Eczema
Definition
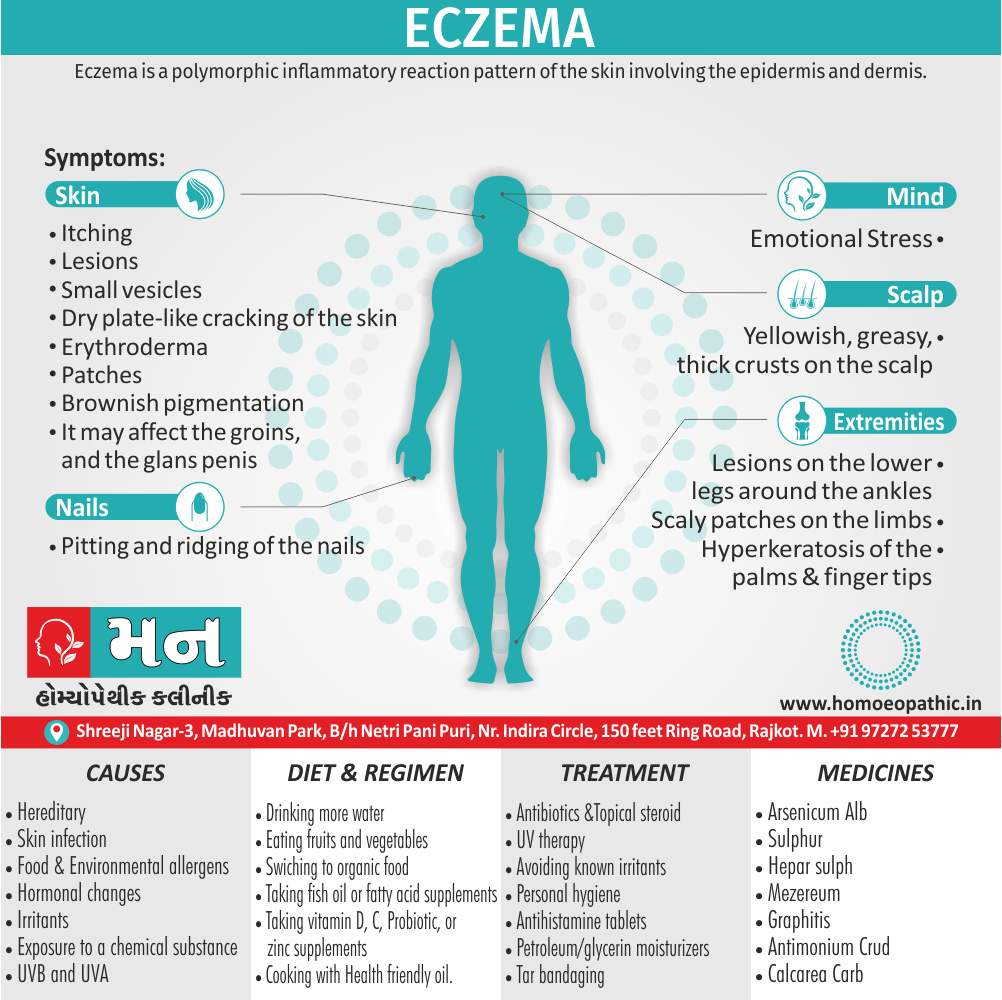
Eczema is a polymorphic inflammatory reaction pattern of the skin involving the epidermis and dermis. [1]
Eczema is a general term for a group of inflammatory skin conditions that cause itchy, red, and dry patches. While "eczema" itself is the most widely used term, there are a few synonyms you might encounter, depending on the specific type of eczema:
Dermatitis:
This is a broader term for any inflammation of the skin. Eczema is a type of dermatitis, but not all dermatitis is eczema.
Atopic dermatitis:
This is the most common type of eczema, especially in children. It’s often referred to as "childhood eczema" and can cause itchy, red patches on the face, hands, and feet.
- Other types of eczema may have more specific names, such as:
- Contact dermatitis: caused by direct contact with an irritant or allergen.
- Dyshidrotic eczema: causes small, itchy blisters on the palms and sides of the fingers and toes.
- Seborrheic dermatitis: affects the scalp and oily areas of the body, like the face, chest, and back.
- Nummular eczema: causes round or oval-shaped patches, often on the hands and feet.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Dont’s
Terminology
References
Also Search As
Overview
Overview
The term ‘eczema’ literally means to ‘boil over’ (Greek).[1]
This reflects that the skin can become so acutely inflamed that fluid weeps out or vesicles appear.
It is synonymous with the term dermatitis and the two words are interchangeable.
It is estimated that 10% of people have some form of eczema at any one time, and up to 40% of the population will have an episode of it during their lifetime.[2]
Epidemiology
Epidemiology
The epidemiology of eczema (also known as atopic dermatitis) in India has shown varying prevalence rates and patterns in different studies.
A systematic review published in 2023 titled "Current Burden of Atopic Dermatitis in India: A Systematic Literature Review" on ResearchGate examined studies between 2011 and 2021 and found the following:
Pediatric population (up to 16 years):
Prevalence ranged from 3.1% to 7.21%
Combined pediatric and adult population:
Prevalence ranged from 0.98% to 9.2%
Economic burden:
Cost of medications was the major contributor
Mental health:
Depression and anxiety were frequently associated with eczema
The wide range in prevalence rates might be attributed to differences in study methodology, populations studied, and diagnostic criteria.
Other studies have also reported varying prevalence rates. For instance, a study published in the Indian Journal of Dermatology, Venereology, and Leprology (IJDVL) in 2008 titled "Atopic dermatitis in infants and children in India" found a prevalence rate of only 0.55% in children.
Overall, eczema is a significant health concern in India, affecting both children and adults. More research is needed to better understand the epidemiology of eczema in India and to develop effective prevention and treatment strategies.
References:
- Ghosh, S., & Banerjee, S. (2023). Current Burden of Atopic Dermatitis in India: A Systematic Literature Review. ResearchGate. https://www.researchgate.net/publication/ 373546002_Current_Burden_of_ Atopic_Dermatitis_in_India_ A_Systematic_Literature_Review
- Kumar, R., & Kaur, S. (2008). Atopic dermatitis in infants and children in India. Indian Journal of Dermatology, Venereology, and Leprology (IJDVL), 74(5), 452-455.
It is important to note that this is just a snapshot of the available information on the epidemiology of eczema in India. The field is constantly evolving, and new research is being published regularly.[7][8]
Causes
Causes
Atopic eczema i.e.:
- Hereditary
- Irritants- e.g. soap, detergents, shampoo Etc.
- Environmental allergens- for example, cold dry weather, dampness, dust, mites etc.
- Food allergies
- Hormonal changes
- Skin infection [1][2]
Discoid eczema i.e.:
- Infective organisms
- Hereditary
- Skin infection, etc. [1][2]
Hand eczema i.e.:
- Irritants
- Fungal infection
- Skin infections [1][2]
Seborrheic eczema i.e.:
- In brief, Overgrowth of Pittosporum ovale (also called Malassezia furfur in its hyphal form) cutaneous immune response to this yeast produces the characteristic inflammation and scaling of seborrheic eczema. [1][2]
Venous eczema i.e.:
- The exact cause remains unknown but it has been suggested that venous hypertension causes endothelial hyperplasia
- In detail, Extravasation of red and white blood cells which in turn causes inflammation, purpura and pigmentation.[1][2]
Asteatotic eczema i.e.:
- Repeated use of soaps
- Hypothyroidism [1][2]
Contact eczema – irritant i.e.:
- Environmental irritants
Contact eczema – allergic i.e.:
- Occurs after repeated exposure to a chemical substance
Photosensitive eczema i.e.:
- Light in the ultraviolet (in other words, UV) part of the spectrum
- UVB and UVA
Lichen simplex/nodular prurigo i.e.:
- Chronic scratching or rubbing in the absence of an underlying dermatosis. [1][2]
Types
Classification
Endogenous:
- Atopic
- Discoid
- Hand
- Seborrheic
- Venous (i.e. ‘gravitational’)
- Asteatotic
Exogenous:
- Contact– irritant
- Contact– allergic
- Photosensitive
- Lichen simplex/nodular prurigo [2]
Risk Factors
Risk factor
- Infection of bacteria
- Viral infections
- Multiple small blisters
- Pyrexia
- Malaise
- Cataract [1][2]
Pathogenesis
Pathogenesis
A comprehensive resource detailing pathogenesis is:
This textbook Rook’s Textbook of Dermatology provides an in-depth discussion on the complex interplay of genetic, immunological, and environmental factors contributing to the development of it. It covers topics such as:
Skin barrier dysfunction:
Impaired function of the skin’s outermost layer allows allergens and irritants to penetrate, triggering inflammation.
Immune dysregulation:
Overactive immune responses, particularly involving T helper 2 (Th2) cells, lead to chronic inflammation.
Genetic predisposition:
Certain gene variants, such as those related to filaggrin production, increase susceptibility to eczema.
- Environmental triggers:
Exposure to allergens, irritants, and microbes can exacerbate eczema symptoms
.Rook’s Textbook of Dermatology is a widely respected reference in the field, providing a wealth of information on the pathogenesis, diagnosis, and management of various skin disorders, including it.[9]
Pathophysiology
Pathophysiology
- Skin is affected from any Allergens. Additionally, It penetrates into the skin.
- Furthermore, Inflammation of skin take place, Skin becomes itchy and Patient starts to scratch his/her skin, Scratching damages the skin barrier so again the allergen is penetrated into the skin
- This process is taken place again also again therefore the more area is affected.[3]
Clinical Features
Clinical Features
A comprehensive resource detailing eczema clinical features is:
This textbook Bolognia Dermatology provides a thorough overview of the clinical manifestations of eczema across different age groups and body sites. It covers topics such as:
- Infantile eczema: Characterized by erythematous, scaly patches on the cheeks, forehead, and scalp.
- Childhood eczema: Often involves flexural areas like the elbows and knees, with lichenification (thickening of the skin) and excoriations (scratches) due to intense itching.
- Adult eczema: Can present with a wider distribution, including the hands, feet, and trunk, with more chronic changes like dryness and scaling.
Bolognia Dermatology is a well-established reference in dermatology, offering detailed descriptions and images of various skin disorders, making it a valuable resource for understanding the clinical features of eczema.[10]
Sign & Symptoms
Sign & Symptoms of Eczema
Atopic Eczema i.e.:
- Generally, Itchy erythematous scaly patches in front of the elbows and ankles, behind the knees, around the neck.
- Acute lesions
- Small vesicles
- Besides this, Scratching can produce excoriations
- Repeated rubbing produces skin thickening
- Pitting and ridging of the nails.[1][2]
Discoid eczema i.e.:
- Scaly patches on the limbs
- Infection of bacteria
- Vesicles
Hand eczema i.e.:
- Itchy vesicles
- Blisters on the palm also Fingers
- Erythematous scaling
- Hyperkeratosis of the palms
- Most marked at the finger tips.[2][1]
Seborrheic eczema i.e.:
- Basically, Affects body sites rich in sebaceous glands
- In child Yellowish, greasy, thick crusts are seen on the scalp
- In child scaly rash can be seen over the trunk
- In detail, In adult scaling along the sides of the nose
- In adult It may affect the skin over the sternum groins, also the glans penis
- Overall, In elder people involve large areas of the body and even cause erythroderma.
Venous eczema i.e.:
- Occur in older people
- Appears on the lower legs around the ankles.
- Brownish pigmentation
- Either Venous leg ulcer or varicose veins may be present.[1][2]
Asteatotic eczema i.e.:
- Dry plate-like cracking of the skin
- Occurs lower legs also the backs of the hands, especially in winter
- Itching
Contact eczema – irritant i.e.:
- Either Unusual or localized distribution
- Paches
- Irritation
Contact eczema – allergic i.e.:
- Occurs on the hands after repeated exposures to irritants
- Vesicles
- Blisters
Photosensitive eczema i.e.:
- Photosensitive rashes.
- Sites exposed to the sun’s rays, face, chest, the ears hands.
Lichen simplex/nodular prurigo i.e.:
- Itching
- increased either rubbing or scratching
- Emotional stress.[1][2]
Clinical Examination
Clinical Examination
A comprehensive resource detailing it’s clinical examination is:
This textbook Fitzpatrick’s Dermatology provides a systematic approach to the clinical examination of it’s , including:
- History taking: Eliciting information about the onset, duration, and pattern of symptoms, as well as potential triggers and aggravating factors.
- Physical examination: Inspecting the skin for characteristic features such as erythema, papules, vesicles, crusting, scaling, lichenification, and excoriations, noting the distribution and severity.
- Differential diagnosis: Considering other skin conditions that may mimic eczema, such as psoriasis, contact dermatitis, and fungal infections.
Fitzpatrick’s Dermatology in General Medicine is a classic reference in the field, offering detailed guidance on the clinical evaluation of various skin disorders, making it a valuable resource for learning how to perform a thorough eczema examination.[11]
Diagnosis
Diagnosis
- In general, By high serum IgE levels
- Skin-prick testing
- Skin biopsy
- History
- Diagnosis is based on clinical findings e.g. onset in infancy
- Severe pruritus
- Blood tests
- Typical distribution, additionally morphology of lesions
- Either Personal or family history of atopic dermatitis, allergic rhinitis or asthma.[1][2]
Differential Diagnosis
Complications
Complications
A comprehensive resource detailing eczema complications is:
This textbook Andrews’ Diseases of the Skin: Clinical Dermatology provides a comprehensive overview of the potential complications associated with it, including:
Skin infections:
It disrupts the skin barrier, increasing susceptibility to bacterial (e.g., Staphylococcus aureus), viral (e.g., eczema herpeticum), and fungal (e.g., Candida) infections.
Allergic contact dermatitis:
Eczema patients may develop allergic reactions to topical medications or other substances that come in contact with their skin.
Neurodermatitis (lichen simplex chronicus):
Chronic scratching due to intense itching can lead to thickened, leathery skin patches.
Sleep disturbances:
Itching and discomfort can disrupt sleep, impacting quality of life.
Psychological impact:
It can cause significant emotional distress, leading to anxiety, depression, and social isolation.
Andrews’ Diseases of the Skin is a classic reference in dermatology, offering detailed information on the diagnosis and management of various skin disorders, including the potential complications associated with it.[12]
Investigations
Investigation
- Physical examination
- Allergy test to check allergies
- Skin biopsy
Treatment
Treatment of Eczema
Atopic Eczema i.e.:
- Topical steroid
- Antibiotics
- Paste bandaging
- UV therapy
- Avoiding known irritants
- Wearing cotton clothes [1][2]
Discoid eczema i.e.:
- Antibiotics
- Avoid irritants
- UV therapy
- Personal hygiene, etc. [2]
Hand Eczema i.e.:
- Topical antibiotics
- UV therapy
- Antihistamine tablets
- Petroleum- or glycerin-based moisturizers
- Avoid irritants [2]
Seborrheic eczema i.e.:
- This is suppressive rather than curative
- Combination of a mild steroid ointment
- Tacrolimus ointment
- Ketoconazole shampoo also arachis oil are useful for the scalp.[1][2]
Venous eczema i.e.:
- Emollients
- Topical steroid
- Either Stockings or compression bandages [2]
Asteatotic eczema:
- Avoidance of soaps
- Humidifying centrally heated rooms may help.
- Topical steroids [1][2]
Contact eczema – irritant i.e.:
- As for atopic eczema
- Wearing of protective clothing such as gloves or in extreme cases even changing occupation or hobbies.
Photosensitive eczema i.e.:
- Phototherapy
- Photoprotection
- Use of sunblock’s
- Desensitization
Lichen simplex/nodular prurigo i.e.:
- Topical steroids
- Tar bandaging
- Intralesional steroids
- Phototherapy
Prevention
Prevention
- Avoid substances that trigger or worsen your symptoms
- Take your medicines as prescribed.
- Apply ointments and creams
- Moisturize frequently
- Avoid sudden change in temperature or humidity.
- Use fragrance free detergents, cleanser and skin care products.
- Wear protective gloves and clothing when handling chemicals.
- Reduce stress. (7)
Homeopathic Treatment
Homeopathic Treatment of Eczema
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
The medical history of the patient,
Physical and mental constitution,
Family history,
Presenting symptoms,
Underlying pathology,
Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Eczema:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicine:
Arsenicum Alb:
People who need this remedy usually are anxious, restless and compulsively neat and orderly.
Chronic eczema; eruption upon scalp and face dry and scaly, or pimples and vesicles upon face with acrid, sometimes foetid, discharge and intense burning itching, the same on likes and genitals.
Margin of hair, itching and burning, by scratching, followed by bleeding.
Indigestion with burning pain and a general feeling of chilliness.
Harsh, dry, rough skin in papers not affected by the eruption; emaciation from disturbances in vegetative sphere; emaciation of urine shows deficiency of urea.[5]
Aggravation at night and in cold air, Amelioration from warmth. Barnlike, scaly eruption, on forehead.
Asterias Rubens:
Eczema on thighs, legs, ankles and instep.
Itching vesicles break and form small ulcers which spread superficially.
Scrofulous and sycotic constitutions.[5]
Calcarea Carb:
This remedy is suited to people who are chilly with clammy hands and feet, and tend to develop eczema and cracking skin that is worse in the wintertime.
They are easily fatigued by exertion and feel anxious and overwhelmed if ill or overworked.
Thick, large, yellow scabs form on the occiput first and spread thence to face.
Eruption mostly dry, but thick, bland pus under the crusts.
Itching not very intense, but on awakening from sleep teething children are apt to scratch their head and make it bleed.
Moist eruption upon legs, about navel and flexure of extremities; no dread of water, but eruptions are aggravated by water.
Chronic eruption with cold feet, as it there were damp stockings on them; chalky stools; skin inclined to ulcerate. Eczema scrofulosum.[5]
Antimonium Crud:
People likely to response to this remedy have eczema with thick, cracked skin and also prone to indigestion.
Suppurating, yellow-crusted eruption, pain to touch and easily detached.
Green sanious pus oozes out from beneath the thick, hard, yellow crusts, irritating the surrounding parts, itching violently.
Aggravation from poultices, bathing, working in water, from alcoholic drinks and in the sun.
Gastric derangement with violent thirst and map tongue; especially on face and genital organs; impetigo scroti.[5]
Cantharis:
Eczema Solare with Much Burning and Itching; when touched burning and smarting.
Complications with urinary troubles; eruption begins in a small spot and spreads so as to involve a large surface, with a watery discharge underneath the scabs.
Amelioration from lying down and in cool weather; Aggravation from warmth.
All in all, Scales form on scalp like enormous dandruff; hair falls out; besides this, perspiration smells urinous; eruption mostly on right side.[5]
Graphitis:
People likely to respond to this remedy have either tough or leathery skin with cracks and soreness and often have a long-term history of skin disorders.
Furthermore, Eruptions cracked, moist, easily bleeding.
Eczema of lids, eruptions moist also fissured.
Dry, rough skin that breaks easily also exudes gluey moisture.
Either Moist eczema or eruptions behind ears.
Moist eczema around mouth also chin.
Eczema oozing glutinous fluid which is watery also transparent.
Such fluid may be thick, honey-like. Lastly, Very dry skin; never perspires.[6]
Hepar sulph:
Basically, It spreading by means of new pimples appearing just behind the original affected parts.
Violent itching.
Sticking or pricking felt especially; on the parts, which may be painful to touch.[6]
Mezereum:
A person who needs this remedy often has strong anxiety, felt physically in the stomach.
It affects, especially, those parts of the skin that are normally deficient in fat.
With intolerable itching, worse in bed and from touch; copious serous exudation.
Eczema also itching eruptions after vaccination.
In detail; The head is covered with thick leather-like crust under which pus collects here and there and the hair is glued together.
Child scratches face incessantly; then it becomes covered with blood: inflammatory redness of face.
Besides this; Craving for fat and a tendency to feel better in open air.
Face becomes covered with a scab which the child constantly tears off anew, leaving raw spots on which fat pustules form.
Lastly, Ichor excoriates other parts. [6]
Rhus tox:
A person whose eczema has blister like eruptions that look red and swollen, itch intensely and are soothed by hot applications.
Moist eruptions on head, beginning with small yellow vesicles with red areolae, forming thick crusts and hard horny scabs which eat off the hair, offensive itching, worse at night.
Surface raw, excoriated, extends to shoulders or eczema scroti on insides of thighs.
Discharging freely, or thickened, infiltrated and between the fields sore and humid.
Aggravation by changes of weather, especially wet weather, in winter.
Eczema of right hand.
Cold fresh air is not tolerated on head making scalp painful.[5]
Sulphur:
Dry, offensive, scabby, easily-bleeding, burning eruption, beginning along margin of hair from ear to ear posteriorly, with sore pain and cracks.
Offensive with thick pus; yellow crusts, itching and burning, painful especially around chin and under the toes.
Colicky babies with dry roughness of the skin of body, which itches from warmth and feels good from scratching.
Soreness between nates and in groins, most comfortable when dirty, hates to be washed in fresh air.
Amelioration from scratching or humid.[5]
Diet & Regimen
Diet & Regimen
Dietary Considerations:
- Identify Potential Triggers: Common culprits include dairy, eggs, gluten, soy, nuts, and seafood. A food diary can help pinpoint which foods worsen your eczema.
- Anti-inflammatory Foods: Emphasize fruits, vegetables, whole grains, and foods rich in omega-3 fatty acids (like fatty fish) to help reduce inflammation.
- Probiotics: Some studies suggest probiotics may improve gut health, which could benefit eczema. Yogurt, kefir, and fermented foods are good sources.
- Hydration: Drink plenty of water to keep your skin hydrated.
- Vitamin D: May be helpful, but more research is needed. Talk to your doctor about potential supplementation.
Regimen:
- Moisturize Regularly: Use a thick, fragrance-free moisturizer several times a day, especially after bathing.
- Gentle Skincare: Avoid harsh soaps and hot water, which can dry out the skin. Opt for mild, fragrance-free cleansers and lukewarm water.
- Avoid Irritants: Identify and avoid triggers like harsh fabrics, chemicals, and allergens.
- Stress Management: Stress can worsen eczema. Practice relaxation techniques like yoga, meditation, or deep breathing.
- Bathing and Moisturizing Routine: Develop a consistent routine that includes lukewarm baths followed immediately by moisturizer application.
- Medication: Your doctor may prescribe topical or oral medications to manage inflammation and itching.
Do’s and Dont’s
Do’s and Dont’s
Of Eczema
Do’s:
- Moisturize regularly: Use emollients (moisturizers) frequently to hydrate the skin and maintain its barrier function.
- Take lukewarm baths or showers: Avoid hot water, which can dry out the skin.
- Use gentle, fragrance-free cleansers: Avoid harsh soaps and cleansers that can irritate the skin.
- Wear soft, breathable fabrics: Cotton and linen are good choices, while wool and synthetic fabrics can irritate the skin.
- Identify and avoid triggers: Common triggers include allergens, irritants, and stress.
Don’ts:
- Scratch: Scratching can damage the skin and worsen inflammation.
- Use harsh soaps or cleansers: These can strip the skin of its natural oils and exacerbate dryness.
- Overheat: Sweating can irritate the skin and trigger flares.
- Stress out: Stress can worsen eczema symptoms.
"Atopic Dermatitis: The Essential Guide" is a valuable resource for patients and caregivers, providing practical tips and strategies for managing eczema effectively.[13]
Terminology
Terminology
Common terminologies used in articles about eczema and their meanings:
Atopic Dermatitis (AD):
The most common type of eczema, often with a genetic component and associated with other allergic conditions like asthma or hay fever.
Acute Eczema:
A sudden onset of eczema, often with intense itching, redness, and oozing.
Chronic Eczema:
Long-term or recurring eczema, often with thickened, dry, and itchy skin.
Flare-up:
A worsening of eczema symptoms, often triggered by certain factors.
Erythema:
Redness of the skin caused by inflammation.
Excoriation:
A scratch or abrasion on the skin, often caused by itching.
Lichenification:
Thickening and hardening of the skin, often caused by chronic scratching.
Papules:
Small, raised bumps on the skin.
Pruritus:
Medical term for itching.
Vesicles:
Small, fluid-filled blisters.
Emollients:
Moisturizers that help to soothe and hydrate the skin.
Topical Corticosteroids:
Anti-inflammatory medications applied to the skin to reduce redness and itching.
Immunosuppressants:
Medications that suppress the immune system to reduce inflammation.
Additional terms that may be used in specific contexts:
Filaggrin:
A protein that helps maintain the skin’s barrier function. Mutations in the filaggrin gene are associated with eczema.
Th2 Cells:
A type of immune cell involved in allergic reactions. Overactive Th2 cells can contribute to eczema.
Skin Barrier Dysfunction:
Impaired function of the skin’s outermost layer, allowing irritants and allergens to penetrate and trigger inflammation.
Understanding these terms can help you better understand the information presented in articles about eczema and communicate with healthcare professionals about your condition.
General Homeopathic Terms:
Vital force:
The body’s innate healing energy or life force that homeopaths believe is disrupted in disease states.
Similia Similibus Curentur:
The principle of "like cures like," the foundation of homeopathic treatment, where a substance that can cause symptoms in a healthy person is used to treat similar symptoms in a sick person.
Potentization:
The process of diluting and succussing (vigorously shaking) a homeopathic remedy to increase its therapeutic effect.
Proving:
A systematic study where healthy volunteers take a remedy and record their physical, mental, and emotional symptoms to determine the remedy’s potential effects.
Repertory:
A reference book listing symptoms and the remedies associated with them, used by homeopaths to select remedies.
Materia Medica:
A comprehensive description of homeopathic remedies, including their sources, preparation, and symptoms they can produce and treat.
Eczema-Specific Terms:
Aetiology:
The underlying cause or factors contributing to the development of eczema.
Constitutional Types:
Different classifications of individuals based on their physical, mental, and emotional characteristics, used to select the most suitable remedy.
Miasm:
A predisposition to certain diseases, such as eczema, believed to be inherited and affecting the body’s response to treatment.
Aggravation:
A temporary worsening of symptoms after taking a remedy, often considered a positive sign of healing.
Suppression:
The masking of symptoms without addressing the underlying cause, potentially leading to deeper health issues in the long run.
Nosodes:
Homeopathic remedies prepared from diseased tissue or products, sometimes used in eczema treatment.
Remedy-Specific Terms:
Modalities:
Factors that make symptoms better or worse, such as time of day, temperature, weather, movement, and emotions.
Keynotes:
Characteristic symptoms that are particularly indicative of a specific remedy.
Understanding these terms can help you navigate homeopathic articles on eczema and make informed decisions about your treatment options.
References
References
- KV Krishna Das – Textbook of Medicine, 5th Edition
- Kumar and Clark Clinical Medicine 7th edition 2009 by WINBOY
- https://pubmed.ncbi.nlm.nih.gov/29063428/#:~:text=The%20pathophysiology%20of%20atopic%20dermatitis,mediated%20hypersensitivity%2C%20and%20environmental%20factors.
- https://www.verywellhealth.com/what-to-eat-when-you-have-eczema-4692428
- Homoeopathic Therapeutics by Lilienthal
- The Homoeopathic Prescriber by K. C. Bhanja
- Ghosh, S., & Banerjee, S. (2023). Current Burden of Atopic Dermatitis in India: A Systematic Literature Review. ResearchGate. https://www.researchgate.net/publication/373546002_Current_Burden_of_Atopic_Dermatitis_in_India_A_Systematic_Literature_Review
- Kumar, R., & Kaur, S. (2008). Atopic dermatitis in infants and children in India. Indian Journal of Dermatology, Venereology, and Leprology (IJDVL), 74(5), 452-455.
- Rook’s Textbook of Dermatology Edition: 10th Edition Authors: Christopher Griffiths, Jonathan Barker, Tanya Bleiker, Richard Chalmers, Fiona Creamer, et al.(2020)Publication: Wiley-Blackwell
- Bolognia Dermatology Edition: 4th Edition Authors: Jean L. Bolognia, Joseph L. Jorizzo, Julie V. Schaffer (2018)Publication: Elsevier
- Fitzpatrick’s Dermatology in General Medicine Edition: 9th Edition Authors: Klaus Wolff, Lowell A. Goldsmith, Stephen I. Katz, Barbara A. Gilchrest, Amy S. Paller, David J. Leffell (2019) Publication: McGraw Hill Professional.
- Andrews’ Diseases of the Skin: Clinical Dermatology Edition: 13th Edition Authors: William D. James, Timothy G. Berger, Dirk M. Elston (2020) Publication: Elsevier
- Atopic Dermatitis: The Essential Guide Edition: 1st Edition Author: Alan Irvine Year of Publication: 2018 Publication: Springer.
Also Search As
Also Search As
Specific terms:
Related terms:
Questions:
Long-tail keywords:
Here are some tips for finding relevant information:
- Use a variety of search engines: Don’t just rely on Google. Try other search engines like DuckDuckGo or Ecosia.
- Search for articles in reputable sources: Look for articles on websites of homeopathic organizations, health publications, or reputable homeopathic practitioners.
- Use specific keywords and phrases: The more specific your search terms, the more likely you are to find relevant articles.
- Read multiple articles: Don’t just rely on one article. Read several articles from different sources to get a well-rounded view of the topic.
There are numerous ways to search for information about eczema, each with its own advantages:
Search Engines:
- Google, Bing, DuckDuckGo: These general search engines are a good starting point. Use keywords like "eczema," "atopic dermatitis," "skin rash," "itchy skin," or specific questions like "what causes eczema?"
- Medical websites: Reputable sites like Mayo Clinic, WebMD, Cleveland Clinic, and Medical News Today provide reliable, medically-reviewed information on eczema.
- Government health websites: Organizations like the National Institutes of Health (NIH) and the National Eczema Association (NEA) offer comprehensive resources on eczema.
Online Forums and Communities:
- Eczema support groups: Connect with other individuals with eczema, share experiences, and get advice on managing the condition.
- Social media groups: Platforms like Facebook and Reddit have eczema-specific groups where you can ask questions and get support.
Academic Databases:
- PubMed, Google Scholar: These databases allow you to search for scientific articles and research papers on eczema. This is especially useful for finding in-depth information on specific aspects of eczema.
Libraries:
- Books and journals: Your local library likely has a collection of books and journals on eczema. These can provide a comprehensive overview of the condition and its management.
Healthcare Professionals:
- Doctors, dermatologists, allergists: Consult with healthcare professionals for personalized advice and treatment options. They can answer your specific questions and help you develop a management plan tailored to your needs.
Additional tips for effective searches:
- Use specific keywords: Instead of just searching for "eczema," use more specific terms like "eczema triggers," "eczema treatment options," or "eczema in children."
- Use quotation marks: Enclose phrases in quotation marks to search for exact matches. For example, search for "atopic dermatitis symptoms" to get results that include those exact words.
- Use Boolean operators: Combine keywords with "AND," "OR," or "NOT" to narrow or broaden your search. For example, search for "eczema AND treatment" to get results that include both words.
- Check the date of publication: Ensure the information you’re reading is current and up-to-date.
By utilizing these various methods, you can access a wealth of information on eczema to better understand and manage the condition.
Frequently Asked Questions (FAQ)
What is Eczema?
Eczema is a polymorphic inflammatory reaction pattern of the skin involving the epidermis and dermis.
What causes Eczema?
causes:
- Hereditary
- Irritants- soap, detergents, shampoo
- Environmental allergens
- Food allergies
- Infective organisms
- Fungal infection
- Light in the ultraviolet (UV) part of the spectrum
- UVB and UVA
Is eczema contagious?
No, eczema is not contagious. It cannot be spread from person to person through contact.
Give the types of Eczema?
types:
- Atopic
- Discoid
- Hand
- Seborrheic
- Venous (‘gravitational’)
- Asteatotic
- Contact– irritant
- Contact– allergic
- Photosensitive
- Lichen simplex/nodular prurigo
What are the symptoms of Eczema?
- Itchy erythematous scaly patches
- Acute lesions
- Small vesicles
- Scratching can produce excoriations
- Infection of bacteria
- Vesicles
- Blisters on the palm & Fingers
- Erythematous scaling
- Hyperkeratosis of the palms
Can homeopathy help in treating eczema?
How does a homeopath select the right remedy for eczema?
A homeopath will conduct a detailed case analysis considering various factors:
- Specific skin symptoms (e.g., location, appearance, triggers)
- Overall health and medical history
- Mental and emotional state
- Lifestyle factors
Homeopathic Medicines used by Homeopathic Doctors in treatment of Eczema?
Homeopathic Medicines for Eczema
- Arsenicum Alb
- Asterias Rubens
- Calcarea Carb
- Antimonium Crud
- Cantharis
- Graphitis
- Hepar sulph
- Mezereum
- Sulphur
How long does it take to see improvement with homeopathic treatment for eczema?
- Response time varies depending on individual factors and the severity of the condition.
Some people experience relief within a few weeks, while others might take longer.
