Fissure
Definition
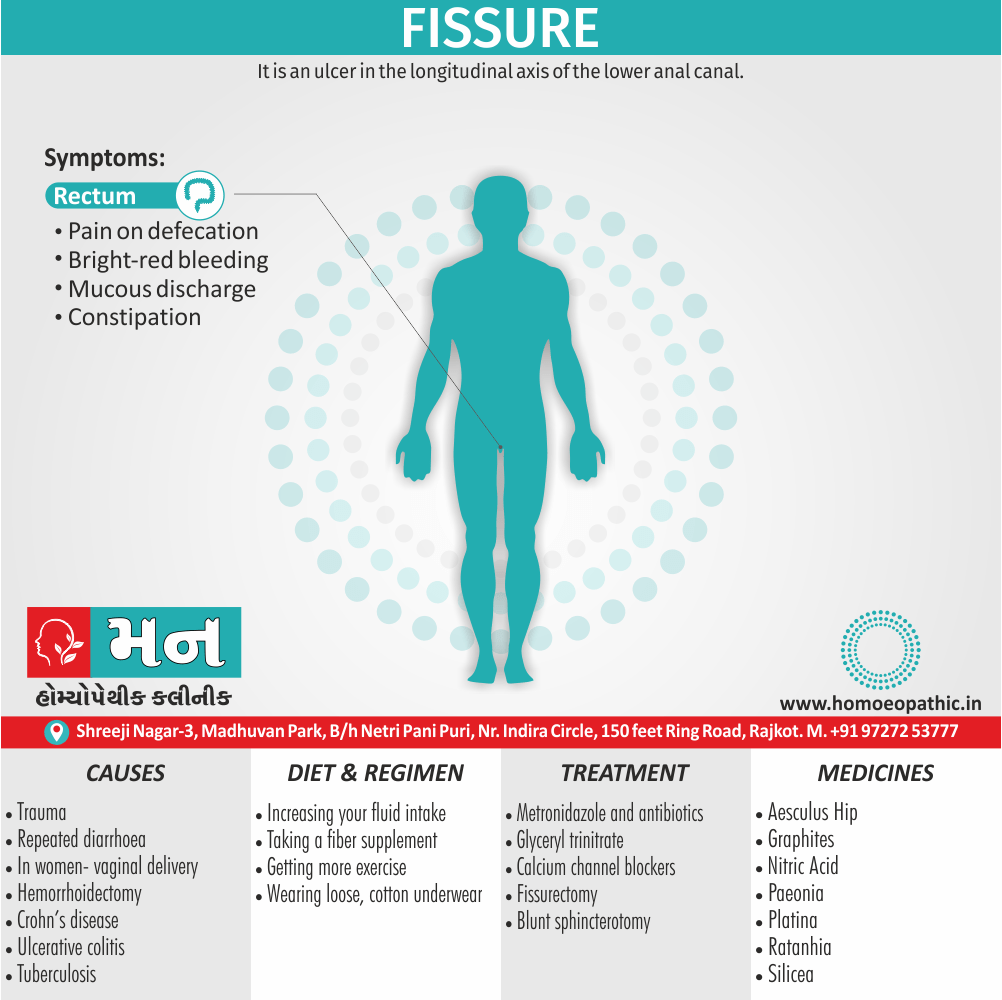
Fissure is an ulcer in the longitudinal axis of the lower anal canal. [1]
Here are some synonyms for "fissure" in medical terms, depending on the specific nuance you want to convey:
- General narrow opening:
- Cleft
- Sulcus (especially in the brain)
- Dehiscence (often used for skin)
- Linear depression:
- Groove
- Furrow
- Other options:
- Sinus (for certain channels, especially in the skull)
- Fissure itself (a widely understood term)
Remember, some organs might have specific terms for their fissures, like the Sylvian fissure in the brain.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
- Commonly it occurs in the midline, posteriorly (more common in males).
- It can also occur in the midline anteriorly (more common in females). [1]
- Although most sufferers are young adults, the condition can affect any age, from infants to the older people.
- all gender are affected equally.
- Anterior fissures account for about 10% of those encountered in women but only 1% in men. [2]
Epidemiology
Epidemiology
A recent study from India (Chaudhary and Dusage, 2019) reported the prevalence of anal fissures among adult patients with anorectal problems to be 17.8%, indicating that approximately every sixth patient with any anorectal problem may have anal fissures as the underlying pathology.[7]
Another study (JCDR, 2019) found a slightly higher prevalence in males (19.41%) than females (14.14%) and a higher prevalence in patients aged between 18 to 40 years compared to those aged 41 to 60 years.[8]
Please note that these studies provide a snapshot of the prevalence of anal fissures in specific patient populations and may not be representative of the entire Indian population.
Causes
Causes
- Trauma
- Repeated passage of diarrhoea
- In women- vaginal delivery [2]
- Hemorrhoidectomy
- Crohn’s disease
- Venereal disease
- Ulcerative colitis
- Tuberculosis [1]
Types
Risk Factors
Risk factor
- Faeces-hard
- Ischemia
- Sphincter hypertonia
- Repeated childbirth
- Enthusiastic usage of ointments and abuse of laxatives. [4]
.
Pathogenesis
Pathogenesis
The pathogenesis of anal fissure is multifactorial and not fully understood. It is believed to involve a combination of factors that contribute to the development and persistence of the fissure.
According to "Bailey & Love’s Short Practice of Surgery" (27th edition, 2018), the following factors are considered important in the pathogenesis of anal fissure:
Trauma: The passage of hard or large stools is considered a major initiating factor. The trauma to the anal mucosa and underlying muscles can lead to a tear or ulceration, which is the primary lesion of the fissure.
Ischemia: The tear in the anal lining can disrupt the blood supply to the area, leading to ischemia. This impaired blood flow can hinder healing and make the fissure more susceptible to further damage.
Hypertonicity of the internal anal sphincter: The internal anal sphincter is a ring of smooth muscle that helps maintain anal continence. In anal fissure, the internal sphincter often exhibits increased resting pressure (hypertonicity). This hypertonicity is thought to contribute to ischemia and impede healing by reducing blood flow to the fissure.
Fecal irritation: The presence of fecal matter in the anal canal can irritate the fissure and prevent healing. The acidic nature of stool can further exacerbate the problem.
Infection: In some cases, bacterial infection may play a role in the persistence of the fissure.
It is important to note that the relative contribution of each factor may vary among individuals, and the pathogenesis of anal fissure is likely a complex interplay of these factors.[2]
Pathophysiology
Pathophysiology
The pathophysiology of anal fissure involves a vicious cycle of events that contribute to the development, persistence, and potential chronicity of the condition.
According to "Sleisenger and Fordtran’s Gastrointestinal and Liver Disease" (11th edition, 2021), the following sequence of events is typically observed:
Initiating Event: The most common initiating event is trauma to the anal canal, often due to the passage of hard or large stools. This trauma leads to a tear in the anoderm (the lining of the anal canal), usually in the posterior midline.
Pain and Spasm: The tear causes pain, especially during defecation. This pain triggers a reflex spasm of the internal anal sphincter (IAS), a ring of smooth muscle that contributes to anal continence.
Ischemia: The spasm of the IAS reduces blood flow to the anoderm, leading to ischemia (reduced oxygen supply) in the region of the fissure.
Impaired Healing: The combination of ischemia and repeated trauma from defecation impairs the healing process of the fissure.
Chronic Fissure: If the fissure does not heal within a few weeks, it becomes chronic. Chronic fissures often develop secondary features like a sentinel pile (a skin tag at the distal end) and hypertrophied anal papilla (an enlarged anal papilla at the proximal end).
Persistence of Spasm: The chronic fissure and associated inflammation perpetuate the spasm of the IAS, further contributing to ischemia and impaired healing.
This vicious cycle of pain, spasm, ischemia, and impaired healing is the hallmark of the pathophysiology of anal fissure. It explains why fissures can be so painful and difficult to heal without intervention.[9]
Clinical Features
Clinical Features
The clinical features of anal fissure are characterized by a classic triad of symptoms:
Pain: Severe, sharp, tearing, or burning pain during defecation is the most common and distressing symptom. The pain typically lasts for several minutes to hours after defecation and may be accompanied by a sensation of spasm.
Bleeding: Bright red blood on toilet paper or stool is another common feature. The bleeding is usually minimal and occurs as streaks or drops.
Constipation: Patients often experience constipation due to fear of pain associated with defecation. This can lead to a vicious cycle, as hard stools further irritate the fissure and perpetuate the symptoms.
In addition to these cardinal symptoms, patients may also report:
- Pruritus (itching) ani: Itching around the anus may occur due to irritation from the fissure or associated discharge.
- Discharge: A small amount of mucus or pus may be present in the anal canal.
- Visible fissure: In some cases, the fissure may be visible as a small tear or ulceration in the anal canal, usually in the posterior midline.
On examination, the clinician may find:
- Tenderness: Palpation around the anus may elicit tenderness.
- Spasm of the internal anal sphincter: Digital rectal examination may reveal spasm and increased tone of the internal anal sphincter.
- Sentinel pile or hypertrophied anal papilla: Chronic fissures may be associated with a skin tag (sentinel pile) at the distal end or an enlarged anal papilla (hypertrophied anal papilla) at the proximal end.[10]
Sign & Symptoms
Sign & Symptoms
- Pain on defecation
- Bright-red bleeding
- Mucous discharge
- Constipation [2]
Clinical Examination
Clinical Examination
The clinical examination of anal fissure involves a careful and gentle assessment of the perianal area and anal canal.
According to "Bailey & Love’s Short Practice of Surgery" (27th edition, 2018), the following steps are typically involved:
Inspection:
- The perianal area is visually examined for signs of skin tags, hypertrophied anal papillae, excoriation, or discharge.
- Gentle separation of the buttocks may reveal the fissure as a small tear or ulceration in the posterior midline (most common) or anterior midline.
Digital rectal examination (DRE):
- This is usually deferred in the acute setting due to severe pain and spasm.
- In chronic cases, DRE may be performed after applying a topical anesthetic.
- It assesses anal sphincter tone, tenderness, and presence of induration or fibrosis.
Anoscopy:
Proctoscopy/Sigmoidoscopy:
- These procedures may be performed in selected cases to rule out other conditions like inflammatory bowel disease or malignancy.
Important Considerations:
- Examination should be performed with utmost gentleness to minimize pain and avoid further trauma.
- Adequate lighting and appropriate positioning (left lateral position) are essential.
- A chaperone should be present during the examination.
- Patient’s consent and explanation of the procedure are crucial for cooperation and comfort.[2]
Diagnosis
Diagnosis
- When the buttocks are spread apart, a longitudinal tear and a hypertrophied, thickened skin is seen near the lower end of fissure-sentinel pile.
- Additionally, Per rectal examination
- Proctoscopy is contraindicated [4]
Differential Diagnosis
Differential Diagnosis
- Carcinoma anal canal
- Inflammatory bowel disease
- Venereal diseases
- Anal chancre (especially painful)
- Tuberculous ulcer [1]
Complications
Complications
While anal fissures often heal with conservative treatment, they can occasionally lead to complications if left untreated or if healing is impaired.
According to "Sabiston Textbook of Surgery" (21st edition, 2022), the following complications may arise:
Chronic Fissure: If an acute fissure fails to heal within 6-8 weeks, it is considered chronic. Chronic fissures often develop fibrotic edges and may be associated with a sentinel pile (skin tag) or hypertrophied anal papilla.
Recurrence: Even after successful healing, anal fissures have a tendency to recur, especially in individuals with predisposing factors like chronic constipation or diarrhea.
Abscess and Fistula Formation: Rarely, an anal fissure can become infected, leading to the formation of an abscess (collection of pus) near the anus. If the abscess tracks through the tissues and forms an abnormal connection between the anal canal and the perianal skin, it is called an anorectal fistula.
Anal Stenosis: Chronic inflammation and fibrosis associated with long-standing fissures can lead to narrowing of the anal canal (anal stenosis), causing difficulty in passing stools.
Impaired Quality of Life: The pain, bleeding, and discomfort associated with anal fissures can significantly impact a person’s quality of life, affecting their daily activities, work, and social interactions.[11]
Investigations
Investigation
In most cases, the diagnosis of anal fissure is primarily clinical, based on the characteristic history and physical examination findings. However, additional investigations may be warranted in certain situations.
According to "Sleisenger and Fordtran’s Gastrointestinal and Liver Disease" (11th edition, 2021), the following investigations may be considered:
Anoscopy:
- This is the most useful investigation for confirming the diagnosis.
- A small, tubular instrument (anoscope) is inserted into the anus to visualize the fissure directly.
- It helps to assess the size, location, and severity of the fissure, as well as identify any associated pathology like sentinel piles or hypertrophied anal papillae.
Flexible Sigmoidoscopy/Colonoscopy:
- These procedures may be indicated in certain scenarios, such as:
- Atypical fissures (located off the midline or with unusual appearance)
- Patients with a history of inflammatory bowel disease (IBD)
- Patients over 50 years old with new-onset symptoms
- These tests help to rule out other conditions like IBD, colorectal cancer, or infections.
- These procedures may be indicated in certain scenarios, such as:
Other Investigations:
- Rarely, additional tests like stool cultures, biopsy, or imaging studies (MRI) may be performed if there is suspicion of an underlying cause or atypical features.
Important Considerations:
- Digital rectal examination (DRE) is usually avoided in acute fissures due to pain and spasm.
- Investigations should be tailored to the individual patient’s presentation and clinical suspicion.
- A thorough discussion of the risks and benefits of each investigation should be done with the patient before proceeding.[9]
Treatment
Treatment
Conservative:
Avoid constipation– e.g. encourage fiber diet, mild laxatives also not to postpone defaecation.
Surface anesthetic creams: i.e. Lignocaine jelly.
Metronidazole also antibiotics
Agents which decrease sphincter pressure:
Glyceryl trinitrate (0.2%)
Purified botulinum toxin injection into internal sphincter
Calcium channel blockers: e.g. Nifedipine, Diltiazem
Surgical treatment:
Lateral anal sphincterotomy of Notaras
Fissurectomy
Blunt sphincterotomy [4]
Prevention
Prevention
The prevention of anal fissures primarily focuses on avoiding constipation and maintaining healthy bowel habits.
According to "Current Surgical Therapy" (13th edition, 2022), the following preventive measures are recommended:
Dietary Modifications:
- Increase fiber intake: Consume a diet rich in fruits, vegetables, whole grains, and legumes to promote soft, bulky stools and prevent constipation.
- Adequate fluid intake: Drink plenty of water and other fluids to keep stools hydrated and easy to pass.
Regular Exercise:
- Engage in regular physical activity to promote bowel motility and prevent constipation.
Avoid Straining:
- Do not strain or hold your breath during bowel movements, as this can increase pressure on the anal canal and lead to tears.
Prompt Treatment of Diarrhea:
- Diarrhea can irritate the anal lining and predispose to fissures. Seek prompt treatment for diarrhea to prevent complications.
Maintain Good Hygiene:
- Clean the anal area gently after bowel movements with soft toilet paper or moist wipes.
- Avoid harsh soaps or irritants in the anal area.
Early Treatment of Anal Fissures:
- If you experience any symptoms suggestive of an anal fissure, seek medical attention promptly to prevent it from becoming chronic.[12]
Homeopathic Treatment
Homeopathic Treatment of Fissure
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Fissure:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Homoeopathic Approach:
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines are selected after a full individualizing examination and case-analysis, which includes the medical history of the patient, physical and mental constitution, family history, presenting symptoms, underlying pathology, possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) is also often taken into account for the treatment of chronic conditions. A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’. The disease diagnosis is important but in homeopathy, the cause of disease is not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness are also looked for.
Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition. The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology is not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can be greatly improved with homeopathic medicines.
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications are also taken into account for selecting a remedy.
Medicines:
Aesculus Hip:
- Anus feels raw, soreness, burning, itching also fulness at anus
- In detail, Pain like a knife sawing backward and forward through anus
- Pains in anus about an hour after stool, continuing for some time.
- Aesculus can be of great help if you are experiencing severe pain in the anus following stool passage.
- Either the stool or poop passed is mainly hard and large followed by severe pains.
Graphites:
- Fissures of recent origin, especially in children; varices of rectum and burning rhagades between them.
- Fissures caused by large faecal masses, no irritability, no frequent desire to stool nor spasmodic contraction of sphincter, only some smarting and soreness, aggravation at night and when sitting.
Lachesis:
- Sensation of little hammers pecking away in fissured parts.
- Tormenting urging, but not to stool.
- Itching at anus, aggravation especially after sleep.
Nitric Acid:
- Sharp, splinter-like cutting pains in rectum during also burning after stool.
- Painful prolapses of bowels also sensation of constriction in anus.
- stitching also tearing pains in the anus, or the pain is cutting or stinging in nature.
- All in all, The stool passed is hard, and is accompanied by bright red bleeding from the anus.
Paeonia:
- Ulcerations of mucous membrane of rectum and anus, with fissures, burning and biting some hours after stools.
- Parts swollen and exhaling an offensive odours.
- Furthermore, Anus damp and disagreeable from constant oozing.
- Paeonia is the best remedy for offensive discharge from the anus due to cracks in it.
- Paeonia is also the best medicine for violent pains in the anus during also after passing stool.
- Besides this, The anus is ulcerated and fissured. Itching and burning usually accompany the fissures.
- Help in treatment of Anal Fissures with offensive discharge.
Platina:
- Fissure in ani with crawling and itching in anus every evening; frequent urging with scanty stool
- Painful sensation of weakness.
Ratanhia:
- Ratanhia is an effective medicine for the treatment of Anal Fissures and is particularly beneficial as a remedy for long-lasting pains in the rectum with excessive burning that follows stool passage.
- Patients often describe the pain as being similar to broken glass or a knife piercing in the rectum.
- The stool requires much effort to be passed out due to the constricted anus.
- Ratanhia is the Homeopathic medicine that can work wonders in such a situation.
- Burning in anus like fire, preceding and accompanying defaecation also lasting a long time after, accompanied by prostration of varices.
- Dry heat in anus, with sudden stitches like stabs with a pen-knife. Lastly, Sensation as if the rectum protruded and went back with a jerk, with most horrible pains.
Silicea:
- Long and painful efforts to expel the contents of the rectum but the sphincter ani seems tightly to resist the effort till suddenly the stool passes, sometimes with pain and nervous shuddering
- Stool partly descends and then slips back again.
Sulphur
- Sulphur works well where the stool is hard and dry, causing tears and immense pain in the anus while passage.
- The patient is fearful of even going to the toilet as he thinks of the pain that will accompany the passage of stool.
- Sulphur is of great help in reducing the pain and softening the stool.
- The pain is almost always accompanied by burning.
- Itching in anus due to fissures is best controlled with the use of Sulphur.
Thuja
- Fissures with edges trimmed with polypoid excrescences or true rectal polypus
- Piles, condylomata, urinary troubles. [5]
Diet & Regimen
Diet & Regimen
- 9 foods that may help if you have fissures: Papayas, Lemons, Bananas, Oatmeal, Turmeric, Ghee, Milk, Probiotic-rich foods
- Increasing your fluid intake
- Taking a fiber supplement, such as psyllium husk
- Getting more exercise
- Wearing loose, cotton underwear. [6]
Do’s and Don'ts
Do’s And Dont’s
Of Fisssure
Do’s:
- Increase fiber intake: Eat plenty of fruits, vegetables, whole grains, and legumes to promote soft, bulky stools.
- Drink plenty of fluids: Aim for 8-10 glasses of water per day to keep stools hydrated and easy to pass.
Hygiene:
- Clean the anal area gently after bowel movements with soft, unscented toilet paper or moist wipes.
- Take warm sitz baths: Soak the anal area in warm water for 10-15 minutes several times a day to relieve pain and promote healing.
Medications:
- Use stool softeners: As recommended by your doctor, stool softeners can help prevent constipation and ease bowel movements.
- Apply topical anesthetics: Lidocaine or other local anesthetics can provide temporary pain relief.
- Consider prescription medications: Your doctor may prescribe medications to relax the anal sphincter and promote healing.
Don’ts:
Avoid Constipation:
- Don’t delay bowel movements: Ignoring the urge to defecate can lead to harder stools and worsen the fissure.
- Don’t strain during bowel movements: Straining increases pressure on the anal canal and can cause further trauma.
Irritants:
- Avoid harsh soaps or perfumed products in the anal area, as they can irritate the skin and delay healing.
- Avoid spicy foods, caffeine, and alcohol, which can exacerbate symptoms in some individuals.
Delaying Treatment:
- Don’t ignore symptoms: If you experience pain, bleeding, or other symptoms suggestive of an anal fissure, seek medical attention promptly. Early treatment can prevent complications and promote faster healing.
Remember, this information is not a substitute for professional medical advice. Always consult your doctor for proper diagnosis and treatment of anal fissure.
Terminology
Terminology
Absolutely! Here are some common terminologies used in articles about anal fissures, along with their meanings:
- Anoderm: The lining of the anal canal, which is very sensitive to pain and injury.
- Anal Canal: The terminal part of the large intestine, extending from the rectum to the anus.
- Anal Sphincter: The muscles that surround the anal canal and control bowel movements. There are two types: * Internal Anal Sphincter: Involuntary smooth muscle that maintains resting anal pressure. * External Anal Sphincter: Voluntary striated muscle that allows for conscious control of defecation.
- Chronic Fissure: An anal fissure that persists for more than 6-8 weeks, often accompanied by a sentinel pile or hypertrophied anal papilla.
- Constipation: Infrequent or difficult bowel movements, often characterized by hard or dry stools.
- Fissurectomy: A surgical procedure to remove the anal fissure and relieve tension in the anal sphincter.
- Hypertrophied Anal Papilla: An enlarged anal papilla, a small projection of tissue at the upper end of the anal canal, often seen in chronic fissures.
- Ischemia: Reduced blood flow to a tissue, leading to inadequate oxygen supply and potential tissue damage.
- Lateral Internal Sphincterotomy (LIS): A surgical procedure that involves cutting a small portion of the internal anal sphincter to reduce spasm and promote healing of the fissure.
- Sentinel Pile: A skin tag that develops at the distal end of a chronic anal fissure.
- Spasm: Involuntary contraction of a muscle, often causing pain or discomfort.
- Topical Nitroglycerin: A medication applied to the skin around the anus to relax the anal sphincter and improve blood flow to the fissure.
Some Other Terminology Related To Homoeopathy
- Miasm: A fundamental disturbance or predisposition in the body that underlies chronic disease, according to homeopathic theory.
- Remedy: A homeopathic medicine prepared from natural substances, used to stimulate the body’s healing response.
- Repertorization: The process of analyzing a patient’s symptoms and matching them to the most appropriate homeopathic remedy.
- Proving: A systematic process of testing a substance on healthy individuals to determine its potential effects and identify the symptoms it can produce.
- Potency: The degree of dilution and succussion (vigorous shaking) a homeopathic remedy undergoes, believed to increase its therapeutic effect.
- Constitutional Remedy: A remedy chosen based on the patient’s overall physical, mental, and emotional characteristics, rather than just their specific symptoms.
- Aggravation: A temporary worsening of symptoms after taking a homeopathic remedy, often considered a positive sign of healing.
- Amelioration: An improvement or relief of symptoms after taking a homeopathic remedy.
- Homeopathic Materia Medica: A reference book containing detailed information about the symptoms and therapeutic applications of various homeopathic remedies.
- "A homeopathic practitioner might consider the patient’s underlying miasm when choosing a remedy for anal fissure."
- "Several remedies are listed in the homeopathic materia medica for the treatment of anal fissure, including Nitric acid, Paeonia, and Graphites."
- "The homeopath will conduct a thorough case-taking to understand the patient’s unique symptom picture and select the most appropriate constitutional remedy."
References
References
- SRB’s Clinical Methods in Surgery
- Bailey_and_Love_s_Short_Practice_of_Surgery
- Clinical Surgery S. Das
- Manipal Manual of Surgery (PDF Drive)
- Homeopathic Therapeutic by Lilienthal
- https://www.healthline.com/nutrition/foods-that-cure-fissures#8.-Probiotic-rich-foods.
- Chaudhary, R., & Dusage, R. N. (2019). Incidence of anal fissure (cases per 1000 persons per year) by sex and age group.
- JCDR. (2019). Constipation, Epidemiology, Fissure-in-ano, Risk factors.
- Sleisenger and Fordtran’s Gastrointestinal and Liver Disease,11th edition, Mark Feldman, Lawrence S. Friedman, Lawrence J. Brandt,2021, Saunders
- Schwartz’s Principles of Surgery, 11th edition,F. Charles Brunicardi, Dana K. Andersen, Timothy R. Billiar, et al., 2019, McGraw Hill Professional
- Sabiston Textbook of Surgery,21st edition,Courtney M. Townsend, Jr., R. Daniel Beauchamp, Kenneth L. Mattox, B. Mark Evers, 2022, Elsevier.
- Current Surgical Therapy, 13th edition, John L. Cameron, Andrew M. Cameron, 2022, Elsevier
Also Search As
Fissure Also Search As
There are several ways people can search for homeopathic articles on anal fissures:
Online Search Engines:
- Use specific search terms: Combine terms like "homeopathy," "anal fissure," "treatment," "remedies," or "case studies" to narrow down the results.
- Use quotation marks: Enclose phrases like "homeopathic treatment for anal fissure" in quotation marks to get exact matches.
- Explore reputable homeopathic websites: Many homeopathic organizations and clinics have online resources and articles on various conditions, including anal fissures.
Homeopathic Journals and Databases:
- Search online databases: Platforms like PubMed, Google Scholar, and the International Journal of Homeopathic Sciences often have research articles and case reports related to homeopathy and specific conditions.
- Browse homeopathic journals: Many homeopathic journals publish articles on various topics, including anal fissures. You can find these journals online or in libraries.
Homeopathic Libraries:
- Visit local homeopathic libraries: Many homeopathic colleges and organizations have libraries with books, journals, and other resources on homeopathic treatment.
- Consult with librarians: Librarians can help you navigate the resources and find relevant articles.
Homeopathic Forums and Communities:
- Join online forums or groups: Many online communities discuss homeopathy and share experiences with different remedies. You can ask questions and get recommendations from other users.
Consult a Homeopathic Practitioner:
- A qualified homeopathic practitioner can provide personalized advice and recommendations for treating anal fissures. They can also direct you to relevant resources and articles.
Here are some additional tips:
- Look for articles published in peer-reviewed journals for reliable information.
- Consider the date of publication, as newer articles may reflect more recent research and advancements.
- Be critical of the information you find online and consult with a qualified homeopathic practitioner before starting any treatment.
By utilizing these resources and strategies, individuals can easily find comprehensive and reliable information on homeopathic approaches to treating anal fissures.
There are several ways to search for information about anal fissures, depending on the type of information you are looking for and your preferred sources:
Medical Websites and Resources:
- Reputable sources: Look for information on websites like Mayo Clinic, Cleveland Clinic, Healthline, and other trusted medical organizations. These sources typically provide reliable, evidence-based information on anal fissures.
- Specific topics: Many websites offer detailed information on the causes, symptoms, diagnosis, and treatment of anal fissures. You can also find information on related conditions, such as hemorrhoids or inflammatory bowel disease.
Medical Literature and Journals:
- PubMed: This online database provides access to millions of medical publications, including research articles and clinical studies on anal fissures. You can use specific keywords to search for relevant articles.
- Google Scholar: This search engine specializes in academic literature, including scholarly articles and books on medical topics. You can use it to find research on anal fissures and related conditions.
Books and Medical Textbooks:
- Surgical textbooks: Textbooks like "Bailey & Love’s Short Practice of Surgery" and "Schwartz’s Principles of Surgery" offer in-depth information on the surgical management of anal fissures.
- Gastroenterology textbooks: Books like "Sleisenger and Fordtran’s Gastrointestinal and Liver Disease" provide comprehensive information on the medical aspects of anal fissures, including their causes, symptoms, and nonsurgical treatments
Consulting a Healthcare Professional:
- Doctor or specialist: If you suspect you have an anal fissure or have any concerns about the condition, consult a doctor or a specialist like a gastroenterologist or colorectal surgeon. They can provide a proper diagnosis, discuss treatment options, and answer any questions you may have.
By using these various approaches, you can gather a comprehensive understanding of anal fissures, their causes, symptoms, treatment options, and preventive measures. Remember to consult a healthcare professional for personalized advice and treatment recommendations.
Frequently Asked Questions (FAQ)
What causes Fissure?
- Trauma
- Repeated passage of diarrhoea
- In women- vaginal delivery
- Hemorrhoidectomy
- Crohn’s disease
- Venereal disease
- Ulcerative colitis
- Tuberculosis
How are anal fissures treated?
Treatment options include:
- Dietary changes: Increasing fiber and fluid intake to soften stools
- Medications: Stool softeners, topical pain relievers, and medications to relax the anal sphincter
- Sitz baths: Soaking in warm water to promote healing and relieve pain
- Surgery: In severe or chronic cases, surgery may be necessary to release the anal sphincter and allow the fissure to heal.
How are anal fissures diagnosed?
Diagnosis
Diagnosis is usually made through a physical examination and a visual inspection of the anus. In some cases, a doctor may use a small instrument called an anoscope to get a better view
What are the symptoms of Fissure?
- Pain on defaecation
- Bright-red bleeding
- Mucous discharge
- Constipation
Are there any side effects of homeopathic remedies for anal fissure?
Homeopathic remedies are generally safe and have minimal side effects when used correctly. However, it’s always recommended to consult a qualified homeopathic practitioner for proper diagnosis and treatment.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Fissure?
Homeopathic Medicines
- Aesculus Hip
- Graphites
- Lachesis
- Nitric Acid
- Paeonia
- Platina
- Ratanhia
- Silicea
- Sulphur
- Thuja
Can I use homeopathic remedies along with conventional treatments for anal fissure?
Yes,
homeopathic remedies can often be safely used alongside conventional treatments. However, it’s important to inform your healthcare providers about all medications and therapies you are using.
Is it safe to use homeopathy for children with fissures?
Homeopathic remedies are generally considered safe for children when prescribed by a qualified practitioner.
How does homeopathy work in the context of fissures?
Homeopathy works on the principle of "like cures like," where a substance that can cause symptoms in a healthy person is used in a diluted form to treat similar symptoms in a sick person. The goal is to stimulate the body’s vital force and promote healing.
