Fistula
Definition:
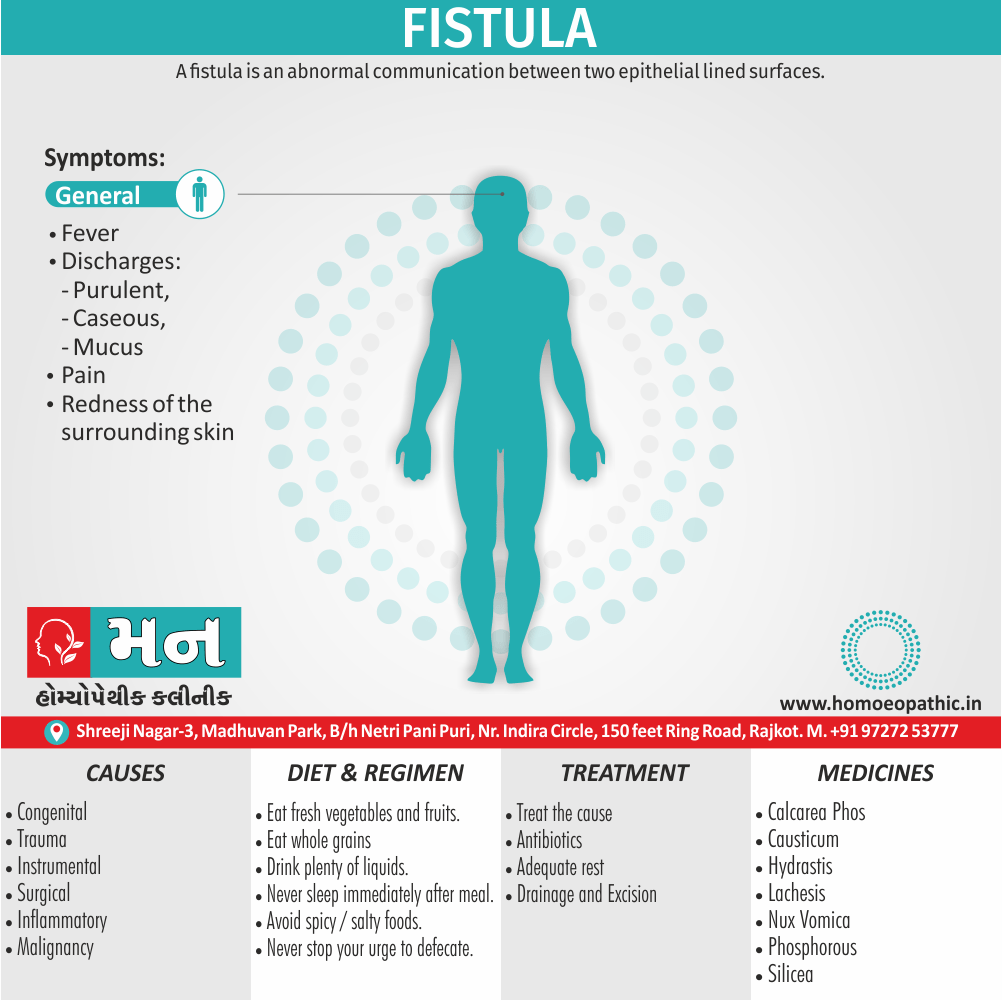
A fistula is an abnormal communication between two epithelially lined surfaces. [1]
Here are some synonyms for "fistula" depending on the context:
General synonyms:
- Sinus: This refers to a similar abnormal passage, but often used for those draining to the skin’s surface.
- Passage: A more general term for any channel or duct.
- Communication: This emphasizes the connection between two organs or spaces.
Formal synonyms:
- Fistulation: This is a less common synonym but emphasizes the formation of the abnormal passage.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Fistula
- It is a communicating track between two epithelial surfaces, commonly between a hollow viscus also the skin (especially external) or between two hollow viscera (specifically internal). [2]
- In detail, This communication or tract may be lined by granulation tissue but may become epithelialized in chronic cases. [1]
Epidemiology
Epidemiology
The epidemiology of fistula in India varies depending on the type of fistula.
Obstetric Fistula:
Key Findings:
- Retrospective data from 24 tertiary care facilities (2000-2006) revealed 717 women underwent genital fistula repair.
- Obstructed labor caused 97% of genital fistulas.
- Genitourinary fistulas were the most common (86.6%).
- The study highlighted the need for systematic data collection on obstetric fistula.[8]
Anal Fistula:
Key Findings:
- Study in a North Indian rural region found varying grades of anal fistulas, with a higher prevalence of Grade 4.
- This higher prevalence may be due to factors like illiteracy, social stigma, poor hygiene, and high recurrence rates.[9]
Additional Notes:
The prevalence of obstetric fistula is higher in underdeveloped regions of India, with Assam, Madhya Pradesh, and Uttarakhand showing higher percentages.
The prevalence of anal fistula in the general population varies, with some studies reporting it as the most common anorectal condition while others found hemorrhoids or fissures more prevalent.
Important Considerations:
Data collection on fistula in India is often limited and may not reflect the true burden of the condition.
There is a need for more comprehensive, nationwide studies to understand the true epidemiology of fistula in India.
It’s important to note that this information is based on available references and may not be fully representative of the entire Indian population.
Causes
Causes of Fistula
Congenital i.e.:
- Branchial
- Tracheoesophageal.
- Congenital AV.
- Umbilical
Acquired i.e.:
- Trauma (especially abdomen)
- Instrumental (during delivery)
- Surgical
- Inflammatory (either intestinal tuberculosis or actinomycosis)
- Malignancy (for example; recto vesical fistula in carcinoma of rectum).[5]
Types
Risk Factors
Risk factors
Obstetric
- Prolonged obstructed labor
- Young age at first birth
- Malnutrition
- Poverty
- Limited access to healthcare
Anal
- Anal abscess
- Crohn’s disease
- Ulcerative colitis
- Trauma
- Tuberculosis
- Diverticulitis
- Sexually transmitted infections
- Cancer
Other Risk Factors:
- Radiation therapy
- Inflammatory bowel disease
- Immunosuppression
It’s important to note that this is not an exhaustive list and other risk factors may exist.[10]
Pathogenesis
Pathogenesis
The development of a fistula generally involves the following steps:
Inflammation and Infection:
The process often begins with an inflammatory or infectious process. In the case of anal fistulas, this usually originates in the anal glands, leading to an abscess. Other types of fistulas may arise from surgical complications, inflammatory bowel disease, or radiation therapy.
Abscess Formation:
The inflammation can lead to the formation of an abscess, a collection of pus. The abscess can then track through the surrounding tissues.
Tract Formation:
As the abscess tries to find a way to drain, it creates a tract through the tissue. This tract can eventually open onto the skin or another organ, forming a fistula.
Epithelialization:
The tract can become lined with epithelial tissue, making it more stable and persistent.
Specific Pathogenesis:
Obstetric
Prolonged obstructed labor leads to tissue necrosis due to pressure and ischemia. The necrotic tissue creates a pathway for fistula formation between the bladder, vagina, and/or rectum.
Anal
The pathogenesis typically involves infection of an anal gland, leading to abscess formation. The abscess can then track through the sphincter muscles and open onto the skin, forming a fistula.
Enterocutaneous
This type often arises from complications of abdominal surgery, such as anastomotic leaks or bowel perforation. Crohn’s disease and other inflammatory conditions can also contribute to formation.
Understanding the pathogenesis of is crucial for effective treatment and prevention.[11]
Pathophysiology
Pathophysiology
It formation generally involves an initiating inflammatory or infectious process that leads to tissue damage and breakdown. The underlying mechanisms vary depending on the type.
General Pathophysiology:
Inflammation/Infection:
The process usually begins with inflammation or infection, which could be due to various factors such as trauma, surgical complications, or inflammatory bowel disease (IBD).
Abscess Formation:
The inflammation can progress and form an abscess (a collection of pus) within the affected tissue.
Tract Formation:
The abscess creates a tract (a tunnel-like pathway) through the tissue as it attempts to drain. The tract can extend to the skin surface or connect with another organ.
Epithelialization:
The tract can become lined with epithelial tissue, making it more stable and persistent.
Specific Pathophysiology:
Obstetric
- Prolonged obstructed labor causes tissue necrosis due to pressure and compromised blood supply.
- The necrotic tissue creates a pathway for formation between the bladder, vagina, and/or rectum.
Anal
Enterocutaneous
- The underlying cause is often a disruption in the bowel wall integrity (e.g., from surgery, IBD, or radiation therapy).
- The fistula tract connects the bowel lumen to the skin surface.
Factors Affecting Fistula Persistence:
Persistent Inflammation/Infection:
Continued inflammation or infection can hinder the healing process and perpetuate the fistula.
High Output:
Fistulas with high output (large volume of drainage) tend to be more challenging to heal.
Foreign Bodies:
The presence of foreign material (e.g., sutures) can impede healing and promote fistula formation.
Malignancy:
Malignant fistulas are often associated with poor healing due to ongoing tumor growth and tissue destruction.
Radiation:
Radiation can damage tissue and impair the healing process, increasing the risk of fistula development.
Epithelialization:
The epithelial lining of the fistula tract can make it more resistant to closure.
Clinical Features
Clinical Features
It’s varies depending on the type and location. However, some common features include:
External Opening:
Most have an external opening, often with surrounding inflammation or induration (hardening of the skin). The opening may discharge pus, blood, stool, or other fluids.
Pain:
It can be associated with varying degrees of pain, from mild discomfort to severe, throbbing pain. The pain may be exacerbated by movement, bowel movements, or pressure on the affected area.
Swelling:
Swelling may occur around the external opening or along the tract.
Drainage:
it may continuously or intermittently drain fluid, which can be foul-smelling or contain pus, blood, or stool.
Constitutional Symptoms:
In some cases, fistulas may be accompanied by systemic symptoms such as fever, chills, fatigue, or weight loss.
Specific Clinical Features:
Anal
- Perianal pain and discomfort
- Purulent or bloody drainage
- Perianal abscess (in some cases)
- Palpable cord-like tract
Obstetric
- Continuous urinary or fecal incontinence
- Vaginal discharge
- Excoriation of the vulva and thighs
- Psychological distress and social isolation
Enterocutaneous
- Drainage of intestinal contents from the skin
- Skin irritation and excoriation
- Malnutrition and dehydration (in severe cases)
Diagnosis:
The diagnosis of a fistula often involves a combination of:
Physical Examination:
The external opening and any associated findings are typically identified during a physical exam.
Imaging Studies:
Fistulography (injection of contrast dye into the fistula tract) and other imaging modalities like CT or MRI can help visualize the tract and determine its extent.
Fistulogram:
This imaging technique involves injecting contrast dye into the fistula tract to visualize its anatomy and course.
Endoscopy (if applicable):
This can be used to assess fistulas involving the gastrointestinal tract.
Understanding the clinical features of fistula is crucial for prompt diagnosis and appropriate management.[11]
Sign & Symptoms
Sign & Symptoms of Fistula
Different discharges e.g.:
- Purulent—Bacterial infection
- Caseous—Tuberculous
- Sulphur granules—Actinomycosis
- Mucus—Branchial
- Saliva—Parotid
- Faeces—Faecal
- Bile—Biliary, duodenal
- Bone—Osteomyelitis sinus
- Urine – Urinary [4]
Pain i.e.:
- If pain is associated with, additionally inflammatory nature is assured.
Fever and redness of the surrounding skin i.e.:
- In brief, It also suggests inflammatory origin [2]
Clinical Examination
Clinical / Physical Examination
Inspection
- Branchial: especially, Anterior border of lower third of stemomastoid
- Parotid: In the parotid region
- Thyroglossal: specifically, Mid line of neck below hyoid bone
- Appendicular: particularly, Right iliac fossa
Palpation
- Induration is present in chronic type, actinomycosis, also osteomyelitis.
- Submandibular stone may be palpable as in submandibular type.
Relevant clinical examination
Diagnosis
Diagnosis
The diagnosis often involves a combination of clinical assessment, imaging studies, and sometimes additional tests depending on the type and location of it.
Clinical Assessment:
History:
A detailed medical history is essential, including the duration and nature of symptoms (e.g., pain, discharge, bleeding), previous surgeries, underlying medical conditions (e.g., Crohn’s disease), and risk factors.
Physical Examination:
The external opening is typically visible, and a digital rectal examination (for anal fistulas) or pelvic examination (for obstetric fistulas) can help assess the extent of the tract and identify any associated abscesses.
Probing:
Gentle probing with a blunt instrument can help determine the direction and depth of the tract.
Imaging Studies:
Fistulography:
This is the gold standard imaging technique for diagnosing fistulas. It involves injecting contrast dye into the fistula tract, followed by X-ray imaging to visualize the tract’s anatomy and course.
MRI:
Magnetic resonance imaging (MRI) can provide detailed anatomical information and surrounding tissues, especially for complex or recurrent fistulas.
CT Scan:
Computed tomography (CT) scan is useful for evaluating deep pelvic fistulas or those associated with abdominal abscesses.
Ultrasound:
Endoscopic ultrasound (EUS) or transperineal ultrasound (TPUS) can help assess anal fistulas and their relationship to the sphincter muscles.
Additional Tests:
Fecal Calprotectin:
This test may be performed to assess for inflammatory bowel disease, which can be a risk factor for fistula development.
Culture and Sensitivity:
If infection is suspected, a sample of the drainage can be cultured to identify the causative organism and determine its antibiotic sensitivity.
Specific Considerations:
Anal Fistula:
Goodsall’s rule can help predict the course of the fistula tract based on the location of the external opening.
Obstetric Fistula:
Dye tests (e.g., methylene blue test) may be used to confirm urinary or fecal incontinence.
Enterocutaneous Fistula:
Contrast studies of the gastrointestinal tract may be performed to assess the location and extent of the fistula.
Differential Diagnosis
Differential Diagnosis
The differential diagnosis of a fistula depends on its location and clinical presentation. Here are some common differential diagnoses for different types of fistulas:
Anal Fistula:
Anal Fissure:
A tear in the lining of the anus that can cause pain and bleeding.
Perianal Abscess:
A collection of pus near the anus that can be a precursor to a fistula.
Pilonidal Disease:
An infection of the skin and subcutaneous tissue at the base of the spine.
Hidradenitis Suppurativa:
A chronic inflammatory skin condition that can cause abscesses and sinus tracts.
Crohn’s Disease:
An inflammatory bowel disease that can cause fistulas in the perianal area.
Rectal Carcinoma:
A malignant tumor of the rectum that can sometimes present with a fistula.
Obstetric Fistula:
Rectovaginal Fistula:
An abnormal connection between the rectum and vagina.
Vesicovaginal Fistula:
An abnormal connection between the bladder and vagina.
Urethrovaginal Fistula:
An abnormal connection between the urethra and vagina.
Enterocutaneous Fistula:
Inflammatory Bowel Disease (Crohn’s Disease/Ulcerative Colitis):
These conditions can cause inflammation and damage to the bowel wall, leading to fistula formation.
Diverticulitis:
Inflammation or infection of diverticula (pouches) in the colon can lead to fistula formation.
Postoperative Complications:
Fistulas can sometimes occur as a complication of abdominal surgery.
Cancer:
Certain cancers, such as colon cancer, can cause fistulas.
Other Differential Diagnoses:
Infected Sebaceous Cyst:
A benign skin growth that can become infected and resemble a fistula.
Foreign Body Reaction:
A foreign body embedded in the tissue can cause inflammation and a draining tract.
Tuberculosis:
Tuberculosis can cause fistulas in various parts of the body, including the intestines.
It’s important to consider these differential diagnoses when evaluating a patient with a suspected fistula. A thorough history, physical examination, and appropriate diagnostic tests can help differentiate between these conditions and guide treatment decisions.[13]
Complications
Complications
It’s can vary depending on the type and location of the fistula, as well as the underlying cause. However, some potential complications include:
General Complications:
Recurrence:
It can sometimes recur after treatment, especially if the underlying cause is not addressed.
Infection:
It can become infected, leading to pain, swelling, and fever. In severe cases, the infection can spread to other parts of the body.
Malnutrition and Dehydration:
Fistulas that drain large amounts of fluid can lead to malnutrition and dehydration, especially in patients with underlying medical conditions.
Skin Irritation and Breakdown:
Constant drainage from the fistula can irritate and damage the surrounding skin, leading to breakdown and ulceration.
Psychological Distress:
It can cause significant emotional and psychological distress due to the associated symptoms and social stigma.
Specific Complications:
Anal Fistula:
- Incontinence: Damage to the sphincter muscles during surgery or from itself can lead to fecal incontinence.
- Anal Stenosis: Scarring from surgery or chronic inflammation can narrow the anal canal, causing difficulty with bowel movements.
- Recurrence: Anal fistulas can recur, especially if the underlying cause (such as Crohn’s disease) is not treated.
Obstetric Fistula:
- Urinary Tract Infections: Frequent urinary leakage can increase the risk of urinary tract infections.
- Kidney Damage: In severe cases, untreated obstetric fistulas can lead to kidney damage and failure.
- Psychological Trauma: The physical and social consequences of obstetric fistula can cause significant psychological trauma and depression.
Enterocutaneous Fistula:
- Sepsis: Infection of the fistula can spread to the bloodstream, leading to a life-threatening condition called sepsis.
- Malabsorption: Fistulas that involve the small intestine can impair nutrient absorption, leading to malnutrition and deficiencies.
- Short Bowel Syndrome: In severe cases, surgical removal of a large portion of the bowel may be necessary, resulting in short bowel syndrome.
Prevention and Management:
Early Diagnosis and Treatment:
Prompt diagnosis and treatment of fistula can help prevent complications.
Proper Wound Care:
Keeping the fistula and surrounding skin clean and dry can help prevent infection and skin breakdown.
Nutritional Support:
Patients with high-output fistulas may need nutritional support to prevent malnutrition and dehydration.
Psychological Support:
Providing emotional and psychological support to patients with fistula can help them cope with the condition and improve their quality of life.[14]
Investigations
Investigation of Fistula
Examination of the discharge i.e.-
- Macroscopically
- Physically
- Chemically
- Microscopically
- Bacteriologically
X-ray Examination i.e.-
- Straight X-ray
- Injection of radio-opaque fluid
Examination using coloured solution i.e.-
- Charcoal powder
- Coloured drug (i.e. Pyridium)
Fistulography [2]
Treatment
Treatment of Fistula
- Treat the cause
- Excision of fistulas. In detail, Always specimen should be sent for histology. [4]
- Antibiotics
- Adequate rest
- Adequate drainage [3]
Prevention
Prevention
It’s strategies vary depending on it’s type:
Obstetric Fistula:
Early and Skilled Obstetric Care:
The most effective way to prevent obstetric fistula is to ensure access to timely and skilled obstetric care, including emergency obstetric care for obstructed labor.
Family Planning:
Providing access to family planning services can help women avoid unintended pregnancies and reduce the risk of obstructed labor.
Delaying Early Marriage and Childbirth:
Encouraging delayed marriage and childbirth can help prevent it, as young girls are more susceptible to obstructed labor.
Improving Nutritional Status:
Ensuring adequate nutrition for women and girls can help prevent malnutrition, a risk factor for obstetric fistula.
Community Education:
Educating communities about the importance of seeking skilled obstetric care and the risks of early marriage and childbirth can help prevent it.
Anal Fistula:
Prompt Treatment of Anal Abscesses:
Treating anal abscesses promptly can prevent the development of anal fistulas.
Managing Underlying Conditions:
Effectively managing underlying conditions such as Crohn’s disease and ulcerative colitis can reduce the risk of it’s formation.
Safe Sex Practices:
Practicing safe sex can reduce the risk of sexually transmitted infections that can lead to anal fistulas.
High-Fiber Diet and Adequate Hydration:
Consuming a high-fiber diet and drinking plenty of fluids can help prevent constipation, which is a risk factor for anal abscesses and fistulas.
Enterocutaneous Fistula:
Careful Surgical Technique:
Minimizing bowel manipulation and ensuring adequate blood supply during abdominal surgery can reduce the risk of it’s formation.
Proper Postoperative Care:
Promptly addressing any signs of infection or complications after surgery can help prevent it.
Managing Underlying Conditions:
Effectively managing conditions like Crohn’s disease and radiation enteritis can reduce the risk of it’s development.
General Prevention Measures:
Maintaining Good Hygiene:
Proper hygiene, especially after bowel movements, can help prevent infection and reduce the risk of fistula formation.
Seeking Prompt Medical Attention:
Seeking medical attention for any signs or symptoms of infection or inflammation can help prevent the progression to fistula formation.
It’s important to note that not all fistulas can be prevented. However, implementing these preventive measures can significantly reduce the risk of developing fistulas and improve outcomes for those affected by this condition.[15]
Homeopathic Treatment
Homeopathic Treatment of Fistula
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Fistula:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
Berberis:
- Violent burning in anus, as if surrounding parts were sore.
- Frequent also constant desire for stool.
- Burning, stitching pains during, before also after stool painful pressure in perineum, stitches in perineum, extending deep into (left side of) pelvis.
- Tearing extending around anus.
- Short cough and chest complaints; additionally biliary colic.
Calcarea Phos:
- After surgical interference.
- Fistula-ani alternating with chest symptoms or in persons who have pains in joints with every spell of cold stormy weather, especially in tall, slim persons.
- Burning also pulsating in anus; bearing down towards anus.
- Sore feeling in anus when getting up in the morning.
Causticum:
- Frequent, sudden, penetrating, additionally Pressive pain in rectum.
- Anus very sensitive to contact.
- Itching also sticking in rectum.
Hydrastis:
- It occurs with constipation, piles also ulceration.
- Offensive, dirty-looking discharge from anus, obliging him to wear a bandage.
Lachesis:
- In brief, It occurs in drunkards with tendency to pulmonary complications.
Nux Vomica:
- Gastritis also constipation, aggravation after mental exertions, after eating
Phosphorous:
- Ulceration of rectum, with discharge of pus also blood.
- Moreover, Tuberculosis in tall, slender, rapidly growing persons, suffering from frequent bronchial attacks.
Silicea:
Diet & Regimen
Diet & Regimen
Do’s:
- Eat different coloured fresh vegetables and fruits.
- Additionally, Eat whole grains instead of refined foods.
- Then, Drink plenty of liquids.
- Use clean and hygiene dresses to avoid infection.
- All in all, To reduce the inflammation, take omega-3 rich fatty fishes.
Don’ts:
- Don’t have heavy meals at once.
- After that, Never sleep immediately after a heavy meal.
- Then, Avoid spicy and salty foods.
- Never stop your urge to defecate.
- Besides this, Never drink much water with meals.
- Don’t use cleaning agents especially in the effected region too often. [6]
Do’s and Don'ts
Do’s & Don’ts
While this book Clinical Practice in Pediatric Surgery, primarily focuses on pediatric surgery, the principles for fistula management apply to all age groups. Here’s a summary of the do’s and don’ts for fistula care based on general surgical principles and information from this reference:
Do’s:
Keep the area clean and dry:
Gently clean the area around the fistula with mild soap and water after each bowel movement or as directed by your doctor. Pat dry or use a hairdryer on a cool setting.
Apply warm compresses:
Warm compresses can help promote blood flow and healing.
Take prescribed medications:
If antibiotics or pain relievers are prescribed, take them as directed.
Follow a high-fiber diet:
Eating plenty of fruits, vegetables, and whole grains can help soften stools and reduce the risk of constipation, which can worsen fistula symptoms.
Drink plenty of fluids:
Staying hydrated is important for overall health and can help prevent constipation.
Attend follow-up appointments:
Regular checkups with your doctor are important to monitor healing and address any concerns.
Don’ts:
Don’t scratch or pick at the fistula:
This can damage the tissue and delay healing.
Don’t use harsh soaps or chemicals:
These can irritate the skin and delay healing.
Don’t wear tight-fitting clothing:
Tight clothing can rub against the fistula and cause irritation.
Don’t ignore signs of infection:
If you notice increased pain, swelling, redness, or drainage, contact your doctor.
Don’t strain during bowel movements:
Straining can put pressure on the fistula and delay healing.
Additional tips (not specifically mentioned in the book):
Consider using a barrier cream:
Applying a barrier cream around the fistula can help protect the skin from irritation caused by drainage.
Wear loose-fitting cotton underwear:
This can help keep the area dry and reduce friction.
Take sitz baths:
Soaking in a warm sitz bath can help soothe discomfort and promote healing.
It’s important to consult with your doctor for personalized advice and treatment recommendations based on your specific type of fistula and individual needs.[16]
Terminology
Terminology
Absolutely! Here are some common terminologies used in articles about fistulas, along with their meanings:
General Terms:
- Fistula: An abnormal connection between two epithelial surfaces (e.g., organs, blood vessels, skin).
- Tract: The tunnel-like pathway of a fistula.
- Epithelialization: The process of the fistula tract becoming lined with epithelial tissue, making it more stable and resistant to closure.
- Abscess: A collection of pus that can form due to infection and may lead to fistula development.
- Drainage: The fluid that leaks from a fistula, which can vary in composition depending on the fistula‘s location (e.g., pus, stool, urine).
- Incontinence: The inability to control bowel or bladder movements, which can be a complication of some fistulas.
Specific Fistula Types:
- Obstetric fistula: A fistula that develops between the vagina and bladder or rectum due to prolonged obstructed labor.
- Anal fistula: A fistula that connects the anal canal to the skin near the anus.
- Enterocutaneous fistula: A fistula that connects the intestine to the skin.
- Rectovaginal fistula: A fistula that connects the rectum and vagina.
- Vesicovaginal fistula: A fistula that connects the bladder and vagina.
Diagnostic Terms:
- Fistulography: An imaging procedure that involves injecting contrast dye into the fistula tract to visualize its anatomy.
- MRI (Magnetic Resonance Imaging): A noninvasive imaging technique used to visualize the fistula and surrounding tissues.
- CT Scan (Computed Tomography): Another imaging technique used to evaluate fistulas, especially deep pelvic fistulas.
- Endoscopy: A procedure used to visualize the inside of the body with a flexible tube equipped with a camera. It can be used to assess fistulas in the gastrointestinal tract.
Treatment Terms:
- Fistulization: The surgical creation of a fistula (usually temporary) for therapeutic purposes, such as draining an abscess.
- Fistuloctomy: A surgical procedure to excise (remove) the fistula tract.
- Seton placement: A surgical technique where a thread or rubber band is placed through the fistula tract to promote drainage and gradual healing.
- Fibrin glue: A biological adhesive used to seal fistula tracts.
Additional Terms:
- Etiology: The cause or origin of the fistula.
- Pathophysiology: The processes involved in the development and progression of the fistula.
- Morbidity: The illness or disability caused by the fistula.
- Prognosis: The likely course and outcome of the fistula.
I hope this helps! Let me know if you have any other questions.
In homeopathic articles discussing fistula, you’ll encounter a mix of standard medical terms and homeopathic-specific terminology:
Standard Medical Terms:
- Fistula: As defined before, an abnormal connection between two body parts.
- Abscess: A collection of pus, often the precursor to a fistula.
- Infection: The presence of harmful microorganisms, often the root cause of fistula formation.
- Inflammation: The body’s response to injury or infection, characterized by swelling, pain, and redness.
- Suppuration: The formation or discharge of pus.
Homeopathic-Specific Terms:
- Miasm: In homeopathy, a miasm is a predisposition to certain types of diseases, believed to be inherited. The three main miasms are psora (related to skin conditions and functional disorders), sycosis (related to overgrowth and chronic inflammation), and syphilis (related to destructive processes).
- Remedy: A homeopathic medicine, usually derived from plants, minerals, or animals, and highly diluted.
- Potency: The degree of dilution of a homeopathic remedy. Higher potencies are believed to be more powerful.
- Proving: A systematic process of testing a substance on healthy individuals to determine its potential effects as a homeopathic remedy.
- Repertory: A reference book used by homeopaths to find remedies based on specific symptoms.
- Materia Medica: A comprehensive reference book that describes the properties and therapeutic uses of homeopathic remedies.
- Constitutional Treatment: A holistic approach to homeopathic treatment that takes into account the individual’s overall physical, mental, and emotional state.
- Aggravation: A temporary worsening of symptoms after taking a homeopathic remedy, often seen as a positive sign of healing.
Homeopathic Remedies Often Mentioned for Fistula:
- Silicea: Often used for chronic, recurrent fistulas with slow healing.
- Hepar sulphuris calcareum: For fistulas with pus formation and sensitivity to touch.
- Calcarea sulphurica: For fistulas with yellow, thick discharge.
- Myristica sebifera: For fistulas with pain and a tendency to bleed.
- Berberis vulgaris: For fistulas associated with urinary tract issues.
Important Note: Homeopathy is a complementary and alternative medicine system. While some people report positive experiences, it is important to consult with both a conventional medical doctor and a qualified homeopath for a comprehensive approach to fistula treatment.
References
References
- Bailey_and_Love_s_Short_Practice_of_Surgery
- Clinical Surgery S. Das
- Manipal Manual of Surgery (PDF Drive)
- SRB_s Manual of Surgery, 3rd Edition
- SRB’s Clinical Methods in Surgery
- https://www.lybrate.com/topic/diet-for-fistula?utm_source=indo&utm_medium=cps&utm_campaign=gkart&lpt=AFLT_INDO
- Homeopathic Therapeutics by Lilienthal
- Obstetric fistula in India: current scenario (2009).
- Fistula in Ano—A 2-Year Prevalence Study on North Indian Rural Population (2022).
Schwartz’s Principles of Surgery, 11th Edition,Writers: F. Charles Brunicardi, Dana K. Andersen, Timothy R. Billiar, David L. Dunn, John G. Hunter, Jeffrey B. Matthews, Raphael E. Pollock
(2019),Publisher: McGraw Hill Professional.Sabiston Textbook of Surgery, 21st Edition,Writers: Courtney M. Townsend Jr., R. Daniel Beauchamp, Kenneth L. Mattox, B. Mark Evers,(2022),Publisher: Elsevier.
Diagnosis and Treatment of Anal Fistula,Editors: Renjie Shi, Lihua Zheng,(2021),Publisher: Springer Singapore.
Sleisenger and Fordtran’s Gastrointestinal and Liver Disease, 11th Edition,Writers: Mark Feldman, Lawrence S. Friedman, Lawrence J. Brandt,(2021),Publisher: Elsevier
Book: Current Therapy in Colon and Rectal Surgery, 2nd Edition,Editor: Steven D. Wexner,(2014),Publisher: Elsevier.
Book: Williams Obstetrics, 25th Edition,Writers: F. Gary Cunningham, Kenneth J. Leveno, Steven L. Bloom, Catherine Y. Spong, Jodi S. Dashe
(2018),Publisher: McGraw Hill Professional.Book: Clinical Practice in Pediatric Surgery, 2nd Edition,Writers: Arnold G. Coran, N. Scott Adzick
(2012),Publisher: CRC Press.
Also Search As
Also Search As
People can search for homeopathic articles on fistula in a variety of ways:
Specific Search Queries:
- Using keywords: Combine terms like "homeopathy," "fistula," "treatment," "remedies," and specific remedy names (e.g., "Silicea fistula").
- Adding modifiers: Include terms like "case studies," "articles," "research," or "journals" to refine results.
- Including synonyms: Search for related terms like "natural treatment," "alternative medicine," or "holistic approach" for fistula.
Search Engines:
- Google: The most popular search engine, offers a wide range of results. Try using different combinations of keywords to refine your search.
- DuckDuckGo: A privacy-focused search engine that can offer different results than Google.
- Specialized search engines: Consider using search engines specific to health or homeopathy for more targeted results.
Online Resources:
- Homeopathic websites and blogs: Many websites and blogs are dedicated to homeopathy and may have articles on fistula. Look for reputable sources with qualified practitioners.
- Homeopathic journals and publications: Search online databases for homeopathic journals or publications that may contain relevant articles.
- Homeopathic forums and communities: Online forums and communities can be a good place to ask questions and connect with others who have experience with homeopathy for fistula.
Tips:
- Be specific in your search terms: The more specific your search, the more relevant the results will be.
- Use quotation marks for exact phrases: Putting phrases in quotation marks will ensure that the exact phrase is searched for.
- Use Boolean operators: Words like "AND," "OR," and "NOT" can help refine your search.
- Look for reputable sources: Not all information online is accurate or reliable. Look for articles from reputable homeopathic organizations or practitioners.
- Consult with a qualified homeopath: The best way to get personalized information about homeopathic treatment for fistula is to consult with a qualified homeopath.
By utilizing these strategies and resources, individuals can find valuable information about the homeopathic approach to fistula treatment.
There are several ways to search for information about fistulas, depending on your needs and the type of information you’re looking for:
General Search:
- Search Engines (Google, Bing, DuckDuckGo): Use broad search terms like "fistula," "types of fistulas," or "fistula treatment" to get a general overview of the topic.
- Online Encyclopedias (Wikipedia, MedlinePlus): These can provide basic information about fistulas, including their causes, symptoms, and treatment options.
Specific Types of Fistulas:
- Include the type of fistula: If you’re interested in a specific type of fistula, include it in your search terms (e.g., "anal fistula," "obstetric fistula," or "enterocutaneous fistula").
- Search for specific symptoms: If you have specific symptoms, include them in your search (e.g., "fistula pain," "fistula discharge," or "fistula incontinence").
Medical Information:
- Reputable Medical Websites (Mayo Clinic, Cleveland Clinic, etc.): These websites often have detailed information about different types of fistulas, their causes, symptoms, diagnosis, and treatment options.
- Medical Journals and Databases (PubMed, Google Scholar): Search for scientific articles and research studies on fistula for in-depth information.
Alternative Treatments:
- Homeopathic Websites and Forums: Search for websites or forums dedicated to homeopathy to find information on homeopathic approaches to fistula treatment.
- Naturopathic Websites and Blogs: These may provide information on natural remedies and lifestyle changes that could be helpful for managing fistulas.
Additional Tips:
- Use specific search terms: Instead of just searching for "fistula," use more specific terms like "fistula surgery," "fistula causes," or "fistula complications."
- Use quotation marks: Enclose phrases in quotation marks to search for the exact phrase (e.g., "fistula treatment options").
- Use Boolean operators: Combine search terms with words like "AND," "OR," and "NOT" to refine your search (e.g., "fistula AND surgery NOT Crohn’s disease").
- Consult with a doctor: If you have concerns about a fistula, always consult with a healthcare professional for personalized advice and treatment recommendations.
Frequently Asked Questions (FAQ)
What causes Fistula?
Causes
- Congenital
- Trauma
- Instrumental
- Surgical
- Inflammatory
- Malignancy
Give the types of Fistula?
Types
- Oro-cutaneous
- Branchial
- Thyroglossal
- Enterocutaneous
- Appendicular
- Tracheoesophageal
- Cholecysto duodenal
- Colovesical
- Recto-vesical
Homeopathic Medicines used by Homeopathic Doctors in treatment of Fistula?
Homoeopathic Medicine for Fistula
- Berberis
- Calcarea Phos
- Causticum
- Hydrastis
- Lachesis
- Nux Vomica
- Phosphorous
- Silicea
Can homeopathy help with fistulas?
Homeopathy aims to stimulate the body’s natural healing response and address the underlying factors contributing to fistula formation. While some studies suggest potential benefits, more research is needed to confirm its effectiveness.
How does homeopathic treatment for fistulas work?
A homeopathic practitioner will conduct a detailed consultation to understand your specific symptoms, medical history, and overall constitution. Based on this information, they will prescribe a personalized remedy to address your individual needs.
How long does homeopathic treatment for fistulas take?
The response time to homeopathic treatment varies depending on the individual, the type of fistula, and its severity. Chronic fistulas may require longer-term treatment.
Can I take homeopathic remedies alongside conventional treatments for fistulas?
It’s generally safe to combine homeopathic remedies with conventional treatments for fistulas. However, inform your doctor and homeopath about all medications and treatments you are using.
What lifestyle changes can help with fistulas?
Maintaining good hygiene, eating a healthy diet, managing stress, and avoiding constipation can support healing and prevent complications.
