: Idiopathic thrombocytopenic purpura
Less common synonyms to avoid:
- Werlhof’s disease: This is a historical term for ITP, less commonly used today.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Idiopathic Thrombocytopenic Purpura (ITP)
Generally, Two distinct clinical syndromes manifest as an acute condition in children and a chronic condition in adults. Additionally, the acute form often follows an infection and spontaneously resolves within two months. In detail, Chronic immune thrombocytopenia persists longer than six months with a specific cause being unknown.
Furthermore, ITP is an autoimmune disease with antibodies detectable against several platelet surface structures.
Besides this, ITP is diagnosed by identifying a low platelet count on a complete blood count (a common blood test). However, since the diagnosis depends on the exclusion of other causes of a low platelet count, additional investigations (such as a bone marrow biopsy) may be necessary in some cases. [1]
Epidemiology
Epidemiology
The prevalence of adult ITP in India is 9.5/100,000 population. (Shilpa Kalal and K Suresh. “Immune Thrombocytopenic Purpura – A Recurrent Case in a Young Lady". Acta Scientific Women’s Health 3.6 (2021): 135-138.) [3]
Causes
Causes of Idiopathic Thrombocytopenic Purpura (IDP)
- Decreased platelet production Hypoplasia of megakaryocytes i.e.
- Chlorothiazide, also ethanol
- A megakaryocytic thrombocytopenia
- Increased platelet destruction
- Idiopathic Immune thrombocytopenia ITP
- Secondary
(i)Immune mechanisms i.e.
- Collagen vascular disease
- Lymphoproliferative disorders
- SLE
- Drug-induced Diclofenac Isoniazid Digoxin Quinine Tamoxifen Gold salts Heparin Glibenclamide
(ii)non-immune mechanisms i.e.
- DIC
- Acute leukaemia
- TIP
- Myelosuppressive drugs
- Aplastic anaemia
- Cyclophosphamide, also busulphan, etc.
(iii)Abnormal pooling of platelets i.e.
- Splenomegaly, congestive, also neoplastic
(iv)Other causes
- Hepatitis
- Malignancy
- Pregnancy
- HIV infection
- Infectious mononucleosis
- Parvovirus
Types
Classification of Idiopathic Thrombocytopenic Purpura (ITP)
- Acute thrombocytopenia
- Chronic ITP
Risk Factors
Risk factors
- Age and Sex: ITP is more common in young women.
- Autoimmune Diseases: Individuals with other autoimmune disorders like systemic lupus erythematosus (SLE) or rheumatoid arthritis are at increased risk.
- Infections: Some viral or bacterial infections can trigger ITP.
- Medications: Certain drugs, such as quinine, heparin, and sulfonamides, can cause drug-induced thrombocytopenia, a condition that mimics ITP.
- Other Factors: Although less common, factors like pregnancy, vaccinations, and underlying malignancies like lymphoma can also be associated with ITP.
Please note that this is not an exhaustive list, and individual risk profiles can vary.[4]
Pathogenesis
Pathogenesis
The pathogenesis of ITP involves a complex interplay of immune dysregulation, leading to both increased platelet destruction and impaired platelet production.
Key Mechanisms:
Autoantibody Production:
ITP is primarily characterized by the production of autoantibodies, usually IgG, that target platelet surface glycoproteins like GPIIb/IIIa or GPIb/IX. These autoantibodies opsonize platelets, marking them for destruction.
Platelet Destruction:
Opsonized platelets are recognized and phagocytosed by macrophages in the reticuloendothelial system, particularly in the spleen and liver. This accelerated clearance significantly reduces the circulating platelet count.
Impaired Platelet Production:
While increased destruction is the primary mechanism, ITP can also involve impaired platelet production. Autoreactive T cells can directly inhibit megakaryocyte maturation and platelet release from the bone marrow.
T-Cell Dysregulation:
There is evidence of T-cell dysregulation in ITP, with an imbalance between effector and regulatory T-cell subsets. This contributes to the breakdown of immune tolerance and perpetuates the autoimmune response.
Other Factors:
Additional factors like impaired clearance of immune complexes, complement activation, and cytokine dysregulation may also play a role in the pathogenesis of ITP.
Please note that the exact triggers for the development of autoimmunity in ITP are not fully understood, and the pathogenesis can vary between individuals.[5]
Pathophysiology
Pathophysiology
The pathophysiology of ITP involves a multifactorial process that includes both increased platelet destruction and impaired platelet production.
Key Mechanisms:
- Autoantibody Production: In ITP, the immune system mistakenly produces autoantibodies, primarily IgG, directed against platelet surface antigens. These antibodies bind to the platelets, marking them for destruction.
- Platelet Destruction: Antibody-coated platelets are recognized and destroyed by phagocytic cells in the spleen and liver, leading to a reduced platelet count. The spleen plays a major role in platelet destruction in ITP.
- Impaired Platelet Production: In addition to increased destruction, ITP can also involve impaired platelet production in the bone marrow. Autoreactive T cells can suppress megakaryocyte maturation and platelet release.
- Immune Dysregulation: ITP is associated with dysregulation of the immune system, including imbalances in T-cell subsets, cytokine production, and impaired regulatory mechanisms. This contributes to the breakdown of immune tolerance and perpetuation of the autoimmune response.
Additional Factors:
- Infection and Inflammation: Viral or bacterial infections may trigger or exacerbate ITP in some cases, possibly through molecular mimicry or bystander activation of the immune system.
- Genetic Predisposition: There may be a genetic predisposition to ITP, with certain individuals having a higher risk of developing the disorder due to variations in immune response genes.
Please note that the exact triggers and mechanisms underlying the development of ITP are still not fully understood, and the pathophysiology can vary between individuals.[6]
Clinical Features
Clinical Features
The clinical features of ITP can range from asymptomatic to life-threatening bleeding, depending on the severity of thrombocytopenia.
Common Clinical Features:
- Mucocutaneous Bleeding: This is the most common presentation, characterized by easy bruising (ecchymosis), petechiae (pinpoint hemorrhages), purpura (larger areas of bruising), and mucosal bleeding (e.g., nosebleeds, bleeding gums, heavy menstrual bleeding).
- Asymptomatic: Many individuals with ITP, particularly those with mild thrombocytopenia, may be asymptomatic and are often diagnosed incidentally during routine blood tests.
- Acute vs. Chronic: ITP can present as an acute self-limited episode, typically seen in children, or as a chronic condition with persistent or recurrent thrombocytopenia, more common in adults.
- Severe Bleeding: In rare cases, ITP can lead to severe or life-threatening bleeding, such as intracranial hemorrhage, gastrointestinal bleeding, or extensive hematomas.
Less Common Features:
- Fatigue: Some individuals may experience fatigue, particularly if anemia is present due to blood loss.
- Splenomegaly: Mild splenomegaly (enlarged spleen) may be present in some cases, but it is usually not a prominent feature.
Important Considerations:
- History and Physical Examination: A thorough history and physical examination are essential to assess bleeding symptoms, identify potential triggers, and rule out other causes of thrombocytopenia.
- Laboratory Tests: Complete blood count (CBC) with platelet count is essential for diagnosis. Peripheral blood smear may show reduced platelet numbers and sometimes larger, younger platelets.
- Additional Testing: Bone marrow examination may be considered in some cases to rule out other hematologic disorders.
Remember that the clinical presentation of ITP can vary widely, and a comprehensive evaluation is crucial for accurate diagnosis and management.[7]
Sign & Symptoms
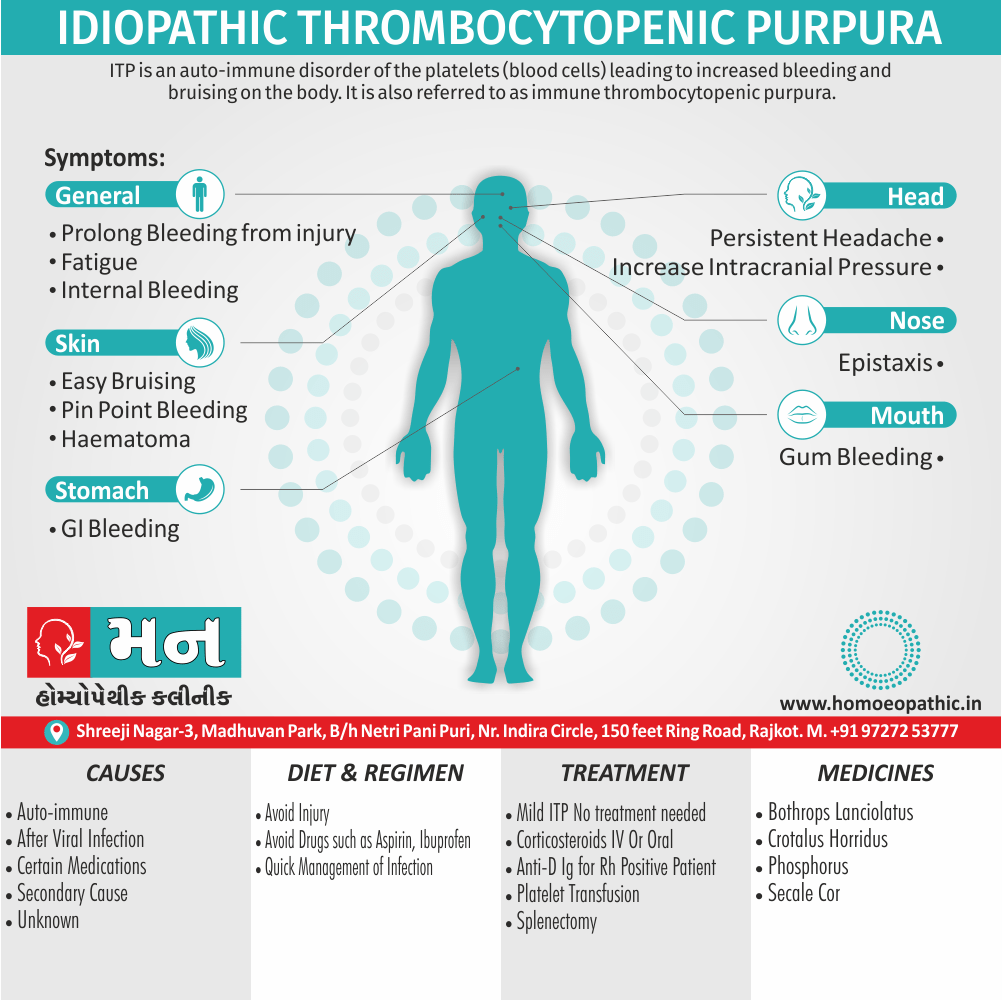
Sign & Symptoms of Idiopathic Thrombocytopenic Purpura (ITP)
Acute thrombocytopenia i.e.–
If severe and of sudden onset, may cause widespread purpura, bruising, mucosal bleeding, cerebral and GI hemorrhage. Moreover, Fundal hemorrhage, persistent headache and other signs of increasing intracranial pressure suggest intracranial bleeding. In detail, Children with acute thrombocytopenia are at less risk than adults. When the condition develops after viral infection, e.g. measles, EBV infection, the duration is brief, active treatment is not required also recovery is nearly always complete.
Chronic ITP i.e.
In brief, It is most common in young adults, especially women. Most patients have purpura, epistaxis, also often menorrhagia. Symptoms tend to fluctuate, with fairly long remissions as well as periods when symptoms increase spontaneously. Commonly occur after a viral infection.
Severity of bleeding in ITP is determined by platelet count. [1]
Platelet count and severity of bleeding in ITP.
- Firstly, Platelet count is > 50 No spontaneous bleed
- Secondly, If Platelet count is 10-50 Bleeding in skin and mucus membranes
- Thirdly, Platelet count is < 10 post-traumatic bleeding, serious GI, and genitourinary bleeding.
Clinical Examination
Clinical Examinations
The clinical examination for ITP focuses on identifying signs of bleeding and ruling out other potential causes of thrombocytopenia.
Key Components of the Examination:
- Skin and Mucosal Assessment:
- Look for petechiae (small, flat, red or purple spots), purpura (larger areas of bruising), and ecchymosis (bruises).
- Examine mucous membranes for bleeding gums, epistaxis (nosebleed), or other signs of mucosal bleeding.
- Abdominal Examination:
- Palpate for splenomegaly (enlarged spleen), although this is not always present in ITP.
- Check for abdominal tenderness or masses that may suggest alternative diagnoses.
- Neurological Examination:
- Assess for any neurological deficits that could indicate intracranial hemorrhage, a rare but serious complication of ITP.
- Other Systems:
- Examine the lymph nodes for enlargement.
- Evaluate for signs of systemic illness, such as fever or weight loss, which could suggest an underlying condition contributing to ITP.
Additional Considerations:
- History: A detailed history is crucial, including questions about bleeding symptoms, recent infections, medications, and family history of autoimmune disorders.
- Laboratory Tests: Complete blood count (CBC) with platelet count is essential. Peripheral blood smear may show reduced platelet numbers and sometimes larger platelets.
- Further Investigations: Bone marrow examination or additional tests may be needed to exclude other causes of thrombocytopenia, especially in cases with atypical features or non-response to initial treatment.
Please note that the clinical examination findings can vary depending on the severity of thrombocytopenia and the presence of other underlying conditions.[8]
Diagnosis
Diagnosis of Idiopathic Thrombocytopenic Purpura (ITP)
- Blood Thrombocytopenia Hb decreased Antiplatelet antibodies
- Bone marrow i.e.
- Megakaryocytic hyperplasia
- Non-functioning megakaryocytes. Additionally, Absence of budding of platelets from cytoplasm
- Erythroid hyperplasia due to anaemia
- Iron stores diminished, if severe bleeding is one of the features
Differential Diagnosis
Differential Diagnosis
The differential diagnosis of ITP includes a wide range of conditions that can cause thrombocytopenia, both immune-mediated and non-immune-mediated.
Immune-Mediated Causes:
- Drug-Induced Thrombocytopenia (DITP): Certain medications can trigger an immune response against platelets, leading to thrombocytopenia. Common culprits include heparin, quinine, and sulfonamides.
- Heparin-Induced Thrombocytopenia (HIT): A specific type of DITP caused by heparin exposure, characterized by both thrombocytopenia and thrombotic complications.
- Secondary ITP: ITP can occur secondary to other underlying conditions, such as autoimmune diseases (e.g., systemic lupus erythematosus), infections (e.g., HIV, hepatitis C), or lymphoproliferative disorders.
- Post-Transfusion Purpura (PTP): A rare but severe immune reaction that can occur after blood transfusion, resulting in profound thrombocytopenia.
Non-Immune-Mediated Causes:
- Inherited Thrombocytopenias: Several genetic disorders can cause thrombocytopenia, including Wiskott-Aldrich syndrome, Bernard-Soulier syndrome, and MYH9-related disorders.
- Bone Marrow Failure Syndromes: Conditions like aplastic anemia, myelodysplastic syndromes (MDS), and acute leukemia can lead to decreased platelet production.
- Hypersplenism: An enlarged spleen can sequester and destroy platelets, leading to thrombocytopenia.
- Thrombotic Microangiopathies (TMA): TMA syndromes, such as thrombotic thrombocytopenic purpura (TTP) and hemolytic uremic syndrome (HUS), involve platelet consumption and can mimic ITP.
Additional Considerations:
- Pseudothrombocytopenia: This laboratory artifact occurs when platelets clump together in vitro, leading to falsely low platelet counts. It can be ruled out by examining a peripheral blood smear.
- Other Causes: Less common causes of thrombocytopenia include vitamin B12 or folate deficiency, disseminated intravascular coagulation (DIC), and certain infections (e.g., dengue, malaria).
A thorough evaluation, including detailed history, physical examination, laboratory tests, and sometimes bone marrow examination, is crucial to accurately diagnose ITP and distinguish it from other potential causes of thrombocytopenia.[9]
Complications
Complications
The primary complication of ITP is bleeding, which can range from mild to severe and life-threatening.
Common Complications:
- Mucocutaneous Bleeding: Easy bruising, petechiae (small red or purple spots on the skin), purpura (larger areas of bruising), epistaxis (nosebleeds), and gingival bleeding (bleeding gums) are common.
- Menorrhagia: Women with ITP may experience heavy menstrual bleeding.
- Gastrointestinal Bleeding: Less commonly, bleeding in the gastrointestinal tract can occur, leading to hematemesis (vomiting blood) or melena (black, tarry stools).
Rare but Serious Complications:
- Intracranial Hemorrhage (ICH): This is the most feared complication of ITP, although it is rare, occurring in less than 1% of cases. ICH can be life-threatening and requires immediate medical attention.
- Other Major Bleeding: Severe bleeding can occur in other organs, such as the lungs, kidneys, or adrenal glands.
Treatment-Related Complications:
- Complications of Splenectomy: Splenectomy is a potential treatment for ITP, but it carries risks like infection (especially with encapsulated bacteria), thrombosis, and increased risk of cardiovascular disease.
- Adverse Effects of Medications: Immunosuppressive therapies and other medications used to treat ITP can have side effects, such as increased susceptibility to infections, gastrointestinal upset, and liver toxicity.
Long-Term Complications:
- Chronic ITP: In some cases, ITP can become chronic, requiring ongoing monitoring and treatment to manage bleeding risk and maintain an acceptable quality of life.
It is important to note that the risk of complications is generally higher in individuals with severe thrombocytopenia (platelet count < 10,000/µL) and those with other underlying medical conditions.[10]
Investigations
Investigations
The investigation of suspected ITP focuses on confirming the diagnosis of thrombocytopenia, excluding other potential causes, and assessing the severity of the condition.
Key Investigations:
Complete Blood Count (CBC): This is the initial test to confirm thrombocytopenia (low platelet count). The CBC also assesses for anemia (low red blood cell count) and leukopenia (low white blood cell count), which may be present in some cases.
Peripheral Blood Smear: Examination of the blood smear helps confirm the presence of reduced platelet numbers and may reveal large platelets, which are often seen in ITP due to increased platelet turnover.
Additional Blood Tests:
- Coagulation Tests: Prothrombin time (PT), activated partial thromboplastin time (aPTT), and fibrinogen levels are usually normal in ITP, helping to distinguish it from other bleeding disorders.
- Direct Antiglobulin Test (DAT): The DAT is usually negative in ITP, but it can help exclude other immune-mediated causes of thrombocytopenia.
- Tests for Underlying Conditions: Depending on the clinical presentation and history, additional tests may be ordered to rule out secondary causes of ITP, such as autoimmune disease tests (e.g., antinuclear antibodies), viral serologies (e.g., HIV, hepatitis C), or bone marrow biopsy.
Other Investigations (if indicated):
Bone Marrow Examination: This is not routinely performed in all cases but may be considered in patients with atypical features, non-response to initial treatment, or suspicion of another underlying hematologic disorder.
Imaging Studies: Ultrasound or CT scan of the abdomen may be done to assess for splenomegaly or other abnormalities.
It is important to note that the investigation of ITP should be tailored to the individual patient, taking into account their clinical presentation, medical history, and response to initial treatment.[11]
Treatment
Treatment of Idiopathic Thrombocytopenic Purpura (ITP)
Conservative treatment
[a] Bleeding not severe i.e.–
Wait and see policy especially in children and young women up to the age of 25, because spontaneous remission, often permanent occurs in number of patients. Moreover, Initiate treatment when PCT <30,000
[b] Severe bleeding i.e.–
(i) Blood transfusion.
(ii) Prednisolone – 40 mg a day for 2 weeks.
- Sometimes permanent remission. Observe patient at intervals for next 12 months.
- If purpura disappears either partially or completely but platelet count remains low, 5-15 mg. of prednisolone daily for a further period of at least 3 months in the hope that permanent remission will occur.
Immunosuppressive therapy
Drugs such as azathioprine or cyclophosphamide are sometimes used in patients who are refractory to splenectomy and steroids or develop relapse.
Immunoglobulin preparations
- IV infusions of large doses result in reticuloendothelial blockade, and may be warranted in life-threatening situation.
Rituximab weekly in doses of 375 mg/m2 can produce remission for a period of time.
TPO receptor agonists – Romiplostim (given subcutaneously) and another orally eltrombopag (given orally) effective in raising platelet counts in patients with ITP and are recommended for adults at risk of bleeding who relapse after splenectomy or who have been unresponsive to at least one other therapy, particularly in those who have a contraindication to splenectomy. [1]
Splenectomy – Indications –
(a) Chronic cases, particularly adults, who have not had sustained response to steroids, and in whom troublesome bleeding persists after 6 months.
(b) Symptoms severe and platelet count very low.
(c) Signs of incipient central nervous system hemorrhage.
(d) Girls approaching age of onset of menstruation.
(e) Young married women likely to become pregnant.
(f) First 5 months of pregnancy.
(g) Steroid refractory
Pregnancy
Anti-platelet auto antibodies in a pregnant woman with ITP will attack the patient’s own platelets and will also cross the placenta and react against fetal platelets. Therefore, ITP is a significant cause of fetal and neonatal immune thrombocytopenia. [1]
Prevention
Prevention
There is no established method for preventing idiopathic thrombocytopenic purpura (ITP) as the exact cause of the autoimmune response is unknown. However, certain measures can be taken to reduce the risk of complications associated with ITP, especially in individuals with known risk factors.
Avoiding Medications Associated with ITP:
Some medications, such as quinine, heparin, and sulfonamides, have been associated with drug-induced thrombocytopenia, which can mimic ITP. If possible, these medications should be avoided, especially in individuals with a history of ITP or other autoimmune disorders.
Prompt Treatment of Infections:
Certain viral and bacterial infections have been linked to the development of ITP. Early diagnosis and treatment of infections may help reduce the risk of triggering ITP in susceptible individuals.
Management of Underlying Conditions:
In cases of secondary ITP, where the condition is associated with another underlying disorder (e.g., SLE, HIV), optimal management of the underlying condition may help control ITP.
Lifestyle Modifications:
Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and adequate sleep, can support overall immune function and potentially reduce the risk of autoimmune disorders like ITP.
Vaccinations:
Although rare, some vaccines have been reported to trigger ITP. Discussing vaccination risks and benefits with a healthcare provider is essential, especially for individuals with a history of ITP or other autoimmune conditions.
It is important to note that these measures are not guaranteed to prevent ITP, but they may help reduce the risk of developing the condition or experiencing complications in individuals with known risk factors. Regular medical checkups and monitoring are also important for early detection and management of ITP. [12]
Homeopathic Treatment
Homeopathic Treatment of Idiopathic Thrombocytopenic Purpura (ITP)
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Idiopathic Thrombocytopenic Purpura (ITP)
The homeopathic remedies (medicines) given below indicate the therapeutic affinity for Idiopathic Thrombocytopenic Purpura but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Bothrops Lanciolatus for Idiopathic Thrombocytopenic Purpura:
- The venom of this snake is most coagulating; therefore, it is expected to be useful in thrombosis and thrombotic affections as hemiplegia.
- Aphasia, without the affection of tongue. Nervous trembling. In detail, Great lassitude and sluggishness.
- Blindness from hemorrhage into retina. Moreover, Day blindness can scarcely see her way after sunrise.
- Paralysis of one arm or one leg only.
- Besides this, Slight shivering, followed by profuse sweat.
- All in all, Intolerable pain in the big toe. Bone becomes bare from gangrene and becomes necrotic. Worse right side. [2]
Crotalus Horridus for Idiopathic Thrombocytopenic Purpura
- Rattle snake poison especially affects blood; heart; liver.
- Basically, It produces profound nervous shock; with deathly sickness, trembling and prostration.
- Furthermore, Easily tired by slight exertion. Paralysis; post- diphtheritic, of the out of control.
- It causes disorganization of blood and tissues.
- Hemorrhages are slow, oozing, of dark thin blood not clots; from all the orifices; also surfaces esp. from pharynx. Additionally, Bloody pus, sweat.
- Tissues rapidly decompose producing putrid also malignant condition.
- Dark or bluish parts. Septic conditions, tonsils; goiter, ulcers, abscesses, blood boils. Petechiae. Gangrene.
- Besides this, Neuralgia as a sequel to sepsis. Chronic biliousness, climacteric conditions. Fainting’s. In detail, Convulsions; epilepsy, with trembling of the limbs, foaming at the mouth, violent cries, delirium. Plague. Yellow fever. Jaundice. General burning. Mouldy odours; of secretions.
- Lastly, Sclerosis; multiple, lateral. Progressive muscular atrophy. Suitable in broken down constitutions, and for old age nutritional troubles. Ill effects especially, of fright; sun; lightning; foul water; noxious effluvia. Affects specifically the right side. Oedema either general or of affected part.
Secale Cor for Idiopathic Thrombocytopenic Purpura
- A vegetable nosode called ergot, contracts the muscles of blood vessels and uterus, decomposes the blood; additionally producing hemorrhage which is thin, fetid, watery, black, oozing continuously.
- Twitching’s; spasms, with fingers spread apart. Gnawing and cramps; with stiffness; in single parts or after the pains.
- Moreover, Insufferable tingling, crawling, starting in face; or back; in the limbs; in finger tips, better rubbing. Sensation of burning in the whole body or as of sparks falling on them, or here and there; like fire.
- Discharges are dark, thin, foul also exhausting. Tetanic spasms with full consciousness. Additionally, Rapid emaciation; of paralyzed part; or with much appetite and excessive thirst.
- Loss of power of voluntary motion. Feels as if walking on velvet. Coldness; but does not want to be covered up. Convulsive jerks also starts in the paralyzed limbs.
- Neuralgia caused by pressure of distended veins. Varicose. Thrombosis. Lymphoid tumors. Sensation of deadness; in any part. Gangrene; traumatic; specifically from application of leeches or mustard, better cold.
- It is suited to irritable plethoric subjects; or to thin, scrawny, feeble women of cachectic appearance; to very old decrepit persons. Petechiae. Small wounds bleed much. Everything feels loose and open.
- Besides this, Contracted arterioles. Chronic, sharp, stinging neuralgic pains, which burn like fire better application of heat. In detail, Paralysis; with distorted limbs; of lower extremities; of one side; of one arm or one leg; with tingling, numbness and prickling.
- Paralysis after spasms. Restlessness, extreme debility; also prostration. Collapse.[2]
Phosphorus for Idiopathic Thrombocytopenic Purpura
- Phosphorus causes inflammation also degeneration of the mucous membrane of stomach and bowels; inflames the spinal cord and nerves; causing paralysis; disorganises the blood; causing fatty degeneration of blood vessels also every tissue and organ of the body; thus it produces a picture of destructive metabolism.
- It is suited to those young people who, grow rapidly and inclined to stoop.
- Chorea of children who grow too fast. Additionally, Tall, slender persons of sanguine temperament; nervous weak delicate persons who like to be magnetized.
- Insidious onset, gradually increasing debility, ending either in severe or rapid disease.
- Hemorrhage, recurrent, vicarious; small wounds bleed much. Blood streaked discharges. In detail, Purpura haemorrhagica.
- Recurrent effects colds, croups etc. Great susceptibility to external impressions, light, sound, odour, touch; electrical changes, etc.
- Suddenness of symptoms; sudden; prostration, faints; weak spells, sweats, shooting pains. Uncertain involuntary acts. Emptiness; in chest, stomach etc. Tightness ; in chest, cough etc.
- Pain or soreness in spots. Paralysis; pseudo-hypertrophic of muscles; of out of control, internal; throat, rectum.
- Internal, itching; tickling; throbbing here also there.
Other symptoms
- Burnings. Jerking; localized; subsultus. Joints; stiff, with little pain; sprains; easily dislocated; weak spells in joints, worse exertion.
- Symptoms due to heart also lung affections. Caries; of the bones; spine; upper jaw.
- Hard swelling here and there. Osteomyelitis. Exostoses. Bone fragility. Polyp; easily bleeding. Jaundice, as a concomitant, hematogenous. Hemophilia. Polycythemia. Erectile tumours. Pyemia. Acidosis. Phthisical habit. Emaciation.
- Spasms on the paralyzed side. Epilepsy with consciousness. Petit mal.
- Totters while walking. Human barometer. Flabby muscles.
- Ill effects of anger, fear, grief; worry; exposure to drenching rains; washing clothes; tobacco; having hair cut. Iodine.
- Excessive use of salt. Healed wounds break out again and bleed. Lipoma. Cancer [2]
Diet & Regimen
Diet & Regimen of Idiopathic Thrombocytopenic Purpura (ITP)
ITP Diet and regimen
Diet
- Supporting overall health: A balanced diet rich in fruits, vegetables, whole grains, and lean protein provides essential nutrients for immune function and overall well-being.
- Managing potential complications: Since ITP can increase bleeding risk, some dietary adjustments may help minimize this risk.
Here are some dietary tips that may be helpful:
Foods to Emphasize:
- Fruits and vegetables: Provide vitamins, minerals, and antioxidants that support immune health.
- Lean protein: Important for cell regeneration and repair.
- Whole grains: Offer fiber and nutrients.
- Healthy fats: Found in avocados, nuts, seeds, and olive oil.
- Foods rich in vitamin K: May play a role in blood clotting (leafy greens, broccoli).
- Iron-rich foods: If you have anemia due to blood loss (lean meats, leafy greens).
Foods to Limit or Avoid:
- Alcohol: Can interfere with platelet function and increase bleeding risk.
- Refined sugars and processed foods: Can contribute to inflammation.
- Artificial sweeteners: May disrupt gut health, which can indirectly affect the immune system.
Regimen
- Manage stress: Stress can worsen autoimmune conditions.
- Get regular exercise: Gentle exercise can improve circulation and overall health.
- Avoid activities that increase bleeding risk: Talk to your doctor about which activities are safe for you.
- Get enough sleep: Adequate rest supports immune function.
Do’s and Don'ts
The Do’s & Don’ts
Do’s:
Do seek medical attention:
If you experience any unusual bruising, bleeding, or other symptoms that could be related to ITP, consult a healthcare professional promptly.
Do follow your treatment plan:
Adhere to your doctor’s recommendations regarding medications, lifestyle changes, and follow-up appointments.
Do protect yourself from injuries:
Avoid activities that could lead to bleeding or bruising, such as contact sports. Use caution when using sharp objects and consider wearing protective gear if necessary.
Do inform your healthcare providers:
Let your dentist and other healthcare providers know about your ITP diagnosis before any procedures.
Do maintain a healthy lifestyle:
Eat a balanced diet, exercise regularly, get enough sleep, and manage stress to support overall health and immune function.
Do monitor your platelet count:
Regular blood tests can help track your platelet levels and assess the effectiveness of treatment.
Do join a support group:
Connecting with others who have ITP can provide valuable emotional support and information.
Don’ts:
Don’t ignore bleeding symptoms:
Even minor bleeding can be a sign of a more serious problem. Don’t hesitate to seek medical attention if you experience any bleeding episodes.
Don’t take medications without consulting your doctor:
Certain medications, such as aspirin and ibuprofen, can interfere with blood clotting and increase the risk of bleeding in individuals with ITP.
Don’t participate in high-risk activities:
Avoid contact sports and activities that could lead to head injuries or excessive bleeding.
Don’t drink alcohol excessively:
Alcohol can impair platelet function and increase the risk of bleeding.
Don’t smoke:
Smoking can negatively impact overall health and may worsen bleeding tendencies.
Don’t hesitate to ask questions:
If you have any concerns about your ITP diagnosis or treatment, talk to your doctor.
Remember, these are general guidelines, and your doctor may have specific recommendations based on your individual situation and the severity of your ITP.
Terminology
Terminology
Idiopathic:
Refers to a condition or disease with an unknown cause or origin. In the case of ITP, the exact trigger for the autoimmune response against platelets is not fully understood.
Thrombocytopenic:
Indicates a low platelet count in the blood. Platelets are essential for blood clotting and preventing bleeding.
Purpura:
Describes purple or reddish discolorations on the skin caused by bleeding under the skin’s surface. This is a common manifestation of ITP due to low platelet levels.
Immune Thrombocytopenia (ITP):
The preferred term for the condition, emphasizing the autoimmune nature of the disorder.
Autoimmune:
Refers to a condition where the body’s immune system mistakenly attacks its own healthy cells or tissues. In ITP, the immune system targets platelets.
Antibodies:
Proteins produced by the immune system that recognize and bind to specific targets, such as foreign substances (antigens). In ITP, autoantibodies are produced against platelet antigens.
Megakaryocytes:
Large cells in the bone marrow responsible for producing platelets.
Splenomegaly:
Enlargement of the spleen, an organ that plays a role in filtering blood and removing old or damaged blood cells, including platelets.
Acute ITP:
Refers to a sudden onset of ITP, often following a viral infection, and usually resolves within six months.
Chronic ITP:
Persists for more than six months and may require ongoing treatment.
Refractory ITP:
ITP that does not respond to standard treatments.
Additional Terms Often Encountered:
Platelet Transfusion:
A procedure where platelets are given to a patient to temporarily increase their platelet count.
Splenectomy:
Surgical removal of the spleen, sometimes considered for patients with chronic ITP who do not respond to other treatments.
Corticosteroids:
Medications used to suppress the immune system and reduce inflammation.
Intravenous Immunoglobulin (IVIG):
A treatment that involves giving high doses of antibodies through a vein to temporarily raise platelet counts.
Thrombopoietin Receptor Agonists (TPO-RAs):
Medications that stimulate the bone marrow to produce more platelets.
Understanding these terminologies is crucial for comprehending medical literature and discussions related to ITP. If you encounter unfamiliar terms, consult a medical professional or reliable resources for clarification.
Terminologies Used in Homeopathic Articles on Idiopathic Thrombocytopenic Purpura (ITP):
General Homeopathic Terms:
Similia Similibus Curentur:
The fundamental principle of homeopathy, meaning "like cures like." It suggests that a substance that can cause symptoms in a healthy person can cure similar symptoms in a sick person.
Potentization/Dilution:
The process of diluting and succussing (vigorously shaking) a homeopathic remedy to increase its potency.
Remedy:
A substance used in homeopathy to treat a specific condition based on the principle of similars.
Proving:
The process of testing a remedy on healthy individuals to determine its potential effects and symptom picture.
Repertory:
A reference book used by homeopaths to find remedies based on specific symptoms.
Materia Medica:
A comprehensive collection of information about homeopathic remedies, including their sources, preparation, and effects.
ITP-Specific Terms:
Anamnesis:
A detailed patient history, including physical, mental, and emotional symptoms, used to select the most appropriate homeopathic remedy.
Constitutional Remedy:
A remedy that matches the overall physical and mental characteristics of the patient, rather than just the specific symptoms of ITP.
Acute Prescribing:
Selecting a remedy based on the current acute symptoms of ITP, such as bleeding or bruising.
Chronic Prescribing:
Selecting a remedy aimed at addressing the underlying susceptibility to ITP and preventing future episodes.
Miasm:
A concept in homeopathy referring to a predisposing factor or inherited tendency towards certain diseases or patterns of illness.
Examples of Remedies Mentioned in Homeopathic ITP Articles:
- Phosphorus: Often used for bleeding tendencies, especially bright red bleeding from mucous membranes.
- Lachesis: May beconsidered for cases with bluish discoloration of the skin and a tendency towards blood clots.
- Crotalus Horridus: Used for hemorrhagic conditions with dark, thin, non-coagulable blood.
- Arnica: Commonly used for trauma and bruising.
- Ferrum Metallicum: May be considered for anemia associated with ITP.
Important Note: Homeopathic treatment for ITP should be individualized based on the patient’s specific symptoms and overall constitution. It is important to consult a qualified homeopathic practitioner for proper diagnosis and treatment.
References
References use for Article Idiopathic Thrombocytopenic Purpura (ITP)
- Harrison-s_Principles_of_Internal_Medicine-_19th_Edition-_2_Volume_Set
- Concise Materia Medica of Hom. Remedies By S.R. Phatak
- Shilpa Kalal and K Suresh. “Immune Thrombocytopenic Purpura – A Recurrent Case in a Young Lady". Acta Scientific Women’s Health 3.6 (2021): 135-138.
- Williams Hematology (9th edition, Kaushansky et al., 2016, McGraw Hill Education.
- Williams Hematology (10th edition, Kaushansky et al., 2021, McGraw Hill Education
- Hoffman’s Hematology: Basic Principles and Practice ,7th edition, Hoffman et al., 2018, Elsevier
- Wintrobe’s Clinical Hematology (14th edition, Greer et al., 2019, Lippincott Williams & Wilkins).
- DeVita, Hellman, and Rosenberg’s Cancer Principles & Practice of Oncology (11th edition, DeVita et al., 2019, Lippincott Williams & Wilkins).
- Hematology: Basic Principles and Practice (7th edition, Hoffman et al., 2018, Elsevier).
- Harrison’s Principles of Internal Medicine (21st edition, Jameson et al., 2022, McGraw Hill Education).
- Hoffman’s Hematology: Basic Principles and Practice (8th edition, Hoffman et al., 2023, Elsevier).
- Rossi’s Principles of Transfusion Medicine (5th edition, Klein & Flanagan, 2016, Wiley-Blackwell)
Also Search As
Also Search As
Online Databases:
Homeopathic Journals: Search reputable homeopathic journals like The Journal of the American Institute of Homeopathy (JAIH) or Homeopathy. These often publish case reports and research articles on various conditions, including ITP.
Research Databases: Utilize platforms like ResearchGate, PubMed, or Google Scholar and include search terms like "homeopathy," "idiopathic thrombocytopenic purpura," and "case reports."
Homeopathic Organizations:
Websites: Check the websites of national and international homeopathic organizations. They may have resources, publications, or case studies related to ITP.
Conferences and Seminars: Attend or access recordings of homeopathic conferences where ITP might be discussed.
Homeopathic Practitioners:
Consultations: Reach out to experienced homeopathic practitioners. They may have access to case studies, research articles, or personal experiences with treating ITP.
Online Forums and Communities:
Homeopathic Forums: Participate in online forums or communities where homeopaths and patients discuss various health conditions, including ITP. You can ask for recommendations, share experiences, or find relevant articles.
Libraries:
Homeopathic Libraries: Many homeopathic colleges or organizations have libraries with a collection of books, journals, and research papers on homeopathy.
Search Tips: Use specific keywords: Combine terms like "homeopathy," "ITP," "immune thrombocytopenia," "case reports," "research," or specific remedy names (e.g., "Phosphorus," "Lachesis"). * Filter by date: Focus on recent publications for the latest research and findings. * Check the credibility of sources: Ensure that the information comes from reputable homeopathic journals, organizations, or experienced practitioners. * Consider different types of sources: Look for a combination of research articles, case reports, and practitioner experiences to get a comprehensive view.
By utilizing these resources and search tips, you can find valuable information on the homeopathic approach to ITP, including case studies, research findings, and insights from experienced practitioners.
There are several ways to search for information on Idiopathic Thrombocytopenic Purpura (ITP), catering to different needs and levels of expertise:
General Information:
Search Engines (Google, Bing, etc.): A simple search for "Idiopathic Thrombocytopenic Purpura" or "ITP" will yield numerous results, including articles, websites, and resources from reputable health organizations.
Health Websites: Reputable websites like Mayo Clinic, National Institutes of Health (NIH), or patient advocacy groups often provide comprehensive information on ITP, including symptoms, causes, diagnosis, and treatment options.
Medical Literature:
PubMed: A database of biomedical literature that allows for searching scientific articles and publications on ITP. Use specific keywords like "ITP," "immune thrombocytopenia," or related terms for targeted results.
Medical Journals: Search for articles in hematology or oncology journals that focus on ITP research, clinical trials, and treatment guidelines.
Specific Areas of Interest:
Clinical Trials: If interested in the latest research and experimental treatments, search for ongoing clinical trials for ITP on platforms like ClinicalTrials.gov.
Support Groups and Forums: Online support groups and forums allow you to connect with other patients and families affected by ITP, share experiences, and learn from each other.
Specialist Websites: Websites dedicated to specific blood disorders or hematology practices may offer specialized information and resources on ITP.
Tips for Effective Searching:
Use specific keywords: Combine terms like "ITP," "immune thrombocytopenia," "treatment," "diagnosis," or specific symptoms you are interested in.
Filter your search: Use filters to narrow down your results by date, type of publication, or source.
Evaluate the credibility of sources: Ensure the information comes from reputable sources like established medical organizations, research institutions, or peer-reviewed journals. Be cautious of information from unreliable or unverified sources.
Consult with healthcare professionals: Always discuss any information you find online with your doctor or a hematologist to confirm its accuracy and relevance to your individual situation.
By utilizing these different search strategies and resources, you can gather comprehensive and reliable information on ITP to better understand the condition, its management, and available support options.
Frequently Asked Questions (FAQ)
What is Idiopathic Thrombocytopenic Purpura?
Definition
Idiopathic thrombocytopenic purpura or immune thrombocytopenia also known as Immune thrombocytopenic purpura (ITP), is a type of thrombocytopenic purpura defined as an isolated low platelet count with a normal bone marrow in the absence of other causes of low platelets.
What causes Idiopathic Thrombocytopenic Purpura?
- Decreased platelet production Hypoplasia of megakaryocytes
- Abnormal pooling of platelets
- Hepatitis
- Malignancy
- Pregnancy
- HIV infection
Give the types of Idiopathic Thrombocytopenic Purpura?
- Acute thrombocytopenia
- Chronic ITP
What are some commonly used homeopathic remedies for ITP?
Some remedies often considered for ITP include Phosphorus, Lachesis, Crotalus horridus, Arnica, and Ferrum metallicum. However, the choice of remedy depends on the individual’s specific symptoms and overall constitution.
What are the symptoms of Idiopathic Thrombocytopenic Purpura?
Symptoms
- Purpura
- Bruising
- Mucosal bleeding
- Cerebral
- GI hemorrhage
Homeopathic Medicines used by Homeopathic Doctors in treatment of Idiopathic Thrombocytopenic Purpura?
Homeopathic Medicines for Idiopathic Thrombocytopenic Purpura
- Bothrops Lanciolatus
- Crotalus Horridus
- Secale Cor
- Phosphorus
Can homeopathy help with ITP?
Homeopathy aims to stimulate the body’s healing response and address the underlying immune system imbalance. Some studies suggest homeopathy may help improve platelet counts and reduce symptoms in ITP, but more research is needed.
How does homeopathic treatment for ITP work?
A homeopathic practitioner will conduct a detailed consultation to understand your individual symptoms, medical history, and overall constitution. Based on this information, they will select a remedy tailored to your specific needs.
How long does homeopathic treatment for ITP take?
The response to treatment varies. Some individuals may see improvement in platelet counts within weeks, while others may take longer. Chronic ITP may require ongoing treatment.