Acute Pancreatitis
Definition
Acute Pancreatitis, refers to inflammation of the pancreas, occurs in acute and chronic forms and may be due to edema, necrosis, or haemorrhage. In men this disease commonly associated with alcoholism, trauma, or peptic ulcer; in women, it’s linked to biliary tract disease. The prognosis is good when pancreatitis follows biliary tract disease, but poor when it follows alcoholism.[1]
Acute pancreatitis doesn’t have perfect synonyms in the sense of a single word conveying the exact meaning. However, depending on the context, here are some options you can consider:
Acute pancreatic inflammation:
This directly translates the medical term and clarifies the nature of the condition.
Acute pancreatic necrosis (less common):
This refers to a more severe form of acute pancreatitis where pancreatic tissue death occurs.
It’s important to note that "acute pancreatic necrosis" is not a perfect synonym as it describes a specific complication of acute pancreatitis, not the condition itself.
For most contexts, "acute pancreatitis" remains the clearest and most accurate term.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do's & Don'ts
Terminology
References
Also Search As
Overview
Overview of Acute pancreatitis
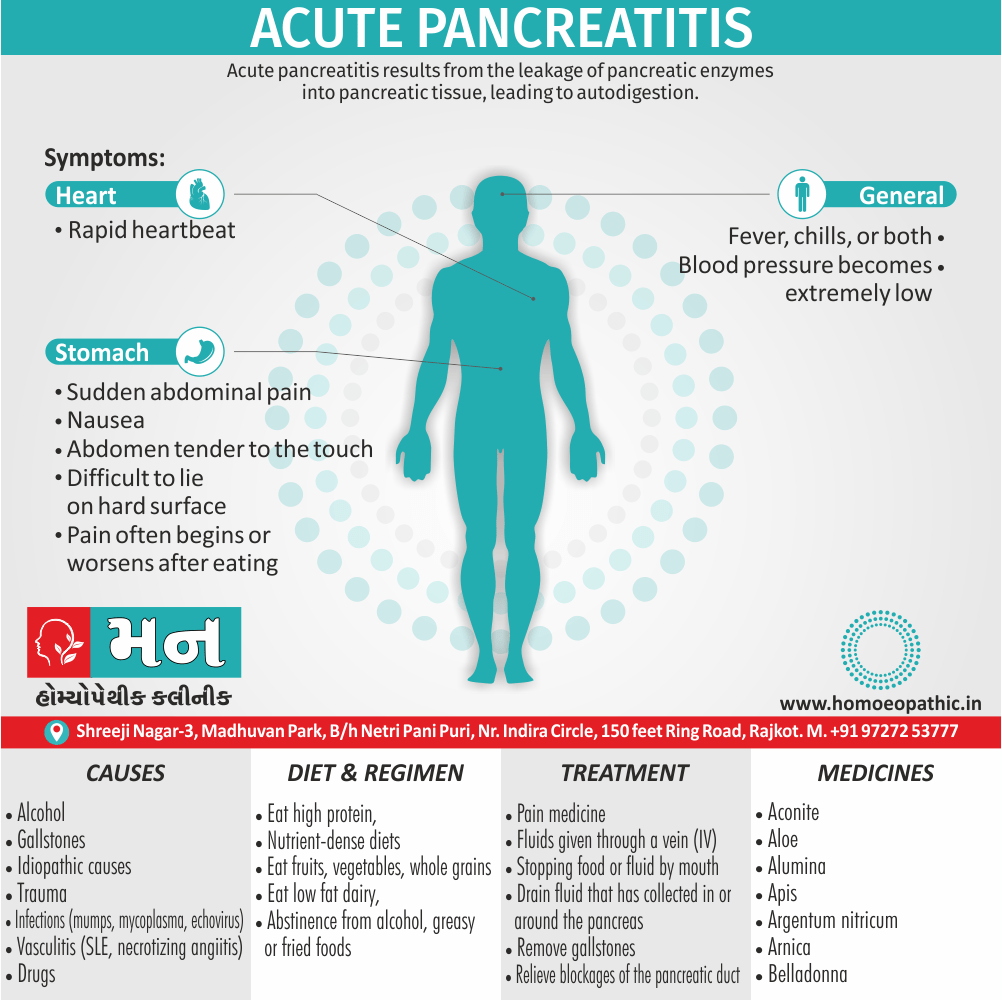
- Acute pancreatitis results from the leakage of pancreatic enzymes into pancreatic tissue, leading to auto digestion. Because acute pancreatitis is particularly, more common than chronic pancreatitis.
- Acute pancreatitis can have severe complications and high mortality despite treatment. While mild cases are often successfully treated with conservative measures.[2]
Epidemiology
Epidemiology
The epidemiology of acute pancreatitis (AP) in India is characterized by diverse etiological factors, regional variations, and evolving trends. Several studies have explored the prevalence, clinical profiles, and etiological factors associated with AP in the Indian population.
1.Prevalence, Clinical and Etiological Profile of Acute Pancreatitis in India: A Single Center Study (ResearchGate, no year specified) This study examined the prevalence, clinical characteristics, and etiologies of AP in a single center in India. The most common etiological factors were gallstones, alcohol, and idiopathic causes.
2.(PDF) Demographic profile of Acute Pancreatitis in Eastern India: A Single Centre Experience (ResearchGate, 2017) This study assessed the etiological risk factors and demographic profile of AP in Eastern India. The most common etiology was alcohol consumption, followed by idiopathic causes and obstructive causes.
3.Acute pancreatitis, Chronic pancreatitis. (Indian Pediatrics, 2004) This study focused on the profile of pancreatic disorders in children in India. It found that acute pancreatitis was the most common pancreatic disorder in children, with diverse etiological factors.
4.Changing Trends in the Epidemiology of Pancreatitis in Rural Population: Study at a Tertiary Health Care Centre (Journal of Medical Science and Clinical Research, 2017) This study examined the changing trends in the epidemiology of pancreatitis in a rural population in India. It highlighted the increasing prevalence of AP and the need for further research to understand the regional variations in etiological factors.
These studies collectively provide valuable insights into the epidemiology of acute pancreatitis in India. However, it’s important to note that the data may not be fully representative of the entire Indian population due to variations in study designs, settings, and sample sizes. Further research is needed to comprehensively understand the epidemiology of AP in India and to develop effective prevention and management strategies.
Causes
Causes of Acute Pancreatitis
Common causes such as:
- Alcohol
- Gallstones
- Idiopathic causes
Uncommon causes
Post operative causes like:
- After endoscopic retrograde cholangiopancreatography
- Trauma
- Metabolic causes ( for instance renal failure, hyperparathyroidism, acute fatty liver of pregnancy)
- Hereditary causes
- Infections ( such as mumps, mycoplasma, echovirus)
- Vasculitis (SLE, necrotizing angilitis)
- Ampulla of vater obstruction ( for example Crohn’s disease, duodenal diverticulitis, penetrating duodenal ulcer)
- Drugs
- Hypotension may be present in as many as half of the patients; it results from vasodilatation, myocardial depressant factor, also the loss of plasma and blood in to the retro-peritoneum. [1]
Types
Types of Pancreatitis
There are mainly two types that is;
- Acute
- Chronic
Risk Factors
Risk Factors
- Excessive alcohol consumption. Research shows that heavy alcohol users (people who consume four to five drinks a day) are at increased risk of pancreatitis.
- Cigarette smoking. Smokers are on average three times more likely to develop chronic pancreatitis, compared with nonsmokers. The good news is quitting smoking decreases your risk by about half.
- Obesity. You’re more likely to get pancreatitis if you’re higher-weight person.
- Diabetes. Having diabetes increases your risk of pancreatitis.
- Family history of pancreatitis. The role of genetics is becoming increasingly recognized in chronic pancreatitis. If you have family members with the condition, your odds increase — especially when combined with other risk factors.[5]
Pathogenesis
Pathogenesis
Acute pancreatitis is an inflammatory condition of the pancreas characterized by varying degrees of pancreatic injury. Several mechanisms are implicated in its pathogenesis.
Obstruction of the Pancreatic Duct:
This can occur due to gallstones or other obstructive lesions. It leads to increased intraductal pressure, causing acinar cell injury and release of activated pancreatic enzymes.
Acinar Cell Injury:
This can be caused by various factors such as alcohol, drugs, ischemia, or trauma. The injured acinar cells release activated pancreatic enzymes, triggering autodigestion of the pancreas.
Defective Intracellular Transport:
This can disrupt the normal segregation of digestive enzymes from lysosomal hydrolases, leading to premature activation of trypsin within the acinar cells.
Impaired Secretion of Proenzymes:
This can result in the accumulation of activated enzymes within the pancreatic duct, leading to autodigestion.
Interstitial Edema and Inflammation:
The release of activated enzymes and inflammatory mediators into the interstitium leads to edema, necrosis, and inflammation of the pancreas.
Systemic Complications:
Severe cases of acute pancreatitis can lead to systemic inflammatory response syndrome (SIRS), acute respiratory distress syndrome (ARDS), and multiorgan failure.[9]
Premature Activation of Trypsin:
This is a central event in acute pancreatitis. Trypsin activates other digestive enzymes, leading to autodigestion of the pancreas.
Intra-Acinar Activation of Enzymes:
This occurs due to various factors such as increased intracellular calcium, decreased ATP levels, and co-localization of lysosomal enzymes with digestive enzymes.
Microvascular Injury and Ischemia:
This can contribute to acinar cell injury and release of inflammatory mediators, exacerbating the inflammatory response.
Leukocyte Activation and Inflammation:
Activated leukocytes release cytokines and other inflammatory mediators, contributing to the systemic inflammatory response.[10]
Toxic-Metabolic Injury:
This can be caused by alcohol, drugs, or hypertriglyceridemia. These factors can induce acinar cell injury and trigger the inflammatory cascade.
Genetic Predisposition:
Certain genetic mutations can increase the risk of acute pancreatitis, such as mutations in the cationic trypsinogen gene (PRSS1).
Infectious Agents:
Certain viruses and bacteria can infect the pancreas and trigger an inflammatory response.[11]
These references provide a comprehensive overview of the complex pathogenesis of acute pancreatitis. Understanding the underlying mechanisms is crucial for developing effective diagnostic and therapeutic strategies.
Pathophysiology
Pathophysiology of Acute Pancreatitis
The pathophysiology of acute pancreatitis is characterized by a loss of intracellular and extracellular compartmentation, by an obstruction of pancreatic secretory transport and by an activation of pancreatic enzymes. In biliary acute pancreatitis, outflow obstruction with pancreatic duct hypertension and a toxic effect of bile salts contribute to disruption of pancreatic ductules, with subsequent loss of extracellular compartmentation.
Alcohol induces functional alterations of plasma membranes and alters the balance between proteolytic enzymes and protease inhibitors, thus triggering enzyme activation, autodigestion and cell destruction. Once the disease has been initiated, the appearance of interstitial edema and inflammatory infiltration are the basic features of acute pancreatitis.
Accumulation of polymorphonuclear granulocytes
The accumulation of polymorphonuclear granulocytes in pancreatic and extrapancreatic tissue, and the release of leukocyte enzymes play an essential role in the further progression of the disease and in the development of systemic complications. Activation of different cascade systems by proteolytic activity, and consumption of alpha 2-macroglobulin further characterize the severe clinical course of acute pancreatitis.[6]
Clinical Features
Clinical Features
- Abdominal pain: This is the cardinal symptom of acute pancreatitis, typically located in the epigastrium or left upper quadrant, often radiating to the back. The pain is usually severe, constant, and worsened by lying supine or eating.
- Nausea and vomiting: These are common accompanying symptoms, often persistent and not relieved by vomiting.
- Fever and tachycardia: These reflect the systemic inflammatory response associated with acute pancreatitis.
- Abdominal tenderness and guarding: Physical examination reveals tenderness and guarding, often with decreased bowel sounds.
- Cullen’s sign and Grey Turner’s sign: These are bluish discoloration around the umbilicus and flanks, respectively, indicating hemorrhagic pancreatitis.
- Hypotension and shock: In severe cases, acute pancreatitis can lead to hypotension and shock due to systemic inflammation and fluid sequestration.[10]
- Abdominal distention: This can occur due to ileus or pancreatic pseudocyst formation.
- Jaundice: This can be present if the common bile duct is obstructed by gallstones or inflammation.
- Pleural effusion: This can occur due to the release of inflammatory mediators and pancreatic enzymes into the pleural space.
- Respiratory distress: Severe cases can lead to acute respiratory distress syndrome (ARDS).
- Renal failure: This can occur due to hypovolemia, shock, or direct toxic effects of pancreatic enzymes on the kidneys.[11]
- Tachycardia and tachypnea: These reflect the systemic inflammatory response and pain.
- Dehydration: This can occur due to vomiting and fluid sequestration in the inflamed pancreas.
- Mental status changes: Severe cases can lead to confusion or encephalopathy due to electrolyte imbalances and organ dysfunction.
- Elevated serum amylase and lipase: These are the most common laboratory abnormalities in acute pancreatitis.
- Imaging findings: Abdominal ultrasound or CT scan can reveal pancreatic inflammation, edema, necrosis, or pseudocyst formation.
Sign & Symptoms
Sign & Symptoms
The most common symptom of acute pancreatitis is pain. Almost everybody with acute pancreatitis experiences pain.
Quality of Pain
- Pain may come on suddenly or build up gradually. If the pain begins suddenly, it is typically very severe. If the pain builds up gradually, it starts out mild but may become severe.
- The pain is usually centered in the upper middle or upper left part of the belly (abdomen). A pain is often described as if it radiates from the front of the abdomen through to the back.
- The pain often begins or worsens after eating.
- After that, Pain typically lasts a few days.
- The pain may feel worse when a person lies flat on his or her back.
People with acute pancreatitis usually feel very sick. Besides pain, people may have other symptoms and signs.
- Nausea (Some people do vomit, but vomiting does not relieve the symptoms.)
- Fever, chills, or both
- Swollen abdomen which is tender to the touch
- Rapid heartbeat (A rapid heartbeat may be due to the pain and fever, dehydration from vomiting and not eating, or it may be a compensation mechanism if a person is bleeding internally.)
In very severe cases with either infection or bleeding, a person may become dehydrated and have low blood pressure.
If the blood pressure becomes extremely low, the organs of the body do not get enough blood to carry out their normal functions. Hence, This very dangerous condition is called circulatory shock and is referred to simply as shock. [1]
Clinical Examination
Clinical Examination
The physical examination findings may be normal or reveal fever, hypotension, tachycardia, tachypnea, or diaphoresis. Abdominal examination typically reveals notable tenderness to palpation, guarding, also possible signs of peritoneal irritation, distension, or rigidity. Bowel sounds are typically decreased. Additionally, Jaundice may be present. In severe disease, patients may present with altered mental status. Overall, history also physical examination have moderate accuracy, especially when findings are abnormal (positive likelihood ratio [LR+] = 3.2; negative likelihood ratio [LR–] = 0.8).9 Two physical signs associated with pancreatitis are Cullen sign (ecchymosis and edema in the subcutaneous tissue around the umbilicus) and Grey Turner sign (ecchymosis of the flank).[7]
Diagnosis
Diagnosis of Acute Pancreatitis
Once a working diagnosis of acute pancreatitis is reached, laboratory tests are obtained to support the clinical impression. In addition to confirming the diagnosis, laboratory tests are helpful in defining an etiology and looking for complications.
Serum amylase and lipase levels
They are typically elevated in persons with acute pancreatitis. Serum amylase determinations are routinely available, but they are not specific for pancreatitis.
Lipase has a slightly longer half-life and abnormalities may support the diagnosis if a delay occurs between the pain episode also the time the patient seeks medical attention.
Elevated lipase levels are more specific to the pancreas than elevated amylase levels. The level of serum amylase or lipase does not indicate whether the disease is mild, moderate, or severe, and monitoring levels serially during the course of hospitalization does not offer insight into prognosis.
blood urea nitrogen
Obtain measurements for blood urea nitrogen (BUN), creatine, and electrolytes; a great disturbance in the electrolyte balance usually found, secondary to third spacing of fluids. Measure blood glucose level because it may be elevated from B-cell injury in the pancreas.
Measure calcium, cholesterol, and triglyceride levels to search for an etiology of pancreatitis (such as; hypercalcemia or hyperlipidemia) or complications of pancreatitis (for example, hypocalcemia resulting from saponification of fats in the retroperitoneum).
A complete blood count (CBC) demonstrates leukocytosis (white blood cell (WBC) count higher than 12,000/µL) with the differential being shifted toward the segmented polymorphonuclear (PMN) cells. Leukocytosis may represent inflammation or infection.
Abdominal radiographs have a limited role in acute pancreatitis.
Ultrasonography of the abdomen is the most useful initial test in determining the etiology of pancreatitis and is the technique of choice for detecting gallstones. Although ultrasonography can be used as a screening test, it may not be specific if overlying gas shadows secondary to bowel distention are present. Ultrasonography cannot measure the severity of disease.
CT is an important common initial assessment tool for acute pancreatitis.
Imaging is indicated during the initial presentation if i.e.:
- The diagnosis of acute pancreatitis is uncertain
- There is abdominal distension also tenderness, fever>102, or leukocytosis
- But Not improvement after 72 hours of conservative medical therapy
- There has been an acute change in status: fever, pain, or shock
While CT considered the gold standard in diagnostic imaging for acute pancreatitis, magnetic resonance imaging (MRI) has become increasingly valuable as a tool for the visualization of the pancreas, particularly of pancreatic fluid collections and necrotized debris. Additional utility of MRI includes its indication for imaging of patients with an allergy to CT’s contrast material, and an overall greater sensitivity to hemorrhage, vascular complications, pseudoaneurysms, also venous thrombosis. [1]
Differential Diagnosis
Differential Diagnosis
It include but is not limited to the following i.e.:
- Peptic ulcer disease
- Cholangitis
- Cholecystitis
- Bowel perforation
- Bowel obstruction
- Mesenteric ischemia
- Acute hepatitis
- Diabetic ketoacidosis
- Basilar pneumonia
- Myocardial infarction
- Renal colic
- Aortic dissection[5]
Complications
Complications
Local Complications:
- Pancreatic pseudocysts: Collections of pancreatic juice enclosed by a wall of fibrous or granulation tissue.
- Pancreatic necrosis: Localized areas of dead pancreatic tissue, which can become infected.
- Pancreatic abscess: A localized collection of pus within the pancreas.
- Pancreatic ascites: Leakage of pancreatic fluid into the peritoneal cavity.
- Pancreatic fistula: An abnormal connection between the pancreas and another organ or the skin.
Systemic Complications:
- Systemic inflammatory response syndrome (SIRS): A systemic inflammatory response to severe pancreatitis.
- Acute respiratory distress syndrome (ARDS): A life-threatening lung condition caused by inflammation and fluid accumulation in the lungs.
- Acute kidney injury (AKI): A sudden decrease in kidney function due to decreased blood flow to the kidneys or direct toxic effects of pancreatic enzymes.
- Gastrointestinal bleeding: Caused by stress ulcers or erosion of blood vessels by pancreatic enzymes.
- Disseminated intravascular coagulation (DIC): A serious condition in which blood clots form throughout the body, leading to bleeding and organ damage.[10]
Local Complications:
- Peripancreatic fluid collections: Collections of fluid in the tissues surrounding the pancreas.
- Walled-off necrosis: A collection of necrotic pancreatic tissue surrounded by a wall of fibrous tissue.
- Pleural effusion: Accumulation of fluid in the pleural space (the space between the lungs and the chest wall).
Systemic Complications:
- Cardiovascular complications: Such as hypotension, shock, and arrhythmias.
- Neurologic complications: Such as encephalopathy and seizures.
- Endocrine complications: Such as hyperglycemia and diabetes mellitus.[11]
Local Complications:
- Pancreatic hemorrhage: Bleeding into or around the pancreas.
- Splenic vein thrombosis: Formation of a blood clot in the splenic vein, which can lead to splenomegaly and variceal bleeding.
Systemic Complications:
- Multiorgan failure: Failure of multiple organs, such as the lungs, kidneys, liver, and heart.
- Sepsis: A life-threatening condition caused by the body’s response to an infection.[12]
Please note that the complications of acute pancreatitis can vary in severity and depend on the underlying cause and the extent of pancreatic damage. Early recognition and prompt management of complications are crucial for improving outcomes in patients with acute pancreatitis.
Investigations
Investigation of Acute Pancreatitis
- Firstly, Elevated serum amylase and lipase are the hallmarks of acute pancreatitis.
- Secondly, Other findings may include leucocytosis, hypoalbuminemia, hyperglycaemia, and elevated aspartate aminotransferase (AST, serum glutamate oxaloacetate transaminase (SGOT), alkaline phosphatase, and bilirubin. [2]
Treatment
Treatment of Acute Pancreatitis
Often Treatment requires a stay in the hospital and may involve i.e.:
- Medicines Pain
- Fluids given through a vein (IV)
- Stopping food or fluid by mouth to limit the activity of the pancreas
Occasionally a tube will inserted through the nose or mouth to remove the contents of the stomach (nasogastric suctioning). This may done if vomiting or severe pain do not improve, or if a paralyzed bowel (paralytic ileus) develops. The tube will stay in for 1 – 2 days to 1 – 2 weeks.
Treating the condition that caused the problem can prevent repeated attacks.
In some cases, therapy needed such as i.e.:
- Drain fluid that has either collected in or around the pancreas
- Remove gallstones
- Relieve blockages of the pancreatic duct
In the most severe cases, surgery is needed to remove either dead or infected pancreatic tissue.
Avoid smoking, alcoholic drinks, and a fatty food after the attack has improved. [1]
Prevention
Prevention of Acute Pancreatitis
You can reduce your risk of developing acute pancreatitis by cutting back on drinking alcohol. This helps to prevent your pancreas being damaged.
It’s recommended that you i.e.:
- don’t drink more than 14 units a week
- spread your drinking over 3 days or more if you drink as much as 14 units a week
A unit of alcohol is equal to about half a pint of normal-strength lager or a pub measure (25ml) of spirits. A small (125ml) glass of wine (ABV 12%) or an alcopop is 1.5 units.
Remember, if you’ve had acute pancreatitis caused by drinking too much alcohol, you should avoid it completely.[8]
Homeopathic Treatment
Homeopathic Treatment
Homeopath treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Acute Pancreatitis:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Aconite:
- When the pain has been caused by a chill.
Aloe:
- Flatulence; weak, as if diarrhoea would ensue. Soreness in sides. Over the liver, heat and pressure. Feeling of a plug in pelvis, between symphysis and coccyx, with urging. Additionally, General feeling of Fullness and heaviness.
Alumina:
- Seems to hang down, heavy, when walking (<) afternoon. Additionally, Sticking pains from below upward. Cutting pains (>) warmth. Lead colic.
- Soreness over the liver, extends to pit of stomach on stooping. Furthermore, Stitches in the region of inguinal ring (has relieved strangulated hernia); the pains extend up to the chest.
Apis:
- General soreness, aggravated by touch. Distention. Sharp, stinging pains, mostly extending upward.
Argentum nitricum:
- Flatulent distention. Flatulent pains, often sharp, followed specifically by evacuations of gas also green, fetid mucus. Pain around hypochondria.
Arnica:
- Distention, hard. Stitches in the region of the spleen, taking away the breath. Pains (after lifting). Colic, with retention of urine. Bruised pains in the sides of the abdomen. at last, Flatulence, extremely foul [4]
Belladona:
- Nausea; vomiting after eating also drinking. Heat, with burning, cutting pain in the region of the stomach. Extreme sensitiveness of the stomach to touch.
Mercurius:
- Flatulent distention of abdomen, with numerous pains. Intestines feel sore, (<) lying on right side. Inguinal glands swollen also inflamed, with shooting pains. Boring pains especially in the right groin.[4]
Diet & Regimen
Diet & Regimen
Acute Pancreatitis Diet
Foods to Avoid:
- High-fat foods: Fried foods, fatty meats, butter, cream, full-fat dairy
- Spicy foods: Can irritate the pancreas
- Alcohol: A major cause of pancreatitis, it should be avoided completely
- Sugary drinks: Can worsen inflammation
- Caffeine: May stimulate pancreatic secretions
Regimen for Acute Pancreatitis
- Pain management: Your doctor will likely prescribe pain medications to help manage the pain.
- Intravenous fluids: These are essential to prevent dehydration
- Rest: Adequate rest is important for recovery.
- Monitoring: Your doctor will monitor your condition closely, including blood tests and imaging studies.
- Treating underlying causes: If the pancreatitis is caused by gallstones or other factors, treatment will address those issues.
- High-fat foods: Fried foods, fatty meats, butter, cream, full-fat dairy
Do's & Don'ts
Do’s & Don’ts
Acute Pancreatitis Do’s & Don’ts
Do’s:
- Seek immediate medical attention if you experience severe abdominal pain, nausea, vomiting, or other symptoms suggestive of acute pancreatitis.
- Follow your doctor’s instructions regarding pain management, hydration, and nutrition.
- Rest and avoid strenuous activity during the acute phase of illness.
- Gradually resume a normal diet as tolerated, starting with clearliquids and progressing to a low-fat, easily digestible diet.
- Avoid alcohol and smoking, as these can worsen pancreatic inflammation and delay healing.
- Stay hydrated by drinking plenty of fluids, such as water, clear broth, or electrolyte solutions.
- If you are unable to tolerate oral fluids, you may require intravenous (IV) fluids.
- Manage pain with medications prescribed by your doctor.
- If you have gallstones, discuss with your doctor the possibility of cholecystectomy (surgical removal of the gallbladder) to prevent recurrent pancreatitis.
- If you have a history of alcohol abuse, seek help to quit drinking.
Don’ts:
- Do not ignore or self-treat severe abdominal pain.
- Do not eat or drink anything if you are experiencing nausea and vomiting.
- Do not consume alcohol or smoke during the recovery period.
- Do not take any medications without consulting your doctor, as some medications can worsen pancreatitis.[10]
- Do not eat a high-fat diet, as this can worsen pancreatic inflammation.
- Do not take medications that can irritate the pancreas, such as nonsteroidal anti-inflammatory drugs (NSAIDs).[11]
- Do not resume alcohol consumption after an episode of acute pancreatitis, as this can increase the risk of recurrence.[12]
Please note that these are general recommendations, and your doctor may provide you with specific instructions based on your individual case. It is important to follow your doctor’s advice and attend all follow-up appointments to monitor your recovery and prevent complications.
Terminology
Terminology
Medical Terms
- Acute Pancreatitis: Sudden inflammation of the pancreas.
- Edema: Swelling caused by fluid buildup in the body’s tissues.
- Necrosis: Death of tissue due to lack of blood supply, injury, or disease.
- Hemorrhage: Excessive bleeding.
- Autodigestion: The process where the pancreas’s own digestive enzymes begin to break down the organ itself.
- Biliary Tract Disease: Conditions affecting the gallbladder, bile ducts, and related structures.
- Etiology: The cause or origin of a disease.
- Pathogenesis: The development of a disease and the chain of events leading to that disease.
- Pathophysiology: The functional changes associated with or resulting from disease or injury.
- Leukocytosis: An elevated white blood cell count, often indicating infection or inflammation.
- Hypoalbuminemia: Low levels of albumin (a protein) in the blood.
- Hyperglycemia: High blood sugar levels.
- Aspartate Aminotransferase (AST): A liver enzyme; elevated levels can indicate liver damage, but it’s also found in other organs including the pancreas.
- Alkaline Phosphatase: An enzyme found in various tissues, including the liver and bones; elevated levels can indicate issues in these areas.
- Bilirubin: A yellowish substance produced during the breakdown of red blood cells; elevated levels can indicate liver or gallbladder problems.
- Miasmatic Tendency: A homeopathic concept referring to a person’s predisposition to certain types of diseases.
Other Key Terms
- Idiopathic: Of unknown cause.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): A procedure used to diagnose and treat problems in the liver, gallbladder, bile ducts, and pancreas.
- Vasculitis: Inflammation of blood vessels.
- Systemic Inflammatory Response Syndrome (SIRS): A serious condition related to inflammation throughout the body.
- Ascites: The accumulation of fluid in the peritoneal cavity (the space within the abdomen).
- Fistula: An abnormal connection between two organs or between an organ and the outside of the body.[13]
References
References use for Acute Pancreatitis
- Acute and Chronic Pancreatitis
- Acute pancreatitis Family Medicine Help
- https://columbiasurgery.org/pancreas/pancreatitis-diet#:~:text=To%20best%20achieve%20those%20goals,to%20prevent%20malnutrition%20and%20pain.
- A Primer of Materia Medica by T. F. Allen.
- https://www.mayoclinic.org/diseases-conditions/pancreatitis/symptoms-causes/syc-20360227
- https://pubmed.ncbi.nlm.nih.gov/8119636/
- https://www.aafp.org/pubs/afp/issues/2014/1101/p632.html#:~:text=The%20physical%20examination%20findings%20may,Bowel%20sounds%20are%20typically%20decreased.
- https://www.nhs.uk/conditions/acute-pancreatitis/prevention/#:~:text=You%20can%20reduce%20your%20risk,than%2014%20units%20a%20week
- Robbins & Cotran Pathologic Basis of Disease, 10th Edition (Kumar, Abbas, Aster, 2021, Elsevier)
- Harrison’s Principles of Internal Medicine, 21st Edition (Kasper, Fauci, Hauser, Longo, Jameson, Loscalzo, 2022, McGraw Hill)
- Sleisenger and Fordtran’s Gastrointestinal and Liver Disease, 11th Edition (Feldman, Friedman, Brandt, 2016, Elsevier)
- The Washington Manual of Medical Therapeutics, 36th Edition (Sabatine, 2023, Lippincott Williams & Wilkins)
- https://hartfordhealthcare.org/about-us/news-press/news-detail?articleId=49925&publicid=395
Also Search As
Also Search As
Given that this seems to be an article from a specific website or resource, there are a few ways people could find it:
Direct Website Search:
If they know the website name, they can use the site’s built-in search function. Most websites have a search bar (usually a magnifying glass icon) that lets users search within the site’s content. They could try terms like "acute pancreatitis," "homeopathy for pancreatitis," or even specific phrases from the article.
General Search Engine:
Using Google, Bing, or another search engine, they can try the following:
- "Acute pancreatitis homeopathic treatment"
- "Homeopathic remedies for acute pancreatitis"
- If they recall any specific phrases from the article, they can try putting those in quotes (e.g., "acute pancreatic inflammation homeopathy") to get more precise results.
Homeopathic Resource Websites:
There are many websites dedicated to homeopathy. If this article is from a well-known homeopathic organization, they might be able to find it by searching the organization’s site directly or by looking through their articles/resources.
Social Media:
If the website/organization is active on social media, they might have shared the article on their pages. Searching their social media profiles could lead people to the article.
Additional Tips:
- Use the author’s name: If the author is mentioned, including their name in the search can be helpful.
- Check the date: If you know the approximate date the article was published, including that in the search can narrow down the results.
- Look for related articles: Often, websites will suggest similar articles at the end of a piece. These might lead to the one you’re looking for.
Given that the provided text appears to be an article compiled from multiple sources, there are a few ways to find the original sources or similar information:
Search Engines (Google, Bing, etc.):
- Use specific phrases from the article in quotes. For example, search for "acute pancreatitis results from the leakage of pancreatic enzymes."
- Combine keywords like "homeopathy," "acute pancreatitis," and any specific remedies or terms mentioned.
- Look for the referenced sources directly. Many are listed at the end of the article (e.g., Robbins & Cotran Pathologic Basis of Disease).
Academic Databases (PubMed, Google Scholar):
These are great for finding scientific articles and studies. Search for keywords like "acute pancreatitis epidemiology India" or "homeopathic treatment pancreatitis."
Homeopathic Websites and Forums:
Many websites and online communities are dedicated to homeopathy. Search their resources using keywords like "acute pancreatitis" and "homeopathic remedies."
Libraries:
If you have access to a medical library, they may have books and journals referenced in the article, or other resources on acute pancreatitis and homeopathy.
Consult a Homeopathic Practitioner:
They can provide information on homeopathic approaches to acute pancreatitis and may have access to resources not readily available online.
Additional Tips:
- Pay attention to references: The article lists several sources. Look them up to find the original information and context.
- Check the website: If the article is from a website (e.g., a homeopathic clinic), search directly on their site using their search bar.
- Refine your search terms: Be specific with your keywords and use synonyms. For example, try "pancreatic inflammation" instead of "pancreatitis."
By using these strategies, you’ll be able to find the original sources of information used in the article and potentially discover other relevant resources on acute pancreatitis and homeopathy.
Frequently Asked Questions (FAQ)
What is Acute Pancreatitis?
Definition
Acute Pancreatitis, refers to inflammation of the pancreas, occurs in acute and chronic forms and may be due to edema, necrosis, or haemorrhage.
Homeopathic Medicines use by Homeopathic Doctors in treatment of Acute Pancreatitis?
Homoeopathic Medicine For Acute Pancreatitis
- Aconite
- Aloe
- Alumina
- Apis
- Argentum nitricum
- Belladona
- Mercurius
What are the causes of Acute Pancreatitis?
- Alcohol
- Gallstones
- Trauma
- Metabolic causes
- Hereditary causes
- Infections (mumps, mycoplasma)
- Vasculitis
What are the sign and symptoms of Acute Pancreatitis?
- Pain- come suddenly or build up gradually.
- Nausea
- Fever, chills, or both
- Swollen abdomen, tender to the touch
- Rapid heartbeat
How is acute pancreatitis diagnosed?
Diagnosis
Diagnosis involves a combination of medical history, physical examination, blood tests (to check for elevated pancreatic enzymes), and imaging studies like ultrasound or CT scans.
What are the treatment options for acute pancreatitis?
Treatment
Treatment focuses on managing pain, supporting the body (often through intravenous fluids and sometimes nutritional support), and addressing the underlying cause. In some cases, surgery may be necessary.
Can acute pancreatitis be prevented?
Prevention
Reducing heavy alcohol consumption is crucial for prevention. Managing gallstones and other underlying conditions can also help lower the risk.
Can homeopathy help with acute pancreatitis?
Acute Pancreatitis in homoeopathy
Homeopathy offers a supportive approach to acute pancreatitis. While it’s crucial to seek conventional medical care for this serious condition, homeopathic remedies may be used as a complementary therapy to potentially alleviate symptoms and aid recovery.
