Infertility
Definition
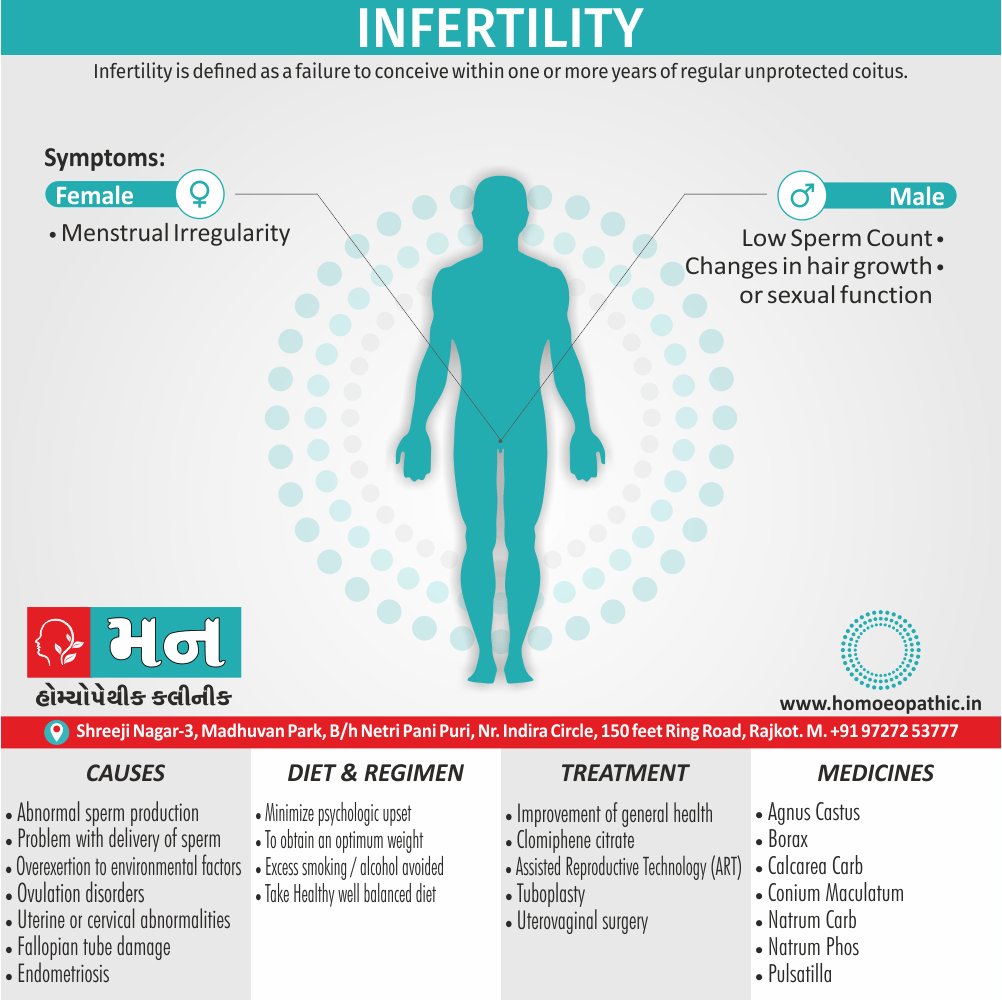
Infertility is defined as a failure to conceive within one or more years of regular unprotected coitus.
While there aren’t perfect synonyms for infertility, here are some options depending on the context and desired nuance:
Formal synonyms:
- Sterility: This term emphasizes the complete inability to conceive.
- Subfertility: This refers to a reduced ability to conceive compared to the average population.
Neutral terms:
- Reproductive challenges: This is a broader term that encompasses various difficulties related to conception.
- Family building difficulties: This focuses on the desired outcome (family building) rather than the medical issue.
- Unexplained infertility: This describes cases where the cause of infertility is unknown.
Informal terms (use with caution):
- Trouble getting pregnant: This is a very general term easily understood by most audiences but might lack precision.
- Being unable to conceive: Similar to "trouble getting pregnant" but emphasizes the inability to achieve pregnancy.
What to avoid:
- Barren: This term can be considered insensitive as it has connotations of being unproductive or empty.
- Impotent: This term usually refers to erectile dysfunction in males and is not an accurate synonym for infertility.
Choosing the best option:
The best choice depends on your audience, the purpose of your communication, and the desired level of formality.
- For medical contexts, "infertility" or the more specific terms like "sterility" or "subfertility" are most appropriate.
- When addressing individuals or couples struggling with infertility, neutral terms like "reproductive challenges" or "family building difficulties" might be more sensitive.
- If targeting a general audience, "trouble getting pregnant" can be understood, but consider following up with more specific information.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Infertility
Eighty percent of the couples achieve conception if they so desire, within one year of having regular intercourse with adequate frequency (4–5 times a week).
Another 10 percent will achieve the objective by the end of second year. As such, 10 percent remain infertile by the end of second year.
Factors Essential for Conception
- Healthy spermatozoa should be deposited high in the vagina at or near the cervix (male factor).
- The spermatozoa should undergo changes (capacitation, acrosome reaction) and acquire motility (cervical factor).
- The motile spermatozoa should ascend through the cervix into the uterine cavity and the fallopian tubes.
- There should be ovulation (ovarian factor).
- The fallopian tubes should be patent and the oocyte should be picked up by the fimbriated end of the tube (tubal factor).
- The spermatozoa should fertilize the oocyte at the ampulla of the tube.
- The embryo should reach the uterine cavity after 3–4 days of fertilization.
- The endometrium should be receptive (by Estrogen, progesterone, IGF-l, cytokines, integrins) for implantation, and the corpus luteum should function adequately.
Epidemiology
Epidemiology
The epidemiology of infertility in India is a complex and evolving issue, with various studies highlighting different aspects and prevalence rates.
- Recent findings from a nationally representative survey conducted during 2019-21 (published in 2023) revealed that the overall prevalence of infertility in India is 18.7 per 1,000 women among those married for at least five years and currently in union. This prevalence increases as the duration of marriage decreases. State-level analysis showed that regions such as Goa, Lakshadweep, and Chhattisgarh exhibit the highest burdens of infertility. (Infertility Burden Across Indian States: Insights from a Nationally Representative Survey Conducted During 2019-21)[4]
- A study published in PLOS ONE in 2023, "Surging trends of infertility and its behavioural determinants in India," delved into the socioeconomic and demographic factors affecting primary and secondary infertility. They found that while primary infertility decreased with age, secondary infertility increased. Urban areas showed a slightly higher prevalence of both types of infertility compared to rural areas. Additionally, the study highlighted associations between certain medical conditions (thyroid, diabetes, cancer) and the use of certain contraceptives with secondary infertility.[5]
- Another 2023 study, "Study of demographic profile and causative factor in female infertility," focused on female infertility, revealing that 57.33% of infertile women experienced primary infertility, while 42.66% had secondary infertility. The 26-30 age group was the most affected, and a majority of these women resided in rural areas. Pelvic inflammatory disease, polycystic ovarian syndrome, myoma of the uterus, and other factors were identified as significant contributors to female infertility.[6]
These studies collectively underscore the multifaceted nature of infertility in India, emphasizing the need for targeted interventions and policy measures to address this growing public health concern. The establishment of a national infertility surveillance system is crucial for monitoring trends and informing effective strategies to tackle this issue.
Epidemiology
The epidemiology of infertility in India is a complex and evolving issue, with various studies highlighting different aspects and prevalence rates.
- Recent findings from a nationally representative survey conducted during 2019-21 (published in 2023) revealed that the overall prevalence of infertility in India is 18.7 per 1,000 women among those married for at least five years and currently in union. This prevalence increases as the duration of marriage decreases. State-level analysis showed that regions such as Goa, Lakshadweep, and Chhattisgarh exhibit the highest burdens of infertility. (Infertility Burden Across Indian States: Insights from a Nationally Representative Survey Conducted During 2019-21)[4]
- A study published in PLOS ONE in 2023, "Surging trends of infertility and its behavioural determinants in India," delved into the socioeconomic and demographic factors affecting primary and secondary infertility. They found that while primary infertility decreased with age, secondary infertility increased. Urban areas showed a slightly higher prevalence of both types of infertility compared to rural areas. Additionally, the study highlighted associations between certain medical conditions (thyroid, diabetes, cancer) and the use of certain contraceptives with secondary infertility.[5]
- Another 2023 study, "Study of demographic profile and causative factor in female infertility," focused on female infertility, revealing that 57.33% of infertile women experienced primary infertility, while 42.66% had secondary infertility. The 26-30 age group was the most affected, and a majority of these women resided in rural areas. Pelvic inflammatory disease, polycystic ovarian syndrome, myoma of the uterus, and other factors were identified as significant contributors to female infertility.[6]
These studies collectively underscore the multifaceted nature of infertility in India, emphasizing the need for targeted interventions and policy measures to address this growing public health concern. The establishment of a national infertility surveillance system is crucial for monitoring trends and informing effective strategies to tackle this issue.
Causes
Causes of Infertility
Male infertility
These may include:
Abnormal sperm production or function
- Due to undescended testicles, genetic defects, health problems such as diabetes, or infections such as chlamydia, gonorrhea, mumps or HIV.
- Enlarged veins in the testes (varicocele) also can affect the quality of sperm.
Problems with the delivery of sperm
- Due to sexual problems, such as premature ejaculation; certain genetic diseases, such as cystic fibrosis; structural problems, such as a blockage in the testicle; or damage or injury to the reproductive organs.
Overexposure to certain environmental factors
- Such as pesticides and other chemicals, and radiation.
- Cigarette smoking, alcohol, marijuana, anabolic steroids, and taking medications to treat bacterial infections, high blood pressure and depression also can affect fertility.
- Frequent exposure to heat, such as in saunas or hot tubs, can raise body temperature and may affect sperm production.
Damage related to cancer and its treatment
- Including radiation or chemotherapy.
- Treatment for cancer can impair sperm production, sometimes severely.
Female infertility
Causes of female infertility may include:
Ovulation disorders
- Affect the release of eggs from the ovaries.
- These include hormonal disorders such as polycystic ovary syndrome.
- Hyperprolactinemia, a condition in which you have too much prolactin — the hormone that stimulates breast milk production — also may interfere with ovulation.
- Either too much thyroid hormone (hyperthyroidism) or too little (hypothyroidism) can affect the menstrual cycle or cause infertility.
- Other underlying causes may include too much exercise, eating disorders or tumors.
Uterine or cervical abnormalities
- Including abnormalities with the cervix, polyps in the uterus or the shape of the uterus.
- Noncancerous (benign) tumors in the uterine wall (uterine fibroids) may cause infertility by blocking the fallopian tubes or stopping a fertilized egg from implanting in the uterus.
Fallopian tube damage or blockage
Often caused by inflammation of the fallopian tube (salpingitis).
- This can result from pelvic inflammatory disease, which is usually caused by a sexually transmitted infection, endometriosis or adhesions.
Endometriosis
- It occurs when endometrial tissue grows outside of the uterus, may affect the function of the ovaries, uterus and fallopian tubes.
Primary ovarian insufficiency (early menopause)
- When the ovaries stop working and menstruation ends before age 40.
- Although the cause is often unknown, certain factors are associated with early menopause, including immune system diseases, certain genetic conditions such as Turner syndrome or carriers of Fragile X syndrome, and radiation or chemotherapy treatment.
Pelvic adhesions
- Bands of scar tissue that bind organs that can form after pelvic infection, appendicitis, endometriosis or abdominal or pelvic surgery.
Cancer and its treatment
- Certain cancers — particularly reproductive cancers — often impair female fertility.
- Both radiation and chemotherapy may affect fertility.[3]
Types
Classification of Infertility
Types of infertility i.e.:
Primary Infertility
A woman who was never pregnant and who can’t conceive after one year of not using birth control.
Secondary Infertility
Secondary Infertility occurs when a woman can’t get pregnant again after having at least one successful pregnancy.[3]
Risk Factors
Risk factor of Infertility
Many of the risk factors for both male and female infertility are the same. They include:
Age
- Women’s fertility gradually declines with age, especially in the mid-30s, and it drops rapidly after age 37.
- Infertility in older women is likely due to the lower number and quality of eggs, and can also be due to health problems that affect fertility.
- Men over age 40 may be less fertile than younger men.
Tobacco use
- Smoking tobacco or marijuana by either partner may reduce the likelihood of pregnancy.
- Smoking also reduces the possible effectiveness of fertility treatment.
- Miscarriages are more frequent in women who smoke.
- Smoking can increase the risk of erectile dysfunction and a low sperm count in men.
Alcohol use
- For women, there’s no safe level of alcohol use during conception or pregnancy.
- Alcohol use may contribute to infertility.
- For men, heavy alcohol use can decrease sperm count and motility.
Being higher-weight person
- Among American women, an inactive lifestyle and being higher-weight person may increase the risk of infertility.
- For men, sperm count also may be affected by being higher-weight person.
Being underweight
- Women at risk of fertility problems include those with eating disorders, such as anorexia or bulimia, and those who follow a very low-calorie or restrictive diet.
Exercise issues
- Basically, A lack of exercise contributes to obesity, which increases the risk of infertility.
- Less often, ovulation problems may be associated with frequent strenuous, intense exercise in women who are not higher-weight person.[3]
Pathogenesis
Pathogenesis of Infertility
Infertility is defined as the inability to conceive after 12 months of regular unprotected intercourse in women younger than 35 years or after 6 months in women 35 years or older. The pathogenesis of infertility is multifactorial and can involve both male and female factors.
Female Factors
- Ovulatory Dysfunction: This is the most common cause of female infertility and can be due to a variety of factors, including polycystic ovary syndrome (PCOS), hypothalamic amenorrhea, premature ovarian insufficiency, and hyperprolactinemia. These conditions disrupt the normal hormonal feedback mechanisms that regulate ovulation.
- Tubal and Pelvic Pathology: Damage to the fallopian tubes due to pelvic inflammatory disease, endometriosis, or previous surgery can prevent the egg from meeting the sperm or the fertilized egg from implanting in the uterus.
- Uterine Factors: Uterine fibroids, polyps, or congenital anomalies can interfere with embryo implantation or growth.
- Cervical Factors: Cervical stenosis or abnormal cervical mucus can impede sperm transport.
Male Factors
- Spermatogenesis Disorders: These disorders affect sperm production or maturation and can be caused by genetic factors, infections, varicocele, hormonal imbalances, or environmental toxins.
- Sperm Transport Disorders: Obstruction of the vas deferens or ejaculatory ducts can prevent sperm from reaching the ejaculate.
- Sexual Dysfunction: Erectile dysfunction or ejaculatory problems can prevent sperm from being deposited in the female reproductive tract.
Combined Factors
In some cases, infertility may be due to a combination of male and female factors or unexplained factors.
Understanding the pathogenesis of infertility is essential for diagnosis and treatment. A thorough evaluation of both partners is necessary to identify the underlying cause(s) and develop an appropriate treatment plan.[7]
Pathophysiology
Pathophysiology
The pathophysiology of infertility encompasses a wide array of factors that can disrupt the complex process of reproduction in both males and females.
Female Infertility
- Ovulatory Dysfunction: This is the most common cause of female infertility, often stemming from hormonal imbalances, polycystic ovary syndrome (PCOS), hypothalamic amenorrhea, premature ovarian insufficiency (POI), or hyperprolactinemia.
- Tubal and Pelvic Pathology: Damage or blockage of the fallopian tubes due to infections, endometriosis, or previous surgeries can prevent the egg from meeting the sperm.
- Uterine Factors: Abnormalities in the uterus, such as fibroids, polyps, or congenital anomalies, can hinder implantation and pregnancy.
- Cervical Factors: Cervical stenosis, inadequate mucus production, or antisperm antibodies can impede sperm transport.
Male Infertility
- Impaired Spermatogenesis: This can be caused by genetic factors, hormonal imbalances, testicular infections or injuries, varicocele (enlarged veins in the scrotum), or exposure to toxins.
- Sperm Transport Disorders: Blockage of the epididymis or vas deferens can prevent sperm from reaching the ejaculate.
- Sexual Dysfunction: Erectile dysfunction or ejaculatory problems can interfere with sperm delivery. [7]
Clinical Features
Clinical Features of Infertility
In Women:
Absence of conception: The primary clinical feature of infertility is the inability to conceive despite regular, unprotected sexual intercourse for at least 12 months.
Menstrual irregularities: This may include irregular periods, abnormally heavy or light bleeding, or the absence of menstruation (amenorrhea).
Pain during intercourse (dyspareunia): This can be a sign of underlying conditions like endometriosis or pelvic inflammatory disease.
Hormonal imbalances: Symptoms like acne, hirsutism (excess hair growth), and weight changes may indicate hormonal problems.
Pelvic pain or discomfort: This may be due to conditions like ovarian cysts, fibroids, or endometriosis.
In Men:
Changes in sexual function: This may include difficulty with erections or ejaculation, reduced sexual desire, or problems with sperm production or quality.
Pain, lump, or swelling in the testicles: These can be signs of underlying medical conditions affecting male fertility.
Hormonal imbalances: Symptoms like reduced facial or body hair growth, breast development, or changes in muscle mass may suggest hormonal issues.
Small or firm testicles: These can be indicators of testicular dysfunction.[8]
Sign & Symptoms
Sign & Symptoms of Infertility
- The main symptom of infertility is not getting pregnant.
- There may be no other obvious symptoms.
- Sometimes, a woman with infertility may have irregular or absent menstrual periods.
- In some cases, a man with infertility may have some signs of hormonal problems, such as changes in hair growth or sexual function.
Clinical Examination
Clinical Examination of Infertility
The clinical examination of infertility is a comprehensive process aimed at identifying potential causes of infertility in both male and female partners. It involves a detailed medical history, physical examination, and specific tests tailored to each individual.
Detailed Clinical Examination:
Medical History:
- Female Partner: Age, duration of infertility, menstrual history, previous pregnancies, history of pelvic infections, surgeries, or sexually transmitted infections.
- Male Partner: Age, duration of infertility, medical history, previous paternity, history of testicular trauma, infections, surgeries, or sexually transmitted infections.
Physical Examination:
- Female Partner: General physical examination, pelvic examination (to assess the uterus, ovaries, and fallopian tubes), breast examination.
- Male Partner: General physical examination, genital examination (to assess the penis, testes, and scrotum), digital rectal examination (to assess the prostate).
Specific Tests:
Female Partner:
- Ovulation Assessment: Basal body temperature charting, ovulation predictor kits, serum progesterone levels.
- Tubal Patency Assessment: Hysterosalpingography (HSG), laparoscopy with dye test.
- Ovarian Reserve Assessment: Anti-Müllerian hormone (AMH) levels, antral follicle count (AFC).
- Hormonal Profile: Thyroid function tests, prolactin levels, follicle-stimulating hormone (FSH) and luteinizing hormone (LH) levels.
- Other Tests: Pelvic ultrasound, endometrial biopsy.
Male Partner:
- Semen Analysis: Assessment of sperm count, motility, morphology, and other parameters.
- Hormonal Profile: Testosterone levels, FSH and LH levels.
- Other Tests: Genetic testing, testicular biopsy.
Additional Investigations (if needed):
- Postcoital test
- Immunological tests
- Genetic testing[9].
Diagnosis
Diagnosis of Infertility
- Before infertility testing, your doctor or clinic works to understand your sexual habits and may make recommendations to improve your chances of getting pregnant.
- In some infertile couples, no specific cause is found (unexplained infertility).
- Infertility evaluation can be expensive, and sometimes involves uncomfortable procedures. Some medical plans may not cover the cost of fertility treatment.
- Finally, there’s no guarantee — even after all the testing and counseling — that you’ll get pregnant.
Tests for men
Male fertility requires that the testicles produce enough healthy sperm, and that the sperm is ejaculated effectively into the vagina and travels to the egg. Tests for male infertility attempt to determine whether any of these processes are impaired.
You may have a general physical exam, including examination of your genitals. Specific fertility tests may include:
Semen analysis
- Your doctor may ask for one or more semen specimens.
- Semen is generally obtained by masturbating or by interrupting intercourse and ejaculating your semen into a clean container.
- A lab analyzes your semen specimen. In some cases, urine may be tested for the presence of sperm.
Hormone testing
- You may have a blood test to determine your level of testosterone and other male hormones.
Genetic testing
- Genetic testing may do to determine whether there’s a genetic defect causing infertility.
Testicular biopsy
- In select cases, a testicular biopsy may perform to identify abnormalities contributing to infertility or to retrieve sperm for assist reproductive techniques, such as IVF.
Imaging
- In certain situations, imaging studies such as a brain MRI, transrectal or scrotal ultrasound, or a test of the vas deferens (vasography) may perform.
Other specialty testing
- In rare cases, other tests to evaluate the quality of the sperm may perfor, such as evaluating a semen specimen for DNA abnormalities.[3]
Tests for women
Generally, Fertility for women relies on the ovaries releasing healthy eggs. Moreover, The reproductive tract must allow an egg to pass into the fallopian tubes and join with sperm for fertilization.
The fertilized egg must travel to the uterus also implant in the lining. In detail, Tests for female infertility try to find out if any of these processes are impaired.
Besides this, You may have a general physical exam, including a regular gynaecological exam. Specific fertility tests may include i.e.:
Ovulation testing
- In brief, A blood test measures hormone levels to determine whether you’re ovulating.
Hysterosalpingography
- Hysterosalpingography evaluates the condition of your uterus also fallopian tubes and looks for blockages or other problems.
- X-ray contrast is injected into your uterus, and an X-ray is taken to determine if the cavity is normal also to see if the fluid spills out of your fallopian tubes.
Ovarian reserve testing
- This testing helps determine the quantity of the eggs available for ovulation.
- This approach often begins with hormone testing early in the menstrual cycle.
Other hormone testing
- Other hormone tests check levels of ovulatory hormones, as well as pituitary hormones that control reproductive processes.
Imaging tests
- Pelvic ultrasound looks for uterine or ovarian disease.
- Sometimes a sonohysterogram, also called a saline infusion sonogram, is used to see details inside the uterus that are not seen on a regular ultrasound.
Depending on your situation, rarely your testing may include:
Hysteroscopy
- Depending on your symptoms, your doctor may request a hysteroscopy to look for uterine disease.
- During the procedure, your doctor inserts a thin, lighted device through your cervix into your uterus to view any potential abnormalities.
Laparoscopy
- This minimally invasive surgery involves making a small incision beneath your navel and inserting a thin viewing device to examine your fallopian tubes, ovaries and uterus.
- A laparoscopy may identify endometriosis, scarring, blockages or irregularities of the fallopian tubes, and problems with the ovaries and uterus.[3]
Differential Diagnosis
Differential diagnosis
The differential diagnosis for infertility is extensive and can vary depending on whether the issue lies with the male or female partner, or both.
Female Infertility:
- Ovulatory disorders: Polycystic ovary syndrome (PCOS), hypothalamic amenorrhea, premature ovarian failure
- Tubal factors: Pelvic inflammatory disease (PID), endometriosis, previous ectopic pregnancy
- Uterine factors: Fibroids, polyps, congenital anomalies
- Cervical factors: Cervical stenosis, antisperm antibodies
Male Infertility:
- Sperm disorders: Azoospermia, oligospermia, asthenospermia, teratospermia
- Testicular factors: Varicocele, cryptorchidism, trauma
- Hormonal factors: Hypogonadotropic hypogonadism, hyperprolactinemia
- Ejaculatory disorders: Retrograde ejaculation, erectile dysfunction
Combined Factors:
- Unexplained infertility: No identifiable cause after comprehensive evaluation
- Genetic factors: Chromosomal abnormalities, single gene mutations
- Immunologic factors: Antisperm antibodies in either partner[10]
Complications
Complications
Infertility, whether primary or secondary, can have a profound impact on individuals and couples, leading to various complications that extend beyond the inability to conceive.
Psychological Complications:
- Emotional Distress: Infertility often triggers a range of negative emotions, including sadness, anger, guilt, anxiety, and depression. These feelings can strain relationships and affect overall well-being.
- Stress: The diagnosis and treatment of infertility can be incredibly stressful, leading to heightened anxiety, sleep disturbances, and difficulty concentrating.
- Relationship Issues: Infertility can put a significant strain on relationships, leading to conflicts, decreased intimacy, and feelings of isolation.
Social Complications:
- Stigma: In many cultures, infertility is still stigmatized, leading to feelings of shame, social isolation, and discrimination.
- Financial Burden: The cost of infertility treatments can be exorbitant, causing financial stress and hardship for couples.
Medical Complications (associated with treatment):
- Ovarian Hyperstimulation Syndrome (OHSS): This is a potentially serious complication of fertility medications, causing enlarged ovaries, fluid buildup in the abdomen, and other symptoms.
- Multiple Pregnancies: Fertility treatments can increase the risk of multiple pregnancies, which carry higher risks for both mother and babies.
- Ectopic Pregnancy: This is a life-threatening condition where the fertilized egg implants outside the uterus.
- Complications from Assisted Reproductive Technology (ART): ART procedures like in vitro fertilization (IVF) carry risks such as infection, bleeding, and adverse reactions to medications.[11]
Investigations
Investigations
Infertility investigations are a crucial step in diagnosing and managing infertility. They help identify the underlying causes and guide treatment decisions. Here are some common investigations mentioned in medical texts:
Female Infertility Investigations:
- Ovulation Assessment:
- Basal body temperature charting
- Serum progesterone levels
- Ovulation predictor kits
- Transvaginal ultrasound
- Tubal and Uterine Evaluation:
- Hysterosalpingography (HSG)
- Sonohysterography (SHG)
- Hysteroscopy
- Laparoscopy
- Hormonal Assessment:
- Follicle-stimulating hormone (FSH)
- Luteinizing hormone (LH)
- Estradiol
- Anti-Müllerian hormone (AMH)
- Thyroid function tests
- Other Tests:
- Genetic testing
- Infectious disease screening
- Imaging studies (e.g., pelvic MRI)
Male Infertility Investigations:
- Semen Analysis:
- Sperm count
- Motility
- Morphology
- Volume
- Hormonal Assessment:
- Testosterone
- FSH
- LH
- Other Tests:
- Genetic testing
- Testicular biopsy
- Ultrasound
Note: The specific investigations chosen will depend on the individual’s medical history, age, and other factors. It’s essential to consult with a healthcare professional to determine the most appropriate investigations for each case.[8]
Treatment
Treatment of Infertility
Infertility treatment depends on i.e.:
- What’s causing the infertility
- How long you’ve been infertile
- Your age also your partner’s age
- Personal preferences
Some causes of infertility can’t be corrected.
In cases where spontaneous pregnancy doesn’t happen, couples can often still achieve a pregnancy through use of assisted reproductive technology. Infertility treatment may involve significant financial, physical, psychological also time commitments.
Treatment for men
Men’s treatment for general sexual problems or lack of healthy sperm may include:
Changing lifestyle factors
- Improving lifestyle and certain behaviors can improve chances for pregnancy, including discontinuing select medications, reducing or eliminating harmful substances, improving frequency and timing of intercourse, exercising regularly, and optimizing other factors that may otherwise impair fertility.
Medications
- Certain medications may improve sperm count and likelihood for achieving a successful pregnancy.
- These medicines may increase testicular function, including sperm production and quality.
Surgery
- For some conditions, surgery may be able to reverse a sperm blockage and restore fertility.
- In other cases, surgically repairing a varicocele may improve overall chances for pregnancy.
Sperm retrieval
- These techniques obtain sperm when ejaculation is a problem or when no sperm are present in the ejaculated fluid.
- They may also be used in cases in which assisted reproductive techniques are planned and sperm counts are low or otherwise abnormal.[3]
Treatment for women
Some women need only one or two therapies to improve fertility. Other women may need several different types of treatment to achieve pregnancy.
Stimulating ovulation with fertility drugs
- Fertility drugs are the main treatment for women who are infertile due to ovulation disorders.
- These medications regulate or induce ovulation.
- Talk with your doctor about fertility drug options — including the benefits and risks of each type.
Intrauterine insemination (IUI)
- During IUI, healthy sperm are placed directly in the uterus around the time the ovary releases one or more eggs to be fertilized.
- Depending on the reasons for infertility, the timing of IUI can be coordinated with your normal cycle or with fertility medications.
Surgery to restore fertility
- Uterine problems such as endometrial polyps, a uterine septum, intrauterine scar tissue and some fibroids can be treated with hysteroscopic surgery.
- Endometriosis, pelvic adhesions, and larger fibroids may require laparoscopic surgery or surgery with a larger incision of the abdomen.
Assisted reproductive technology (ART)
Assisted reproductive technology (ART) is any fertility treatment in which the egg and sperm are handled. There are several types of ART.
In vitro fertilization (IVF) is the most common ART technique. IVF involves stimulating and retrieving multiple mature eggs, fertilizing them with sperm in a dish in a lab, and implanting the embryos in the uterus several days after fertilization.
Other techniques are sometimes used in an IVF cycle, such as:
Intracytoplasmic sperm injection (ICSI)
- A single healthy sperm is injected directly into a mature egg.
- ICSI is often used when there is poor semen quality or quantity, or if fertilization attempts during prior IVF cycles failed.
Assisted hatching
- This technique assists the implantation of the embryo into the lining of the uterus by opening the outer covering of the embryo (hatching).
Donor eggs or sperm
- Most ART is done using a couple’s own eggs and sperm.
- However, if there are severe problems with either the eggs or the sperm, you may choose to use eggs, sperm or embryos from a known or anonymous donor.
Gestational carrier
- Women who don’t have a functional uterus or for whom pregnancy poses a serious health risk might choose IVF using a gestational carrier.
- In this case, the couple’s embryo is placed in the uterus of the carrier for pregnancy.[3]
Prevention
Prevention of Infertility
Some types of infertility aren’t preventable. But several strategies may increase your chances of pregnancy.
Couples
- Have regular intercourse several times around the time of ovulation for the highest pregnancy rate.
- Intercourse beginning at least five days before and until a day after ovulation improves your chances of getting pregnant.
- Ovulation usually occurs in the middle of the cycle — halfway between menstrual periods — for most women with menstrual cycles about 28 days apart.
Men
Although most types of infertility aren’t preventable in men, these strategies may help:
- Avoid drug and tobacco use and drinking too much alcohol, which may contribute to male infertility.
- Avoid high temperatures found in hot tubs and hot baths, as they can temporarily affect sperm production and motility.
- Avoid exposure to industrial or environmental toxins, which can affect sperm production.
- Limit medications that may impact fertility,both prescription and nonprescription drugs. Talk with your doctor about any medications you take regularly, but don’t stop taking prescription medications without medical advice.
- Exercise moderately.Regular exercise may improve sperm quality and increase the chances for achieving a pregnancy.
Women
For women, a number of strategies may increase the chances of becoming pregnant:
- Quit smoking- Tobacco has many negative effects on fertility, not to mention your general health and the health of a fetus. If you smoke and are considering pregnancy, quit now.
- Avoid alcohol and street drugs-These substances may impair your ability to conceive and have a healthy pregnancy. Don’t drink alcohol or use recreational drugs, such as marijuana, if you’re trying to get pregnant.
- Limit caffeine-Women trying to get pregnant may want to limit caffeine intake. Ask your doctor for guidance on the safe use of caffeine.
- Exercise moderately- Regular exercise is important, but exercising so intensely that your periods are infrequent or absent can affect fertility.
- Avoid weight extremes- Being higher-weight person or underweight can affect your hormone production and cause infertility.[3]
Homeopathic Treatment
Homeopathic Treatment of Infertility
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Infertility:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
For Infertility in Women
Borax
- These medicines are recommended if there is acidic vaginal discharge.
- Such discharge typically kills the sperms.
- Thereby not allowing the fertilization.
- These medicines are effective when the discharge is acidic, whitish, copious and warm.
Calcarea Carbonica
- Calcarea Carbonica is normally administered to women who bleed a lot during their menstrual cycle or those with prolonged periods (known as menorrhagia), both of which can contribute to infertility.
- Females who experience these issues can also have irregular periods.
- When you experience a combination of the above symptoms, Calcarea Carbonica is the best medicine.
- Menorrhagia or prolonged periods may be accompanied by general body weakness and fatigue, anemia, or having a thick vaginal discharge that is whitish, greenish, or yellowish (also referred to as leucorrhoea).
- You can also take this medication if you have had many abortions or if you have early and heavy menstrual flow.
Aletris Farinosa
- Aletris Farinosa for infertility prescribe in case of early and copious menses.
- Other accompanying symptoms are – leucorrhoea, anaemia, weakness, fatigue with menorrhagia.
- It also recommend when a tendency of frequent abortions observe.
Pulsatilla
- Pulsatilla is great for females who have short and extremely light periods from the time they started having menstrual flow.
- If you fall in this category, you may notice that your periods come later than the expected date.
- Pulsatilla also use to treat infertility resulting from Polycystic Ovarian Disease (PCOD) which significantly contributes to infertility.
Sepia
- It prescribe when there is irregular or absent ovulation. Patient feels aversion to intercourse.
- Patient feels dryness and pain while intercourse.
- Menses are short, scanty and suppressed.
Agnus Castus
- Women with infertility who have low sex drive are usually put on Agnus Castus.
- This medication also recommend for women who constantly give excuses not to have sex.
- Most of the time when these two happen, you may also notice that your vaginal discharge is transparent in color.
- There may many reasons for a decrease interest in sex and Agnus Castus helps to fix this.
- Another variation of this scenario is when you have a low sex drive which accompany by excessive dryness which makes sex painful.
Natrum Carb
- Being unable to retain sperms means getting pregnant becomes an uphill task. Natrum Carb is therefore used in this scenario.
- If you have this issue, you may also experience thick, yellow, irritational vaginal discharge.
- Your periods may be short, come late or early, or heavy. In short, your periods may not be normal.
- This condition can also be accompanied by high sexual desire so you may wonder why you are having a lot of sex but are not getting pregnant.
- The solution lies in improving your semen retention levels by taking Natrum Carb.
Infertility in male:
Sabal Serrulata
- Sabal Serrulata is one of the best medicines for infertility in males with wasting (atrophy) of testes.
- It is also the perfect medicine for infertility in males with prostate enlargement or prostatitis.
Agnus Castus
- Agnus Castus use when a man’s sexual desire and physical ability reduce.
- The genitals stay relaxed, cold, and flaccid. Caladium use when infertility or impotency results because of mental depression.
- The genitals stay relaxed and weak erections are likely.
Selenium
Selenium use for erectile dysfunction featured by slow and weak erections. Involuntary semen discharge may also indicate as a symptom.
X-Ray
- The homeopathic medicine X-Ray is very effective in treating low sperm count in men.
- Sperm count gets increased, enhancing both the quantity and quality of sperm.
Conium
- Conium use for treating infertility in men, which occurs due to orchitis.
- The testicles get swollen, enlarged and hardened.
- Conium also helps patients with a history of suppressed sexual desire.
Caladium Seguinum
- Erectile dysfunction and premature ejaculation can effectively treated with Caladium Seguinum.
- In some men, erectile dysfunction results in pruritus in the genital organs.
- Caladium the best bet to deal with pruritus.
Diet & Regimen
Diet & Regimen for Infertility
Based on the principles of Ayurveda, the following diet and regimen recommendations can be beneficial for managing infertility:
Diet:
Foods to Include:
- Fresh fruits and vegetables (especially leafy greens, berries, and citrus fruits)
- Whole grains (brown rice, quinoa, oats)
- Legumes (lentils, beans, chickpeas)
- Nuts and seeds (almonds, walnuts, flaxseeds)
- Healthy fats (avocado, olive oil, ghee)
- Dairy products (milk, yogurt, paneer) in moderation
- Herbal teas (shatavari, ashwagandha, licorice)
Foods to Avoid:
- Processed foods
- Refined sugars
- Caffeine
- Alcohol
- Excessive spicy or fried foods
Regimen :
- Regular Exercise: Moderate exercise like yoga, walking, or swimming can improve blood circulation and hormonal balance.
- Stress Management: Practices like meditation, deep breathing exercises, and spending time in nature can help reduce stress levels.
- Adequate Sleep: Aim for 7-8 hours of quality sleep each night.
- Maintain a Healthy Weight: Being Higher weight or underweight can affect fertility.
- Abhyanga (Self-massage): Regular oil massage can improve circulation and relaxation.[12]
Do’s and Don'ts
The Do’s & Don’ts
Do’s:
- Seek medical advice: Consult a fertility specialist or reproductive endocrinologist for a comprehensive evaluation and personalized treatment plan.
- Maintain a healthy lifestyle: Eat a balanced diet, exercise regularly, and maintain a healthy weight.
- Manage stress: Practice relaxation techniques such as yoga, meditation, or deep breathing exercises.
- Get enough sleep: Aim for 7-8 hours of sleep per night to promote hormonal balance and overall well-being.
- Track your menstrual cycle: Monitor your ovulation patterns to optimize the timing of intercourse.
- Take prenatal vitamins: Folic acid and other essential nutrients can support healthy egg development and fetal growth.
- Communicate with your partner: Open and honest communication about your feelings and concerns can strengthen your relationship during this challenging time.
- Join a support group: Connecting with others who are experiencing infertility can provide emotional support and helpful information.
Don’ts:
- Don’t blame yourself or your partner: Infertility is a medical condition, not a personal failure.
- Not isolate yourself: Talk to trusted friends, family members, or a therapist about your feelings.
- Don’t compare yourself to others: Everyone’s fertility journey is unique.
- Never give up hope: Many couples facing infertility are able to conceive with the help of medical interventions or naturally over time.
- Don’t neglect your overall health: Focus on maintaining a healthy lifestyle to optimize your chances of conception.
- Don’t smoke, drink alcohol excessively, or use recreational drugs: These substances can negatively impact fertility.
- No delay In seeking help: If you have been trying to conceive for a year without success (or six months if you are over 35), consult a doctor.
- Don’t make assumptions about the cause of infertility: Many factors can contribute to infertility, so it’s important to get a comprehensive evaluation.
Remember, infertility is a common and treatable condition. With the right support and guidance, many couples are able to overcome infertility and achieve their dream of starting a family.
Terminology
Terminologies & Its Meaning
- Infertility: The inability to conceive a child after 12 months of regular unprotected sexual intercourse (or 6 months if the woman is 35 years or older).
- Primary Infertility: Infertility in a couple who has never conceived a child.
- Secondary Infertility: Infertility in a couple who has previously conceived a child.
- Ovulation: The release of an egg from an ovary.
- Fallopian Tubes: Tubes that carry eggs from the ovaries to the uterus.
- Uterus: The organ where a fetus develops.
- Endometriosis: A condition where tissue similar to the lining of the uterus grows outside the uterus.
- Polycystic Ovary Syndrome (PCOS): A hormonal disorder causing enlarged ovaries with small cysts on the outer edges.
- Male Factor Infertility: Infertility caused by problems with the male’s reproductive system, such as low sperm count or poor sperm motility.
- Assisted Reproductive Technology (ART): Medical procedures used to treat infertility, such as in vitro fertilization (IVF).
- In Vitro Fertilization (IVF): A procedure where eggs are fertilized by sperm outside the body and then implanted in the uterus.
- Intrauterine Insemination (IUI): A procedure where sperm is placed directly into the uterus around the time of ovulation.
- Ovulation Induction: Medications used to stimulate ovulation in women who do not ovulate regularly.
- Fertility Preservation: Procedures to preserve fertility in people who are undergoing medical treatments that may affect their ability to have children in the future.
- Unexplained Infertility: Infertility that cannot be attributed to a specific cause after a thorough evaluation.
Additional Terms:
- Anovulation: Absence of ovulation.
- Hysterosalpingogram (HSG): An X-ray test to check the fallopian tubes.
- Semen Analysis: A test to evaluate the quality and quantity of sperm.
- Anti-Müllerian Hormone (AMH): A hormone used to assess ovarian reserve.
- Follicle-Stimulating Hormone (FSH): A hormone that stimulates egg growth in the ovaries.
Homoeopathic Terminology
Homeopathic Remedies Frequently Mentioned in Infertility Articles:
- Sepia: Often used for women with hormonal imbalances, irregular periods, and low libido.
- Pulsatilla: Used for women with emotional sensitivity, mood swings, and changeable symptoms.
- Natrum Muriaticum: For those experiencing grief, suppressed emotions, and dryness of mucous membranes.
- Lycopodium: Suitable for men with low self-confidence, digestive issues, and right-sided complaints.
- Agnus Castus: For decreased libido and sexual function.
References
References
- DC Text book of Dutta’s Gynaecology
- https://www.drhomeo.com/homeopathic-treatment/homeopathic-medicines-infertility/
- https://www.mayoclinic.org/diseases-conditions/infertility/symptoms-causes/syc-20354317
- Nationally representative survey conducted during 2019-21 (published in 2023).
- A study published in PLOS ONE in 2023.
- Study of demographic profile and causative factor in female infertility 2023.
Speroff’s Clinical Gynecologic Endocrinology and Infertility, 9th Edition, Hugh S. Taylor, Lubna Pal, Emre Seli, 2019,Wolters Kluwer.
- Williams Obstetrics, 26th Edition,F. Gary Cunningham, Kenneth J. Leveno, Steven L. Bloom, Catherine Y. Spong, Jodi S. Dashe, Barbara L. Hoffman, Brian M. Casey, Jeanne S. Sheffield , 2020, McGraw Hill Professional.
- Infertility: A Comprehensive Text,1st Edition,Gautam N Allahbadia, 2021, Jaypee Brothers Medical Publishers.
- Comprehensive Gynecology (7th Edition), William’s Gynecology, Hoffman BL, Schorge JO, Bradshaw KD, Halvorson LM, Schaffer JI, Corton MM,2017, McGraw Hill Professional.
- Clinical Management of Infertility: Problems and Solutions, Liselotte Mettler, Martin H. Birkhäuser, 1st Edition, 2021,Springer.
- Ayurveda and Infertility: A Comprehensive Guide, Dr. Aswini Kumar Sastry,1st Edition ,2020, Chaukhambha Orientalia.
Also Search As
Infertiity Also Search As
There are several ways people can search for homeopathic articles on infertility:
Online Databases:
- PubMed: While primarily focused on biomedical literature, you can find some homeopathic studies here by using specific search terms like "homeopathy AND infertility."
- Homeopathic Journals: Many homeopathic journals have online archives that you can search directly. Some notable journals include:
- The Homeopathic Journal
- International Journal of High Dilution Research
- Homeopathy
- ClinMed International Library: This database includes articles on reproductive medicine, including some related to homeopathy.
Search Engines:
- Google Scholar: Use keywords like "homeopathy," "infertility," and "case study" or "research" to find relevant articles.
- DuckDuckGo: This search engine prioritizes user privacy and can offer a different set of results compared to Google.
Homeopathic Organizations:
- Websites of national and international homeopathic organizations often have resources, including articles and research papers on infertility.
- Some organizations to explore include:
- National Center for Homeopathy (NCH)
- American Institute of Homeopathy (AIH)
- Faculty of Homeopathy (UK)
Libraries:
- Many university libraries and some public libraries have collections of homeopathic journals and books.
Social Media:
- Homeopathic groups and forums on platforms like Facebook can be a good place to ask for recommendations on articles or research papers.
Tips for Effective Searching:
Use specific keywords: Instead of just "homeopathy and infertility," try "homeopathic treatment of PCOS infertility" or "homeopathic remedies for male infertility."
Combine search terms: Use "AND" or "+" to narrow your results (e.g., "homeopathy AND infertility AND case study").
Look for peer-reviewed articles: These have undergone a rigorous review process and are generally considered more reliable.
Check the date of publication: The field of homeopathy is constantly evolving, so newer research may be more relevant.
Frequently Asked Questions (FAQ)
What is Infertility?
Definition
Infertility define as a failure to conceive within one or more years of regular unprotected coitus.
What causes Infertility?
Causes
- Abnormal sperm production or function
- Problems with the delivery of sperm
- Overexposure to certain environmental factors
- Damage related to cancer and its treatment
- Ovulation disorders
- Uterine or cervical abnormalities
- Fallopian tube damage or blockage
- Endometriosis
- Primary ovarian insufficiency
- Pelvic adhesions
How is infertility diagnosed?
Diagnosis
Infertility is diagnosed through a comprehensive evaluation of both partners, which may include medical history, physical exams, blood tests, semen analysis, imaging studies (ultrasound, HSG), and other diagnostic tests.
Can homeopathy treat infertility?
Homoeopathy For Infertility
Homeopathy aims to stimulate the body’s innate healing abilities and address the underlying causes of infertility.While not a guaranteed cure, it has shown promising results in some cases
What are the symptoms of Infertility?
- The main symptom of infertility is not getting pregnant.
- Irregular or absent menstrual periods.
- Signs of hormonal problems
Is homeopathic treatment for infertility safe?
Homeopathic remedies are generally considered safe when prescribed by a qualified practitioner.However, it’s essential to discuss any existing medications or health conditions with your homeopath
What are the treatment options for infertility?
Treatment
depend on the underlying cause and may include lifestyle changes, medications, surgery, intrauterine insemination (IUI), in vitro fertilization (IVF), and other assisted reproductive technologies (ART).
Homeopathic Medicines used by Homeopathic Doctors in treatment of Infertility?
Homeopathic Medicines of Infertility
- Borax
- Calcarea Carbonica
- Aletris Farinosa
- Pulsatilla
- Sepia
- Agnus Castus
- Natrum Carb
- Sabal Serrulata
- Agnus Castus
Can homeopathy cure infertility?
Homeopathy aims to address the root cause of infertility by stimulating the body’s natural healing abilities. It may help improve overall health and hormonal balance, potentially increasing the chances of conception. However, it’s essential to remember that homeopathy is a complementary therapy and should not replace conventional medical treatments for infertility.
. How long does it take to see results with homeopathic treatment for infertility?
The response to homeopathic treatment varies depending on the individual, the underlying cause of infertility, and overall health. It may take several months to see significant improvements in fertility.
What lifestyle changes can support homeopathic treatment for infertility?
Maintaining a healthy weight, eating a balanced diet, managing stress, and avoiding smoking and excessive alcohol consumption can all contribute to improved fertility and support homeopathic treatment.
