Pityriasis Versicolor
Definition
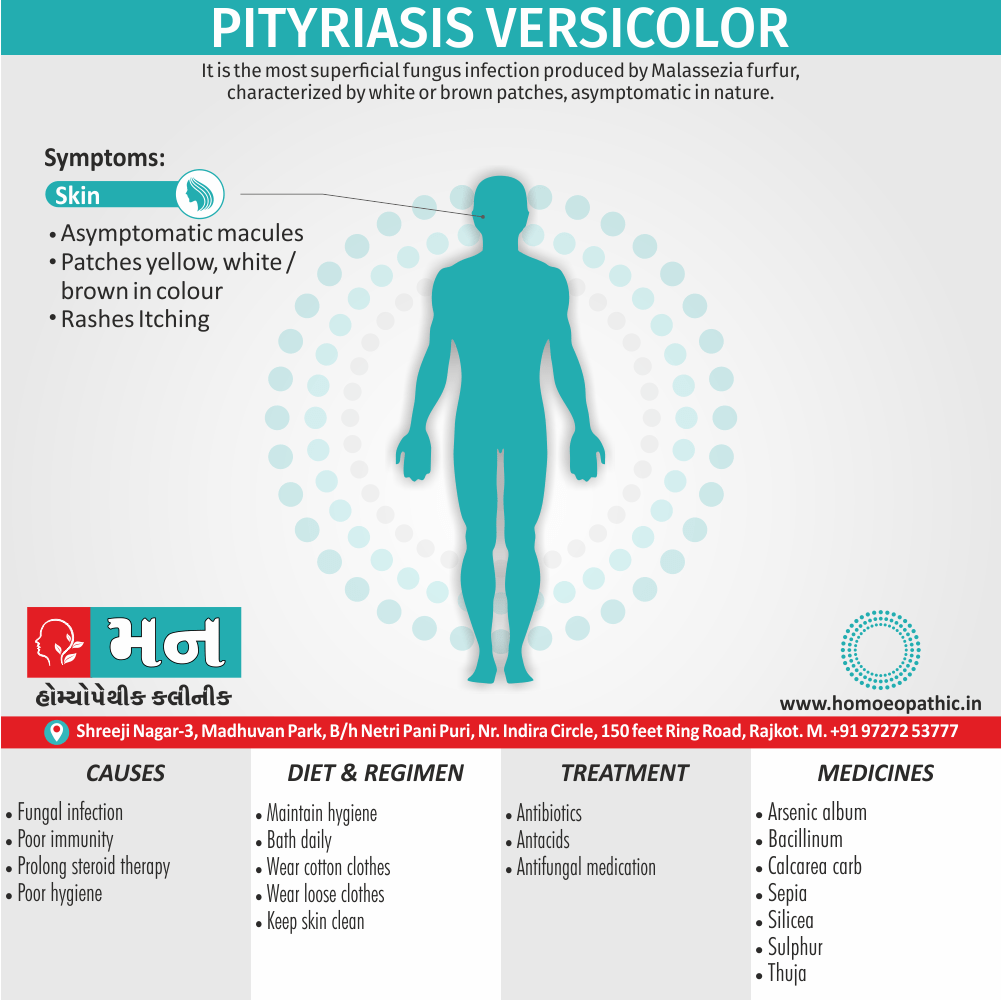
Pityriasis Versicolor is the most superficial fungus infection produced by Malassezia furfur, characterized by scaly white or brown patches, asymptomatic in nature.[1]
Pityriasis versicolor has a few synonyms, some more accurate than others:
- Tinea versicolor: This is the most common synonym, but it’s technically not entirely accurate. Tinea refers to fungal infections caused by dermatophytes, while pityriasis versicolor is caused by a yeast called Malassezia.
- Tinea flava: This term refers to the lighter patches of skin that can occur with pityriasis versicolor.
- Beach fungus: This is an informal term that highlights the fact that pityriasis versicolor can become more noticeable after sun exposure.
It’s important to note that while these terms are used interchangeably, "pityriasis versicolor" is the most precise way to describe this fungal infection.
Overview
Epidemiology
Causes
Risk Factors
Pathogenesis
Pathophysiology
Types
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Pityriasis Versicolor
Pityriasis versicolor, also known as tinea versicolor, is a common, benign, superficial fungal infection of the skin.
Clinical features of pityriasis versicolor include either hyperpigmented or hypopigmented finely scaled macules.
Pityriasis versicolor has been reported worldwide, but it is more common in warm and humid conditions.
It occurs more frequently in adolescents and young adults probably due to the increase of sebum production by the sebaceous glands which allow for a more lipid-rich environment in which Malassezia can grow.
Pityriasis versicolor affects people of all genders equally and no specific ethnic predominance has been noted.[5]
Epidemiology
Epidemiology
Pityriasis versicolor (PV) is a common superficial fungal infection in India, particularly prevalent in tropical and subtropical regions due to the hot and humid climate. Several studies have explored the epidemiology of PV in India, revealing key insights into its prevalence, demographics, and clinical presentation.
A study published in 2014 in the International Journal of Dermatology, Venereology and Leprology found that PV was more common in males (70%) than females (30%), with the most affected age group being 21-30 years (43%). The youngest patient was 13 years old, while the oldest was 65. The majority of patients (65%) had the infection for 1-6 months, while 9% had it for more than a year. Recurrence was observed in 35% of cases. [7]
Another study published in 2021 in the Indian Journal of Dermatology, Venereology and Leprology looked at the prevalence of different Malassezia species in PV in central India. They found that M. globosa was the most common species isolated, followed by M. sympodialis. The study also highlighted that hypopigmented lesions were more frequent (91%) than hyperpigmented lesions (9%). [8]
Other Study
A 2023 study published in the Annals of Indian Academy of Medical and Dental Sciences investigated the demographic profile and risk factors associated with PV. They found a slight female preponderance (56.03%) and the majority of patients were young adults (36.21% in the age group of 11-20 years). Excessive sweating was associated with 74.14% of cases. [9]
These studies collectively demonstrate that PV is a prevalent condition in India, affecting predominantly young adults and males. The hot and humid climate, along with factors such as excessive sweating and oily skin, contribute to its occurrence. While hypopigmented lesions are more common, hyperpigmented lesions can also occur. M. globosa appears to be the predominant causative species in central India.
It’s important to note that the epidemiology of PV can vary across different regions within India due to differences in climate, lifestyle factors, and genetic predisposition. Further research is needed to fully understand the regional variations in PV epidemiology in India.
Causes
Causes of Pityriasis Versicolor
Generally, An overgrowth of yeast on your skin’s surface causes tinea versicolor. Additionally, This yeast thrives in warm, moist also oily environments, causing it to grow out of control in small colonies. Besides this, These yeast colonies cause the symptoms of tinea versicolor.
Some things that can trigger the yeast to grow out of control are i.e.:
- Hormonal changes
- Weakened immune system
- Hot, humid weather
- Sweating
- Oily skin [6]
Risk Factors
Risk Factors
- Hot and Humid Climate: High temperature and humidity favor the growth of Malassezia yeasts.
- Oily Skin: Increased sebum production provides a favorable environment for yeast proliferation.
- Excessive Sweating: Creates a moist environment conducive to fungal growth.
- Immunosuppression: Weakened immune system makes individuals more susceptible to infections.
- Genetic Predisposition: Some individuals may have a genetic susceptibility to developing PV.
- Use of Oily Skin Products: Certain oils and lotions can promote yeast growth.
- Certain Medical Conditions: Conditions like Cushing’s syndrome, malnutrition, and diabetes can increase the risk. [10]
Pathogenesis
Pathogenesis of Pityriasis versicolor
Pityriasis versicolor is caused by an overgrowth of Malassezia yeasts, which are part of the normal skin flora. Several factors contribute to the transformation of these commensal yeasts into pathogenic ones, leading to the characteristic skin lesions.
Key factors in the pathogenesis:
Yeast Overgrowth: Malassezia yeasts proliferate excessively due to favorable conditions like high humidity, oily skin, and immunosuppression.
Morphological Change: The yeasts undergo a morphological change from the round budding yeast form to the filamentous mycelial form, which is associated with the disease.
Lipid Dependence: Malassezia species are lipophilic, meaning they require lipids for growth. They obtain these lipids from sebum and the stratum corneum of the skin.
Disruption of Melanin Production: The yeasts produce azelaic acid, which inhibits tyrosinase, an enzyme crucial for melanin synthesis. This leads to hypopigmentation or hyperpigmentation of the affected skin.
Immune Response: While the exact mechanism is unclear, the host’s immune response may also play a role in the development of lesions. [11]
Pathophysiology
Pathophysiology of Pityriasis Versicolor
- Malassezia is commensal of healthy skin, and it is most common in oily areas such as the face, scalp, and back.
- However, Malassezia can cause pityriasis versicolor when it converts to its pathogenic filamentous form.
- Factors that lead to this pathogenic conversion include a genetic predisposition, environmental conditions such as heat and humidity, immunodeficiency, pregnancy, oily skin, and application of oily lotions and creams.[5]
Types
Types
Pityriasis versicolor presents with different types of skin lesions based on their appearance. The primary types include:
Hypopigmented: These are the most common type, appearing as pale or white patches on the skin. They occur due to the inhibition of melanin production by the Malassezia yeasts.
Hyperpigmented: Less common than hypopigmented lesions, these patches appear darker than the surrounding skin. The mechanism behind hyperpigmentation is not fully understood, but it’s thought to involve an inflammatory response or post-inflammatory hyperpigmentation.
Erythematous: These patches are reddish or pink in color and may be slightly scaly. They are often seen in the early stages of the infection or in individuals with sensitive skin.
Mixed: Some individuals may present with a combination of hypopigmented, hyperpigmented, and erythematous lesions, creating a varied appearance. [12]
Clinical Features
Clinical Features
The clinical features of pityriasis versicolor can vary, but here are some common presentations:
- Macules: The primary lesions are flat, discolored patches on the skin. They can be hypopigmented (lighter than the surrounding skin), hyperpigmented (darker than the surrounding skin), or erythematous (reddish).
- Scaling: The patches often have a fine, powdery scale, which is more easily seen when the skin is scraped.
- Distribution: The lesions typically appear on the upper trunk, back, neck, and upper arms. They can also affect the face, especially in children.
- Pruritus: Itching is usually mild or absent, but some individuals may experience moderate itching.
- Asymptomatic: In many cases, the lesions are asymptomatic and only noticed for their cosmetic appearance.
- Fluorescent under Wood’s lamp: Under Wood’s lamp examination, the lesions may exhibit a characteristic yellow-green or copper-orange fluorescence due to the presence of the yeast. [12]
Sign & Symptoms
Sign & Symptoms of Pityriasis Versicolor
- Asymptomatic macules and patches of various sizes and shapes, yellow, white or brown in color.
- Occur at any site in the body commonly on the trunk. The lesions are scaly and easily detected when the part is abraded with a pin.
- Pityriasis versicolor is usually seen in people who sweat excessively. The patches resemble vitiligo, but presence of scaling is typical and the lesions are never totally lacking in pigment.
- Scales can be made more obvious by striking the lesions with a blade or knife (Scratch sign). At times the lesions may assume different colors such as reddish brown, dark brown or even black seen in Tinea versicolor.[1]
Clinical Examination
Clinical Examination of Pityriasis Versicolor
Key Points:
Inspection:
- Lesion appearance: Look for well-demarcated macules (flat spots) that can be:
- Hypopigmented (lighter than surrounding skin)
- Hyperpigmented (darker than surrounding skin)
- Erythematous (reddish)
- Scaling: May have a fine, powdery scale, especially when scraped gently.
- Distribution: Commonly found on the upper trunk, back, neck, and upper arms. Can also affect the face, especially in children.
- Lesion appearance: Look for well-demarcated macules (flat spots) that can be:
Wood’s Lamp Examination:
- Shine a Wood’s lamp (ultraviolet light) in a darkened room.
- Lesions may show a characteristic yellow-green or copper-orange fluorescence.
KOH Preparation:
- Scrape scales onto a slide.
- Add a drop of potassium hydroxide (KOH) solution.
- Examine under a microscope for the presence of hyphae and budding yeast cells, confirming the diagnosis. [11]
Diagnosis
Diagnosis of Pityriasis Versicolor
- The patches fluoresce golden yellow, under Wood’s light .
- Scraping the lesions and mounting them in 10% KOH solution reveals clusters of spores and short broad hyphae, resembling ‘spaghetti and meat balls’ .[1]
Differential Diagnosis
Differential Diagnosis of Pityriasis Versicolor
- Pityriasis Rosea
- Tinea corporis
- Vitiligo
- Pityriasis alba
- Confluent reticulated papillomatosis
- Post inflammatory hypo- also hyperpigmentation
- Seborrheic dermatitis
- Guttate psoriasis
- Tinea corporis
- Nummular eczema
- Secondary syphilis
- Mycosis fungoides [5]
Complications
Complications of Pityriasis Versicolor:
While pityriasis versicolor is generally a benign and self-limiting condition, it can occasionally lead to a few complications:
Post-inflammatory Hypopigmentation or Hyperpigmentation: The most common complication is the persistence of skin discoloration even after successful treatment of the fungal infection. This can take weeks or even months to resolve, and in some cases, it may be permanent.
Recurrence: Pityriasis versicolor has a high recurrence rate, especially in individuals living in hot and humid climates or those with predisposing factors like oily skin or excessive sweating. This can be frustrating for patients and may require ongoing maintenance therapy.
Cosmetic Concerns: The discolored patches, especially on exposed areas like the face and neck, can cause significant cosmetic distress and impact self-esteem, particularly in individuals with darker skin tones.
Secondary Bacterial Infection: In rare cases, the affected skin may become secondarily infected with bacteria, leading to redness, swelling, and pus formation. This usually occurs due to scratching or picking at the lesions.
Folliculitis: Rarely, Malassezia yeasts can invade hair follicles, causing folliculitis, which presents as small, itchy bumps around hair follicles. [11]
Investigations
Investigations for Pityriasis Versicolor:
Pityriasis versicolor is often diagnosed clinically based on its characteristic appearance and distribution. However, certain investigations can help confirm the diagnosis and rule out other conditions.
Wood’s Lamp Examination:
- A Wood’s lamp emits ultraviolet light, which causes the lesions of pityriasis versicolor to fluoresce.
- Hypopigmented lesions typically show a yellow-green fluorescence, while hyperpigmented lesions may exhibit a dull brown or copper-orange fluorescence.
- This is a quick and non-invasive test that can aid in diagnosis, especially in cases where the clinical presentation is atypical.
Potassium Hydroxide (KOH) Preparation:
- Skin scrapings from the affected area are placed on a slide with a drop of KOH solution.
- KOH dissolves the keratin in the skin cells, making the fungal elements more visible under a microscope.
- The presence of short, curved hyphae and clusters of round yeast cells ("spaghetti and meatballs" appearance) is characteristic of Malassezia species and confirms the diagnosis of pityriasis versicolor.
Fungal Culture:
- Although not routinely performed, a fungal culture can be done to identify the specific species of Malassezia causing the infection.
- This may be helpful in cases of treatment failure or recurrent infections.
Skin Biopsy:
- A skin biopsy is rarely needed for diagnosing pityriasis versicolor.
- However, it may be considered in atypical cases or when other conditions are suspected.
- Histopathological examination will show hyperkeratosis, mild acanthosis, and the presence of yeast and hyphae in the stratum corneum. [12]
Treatment
Treatment of Pityriasis Versicolor
Any of the following may be used locally:
1.Topical therapy –
- Sodium thiosulphate – in a 20 per cent solution
- applied, allowed to dry also left in place before
- rinsing, for 5–7 days.
- Ketoconazole 2% shampoo applied to the skin, allowed to dry and left on overnight as a single dose or daily for 3-day dose or daily for 3 days.
- Selenium sulphide – 2.5% as shampoo applied to [1]
- the skin for 5–10 minutes once daily for 3–4 weeks
- before bath.
- Either Antifungal creams or solutions including imida
- zoles, tolnaftate.
- Zinc pyrithione shampoo applied for 5 minutes
- daily for –2 weeks.
- Keratolytic either creams or lotions.
- Retinoic acid cream.
2. Systemic therapy –
Oral antifungals, e.g., ketoconazole 200 mg OD × 14 days or Fluconazole 200 mg OD × 10 days if persistent or recurrent.[1]
Prevention
Prevention of Pityriasis Versicolor:
Pityriasis versicolor tends to recur, especially in hot and humid climates. However, certain preventive measures can help reduce the frequency and severity of recurrences.
Maintain Good Skin Hygiene:
- Shower regularly, especially after sweating.
- Use a mild soap or cleanser and avoid harsh scrubbing.
- Dry the skin thoroughly, paying attention to skin folds and areas prone to moisture accumulation.
Avoid Excessive Sweating:
- Wear loose-fitting, breathable clothing.
- Avoid activities that cause excessive sweating, especially during hot and humid weather.
Use Anti-Fungal Cleansers:
- Consider using an anti-fungal cleanser, such as one containing ketoconazole or selenium sulfide, once or twice a week on areas prone to infection.
- This can help reduce the yeast population on the skin and prevent recurrence.
Avoid Oily Skin Products:
- Limit the use of oily lotions, creams, and cosmetics, especially on areas prone to infection.
- These products can create a favorable environment for yeast growth.
Consider Prophylactic Treatment:
- In individuals with frequent recurrences, a dermatologist may recommend prophylactic treatment during warm months or periods of high humidity.
- This may involve using an anti-fungal shampoo or body wash once or twice a month or taking oral anti-fungal medication for a short duration. [12]
Homeopathic Treatment
Homeopathic Treatment of Pityriasis Versicolor
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Pityriasis (Tinea) Versicolor:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
Arsenic Alb
- Itching, burning, swellings, Oedema.
- Eruption, papular, dry, rough, scaly.
- Worse cold also scratching. Additionally, Malignant pustules.
- Ulcers with offensive discharge. Anthrax. Poisoned wounds. In detail; Urticaria, with burning and restlessness. Psoriasis. Scirrhous.
- Besides this, Icy coldness of body. Epithelioma of the skin. All in all, Gangrenous inflammations.[4]
Ars-iod
- Basically, Dry, scaly, itching, marked exfoliation of skin in large scales, leaving a raw exuding surface beneath, ichthyosis.
- Furthermore, Enlarged scrofulous glands, venereal bubo. In detail, Debilitating night- sweats.
- Eczema of the beard; watery, oozing, itching; worse, washing. Additionally, Emaciation. Psoriasis.
- Acne hard, shotty, indurated base with pustule at apex.
Bacillinum for Pityriasis Versicolor
- Ringworm, pityriasis. Eczema of eyelids. Glands of neck enlarged also tender Bacillinum is especially indicated for lungs of old people.
- Chronic catarrhal condition also enfeebled pulmonary circulation, attacks of suffocation at night with difficult cough. Suffocative catarrh.
- Tubercular meningitis. Additionally, Favors falling off of tartar of teeth. Constant disposition to take cold.
Calcarea carb
- Unhealthy; readily ulcerating; flaccid. Small wounds do not heal readily. Glands swollen.
- Nettle rash; better especially, in cold air. Warts on face and hands. Petechial eruptions, Chilblains.
- Boils Great sensitiveness to cold; partial sweats. In detail, Children crave eggs and eat dirt and other indigestible things; are prone to diarrhoea.
- Calcarea patient is fat, fair, flabby and perspiring and cold, damp and sour.[4]
Kali-sulph
- Psoriasis, Eczema; burning, itching, papular eruption. Nettle-rash. Polypi. Epithelioma. Seborrhea. Favus.
- Furthermore, Ring-worm of scalp or beard with abundant scales.
Mezereum
- Eczema; intolerable itching, chilliness with pruritus; worse specifically in bed. Ulcers itch and burn, surrounded by vesicles and shining, fiery-red areola. Zona, with burning pain.
- Bones especially long bones, inflamed also swollen; caries, exostosis; pain worse night, touch, damp weather.
- Eruption ulcerates and form thick scabs under which purulent matter exudes.[4]
Psorinum for Pityriasis Versicolor
- Dirty, dingy look, Dry, lusterless, rough hair, intolerable itching.
- Herpetic eruptions, especially on scalp and bends of joints with itching; worse, from warmth of bed. Enlarged glands.
- Sebaceous glands secrete excessively; oily skin.
- Indolent ulcers, slow to heal Eczema behind ears.
- Crusty eruptions all over.
- Urticaria especially after every exertion. Lastly, Pustules near finger- nails
Sepia
- Herpes circinate in isolated spots.
- Itching; not relieved by scratching; worse especially in bends of elbows and knees.
- Moreover, Chloasma; herpetic eruption on lips, about mouth and nose.
- Ringworm-like eruption every spring.
- Urticaria on going in open air; better in warm room. Hyperhidrosis also bromidrosis.
- Sweat on feet, worse on toes; intolerable odor.
- All in all, Lentigo in young women. Ichthyosis with offensive odor of skin.[4]
Silicea
- people who have been incarcerated, abscess, boils, old fistulous ulcers.
- Delicate, pale, waxy. Cracks at ends of fingers. Additionally, Painless swelling of glands. Rose-colored blotches.
- Scars suddenly become painful. Pus offensive.
- Moreover, Promotes expulsion of foreign bodies from tissues, every little injury suppurates. Long lasting suppuration also fistulous tracts. Dry finger tips.
- Eruptions itch only in daytime and evening.
- Besides this, is physically disabled nails.
- Indurated tumors, Abscesses of joints, After impure vaccination. Bursa. Lepra, nodes, also coppery spots.
- Keloid growths.
Sulphur for Pityriasis Versicolor
- Dry, scaly, unhealthy, every little injury suppurates, Freckles.
- Itching, burning, worse scratching also washing.
- Pimply eruption, pustules, rhagades, hang-nails.
- Excoriation, especially in folds.
- Feeling of a band around bones. Skin affections after local medication.
- Pruritus, especially from warmth, in evening, often recurs in spring-time, in damp weather.
Tellurium
- Itching of hands and feet.
- Herpetic spots; ringworm, ring-shape lesion, offensive odors from affected parts.
- Barber’s itch. Stinging especially, in skin.
- Fetid exhalation.
- Offensive foot-sweat. Eczema, back of ears and occiput. Circular patches of eczema.[4]
Thuja
- Polyp, tubercles, warts epithelioma, naevi, carbuncles; ulcers, especially in ano-genital region.
- Freckles and blotches. Perspiration sweetish, also strong.
- Dry skin, with brown spots. Besides this, Zona; herpetic eruptions.
- Tearing pains in glands. Glandular enlargement.
- Nails is physically disabled ; brittle also soft.
- Eruption only on covered parts, worse after scratching.
- Very sensitive to touch. In detail, Coldness of one side.
- Sarcoma; polypi, brown spots on hands also arms.[4]
Diet & Regimen
Diet & Regimen
Diet:
- Boost Your Immune System: A healthy immune system can help keep the fungus that causes pityriasis versicolor in check. Focus on:
- Fruits and vegetables rich in antioxidants (berries, leafy greens, citrus fruits).
- Probiotic-rich foods like yogurt and kefir to support gut health.
- Foods high in Vitamin D (fatty fish, eggs, fortified foods) as Vitamin D plays a role in immunity.
- Manage Blood Sugar: Some studies suggest that managing blood sugar levels may be helpful. Limit sugary drinks and refined carbohydrates.
Regimen:
- Keep Skin Clean and Dry:
- Shower regularly, especially after sweating.
- Dry your skin thoroughly, paying attention to areas prone to the rash.
- Avoid tight-fitting clothing that traps moisture.
- Opt for breathable fabrics like cotton.
- Sun Exposure (with caution):
- Limited sun exposure may help improve the appearance of the rash, but always use sunscreen to protect your skin from damage.
- Manage Stress:
- Stress can sometimes worsen skin conditions. Practice stress-management techniques like exercise, yoga, or meditation.
- Boost Your Immune System: A healthy immune system can help keep the fungus that causes pityriasis versicolor in check. Focus on:
Do’s and Don'ts
The Do’s & Don’ts
Do’s
- Maintain good skin hygiene: Shower regularly, especially after sweating. Use a mild soap or cleanser and dry your skin thoroughly.
- Wear loose-fitting, breathable clothing: Avoid tight-fitting clothes and synthetic fabrics that can trap moisture and heat.
- Use anti-fungal cleansers or shampoos: These can help reduce the yeast population on your skin and prevent recurrences. Use them as directed by your dermatologist.
- Follow your dermatologist’s treatment plan: Use prescribed medications as directed and complete the full course of treatment even if your symptoms improve.
- Protect your skin from the sun: Use sunscreen with a high SPF to prevent sunburn and further discoloration of the affected areas.
- Be patient: It may take several weeks or even months for the skin discoloration to fade completely after successful treatment.
Don’ts
- Don’t scratch or pick at the lesions: This can lead to secondary bacterial infections and worsen the discoloration.
- Don’t use oily skin products: Avoid lotions, creams, and cosmetics that can trap moisture and create a favorable environment for yeast growth.
- Don’t share personal items: Avoid sharing towels, clothing, or other items that come into contact with your skin to prevent spreading the infection to others.
- Don’t self-diagnose or self-treat: If you suspect you have pityriasis versicolor, consult a dermatologist for proper diagnosis and treatment.
- Don’t get discouraged by recurrences: Pityriasis versicolor can recur, especially in hot and humid climates. Talk to your dermatologist about preventive measures and long-term management options.
Terminology
Terminology
- Pityriasis Versicolor: A common fungal infection of the skin that causes patches of discolored skin.
- Malassezia: A type of yeast that is naturally found on the skin but can overgrow and cause pityriasis versicolor.
- Hypopigmented: Patches of skin that are lighter than the surrounding skin.
- Hyperpigmented: Patches of skin that are darker than the surrounding skin.
- Macules: Flat, discolored spots on the skin.
- Scaling: The shedding of dead skin cells, which can occur in pityriasis versicolor.
- Pruritus: Itching.
- Wood’s Lamp: A special light used to examine the skin for certain conditions, including pityriasis versicolor.
- KOH Preparation: A test in which skin scrapings are mixed with potassium hydroxide to visualize fungal elements under a microscope.
Additional Terms:
- Topical Antifungals: Medications applied to the skin to treat fungal infections.
- Oral Antifungals: Medications taken by mouth to treat fungal infections.
- Recurrence: The return of pityriasis versicolor after treatment.
- Commensal: An organism that lives on or in another organism without causing harm.
- Lipophilic: Having an affinity for or an attraction to fat and oils.
- Tyrosinase: An enzyme involved in the production of melanin, the pigment that gives skin its color.
- Azelaic Acid: A naturally occurring acid that can inhibit tyrosinase and has antifungal properties.
- Keratin: A protein that forms the main structural component of the outer layer of skin, hair, and nails.
Commonly used homeopathic remedies for Pityriasis Versicolor:
Sulphur: Often indicated when there’s a history of skin conditions, burning sensations, and a tendency for skin infections.
Sepia: May be helpful for individuals with hormonal imbalances, irregular menses, and a sense of indifference.
Thuja: Often considered when there’s a history of warts, fungal infections, and a sense of suppressed emotions.
Arsenicum album: May be useful for individuals with anxiety, restlessness, and sensitivity to cold.
Natrum muriaticum: Considered when there’s a history of emotional suppression, dryness of skin, and cracking.
References
References use for Article Pityriasis Versicolor
- Text book of medicine by Golwala
- https://www.lybrate.com/topic/homeopathic-treatment-of-tinea-versicolor/7eeacbe36cbf4c4735b51d410a226266
- Materia Medica by Boericke W.
- https://www.ncbi.nlm.nih.gov/books/NBK482500/#:~:text=Pityriasis%20versicolor%2C%20also%20known%20as,%2C%20neck%2C%20and%20proximal%20extremities.
- https://my.clevelandclinic.org/
- International Journal of Dermatology, Venereology and Leprology in 2014
- The Indian Journal of Dermatology, Venereology and Leprology in 2021
- The Annals of Indian Academy of Medical and Dental Sciences in 2023
- Fitzpatrick’s Dermatology in General Medicine, 9th Edition, by Klaus Wolff, Lowell A. Goldsmith, Stephen I. Katz, Barbara A. Gilchrest, Amy S. Paller, David J. Leffell, Published by McGraw Hill Professional in 2019
- Andrews’ Diseases of the Skin: Clinical Dermatology (13th Edition), by William D. James, Timothy G. Berger, Dirk M. Elston, 2020, Published by Elsevier
- Bolognia JL, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
Also Search As
Also Search As
There are several effective ways to search for homeopathic articles on Pityriasis Versicolor:
1. Utilize Search Engines:
Specific search terms:
Use search engines like Google, DuckDuckGo, etc., with targeted keywords like:
- "homeopathic treatment for pityriasis versicolor"
- "homeopathy for tinea versicolor"
- "homeopathic remedies for pityriasis versicolor"
- "case studies homeopathy pityriasis versicolor"
Advanced search options:
Use advanced search operators to refine your search:
- Use quotation marks for exact phrases, e.g., "pityriasis versicolor homeopathy"
- Use the minus sign to exclude terms, e.g., "pityriasis versicolor -conventional treatment"
2. Explore Homeopathic Journals & Databases:
Online Journals:
Search within online journals dedicated to homeopathy, such as:
- The American Journal of Homeopathic Medicine
- The European Journal of Integrative Medicine
- Homeopathy
- Indian Journal of Research in Homeopathy
Homeopathic Databases:
Utilize specialized databases that index homeopathic literature, such as:
- HomBRex
- RadarOpus
3. Visit Homeopathic Websites & Blogs:
Reputable Homeopathic Organizations:
Explore the websites of well-known homeopathic organizations for articles and resources.
Homeopathic Blogs:
Search for blogs run by experienced homeopaths that focus on skin conditions or specific remedies.
4. Consult Homeopathic Libraries & Practitioners:
Homeopathic Libraries:
Visit libraries with a collection of homeopathic books and journals.
Homeopathic Practitioners:
Ask a qualified homeopath for recommendations on relevant articles and research.
There are a number of ways to search for information about Pityriasis Versicolor:
1. Using Search Engines:
Keywords:
The most straightforward approach is to use a search engine like Google, Bing, or DuckDuckGo. You can use a variety of search terms, such as:
- Pityriasis Versicolor
- Tinea Versicolor (an older, but still commonly used term)
- Skin discoloration
- Fungal skin infection
Specific Queries:
If you are looking for specific information, you can add more targeted terms to your search. For example:
- "Pityriasis Versicolor treatment"
- "Pityriasis Versicolor causes"
- "Pityriasis Versicolor home remedies"
- "Pityriasis Versicolor images"
2. Medical Websites and Databases:
Reputable Medical Websites:
Many websites provide reliable medical information, including information on Pityriasis Versicolor. Some popular options include:
- Mayo Clinic
- Cleveland Clinic
- WebMD
- MedlinePlus
- National Institutes of Health (NIH)
Medical Databases:
If you are looking for more in-depth or scientific information, you can search medical databases such as PubMed or Google Scholar.
3. Social Media & Online Communities:
Social Media Platforms:
This platforms like Facebook, Instagram, and Twitter can be a source of information and support. You can search for relevant hashtags (#pityriasisversicolor, #tineaversicolor) or join online communities and support groups.
Online Forums:
There are also online forums and communities dedicated to skin conditions, where you can connect with other people who have Pityriasis Versicolor and share experiences.
4. Books and Libraries:
Medical Textbooks:
If you prefer traditional resources, you can find information about Pityriasis Versicolor in medical textbooks and dermatology books.
Libraries:
Local libraries may have a selection of medical books or access to online medical databases that you can use for your research.
5. Consult a Healthcare Professional:
Dermatologist:
If you have concerns about Pityriasis Versicolor or any other skin condition, it is always best to consult a dermatologist for proper diagnosis and treatment recommendations.
Frequently Asked Questions (FAQ)
What is Pityriasis Versicolor?
Definition
Pityriasis Versicolor is the most superficial fungus infection produced by Malassezia furfur, characterized by scaly white or brown patches, asymptomatic in nature.
What causes Pityriasis Versicolor?
- Hormonal changes
- Weakened immune system
- Hot, humid weather
- Sweating
- Oily skin
Is Pityriasis Versicolor contagious?
No, it’s not contagious. You can’t catch it from someone else or spread it to others.
How is Pityriasis Versicolor treated?
Treatment options include antifungal creams, lotions, shampoos, or oral medications. The specific treatment will depend on the severity and extent of the infection.
What are the symptoms of Pityriasis Versicolor?
Symptoms
- Asymptomatic macules and patches of various sizes and shapes, yellow, white or brown in color.
Can homeopathy cure Pityriasis Versicolor?
Homeopathy aims to stimulate the body’s self-healing abilities to address the underlying imbalances that may contribute to Pityriasis Versicolor.
While some individuals report positive outcomes with homeopathic treatment, more research is needed to establish its definitive efficacy.
Is homeopathic treatment safe for everyone with Pityriasis Versicolor?
Homeopathic remedies are generally considered safe when prescribed by a qualified practitioner.
However, pregnant or breastfeeding women, individuals with severe medical conditions, and those taking medications should consult their healthcare provider before starting any new treatment, including homeopathy.
How long does homeopathic treatment take to work for Pityriasis Versicolor?
The response to homeopathic treatment can vary. Some individuals may experience improvement within a few weeks, while others may require a longer duration of treatment.
Can homeopathy be used alongside conventional treatments for Pityriasis Versicolor?
Yes, homeopathy can be used as a complementary approach alongside conventional treatments. It’s crucial to inform your healthcare providers about all therapies you’re using to ensure safety and avoid potential interactions.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Pityriasis Versicolor?
Homoeopathic medicines for Pityriasis Versicolor
- Arsenic Alb
- Ars-iod
- Bacillinum
- Calcarea carb
- Kali-sulph
- Mezereum
- Psorinum
